PIV-Measured Versus CFD-Predicted Flow Dynamics in
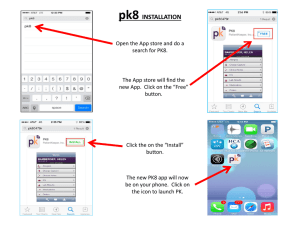
advertisement

PIV-Measured Versus CFD-Predicted Flow Dynamics in Anatomically-Realistic Cerebral Aneurysm Models Matthew D. Ford1,2,6, Hristo N. Nikolov1, Jaques S. Milner1, Stephen P. Lownie1,3, Edwin M. DeMont4, Wojciech Kalata5, Francis Loth5, David W. Holdsworth1,2, David A. Steinman1,2,6 1 2 Imaging Research Laboratories, Robarts Research Institute, London, Canada Departments of Medical Biophysics and 3Clinical Neurological Sciences, The University of Western Ontario, London, Canada 4 5 Department of Biology, Saint Francis Xavier University, Antigonish, Canada Department of Mechanical Engineering, University of Illinois at Chicago, Chicago, USA 6 Biomedical Simulation Laboratory, University of Toronto, Toronto, Canada Journal of Biomechanical Engineering, Accepted June 8, 2007 Address correspondence to: David A. Steinman University of Toronto 5 King’s College Road Toronto, Ontario, Canada M5S 3G8 Tel: 416-978-7781 Fax: 416-978-7753 Email: steinman@mie.utoronto.ca PIV vs. CFD of Realistic Aneurysm Models ABSTRACT Background: Computational fluid dynamics (CFD) modeling of nominally patient-specific cerebral aneurysms is increasingly being used as a research tool to further understand the development, prognosis, and treatment of brain aneurysms. We have previously developed virtual angiography to indirectly validate CFD-predicted gross flow dynamics against the routinely acquired digital subtraction angiograms. Towards a more direct validation, here we compare detailed, CFD-predicted velocity fields, against those measured using particle imaging velocimetry (PIV). Methods of Approach: Two anatomically-realistic flow-through phantoms, one a giant internal carotid artery (ICA) aneurysm and the other a basilar artery (BA) tip aneurysm, were constructed of a clear silicone elastomer. The phantoms were placed within a computer-controlled flow loop, programmed with representative flow rate waveforms. PIV images were collected on several anterior-posterior (AP) and lateral (LAT) planes. CFD simulations were then carried out using a well-validated, in-house solver, based on micro-CT reconstructions of the geometries of the flow-through phantoms and inlet/outlet boundary conditions derived from flow rates measured during the PIV experiments. Results: PIV and CFD results from the central AP plane of the ICA aneurysm showed a large stable vortex throughout the cardiac cycle. Complex vortex dynamics, captured by PIV and CFD, persisted throughout the cardiac cycle on the central LAT plane. Velocity vector fields showed good overall agreement. For the BA aneurysm agreement was more compelling, with both PIV and CFD similarly resolving the dynamics of counter-rotating vortices on both AP and LAT planes. Despite the imposition of periodic flow boundary conditions for the CFD simulations, cycle-to-cycle fluctuations were evident in the BA aneurysm simulations, which agreed well, in terms of both amplitudes and spatial distributions, with cycle-to-cycle fluctuations measured by PIV in the same geometry. Conclusions: The overall good agreement between PIV and CFD suggests that CFD can reliably predict the details of the intra-aneurysmal flow dynamics observed in anatomically-realistic in vitro models. Ford MD et al. 2 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Nevertheless, given the various modeling assumptions, this does not prove that they are mimicking the actual in vivo hemodynamics, and so validations against in vivo data are encouraged whenever possible. Keywords: cerebral aneurysm, computational fluid dynamics, particle image velocimetry, anatomic realism Ford MD et al. 3 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models INTRODUCTION Brain aneurysms occur in approximately 5% of the population [1] and, with improvements in the quality and availability of medical imaging, the number of detected unruptured brain aneurysms is on the rise [2]. Interventionalists are faced with the fundamental question of when and if to treat an unruptured brain aneurysm, because the risks of treatment potentially outweigh the risk of rupture. When the decision to intervene has been made, the primary question is when to clip vs. coil [3,4]. When coiling is selected, interventionalists are left with concerns related with the sufficiency of packing density to prevent aneurysm regrowth and coil compaction [5-7]. It is widely believed that an understanding of aneurysmal blood flow dynamics can enhance clinical decisions [8]; however, medical imaging alone is not yet able to provide the anticipated necessary hemodynamic information. Instead, computational fluid dynamics (CFD) may provide the ideal tool to help tackle these and other problems related to cerebral aneurysms. Advances in medical imaging and vessel segmentation/reconstruction algorithms have led to increasingly widespread use of CFD modeling of so-called “patient-specific” cerebral aneurysm hemodynamics [9-12]. Cebral et al. have recently demonstrated the development of an efficient pipeline for the CFD simulation of large numbers of aneurysms [13], with the eventual possibility of determining hemodynamic risk factors implicated in a high probability of rupture [14]. CFD has been used to infer the effects of endovascular therapy on hemodynamics in idealized brain aneurysm models [15-18], and is being proposed as a tool for patient-specific testing and treatment planning of endovascular devices [19]. While such CFD models are compelling in their detail and enticing in their potential to improve our understanding of aneurysm development and treatment, to our knowledge there have been no attempts to validate their predictions against independent experimental measurements. Recent work from our group has demonstrated that so-called virtual angiography can be used to indirectly validate patient-specific CFD models against clinical digital subtraction angiography (DSA) Ford MD et al. 4 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models data [20]. However, DSA is only a two-dimensional projection of a three-dimensional flow field, and agreement with DSA does not necessarily mean agreement in the underlying three-dimensional flow dynamics. A preliminary study has shown good agreement between in vitro and CFD-derived particle visualizations of steady flow in an anatomically-realistic aneurysm model [21]. In this study we use particle image velocimetry (PIV) to more directly validate the detailed velocity fields predicted by CFD models of pulsatile flow in two anatomically-realistic cerebral aneurysms. METHOD OF APPROACH Two anatomically-realistic model geometries were used in this study: a giant internal carotid-posterior communicating artery (ICA) aneurysm and a basilar artery tip (BA) aneurysm. The giant ICA aneurysm was chosen as a subject because we have studied it previously in great detail [9,20,21]. The BA aneurysm was selected because of the nominally more challenging hemodynamics found at the basilar tip location; with the potential for flow instability [22], the BA aneurysm was considered a “worst case scenario”. Using the lumen surface triangulation derived from computed rotational angiography (CRA) [23] of the respective patients, and previously employed to generate a CFD model of the ICA aneurysm [9], we produced a stereolithography file, from which a positive of the lumen was constructed of acrylonitrile butadiene styrene (ABS), using a fused-deposition rapid prototyping system (Stratasys FDM 1650; Stratasys, Eden Prairie, MN) [24]. After smoothing to remove roughness of the deposited layers, a negative mould was created, from which a wax positive was cast. The wax core was embedded into a silicone elastomer (Sylgard 184; Dow Corning, Midland, MI) and then removed after the elastomer solidified, leaving the rigid, transparent, life-sized, flow-through phantom [25,26] shown in Figure 1. The BA phantom, also shown in Figure 1, was constructed similarly, but at twice life-size to compensate for its small size in vivo and so allow for equivalent-quality PIV experiments. The nominal Ford MD et al. 5 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models inlet diameters of the ICA and BA phantoms, measured from the wax positive cores, were 4.25 mm and 4.1 mm. The phantoms were placed in a flow loop, driven by a computer-controlled flow pump (RG Shelley Limited, North York, ON) programmed with a representative flow rate waveform shape [27]. Care was taken to ensure that the tubing to the inlet and from each of the outlets was straight and level, to allow for the later prescription of fully-developed flow to the CFD models. To allow for later phase averaging and statistical analysis of data acquired from multiple cycles, the pump was also programmed with a five-volt trigger to signal the PIV system to begin collecting data starting from the same point in each cardiac cycle. Although care was taken to precompensate the programmed waveforms for anticipated damping and dispersion due to compliance and wave reflections in the flow loop [28], ultimately the inlet and outlet flow rates were measured using an electromagnetic (EM) flow meter (Carolina Medical Electronics Inc., King, NC) in combination with a Power Lab A/D converter (ADInstruments, Colorado Springs, CO). The working fluid used in the experiment was a 50:50 mixture (by volume) of water:glycerol, having a nominal viscosity of 6.2 mm2/s. [29]. This mixture was found to minimize the effects of refraction on the imaging planes during the PIV experiment, as evidenced by visual inspection of the filled phantom against a grid [30]. The working fluid also contained 0.5% salt (by volume), required to run the EM flowmeter, and was seeded with 10 μm hollow glass spheres (Dantec Dynamics, Skovlunde Denmark), used as the imaging particles by the PIV system. Based upon the nominal inlet diameters, fluid viscosity, and an assumed heart rate of 60 beats-per-minute, the nominal mean flow rate was set to 8 mL/s, with periods of 0.56 s and 0.98 s for the ICA and BA cases respectively. This resulted in Reynolds and Womersley numbers of 387 and 2.85, respectively, for the ICA model, and 401 and 2.08, respectively, for the BA model, well within the range of in vivo values [31]. For the PIV acquisitions a New Wave Solo PIV research laser (Dantec Dynamics, Skovlunde, Denmark) was used to provide a nominal 1-mm thick laser sheet through the plane of interest, Ford MD et al. 6 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models illuminating the hollow glass particles. The laser was synchronized to a 1-megapixel digital camera (Megaplus ES 1.0; Eastman Kodak Co., Rochester, NY) mounted above the phantom. Image pairs were collected at a rate of 15 Hz, with the time between the two images within a pair (i.e., between successive laser pulses) fixed at 250 μs. This frame rate allowed for 8 frames per cardiac cycle to be collected for the ICA case and 14 frames per cycle for the BA case. To allow for later quantification of any fluctuations that might have occurred between cycles, a total of 8 cardiac cycles were collected for each plane of the ICA phantom, and 9 cycles for the BA phantom. In the case of the ICA phantom, the 8 cycles of data were collected in one continuous acquisition. Due to memory limitations and the increase in the number of frames collected per cycle, for the BA phantom, the data were collected in three separate runs of three cycles each. The image fields-of-view were: 33.4 x 33.7 mm2 for the ICA phantom AP planes; 37.1 x 37.4 mm2 for the ICA phantom LAT planes; 35.1 x 35.3 mm2 for the BA phantom AP planes; and 34.3 x 34.5 mm2 for the BA phantom LAT planes. Images were collected on five separate planes: first on the nominal central plane, followed by two planes each above and below the central plane (Figure 2). The spacing between the planes was not fixed; instead, planes were selected to focus on the most interesting fluid dynamic regions by inspection. Images were uploaded from the camera to a PIV 2000 processor (Dantec Dynamics, Skovlunde, Denmark) after each run, and then transferred and stored on a personal computer for later data analysis. Analysis of the particle-image pairs began with the manual creation of a mask to be placed over the particle images, to remove unwanted background signal. The masked imaged pairs were then analyzed on the PIV 2000 processor using the supplied cross-correlation algorithm. The interrogation regions were set at 32 x 32 pixels with a 25% overlap between neighboring interrogation regions, in both the horizontal and vertical directions. The resulting in-plane velocity data were output onto a 41 x 42 grid. Velocity vectors were phase averaged over the collected cycles to produce velocity vector plots for each Ford MD et al. 7 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models acquired phase of the cardiac cycle. To quantify fluctuations at each phase, the velocity magnitude at each point was calculated, from which the phase average and standard deviation were calculated. To account for any geometrical changes that might have been introduced during the fabrication process, the flow-through phantoms were scanned on a conebeam flat-panel micro-CT scanner (Locus Ultra, GE Healthcare Biosciences, London, ON) with 0.15 mm isotropic voxel spacing. To generate sufficient lumen contrast, phantoms were filled with a 1:2 (by volume) mixture of saline and Omnipaque 300 contrast agent (Nycomed Imaging AS, Oslo, Norway). The lumen boundary was extracted from the resulting high-resolution volume image data and then triangulated using level-set and marching-cube algorithms [32]. The triangulated surface mesh was then passed to ICEM CFD (Ansys Inc, Canonsburg, PA) and a volume mesh was created. In this manner the silicone phantom geometry and the geometry used for the CFD simulations were assured to be equivalent. From the reconstructed micro CT data the diameters of the parent arteries of the ICA and BA phantoms were found to be 4.18 mm and 3.75 mm, respectively, within 10% of the nominal values based on the wax positive cores. The viscosity of the working fluid, which was initially estimated from an engineering handbook [29], was measured using a Cannon-Fenske Routine Viscometer (Model 100, Cannon Instrument Co., College Park, PA). The viscosity was measured a total of six times and the first two measurements were discarded due to a thin film of water initially present on the working surface of the viscometer. The fluid was found to have a measured viscosity of 7.41 ± 0.05 mm2/s (n = 4), significantly higher than the assumed viscosity of 6.2 mm2/s. The EM-flowmeter-measured inlet and outlet flow rates (Figure 3) were phase averaged over ten cycles and the mean inlet flow rates were found to be 7.92 mL/s and 8.37 mL/s for the ICA and BA phantoms, respectively, within the 0.4 mL/s cycle-to-cycle reproducibility of the pump [28]. These differences in the artery inlet diameters and mean inlet flow rates, combined with the error in the assumed viscosity of the working fluid, led to actual Ford MD et al. 8 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Reynolds and Womersley numbers of 326 and 2.6, respectively, in the ICA model and 384 and 1.75, respectively, in the BA model, still within the normal physiological range. With the modeling parameters and geometry correctly determined, CFD simulations were carried out using a well-validated, in-house CFD solver [33-35]. The CFD simulation assumed Newtonian fluid and rigid walls, and were constrained by imposing, at the inlet and all but one outlet, fully developed velocity boundary conditions based on the waveforms measured during the PIV experiment. Tractionfree boundary conditions were imposed at the remaining outlet. Owing to slight differences between the measured inflow and total outflow, the outlet waveforms actually imposed on the CFD model were based on scaling the inlet waveform by the respective instantaneous outlet flow divisions [36]. Flow extensions, each 8× the inlet diameter in length, were added to the inlets and each of the outlets to match the nominal fully-developed flows entering and exiting the in vitro models.. The CFD meshes of the ICA and BA aneurysm geometries were composed of 373,000 and 470,000 quadratic tetrahedral elements, respectively, corresponding to an average node spacing of roughly 0.25 mm. This resolution was chosen based on mesh refinement studies previously carried out for the ICA aneurysm model [9]. In order to meet the stability criteria of our CFD solver, the number of uniform time steps per cardiac cycle was set to 9600. At these fine spatial and temporal resolutions, typical run times were on the order of 5 CPU-days/cycle on a 1.5 GHz Intel Itanium 2 processor. Each simulation was run for at least three cycles to allow any initial transients to die down, followed by 8 (or 9) cycles to match the number of cycles collected during the ICA (or BA) aneurysm PIV measurements. In order to facilitate a direct comparison of the CFD-predicted flow fields with the PIV-measured flow fields, the matching planes in the CFD model first had to be identified. This was done by manually slicing through the CFD geometry, using 1-mm-thick, and comparing geometric features from the lumen boundary with those present in the PIV-collected raw particle images. Once the correct plane was determined, the CFD data were re-sampled onto a grid with the same spacing and field-of-view as the Ford MD et al. 9 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models PIV data set. The re-sampled CFD data were then put through the same analysis as the PIV data set to calculate the average in-plane velocity components as well as the velocity magnitudes and corresponding standard deviations. RESULTS The aim of this work was to show that CFD could accurately capture complex aneurysmal flow dynamics in two anatomically-realistic, flow-through phantoms under pulsatile flow conditions. The first subject of the study was a giant ICA aneurysm phantom. PIV velocity data were extracted on five planes in both the AP and LAT views, and their locations can be seen in Figure 2. Owing to space limitations, the results presented here will focus on the nominal central plane (plane 1) and an off-axis plane (plane 4) which exhibited unique and interesting flow dynamics.* As shown in Figures 4A,B, the central AP plane of the ICA aneurysm is dominated by the circulation of flow down the left side of the aneurysm and then up through the middle. Within this appear two persistent, counter-rotating vortices: one in the aneurysm's lower half; and another in the upper half, which CFD predicts to be stronger and displaced relative to the location in the corresponding PIV frame. CFD predicts a third, persistent vortex at the top right, which is associated with the strong, helical flow entering the aneurysm from the parent artery. This vortex and the high-speed flow down the left side of the aneurysm at peak systole (Figure 4A, arrow) are not captured by PIV, for reasons discussed later. During late diastole, there is also some discrepancy between the direction of flow up the middle of the aneurysm (Figure 4B, arrows). On the off-center AP plane 4 (Figures 4C,D), the general flow patterns are consistent between CFD and PIV, notably the persistent, counter-clockwise vortex at the bottom of the aneurysm. Again, however, CFD predicts stronger flow from the top right and around the left side of the aneurysm compared to PIV, and higher velocity magnitudes up the middle of the aneurysm during late diastole (Figure 4D, arrows). * PIV data from all planes, as well as volumetric CFD data, are available at http://www.mie.utoronto.ca/labs/bsl/data.html. Ford MD et al. 10 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models The flow patterns on LAT plane 1 of the ICA phantom (Figure 5A,B) are more complex than those on the corresponding AP plane, with two vortices evident: one on the left side of the aneurysm just above the bleb; and a second at the bottom of the aneurysm. PIV did not capture the complete details of the second vortex structure in the bottom region of the aneurysm, due to the near-wall limitation discussed later. At peak systole there was a large area, in the bottom right of the aneurysm, where the PIV-measured flow patterns disagreed with those predicted by CFD (Figure 5A, arrows). The major area of discrepancy during late diastole was at the bottom right of the aneurysm, where CFD overestimated the velocity magnitudes measured by PIV (Figure 5B, arrows). The results for LAT plane 2 (Figure 5C,D) show flow moving from the top left to the bottom right of the aneurysm. CFD accurately captures the area of slow flow in the bottom right corner of the aneurysm, but generally over-predicts the velocity magnitude in the bottom half of the aneurysm (Figure 5C,D, arrows). For the AP and LAT planes of the ICA model not presented here, CFD-predicted and the PIV-measured flow patterns showed similar levels of agreement. The second subject of this study was the twice-life-size BA aneurysm model. PIV velocity measurements were made on five separate planes in each of the AP and LAT orientations (Figure 2). On LAT plane 1, flow is dominated by a single, large, clockwise-rotating vortex (Figure 6A,B), which is generated by the high-speed flow entering along the left wall of the aneurysm and looping all the way around the aneurysm and out. A second, smaller vortex is formed in the upper left corner of the aneurysm; this is only partially captured by PIV, due to near-wall limitations. On LAT plane 4, (Figure 6C,D), a large vortex is present in the bottom three quarters of the aneurysm, while a smaller vortex is again present at the upper left. As shown in Figure 7A,B, flow on AP plane 1 is dominated by a pair of counter-rotating vortices present in the top half of the aneurysm. CFD not only accurately captures these vortices; it accurately predicts their development throughout the cardiac cycle. At late diastole the only area of discrepancy is Ford MD et al. 11 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models located in the upper right of the aneurysm bulb, where CFD overestimates the PIV-measured velocity magnitude (Figure 7B, arrows). At peak systole, AP plane 4 is also dominated by a pair of counterrotating vortices in the upper half of the aneurysm bulb. At late diastole CFD accurately captures the dissociation the upper left vortex and the reduction of flow magnitude and change of position of the upper right vortex. On the other hand, at peak systole CFD under-predicts the velocity magnitude on the right side of the aneurysm (Figure 7C, arrows). For the AP and LAT planes of the BA model not presented here, CFD-predicted and PIV-measured flow patterns also showed similar levels of agreement. It is important to note that all CFD and PIV results presented thus far represent data phase-averaged over multiple cardiac cycles. Cycle-to-cycle fluctuations were investigated by considering the phase standard deviations of velocity magnitude data from the multiple cycles, acquired or simulated. To determine whether CFD simulations had stabilized to a periodic solution, we looked at two standard measures of convergence: L∞, the maximum difference between velocity data, at a given time step, from cycle n+1 and cycle n; and L2, the r.m.s. value of those differences. In a perfectly converged solution both L∞ and L2 should approach zero. This was the case for the ICA model; however, as shown in Figure 8A, this was not the case for the BA model. Instead, both L∞ and L2 initially tended toward zero as the initial conditions were washed out, and then leveled off well above zero for subsequent cycles. (In contrast, for the ICA model both L∞ and L2 had converged to within three decimal places by the end of the 7th cycle.) Inspecting the CFD velocity data for the BA phantom, it became clear that there were changes in the velocity field from one cycle to the next, as illustrated in Figure 8B. In particular, note the changes in both the size and amplitude of the vortices formed in the upper half of the aneurysm, and the changes in velocity patterns in the lower half. Looking at the PIV velocity data from the same plane and cardiac phase (Figure 8C), similar changes are observed. To confirm these finding more directly, the distribution of the velocity magnitude standard deviation – a measure of the cycle-to-cycle fluctuations – Ford MD et al. 12 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models was mapped for the PIV and CFD data sets, as shown in Figure 9. Although there is not precise one-toone agreement between areas of high and low fluctuation, there is good general agreement of the overall patterns and magnitudes, although it should be noted that for PIV the standard deviations tended to be higher than those for CFD. DISCUSSION If CFD is to advance as a medical tool for the diagnosis of aneurysmal flow dynamics and the validation of novel interventional devices, it is essential that the results predicted by a CFD simulation can be trusted. The findings presented in this paper are a step towards this ultimate goal. This work has shown that CFD can accurately capture not only the gross patterns of flow, but also many of the finer details of the flow dynamics in two geometrically distinct, anatomically-realistic models, each with unique and complex flow dynamics. Even more encouraging was the ability of the CFD simulations to accurately capture the cycle-to-cycle variations in the velocity field. These results are a promising indicator that CFD predictions of the aneurysmal flow details are indeed reliable. Although we do not claim to have carried out direct numerical simulations of turbulence, the high spatial and temporal resolutions used here amount to a kind of large-eddy simulation, with an implied rather than explicit model for the small spatial scales. CFD simulations of the BA case – with half the number of finite elements but the same temporal resolution – showed little change in the amplitude and distribution of velocity magnitude standard deviations, indicating that our models were adequately resolved. The fact that significant cycle-to-cycle variations in the CFD simulations were observed only in the case of the BA model – fluctuations in the CFD model for the ICA case were roughly two orders of magnitude less – is consistent with earlier reports of turbulent flow in basilar tip aneurysms [22]. PIVmeasured cycle-to-cycle variations were slightly higher then those predicted by CFD, which is expected due to the superposition of the cycle-to-cycle variations with inherent experimental uncertainties Ford MD et al. 13 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models associated with measuring flow experimentally using PIV. Still, the spatial distribution of extremes in cycle-to-cycle variations was consistent between PIV and CFD, suggesting that preferred sites for flow instability are relatively insensitive to upstream perturbations. Whether or not these instabilities are clinically relevant remains an open question; however, it is clear that, without adequate temporal resolution in the CFD models, they could easily be overlooked. To the authors’ knowledge there has been only one previous work done to validate CFD predicated flow dynamics in anatomically-realistic geometries, besides those of our group [20,21]. This work [37] similarly involved the construction of a silicone flow through phantom, but with velocities measured using phase-contrast MRI. The results of that study concur with the results presented here, namely that CFD can accurately capture the intra-aneurysmal flow dynamics. Dye visualization has been used to look at the flow patterns in two ruptured cerebral aneurysms [38], and also to investigate the effect of stenting and coiling on a wide necked basilar artery aneurysm [39]. Anatomically-realistic flow-through phantoms have also been used as a validation tool to compare the predictions of phase contrast MRI [40] against laser Doppler velocimetry measurements made in the same phantom [41]. PIV has also been used previously in combination with idealized flow-through aneurysm phantoms to determine the effect stent placement can have on the aneurysmal and parent vessel flow patterns [42,43]. As CFD becomes used more and more in an attempt to understand the growth and rupture of aneurysms [8-14,44] and the effect endovascular devices have on the intra-aneurysmal flow dynamics [15-19] it becomes imperative that validation studies be carried out. Moreover, from a practical standpoint, it is not sufficient to show that CFD can accurately model the in vivo flow dynamics; the level of detail necessary to predict clinically meaningful results must be understood. Of course it cannot be assumed that agreement between the PIV-measured flow fields and corresponding CFD predictions presented in this work implies that these CFD models are a faithful representation of the patient’s actual hemodynamics. For example, this study employed a Newtonian Ford MD et al. 14 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models fluid for the PIV experiments, and the CFD simulation similarly assumed Newtonian rheology. Blood is obviously a non-Newtonian fluid, although recent work suggests that Newtonian rheology may be a reasonable approximation [45]. Our study had the advantage of being carried out under controlled conditions, so that the flow rates at the inlet and outlets could be measured accurately. Although it is possible to measure inlet and outlet flow rates in vivo using phase contrast MRI or Doppler ultrasound, this is not a routine procedure owing to the extra time and effort, which are usually not clinicallyindicated for these often-fragile patients. To eliminate the possibility of geometric differences between the phantom and CFD geometry, the phantoms were scanned under ideal conditions on a micro-CT scanner. Such high-resolution scans with very low background noise are not practical to acquire in vivo, so the question of how accurately we truly know the in vivo geometry remains. For example, the models were simplified by including only those branching or perforating vessels that could be resolved by CRA; and for the BA model the vertebral arteries proximal to the basilar artery were excluded owing to the selective nature of the contrast agent injection. At the same time, it remains unclear what degree of geometric accuracy is required to produce a reliable or even clinically meaningful CFD solution. Although the issues mentioned here are all strengths of the present study and required for rigorous validation, it is now required that a method be found to apply the same rigorous validation to the in vivo setting as has been attempted in earlier work [21,37]. Moreover, it should be appreciated that aneurysms in general experience a wide range of flow types [14], of which we have necessarily presented only a small sample in this study. Other limitations of this study included the fact that the CFD simulations assumed rigid walls, whereas the silicone-elastomer flow-through phantoms were slightly distensible, as evidenced by an observable phase shift of approximately 30 ms between the inlet and outlet flow rate waveforms measured for the ICA phantom (Figure 3). Such distensibility might explain some of the discrepancies between CFD predictions and PIV measurements; bulk velocities at maximum distension (peak systole) Ford MD et al. 15 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models would be reduced slightly in the latter compared to the former. In the case of the BA phantom there was no phase shift between the inlet and outlet waveforms (Figure 3), and there was better overall agreement between CFD and PIV. A key limitation of the PIV experiment was the lack of information collected along the outer edges of the phantoms: looking at Figures 4-8 it is clear that the velocity vectors were not captured along the wall. This was due to two constraints on the experimental setup. The first was the desire to build life-size (or near-life-size) phantoms that could be used for subsequent studies involving stenting and/or coiling. The second was unavoidable, due to the fact that the laser sheet was approximately 1-mm thick, which led to bright edges where the out-of-plane curvature was steep, thus obscuring the particles there. The three-dimensional nature of the geometry and resulting flow patterns also led to difficulties resolving areas where the out-of-plane velocity component was high, such as the strong, helical jet entering the ICA aneurysm from the parent artery [9]. In such cases, PIV is limited by the fact that the particles can move out of the imaging plane faster than the image pair can be collected. Moreover, seemingly pronounced differences between CFD and PIV in-plane velocity vector fields could arise from slight differences in the absolute position of a particular flow feature above or below the nominal viewing plane. Together, these practical limitations likely also explain why the agreement between CFD and PIV seen for the BA phantom, with its relatively planar flow dynamics, was superior to that of the ICA phantom, with its more oblique flows. For such three-dimensional flows, 3D or holographic PIV may be required for a more comprehensive validation. Finally, in some areas of the PIV-measured velocity field, particularly on the LAT plane of the BA phantom (Figure 6), it is apparent that the velocity has exceeded the maximum value the PIV system was calibrated to measure within the prescribed field-of-view. In these rare instances, the PIV system was calibrated to capture the widest range of velocities possible, while still resolving the overall flow patterns. Ford MD et al. 16 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models CONCLUSION The results presented in this paper are a first attempt to compare CFD-predictions against PIV measurements of flow dynamics in anatomically-realistic aneurysm models. They demonstrate that CFD not only captures the gross flow patterns but also many of the finer flow details and their associated cycle-to-cycle variations. Still, owing to the various modeling assumptions, these results do not necessarily prove that we are mimicking the in vivo hemodynamics, and so indirect validation against in vivo data are recommended whenever possible. ACKNOWLEDGMENTS The authors would like to thank Dr. Willie Quinn and Dr. Luca Antiga for helpful discussions and technical advice. This work was supported by grants from the Canadian Institutes of Health Research (MOP-53185) and the Whitaker Foundation (RG-01-0219). We thank the CIHR Group in Vascular Imaging (GR-14973) physical model core for supporting the construction of the phantoms. A Canadian Foundation for Innovation grant to Saint Francis Xavier University funded the PIV facility. M.F. was supported by a Focus on Stroke Doctoral Fellowship from the Heart and Stroke Foundation. D.W.H. and D.A.S. were supported by Career Investigator Awards from this same agency. REFERENCES [1] ISUIA Investigators, 1998, "Unruptured intracranial aneurysms--risk of rupture and risks of surgical intervention.," N Engl J Med, 339, pp. 1725-33. [2] R. P. Tummala, M. K. Baskaya, and R. C. Heros, 2005, "Contemporary management of incidental intracranial aneurysms," Neurosurg Focus, 18, pp. e9. [3] A. Molyneux, R. Kerr, I. Stratton, P. Sandercock, M. Clarke, J. Shrimpton, and R. Holman, 2002, "International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus Ford MD et al. 17 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial," Lancet, 360, pp. 1267-74. [4] A. J. Molyneux, R. S. Kerr, L. M. Yu, M. Clarke, M. Sneade, J. A. Yarnold, and P. Sandercock, 2005, "International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion," Lancet, 366, pp. 809-17. [5] S. Asgari, I. Wanke, B. Schoch, and D. Stolke, 2003, "Recurrent hemorrhage after initially complete occlusion of intracranial aneurysms," Neurosurg Rev, 26, pp. 269-74. [6] Y. Kawanabe, A. Sadato, W. Taki, and N. Hashimoto, 2001, "Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: correlation between coil packing density and coil compaction," Acta Neurochir (Wien), 143, pp. 451-5. [7] H. Nagashima, S. Kobayashi, Y. Tanaka, and K. Hongo, 2004, "Endovascular therapy versus surgical clipping for basilar artery bifurcation aneurysm: retrospective analysis of 117 cases," J Clin Neurosci, 11, pp. 475-9. [8] A. Mantha, C. Karmonik, G. Benndorf, C. Strother, and R. Metcalfe, 2006, "Hemodynamics in a cerebral artery before and after the formation of an aneurysm," AJNR Am J Neuroradiol, 27, pp. 1113-8. [9] D. A. Steinman, J. S. Milner, C. J. Norley, S. P. Lownie, and D. W. Holdsworth, 2003, "Imagebased computational simulation of flow dynamics in a giant intracranial aneurysm," AJNR Am J Neuroradiol, 24, pp. 559-66. [10] M. Shojima, M. Oshima, K. Takagi, R. Torii, M. Hayakawa, K. Katada, A. Morita, and T. Kirino, 2004, "Magnitude and role of wall shear stress on cerebral aneurysm: computational fluid dynamic study of 20 middle cerebral artery aneurysms," Stroke, 35, pp. 2500-5. Ford MD et al. 18 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models [11] T. Hassan, E. V. Timofeev, T. Saito, H. Shimizu, M. Ezura, Y. Matsumoto, K. Takayama, T. Tominaga, and A. Takahashi, 2005, "A proposed parent vessel geometry-based categorization of saccular intracranial aneurysms: computational flow dynamics analysis of the risk factors for lesion rupture," J Neurosurg, 103, pp. 662-80. [12] L. D. Jou, G. Wong, B. Dispensa, M. T. Lawton, R. T. Higashida, W. L. Young, and D. Saloner, 2005, "Correlation between lumenal geometry changes and hemodynamics in fusiform intracranial aneurysms," AJNR Am J Neuroradiol, 26, pp. 2357-63. [13] J. R. Cebral, M. A. Castro, S. Appanaboyina, C. M. Putman, D. Millan, and A. F. Frangi, 2005, "Efficient pipeline for image-based patient-specific analysis of cerebral aneurysm hemodynamics: technique and sensitivity," IEEE Trans Med Imaging, 24, pp. 457-67. [14] J. R. Cebral, M. A. Castro, J. E. Burgess, R. S. Pergolizzi, M. J. Sheridan, and C. M. Putman, 2005, "Characterization of cerebral aneurysms for assessing risk of rupture by using patientspecific computational hemodynamics models," AJNR Am J Neuroradiol, 26, pp. 2550-9. [15] H. S. Byun and K. Rhee, 2004, "CFD modeling of blood flow following coil embolization of aneurysms," Med Eng Phys, 26, pp. 755-61. [16] C. Groden, J. Laudan, S. Gatchell, and H. Zeumer, 2001, "Three-dimensional pulsatile flow simulation before and after endovascular coil embolization of a terminal cerebral aneurysm," J Cereb Blood Flow Metab, 21, pp. 1464-71. [17] G. R. Stuhne and D. A. Steinman, 2004, "Finite-element modeling of the hemodynamics of stented aneurysms," J Biomech Eng, 126, pp. 382-7. [18] M. Aenis, A. P. Stancampiano, A. K. Wakhloo, and B. B. Lieber, 1997, "Modeling of flow in a straight stented and nonstented side wall aneurysm model," J Biomech Eng, 119, pp. 206-12. [19] J. R. Cebral and R. Lohner, 2005, "Efficient simulation of blood flow past complex endovascular devices using an adaptive embedding technique," IEEE Trans Med Imaging, 24, pp. 468-76. Ford MD et al. 19 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models [20] M. D. Ford, G. R. Stuhne, H. N. Nikolov, D. F. Habets, S. P. Lownie, D. W. Holdsworth, and D. A. Steinman, 2005, "Virtual angiography for visualization and validation of computational models of aneurysm hemodynamics," IEEE Trans Med Imaging, 24, pp. 1586-92. [21] M. D. Ford, H. N. Nikolov, J. S. Milner, W. Kalata, F. Loth, S. P. Lownie, D. W. Holdsworth, and D. A. Steinman, "In vitro validation of an image-based CFD model of an anatomically realistic cerebral aneurysm," presented at ASME Summer Bioengineering Conference, Vail, Colorado, 2005. [22] G. G. Ferguson, 1970, "Turbulence in human intracranial saccular aneurysms," J Neurosurg, 33, pp. 485-97. [23] R. Fahrig, A. J. Fox, S. Lownie, and D. W. Holdsworth, 1997, "Use of a C-arm system to generate true three-dimensional computed rotational angiograms: preliminary in vitro and in vivo results," AJNR Am J Neuroradiol, 18, pp. 1507-14. [24] R. V. Yedavalli, F. Loth, A. Yardimci, W. F. Pritchard, J. N. Oshinski, L. Sadler, F. Charbel, and N. Alperin, 2001, "Construction of a physical model of the human carotid artery based on in vivo magnetic resonance images," J Biomech Eng, pp. 372-6. [25] S. G. Wetzel, M. Ohta, A. Handa, J. M. Auer, P. Lylyk, K. O. Lovblad, D. Babic, and D. A. Rufenacht, 2005, "From patient to model: stereolithographic modeling of the cerebral vasculature based on rotational angiography," AJNR Am J Neuroradiol, 26, pp. 1425-7. [26] K. Knox, C. W. Kerber, S. A. Singel, M. J. Bailey, and S. G. Imbesi, 2005, "Stereolithographic vascular replicas from CT scans: choosing treatment strategies, teaching, and research from live patient scan data," AJNR Am J Neuroradiol, 26, pp. 1428-31. [27] M. D. Ford, N. Alperin, S. H. Lee, D. W. Holdsworth, and D. A. Steinman, 2005, "Characterization of volumetric flow rate waveforms in the normal internal carotid and vertebral arteries," Physiol Meas, 26, pp. 477-88. Ford MD et al. 20 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models [28] R. Frayne, D. W. Holdsworth, L. M. Gowman, D. W. Rickey, M. Drangova, A. Fenster, and B. K. Rutt, 1992, "Computer-controlled flow simulator for MR flow studies," J Magn Reson Imaging, 2, pp. 605-12. [29] CRC Handbook of Chemistry and Physiscs, 61 ed. Boca Raton, Florida: CRC Press, Inc., 1981. [30] L. N. Hopkins, J. T. Kelly, A. S. Wexler, and A. K. Prasad, 2000, "Particle image velocimetry measurements in complex geometries," Exp Fluids, 29, pp. 91-95. [31] R. Fahrig, H. Nikolov, A. J. Fox, and D. W. Holdsworth, 1999, "A three-dimensional cerebrovascular flow phantom," Med Phys, 26, pp. 1589-99. [32] L. Antiga, B. Ene-Iordache, L. Caverni, G. P. Cornalba, and A. Remuzzi, 2002, "Geometric reconstruction for computational mesh generation of arterial bifurcations from CT angiography," Comput Med Imaging Graph, 26, pp. 227-35. [33] C. R. Ethier, S. Prakash, D. A. Steinman, R. I. Leask, G. G. Couch, and M. Ojha, 2000, "Steady flow seperation patterns in a 45 degree junction," J Fluid Mech, 411, pp. 1-38. [34] P. D. Minev and C. R. Ethier, 1999, "A characteristic/finite element algorithm for the 3-D Navier-Stokes equations using unstructured grids," Computer Methods in Applied Mechanics and Engineering, 178, pp. 39-50. [35] C. R. Ethier, D. A. Steinman, and M. Ojha, Comparisons between computational hemodynamics, photochromic dye flow visualization and magnetic resonance velocimetry. Southhampton: WIT Press, 1999. [36] D. A. Steinman, J. B. Thomas, H. M. Ladak, J. S. Milner, B. K. Rutt, and J. D. Spence, 2002, "Reconstruction of carotid bifurcation hemodynamics and wall thickness using computational fluid dynamics and MRI," Magn Reson Med, 47, pp. 149-59. [37] G. Acevedo-Bolton, L. D. Jou, B. P. Dispensa, M. T. Lawton, R. T. Higashida, A. J. Martin, W. L. Young, and D. Saloner, 2006, "Estimating the hemodynamic impact of interventional Ford MD et al. 21 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models treatments of aneurysms: numerical simulation with experimental validation: technical case report," Neurosurgery, 59, pp. E429-30; author reply E429-30. [38] S. G. Imbesi and C. W. Kerber, 1999, "Analysis of slipstream flow in two ruptured intracranial cerebral aneurysms," AJNR Am J Neuroradiol, 20, pp. 1703-5. [39] S. G. Imbesi and C. W. Kerber, 2001, "Analysis of slipstream flow in a wide-necked basilar artery aneurysm: evaluation of potential treatment regimens," AJNR Am J Neuroradiol, 22, pp. 721-4. [40] S. Tateshima, J. Grinstead, S. Sinha, Y. L. Nien, Y. Murayama, J. P. Villablanca, K. Tanishita, and F. Vinuela, 2004, "Intraaneurysmal flow visualization by using phase-contrast magnetic resonance imaging: feasibility study based on a geometrically realistic in vitro aneurysm model," J Neurosurg, 100, pp. 1041-8. [41] S. Tateshima, Y. Murayama, J. P. Villablanca, T. Morino, H. Takahashi, T. Yamauchi, K. Tanishita, and F. Vinuela, 2001, "Intraaneurysmal flow dynamics study featuring an acrylic aneurysm model manufactured using a computerized tomography angiogram as a mold," J Neurosurg, 95, pp. 1020-7. [42] B. B. Lieber, V. Livescu, L. N. Hopkins, and A. K. Wakhloo, 2002, "Particle image velocimetry assessment of stent design influence on intra-aneurysmal flow," Ann Biomed Eng, 30, pp. 76877. [43] T. M. Liou, S. N. Liou, and K. L. Chu, 2004, "Intra-aneurysmal flow with helix and mesh stent placement across side-wall aneurysm pore of a straight parent vessel," J Biomech Eng, 126, pp. 36-43. [44] T. Hassan, E. V. Timofeev, M. Ezura, T. Saito, A. Takahashi, K. Takayama, and T. Yoshimoto, 2003, "Hemodynamic analysis of an adult vein of Galen aneurysm malformation by use of 3D image-based computational fluid dynamics," AJNR Am J Neuroradiol, 24, pp. 1075-82. Ford MD et al. 22 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models [45] A. Valencia, Zarate, A., Galvez M., Badilla, L., 2006, "Non-newtonian blood flow dynamics in a right internal carotid artery with a saccular aneurysm," Int J Numer Meth Fluids, 50, pp. 751 764. Ford MD et al. 23 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 1. Anatomically-realistic flow-through phantoms of a giant internal carotid artery (ICA) aneurysm and a basilar artery (BA) tip aneurysm, each shown in anterior-posterior (AP) and lateral (LAT) views. Both phantoms are shown to the same scale, per the indicated scaling bar. Numerals identify the outlet numbers referred to in Figure 3. For the ICA model, outlets 1 and 2 arise from the middle cerebral artery; and outlet 3 arises from the anterior cerebral artery. For the BA model the two outlets arise from the two posterior cerebral arteries. Ford MD et al. 24 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 2. CFD meshes derived from micro-CT imaging of the flow-through phantoms, showing the positions of the five AP and LAT planes for the ICA model and BA models. Note that in all cases plane 1 is the nominal central plane, and the thickness of the lines corresponds to the nominal thickness of the PIV laser light sheet. Darker planes are those for which data are shown in the Results. Ford MD et al. 25 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 3. Inlet and outlet flow rate waveforms, measured by the EM flow meter, during acquisitions of PIV data for the ICA and BA cases. Vertical bars indicate the standard deviations of the phase-averaged flow rate measurements. Note the different time (x) axes, owing to the different periods required for the two models. Ford MD et al. 26 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 4. PIV vs. CFD velocities on AP planes of the ICA model: (A) AP plane 1, peak systole; (B) AP plane 1, late diastole; (C) AP plane 4, peak systole; and (D) AP plane 4, late diastole. For this and subsequent Figures 5-7, PIV data are on the left side of each panel, and CFD data are on the right. Translucent circles correspond to vortex cores and transparent arrows to areas of discrepancy between PIV and CFD, as described in the results. Ford MD et al. 27 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 5. PIV vs. CFD velocities on LAT planes of the ICA model: (A) LAT plane 1, peak systole; and (B) LAT plane 1, late diastole; (C) LAT plane 2, peak systole; and (D) LAT plane 2, late diastole. Refer to the caption of Figure 4 for further details. Ford MD et al. 28 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 6. PIV vs. CFD velocities on LAT planes of the BA model: (A) LAT plane 1, peak systole; (B) LAT plane 1, late diastole; (C) LAT plane 4, peak systole; and (D) LAT plane 4, late diastole. Refer to the caption of Figure 4 for further details. Ford MD et al. 29 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 7. PIV vs. CFD velocities on AP planes of the BA model: (A) AP plane 1, peak systole; (B) AP plane 1, late diastole; (C) AP plane 4, peak systole; and (D) AP plane 4, late diastole. Refer to the caption of Figure 4 for further details. Ford MD et al. 30 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 8. Cycle-to-cycle fluctuations for the BA model, (A) CFD convergence history, showing the maximum (L∞) and rms (L2) differences in the velocity fields between successive cycles (as defined in the Results), each normalized with respect to the characteristic (mean inlet) velocity. Also shown is the inlet flow rate waveform shape for reference. (B) CFD and (C) PIV velocity vector fields from three consecutive cycles on the central AP plane, at a phase mid-way through the cycle where the greatest fluctuations are evident in panel A. Ford MD et al. 31 Accepted June 8, 2007 PIV vs. CFD of Realistic Aneurysm Models Figure 9. Standard deviations of the velocity magnitude from PIV and CFD data on the central AP and LAT planes, at the same phase shown in Figure 8. Ford MD et al. 32 Accepted June 8, 2007