THE MENACING FUNGI
by
George A. Wistreich
Ph.D., F(AAM)
RC Educational Consulting Services, Inc.
16781 Van Buren Blvd, Suite B, Riverside, CA 92504-5798
(800) 441-LUNG / (877) 367-NURS
www.RCECS.com
THE MENACING FUNGI
BEHAVIORAL OBJECTIVES
UPON COMPLETION OF THE READING MATERIAL, THE PRACTITIONER WILL BE
ABLE TO:
1. Briefly describe the general features of fungi.
2. Briefly describe a common method of classifying fungal diseases (mycoses) based on
the site of infection.
3. Distinguish among the various epidemiological patterns exhibited by infectious
diseases.
4. Describe the features of fungi with a special emphasis on dimorphic fungi.
5. Discuss the distinguishing microscopic and related cultural properties of selected
pathogenic fungi, with a special emphasis on respiratory pathogens.
6. List and briefly describe the actions of examples of anti-fungal agents used in
treatment of fungal infections and/or diseases.
7. Distinguish between primary and opportunistic fungal pathogens and describe
their respective habitats.
8. Recognize the distinguishing microscopic and related cultural properties of primary and
opportunistic fungal pathogens.
9. Discuss the means of transmission of primary and opportunistic fungal pathogens.
10. Recognize the importance of biofilms in certain fungal infections.
11. Briefly describe the clinical forms and associated features of disease states caused by
primary and opportunistic fungal pathogens.
12. List and briefly describe representative mycotoxins (fungal metabolic products) and
their effects.
13. Outline the general laboratory approach followed in the diagnosis of primary and
opportunistic fungal pathogens.
14. Briefly discuss the medications and approaches used in the treatment of fungal
pathogens.
15. Describe the prevention and control measures used with primary and opportunistic
fungal pathogens.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
2
THE MENACING FUNGI
16. Briefly discuss the current understanding of the relationship between mycotoxins and
sick-building syndrome.
COPYRIGHT © 2006 By RC Educational Consulting Services, Inc.
TX 6-147-048
Authored by: George A. Wistreich, Ph.D., F(AAM) 2006
ALL RIGHTS RESERVED
This course is for reference and education only. Every effort is made to ensure that the clinical
principles, procedures and practices are based on current knowledge and state of the art
information from acknowledged authorities, texts, and journals. This information is not intended
as a substitution for a diagnosis or treatment given in consultation with a qualified health care
professional.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
3
THE MENACING FUNGI
TABLE OF CONTENTS
PREFACE ..........................................................................................................................10
INTRODUCTION .............................................................................................................10
ENDEMIC, EPIDEMIC, PANDEMIC AND SPORADIC PATTERNS
OF INFECTIOUS DISEASES ..........................................................................................10
GENERAL PROPERTIES OF FUNGI .............................................................................11
STRUCTURAL FEATURES .......................................................................................11
REPRODUCTION........................................................................................................13
A BRIEF WORD ABOUT CLASIFICTION ...............................................................15
CLASSIFYING FUNGAL DISEASES BASED ON THE
SITE OF INFECTION.............................................................................................16
ANTI-FUNGAL AGENTS USED IN TREATMENT......................................................19
VACCINES ........................................................................................................................21
THE PRIMARY FUNGAL PATHOGENS.......................................................................21
BLASTOMYCOSIS .....................................................................................................21
GEOGRAPHIC DISTRIBUTION...........................................................................21
HABITAT ................................................................................................................21
CULTURE AND MICROSCOPIC FEATURES ....................................................21
TRANSMISSION ....................................................................................................23
CLINICAL STATES ...............................................................................................23
LABORATORY AND RELATED ASPECTS OF DIAGNOSIS...........................24
TREATMENT .........................................................................................................24
PREVENTION AND CONTROL...........................................................................24
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
4
THE MENACING FUNGI
COCCIDIOIDOMYCOSIS ..........................................................................................24
HABITAT ................................................................................................................25
CULTURE AND MICROSCOPIC PROPERTIES .................................................25
TRANSMISSION ....................................................................................................26
LIFE CYCLE ...........................................................................................................27
PATHOGENESIS ....................................................................................................28
INDIVIDUALS AT RISK .......................................................................................29
CLINICAL STATES ...............................................................................................29
THE HIV-INFECTED PATIENTS .........................................................................32
SIGNS AND SYMPTOMS ................................................................................32
SOLID-ORGAN TRANSPLANT RECIPIENTS ....................................................32
LABORATORY AND RELATED ASPECTS OF DIAGNOSIS...........................33
SKIN TESTS ......................................................................................................33
TREATMENT .........................................................................................................34
PREVENTION AND CONTROL...........................................................................35
HISTOPLASMOSIS..........................................................................................................35
THE CAUSATIVE AGENTS ......................................................................................35
HABITAT .....................................................................................................................36
CULTURE AND MICROSCOPIC FEATURES .........................................................36
LIFE CYCLE ................................................................................................................37
TRANSMISSION .........................................................................................................37
EXPOSURE RISKS......................................................................................................38
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
5
THE MENACING FUNGI
PATHOGENESIS .........................................................................................................38
CLINICAL STATES ....................................................................................................38
LABORATORY AND RELATED ASPECTS OF DIAGNOSIS................................40
SKIN TESTS ...........................................................................................................40
TREATMENT ..............................................................................................................41
PREVENTION AND CONTROL................................................................................41
THE IMMUNOSUPPRESSED PATIENT........................................................................42
INDIVIDUALS AT RISK ............................................................................................42
PARACOCCIDIOIDOMYCOSIS.....................................................................................42
HABITAT .....................................................................................................................42
CULTURE AND MICROSCOPIC FEATURES .........................................................42
TRANSMISSION AND PATHOGENSIS ...................................................................43
CLINICAL STATES ....................................................................................................43
LABORATORY AND RELATED ASPECTS OF DIAGNOSIS................................44
TREATMENT ..............................................................................................................44
PREVENTION AND CONTROL................................................................................45
THE OPPORTUNISTIC FUNGAL PATHOGENS..........................................................45
THE ASPERGILLOSES ...................................................................................................45
GENERAL PROPERTIES OF THE ASPERGILLI.....................................................45
HABITAT ................................................................................................................46
MICROSCOPIC AND CULTURAL PROPERTIES ..............................................46
NONPATHOGENIC AND PATHOGENIC ASPERGILLI ...................................47
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
6
THE MENACING FUNGI
MYCOTOXINS .......................................................................................................47
DISEASE STATES .................................................................................................47
NOSOCOMIAL INFECTIONS.........................................................................................48
ASPERGILLUS FUMIGATUS, AN IMPORTANT PATHOGEN ....................................48
CULTURE FEATURES ...............................................................................................49
PATHOGENICITY ......................................................................................................49
SELECTED A. FUMIGATUS-ASSOCIATED DISEASES ..............................................50
INVASIVE ASPERGILLOSIS ....................................................................................50
PREDISPOSING FACTORS ..................................................................................51
GASTROINTESTINAL INVOLVEMENT ............................................................51
LIVER TRANSPLANT RECIPIENTS ...................................................................51
SIGNS AND SYMPTOMS .....................................................................................52
DIAGNOSIS ............................................................................................................52
OTHER ASPERGILLOSES CAUSED BY A. FUMIGATUS .....................................52
MAJOR SYNDROMES FOUND WITH AIDS PATIENTS .......................................54
GENERAL ASPECTS OF LABORATORY DIAGNOSIS..............................................54
TREATMENT ..............................................................................................................55
PREVENTION AND CONTROL................................................................................56
CANDIDIASIS AND CANDIDA SPECIES .....................................................................56
PATHOGENIC CANDIDA SPECIES ..........................................................................56
HABITAT ................................................................................................................57
TRANSMISSION ....................................................................................................57
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
7
THE MENACING FUNGI
RISK FACTORS ................................................................................................57
MEDICAL DEVICES AND BIOFILMS ...........................................................58
CULTURE AND MICROSCOPIC PROPERTIES .................................................58
DISEASE STATES .................................................................................................60
INDIVIDUALS AT RISK .......................................................................................63
TREATMENT .........................................................................................................64
DIAGNOSIS ............................................................................................................64
PREVENTION AND CONTROL...........................................................................65
CRYPTOCOCCOSIS ...................................................................................................65
HABITAT ................................................................................................................65
MICROSCOPIC AND CULTURE PROPERTIES .................................................66
TRANSMISSION ....................................................................................................67
PATHOGENESIS ....................................................................................................67
RISK FACTORS .....................................................................................................68
CLINICAL STATES ...............................................................................................68
TREATMENT .........................................................................................................70
DIAGNOSIS ............................................................................................................70
PREVENTION AND CONTROL...........................................................................70
PENICILLIOSIS ...........................................................................................................70
GEOGRAPHIC DISTRIBUTION AND HABITAT...............................................70
CULTURE AND MICROSCOPIC FEATURES ....................................................71
TRANSMISSION ....................................................................................................71
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
8
THE MENACING FUNGI
CLINICAL STATES ...............................................................................................71
SIGNS AND SYMPTOMS ................................................................................71
TREATMENT .........................................................................................................71
LABORATORY AND RELATED ASPECTS OF DIAGNOSIS...........................71
PREVENTION AND CONTROL...........................................................................72
THE MYCOTOXICOSES ............................................................................................72
THE MAJOR MYCOTOXINS................................................................................72
THE AFLATOXINS AND ERGOT POISONING.................................................73
THE SICK-BUILDING SYNDROME....................................................................74
CAUSATIVE AGENTS .....................................................................................74
SOURCES ...........................................................................................................74
SIGNS AND SYMPTOMS ................................................................................75
CONCLUDING STATEMENTS ......................................................................................75
GLOSSARY ......................................................................................................................76
TERMS .........................................................................................................................76
SUGGESTED READING AND REFERENCES .............................................................78
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
9
THE MENACING FUNGI
PREFACE
A
number of fungus diseases (mycoses) have a restricted geographic distribution, being
mainly confined to areas where the causative fungi are found in nature. However,
increased domestic and international travel has led to a rise in the number of reported
outbreaks and sporadic cases of such endemic diseases among individuals who normally live in
places far from the areas where these diseases are present. This course presents the features of
mycotic diseases that pose risks of infection for travelers, individuals who are
immunocompetent, and persons who are immunocompromised as well. This course also briefly
considers the potential health effects posed by moldy indoor environments. Health care
personnel need to be aware and familiar with these diseases and associated conditions from the
standpoint of being able to minimize the risk of infection, contribute to the accurate diagnosis,
and to provide the appropriate treatment for victims.
INTRODUCTION
T
he growth of fungi on or in humans and/or lower animals produces diseases collectively
called mycoses, while respiratory, dietary, dermal, and other exposures to toxic fungal
metabolic products produce the diseases collectively known as mycotoxicoses. Mycoses
are frequently acquired via the inhalation of the reproductive units of fungi (spores) from an
environmental reservoir (source), or by unusual growth of a fungus that is normally resident on
human skin or in the gastrointestinal tract. The majority of mycotoxicoses, on the other hand, are
acquired from eating contaminated foods.
Fungal diseases also represent an especially important complication for immunosuppressed
persons and are associated with high morbidity and mortality. Limited familiarity with many of
the fungal pathogens, as well as the limited diagnostic tools available can and in several
situations delay the diagnosis and treatment of mycoses. This course presents several
representative fungal diseases, the general properties of the causative pathogens, together with
approaches used in treatment, and prevention and control.
ENDEMIC, EPIDEMIC, PANDEMIC, AND SPORADIC PATTERNS OF INFECTIOUS
DISEASES
D
iseases are often classified in terms of how they behave within a host and within a given
population. The incidence of a disease, for example, refers to the number of individuals
within a population who develop a specific disease during a particular time period. A
particular standard used in the classification of diseases is the frequency of occurrence. Thus,
if a particular disease occurs only occasionally, it would be referred to as being sporadic, while a
disease that is constantly present in a population would be considered as being endemic. In the
event a large number of individuals in a given geographic area acquire a specific disease such as
the viral disease influenza, in a relatively short time period, the frequency of occurrence is
considered to be epidemic. In situations where a series of epidemics of a disease take place on a
worldwide scale, the frequency of occurrence is called a pandemic.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
10
THE MENACING FUNGI
Abbreviations Used
AIDS:
BAL:
BMT:
CDC:
CT:
DH:
DNA:
ELISA:
GVH:
HIV:
HVAC:
IA:
LSD:
PCM:
SBS:
SOTR:
acquired immune deficiency syndrome
bronchoalveolar lavage
bone marrow transplant
Centers for disease Control and Prevention
computerized tomography
disseminated histoplasmosis
deoxyribonucleic acid
enzyme-linked immunoabsorbent assay
graft-versus-host
human immunodeficiency virus
heating, ventilation, and air conditioning
invasive aspergillosis
lysergic acid diethylamide
paracoccidioidomycosis
sick-building syndrome
solid-organ transplant patients
GENERAL PROPERTIES OF FUNGI
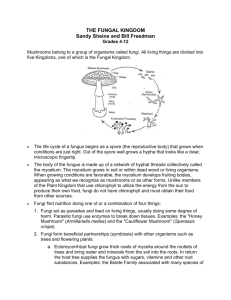
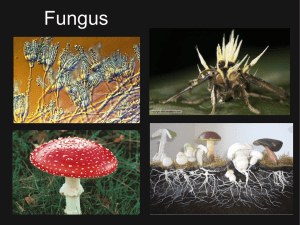
M
olds, yeast and certain related forms such as mushrooms, and toadstools constitute the
forms of life known as the fungi. (Mushrooms and toadstools are reproductive
structures. The major portion of such fungal forms are located underground). The
presence of mold is a common sight on stale bread (without preservatives), rotten fruit, or damp
leather goods. Be it fuzzy or powdery, green, black, or white, the growth on so-called moldy
food and clothing is familiar to most everyone (Figure 1).
Fungi (approximately 100,000 species) are among the most plentiful forms of life. A significant
number of species, however, affect humans, lower animals, and plants in various ways. Of these
species, at least 30 cause potentially fatal disease in humans, over 35 cause less severe systemic
involvement, and about 45 or so species are responsible for more or less minor superficial
infections of the skin and mucous membranes. Certain fungi also are known for their production
of various types of toxins and enzymes, which have far reaching effects on humans, lower
animals, and plant-life. Since fungi, are unable to produce their own food by photosynthesis, as
plants do, they exist as parasites on or in other living organisms, or as saprophytes using the
nutrients in the dead remains of plant and related organic matter.
Structural Features
Fungi have well-defined nuclei in their individual cells, and possess certain distinguishing
properties that separate them from other microorganisms. Some fungi, such as mushrooms, are
large and easily visible to the naked eye. However, most medically important ones are
microscopic, and their basic structures require the use of a microscope for a complete
identification. A given fungus may be a single cell, or may form growths composed of many
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
11
THE MENACING FUNGI
cells known as a mycelium (Figure 1). On the basis of their growth pattern, fungi are divided
into two groups: yeasts and molds.
Figure 1. The two general forms of fungi are shown in this photograph. The typical mycelial
growth of the mold Penicillium can be distinguished from the round, dome-like creamy growth
of baker’s yeast, Saccharomyces cerevisiae.
Yeasts are single-celled fungi that reproduce by budding (Figure 2) or, in the case of a few
species, by a splitting process known as fission. Yeast colonies appear to the naked eye as moist
growths on surfaces or on laboratory culture preparations. Molds (also spelled as moulds) are
multicellular and form threadlike networks, recognizable as cottony, or fuzzy mycelia (singular,
mycelium) mentioned earlier (Figure 1). The threadlike parts of a mycelium (Figure 3) are called
hyphae (singular, hypha). The portion of the mycelium concerned with nutrition is known as the
vegetative mycelium, while the part that usually projects into the air is known as the aerial or
reproductive mycelium.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
12
THE MENACING FUNGI
Figure 2. A microscopic view of yeast cells. Buds can be seen on a few of the cells shown.
The bar marker represents 20 micrometers.
At different temperatures or under different environmental conditions certain fungi may appear
as single cells, or may appear as many cells arranged in a definite pattern. This distinction is not
always clear, for the two forms may represent different phases of fungal growth. For example,
certain pathogens producing disease in human body tissues at 37o C. appear as single cells.
However, when grown on laboratory culture preparations maintained at 25o C., the pathogens
appear as molds. The capacity of a fungus to exhibit both yeast and mold phases is called
dimorphism. Many pathogenic fungi are dimorphic.
Reproduction
The two major ways in which fungi reproduce are asexual and sexual. These processes are not
exclusive and a given fungus may reproduce in one or the other way, or in both ways.
Reproductive units (propagules), also generally referred to as spores, are the bases for the
asexual growth of most fungi. Multicellular fungi reproduce by the conversion of a reproductive
unit into an actively metabolizing vegetative fungus. These units take the form of a variety of
spores known as conidia and sporangiospores, depending on the way they are formed. They
are formed in a variety of ways, depending on the species. Some spores are formed on the sides
or ends of hyphae, and are simply pinched free when they mature (Figure 3).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
13
THE MENACING FUNGI
Figure 3. A scanning electron micrograph showing the long hyphae and the round reproductive
units known as microconidia attached to them.
Conidia are often given special names that more specifically define the nature of way they are
formed or the type of cell producing them. For example, an arthroconidium (also known as an
arthrospore) is produced by the conversion of a preexisting, hyphal segment into a conidium that
breaks loose from the remaining portion of the mycelium (Figure 4). This type of reproductive
unit formation is typical of the respiratory pathogen, Coccidioides immitis.
Figure 4. A scanning electron micrograph showing the formation of barrel-shaped arthroconidia
(arthrospores) by breaking away from parts (hyphae) of a mycelium.
Sporangiospores are formed by the splitting of cells within a sac-like structure called a
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
14
THE MENACING FUNGI
sporangium. At the end of the splitting process the sac breaks, thus releasing the newly formed
sporangiospores (Figure 5).
Figure 5. A scanning micrograph showing the sac-like sporangium and several oval
sporangiospores.
The microscopic appearance of conidia is one of the major bases for laboratory identification of
a fungal species.
Most fungi have a sexual reproductive phase. Sexual reproduction involves the same basic
process as found with all other forms of life having well-defined nuclei. Such forms of life are
called eukaryotes. The end product of the process is the sexual spore . It is formed after the
nuclei of two different hyphae have made contact and fused. While the asexual spores described
earlier are formed in great numbers, sexual spores are formed only occasionally. The appearance
and the development of sexual spores also are used for the identification and classification of
fungal species.
A Brief Word About Classification
The fungi are contained in one of the five recognized biological kingdoms. This kingdom, which
consists only of fungi, is further subdivided into phyla and based on the type of sexual
reproduction, or lack thereof, within a specific phylum. There are 5 phyla and are known as
follows: Zygomycota, Ascomycota, Basidiomycota, Deuteromycota, and Mycophycophyta.
The only phylum for which sexual reproduction has not been observed is the Deuteromycota.
Fungi pathogenic for humans are found in all phyla with the exception of the Mycophycophyta.
Table 1 lists the placement of several fungal pathogens.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
15
THE MENACING FUNGI
Table 1. The Phyla of Fungal Pathogens
Fungus species
Associated Phylum
Disease(s) Caused
Asperegillus fumigatus
and other Aspergillus
species
Deuteromycota
aspergillosis, invasive
aspergillosis, allergic
bronchopulmonary
aspergillosis, aspergilloma
Blastomyces dermatitidis
Deuteromycota
blastomycosis (North American
blastomycosis, Gilchrist disease)
Candida albicans (and
and other Candida species)
Ascomycota
candidiasis, moniliasis,
oral and vaginal thrush, Candida
paronychia, bronchomycosis,
Candida endocarditis, mycotic
vulvovaginitis, candidosis
Claviceps purpurea
Ascomycota
ergot poisoning
Coccidioides immitis
Deuteromycota
coccioidomycois (San Joaquin
Valley fever, Valley fever)
Cryptococcus neoformans
Deuteromycota
cryptococcosis, meningoencephalitis,
crytococcomas, pulmonary
crytococcosis, skin involvement
Histoplasma capsulatum
Deuteromycota
histoplasmosis, (Darling’s disease,
reticuloendothelial cytomycosis )
Paracoccidioides
brasiliensis
Deuteromycota
paracoccidiomycosis (South
American blastomycosis, Brazilian
blastomycosis, Lutz-SplendoreAlmeida’s disease, paracoccidioidal
granuloma
Penicillium marneffi
Ascomycota
penicilliosis
Classifying Fungal Disease Based on the Site of Infection
One of the most common methods of classifying mycoses (fungal diseases), which partly reflects
their varying extent of severity and their degree of invasiveness, is based on the location of the
infection. According to this type of approach, mycoses are considered to be superficial
(cutaneous), subcutaneous , and deep-seated (systemic). Mycoses range from merely annoying
to life-threatening. Table 2 lists examples of fungi categorized according to this approach. (It
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
16
THE MENACING FUNGI
should be noted that several fungal pathogens involve and attack different body sites.)
Superficial and cutaneous mycoses, but not their fungal cause, have been known since the days
of Hippocrates in ancient Greece. Both types of disease involve infections of the skin, nails, and
hair. In certain cases the mucous membranes also may be infected. Examples of the superficial
mycoses mainly include the various types of ringworm, known as the tineas (Figure 6). The
protein, keratin, found in the top layers of the skin, nails, and hair is the main target and nutrient
for the causative fungi, which are mostly molds.
Figure 6. A case of athlete’s foot, also known as tinea pedis.
Yeasts such as Candida albicans, which also can attack the skin and nails, can cause infections
of the mouth and vaginal areas known as oral and vaginal thrush, respectively. Oral Candida
infections (Figure 7), especially those involving the esophagus, are considered as indicator
diseases in cases of human immunodeficiency virus (HIV) infection and acquired
immunodeficiency syndrome (AIDS).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
17
THE MENACING FUNGI
Figure 7. A case of oral candidiasis, also known as oral thrush.
Table 2. Examples of Fungus Infections and/or Diseases
Fungus Infection
and/or Disease
Cause
Category
various types of tinea
(fungus infections of
the nails, skin and hair)
a number of mold species,
and yeasts such as Candida
species
superficial mycosis
blastomycosis
dimorphic fungus
deep-seated mycosis
candidiasis
yeast
superficial and subcutaneous
mycoses
chromoblastomycosis
mold
subcutaneous mycosis
coccidioidomycosis
dimorphic fungus
deep-seated mycosis
cryptococcosis
yeast
deep-seated mycosis
histoplasmosis
dimorphic fungus
deep-seated mycosis
invasive aspergillosis
mold
deep-seated mycosis
paracoccidioidomycosis
dimorphic fungus
deep-seated mycosis
penicilliosis
mold
deep-seated mycosis
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
18
THE MENACING FUNGI
sporotrichosis
mold
subcutaneous mycosis
The subcutaneous mycoses can be quite destructive and disfiguring for victims. Such infections
attack the upper skin layers, bone, tendons, and muscles. They include sporotrichosis, and
chromoblastomycosis. Unfortunately some of these infections can develop into the last category,
namely systemic mycoses.
Systemic mycoses, also known as deep-seated mycoses, are caused by either primary or
opportunistic infectious fungi. These fungi can be divided into two categories, primary
pathogens , which include the highly virulent Coccidioides immitis and Histoplasma capsulatum,
and opportunistic pathogens such as Aspergillus fumigatus and Candida albicans. Primary
pathogens can affect otherwise healthy individuals with normal immune systems, while
opportunistic pathogens produce illness by taking advantage of debilitated or
immunocompromised hosts. The majority of human mycoses are caused by opportunistic fungi.
Initially, many of the deep-seated infections are asymptomatic or mild in their effects, infecting
the sinuses and other portions of the respiratory and related body systems. Left untreated several
of these mycoses can become systemic as well as lethal. The body organs and systems that can
be involved include the lymphatic system, liver, spleen, kidneys, and the components of the
central nervous system. These infections occur in fairly large sections of human populations
where the causative fungi are endemic.
Opportunistic fungi are not restricted to any specific geographic area and are found worldwide.
The three genera of fungi most frequently found as severe agents of opportunistic infections are
Aspergillus, Candida, and Cryptococcus. It should be noted that in recent years unusual
opportunistic fungal pathogens have also emerged and thereby have increased the need by health
care personnel for a greater awareness of the risk of immunocompromised as well as
immunocompetent patients developing severe forms of mycotic infections.
Several factors are known to contribute to the increasing number of opportunistic fungal
infections. These include: 1) immune defects and/or deficiencies such as acquired immune
deficiency syndrome (AIDS), 2) the inappropriate and/or prolonged use of antibiotics, 3) the use
of immunosuppressive drugs, 4) endocrine disorders, 5) malignancies, 6) surgical procedures, 7)
organs transplants, 8) indwelling catheters or shunts, and 9) various other procedures currently
used in medicine.
ANTI-FUNGAL AGENTS USED IN TREATMENT
T
he drugs used to treat fungal infections work differently from those used for bacterial
infections, and belong to different chemical groups. Amphotericin B belongs to the oldest
class of antifungal agents, the polyene macrolides. This antimycotic agent binds to
ergosterol, a major component of the plasma membrane of fungal cells. This binding creates
channels in the fungal membrane that increase permeability and cause cell death through leakage
of essential nutrients. Azole antimycotics interfere with ergosterol formation.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
19
THE MENACING FUNGI
Amphotericin B deoxycholate (AmB-d) has been the agent-of-choice for treatment of patients
who are at high risk for or who have documented invasive fungal infections. In attempts to
decrease the incidence of drug infusion-related and renal toxicities, bench-to-bedside studies
were used to develop other formulations and approaches to the use of amphotericin B for clinical
use. Through such investigations three commercially available lipid formulations were
developed which have been shown to be significantly less nephrotoxic than AmB-d. The
resulting compounds were: 1) liposomal amphotericin B, 2) amphotericin B lipid complex, and
3) amphotericin B colloidal dispersion (ABCD). In addition, a lower incidence of infusionrelated toxicity was found with the use of liposomal amphotericin B. In reported clinical trials
with ABCD, the antimycotic agent was shown to have an excellent renal safety profile, even
when used to treat patients with preexisting renal insufficiency.
In addition to the lipid formulations of amphotericin B, newer antimycotic agents including
triazoles such as voricinzole, posaconzole, and ravuconazole, and the echinocandins such as
pofungin, micafungin and anidulofungin have provided more treatment choices for lifethreatening invasive fungal infections. The echinocandins interfere with formation of the
outermost part of fungal cell, the cell wall.
Other approaches also are being studied which have the potential of reducing drug toxicity and
increasing drug effectiveness. One of these is the use of an echinocandin-triazole combination in
the treatment of invasive aspergillosis. The combination may result in the inhibition of the
formation of both the cell wall and cell membrane of A. fumigatus. Additional studies are
needed to determine the effectiveness of drug combinations such as these.
Table 3 lists several examples of anti-fungal (anti-mycotic) drugs used in the treatment of serious
fungus infections, together with their mechanisms of action.
Table 3. Examples of Anti-fungal Agents Used in the Treatment of Fungal Infections
Anti-fungal Agent
Class
Mechanism of Action
amphotericin B
polyene
binds to sterols in fungal plasma (cell)
membranes, making such membranes
excessively permeable and killing the cells a
caspofungin
echinocandin
interferes with fungal cell wall formation
clotrimazole
imidazole
primarily interfere with sterol synthesis in
fungi
flucytosine
nucleoside
analogue
inhibits DNA and RNA synthesis
fluconazole
triazole
same as for clotrimazole
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
20
THE MENACING FUNGI
itraconazole
triazole
same as for clotrimazole
ketoconazole
imiddazole
same as for clotrimazole
miconazole
imidazole
same as for clotrimazole
a
Sterols are high molecular weight alcohol compounds related to fats, and common components
of fungal and other plasma (cell) membranes.
VACCINES
C
urrently there are no vaccines available for the primary fungal pathogens or any of the
opportunistic fungal pathogens. However, various preparations are under study.
THE PRIMARY FUNGAL PATHOGENS
Blastomycosis
B
lastomycosis is a deep-seated mycosis caused by the fungus Blastomyces dermatitidis.
This disease usually starts as a respiratory infection and spreads with pulmonary, bone,
and skin involvement predominating.
Geographic Distribution
This disease occurs sporadically in African countries such as South Africa, Tanzania, and Zaire,
Canada, central and southeastern United States, India, Israel, and Saudi Arabia.
Habitat
The usual habitat of Blastomyces dermatitidis is largely moist soil and wooded areas along
waterways and undisturbed places containing organic debris, such as porches or wood sheds.
Culture and Microscopic Features
Blastomyces dermatitidis a dimorphic fungus. In culture at room temperature, the fungus grows
slowly and forms a white cottony mycelium consisting of hyphae bearing spherical or ovoid
conidia measuring 2 to 10 micrometers in diameter. The conidia are situated at the end of hyphae
or on short stalk-like structures, known as conidiophores (Figure 8).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
21
THE MENACING FUNGI
Figure 8. A microscopic view of Blastomyces dermatitidis hyphae and spherical to ovoid conidia
(spores).
In tissues and laboratory cultures incubated at 37 o C., the fungus takes the form of large spherical
or oval cells ranging in size from 8 to 15 micrometers (Figure 9). These cells reproduce by
budding.
Figure 9. A microscopic view of the yeast form of B. dermatitidis.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
22
THE MENACING FUNGI
Transmission
Humans and other mammals such as dogs acquire blastomycosis by inhaling conidia from
mycelia growing in soil or from various articles contaminated by conidia. Infections are
sporadic and can occur with all ages. However, there appears to be a higher incidence with
individuals in the age range of 30 to 50. There is no evidence of person-to-person transmission.
Cases of the disease have been reported in a horse, a captive lion, and sea lion.
Clinical States
Clinical manifestations of the disease have been classified into three general groups:
1. pulmonary blastomycosis;
2. disseminated blastomycosis;
3. cutaneous blastomycosis.
Table 4 lists these conditions together with their distinguishing features.
Table 4. The Clinical Manifestations of Blastomycosis
Clinical Manifestation
Distinguishing Features
pulmonary blastomycosis
usually begins as a mild respiratory infection which
progresses with dry cough, pleuritic pain, hoarseness, and
low grade fever; chest X-ray examination in early stages
shows hilar shadow widening or disease process suggestive
of tuberculosis or carcinoma; disease progresses to death, if
untreated
Signs and Symptoms: as disease progress, sputum
becomes purulent and blood-streaked; fever, dyspnea, loss
of weight and strength, night sweats
disseminated blastomycosis
involves the skin, oronasal mucosa, and subcutanous
tissues, and the respiratory, musculoskeletal, urogenital,
and central nervous systems; the gastrointestinal system is
rarely involved;
Signs and Systems: are determined by body system
affected; destructive lesions occur in vertebrae, tibia and
femur;
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
23
THE MENACING FUNGI
musculoskeletal system - pain and loss of function, takes
the form of osteomyelitis, inflammation of membranes
surrounding bones (periostitis) and septic arthritis;
urogenital system - painful urination, and the presence of
blood and pus in the urine.
cutaneous blastomycosis
a wide variety of skin lesions may occur; ulcerated,
crusted lesions appear resulting from an extension of
lesions from underlying bone and/or subcutaneous lesions,
the introduction of the pathogen by direct inoculation of the
skin; these lesions are secondary to the lung infection;
Laboratory and Related Aspects of Diagnosis
A clinical diagnosis of blastomycosis is presumptive and must be supported by a laboratory
diagnosis. It is necessary to demonstrate the fungus in clinical specimens such as pus, sputum,
or biopsy materials, and to isolate it in culture. Blood (serologic) tests are not useful.
Treatment
The drug-of-choice is itraconazole. However, amphotericin B is used with seriously ill
individuals and in cases of the presence of brain lesions.
Prevention and Control
The most obvious preventative measure in the prevention of PCM infection is the avoiding of
contact with soil contaminated objects possibly containing conidia and/or mycelial fragments in
endemic areas. Disinfection of all contaminated articles is an important preventative measure.
COCCIDIOIDOMYCOSIS
C
occidioidmycosis, also known as San Joaquin Valley fever or simply Valley fever, is a
mycotic disease caused by Coccidioides immitis and the newly proposed related species
C. posadasii. This disease is considered to be a reemerging disease as a result of the
dramatic increase in cases during the 1990’s. Major outbreaks occurred in southern California in
1977, and late 1991 through 1994. A significant increase in cases also occurred in 2003.
Coccidioidomycosis also has long been recognized as a travel-related mycosis associated with
visits to endemic areas in southern California, Arizona, and other neighboring states. Sporadic
cases have been reported in areas where the disease is not endemic. Adding to the importance of
C. immitis is its being added to the growing list of bioterrorism agents.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
24
THE MENACING FUNGI
Habitat
Coccidioides immitis grows in soil in areas of low rainfall, high summer temperatures, and
moderate winter temperatures. The fungus is endemic to the South-western United States
including the San Joaquin Valley of California and southern portions of Arizona, northern
Mexico, parts of Central America such as Guatemala, and Honduras, and in several countries of
South America including Venezuela, Columbia, Paraguay, and Argentina. Coccidioidomycosis
is also endemic in Utah, Nevada, New Mexico, and Texas.
Culture and Microscopic Properties
At room temperature, a C. immitis culture grows as a mycelium (Figure 10) composed of hyphae,
which form typical barrel-shaped arthroconidia (conidia). The conidia are highly infectious
(Figures 4 and 11). In the body (in vivo), C. immitis exists as large spherules ranging in size
from 30 to 200 micrometers, and containing numerous small endospores (Figure 12). Spherules
generally average from 30 to 60 micrometers in diameter, while endospores measure about 2 to 5
micrometers in diameter.
Figure 10. The cottony mycelium of C. immitis. Variations in size and color do occur.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
25
THE MENACING FUNGI
Figure 11. A microscopic view of stained C. immitis arthrospores. Note the barrel-shape of the
conidia and the spaces between the conidia.
Transmission
Humans and other certain other mammals acquire Coccidioidomycosis generally by the
inhalation of C. immitis arthroconidia (spores). The mycelia of the fungus give rise to these
infectious spores (arthroconidia), which become aerosolized when the soil is disturbed.
Outbreaks of the disease often occur after dust storms, earthquakes, and major soil excavations.
In Southern California factors considered to contribute to making the spores more airborne than
usual include wildfires that destroy vegetation thereby exposing soil, followed by high winds.
Rare outbreaks of coccidioidomycosis have been reported among anthropologists, and
archaeologists digging in ruins located in endemic areas. In addition, cases of the disease have
occurred among farmers, construction workers, and ranchers engaged in various types of
activities and exposed to spore-containing soil and dust. The risk of infection in such situations
is quite high.
Coccidioidomycosis is one of the most commonly reported infections among travelers. Such
travel-associated mycoses are the result of a wide range of recreational activities, many of which
involve long-recognized risk factors for the infection.
A number of lower warm-blooded animals can be victims of coccidioidomycosis, and acquire
infection through the inhalation of conidia-bearing dust particles. Cattle, dogs, horses, sheep and
certain wild rodents are susceptible to infection. Birds generally are not susceptible to the
disease.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
26
THE MENACING FUNGI
Life Cycle
The life cycle of C. immitis is somewhat more complicated than most other systemic mycoses. It
involves the development of a hyphae, mycelium, arthroconidia, and spherules, and
endospores. In soil, or on routine culture media preparations for the isolation, the fungus
produces a mycelium with characteristic branching hyphae and arthroconidia that usually, but
not invariably, form in alternate hyphal cells (Figures 4 and 11). As the arthroconidia mature,
the hyphal cells between them disintegrate, and the arthroconidia are released as single
structures. These conidia are barrel-shaped (Figure 11), bear fragments of the cell material from
the disrupted adjacent hyphal cells, and measure about 3 by 6 micrometers.
In tissue or on specially prepared media, the arthroconidia transform into spherical, large
endospore-containing spherules (Figure 12). These spherules range in size and can reach 200
micrometers in diameter. Upon maturity, the spherules rupture to release their endospores,
which may in turn develop into spherules. Figure 13 provides a general view of the life cycle of
C. immitis.
Figure 12. A stained tissue specimen containing a typical endospore-containing C. immitis
spherule.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
27
THE MENACING FUNGI
Mycelium Development
Soil Cycle
Arthroconidia
Endospores
Endospore
Stage
Immature
spherules
Parasitic Cycle
In Host
Segmentation
Spherule
Development
Figure 13. The life cycle of C. immitis. The soil cycle and the host parasitic cycle, which
takes place in the human, are shown.
Pathogenesis
Coccidioidomycosis is usually initiated when aerosolized arthroconidia are inhaled. Such
conidia are small enough to reach the lower respiratory tract, including the alveolar air spaces.
Upon gaining entrance to this body area, the interaction of host defenses and various fungal
factors, determines the outcome of the infection. A combined pyogenic and chronic
inflammatory response often develops. In a small percentage of cases, the spherules rupture and
the infectious process spreads and produces the progressive form of the disease described in a
later section.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
28
THE MENACING FUNGI
Since most cases of the mycosis are self-limiting and produce minimal symptoms, the only
evidence of infection is the development of an immune response. This response usually takes the
form of a conversion of the individual’s negative skin test response to a positive delayed type
skin reaction and the production of specific antibodies (immunoglobulins) to C. immitis proteins.
Individuals At Risk
This group includes HIV-infected persons, the elderly, diabetics, pregnant women in their third
trimester, and a variety of ethnic groups including African-American, and Filipino-Americans.
Both localized pneumonia and disseminated (spreading) infection are usually observed in those
individuals with CD4+ T lymphocyte counts less than 250 cells / microliter.
The disseminated form of coccidioidomycosis also is more likely to occur among persons with
blood group B and individuals with genes that code for certain histocompatibility (tissue)
antigens. The histocompatibility antigens are also known as the human leukocyte antigen
(HLA) complex.
Clinical States
The severity of coccidioidomycosis varies from an inapparent upper respiratory infection to a
disseminated (spreading) fatal disease, and is only symptomatic in approximately 40 percent of
cases. Most patients experience the signs and symptoms of a flu-like illness. The two most
common clinical presentations of coccidioidomycosis are disseminated disease and meningitis.
Asymptomatic infections are generally detected only with the aid of positive skin tests showing a
hypersensitivity to coccidioidin or spherulin. These skin testing materials are specific proteins
extracted from C. immitis. It should be noted that the disease is not contagious.
Clinical manifestations of the disease have been classified into three general groups:
1. initial (primary) pulmonary coccidioidomycosis;
2. pulmonary complications;
3. extrapulmonary disease.
Table 5 lists these conditions together with their distinguishing features.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
29
THE MENACING FUNGI
Table 5. Coccidioidomycosis Clinical Manifestations
Clinical Manifestation
Distinguishing Features
initial (primary or acute)
pulmonary coccidioidomycosis
usually self-limiting and is symptomatic in
approximately 40 percent of cases; usually begins
as a respiratory infection after inhaling airborne C.
immitis arthrospores; incubation period generally varies
between 7 to 28 days. a
Signs and Symptoms: backache, fatigue, fever, cough,
headache, and muscle and joint aches and pains; a
generalized macular, erythematous rash (small red spots)
may appear in about 10 percent of patients. (The presence
of a rash and associated joint pains were, in fact responsible
for the name “desert rheumatism” given to the disease by
some of the early victims.)
pulmonary complications
Signs and Symptoms:
lesions are confined to the lungs, giving pulmonary
symptoms of varying severity, and sometimes result in
cavitation; chest X-rays typically show pulmonary
infiltrates, which may be single or multiple, segmental, or
lobar - such X-rays also may show a widening of hilar
shadows (hilar adenopathy).
frequent pleuritic pains, which may be severe and appear so
suddenly as to simulate a traumatic rib fracture, heart
attack, an acute inflammation of sac enclosing the heart, or
a gall bladder attack (pain associated with respiration may
be accompanied by substernal pain or pressure, and when
the latter is severe it may interfere with swallowing).
EXAMPLES OF COMPLICATIONS
a.) Chronic pulmonary cavitation: most frequent
complication of primary coccidioidomycosis; occurs in
approximately 2 to 8 percent of symptomatic infections; the
cavity usually, but not always, has a thin wall with little
surrounding reaction, and is solitary; this complication may
be almost without symptoms, and discovered only
accidentally during a routine X-ray examination; cavities
may not respond to chemotherapy, and progressive
enlargement of a chronic cavity often is related to
secondary bacterial infection.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
30
THE MENACING FUNGI
Signs and Symptoms: cough, slight chest pain, sputum
production, and hemoptysis; the cavity may persist for
several years without the disease spreading to other body
areas;
b) Coccidioidoma: usually represents a healed or arrested
pneumonitis or granuloma; such conditions usually remain
stable, but may contain some calcium;
Signs and Symptoms: patients are asymptomatic, and the
condition does not represent a hazard of probable
reactivation; the lesion however, may present a medical
problem in that it may be difficult to differentiate it from a
carcinoma.
c) Bronchiectasis and pulmonary fibrosis: occasional
complications of primary coccidioidomycosis;
Signs and Symptoms: empyema, pneumothorax, and
hydropneumothorax may complicate the primary form of
coccidioidomycosis, and may be related to a spreading of
the initial lesion.
d) Chronic coccidiodomycosis: most frequently observed
in diabetics and in immunocompromised patients.
Extrapulmonary Disease
as a rule, primary infection usually ends in recovery,
however, in a small percentage of cases, the infection
spreads from the lungs to produce the progressive form of
coccidioidomycosis; this form of disseminated disease
occurs most often in non-white individuals, particularly
African- and Filipino-Americans, males, pregnant women,
and immunocompromised persons;
Disseminated (spreading) infections may occur promptly
and rapidly by the circulatory spreading of endospores
(Figure 7) from the lungs to other organs; the rapidity of
spreading spores appears to be related to the failure of the
immune system to stop the process; in the progressive or
secondary form (also known as coccidioidal granuoma);
the progression of this form of coccidioidomycosis may be
slow or rapid, or the patient may recover, except in cases of
acute wide spreading of the spores and meningitis.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
31
THE MENACING FUNGI
Signs and Symptoms: disease process spreads to the skin,
subcutaneous tissues, the bones, meninges, and internal
organs; skin lesions resemble those of certain other deepseated mycoses, while in other parts of the body they
resemble those of tuberculosis;
The signs and symptoms are site-specific and include wartlike nodules, papules, and ulcers involving the skin,
headache, and arthritic pains and swelling in the joints,
especially in the knees and/or ankles; multiple painful
lesions also may develop in the skull, hands, feet, spine, or
long bones; the course of the disease is marked by
remissions and exacerbations; unfortunately, the mortality
is high.
a
A massive exposure to contaminated soil or to the careless handling of positive C. immitis
cultures in a laboratory is followed usually by a shorter incubation period.
C. immitis as well as Histoplasma capsulatum are among the know causes of communityacquired pneumonia (CAP).
HIV-Infected Patients
As indicated earlier, immunocompromised individuals are at a much higher risk for severe forms
of coccidioidomycosis. Pulmonary infection in such patients may develop into one of several
complications including pulmonary nodules, thin-walled cavities, progressive pneumonia,
pyopneumothorax, and bronchopleural fistula.
Disease susceptibility to coccidioidomycosis is highest in HIV-infected persons who have a
severe depletion in their CD4+ lymphocytes. This condition corresponds to a laboratory finding
of <200 CD4+ cell/ cubic millimeters of blood. Cocccidioidomycosis should be suspected in
such individuals if they have lived or traveled in an endemic area for the disease, or who may
have otherwise been exposed to the disease agent. Unfortunately, the prognosis for individuals
with a low CD4+ count is poor. The progression of the disease is rapid and inevitably fatal.
Signs and Symptoms: HIV-infected patients commonly experience a cough, dyspnea, and
fever. Skin lesions and meningitis are uncommon. Chest X-rays typically show the diffuse
reticulonodular pattern of extensive involvement as well as focal pulmonary infiltrates similar to
those found with bacterial pneumonias.
Solid-Organ Transplant Recipients
Recipients of solid-organ transplants also are at an increased risk of developing disseminated
coccidioidomycosis. This form of the disease was first reported among solid-organ transplant
recipients (SOTRs) in the late 1960’s. Since this time it has been increasingly recognized among
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
32
THE MENACING FUNGI
SOTRs, with the majority of infections occurring in the first year after transplantation. The
mortality rate associated with the disseminated disease has been reported to be as high as 72
percent among such patients. The possible sources of C. immitis in SOTRs is believed to be
donor organs. In 2003, P.W. Wright reported two cases of disseminated coccidioidomycosis in
SOTRs that resulted from the transmission of C. immitis from a single organ donor with
unrecognized active coccidioidomycosis at the time of his death.
Laboratory and Related Aspects of Diagnosis
Radiologic studies such as chest X-rays, and bone scans, are of value in determining the extent
and severity of the disease process, but unfortunately cannot distinguish coccidioidomycosis
from other pulmonary diseases. A definitive diagnosis requires laboratory procedures including
the microscopic examination of body fluids and/or tissue specimens, culture, and
immunoserologic evidence. The latter approach involves tests to detect specific antibodies (the
immunoglobulins IgG and IgM) against C. immitis antigens, and skin testing procedures.
The isolation and culture on appropriate laboratory culture media and demonstrating the presence
of arthroconidia (Figure 11) as described earlier is specific, but requires a significant long
incubation period for results. The finding of typical spherules (Figure 12) in sputum, and/or
tissues biopsy materials also is diagnostic and much faster than the isolation approach. A
commercially available deoxyribonucleic acid (DNA) probe also can be used to identify isolated
cultures of the fungus.
Serologic diagnosis is of value showing the presence of specific antibodies against C. immitis
antigens. Several antibody (immunoglobulin) responses are particularly diagnostic. The tests
used include the immunodiffusion test, enzyme-linked immunoabsorbent assay (ELISA),
complement fixation test, and the polymerase chain reaction (PCR). Each procedure has distinct
advantages and disadvantages. The PCR assay is the most rapid of the ones listed.
Skin Tests. Skin tests are performed in a manner similar to that used with the tuberculin skin
test. A filtered extract of a C. immitis culture, known as coccidioidin, is commonly used for
testing purposes and is injected intradermally. Spherulin, an extract of the spherule phase of the
fungus also has been used for skin testing.
Skin tests measure the delayed type hypersensitivity response of the individual to C. immitis
antigens. The results of the procedure are usually read 48 hours after the injection of the skin
testing material. It should be noted that it takes approximately 3 weeks after exposure to C.
immitis to develop a positive skin test. A positive reaction indicates previous exposure to the
fungus, or in some cases the result of repeated testing. Generally, individuals with a normal
positive skin test are immune to a second attack of the fungus.
A negative skin test may mean several things including: 1) the test was performed too early in
the disease process, 2) a case of disseminated coccidioidomycosis exists in which the individuals
immune response has been impaired; 3) the current illness of the patient is not the disease being
tested for, 4) the individual being tested is immunocompromised and the immune system has
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
33
THE MENACING FUNGI
been impaired.
While skin tests have limited diagnostic value, they can be useful in epidemiologic investigations
and in evaluations of individuals exposed to C. immitis after previously producing negative skin
test reactions.
Treatment
The common form of coccidioidomycosis is a self-limited type of infection and other than
supportive care usually does not require antimycotic therapy. Treatment is recommended in
certain cavitary forms of the disease, and is required for disseminated coccidioidomycosis.
Amphotericin B, the first effective antimycotic used for treatment, remains the drug standard by
which all newer preparations are judged. It is not the drug-of-choice for long term use largely
because of its toxicity. Amphotericin is administered intravenously for two to three months for
the treatment of both localized and disseminated forms of the disease. Newer antimycotics such
as fluconazole, itraconazole, and ketoconzole provide many of the same benefits found with
amphotericin B and are significantly less toxic. Table 6 lists examples of drugs used in treatment
together with dosages and associated side-effects. These newer preparations are available for
oral administration.
Table 6. Examples of Drugs Used in the Treatment of Coccidioidomycosis
Drug
Dosage
Noted Side -Effects
amphotericin B
0.5-0.7mg/kg/day
fever; nausea, vomiting, kidney toxicity,
potassium and magnesium depletion
fluconazole
400-600 mg/day
high relapse rate
itraconazole
200 mg/twice per day
poor absorption of the drug, drug
interactions, and relapse rate
ketoconazole
400 mg/day
nausea, vomiting, liver toxicity, adrenal
suppression, abnormal breast development
in males, no absorption in patients with no
hydrochloric acid in their stomachs, drug
interactions, and high relapse rates
Since most of the newer drugs inhibit fungal growth (fungistatic) rather than kill the disease
causing fungus (fungicidal), relapses are common occurrences. In addition, the optimal time
period of therapy is not known. The information currently available on relapse situations points
to the continuation of treatment for at least six months after fever, and a significant reduction
and/or elimination of the signs and symptoms have occurred.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
34
THE MENACING FUNGI
Several drugs for treatment are under study. These include new formulations of amphotericin B
and the azoles. Among these are the azoles DO870, which is effective against fluconazoleresistant fungi, and nikomycin A, which inhibits fungal growth not only of C. immitis, but other
dimorphic pathogens as well.
In 2004, T.T. Kuberski et al, reported the use of the immune-modulating (strengthening) agent
interferon-gamma as an adjunct to conventional antifungal therapy for a patient with
disseminated C. immitis infection and respiratory failure. The addition of the agent resulted in
the improvement of the patient’s condition and subsequent discharge from the hospital.
Surgery, in the form of pulmonary resection, while being required less often, continues to play a
role in the management of hemoptysis and extensive pulmonary cavitation. Other invasive
procedures may be used in managing empyema, or persistent bronchopleural fistula.
Potential organ transplant patients should receive antifungal therapy prior to their respective
operations. Therapy should also be given as soon as possible to patients experiencing acute
organ rejection, and to HIV-infected pregnant women who have previously experienced C.
immitis infection.
Prevention and Control
The most obvious preventative measure in the prevention of C. immitis infection is the avoiding
of contact with dusty soil and/or body fluids and tissues possibly containing arthroconidia,
spherules, or endospores. The planting of grass and other types of plants, as well as paving
roads in highly populated endemic areas are valuable preventative measures.
Periodic skin testing and the testing for IgG (antibodies) against C. immitis at about six-month
intervals may provide the basis for an early detection of the disease.
The use of oral azoles as a preventative measure is not recommended, and should be used only in
cases of serious complications. The use of these drugs is different for HIV-infected persons.
Once started, oral azole treatment in such cases must be continued for the lifetime of the
individual.
HISTOPLASMOSIS
H
istoplasmosis, also known as Darling’s disease is caused by the dimorphic fungus
Histoplasma capsulatum. The name of this pathogen was suggested by S.T. Darling in
1906 and was based on the histological appearance of yeast-like cells in the
macrophages of a patient.
The Causative Agents
There are three known varieties of H. capsulatum, namely H. capsulatum variety capsulatum, H.
capsulatum variety duboissi, and H. capsulatum variety farciminosim. Each of these varieties
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
35
THE MENACING FUNGI
produce a distinctive histoplasmosis syndrome. Only the H. capsulatum variety capsulatum will
be principally considered in this course.
H. capsulatum is recognized as an intracellular pathogen. This fungus can involve the
lymphatic system, spleen, liver, adrenals, kidneys, skin, and the central nervous system.
Habitat
H. capsulatum has been isolated from soil containing high nitrogen concentrations, especially
those relating to the fecal droppings of chickens and birds such as blackbirds which include
starlings, grackles, red-winged blackbirds, and cowbirds, and those of bats. Outbreaks of
pulmonary histoplasmosis have been linked to exposure to these H. capsulatum reservoirs in
their natural settings as well as to materials contaminated by the fecal material. Because of their
high body temperatures birds are not infected with H. capsulatum, however, their fecal droppings
provide a rich source of nutrients and a favorable growth environment. The habitats of pigeons,
and poultry houses with dirt floors, have been found to be heavily contaminated with H.
capsulatum. Determining whether or not soil and other types of materials are contaminated with
this fungus requires the collection of specimens and the subsequent culturing on appropriate
nutrient media by trained laboratory personnel.
Bats on the other hand, because of their lower body temperature, can become infected and carry
the fungus to other locations. Other warm-blooded animals also can become infected with H.
capsulatum. These include bears, cats, dogs, mice, opossums, raccoons, rats, and skunks.
Although histoplasmosis is found throughout the world, it is principally endemic along the Ohio,
Mississippi, and St. Lawrence rivers. The disease agent also has been found in other areas of the
United States. Wet or dry seasons do not appear to have an association with infections.
Culture and Microscopic Features
In soil and on laboratory culture media incubated at 25o C. (room temperature) H. capsulatum
produces a typical white to brown mycelium. Microscopically, a mycelium consists of
branching hyphae that form small single conidia (microconidia) and larger spores with spiny or
fingerlike structures on their surfaces. The large spores are distinctive and are referred to as
tuberculated macroconidia (Figure 14). This form of the fungus can be converted to its yeast
form by cultivation at 37o C. (body temperature). The microconidia are infectious and cultures
should be handled with strict biosafety precautions.
It should be noted that the mycelia of H. capsulatum, as well as other pathogenic fungi do not
appear overnight. In most cases at least three to four weeks are required for best results.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
36
THE MENACING FUNGI
Figure 14. A microscopic view of a tuberculated macroconidium at the end of a branching
hypha of H. capsulatum.
After the microconidia are inhaled by an individual, they undergo a sequence of changes that
transform them into yeast cells. These transformed cells are generally found in tissue
macrophages, however, they can also be found extracellularly.
Life Cycle
The life cycle of H. capsulatum involves the development of hyphae, a mycelium, micro- and
macro-conidia, and yeast cells. In soil, or on routine culture media preparations for the
isolation, the fungus produces a mycelium with characteristic branching hyphae and micro- and
macroconidia when incubated at room temperature. The yeast phase of the cycle occurs in tissue
or when cultures are incubated at body temperature (37o C). Inhaled microconidia are engulfed
by macrophages and are transformed into oval to spherical-shaped yeast cells.
Transmission
Histoplasmosis follows the inhalation of small conidia into the lungs, where they germinate and
are transformed into budding yeast cells. The disease is not contagious since it cannot be
transmitted from an infected individual or lower animal to someone else.
H. capsulatum can be carried on the wings, feet, and beaks of birds and thereby bring about the
contamination of soil under bird roosting sites, or manure accumulations inside or outside of
building.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
37
THE MENACING FUNGI
Exposure Risks
Histoplasmosis also is known as cave sickness or speleonosis, largely because some of its
victims have been spelunkers (cave explorers). Other victims of the disease tend to be outdoor
types such as farmers, construction workers, gardeners, roofers, chimney sweeps, heating and/or
air conditioning service personnel, individuals involved with the restoration of historic or
abandoned buildings, and pest control workers.
Pathogenesis
Histoplasmosis usually starts when microconidia of H. capsulatum growing in soil or on material
contaminated with infectious bird or bat fecal matter is aerosolized. Upon gaining entrance to
this body area, the interaction of host defenses and various fungal factors, determines the
outcome of the infection.
The inhaled microconidia are engulfed by macrophages of the body where the fungal cells
undergo as sequence of structural changes and become yeast cells. These cellular events are
crucial to both natural and acquired resistance of the host to H. capsulatum. The yeast cells of
this fungus survive in host polymorphonuclear leukocytes and grow and reproduce in circulating
mononuclear phagocytes. Progressive spreading of the infection involves reticuloendothelial
host cells such as those found in the lymph nodes, liver, and spleen.
Clinical States
Histoplasmosis can present a variety of clinical manifestations, which may be grouped according
to the following categories:
1. body location: pulmonary, extrapulmonary, or disseminated;
2. duration of infection: acute, subacute, or chronic;
3. pattern of infection: primary versus reactivation.
Table 7 lists examples of these forms of H. capsulatum disease according to body location and
duration of infection, together with descriptions of the conditions.
Primary pulmonary infections may develop in healthy, immunocompetent hosts exposed to a
massive concentration of H. capsulatum conidia, while elderly individuals, and
immunocompromised patients, may experience a reactivation of primary histoplasmosis. Cases
of reactivated disease must be distinguished from other fungus infections, tuberculosis, and
various types of cancers.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
38
THE MENACING FUNGI
Table 7. Clinical Manifestations of H. capsulatum Infection
Clinical Manifestation
Features of the Condition
primary pulmonary infections
may be asymptomatic, subclinical, or a self-limited
pulmonary disease of varying degrees of severity that
leaves multiple areas of calcification (small calcified foci)
in the lungs and lymph nodes of the chest.
Chronic cavitary disease: may result from a small
percentage of primary pulmonary cases and can worsen
with time, especially if the condition is not diagnosed and
treated appropriately; resembles tuberculosis.
Disseminated disease: the most severe and rarest form of
histoplasmosis.
primary acute histoplasmosis
the vast majority of individuals are asymptomatic.
the only evidence of exposure and of the asymptomatic
infection is a positive skin test, which uses an antigen
prepared from the mycelial phase of H. capsulatum called
histoplasmin.
Signs and Symptoms: appear within 3 to 17 days, and
generally suggest a flu-like illness, and include fever, a dry
or nonproductive cough, headache, chest pain, shortness of
breath, chills, and joint and muscle aches and pains.
disseminated histoplasmosis
involves the reticuloendothelial cells of the body, such as
those found in the liver, spleen, and lymph nodes. Yeast
cells are present intracellularly.
Signs and Symptoms: irregular fevers, loss of weight, a
reduction in the number of leukocytes, ulcerating lesions in
the nose and mouth, and enlargements of the spleen, liver,
and lymph nodes are evident.
cavitary histoplasmosis
occurs predominantly in adults; some cases may represent
reactivation of a primary lung lesion, or an uninterrupted
progression of a pulmonary lesion. In this form of
histoplasmosis, the disease process has spread and if the
severity of the condition increases, any of the usual
manifestations of disseminated histoplasmosis listed earlier
may appear.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
39
THE MENACING FUNGI
Signs and Symptoms: closely resemble those found with
tuberculosis, and include productive cough, low-grade
fever, occasional hemoptysis, and radiological findings of
pulmonary cavitation.
extrapulmonary histoplasmosis
exposure to massive numbers of conidia results in a rapid
fatal end.
Signs and Symptoms: the pulmonary manifestations may
be less prominent and the signs and symptoms listed for
earlier for the primary acute form of histoplasmosis
characterize the condition; any of the manifestations may
predominate and the illness then appears as carditis,
meningitis, adrenal gland or liver insufficiency, or as large
solitary or multiple lesions in various parts of the
gastrointestinal system. When intestinal lesions
predominate, it is possible that the primary lesions may
have been in the intestinal lymphatics, and that infection
followed ingestion rather than inhalation of H. capsulatum
microconidia.
Laboratory and Related Aspects of Diagnosis
Radiologic studies, which include chest X-rays, and body scans, are of value in determining the
extent and severity of the disease process, but unfortunately cannot distinguish histoplasmosis
from other fungus-caused pulmonary diseases, tuberculosis, or various forms of cancers. A
definitive diagnosis requires laboratory procedures including the microscopic examination of
sputum, peripheral blood, and aspirated material from lymph nodes and bone marrow. Culture
isolation and immunoserologic evidence (blood tests) also are important to diagnosis. The latter
approach involves tests to detect specific antibodies (the immunoglobulins: IgA, IgE, IgG and
IgM) against H. capsulatum antigens, and skin testing. Several specific immunologic tests are
used. These include immunodiffusion, complement fixation, and latex agglutination. A PCR
assay, which is one of the most rapid procedures, also is available.
The isolation of H. capsulatum on appropriate laboratory culture media and demonstrating the
presence of the tuberculated macroconidia (Figure 9) as described earlier is specific, but requires
a significant long incubation period for results. The finding of the yeast cell phase in sputum,
and/or tissues biopsy materials also is diagnostic and much faster than the isolation approach.
Skin Tests. Skin tests are performed in a manner similar to that used with the tuberculin skin
test. A filtered extract of a H. capsulatum mycelial culture, known as histoplasmin is used for
testing purposes and is injected subcutaneously.
Skin tests measure the delayed type hypersensitivity response of the individual to H. capsulatum
antigens. The results of the procedure are usually read 48 hours after the injection of the skin
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
40
THE MENACING FUNGI
testing material. It should be noted that it takes approximately 3 weeks after exposure to the
fungal pathogen in order to develop a positive skin test. A positive reaction indicates previous
exposure (infection) to the fungus.
Treatment
In its common form, histoplasmosis is an acute, self-limited infection that generally does not
require therapy other than supportive care. In some cavitary forms of the disease therapy is
recommended with amphotericin B. Some of the newer antimycotic drugs mentioned earlier for
the treatment of coccidioidomycosis may prove useful as experience with them develops.
Amphotericin B is currently considered to be the first-line treatment for patients with severe
forms of disseminated histoplasmosis. In other cases, itraconzole may be used. The advantages
of itraconzole therapy over amphotericin B include lower toxicity, and the possibility of oral
administration.
Prevention and Control
The most obvious measure for the prevention of H. capsulatum infection is avoiding contact with
areas and/or objects that may harbor the fungus such as bird or bat fecal matter. Other
recommended preventative measures include:
1) posting of signs warning of health risks,
2) preventing the accumulations of bat and/or bird fecal matter, which would include
areas such as bird roosts, attics, and related locations,
3) removing and excluding bats and/or birds from buildings, (this involves the closure
and sealing of any and all possible entrances),
4) carefully wetting areas from which infectious material is to be removed before any
removal is attempted,
5) using industrial vacuum systems for removal of bat and/or bird droppings,
6) collecting infectious material in secure containers for immediate disposal,
7) properly using formaldehyde solutions to treat contaminated areas when removal
procedures are impractical (formaldehyde solutions are the only disinfectants proven
to be effective for soil decontamination),
8) using water sprays or other dust suppressing techniques to reduce the amount of dust
aerosolized during times of construction, excavation, or demolition in locations
where H. capsulatum is endemic,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
41
THE MENACING FUNGI
9) wearing National Institute for Occupational Safety and Health (NIOSH)-approved
respirator and other equipment items by workers to reduce the risk of H. capsulatum
exposure, using the appropriate respirator selected on the basis of the circumstances
associated with airborne contaminant exposure in line with occupational exposure.
Respirators provide different levels of protection. They are divided into classes based on
assigned protection factors to provide comparisons of the protective capabilities in relation to
other respirator classes. The protection factor assigned to a respirator is a unitless number
determined statistically from a set of experimental or work place data. Regardless of which
respirator is selected, the device should be NIOSH-certified, and used in the context of a
respiratory protection program. (Additional information can be obtained from the following
agencies: National Institute for Occupational Safety and Health, National Center for Infectious
Diseases, the Centers for Disease Control and Prevention, or local health departments).
THE IMMUNOCOMPROMISED PATIENT
S
ince 1987, disseminated histoplasmosis (DH) has been included among AIDS-defining
infections. The disease state generally occurs when a patient’s CD4 + T lymphocyte count
is <150 cells/mictoliter. The most frequently infected organs are the lungs and bloodforming organs, although all body organs are susceptible. Localized pulmonary histoplasmosis
might occur among individuals with CD4+ T lymphocyte counts greater than 300 cells/
microliter. Without appropriate treatment, the disease has a rapidly fatal course.
Individuals at Risk. In addition to persons with AIDS, other individuals are at risk for
developing severe and disseminated histoplasmosis. These include persons with cancer,
recipients of high-dose, long-term steroid therapy, and individuals undergoing cancer
chemotherapy.
PARACOCCIDIOIDOMYCOSIS
P
aracoccidioidomycosis (PCM) is an important systemic mycosis in Central and South
America. The disease is frequently diagnosed in Brazil and Columbia. The lungs are the
main target and the site at which both active and residual lesions appear regularly.
Habitat
Although the exact habitat of P. brasiliensis is not known, the pathogen occurs most often in
subtropical forests. Isolations during the early history of the fungus were made from soil. The
habit of cleaning teeth with twigs, grass and other pieces of vegetation may serve as the primary
means of introducing the pathogen and initiating lesions in the oral mucosa, tongue, or gums.
Culture and Microscopic Features
Paracoccidioides brasiliensis is a large dimorphic fungus. In culture at room temperature, the
fungus grows slowly and forms a white cottony mycelium consisting of very short hyphae
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
42
THE MENACING FUNGI
without conidia. In tissues and laboratory cultures incubated at 370 C., the fungus takes the form
of large spherical or oval cells capable of reaching diameters of 30 micrometers. Such
distinctive large cells bear buds ranging in size from 1 to 5 micrometers in diameter.
Transmission and Pathogenesis
Humans probably acquire P. brasiliensis by the inhalation of conidia and mycelial fragments.
These infectious particles reach the lungs, convert to the yeast form, and initiate the primary
infection. The process usually is silent (asymptomatic), and may result in the appearance of
signs and symptoms over the course of a few years. The silent course of the disease results in a
steady progression of lung injury, which ultimately affects the health of patients.
There is no evidence for person-to-person transmission.
Clinical States
The duration of PCM varies from a few months to 2 or 3 years. When the clinical manifestations
become apparent, the disease may appear in several different forms. The most frequent site of
primary lesions is the mouth, followed by the lungs, larynx, and skin, respectively. Table 8 list
the known clinical forms of PCM together with their main clinical features.
Table 8. The Clinical States Found with Paracoccidioidomycosis.
Clinical Manifestation
Feature(s)
pulmonary lesions
the lungs are the primary site and the main target of
PCM; pulmonary involvement occurs in most individuals;
the disease may appear as an acute-subacute (juvenile)
form or chronic, adult form; the oral mucosa is usually the
site of primary lesions;
Signs and Symptoms: the lesions are bilateral and
symmetrical with involvement of all pulmonary areas;
cavity formation occurs with residual fibrotic lesions
appearing in approximate 60 percent of patients; the
progression of PCM results in the involvement of other
body organs such as adrenal glands, liver, lymph nodes,
spleen, and skin.
oral lesions
conspicuous lesions develop in the nasal or oral mucosa,
the gums, and at times in the lining of the eyelid or the
anorectal area;
Signs and Symptoms: the oral infection can spread slowly
producing severe, ulcerative and painful gum infection;
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
43
THE MENACING FUNGI
gum lesions and those surrounding teeth loosen teeth which
are lost by natural means or may require extraction; the loss
of teeth, and gum involvement interfere with the feeding
contributes to a rapid wasting of patients; these lesions may
also appear on the plate, tonsils, and tongue.
skin lesions
a wide variety of skin lesions may occur;
Signs and Symptoms: ulcerated, crusted lesions appear on
the face resulting from an extension of lesions from the oral
cavity or, are secondary to the spreading of PCM
throughout the body via the circulatory system and result
from lymph drainage.
visceral lesions
the lymphatic system, intestines, spleen and liver
also are often infected in PCM;
Signs and Symptoms: lesions typically develop in the
spleen and the intestines; the stomach is rarely involved.
Laboratory and Related Aspects of Diagnosis
Laboratory diagnosis primarily depends on obtaining suitable specimens from lesions in the
mouth and/or draining lymph nodes. Microscopic examination usually will reveal P. brasiliensis
cells. Culture methods are also effective, but due to the slow growth rate of the pathogen,
mycelia will not appear for at least 20 days.
Radiologic abnormalities with this mycosis are often extensive and should alert physicians in
areas where P. brasiliensis is endemic to the possibility of infection. In addition, individuals
from endemic areas residing or visiting other parts of the world, and who have a history of
chronic, nonspecific constitutional signs and symptoms should be examined radiologically. This
type of inexpensive may reveal findings that are suggestive of PCM and provide an earlier
opportunity to initiate treatment and to avoid or control the extensive fibrosis that occurs with the
mycosis.
Treatment
Through the years has profoundly changed the outcome for patients with
paracoccidioidomycosis. The most important advance was the introduction and use of the azole
derivatives: ketoconazole and itraconazole. With these drugs, a relatively short course of
treatment and few secondary effects usually is experienced by patients. A course of treatment
with itraconazole with daily doses of 100-200 milligrams for 6 months has been found to be
effective in approximately 95 per cent of patients with active disease. The relapse rate is around
5 per cent.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
44
THE MENACING FUNGI
Despite the effectiveness of itraconazole treatment, the development of lung fibrosis does not
appear to be modifies. Such fibrotic sequelae is related to the severity and infiltration of the
pathogen and may be avoided to a large extent by prompt initiation of appropriate treatment.
Prevention and Control
The most obvious preventative measure in the prevention of PCM infection is the avoiding of
contact with soil contaminated objects possibly containing conidia and/or mycelial fragments in
endemic areas.
THE OPPORTUNISTIC FUNGAL PATHOGENS
THE ASPERGILLOSES
A
spergilloses are fungus diseases that occur worldwide and can affect all ages and sexes.
These diseases can be broadly defined to collectively include any infection caused by a
species of Aspergillus. One of the first identifiable cases of aspergillosis (singular form)
was reported by the renown pathologist Rudolph Virchow in 1856. Several aspergilli are known
to cause disease in lower animals as well.
General Properties of the Aspergilli
Aspergilli are rapidly growing molds producing fluffy, variously colored colonies (mycelia)
within 2 days on laboratory media or food (Figure 15). Aspergillus species are identified on the
basis of differences in their microscopic structures including hyphae (conidiophores) and the
arrangement of spores (conidia).
Figure 15. The appearance of mycelia. Two growths of two different aspergilli are shown. The
greenish (lighter color) growth is that of A. flavus, and the black mycelium is that of A. niger.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
45
THE MENACING FUNGI
Habitat
The aspergilli are widely distributed in nature and found throughout the world. They are
common inhabitants of soil, and air, and seem to adapt to a wide range of environmental
conditions. Their natural ecological niche is the soil, wherein they survive and grow on organic
matter. In general, because the majority of aspergilli live on decaying organic matter, they are
considered to be saprophytes. Several species play essential roles in recycling environmental
carbon and nitrogen. Since the aspergilli are capable of producing a large variety of digestive
enzymes, they can use an enormous number of substances as nutrients, it is difficult to find a
substance containing some organic matter and a little moisture on which these fungi cannot grow
and reproduce.
Microscopic and Cultural Properties
In the clinical laboratory, aspergilli are easily isolated on most media used for fungi, and tend to
reproduce in their asexual form (Figure 16). The microscopic appearance of these fungi in
culture consists of long, branching filaments (hyphae) containing typical cross-walls. Hyphae
may or may not give rise to asexual reproductive structures called conidiophores. The
conidiophores arise directly from hyphae, and end in thick rounded heads known as vesicles.
These vesicles may be either totally or partially covered by flask-shaped structures from which
the reproductive units known as condiospores (conidia for short) are blown out into the
surrounding environment. Every vesicle produces spores numbering in the thousands. While the
size, shape, color, and thickness differ among the species of aspergilli, they generally have an
average diameter of about 2.0 to 3 micrometers. Their small size allows for easy dispersion on
air currents, and easy access to lung alveoli.
Figure 16. A microscopic view of Aspergillus fumigatus showing hyphae, conidiophores (Cp),
vesicles (V), and conidia (C).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
46
THE MENACING FUNGI
Aspergilli generally do not have elaborate mechanisms for releasing their conidia into the air.
Spreading of the conidia relies on disturbances and strong air currents. Once in the air, the small
size of conidia enables them to float, and to be airborne both indoors and outdoors. Interestingly,
some environmental surveys indicate that all humans will inhale at least several hundred spores
of Apergillus fumigatus conidia per day. A. fumigatus is the most common cause of Aspergillus
infection worldwide.
Aspergilli are rapidly growing molds producing fluffy, variously colored colonies known as
mycelia (singular, mycelium) within 2 days on laboratory media or food stuffs (Figure 16).
Aspergillus species are identified on the basis of differences in the structure of conidiophores and
the arrangement of conidia.
Nonpathogenic and Pathogenic Aspergilli
Of the hundreds of recognized species of aspergilli, only a little over 20 have been verified to
cause human infections, and only 5 of these consistently and regularly are encountered as causes
of disease.
Because of their great enzymatic capabilities, several aspergilli are used in various industrial
processes. These include the commercial production of citric acid by A. niger for use by the soft
drink industry, and the processing of soybeans by A. wentii in Japan.
Aside from their disease causing-associations, certain aspergilli also cause considerable
problems as contaminants in diagnostic laboratories by interfering with the isolation of various
bacterial and fungus pathogens. Others reduce the commercial value of and ruin leather and
cloth fabrics by being capable of growing on such products. The aspergilli impart a musty odor
to clothes and shoes. In humid tropical climates, these are especially troublesome and
individuals have to keep their wardrobes as dry as possible from being covered with heavy
fungal growths.
Mycotoxins. Aspergilli are often found growing on various types of foodstuffs, which they are
capable of decomposing and causing decay. In so doing some species of Aspergillus and of
other genera produce toxic substances known as mycotoxins. One of the most important of such
poisonous products are the aflatoxins. These toxic metabolic products are associated with
contaminated cereals, nuts, and animal feed. The aflatoxins as well as other mycotoxins are
discussed in greater detail in a later section.
Disease States. The most common Aspergillus species causing invasive disease include A.
fumigatus, A. niger, A. terreus, and A. nidulans. Certain species are known to cause a variety of
allergic states. These include A. fumigatus, and A. clavatus. Another important pathogen of the
genus is the already mentioned A. flavus, which is known for the production of aflatoxins. The
diseases caused by the aspergilli, and in particular A. fumigatus, can be divided into the
following categories:
1. allergic reactions and complications caused by the presence of conidia or temporary
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
47
THE MENACING FUNGI
growth of the fungi in the mouth, nose and other orifices; such allergic diseases
include allergic sinusitis, alveolitis, and asthma will not be discussed in any great
detail this course;
2. colonization without extension in preformed cavities and debilitated tissues within the
respiratory tract, often called aspergilloma or fungus ball;
3. superficial infection of the skin paranasal sinuses (Figure 3), external ear canal, and
more rarely, burn areas after sloughing of tissue, nails, and other body sites;
4. invasive, granulomatous, necrotizing infection of the lungs; and
5. systemic and fatal disseminated disease.
The clinical aspects of several of these disease categories (to be described in a later section) are
determined to a large degree by the general immunologic and physiologic state of the host. It
should also be noted that certain forms of Aspergillus-caused diseases may become integrated or
overlap within a patient
Nosocomial Infections . Aspergillus species are infrequent causes of nosocomial infection. As a
later section will discuss, pulmonary disease is the most common presentation. Wound
infections occur much less frequently, but have been reported to occur after cardiac and
abdominal surgery. Most surgery-associated infections appear to develop from the use of
contaminated dressings, and airborne contamination of wounds in the operating theater.
In 2003, hospital water systems and variable airflow volume (VAV) units located in air ducts just
downstream from final filters in operating rooms were implicated as sources of nosocomial
aspergillosis. The VAV units identified as sources of mold contamination were found to have
insulation, which had deteriorated after becoming wet. Aspergillus conidia released from mold
growing on the insulation were not effectively filtered out before entering the operating theater.
Interestingly in this case, the source of the nosocomial outbreak was located by means of a
closed-space video camera that allowed viewing of otherwise inaccessible ductworks.
Nosocomial outbreaks are encountered most often during or after hospital construction or
renovation, and usually in severely immunocompromised patients.
ASPERGILLUS FUMIGATUS, AN IMPORTANT PATHOGEN
I
n the past 25 years, the mold Aspergillus fumigatus has gone from being a fungus commonly
found in the environment and of minor interest, to one of the most important fungal
pathogens. The main reason for this relatively sudden rise in status is the increase in
systemic infections caused by this microorganism. A. fumigatus has become the most prevalent
airborne fungal pathogen, causing severe and usually fatal invasive infections in
immunocompromised hosts in developed countries. Although the conidia of A. fumigatus make
up only about 0.3 percent of the fungal spores found in the air of a particular hospital, it causes
roughly 90 percent of systemic Aspergillus infections.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
48
THE MENACING FUNGI
Culture Features. A. fumigatus is known as a thermophilic species. It is capable of growing at
temperatures as high as 55o C. and can survive temperatures up to 70o C. As most aspergilli, it is
a rapid grower on laboratory nutrient preparations generally forming a gray-green pigmented
mycelium (Figure 17).
Figure 17. The characteristic gray-green pigmented A. funigatus mycelium.
Pathogenicity
To invade a host, A. fumigatus must be able to attach to and penetrate respiratory epithelial tissue
and kill surrounding cells, specifically phagocytic cells, actively involved in protecting the body
against invasion by A. fumigatus and other pathogens or opportunists. A. fumigatus has several
virulence factors that contribute to its ability to cause disease or pathogenicity. These include the
following:
1. spore size - the small size of A. fumigatus conidia (3 to 5 micrometers) permits
penetration deep into the lung; in addition, such spores are capable of withstanding
extraordinary conditions such as less than optimal host defenses;
2. spore pigment - the pigment of conidia provides some protection against phagocytosis
by macrophages in the lungs and presumably in the nose; macrophage ingestion and
killing of spores in the lungs is the first immunologic line of defense against
Aspergillus;
3. adhesins - enable Aspergillus fumigatus conidia to bind specially to various
circulating host proteins including fibrinogen, albumin immunoglobulins (antibodies),
collagen, and complement;
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
49
THE MENACING FUNGI
4. enzymes - these proteins may provide protection against damage from hydrogen
peroxide, singlet oxygen, hydroxyl, and other free radicals produced by phagocytes;
they include superoxide dismutases, catalases, and phospholipases; these fungal
enzymes can cause damage to host epithelial cells, protect against phagocytosis, and
promote colonization of the lung;
5. toxic molecules - several metabolic products produced by the A. fumigatus are
toxic to the host and can cause cell death, destruction of red blood cells, and suppress
immune responses (immunosuppression); toxic products of A. fumigatus include
hemolysin, a specific toxic molecule known as gliotoxin, and an enzyme to
decompose ribonucleic acid..
Selected A. fumigatus-Associated Diseases
For most individuals, respiratory tract is the main portal of entry and site of infection for A.
fumigatus infections. Other sites have also been reported in immunocompromised patients and
include the skin, bone, eyes, peritoneum, and the gastrointestinal tract.
Allergic disease occurs following repeated exposure to conidia or Aspergillus-antigens in the
absence of mycelial colonization of lung tissue, and in most cases, removal of the individual
from the environmental source of the causative agent results in clinical improvement.
In certain situations, a single parenchymal lesion may develop and subsequently heal with
calcification to form a “coin lesion”. However, in clinically severe forms of aspergillosis,
necrosis and pulmonary cavitation occur. Lesions in such situations continue to spread by radial
extension of the mold’s hyphae beyond the cavity with eventual circulatory system spread to the
kidneys and other body organs.
Invasive Aspergillosis
Invasive aspergillosis (IA) has long been recognized as a leading cause of death, mainly among
hematology patients. The fungus infection, which follows solid-organ transplantation is most
common in heart-lung transparent patients and is found, in decreasing order, in liver, heart, lung,
and kidney recipients. Although IA is considered to be the main fungal infection in cancer
patients, its true incidence is believed to be underestimated due to the low sensitivity of
laboratory diagnostic tests.
While IA is rarely found in immunocompetent individuals, it is reported to occur in AIDS
patients, and is a common infectious complication of chronic granulomatous disease.
Four types of IA are recognized. These are:
1. acute or chronic pulmonary aspergillosis (the most common form of the
disease;
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
50
THE MENACING FUNGI
2. tracheobronchitis and obstructive bronchial disease with pseudomembrane
formation and various degrees of invasion the mucosa and cartilage (this form
seen predominantly in AIDS patients);
3. acute invasive rhinosinusitis;
4. disseminated disease (commonly involves the brain, skin, kidneys, heart, and
eyes, and occurs in 10 to 40 percent of bone marrow transplantation (BMT)
patients).
Predisposing Factors. Patients at greatest risk for developing IA include:
1. recipients receiving bone marrow transplants from genetically unrelated individuals
(allogenic BMT), who have a prolonged neutropenia or are under corticosteroid
treatment for graft versus host (GVH) reaction or disease;
2. recipients of BMT from their own bone marrow (autologous BMT) or recipients of
solid-organ transplants and who have been neutropenic for more than 2 weeks;
3. patients with acute leukemia and lymphomas undergoing intense chemotherapy;
4. patients with prolonged neutropenia and aplastic anemias that were not
chemotherapeutically caused;
5. patients with previously documented aspergillosis and subjected to a new
chemotherpeutic regimen or a BMT;
6. patients with neutrophil deficits as seen in cases of chronic granulomatous disease;
7. patients with advanced human immunodeficiency virus (HIV) disease.
Gastrointestinal Involvement. Both inflammation of the mouth and invasive aspergillosis are
common problems during radiation therapy and cytotoxic chemotherapy for hematological
malignancies such as acute leukemia. Certain studies have demonstrated that the gastrointestinal
(GI) tract (including the oral cavity) can be a common target for invasive aspergillosis. It
remains unknown whether invasive gastrointestinal aspergillosis is primary or secondary in
origin. Aspergillus species may invade through the GI tract after disruption of the intestinal
mucosal barrier caused by chemotherapy, or they may spread from the lungs by means of the
circulatory system. Early diagnosis of GI aspergillosis and prompt initiation of appropriate
therapy pose problems if invasive gastrointestinal aspergillosis is not considered as a possible
complication of patients undergoing cytotoxic therapy for hematological malignancies.
Liver Transplant Recipients. IA has been a long time, major problem in liver transplant
recipients. Virtually all liver transplant patients with IA have evidence of significant hepatic
and/or renal dysfunction. Studies also have shown that recipients of a liver retransplantation
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
51
THE MENACING FUNGI
have a risk for IA that is 30-fold higher than that of other patients.
A study reported by N. Singh and associates in 2003, demonstrated that the risk profile and the
epidemiology of IA in liver transplant recipients has changed. The disease seen in the current
era occurs later, is less likely to be associated with central nervous system infection, and has a
lower mortality rate when compared with IA seen in the early 1990’s.
Signs and Symptoms. Clinical signs and symptoms are usually too nonspecific to be helpful in
diagnosing IA. As with other forms of aspergillosis, patients primarily experience chest pain,
cough, fever, general discomfort, difficulty in breathing, and weight loss. A positive CT scan
may be the first definitive suggestion of IA.
Diagnosis. The diagnosis of IA generally involves at least lines of evidence of infection. These
are: a positive computerized axial tomogram (CAT scan), a positive culture and/or microscopic
demonstration of Aspergillus fumigatus, and detection of Aspergillus antigens in a patient’s
serum. In early stages of IA, CT scans may reveal specific signs of infection such as the typical
“halo” resulting from hemorrhagic necrosis surrounding a fungal lesion or pleura-based lesions.
CT scanning can be used in conjunction with brain magnetic resonance imaging with cerebral
aspergillosis patients.
Other Aspergilloses Caused by A. fumigatus
Table 9 summarizes other examples the most common clinical manifestations caused by A.
fumigatus. Note that in this table, the approaches to diagnosis are provided in the form of
footnotes for the respective manifestations since these conditions are quite specific.
Table 9. Aspergillus fumigatus Clinical Manifestations
Clinical Manifestation
Distinguishing Features
allergic bronchopulmonary
(ABPA)
most severe allergic pulmonary complication aspergillosis
caused by Aspergillus species; occurs in patients with
chronic lung disease, especially asthma, chronic obstructive
pulmonary disease, or cystic fibrosis; follows the same
course as classic asthma, with a unique cellular immune
response and pathophysiologic findings caused by
responses to products of T-lymphocytes; effects range
from asthma to lethal destruction of the lungs.
Signs and Symptoms: manifests itself as a bronchial
asthma with temporary pulmonary infiltrates that may
proceed to proximal bronchiectasis and lung fibrosis;
central bronchiectasis generally is detected in the late
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
52
THE MENACING FUNGI
stages of the disease; patients exhibit remittent low-grade
fever, weight loss, difficulty in breathing, coughing, and the
production of a foul smelling sputum in the morning or
when changing position.
In untreated patients, ABPA eventually progresses to
pulmonary fibrosis and respiratory failure.
ABPA presents diagnostic difficulties, which have led to
the concept of “silent” ABPA. Some cystic fibrosis
patients in whom the classic diagnostic criteria have not
been met, for example, experience damage to their
respiratory mucosa in response to exposure to Aspergillus
conidia. a
aspergilloma
in the early 1950’s, aspergilloma was the classical form of
aspergillosis; occurs in preexisting pulmonary cavities
caused by tuberculosis, sarcoidosis, conditions
characterized by deep-seated vesicles, and chronically
blocked paranasal sinuses.
aspergilloma, also referred to as “fungus ball,” consists of a
sphere-shaped mass of fungal hyphae embedded in a
proteinaceous substance with conidia-forming structures at
its edges; aspergillomas are found external to the cavity
lining; on chest radiographs an aspergilloma appears as a
spherical mass surrounded by a radiolucent crescent.
Signs and Symptoms: patients are usually asymptomatic;
marked pleural thickening typically occurs; a common sign
of aspergilloma is the spitting of blood coming from the
bronchi or lungs (such hemoptysis results from the
disruption of blood vessels in the wall of the cavity
occupied by aspergilli, or in the bronchial artery supply
centimeters away from the aspergilloma). b
a
ABPA is a difficult condition to diagnose. The classic criteria listed for a definitive diagnosis
include asthma, a history of pulmonary infiltrates, central bronchiectasis, immediate skin
reaction within 10 to 20 minutes following the application of A. fumigatus antigenic extracts.
b
Aspergillomas are most often found on chest radiographs obtained for the evaluation of
another pulmonary or allergic disease. Computed tomography (CT) scans of the chest are of
great value in diagnosis. In addition, a significant increase in anti-Aspergillus fumigatus
antibody occurs as patients recover.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
53
THE MENACING FUNGI
Laboratory diagnosis includes the isolation of A. fumigatus and the finding of large numbers of
eosinophils in the peripheral blood and Charcot-Leyden crystals in brown plugs from sputum
specimens and related secretions. Elevated levels of immunoglobulin E (IgE) to A. fumigatus in
serum and immediate skin reactivity (within 15 +/- minutes) after the application of A. fumigatus
antigenic extracts also are important to the diagnosis of the disease
Major Syndromes Found with AIDS Patients
Two major Aspergillus species-syndromes can be found with patients with AIDS. These are
respiratory tract disease (either semi-invasive pseudomembranous tracheitis or invasive
pneumonitis) and central nervous system (CNS) infection presenting as a febrile diffuse
meningoencephalitis. Vascular infarction is a central feature of the CNS infection. The signs
and symptoms of the respiratory tract disease states are given in Table 10.
Table 10. Major Syndromes Found with AIDS Patients
Syndrome
semi-invasive
pseudomembranous tracheitis
invasive pneumonitis
Signs and Symptoms
cough, dyspnea, fever, stridor or wheezing caused by
airway constriction culminating in airway obstruction if
untreated; endoscopic examination show a confluent,
exudative pseudomembrane sticking to the tracheal wall
chest pain, cough, fever, hemoptysis, and hypoxemia;
radiographs show either a diffuse interstitial pneumonitis or
a localized wedge-shaped dense infiltrate representing a
pulmonary infarction.
General Aspects of Laboratory Diagnosis
Establishing a laboratory diagnosis of invasive infection due to Aspergillus species can pose
difficulties. Convincing evidence includes the isolation and growth of Aspergillus species from
specimens obtained from normal sterile sites or histopathological findings showing the presence
of fungal elements invading tissue. Such elements would include typical branching hyphae and
spores (Figure 18). Specimens of value for the isolation of aspergilli include bronchoalveolar
lavage fluid (BAL), sputum, and nasal swabs. Bronchoscopy may also provide a suitable
specimen for culture. The specimens-of-choice are BAL samples, percutaneous lung biopsy, or
aspirated specimens obtained with radiological or ultrasound guidance.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
54
THE MENACING FUNGI
Figure 18. The microscopic features of a histopathologic examination of tissue taken from an
individual with invasive aspergillosis. The branching hyphae and spores typical of aspergilli are
shown in this stained preparation.
Pathogenic aspergilli generally grow easily and relatively rapidly on routine media preparations
used for fungal isolations. Typical mycelia only pathogens are capable of growing at 35 to 37 o
C. In addition, A. fumigatus has the unique property of being able to grow and reproduce at
temperatures of 50o C or higher.
Serological testing for the detection of circulating Aspergillus antigens or antibodies can be very
helpful in the diagnosis of aspergilloma or ABPA, the aspergilloses observed in
immunocompetent individuals. Of the more than 20 diagnostic procedures, the techniques that
appear to be the most reliable to detect anti-Aspergillus antibodies are double immunodiffusion
and counterimmunoelectrophoresis. Radioimmunoassays and enzyme-linked immunosorbent
assays (ELISAs) are used for the detection of circulating Aspergillus antigens.
In the case of immunosuppressed individuals, an increase in the concentration (titer) of antiAspergillus antibody at the end of immunosuppression indicates recovery from IA, whereas an
absence of antibody or declining antibody titers is suggestive of a poor prognosis. The detection
of circulating antibodies to Aspergillus, thus has prognostic and not diagnostic value in
immunosuppressed patients.
The serological diagnosis of IA is based on the detection of circulating Aspergillus antigens, not
anti-Aspergillus antibodies, in biological fluids such as serum, urine and BAL specimens.
Treatment
Until recently, there were only two antimycotic agents with activity against Aspergillus species,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
55
THE MENACING FUNGI
amphotericin B deoxycholate (AmB-d) and itraconazole. Despite advances in newer antifungal
agents, AmB-d remains the treatment of choice for invasive aspergillosis. The effective use of
this antimycotic may be complicated or limited by potential adverse effects such as renal
impairment.
The therapeutic options available to treat IA are limited to a small number of antifungal
compounds. Since approximately the early 1980’s, deoxycholate amphotericin B has been used
as the standard antifungal agent for the treatment of IA in severely immunocompromised
patients. This has been largely because of the drug’s long historical record and the absence of
suitable parenteral antifungal alternatives. The usefulness of amphotericn B, depending on the
patient involved, can range from 10 to 40 percent largely because its toxicity. Newer antifungal
agents such as the triazoles, itraconazole and voriconazole, are used for IA treatment. However,
the effectiveness of these agents may be hampered by drug-related liver toxicity and hazardous
drug interactions in patients.
More recently, the use of caspfungin, an echinocandin, has been found to be well tolerated by IA
patients who were refractory to standard therapy. In addition, the antifungal agent’s-toxicity
level was minimal.
Prevention and Control
Rapid diagnosis and appropriate therapy are essential to the prevention and control of the various
forms of aspergilloses. Quarantine measures are not indicated. In addition, there are no
vaccines.
In cases of allergic diseases, such as asthma, allergic sinusitis, and alveolitis approaches to
prevention include, ordinary cleaning procedures directed at removal of fungal conidia, and if
possible, removing the allergic individual from the environmental sources of the fungi. In health
care facilities, the use of high efficiency particulate air (HEPA) filters, are effective in removing
conidia and related fungal components. Inspection of filter systems on a regular basis and
replacement of defective filters is essential to preventing and decreasing the incidence of
invasive aspergillosis and other of the aspergilloses in immunosuppressed patients. Ordinary
cleaning procedures also are important in prevention and control.
CANDIDIASIS AND CANDIDA SPECIES
C
andidiasis is an acute or chronic, superficial or disseminated mycosis, caused by various
Candida species. C. albicans is the most common species associated with disease. The
clinical manifestations of this group of fungal pathogens are extremely are extremely
diverse. In recent years Candida species have come to be recognized as the most common cause
of fungal infections among HIV-infected children.
Pathogenic Candida Species
Several Candida species have been identified on the basis of a combination of biochemical and
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
56
THE MENACING FUNGI
structural properties. The species commonly associated with human disease include the
following:
1. C. albicans
2. C. dubliniensis
3. C. glabrata
4. C. guilliermondii
5. C. krusei
6. C. parapsilosis
7. C. tropicalis
Habitat
Candida albicans is a common member of the microbial populations in different sites of the
human body. The human is the reservoir of the yeast. C. albicans occurs worldwide and is
usually normally found in small numbers on the mucous membranes of the oral cavity, lower
intestinal tract, and female genital tract. This colonization is aided by the ability of the yeast o
attach to mucosal cells, a property that distinguishes it from other Candida species. Changes in
host immunity such as significant reduction in or depletion of the CD4+ lymphocytes in patients
with AIDS result in disease at these sites.
Invasive disease can occur as a result of neutropenia after cancer immunotherapy or in
individuals who have undergone a transplantation procedure.
Transmission
Most C. albicans infections are caused by the yeast normally found in the body’s microbial
(endogenous) population. This is the case with most nosocomial infections as well. Infections
also can occur as a result of direct contact with lesions in other individuals such as through
unprotected sexual intercourse, and in situations involving invasive surgical procedures.
Neonatal infections may also result from passage through an infected birth canal, or exposure to
infectious vaginal secretions shortly after birth.
Risk Factors . In order for Candida species to act as pathogens, interruption of normal host
defenses is necessary. General risk factors for Candida infections include diabetes mellitus,
immunocompromised states including HIV-infection, immunosuppression, and iatrogenic factors
such as antibiotic use, indwelling devices (pacemakers, and urinary or vascular catheters),
surgery, intravenous drug use, and hyperalimentation fluids.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
57
THE MENACING FUNGI
Medical Devices and Biofilms . The combination of an increasing aging population and
consistently growing number of inserted medically-related devices is quite likely to escalate the
occurrence of infectious complications related to medical devices. At least half of all cases of
nosocomial infections are associated with such devices. The medical consequences of devicerelated infections can be disastrous, and include potentially life-threatening systemic infections
and device malfunction that may require its removal. The removal of medical devices is often
complicated by tissue destruction. An increasing proportion of device-related infections,
particularly those involving the bloodstream and urinary tract, are caused by Candida species.
A significant proportion of human infections involve microbial biofilms. Such biofilms develop
when microorganisms adhere (stick) to a surface and produce extracellular multiple units
(polymers) of carbohydrates, or proteins, that provide a matrix (basic structural surrounding
substance) and aid in further attachments. Microorganisms in biofilms behave differently from
freely suspended microbes and have been shown to be relatively refractory to medical therapy.
Both bacteria and Candida species within biofilms are markedly resistant to antimicrobial agents
Thus, biofilm associated infections of retained medical devices may recur after cessation of
antibiotic therapy and may require device removal. Candida species are emerging as important
nosocomial pathogens, and an implanted device with a detectable Candida-biofilm is frequently
associated with infection.
Candida albicans biofilm formation has the following 3 developmental phases:
1. early phase - yeast cell adheres to device surface,
2. intermediate phase - matrix formation with yeast cells changing to hyphal forms,
3. maturation phase - substantial increase in matrix material.
Fully formed (mature) Candida biofilms contain a mixture of yeast cell, hyphae, and
pseudohyphae in a matrix consisting of carbohydrate, protein, and unknown components. The
formation of such biofilms is influenced by the chemical make-up of the contact surface,
environmental factors, the development of Candida phases, and the Candida species involved.
Culture and Microscopic Properties
Candida albicans grows in either of two basic forms, yeast and hyphal. The yeast form with
buds is seen under most conditions (Figure 19.) The hyphal forms begin with what appears to be
elongated blastospores extending out many times the diameter of the original cell. Such
situations may result in the formation of several cells being connected into what is called
pseudohyphae.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
58
THE MENACING FUNGI
Figure 19. A scanning micrograph showing the yeast form with smaller buds connected to
several of them.
Most Candida species grow rapidly on enriched laboratory media and appear a smooth, white to
cream colored colonies measuring 2 to 4 millimeters in diameter. These growths resemble
bacterial colonies rather than the typical mold mycelia. On special media C. albicans forms
sproutlike distinctive hyphae know as germ tubes. This yeast also forms thick-walled spores
called chlamydoconidia, which distinguishes it from other Candida species. Figure 20 shows a
microscopic view of characteristic C. albicans chlamydospores and clusters of blastospores.
Figure 20. A microscopic view of the large spherical C. albicans chlamydospores and the
smaller blastospores appearing in clusters.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
59
THE MENACING FUNGI
Disease States
As indicated earlier, Candida infections are quite numerous and variable. Table 11 lists the most
commonly encountered forms together with their clinical signs and symptoms.
Table 11. Candida Clinical Manifestations
Clinical Manifestation
Distinguishing Features
bronchocandidiasis
chronic bronchitis.
Signs and Symptoms: cough, varying amounts of
sputum, medium and coarse rales at the lung bases;
roentgenologic appearance of peribronchial thickening,
hazy linear fibrosis.
candidids
represents local skin reaction to circulating Candida
antigens.
Signs and Symptoms: red area with little blisters; usually
appear in areas distant from infected skin sites; itching is
quite common.
endocarditis
condition resembles bacterial endocarditis; it differs
mainly in the greater presence of large vegetations
(growths) on heart valves, and emboli associated with
major blood vessels such as the splenic, renal, and iliac
arteries.
Signs and Symptoms: anemia; congestive heart failure,
fever, heart murmur, and enlarged spleen.
esophageal candidiasis
typical signs and symptoms may be absent; found with low
CD4 + counts;
Signs and Symptoms: inability or difficulty to swallow;
pain on swallowing; retrosternal pain; dehydration; weight
loss (especially in children); the presence of oropharyngeal
candidiasis may or may not be present;
Children, unlike adults might experience nausea and
vomiting.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
60
THE MENACING FUNGI
fungemia (septicemia)
mainly results as a rapidly fatal conclusion to some
underlying condition such as immunosuppression, and
malignancies.
Signs and Symptoms: fever impaired renal function,
leukopenia.
generalized cutaneous candidiasis
condition seen most often in individuals with diabetes,
some form of immunosuppression such as HIV-infection
or AIDS, or with congenital skin defects, and during
pregnancy.
Predisposing Factors : diabetes, obesity, alcoholism,
immunosuppression, and continual and routine immersion
of hands in water or other irritating substances associated
with certain occupations.
Signs and Symptoms: skin lesions are red, scaling, moist
or weeping and exhibit sharp borders and may occur in
body areas such as the armpits, groin, gluteal folds, mouth,
nails, perineum, and between fingers; central areas of such
lesions may have blisters, and pus-containing centers;
This clinical manifestation usually is associated with oral
lesions, infections involving various structures of the
mouth, and heavy intestinal colonization resulting in
gastrointestinal discomfort.
intertriginous candidiasis
this condition is quite similar in most respects to the
features listed for generalized cutaneous candidiasis
condition seen most often in individuals with diabetes,
some form of immunosuppression such as HIV-infection or
AIDS, or with congenital skin defects, and during
pregnancy.
Predisposing Factors : diabetes, obesity, alcoholism,
immunosuppression, and continual and routine immersion
of hands in water or other irritating substances associated
with certain occupations.
Signs and Symptoms: skin lesions are red, scaling, moist
or weeping, painful, itching, and exhibit sharp borders and
may occur in body areas containing skin folds
(intertriginous) such as the armpits, groin, gluteal folds,
mouth, nails, perineum, and between fingers, central areas
of such lesions may have blisters, and pus-containing
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
61
THE MENACING FUNGI
of such lesions may have blisters, and pus-containing
centers;
meningitis
serious condition that may result in significant morbidity
and mortality if not detected and treated effectively;
Predisposing factors: previous antibiotic or corticosteroid
therapy, malignant disease, immunosuppressed states; in
adults postoperative complications of neurosurgery, result
of disseminated disease, or immunosuppession.
Signs and Symptoms: contracted pupils, convulsions,
delirium, fever, intense headache, lethargy, loss of appetite,
nausea and vomiting, sensitivity to light and/or sound,
onychia and paronychia
a localized form of Candida infection involving the nails
and/or nail bed; condition is an inflammation of the
subcutaneous tissues at the base of finger or toenails
(onychia), or the marginal structures around the nail
(paronychia).
Predisposing factors : malignant disease,
immunosuppressed states, or occupational exposure to
excessive moisture and/or chemicals causing injury to
nails; in adults postoperative complications of
neurosurgery, result of disseminated disease, or
immunosuppession.
Signs and Symptoms: prominent swelling redness, and
pain extending as far back as 1 centimeter from the edge of
the nail; very little pus formation unless there is a mixed
infection with bacteria; nails may become brown, exhibit
lines, or brittle.
oral candidiasis (thrush)
condition seen most often in individuals with a riboflavin
deficiency, diabetes, some form of immunosuppression
such as HIV-infection or AIDS, and during pregnancy;
condition is also seen among infants and results from
passage through an infected birth canal; occasional
epidemic of oral thrush can also occur in nurseries; the
elderly also experience oral thrush largely because of the
presence of a debilitating disease.
Signs and Symptoms: discrete or confluent patches of a
cream-white to gray pseudomembrane cover various parts
of the oral cavity including the tongue, soft palate, and
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
62
THE MENACING FUNGI
of the oral cavity including the tongue, soft palate, and
gums; removal of patches may cause bleeding; membrane
may extend and penetrate deeply into tissues to be painful
and to interfere with swallowing; in severe cases with
infants interference with breathing may occur; enlargement
of projections of the tongue (papillae) can result in a
condition known as “black hairy tongue”;
Oral candidiasis often extends to the corners of the mouth
which results in painful, bleeding slits or deep lesions.
oropharyngeal esophagitis
very common among HIV-infected children;
Signs and Symptoms: the presence of a creamy white
curd-like (cottage cheese consistency) patches with
inflamed underlying mucosal on the palate, tonsils, and
oropharyngeal mucosa; raised white plaques on the lower
tongue surface, palate, and mucosal surfaces; red crack-like
sores in the corner of the mouth.
pulmonary candidiasis
Candida albicans and other species can cause disease at
various levels of the respiratory tract, can easily colonize
mucosal surfaces damaged by other microbial pathogens.
Signs and Symptoms: cough with mucoid and sometimes
blood-streaked sputum, effusion, low grade fever, medium
moist rales, pleurisy; altered breath sound develop with
severe confluent lesions, bronchopneumonic lesions may
extend yo result in lobar pneumonia.
vulvovaginal candidiasis
(vaginal thrush)
condition seen most often in women with diabetes, some
form of immunosuppression such as HIV-infection or
AIDS, and during pregnancy.
Signs and Symptoms: vaginal itching, burning sensation
on urination, presence of a cottage cheese-like discharge,
abscesses and kidney involvement may also occur in
untreated cases.
Individuals At Risk
Candidiasis occurs in a variety of conditions including persons with AIDS, patients in an ICU
after general surgery, patients immunosuppressed resulting from chemotherapy and related
procedures, and in patients with liver diseases. Factors such as the administration of
supraphysiologic doses of adrenal corticosteroids, the use of indwelling intravenous catheters,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
63
THE MENACING FUNGI
and low birth weight in neonates are known to predispose individuals to deep candidiasis.
Of particular concern is candidiasis occurring among HIV-infected children. It is the most
common fungal infection found this group of individuals. Oral thrush and diaper dermatitis
ranges from 50 to 85 percent among HIV-infected children. In the United States, Candida
albicans-caused esophagitis is reported as the AIDS-defining condition in adults and in about 12
to 16 percent of children less than 13 years of age. This condition continues to be seen in the
post-HAART (highly active antiretroviral therapy) era among children not responding to therapy.
While disseminated candidiasis (candidemia) is infrequent among HIV-infected children,
Candida species can spread from the esophagus particularly when coinfections with herpes
simplex virus or cytomegalovirus are present. Infection can also develop from chronically
indwelling central venous catheters used for total parental nutrition or intravenous antibiotics.
Approximately 50 percent of reported cases are caused by non-C. albicans species including C.
dubliniensis, C. glabrata, C. krusei, C. parapsilosis, C. pseudotropicalis, and C. tropicalis.
Treatment
Eliminating possible underlying causes of candidiasis such as the removal of indwelling venous
catheters, and diabetes control often facilitates cure. C. albicans is usually susceptible to
amphotericin B, nystatin, flucytosine, and an azole such as clotrimazole, fluconazole, or
ketoconazole. Table 12 lists several examples of the drugs used to treat various form of
candidiasis.
Table 12. Examples of Drugs Used to Treat Candidiasis
Infection or Disease State
Treatment
oral and esophageal candidiasis
fluconazole
oral thrush
nystatin suspension, itraconazole suspension,
fluconazole
vaginal thrush
oral fluconazole, or topical butoconazole,
clotrimazole, micoazole, nystatin,terconazole
visceral/invasive candidiasis
amphotericin B with or without 5-flurocytosine
Diagnosis
Diagnosis of candidiasis requires evaluation of both clinical and laboratory findings. The most
valuable laboratory evidence of infection is the microscopic demonstration of Candida yeast
cells and/or pseudohyphae in infected tissue or body fluid specimens. Specimens usually are
suspended in potassium hydroxide to reveal the yeast cells. Laboratory confirmation with
positive cultures finding also is important. A direct aspirate, biopsy, or bronchoalveolar lavage
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
64
THE MENACING FUNGI
(BAL) is often required to establish diagnosis of deep organ involvement. The finding in severe
or recurrent oropharyngeal infection in an adult patient with no obvious underlying cause should
suggest the possibility of HIV infection.
The presence of systemic Candida infection requires the culturing of blood specimens. In such
cases several other diagnostic approaches might be appropriate. The include the following:
1. retinal examination for endophthalmitis,
2. abdominal computerized tomography or ultrasound for hepatic or renal involvement,
3. bone scans for osteomyelitis.
Prevention and Control
Early detection and appropriate treatment of any infection involving the oral cavity, esophagus,
or urinary bladder, especially in persons with the risk factors indicated earlier is extremely
important to prevent possible systemic spread of candidiasis. In addition, secretions and
contaminated articles should be disinfected.
In cases of vaginal infection, additional steps can be taken. These include avoiding the wearing
of tight undergarments and jeans, and the use of deodorant tampons and feminine hygiene
products if the signs and symptoms of an infection are apparent. Since Candida grows and
reproduces well in warm, moist environments, the genital area should be kept dry.
CRYPTOCOCCOSIS
C
ryptococcus neoformans is the infectious causative yeast of the disease known as
cryptococcosis. Formerly a rare disease, the incidence of cryptococcosis has increased in
recent years because of its frequent occurrence in persons with AIDS. Cryptococcosis is
the fourth most common opportunistic infection in AIDS patients after Pneumocystis carinii
pneumonia, and cytomegalovirus and Mycobacterium avium complex infections. This yeast
infection is classified as an AIDS-indicator opportunistic disease.
Two varieties of C. neoformans are recognized. These are C. neoformans variety (var.)
neoformans and C. neoformans var. gattii. The two varieties exhibit a difference in geographical
distribution with C. neoformans var. neoformans being found worldwide, and C. neoformans
occurs mainly in tropical and temperate climates. Attention will be limited to C. neoformans var.
neoformans since infections caused by this yeast are far more frequent.
Habitat
C. neoformans (cryptococcus) is found in soil contaminated with pigeon or the droppings of
other birds such as sparrows and starlings. The yeast also has been recovered from the dried
excreta of chickens, the beaks and feet of pigeons, and from bat droppings. Cryptococcus does
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
65
THE MENACING FUNGI
not cause disease in pigeons or other bird species, presumably because the body temperature of
these animals is too high for the growth and reproduction of the yeast. Bats also can be infected
with C. neoformans. This yeast gains a competitive advantage over other microbes by being able
to grow and multiply exceedingly well in a dried bird droppings accumulated in places that are
not in direct sunlight.
Microscopic and Culture Properties
Cryptococcus neoformans is a spherical yeast which reproduces by budding at any point on the
surface. Sometimes several buds are formed simultaneously (Figure 21).
Figure 21. A microscopic view of Cryptococcus neoformans and its buds suspended in an India
ink preparation.
Individual cells measure approximately 4 to 6 micrometers in diameter and characteristically can
form an outer structure known as a capsule (Figure 22). The capsule, which is unique among
pathogenic fungi, contributes to the disease producing capability of the pathogen by interfering
with host immune processes such as phagocytosis.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
66
THE MENACING FUNGI
Figure 22. A microscopic view of an India ink preparation of Cryptococcus with a bud and
surrounded by an outer capsule. The capsule appears as a halo surrounding this yeast and its
bud.
Transmission
The mode of transmission for C. neoformans is through inhalation of the pathogen.
Cryptococcosis is not contagious.
Pathogenesis
Cryptococcal infection is believed to start with the inhalation of C. neoformans from an
environmental source, followed by pulmonary infection or disease. In most individuals the signs
and symptoms are minimal. Occasionally the infectious process progresses in the lungs and is
spread via the circulatory system to the central nervous system and other areas of the body.
Initial interactions with immune system cells such as alveolar macrophages are crucial in the
outcome of cryptococcal infections. Nonencapsulated C. neoformans are generally engulfed and
destroyed by polymorphonuclear leukocytes. However, encapsulated forms of the pathogen
(Figure 21) are capable of escaping from the clutches of such host cells. Specific antibody
enhances phagocytosis and the killing of the cryptococci.
The polysaccharide capsule of cryptococci also can interfere with other host immune
mechanisms. The circumstances are identical to those occurring with encapsulated
pneumococcus. Tissue reactions to the pathogen vary from none to pus formation and tumor
formation.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
67
THE MENACING FUNGI
Risk Factors
Before 1946, only 200 or so cases of cryptococcosis had been reported in the medical literature.
By 1955, many more cases had been reported and repeated isolation from environmental sources
also had been described. Cryptococcosis generally remains localized in immunocompetent
individuals and resolves. The disease is relatively rare among immunocompetent person.
However, the infection is one of the most frequent fungal infections occurring in persons with
AIDS. In such cases, the pathogen is known to readily spread from the lungs to the central
nervous system. Individual experiencing other conditions that impair their immunity also are
susceptible to C. neoformans infection. Examples of such conditions include alcoholism,
chronic corticosteroid therapy, Cushing’s syndrome, malignancies of various types, neutropenia
after cancer immunotherapy, sarcoidosis, and tissue transplantation procedures.
Clinical States
In most situations cryptococcus infection begins as a pulmonary disease with hematogenous
spread to the skin, bones, abdominal viscera, and especially to the central nervous system. A
temporary pulmonary lesion does develop which either heals by the body enclosing it in a sheath
or capsule (encapsulation) leaving a cryptococcoma, or heals without leaving any residual scar.
Table 13 lists the most commonly encountered forms of cryptococcal clinical infections together
with their signs and symptoms.
Table 13. Cryptococcus Clinical Manifestations
Clinical Manifestation
Distinguishing Features
benign pulmonary cryptococcosis
represents mild or minimal exposure; may be manifested
only an accidental autopsy finding of an encapsulated,
healed subpleural tumor; with active lesions, masses of
pathogen penetrate the bronchus wall, displace host tissue,
and large numbers of Cryptococcus are discharged into
sputum; pulmonary lesions do not calcify upon healing, and
most heal without leaving residual evidence of infection.
Signs and Symptoms: cough, scanty mucoid or bloodtinged sputum; low grade fever, malaise, and weight loss
may occur in some cases; bronchitis, consolidation,
dullness to percussion, rales or pleural effusion may also be
present.
cutaneous cryptococcosis
may be a site or sites of primary inoculation with pathogen;
may accompany a systemic infection and probably is
preceded by a respiratory infection;
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
68
THE MENACING FUNGI
Signs and Symptoms: lesions may take the form of
papules (small, elevated, hard red areas on the skin) pusfilled blisters, or subcutaneous abscesses which form
ulcers.
Mucosal lesions may also develop as a result of
hematogenous spread or by extension of skin lesions; may
be in the form of small lumps, or superficial ulcers on any
oral or nasal mucosal surfaces.
meningitis
most commonly recognized form of cryptococcal disease;
the usual course is fairly rapid and marked by progressive
deterioration of the individual; the infection is more rapid
in AIDS patients.
Signs and Symptoms: insidious onset with relatively
nonspecific finding until late in the course of the infection;
dizziness; intermittent headache; irritability; difficulty in
performing complex cerebral functions gradually appear
over weeks or months with no consistent pattern; fever
usually present.
Later in clinical course of the disease: seizures, cranial
nerve signs, edema and inflammation of the optic nerve,
dementia, and decreased levels of consciousness.
osseous cryptococcosis
occurs in about 10 percent of reported cases of
crytococcosis lesions spread slowly, destructive to bone
spread to the skin by extension or tissue, and often
following some type of surgical exploration.
Signs and Symptoms: frequently associated with bone
pain and swelling occur for several months.
visceral cryptococcosis
may resemble tuberculosis; lesions also are suggestive of a
malignancy.
Signs and Symptoms: swelling and inflammation of the
optic nerve; inflammation also involving the retina, and
cornea.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
69
THE MENACING FUNGI
Treatment
Amphotericin B either alone or in combination with 5-fluorocytosine is effective in many
situations of systemic disease. Cryptococcus infections present problems in AIDS patients. In
such cases fluconazole is beneficial after an initial course of Amphotericin B and is continued
indefinitely.
Unfortunately, one-half of cured individual experience some type of neurologic damage
Diagnosis
In all cases of diagnosis, it is important to note that the number of cryptococci is quite small.
Demonstrating the pathogen in clinical specimens such as spinal fluid, is diagnostic. The use of
India ink for material microscopically examined is standard (Figures 20 and 21).
Culture also is effective. However, a large amount of specimen is usually necessary. Other
approaches to diagnosis include detection of capsular material by procedures such as enzyme
immunoassays.
Prevention and Control
The chemical disinfection of accumulated pigeon droppings followed by their appropriate
removal and disposal is recommended as a preventative and control measure. The droppings
should be adequately wetted by a chemical agent such as iodophor to prevent aerosolization of
any pathogens present.
Any body fluids, surgical dressings and/or other types contaminated articles should be
disinfected as well.
PENICILLIOSIS
P
enicilliosis is a systemic and progressive infection caused by Penicillium marneffei.
Infections with this pathogenic fungus are becoming increasing common in Southeast
Asia, and is now recognized as one of the most frequently encountered opportunistic
infections among person with AIDS. However, cases of infection have also been reported in
immunocompetent individuals.
Geographic Distribution and Habitat
The first natural case of human penicilliosis was reported in 1973, in a 61-year old male U.S.
citizen who had traveled to Southeast Asia. This person had Hodgkin’s disease, and was
diagnosed with P. marneffei infection on being found to have a splenic abscess. A second case
was found approximately 10 years later in a U.S. male who had traveled throughout Southeast
Asia. Between 1988 and 1994, 14 AIDS-associated penicilliosis cases were reported among
HIV-infected persons returning to their respective native countries after visits to Southeast Asia.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
70
THE MENACING FUNGI
From the gathered epidemiological data, P. marneffei infections are most common in northern
Thailand, and the southern part of the People’s Republic of China (Guang Xi Province). The
pathogen in all probably resides in soil where it reproduces.
Culture and Microscopic Features
P. marneffi is a dimorphic fungus. When grown on appropriate laboratory media at room
temperature the mold produces a distinctive red pigment, which diffuses into the medium.
Transmission
Humans acquire penicilliosis by inhaling the spores of the mold.
Clinical States
The incubation period of disseminated P. marneffei infection is variable. In some cases
symptomatic disease appears within a few weeks after exposure. In others, victims are reported
to have long periods without any signs or symptoms.
Signs and Symptoms. The most common clinical features include anemia, fever,
lymphadenopathy, enlarged liver and spleen, nonproductive cough, and marked weight loss.
About 60 to 70 percent of patients exhibit a large number of papular skin lesions (solid, red
elevated areas), which may become centrally necrotic. Chest radiographs may show infiltrates or
cavitary lesions.
Treatment
Amphotericin B is the drug-of-choice for severe cases. The usual dosage administered is 1
milligram (mg)/kilogram of body weight daily for 2 weeks, after which itraconzaole (200 to 400
mg daily) or ketoconazole (400 mg) should be given for 6 weeks.
An azole drug can be used for treatment of milder infections. Fluconazole, while being less
effective than itraconazole, can be useful with patients who fail to absorb itraconazole.
Laboratory and Related Aspects of Diagnosis
Diagnosis can be made by direct microscopic examination of stained clinical specimens such as,
skin, bone marrow, lymph nodes, and other infected sites, or culture material. The pathogen
typically exhibits round or oval cells with prominent cross walls.
The culture of specimens is critical to diagnosis since other system infections such as
cryptococcosis and histoplasmosis have similar clinical manifestations.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
71
THE MENACING FUNGI
Prevention and Control
Avoiding environmental sources of P. marneffi is difficult. The highest number of cases appear
to occur during the rainy season from May to October.
Immunocompromised individuals should be advised about the risk of acquiring penicillinosis
when traveling to areas of Southeast Asia and the southern part of the People’s Republic of
China, where P. marneffei is known to be endemic.
THE MYCOTOXICOSES
The Major Mycotoxins
F
ungal pathogens, in addition to causing infection, can also have an impact on human health
by producing harmful toxins, and/or initiating allergies. Table 14 lists representatives of
known major mycotoxins (fungal poisons) and their modes of action.
Table 14. Representative Known Major Mycotoxins and Their Actions
Mycotoxin
Main Fungus Source(s)
Examples of Food
Sources
aflatoxins a
Aspergillus flavus and
A. parasiticus and other
Aspergillus species
contaminated cereals,
figs, oil seeds, nuts,
tobacco, etc.
citrinin
ergot
alkaloids
fumonisins
Selected Properties
and Actions
four major types, B1 ,
B2 , G1 , and G2 ; associated
with immune suppression,
cancer of the liver and other
organs particularly the lungs
Penicillium citrinum,
several Penicllium,
and Aspergillus species
contaminated corn,
barley, oats, rice,
rye, and wheat
Claviceps species
contaminated cereals
two forms of disease states
usually in the form of are recognized: convulsive
bread
which affects CNS, and
gangrenous which affects
blood supply to the
extremities
Fusarium species
contaminated
corn products
yellow rice disease in
Japan; highly toxic
for nervous tissue
in humans linked to
esophageal cancer; harmful
to agricultural products, and
certain farm animals
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
72
THE MENACING FUNGI
ochratoxin
Aspergillus species
contamination of
barley, coffee, oats
rye, wheat and other
phenylalanine plant
products; may be
present in certain
wines made from
contaminated grapes
Ochratoxin A; kidney
and liver are major beans
targets; interferes with
metabolism; a problem for
certain farm animals
patulin
Penicillium patulum
and other Penicillium
species
contaminated
unfermented apple
juice
toxic to both plants and
animals
trichothecenes Several fungal species
including Fusarium,
Stachybotrys, and
Trichoderma
contaminated food
and feed products
zeralenone
a
Fusarium
graminearum
contaminated cereal
products
direct contact causes
dermatitis; ingestion causes
vomiting, and abdominal
and pulmonary bleeding
causes increased estrogen
production
Kwashiorkor, a severe malnutrition disease, may be a form of aflatoxin poisoning in children.
The Aflatoxins and Ergot Poisoning
Aflatoxins are toxic metabolic products produced by the two molds Aspergillus flavus (Figure
15), and A. parasticus. Both species are fairly common fungi found in general, and are often
found growing on various types of foodstuffs, which they are capable of decomposing and
causing decay. In doing so, some species of Aspergillus produce aflatoxins. (The first part of
the name for the mycotoxin is derived from using the A from the genus, and the fla from the
species designations, respectively.) Two structural forms of aflaoxins are known, B and G
types, of which the subtype aflatoxin B 1 is considered to be the most toxic. These mycotoxins
have been found in various foods, including stored cereals, nuts such as peanuts, and hay and
other forms of animal feed. There is also some evidence to indicate that aflatoxins were
produced by Iraqi scientists as part of a bioweapons program during the 1980’s. Most of the
toxin produced, some 2,300 liters, was used to fill warheads, with the remainder being
stockpiled. There are no indications for the deployment of the warheads.
The real and potential dangers of aflatoxin poisoning, also known as aflatoxicosis, was
dramatically shown in 1960 when, by the occurrence of large-scale trout poisoning in
commercial fish hatcheries, and concurrent outbreaks of turkey X disease in England. Both
incidents were found to be caused by aflatoxins
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
73
THE MENACING FUNGI
Although the risk to humans is unknown, there is significant evidence that aflatoxin contributes
to liver cirrhosis, liver cancer, and can have immunosuppresive, embryonic and oncogenic
effects. In parts of the world, such as India and portions of Africa, many people being treated for
malnutrition may experience aflatoxin poisoning, because of poor storage facilities for the
protein sources. Stored food items such as peanuts and cereals which often are used to correct
malnutrition, also can serve as ideal nutrients for aflatoxin-producing fungi. Exposure to
aflatoxins occurs primarily through the ingestion of contaminated foods. It should be noted that
aflatoxin poisoning does not necessarily produce immediate effects upon ingestion. These
poisons are stored in the liver, and depending on the amounts ingested may not produce disease
for a long time. Severe, acute liver injury with high morbidity and mortality has been associated
with high-dose exposures to aflatoxins. Ingestion of 2 to 6 milligrams/day of the mycotoxin for
a month can cause acute hepatitis and death.
Aflatoxins also can affect lower animals. These effects include miscarriages, stunting, and
premature deaths of farm animals.
Efforts to prevent aflatoxin poisoning include increased food inspections to detect the presence
of aspergilli and to ensure food safety, local education and assistance to keep susceptible foods
completely dry and properly stored.
Ergot poisoning is caused by the mold Claviceps purpurea which attacks grain crops.
Individuals become poisoned by ingesting rye or other cereal grains contaminated by this mold.
The toxin is known to cause hallucinogenic effects and convulsions resulting in rather bizarre
behavior similar to that described for individuals taking lysergic acid diethylamide (LSD). Ergot
can also interfere with blood flow in the arms and legs which can result in local gangrene.
The Sick-Building Syndrome
The presence of mold on the internal surfaces of damp dwellings often results in a high airborne
fungal spore count, which in turn, presents a distinct health risk to the occupants. Although these
conditions tend to be principally of a respiratory nature, a prevalence of possible toxigenic signs
and symptoms also have been reported.
Causative Agents. The spores and mycelial fragments of a number of fungal species in high
densities in buildings pose a potential health hazard from allergic reactions, and on some
occasions, from infections. The presence of fungi producing mycotoxins may also contribute to
adverse health effects called sick-building syndrome (SBS). Examples of fungal genera believed
to be associated with SBS include Aspergillus, Fusarium, Penicillium, and Stachybotrys.
Sources. The results of a number of studies involving analyses of indoor air samples, building
materials, heating, ventilation, and air conditioning (HVAC) components, suggest that these
environments and materials contribute to the fungal burden of indoor air under certain
conditions. These studies emphasize that building materials including fiberglass duct liner and
board, acrylic facing material, and painted metal vent surfaces of HVAC systems may be
colonized by various fungal species.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
74
THE MENACING FUNGI
Signs and Symptoms: Individuals living in damp, moldy housing may complain of such
conditions as backache, blocked nasal passages, breathlessness, fainting, nausea, nervousness,
and vomiting.
Toxic-mold fears have precipitated a number of lawsuits. Unfortunately, much of the evidence is
conjectural. Although the results of available studies have provided information regarding which
microorganisms are present in the indoor environment, there are significant omissions, and
sampling limitations and errors. For example, the presence of potential toxin-producing fungi
does not necessarily imply the presence of mycotoxins, nor does the finding of mycotoxins prove
that a particular fungus species is, or was present. While many fungal species can produce toxins
(Table 14), the ability to produce toxins varies under particular environmental conditions. Often
such “known” toxin producers will not make the toxic compounds. Moreover, while various
fungal species, mycotoxins, and other microbial products have been implicated as causative
agents of SBS, the range of signs and symptoms credited to these agents are greater than what
can be explained rationally in terms of toxicological mechanisms.
CONCLUDING STATEMENTS
F
ungi cause human illness in a variety of ways. Both the mycoses, which are the bestknown diseases caused by fungi, as well as the toxic metabolic products produced by some
fungal species pose important health hazards. The danger is not only applicable to humans
but, to a number of lower animals as well. The incidence of mycoses and mycotoxicoses may be
more common than suspected. The successful diagnosis and appropriate treatment of these
menacing diseases requires the coordination of the knowledge and the expertise of laboratory
technologists and of clinical health care personnel treating patients.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
75
THE MENACING FUNGI
GLOSSARY
Terms
analogue:
a compound that is structurally similar to another
antibody:
a protein molecule formed in response to, and interacting specifically with
an antigen; also known as immunoglobulin
antigen:
a substance that causes the formation of antibodies (immunoglobulins)
bronchopleural
fistula:
an abnormal tube-like passage involving the bronchi and pleura cavity
cavitation :
cavity formation
CD4 cell:
a lymphocyte component of the immune system that signals other cells of
this system to perform their respective functions; this cell type is HIV’s
target for infection
Cushing’s
syndrome:
a condition resulting from abnormal hyper-secretion of adrenal cortex
hormones
empyema:
pus in a body cavity
hemoptysis:
the spitting of blood arising from the mouth, voice box, trachea, bronchi,
or lungs
hypha:
the microscopic threadlike structural unit of molds; forms the structure of
the fungus colony or mycelium
immunoglobulin:
a glycoprotein molecule that reacts specifically with the substance and/or
cells that caused its formation; also known as antibody
mycelium:
the fungal colony
nosocomial:
refers to hospital acquired infections
PCR:
polymerase chain reaction assay; a laboratory method for measuring
circulating antigens or antibodies associated with a disease and/or foreign
agent
pyopneumthorax:
the presence of pus and gas in the pleural cavity
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
76
THE MENACING FUNGI
sarcoidosis:
a disease of unknown cause resulting in the formation to tubercle-like
lesions that may occur in any body organ
sign:
any objective evidence or manifestation of an illness or disease state
symptom:
any subjective perceptible change in the body or its functions that
indicates disease or a form or phases of diseases
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
77
THE MENACING FUNGI
SUGGESTED READING AND REFERENCES
Alangaden, G.J., et al., “Aspergillosis: the Most Common Community-Acquired Pneumonia
with Gram-Negative Bacilli As Copathogens in Stem Cell Transplant Recipients with GraftVersus-Host Disease”. Clinical Infectious Disease. 35:659-664; 2002;.
Bennett, J.W. and M. Klich. “Mycotoxins.” Clinical Microbiology Reviews. 16:497-516; 2003.
Denning, D.W., et al., “Efficacy and Safety of Viriconazole in the Treatment of Acute Invasive
Aspergillosis.” Clinical Infectious Disease. 2002; 34:563-571.
Johnson, P.C., et al., “Safety and Efficacy of Liposomal Amphotericin B Compared with
Conventional Amphotericin B for Induction Therapy of Histoplasmosis in Patients with AIDS.”
Annals of Internal Medicine. 137: 105; 2002.
Kuberski, T.T., et al., “Successful Treatment of a Critically Ill Patient with Disseminated
Coccidioidomycosis, Using Adjunctive Interferon-gamma.” Clinical Infectious Diseases. 38:
910, 2004.
Kuhn, D.M. and M.A. Ghannoum. “Indoor Mold, Toxigenic Fungi, and Stachybotrys chartarum:
Infectious Disease Perspective.” Clinical Microbiology Reviews. 16:144-172; 2003.
Masur, H. et al., “Introduction to the 1999 USPHS/IDSA Guidelines for the Protection of
Opportunistic Infections in Persons Infected with Human Immunodeficiency Virus.” Clinical
Infectious Diseases. 30: S1, 2000.
McNeil, N.M. and N.M. Ampel. “Opportunistic Coccidioidomycosis in Patients Infected with
Human Immunodeficiency Virus: Prevention Issues and Priorities.” Clinical Infectious
Diseases. 21 (Supplement 1): 111, 1995.
Mocheria, S. and L.J. Wheat. “Treatment of Histoplasmosis.” Seminars in Respiratory
Infections. 16:141; 2001.
Stoodley, P. et al., “Biofilms As Complex Differentiated Communities.” Annual Review of
Microbiology. 56; 187-209; 2002.
Tobon, A.M, et al., “Residual Pulmonary Abnormalities in Adult Patients with Chronic
Paracoccidioidomycosis: Prolonged Follow-up after Itraconazole Therapy.” Clinical Infectious
Disease. 2003; 37:898-904.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
78
THE MENACING FUNGI
POST TEST
DIRECTIONS: IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS ON THE ANSWER SHEET PROVIDED AND RETURN TO: RCECS, 16781
VAN BUREN BLVD, SUITE B, RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861.
IF YOU ELECTED ONLINE DELIVERY, COMPLETE THE TEST ONLINE – PLEASE
DO NOT MAIL OR FAX BACK.
1. Which of the following terms refers to the number of individuals within a population who
develop a specific disease during a particular time period?
a.
b.
c.
d.
e.
frequency
epidemic
sporadic condition
incidence
pandemic
2. If a particular disease suddenly affects large numbers of people in different parts of the world
would be considered as being which of the following?
a.
b.
c.
d.
e.
endemic
frequent
epidemic
pandemic
sporadic
3. The fuzzy, cottony, threadlike network of a fungus that is visible to the eye is specifically
called which of the following?
a.
b.
c.
d.
e.
mold
conidia
hypha
mycelium
yeast
4. Which of the following choices gives the term for the capacity of a fungus to exhibit both
yeast and mold phases?
a.
b.
c.
d.
e.
asexual reproduction
sexual reproduction
dimorphism
choices a and b only
none of these
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
79
THE MENACING FUNGI
5. Which of the following fungal diseases is an example of a superficial mycosis?
a.
b.
c.
d.
e.
ringworm
Candida albicans infection
histoplasmosis
sporotrichosis
coccidioidomycosis
6. Which of the following fungal diseases is an example of a subcutaneous mycosis?
a.
b.
c.
d.
e.
tinea pedis
Candida albicans infection
histoplasmosis
sporotrichosis
coccidioidomycosis
7. Which of the following choices represent the means by which humans can acquire
Blastomyces dermatitidis?
a.
b.
c.
d.
e.
ingestion of contaminated food or drink
conidia-infected fleas
tick bites
inhalation of conidia from mycelia growing in soil
infected person-to-person contact
8. Which of the following choices lists the CURRENTLY RECOGNIZED causative agents of
San Joaquin Valley fever?
a.
b.
c.
d.
e.
Candida albicans and C. immitis
Blastomyces dermatitidis and C immitis
Coccidioides immitis and C. posadasii
Paracocidioides brasiliensis and C. posadasii
Coccidioides immitis and Paracocidioides brasiliensis
9. Which of the following animals are generally NOT susceptible to C. immitis infection?
a.
b.
c.
d.
e.
cattle
dogs
birds
horses
sheep
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
80
THE MENACING FUNGI
10. Which of the following choices is NOT CORRECT in the case of coccidioidomycosis?
a.
b.
c.
d.
e.
coccidioidomycosis is not contagious
coccidioidomycosis can be spread from person-to-person
about 40 percent of cases are symptomatic
about 40 percent of cases are asymptomatic
most infected persons exhibit typical flu-like symptoms
11. C. immitis spores would generally NOT BE found in which of the following areas?
a.
b.
c.
d.
e.
San Joaquin Valley of California
Alaska
southern portions of Arizona
parts of Central America such as Guatemala, and Honduras
countries of South America including Venezuela, Columbia, Paraguay, and Argentina
12. Coccidioidomycosis generally results from which of the following?
a.
b.
c.
d.
e.
the ingestion of C. immitis spores
tick bites
earthquakes
the inhalation of C. immitis spores
fomites (contaminated inanimate objects)
13. Which of the following materials is used in skin tests to determine an exposure and/or the
sensitivity (hypersensitivity or allergy) of individuals to C. immitis?
a.
b.
c.
d.
e.
tuberculin
purified protein derivative
coccidioidin
C. immitis arthrospores
None of these
14. Which of the following conditions is the MOST FREQUENT complication of primary
coccidioidomycosis?
a.
b.
c.
d.
e.
chronic pulmonary cavitation
coccidioidoma
bronchiectasis
pulmonary fibrosis
pneumothorax
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
81
THE MENACING FUNGI
15. A negative skin test for C. immitis MAY NOT indicate which of the following conditions?
a.
b.
c.
d.
the test was performed too early in the disease process
the current illness in the patient is not the disease being tested for
previous exposure to C. immitis
a case of disseminated coccidioidomycosis in which the individuals immune response
has been impaired
e. choices a and d only
16. Which of the following types of individuals WOULD NOT be a likely victim of
histoplasmosis?
a.
b.
c.
d.
e.
spelunkers (cave explorers)
farmers
sailors
construction workers
heating and/or air conditioning service personnel
17. Histoplasmosis generally results from which of the following?
a.
b.
c.
d.
e.
the ingestion of H. capsulatum spores
tick bites
the inhalation of H. capsulatum spores
dog bites
fomites (contaminated inanimate objects)
18. Which of the following materials is used in skin tests to determine an exposure and/or the
sensitivity (hypersensitivity or allergy) of individuals to H. capsulatum?
a.
b.
c.
d.
e.
tuberculin
histoplasmin
purified protein derivative
coccidioidin
H. capsulatum macroconidia
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
82
THE MENACING FUNGI
19. When procedures for the removal of infectious soil containing bat or bird fecal matter and H.
capsulatum are impractical, which of the following choices lists a suitable approach for
effective soil decontamination?
a.
b.
c.
d.
e.
periodic water sprays applied to the involved area
covering the area with sterilized soil
allow the material to decay with time
the application of formaldehyde solutions to treat contaminated areas
either choice a or c only
20. Aflatoxins usually MAY NOT be associated with which of the following?
a.
b.
c.
d.
e.
nuts
cereals
mushrooms
animal feed
none of the above
21. Which of the following choices BEST DESCRIBES the main portal of entry and site for
Aspergillus fumigatus infections?
a.
b.
c.
d.
e.
gastrointestinal tract
kidneys
skin
respiratory tract
bones
22. Which of the following choices lists the MOST COMMON cause of nosocomial Candida
albicans infections?
a.
b.
c.
d.
e.
ingestion of contaminated food or water
infectious flies
yeast normally found in the body’s microbial (endogenous) population
direct contact with lesions in other individuals
through sexual intercourse
23. The microscopic finding of yeast cells and/or pseudohyphae in infected tissue or body fluid
specimens would suggest an infection of which of the following fungi?
a.
b.
c.
d.
e.
Histoplasma capsulatum
Aspergillus fumigatus
Crytococcus neoformans
Coccidioides immitis
Candida albicans
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
83
THE MENACING FUNGI
24. Which of the following choices lists a disease state considered in the United States as an
AIDS-defining condition?
a.
b.
c.
d.
e.
paracococcidiomycosis
coccidioiomycosis
Candida albicans-caused esophagitis
histoplasmosis
aflatoxin poisoning
25. Which of the following is INCORRECT with respect to biofilms?
a. a significant proportion of human infections involve biofilms formed by
microorganisms
b. microbial biofilms develop when microorganisms adhere to a surface and produce
extracellular polymers of carbohydrates, or proteins, that provide a matrix and aid in
further attachments
c. microorganisms in biofilms do not behave differently from freely suspended
microbes
d. both bacteria and Candida species within biofilms are markedly resistant to
antimicrobial agents
e. biofilm-associated infections with retained medical devices may recur after cessation
of antibiotic therapy and may require device removal..
26. Which of the following structures an/or components associated with Cryptococcus
neoformans is unique among pathogenic fungi and contributes to the disease producing
capability of the pathogen by interfering with host immune processes such as phagocytosis?
a.
b.
c.
d.
e.
individual cells
pseudohyphae
mycelium
cell wall
capsule
27. Cryptococcus neoformans is normally acquired by humans by which of the following?
a.
b.
c.
d.
e.
ingestion of contaminated food or water
through inhalation of the pathogen
infected tick bites
infected bats
choices c and d only
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
84
THE MENACING FUNGI
28. Which of the following choices would likely be the original location of P. marneffei
infections?
a.
b.
c.
d.
e.
San Joaquin Valley of California
Certain countries in Southeast Asia
Alaska
southern portions of Arizona
countries of South America including Venezuela, Columbia, Paraguay, and
Argentina
29. Penicilliosis generally results from which of the following?
a.
b.
c.
d.
e.
the ingestion of P. marneffei spores
tick bites
infected mosquitoes
the inhalation of P. marneffei spores
fomites (contaminated inanimate objects)
30. Which of the following choices lists the two MAJOR consequences of ergot poisoning?
a.
b.
c.
d.
e.
convulsions and gangrenous ergotism of the extremities
meningitis and cutaneous ergotism
immune suppression and dermatitis
sick-building syndrome and bleeding
bleeding and vomiting
GW: Test Version A
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
85
THE MENACING FUNGI
ANSWER SHEET
NAME____________________________________ STATE LIC #_______________________
ADDRESS_________________________________ AARC# (if applic.)___________________
DIRECTIONS: (REFER TO THE TEXT IF NECESSARY – PASSING SCORE FOR CE
CREDIT IS 70%). IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS AND RETURN TO: RCECS, 16781 VAN BUREN BLVD, SUITE B,
RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861. IF YOU ELECTED ONLINE
DELIVERY, COMPLETE THE TEST ONLINE – PLEASE DO NOT MAIL OR FAX BACK.
1. a b c d e
16. a b c d e
2.
a b c d e
17. a b c d e
3.
a b c d e
18. a b c d e
4.
a b c d e
19. a b c d e
5. a b c d e
20. a b c d e
6. a b c d e
21. a b c d e
7. a b c d e
22. a b c d e
8. a b c d e
23. a b c d e
9. a b c d e
24. a b c d e
10. a b c d e
25. a b c d e
11. a b c d e
26. a b c d e
12. a b c d e
27. a b c d e
13. a b c d e
28. a b c d e
14. a b c d e
29. a b c d e
15. a b c d e
30. a b c d e
GW: Test Version A
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
86
THE MENACING FUNGI
EVALUATION FORM
NAME:____________________________________________ DATE:______________
AARC # (if applic.)________________________ STATE LICENSE #:______________
RC Educational Consulting Services, Inc. wishes to provide our clients with the highest quality
CE materials possible. Your honest feedback helps us to continually improve our courses and
meet CE regulations in many states. Please complete this form and return/submit it with your
answer sheet. Thank you.
YES
NO
Were the objectives of the course met?
Was the material clear and understandable?
Was the material well-organized?
Was the material relevant to your job?
Did you learn something new?
Was the material interesting?
Were the illustrations, if any, helpful?
Would you recommend this course to a friend?
What was the most valuable portion of the material?
________________________________________________________________________
What was the least valuable portion of the material?
________________________________________________________________________
Suggestions for future courses: ______________________________________________
Comments: ______________________________________________________________
________________________________________________________________________
What is your specialty area?______________________________ Credentials?________
How did you hear about RCECS?____________________________________________
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
87