Available online at www.sciencedirect.com
British Journal of Oral and Maxillofacial Surgery 52 (2014) 185–189
Distal cervical caries in the mandibular second molar: an
indication for the prophylactic removal of third molar teeth?
Update
Louis W. McArdle a,∗ , Fraser McDonald b , Judith Jones c
a
b
c
Department of Oral Surgery, KCL Dental Institute, Guy’s & St Thomas’s NHS Foundation Trust, Great Maze Pond, London SE1 9RT, United Kingdom
Department of Orthodontics, KCL Dental Institute, Guy’s & St Thomas’s NHS Foundation Trust, Great Maze Pond, London SE1 9RT, United Kingdom
Department of Oral Surgery, QMUL Dental Institute, The Royal London Hospital NHS Foundation Trust, Whitechapel, London E1 1BB, United Kingdom
Accepted 13 November 2013
Available online 7 December 2013
Abstract
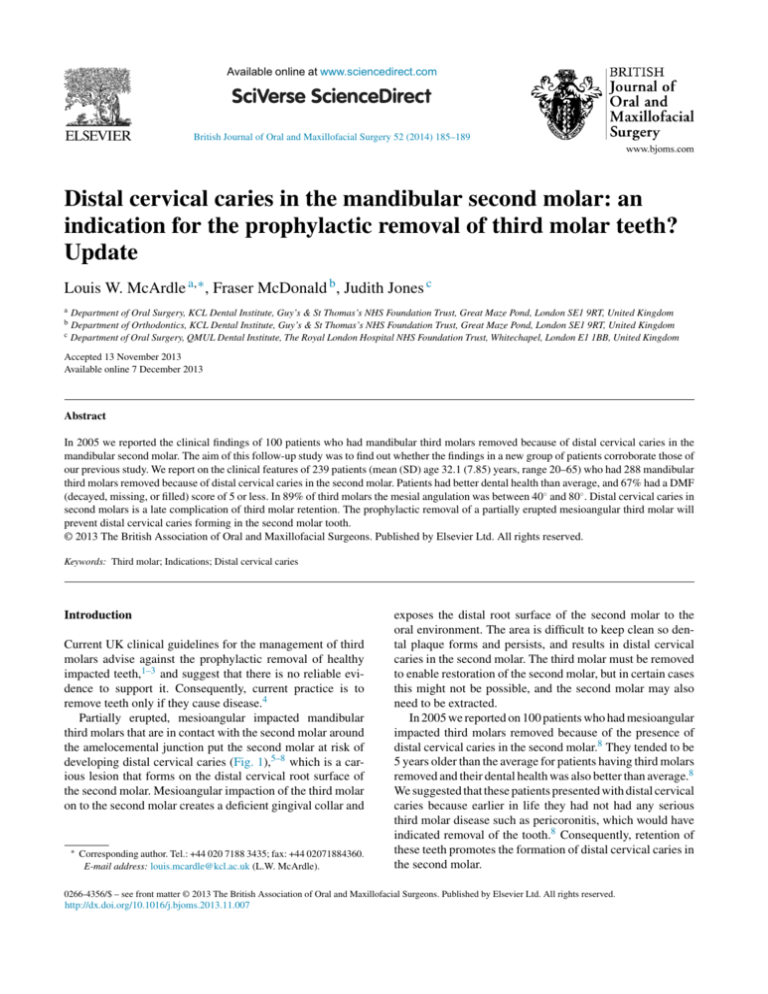
In 2005 we reported the clinical findings of 100 patients who had mandibular third molars removed because of distal cervical caries in the
mandibular second molar. The aim of this follow-up study was to find out whether the findings in a new group of patients corroborate those of
our previous study. We report on the clinical features of 239 patients (mean (SD) age 32.1 (7.85) years, range 20–65) who had 288 mandibular
third molars removed because of distal cervical caries in the second molar. Patients had better dental health than average, and 67% had a DMF
(decayed, missing, or filled) score of 5 or less. In 89% of third molars the mesial angulation was between 40◦ and 80◦ . Distal cervical caries in
second molars is a late complication of third molar retention. The prophylactic removal of a partially erupted mesioangular third molar will
prevent distal cervical caries forming in the second molar tooth.
© 2013 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
Keywords: Third molar; Indications; Distal cervical caries
Introduction
Current UK clinical guidelines for the management of third
molars advise against the prophylactic removal of healthy
impacted teeth,1–3 and suggest that there is no reliable evidence to support it. Consequently, current practice is to
remove teeth only if they cause disease.4
Partially erupted, mesioangular impacted mandibular
third molars that are in contact with the second molar around
the amelocemental junction put the second molar at risk of
developing distal cervical caries (Fig. 1),5–8 which is a carious lesion that forms on the distal cervical root surface of
the second molar. Mesioangular impaction of the third molar
on to the second molar creates a deficient gingival collar and
∗
Corresponding author. Tel.: +44 020 7188 3435; fax: +44 02071884360.
E-mail address: louis.mcardle@kcl.ac.uk (L.W. McArdle).
exposes the distal root surface of the second molar to the
oral environment. The area is difficult to keep clean so dental plaque forms and persists, and results in distal cervical
caries in the second molar. The third molar must be removed
to enable restoration of the second molar, but in certain cases
this might not be possible, and the second molar may also
need to be extracted.
In 2005 we reported on 100 patients who had mesioangular
impacted third molars removed because of the presence of
distal cervical caries in the second molar.8 They tended to be
5 years older than the average for patients having third molars
removed and their dental health was also better than average.8
We suggested that these patients presented with distal cervical
caries because earlier in life they had not had any serious
third molar disease such as pericoronitis, which would have
indicated removal of the tooth.8 Consequently, retention of
these teeth promotes the formation of distal cervical caries in
the second molar.
0266-4356/$ – see front matter © 2013 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.bjoms.2013.11.007
186
L.W. McArdle et al. / British Journal of Oral and Maxillofacial Surgery 52 (2014) 185–189
40
35
Percentage
30
25
20
15
10
5
Age range of patients (years)
Fig. 2. Age range of patients (years) compared with percentage number of
patients. Mean (SD) age 32.1 (7.85) years (range 20–65).
Fig. 1. Radiograph of distal cervical caries in the mandibular second molar
with associated impacted mesioangular third molar.
The aim of this follow-up study was to assess a further
group of patients with distal cervical caries in their mandibular second molars to find out if the findings corroborated those
of our 2005 study.
Methods
We evaluated 239 patients who had mandibular third molars
removed because of the presence of distal cervical caries in
the second molar. Data were prospectively collected over a
24-month period.
The variables that we recorded were sex, age, angulation
and eruption status of the third molar, DMF (decayed, missing, or filled) score, and the proximity of the third molar to
the amelocemental junction of the second molar.
As in our previous study, the DMF score was used as
a measure of dental health. In calculating the score we
compensated for, and excluded, the second molar if distal
cervical caries was the only lesion associated with the tooth.
The mesial angulation of the third molar was calculated by
measuring the angle of intersection between the mandibular occlusal plane and the occlusal plane of the third molar.
This angle equates to the mesial inclination of the third molar
relative to the second molar.8
All 288 teeth were partially erupted. Radiographic examination showed that all were in contact with, or close to, the
amelocemental junction of the second molar, and all were
mesioangularly impacted against the second molar. Mesial
angulations of the third molars were grouped accordingly:
255 (89%) had an angulation of between 40◦ and 80◦ ; in 28
(10%) it was less than 40◦ , and in 5 (1%) it was more than
80◦ .
Discussion
To our knowledge, distal cervical caries in the second molar
has not been reported without an associated mesioangular
third molar, and we have not observed it. Although caries
can form on the distal aspect of any tooth, distal cervical
caries is unique as it is seen at the amelocemental junction
and is, in effect, a variant of root surface caries. We think that
it would not develop without an associated impacted third
molar.
Concern has been raised that in some studies, radiographic
cervical burnout may have been misdiagnosed as distal cervical caries resulting in a higher reported incidence.9 In this
study, as in our previous study, patients whose radiographic
images suggested cervical burnout were excluded from the
study (Fig. 3).
A factor that is associated with the risk of distal cervical caries developing in the second molar is the angulation
of the third molar. This type of second molar caries is seen
Results
The study included 239 patients (142 men and 97 women).
In 190 patients, a single second molar was affected, and both
were affected in 49 (bilateral disease). In total, 288 mandibular third molars were extracted, 144 from each side.
The mean (SD) age of the patients was 32.1 (7.85) years
(range 20–65) (Fig. 2). A total of 161 patients (67%) had a
DMF score of 5 or less; 56 (23%) had a score of between 6
and 10, and 22 (9%) had a score of 11 or more. Of note, 50
patients (21%) had a compensated DMF score of zero as the
only lesion was the distal cervical caries associated with the
second molar tooth.
Fig. 3. Radiograph of radiographic distal cervical burnout potentially misinterpreted as distal cervical caries.
Mean DMF score
L.W. McArdle et al. / British Journal of Oral and Maxillofacial Surgery 52 (2014) 185–189
25
35
20
30
15
187
25
2012
10
20
mean age
(years)
ADHS 09
5
15
10
incidence (%)
of caries &
related disease
Age group (years)
5
Fig. 4. Mean DMF (decayed, missing or filled) score of patients having
third molars removed because of distal cervical caries (2012) (light blue)
compared with mean DMF score calculated from the Adult Dental Health
Survey 2009 (dark blue).15
primarily in association with mesioangular impacted third
molars and, as in other studies, we found that a mesial angulation of between 40◦ and 80◦ was common.8–14 Of the 288
third molars extracted, 255 (89%) were within this range.
Mesial angulations outwith this range and in some cases of
horizontal impaction have been associated with distal cervical caries in second molars, but it has not been seen in vertical
or disto-angular impactions.
Based on the 2009 Adult Dental Health Survey (ADHS),
the mean DMF score for patients with distal cervical caries
was less than half the mean score for similar age groups in the
general population (Fig. 4).15 This also corresponds to our
findings in 2005 which were based on the 1998 ADHS.8,16 It
supports our suggestion that patients with better dental health
are more likely to retain a partially erupted third molar later
into life, and when this is mesioangular, are at risk of distal cervical caries developing in the second molar.8 It also
contradicts the notion that susceptibility to distal cervical
caries in second molars is solely associated with an increased
susceptibility to dental caries.5–7
It is logical to assume that people with low DMF scores
have a good standard of oral hygiene and this includes the
coronal aspect of partially erupted third molar teeth. Good
oral hygiene minimises the likelihood of pericoronitis and
results in the long-term retention of such teeth, but in the
case of a mesioangular third molar and a second molar with
a distal cervical root exposed to the oral cavity, distal cervical caries is a potential outcome. It seems to develop in
older patients and this may be reflected in the protracted time
it takes for dental caries to form compared with the time
it takes for pericoronitis to develop after a third molar has
erupted.8,17
The mean age of patients in this study was 32.1 years
(range 20–65), which is comparable with the mean age
(32 years) for all patients who have third molars removed
in the UK.18,19 In our previous study patients with distal cervical caries tended to be 5 years older than average
whereas this study suggests that they are similar in age.19
This may be because in the UK, the introduction of third
molar guidelines by the National Institute for Health and
Care Excellence (NICE) and others has resulted in a shift
0
Year
Fig. 5. Increasing percentage incidence of caries and related disease (blue
line) as main indication for removal of third molars, and increase in mean
age of patients (orange line) having third molars removed.18,19
away from the prophylactic removal of third molars, primarily in younger patients, to removal based on definitive
clinical indications.1–4,19 The consequence of this has been an
increase in the mean age of patients from 28 to 32 years.18,19
The incidence of third molars being removed because of
caries and related sequelae such as periapical infection has
also increased from 4% to about 30% (Fig. 5).18,19 The mean
age in our group suggests a relation with an increased mean
age and a higher incidence of third molar caries in general,
as is the case with an increasing incidence of distal cervical
caries in older patients.17,19
It is not possible to isolate data from NHS agencies on
caries that solely affect the third molar or on distal cervical
caries of the second molar that is attributed to the third molar,
but the general trend of an increase in caries related to third
molars is noteworthy.18,19 Distal cervical caries in second
molars in association with impacted third molars is becoming
more widely reported, and is not isolated to any specific racial
group.10–14 Recent studies have reported an incidence of up
to 20% in patients having third molars assessed, and some
report an incidence of about 40% in mesioangular impacted
third molars.10,11
Older studies report a mean age of around 25 years for
patients having third molars removed, and report pericoronitis as the most common indication.20–24 As these studies
were published when the prophylactic removal of third
molars in younger patients was common, their mean age
was lower.20–24 The incidence of third molars being removed
because of caries in younger patients is relatively low, and
historically the reported incidence of distal cervical caries in
second molars in these patients has also been relatively low
(2–5%).8,17,19,20
As distal cervical caries is responsible for a rising percentage of third molars being removed we think that there is
a high risk of it developing in a second molar.10–14,17 However, pericoronitis is still the most common indication for
the removal of third molar teeth, and it is diagnosed more
often in younger patients.5,7,17,20,23,24 In these patients the
extraction of mandibular mesioangular third molars removes
188
L.W. McArdle et al. / British Journal of Oral and Maxillofacial Surgery 52 (2014) 185–189
the main contributing factor for distal cervical caries in the
second molar. If pericoronitis was less common in younger
patients then more third molar teeth would be retained later
into life. As a consequence, we suggest that the incidence
of distal cervical caries in the second molar will rise accordingly, as is the case with that of general caries that are related
to third molars in older patients.17–19
We need to consider whether all partially erupted mesioangular third molars would eventually cause distal cervical
caries in the second molar. A study of this latent potential
would require the enforced retention of a mesioangular third
molar to observe its effect on the adjacent tooth, but this
would be unethical and unavoidably protracted over many
years. The introduction of clinical guidelines such as NICE
has resulted in an older patient population whose third molars
are retained until specific problems indicate their removal. In
some respects the patient whose third molar is retained later
into life is acting as their own control to the long term consequences of retention as is demonstrated by the increasing
incidence of third molar caries (4-30%) correlating with the
increasing mean age of patients (Fig. 5).
The potential risk of distal cervical caries forming in second molar teeth that are associated with mesioangular third
molars presents a clinical dilemma: should the third molar
be left until disease develops, or should it be removed, and if
so, when? Clinical risk should influence the decision and the
relative risk – for example, of nerve damage, is an important
consideration. Early removal of a third molar with a high risk
of injury to the inferior dental nerve may not be prudent and
in such a case alternative options such as coronectomy could
be considered.
Conclusion
We do not think that all third molars should be removed prophylactically, but early, prophylactic removal of a partially
erupted mesioangular mandibular third molar will prevent
distal cervical caries forming in the adjacent tooth. Mesioangular third molars will not always cause distal cervical caries
to form as many will be removed because of pericoronitis and
other diseases before it ensues, but we do suggest that every
partially erupted mesioangular third molar has this potential. Only with further research and debate will we know
whether or not targeted prophylactic removal of such teeth
is acceptable. The cost–benefit and cost–effectiveness of this
are complex issues and are out of the sphere of this paper,
but prophylactic removal will be explored in further ongoing
research.
The results of our 2 studies and others confirm that distal cervical caries in the second molar is associated with the
retention of a partially erupted mesioangular third molar tooth
into later life.8,10–14 As this study corroborates our previous findings we suggest that the conservative management
of disease-free, partially erupted, mesioangular mandibular
third molars may be detrimental to dental health.
Conflict of interest
None.
Ethics statement
Not required.
References
1. National Institute for Clinical Excellence. Guidance on the removal
of wisdom teeth. Available from: http://www.nice.org.uk/nicemedia/
pdf/wisdomteethguidance.pdf [March 2000].
2. Scottish Intercollegiate Guidelines Network. Management unerupted
and impacted third molar teeth. Available from: http://www.sign.ac.uk/
pdf/sign43.pdf [September 1999].
3. Prophylactic removal of third molars: is it justified? Effectiveness Matters, Vol. 3. University of York: NHS Centre for
Reviews and Dissemination; 1998. Available from: http://www.york.
ac.uk/inst/crd/EM/em32.pdf
4. Mettes TD, Ghaeminia H, Nienhuijs ME, Perry J, van der Sanden WJ,
Plasschaert A. Surgical removal versus retention for the management
of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev
2012;6:CD003879.
5. van der Linden W, Cleaton-Jones P, Lownie M. Diseases and lesions
associated with third molars. Review of 1001 cases. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod 1995;79:142–5.
6. Current clinical practice and parameters of care: the management of patients with third molar (syn: wisdom) teeth. Faculty
of Dental Surgery of the Royal College of Surgeons of England.
Available from: http://www.rcseng.ac.uk/fds/publications-clinical[September
guidelines/clinical guidelines/documents/3rdmolar.pdf
1997].
7. Knutsson K, Brehmer B, Lysell L, Rohlin M. Pathoses associated with
mandibular third molars subjected to removal. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 1996;82:10–7.
8. McArdle LW, Renton TF. Distal cervical caries in the mandibular second
molar: an indication for the prophylactic removal of the third molar? Br
J Oral Maxillofac Surg 2006;44:42–5.
9. Littler B. X-ray burn out. Br Dent J 2009;207:194.
10. Ozeç I, Hergüner Siso S, Taşdemir U, Ezirganli S, Göktolga G. Prevalence
and factors affecting the formation of second molar distal caries in a
Turkish population. Int J Oral Maxillofac Surg 2009;38:1279–82.
11. Chang SW, Shin SY, Kum KY, Hong J. Correlation study between distal
caries in the mandibular second molar and the eruption status of the
mandibular third molar in the Korean population. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod 2009;108:838–43.
12. Allen RT, Witherow H, Collyer J, Roper-Hall R, Nazir MA, Mathew
G. The mesioangular third molar—to extract or not to extract? Analysis
of 776 consecutive third molars. Br Dent J 2009;206:E23, discussion
586–7.
13. Falci SG, de Castro CR, Santos RC, et al. Association between the presence of a partially erupted mandibular third molar and the existence of
caries in the distal of the second molars. Int J Oral Maxillofac Surg
2012;41:1270–4.
14. Oderinu OH, Adeyemo WL, Adeyemi MO, Nwathor O, Adeyemi
MF. Distal cervical caries in second molars associated with impacted
mandibular third molars: a case–control study. Oral Surg Oral Med Oral
Pathol Oral Radiol 2012. PMID: 22981096 [Epub ahead of print].
15. Health & Social Care Information Centre. Adult dental health survey.
London: HMSO; 2009. Available from: http://www.ic.nhs.uk/statisticsand-data-collections/primary-care/dentistry/adult-dental-health-survey2009–summary-report-and-thematic-series [March 2011].
L.W. McArdle et al. / British Journal of Oral and Maxillofacial Surgery 52 (2014) 185–189
16. Office for National Statistics. Adult dental health survey (1998): oral
health in the United Kingdom, 1998. London: HMSO; 2000.
17. Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc
1980;101:240–5.
18. Health & Social Care Information Centre. Hospital episodes statistics.
HES online. Available from: www.hesonline.nhs.uk
19. McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J 2012;213:E8.
20. Brickley MR, Shepherd JP. An investigation of the rationality of lower
third molar removal, based on USA National Institutes of Health criteria.
Br Dent J 1996;180:249–54.
189
21. Chiapasco M, De Cicco L, Marrone G. Side effects and complications
associated with third molar surgery. Oral Surg Oral Med Oral Pathol
1993;76:412–20.
22. de Boer MP, Raghoebar GM, Stegenga B, Scheon PJ, Boering G. Complications after mandibular third molar extraction. Quintessence Int
1995;26:779–84.
23. Nordenram Å, Hultin M, Kjellman O, Ramström G. Indications for surgical removal of the mandibular third molar. Study of 2,630 cases. Swed
Dent J 1987;11:23–9.
24. Lysell L, Rohlin M. A study of indications used for removal of
the mandibular third molar. Int J Oral Maxillofac Surg 1988;17:
161–4.