Colonic Hydrotherapy
advertisement

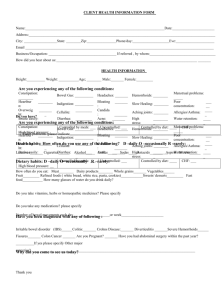
Colonic Hydrotherapy; should we take another look? Colonic irrigation is an old technique that has retained its popular appeal despite intense scepticism on the part of the medical profession. It harks back to the time when the great and the good would flock to the spas of Europe to cleanse mind and body by taking the water cure. Even Charles Darwin used to travel north to Ilkley to partake of the health giving waters that issued from the springs where ailing swains would court their Mary Janes. It has resonances with Sir Arbuthnot Lane, London Surgeon, who would remove the colon at the drop of a purse for anything from short sightedness to knock knees. Then, the rage was auto-intoxication. Encouraged by Nobel prizewinner, Eli Metchnikoff, many believed that the colon was a Stygian morass of stinking corruption which could not fail to damage the body politic. Fast forward a hundred years and more bottles of health restoring live yoghurts than glasses of Guinness are consumed every day to maintain a healthy colonic culture, and Colonic Hydrotherapy outlets are springing up on every High Street of every small town in the Kingdom. There’s nothing new, just different ways of doing it! The colonic ecosystem is perhaps the most rapidly evolving field of research in gastroenterology An adverse population of colonic microflora has been implicated not only in colitis, but also Rheumatoid Arthritis, Parkinson’s Disease, Depression, Heart Attacks and even the epidemic of Obesity (see GR 80). Come back Eli; all is forgiven! So is it time to take another look at Colonic Hydrotherapy? Anne-Lise Miller, has been a qualified Nutritionist and Colonic Hydrotherapy Practitioner and Teacher since 1991 and is currently honorary secretary to The Institute of Professional Colon Hydrotherapy. www.cleansingforlife.co.uk www.colonicpracticelondon.co.uk She writes; ‘Colonic hydrotherapy is more than a procedure to cleanse the colon. It is an approach to health and wellbeing that looks at the individual interactions between the physical, emotional and chemical functions of the body in the context of genetic inheritance and cultural background. When supported by a sensitive approach and sound dietary/ lifestyle recommendations, colonic hydrotherapy can be an effective tool for the management and treatment of IBS, constipation and flatulence. It can also be used as part of a weight loss regimen.’ ‘During colonic hydrotherapy, a short tube (2” inches long and 3/4” diameter) is introduced into the rectum and then water warmed to body temperature is gradually infused. The amount of water is the minimum to induce peristalsis. With the aid of gentle massage, breathing and posture, the fluid gently stretches and stimulates the colon and then is allowed to drain out through the same tube along with any faecal material. The procedure may be repeated several times unto the fluid leaving the bowel is clean. There is no obvious smell or direct contact with faeces.’ Ms Miller further adds that, ‘Addition of herbal tinctures, colloidal minerals and salts to the water maintains a healthy colonic environment, while antihelminthics may be used to eliminate parisites. Speedy removal of ‘toxic’ bowel content coupled with dietary interventions and probiotic implants after irrigation restore a healthy colonic bacterial flora. Colonic hydrotherapy raises awareness of gut function and evacuation, bringing about a state of general wellbeing, which can reinforce a positive change of behavior and eating habits. It’s much more than a colonic washout; it’s a holistic therapy’ Colonic therapists take a careful history from the patient enquiring not only about bowel function, abdominal symptoms, but also chronic disease, family history, diet and life style, life situation and events and attitudes towards defaecation. They also examine the patient noting their client’s posture especially during defaecation, their breathing, the tone and function of the pelvic floor and any pain or lesions delaying defecation.’ Ms Miller claims that ‘Colonic hydrotherapy is a safe procedure and I know of no recorded cases of adverse reactions from colonic treatments administered by trained and competent therapists.’ Occasionally distension of the colon may lead to faintness because of a vasovagal drop in blood pressure. Water intoxication is avoided by increasing the osmotic pressure of the fluid. Either pumps or gravity is used to deliver filtered water at low pressure through disposable tubing.’ ‘The procedure is not carried out if the patient has anal fissures, fistulae or severe haemorrhoids. Hernias should be treated and abdominal surgery healed before the procedure is carried out. Caution must be applied if the patient has liver/kidney disease, pregnancy and hypertension. If there is any doubt about the safety of the procedure, she asserts, a physician’s consent should be obtained.’ Colonic therapists should be qualified and registered. Currently organizations that govern colonic hydrotherapy are self-regulated. Consequently it behoves the patient to evaluate the therapist and their training. The things to enquire about are: 1. registration to an organisation will ensure standards of hygiene and insurance as well as a desire from the therapist to maintain professional standard. 2.if they use disposable speculum and tubing. 3.the length of appointment times (should be over 60 minutes) ARCH (Association of Colonic Hydrotherapists; http://www. colonic-association.org/) is the biggest organisation for colonic hydrotherapists in the UK. It runs assessments on the approved training colleges and is selective about its member’s background favoring nurses and regarding colonic hydrotherapy as a semi-medical intervention. IPCH (Institute of Professional Colonic Hydrotherapy; http:// www.ipch.org.uk/) is much smaller, but maintains excellent standards and adopts a holistic and personal, client centred approach. This all sounds very fair and responsible. Nevertheless, colonic hydrotherapy is not generally approved by the medical profession. We asked Dr Anton Emmanuel, Gastroenterologist, international expert on IBS, and a member of our professional advisory panel, why. As regards safety, those studies have shown a 1 in 100,000 perforation rate. So, no matter how careful the practitioner it is not possible to guarantee that no harm could be done with irrigation. The process of introducing 2 litres of hypertonic solution “several times” until the effluent is clear could be a concern in patients with sub-clinical incipient renal or heart failure. The use of irrigation as part of weight loss is also something that could be considered abusive in patients with eating disturbances, and extreme caution must be advocated in this group of vulnerable patients.’ It can be dreadful to be bunged up with constipation. The feeling of frustration and rectal discomfort, the heaviness, slowness, inertia, hopelessness, the bad breath, bloatedness, can really get you down. You would do anything to get rid of it, wouldn’t you? Colonic hydrotherapy offers a solution; just clean it all out! No wonder it’s so popular. But how many of those symptoms are the direct result of faecal retention and how many the feelings that cause it? And to what extent is colonic hydrotherapy an elaborate placebo? And does that matter if it works? Resolution must hinge on appropriate regulation and safety. Have you undergone colonic hydrotherapy or irrigation? What was your experience? We’d love to know. Do you think more efforts should be made towards effective regulation? We’d love to know. Do write in with your comments and we’ll print a report in the next issue of Gut Reaction. maintain your Intestinal comfort ‘The problem is with the concept not the professional’, he replied. I’m sure that most colonic hydrotherapists are well meaning and responsible practitioners. If you remove all mention of bowel irrigation from Ms Miller’s piece, you are left with all the basics of an effective consultation. But what of the procedure? It could be argued that it is more the combination of antihelminthics and probiotics that are responsible for maintaining a healthy colonic environment than the colonic irrigation, but it would be inaccurate for patients to believe that they need to have colonic irrigation in order to get the benefits of probiotics. I know of no research that shows which patients are likely to benefit from colonic hydrotherapy in the absence of the package of care outlined above. The medical literature is moving towards considering faecal transplants for some conditions - seemingly the opposite of irrigation – and subgroups of responders are being defined. Perhaps a similar trial design could be used to assess the true efficacy of colonic irrigation. Transanal irrigation using self-administered medical devices has been assessed in patients with neurological disease and associated bowel dysfunction and demonstrates efficacy in about two-thirds of patients, but the procedure differs from the form of irrigation being described by Ms Miller. Bimuno Supports 2 www.thegutrust.org