European Psychiatry 26 (2011) 11-14
Diagnosis and classification of mental disorders
in Russian speaking psychiatry: focus on affective spectrum disorders
V.N. Krasnov
Moscow Research Institute of Psychiatry, Poteshnaya 3, Moscow, 107076, Russia.
ABSTRACT
Keywords:
Classification
ICD-10
DSM-IV
Psychopathology
Dynamic approaches in diagnostics
Psychopharmacological analysis
Affective spectrum disorders
Depression
Anxiety
PTSD
Somatoform disorders
Russian–speaking psychiatry
The paper deals with present-day classification of mental disorders regarded from the positions of
Russian-speaking psychiatrists. Consideration of depressive and anxiety disorders, in particular in
the context of a multi-year research within the settings of the primary care network, points to close
links between these disorders. The concept of a psychopathological commonality among affective
spectrum disorders is set forth with references to earlier studies and the data of other Russianlanguage writers. The affective spectrum disorders cover typical affective disorders, mixed anxiety
and depressive disorders, as well as somatoform and stress-related disorders.
Current classifications ICD-10 and DSM-IV reflect many
contradictory tendencies in recent developments in psychiatry.
The principal among them are as follows:
• necessity to use standard and internationally accepted diagnostic categories;
• simplification of diagnosis reached by counting symptoms of
disorder (operational diagnostics);
• prevalent static evaluation of disorders, i.e. identifying an
actual combination of symptoms at a certain moment of
time, as a diagnostic unit, instead of dynamic evaluation of
the syndrome.
• the impact of public perception on the classification or name
of disorders, the perception stemming from notorious bias or
prejudice with regard to psychiatry. There have been some
precedents when reciprocal striving of both psychiatrists
and associations of patients and their relatives brought about
radical suggestions of denying certain long-established medical diagnostic terms such as schizophrenia [1]. Rejection of
Correspondance.
E-mail address: krasnov@mtu-net.ru
© 2011 Elsevier Masson SAS. All rights reserved.
© 2011 Elsevier Masson SAS. All rights reserved.
generally accepted terminology is fraught with losing scientific
landmarks in both psychiatry and medicine as a whole.
The mentioned tendencies reflect utilitarian essence of the
classification as a technological facet of psychiatric practice.
And this is their difference as a consensus of experts from
psychopathology as a theoretical and conceptual level of
clinical analysis based on structural connections and dynamic
interactions of mental phenomena (both abnormal and natural,
including defensive and compensatory ones). To a certain degree
one can hardly expect obligatory correspondence between the
psychopathological (systemic) evaluation of some condition and
establishing its place in the nomenclature of mental disorders
recognized at concrete period of time.
Though the majority of Russian and Russian-speaking psychiatrists in Belarus, the Ukraine, Kazakhstan, Kyrgyz Republic
and Armenia do recognize the advantages of the ICD-10 as a common language for psychiatrists all over the world, they are rather
critical about certain general and specific aspects of the ICD-10
and DSM-IV. They consider renunciation of nosology (as a basis
for classification), as a temporary retreat necessary for review
and analysis of data concerning etiology and pathogenesis of the
majority of mental disorders. Atheoretical character of the ICD-10
and DSM-IV is presented as renunciation of ideology, while the
12
V.N. Krasnov / European Psychiatry 26 (2011) 11-14
nosological clinical system initially developed by E. Kraepelin [2]
is considered as a variant of ideology. Actually, the nosological
system was a means of learning about morbid phenomena using
the knowledge, and data available in certain period of history.
Russian-speaking psychiatrists educated in accordance with traditions of classical clinical psychiatry, primarily German, French and
Russian, do not reject the nosological principle completely. They
still hope that a new nosology will arise as a unity of etiology,
symptomatology and the course of disease.
Methodology of diagnosis implies the development of
symptoms in time, grouping particular features, organizing
them in systematic way, finding internal relationships between
individual elements and observing the shaping of the syndrome.
The syndrome is understood as a dynamic formation with
changing structural ratios of symptoms. In an autochthonous,
spontaneous development of a disease, some symptoms may
come to foreground, some decrease or remain hidden, but still
present. This is an essential characteristic of syndromokinesis, or
syndrome trend. In the course of a relatively long-term observation and treatment the psychiatrist can observe the reshaping
and transformation of syndromes.
Psychopharmacological analysis, i.e. using medication both
as a treatment factor and a means of investigation, offers an
opportunity to study the psychopathological dynamics of the
syndrome and specify the diagnosis [3,4]. Thus, use of antipsychotics (olanzapine, risperidon or other) in paranoid schizophrenia may help to detect underlying depression. In other cases,
the use of antidepressants with a stimulating component for
the treatment of depression can reveal incongruent delusional
ideas (e.g. ideas of persecution) and thus cause alteration of
diagnosis and adjustment of treatment. Another example could
be relatively fast relief of seemingly dominant anxiety by means
of antidepressant medication with anxiolytic properties (like
trazodon, mianserin, mirtazapin), while the depressive “nucleus”
lags behind and gradually decreases two to three weeks after the
primary anxiolytic effect of the medication. Similar combined
treatment and diagnostic approaches we can find not only in
Russian clinical psychiatry [5].
Russian and Russian-speaking specialists still take efforts to
confirm the single nature of depression and majority of anxiety
disorders within frames of anxiety-depressive conditions despite
their current separate positions in the ICD-10 and DSM-IV as
depressive disorder and anxiety disorder.
Close clinical relationships between anxiety and depression have been formulated in traditional psychiatry [6-8]. It
is a well-known fact from psychiatric practice dealing with
recurrent depression that in every next depressive episode the
representation of anxiety components decreases while the representation of typically depressive ones (like diurnal variations
with morning worsening, diminished motivation for activity,
and feeling of guilt) increases. Clinically and epidemiologically
the distinction between long-term anxiety disorders and major
depression (specifically regarding first depressive episode) are
not clear-cut [9-12].
Our special research of affective spectrum disorders in
primary health care system in framework of the Programme
“Recognition and treatment of depression in primary care” [13]
also suggests transformation of anxiety disorders into depressive disorder within one continuum. Purpose was to study of
the prevalence of affective spectrum disorders in primary care
setting. Methods used are as follows: screening questionnaire,
semistructured psychiatric interview, SCL-90-R, Hamilton
Depression Rating Scale (HDRS-17), Hamilton Anxiety Rating
Scale (HARS).
In 2000–2001 a screening of affective spectrum disorders
in several territorial (general medical) polyclinics in three cities
of Russia has been carried out. Subjects of investigation were
working or studying persons, aged from 18 to 55 years.
During the first stage, we identified with the help of a
7-item screening instrument a group of outpatients with
various affective spectrum disorders, including subthreshold
depression, anxiety and somatoform (psychovegetative) disorders. This group consisted of 2.749 persons (51.2%) of the
5.366 outpatients screened. They were offered a consultation of
a psychiatrist concerning their symptoms, in a special (so called
“psychotherapeutic”) room. 1.919 (35.8%) agreed to this proposal
and were interviewed by a psychiatrist. 1.616 (30.1%) cases of
those investigated were diagnosed as suffering from depression according to ICD-10 criteria for a depressive episode; in
1.334 cases (24.8%) severity of depression was 15 or more on the
Hamilton Depression Scale. Diagnoses distribution is presented
in Table 1. In accordance with the terms of the above-mentioned
Program, these persons could enter a 6-week course of medication with modern antidepressants, mainly with sertraline.
In about 90% of these cases depression dominated in patients’
condition but it was accompanied by subsyndromal or obvious
moderate anxiety disorders. At the same time, there were different combinations of depression with anxiety and somatoform
disturbunces--with similar score levels of somatization, depression and anxiety by SCL-90-R. As for prevalent anxiety disorders
(like generalized anxiety disorder or panic disorder), they were
diagnosed only in 238 (4.4%) persons. Somatoform disorders
were mostly preliminary diagnosed for further observation.
In 2002-2003, a second screening with subsequent diagnostic
procedure and following the same research design took place
in two policlinics. Screening covered 4.020 persons, and 2.046
(50.9%) had signs of affective spectrum disorders. A psychiatric
interview helped to detect 1178 (29.3%) cases of depression,
including 992 cases (24.7%) with score 15 and higher on the
Hamilton Depression Scale.
138 of the latter subgroup had previously been included
in the sample of previous research in 2000 - 2001, and 34 of
them then had been diagnosed as anxiety disorders, including
9 cases of “generalized anxiety disorder” (GAD), 19 cases of
“panic disorders” and 6 other cases of anxiety disorders.
At the period 2002-2003 the above mentioned cases met
the criteria of depressive episode. Former dominated anxiety
Table 1
ICD-10 diagnoses distribution of depressive disorders in primary care.
F 32
Depressive episode
31.2%
F 33
Recurrent depressive disorder
24.1%
F 34
Chronic depressive disorder
(mainly “double depression” within dysthymia)
26.3%
F 41.2
Mixed anxiety and depressive disorder
11.0%
F 43.21
Long-term depressive reaction
3.1%
Others
4.3%
V.N. Krasnov / European Psychiatry 26 (2011) 11-14
happened to be on subordinated position because of pronounced
symptoms of depression.
In 2004-2005 more 28 cases of anxiety disorders from
observed sample have been changed for diagnosis “depression”,
including 13 with former diagnosis GAD. Besides during the
period of observation a part of patients with mixed anxiety and
depressive disorder entered for secondary consultative aid,
and their condition turned out more close to strict criteria of
depression. It is noteworthy that the so-called social phobia was
hardly considered as a basis for seeking help within primary care
system. Separate somatoform disorders without (sub) depressive
and anxiety features were also identified in rare cases.
Thus, one can suggest a tendency for transformation of affective disorders in the course of time or subsequent episodes – from
prevalent anxiety symptoms to mixed anxiety – depressive
condition, and further on to depressive syndrome per se. It seems
like another argument in favor of single pathogenetic entity for
majority of affective spectrum disorders. Then anxiety shows at
the initial stage or as the foreground primary affect that tends
to evolve in direction of typical depression.
On the basis of our previous study on psychopathology and
dynamics of different types of depression [14] we suggest, and
this suggestion is confirmed by the data from primary care, that
depression has several stages of development. Those are:
• Prodrome with non-specific symptoms of emotional and
vegetative instability;
• Anxious stage including three substages:
Ⱦ situation anxiety with a concrete cause,
Ⱦ free-floating anxiety with changing subjects of anxiety,
mainly determined by chance,
Ⱦ anxiety with no cause (without subject);
• Depressive stage including three substages:
Ⱦ depression with “anxious” elements within sadness
condition,
Ⱦ depression with hidden anxiety, but with domination of
sadness,
Ⱦ depression with areactivity / hyporeactivity and psychomotor retardation.
Operational diagnosis registers only a concrete stage at the
moment the patient is seeking help. Identifying dynamic aspects
of diagnosis seem to be a task for future classifications.
A dynamic hierarchy and multiple interrelationships
between depression and anxiety should be taken into account
in the development of future psychiatric diagnostic systems.
It could be functional diagnostics, which consider, anxietydepressive affective disorder as cohesive entity, a kind of clinical
continuum from adjustment disorders with protracted anxiety
and depressive symptoms to severe melancholic depression.
The symptoms of GAD share many features with depression
and often represent the prodromal phase of depressive episode.
More or less similar relationship can be revealed between panic
disorder at the whole context and affective spectrum disorders. The
differences are much more connected with physiological (including
emotional and vegetative) reactivity than psychopathology itself.
There are also some specific problems Russian and Russianspeaking psychiatrists face while using ICD-10. Regarding the affective spectrum disorders more few categories should be considered.
Majority of Russian-speaking psychiatrists, especially those
who have much experience in treatment of victims of large-scale
13
disasters, military combat or terrorist attacks are critical about a
wider application of the clinical diagnosis “post-traumatic stress
disorder” (PTSD) [15-18]. A significant part of conditions identified in English-language publications as PTSD are interpreted in
Russia in a different way: primarily as long-term depression, or
polymorphic conditions, or a combination of dysthymia, mild
cognitive disorders, personality deviations and psychosomatic
dysfunctions, sometimes with excessive alcohol consumption or
drug abuse. The nature of such disorders is understood rather as
multifactorial, and not exclusively psychotraumatic. For instance,
in the persons involved in elimination of the consequences of the
Chernobyl disaster in 1986, persistent disorders developed as a
response to a combined (synergic) effect of a number of harmful factors while every single factor was not really pathogenic.
Among them are extreme psychological and physical tension,
disrupted biological rhythm in the first months after the disaster
because of hard work in shifts associated with construction of
protective “sarcophagus”, exposure to low doses of radiation
(insufficient for development of radiation disease), dust, polluted
air, especially in the environment of miners digging a tunnel
under the destroyed nuclear reactor, other unfavorable factors
connected with emergency work in Chernobyl. Many of the
rescue workers experienced asthenic, psychovegetative, affective spectrum disturbances or stable disorders for the long time
[19]. But official medicine didn’t find some specific reason and
specific “name” for their morbid condition. It didn’t meet criteria
of radiation disease and didn’t meet full criteria of PTSD. Their
symptomatology in development with tendency of worsening
intellectual and physical productivity was much more close to
so called organic psychosyndrom by E. Bleuler [20]. Similar ideas
about multiple nature and polymorphism of symptomatology
of the post-traumatic stress disorders are rather rare but can be
found in current English-language literature [21,22].
There is a semantic inaccuracy that should absolutely be
deleted from the future ICD-11: it has to do with the categorization of stress related disorders (F 43). It has been formulated as
“reaction to severe stress”. This seems illogical because «stress»
in itself is a “reaction” of adaptation to changing environment.
More appropriate could be use the common category stress
disorders.
According to opinion of the most of Russian speaking psychiatrists, the category “somatization disorder” (F45.0) has no
real clinical ground and is contradictory in itself. The point is that
somatization is not a state but the process of involvement of different somatic functions (vegetative, metabolic,neuroendocrine,
immune, trophic) into pathological condition. According to
tradition [23,24], somatization can be interpreted as reflection
of primary affective disorders (anxiety and depression) on
vegetative-somatic level. Historically the notion “somatization
disorder” is only other name of “conversion disorder”, that consider psychodynamic interpretation of psychogenic or neurotic
disturbances in old terminology. “Somatoform disorders” in
the whole are very common, mostly as somatoform autonomic
dysfunction (F 45.3) as usual with subaffective ground.
Declarations of interests
The author has no interests that may be affected by the
publication of this paper.
14
V.N. Krasnov / European Psychiatry 26 (2011) 11-14
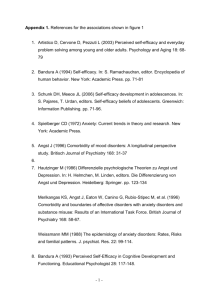
References
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
Van Os J. A salience dysregulation syndrome. Br J Psychiatry 2009;194:101-3.
Kraepelin E. Lehrbuch der Psychiatrie. A. Barth, Leipzig. 1896.
Avrutsky GY, Neduva AA. Treatment of mentally ills: Guideline for physicians. Moscow: Meditsina; 1988.
Krasnov V, Gurovich I. Current state of Russian psychiatry. In: Bhui K,
Bhugra D, editors. Culture and mental health. A comprehensive textbook.
London, UK: Hodder Arnold; 2007. p. 109-21.
Fink M, Taylor MA. Melancholia: the diagnosis, pathophysiology and
treatment of depressive illness. Cambridge: Cambridge University
Press; 2006.
Schneider K. Klinische Psychopathologie. G. Stuttgart: Thieme Verlag; 1962.
Lewis A. The state of psychiatry: essay and addresses. New York: Science
House; 1967.
Weitbrecht HJ. Psychiatrie im Grundriss. Berlin: Springer Verlag; 1973.
Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence
of anxiety disorders and their comorbidity with mood and addictive
disorders. Br J Psychiatry 1998;34:24-8.
Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence,
severity, and comorbidity of 12-month DSM-IV disorders in the National
Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:617-27.
Wittchen HU, Kessler RC, Pfister H, Lieb R. Why do people with anxiety
disorders become depressed? A prospective-longitudinal community
study. Acta Psychatr Scand 2000;102:14-23.
Preisig M, Merikangas KR, Angst J. Clinical significance and comorbidity
of subthreshold depression and anxiety in community. Acta Psychiatr
Scand 2001;104:96-103.
[13]
[14]
[15]
[16]
[17]
[18]
[19]
[20]
[21]
[22]
[23]
[24]
Krasnov VN. The Programme “Recognition and treatment of depression
in primary care settings”. Soc Clin Psychiatry 1999;4:5-8.
Krasnov VN. Principals of dynamics of depression: clinical, pathogenetical and therapeutical aspects. In: Smoulevich A, editor. Depression and
comorbid disorder. Moscow, Russian: RAMN; 1997. p. 80-97.
Evsegneev RA. Psychiatry for general physician. Minsk: Belarus; 2001.
Sukiasyan SG, Tadevosyan AS, Chshmarityan SS, Manasyan NG. Stress
and post-stress disorders. Yerevan: Asogik; 2003.
Morozov AM, Kryzhanovskaya LA. Clinic, dynamics and treatment of
mental disorders in «liguidators» of disaster at Chernobyl NPP. Kiev:
Russian Chernobylinform; 1998.
Kokhanov VP, Krasnov VN. Psychiatry of disasters and emergency situations. Moscow: Prakticheskaya Meditsina; 2008.
Krasnov V. Psychopathological consequences of the Chernobyl disaster as a subject of ecological psychiatry. It J Psychiatry Behav Sci
2004;14:9-13.
Bleuler E. Lehrbuch der Psychiatrie. Berlin: Springer-Verlag; 1916.
Everett B, Ismail K, David A, Wessely S. Searching for a Gulf War syndrome
using cluster analysis. Psychol Med 2002;32:1371-8.
McFarlane AC. Psychiatric Morbidity following disasters: epidemiology,
risk and protective factors. In: Lopez-Ibor JJ editor. Disasters and Mental
Health. Chichester, UK: John Wiley & sons; 2005. p. 37-63.
Lesse S. The multivariant masks of depression. Am J Psychiatry
1968;11:35-40.
Lopez Ibor JJ. Larvierte Depressionen und Depressionsaequivalente. In:
Kielholz P editor. Depressive Zustaende. Bern, Stuttgart, Wien: Verlag
Hans Huber; 1972. p. 38-43.