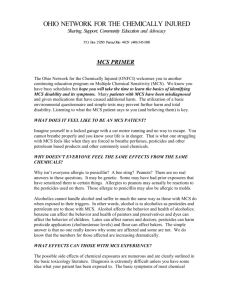
An Olfactory-Limbic Model of Multiple Chemical Sensitivity Syndrome
advertisement

218 BIOL PSYCHIATRY i 992 ;32:218-242 An Olfactory-Limbic Model of Multiple Chemical Sensitivity Syndrome: Possible Relationships to Kindling and Affecf.ve Spectrum Disorders Iris R. Bell, Claudia S. Miller, and Gary E. Schwartz This paper reviews the clinical and experimental literature on patients with multiple adverse responses to chemicals (Multiple Chemical Sensitivity Syndrome-MCS) and develops a model for MCS based on olfactory-limbic system dy~mction that overlaps in part with Post's kindling model for affective disorders. MCS encompasses a broad range of chronic polysymptomatic conditions and complaints whose triggers are reported to include low levels of common indoor and outdoor environmental chemicals, such as pesticides and solvents. Other investigawrs have found evidence of increased prevalence of depression, anxiety, and somatization disorders in MCS patients and have concluded that their psychiatric conditions account for the clinical picture. However, none of these studies has presented any data on the effects of chemicals on symptoms or on objective measures of nervous system fimction. Synthesis of the MCS literature with large bodies of research in neurotoxicology, occupational medicine, and biological psychiatry, suggests that tile phenorzenology of MCS patients overlaps that of afj~ctive spectrum disorders and that both involve dysfunction of the limbic pathways. Animal studies demonstrate that intermittent repeated low level environmental chemical exposures, including pesticides, cause iimbic kindling. Kindling (full or partial) is one central nervous system mechanism that could amplify reactivity to low levels of inhaled and ingested chemicals and initiate persistent affective, cognitive, and somatic symptomatology in both occupational and nonoccupational settings. As in animal studies, inescapable and novel stressors could cross-sensitize with chemical exposures in some individuals to generate adverse responses on a neurochemical basis. The olfactory-limbic model raises testable neurobiological hypotheses that could increase understanding of tile multifactorial etiology of MCS and of certain overlapping affective spectrum disorders. From the Department of Psychiatry, University of Arizona Health Sciences Center, Tucson, Arizona dRB); Department of Family Practice (Environmental Medicine Division), University of Texas Health Science Center, San Aptonio, Texas (CSM); and Department of Psychology, University of Arizona, Tucson, Arizona (GES). This research (CSM) was supported in part by an appointment to the Agency for Toxic Substances and Disease Registry Clinical Fellowship Program in Environmental Medicine, administered by Oak Ridge Associated Universities through an interagency agreement between the U.S. Department of Energy and ATSDR, Address reprint requests to Dr. Iris Bell at the Department of Psychiatry, University of Arizona Health Sciences Center, Tucson, AZ 85724. Received lanuary 1, 1992; revised March 14, 1992. Presented in part at the 119th Annual Meeting of the American Public Health Association, Atlanta, Georgia, November 1~14, 1991. © 1992 Society of Biological Psychiatry 0006-3223/921505.00 Limbic Kindlingand ChemicalSensitivity BIOLP~YCHiATRY 1992;32:218-242 219 Introduction Multiple chemical sensitivity (MCS) has been described as a chronic syndrome characterized by patterns of multiple somatic, cognitive, and affective symptoms with no consistently abnormal findings on routine laboratory testing to date (Ashford and Miller 1991; Bell 1975, 1982, 1987, 1992a). Proponents of the syndrome propose that acute higher level exposures to common environmental chemicals often initiate sensitivity, and chronic lower level exposures--and sometimes foods---perpetuate the problem (Randolph 1970, 1974, 1978; Rea 1977, 1978; Boyles 1985). Symptoms emerge from the interaction of sensitivity with time factors. That is, after sensitivity develops, proponents further claim that chronic exposures induce adaptation and blunted symptomatology, whereas removal from exposure followed by reexposure produces deadaptation and heightened symptoms (Randolph 1978). Skeptics suggest that the syndrome is simply a manifestation of traditional psychiatric disorders, especially depression, anxiety, and somatization disorders, in combination with a misattributed, projective belief in an environmental chemical etiology (Brodsky 1983; Stewart and Raskin 1985; Ten" 1986; Staudenmayer and Camazine 1989; Black et ai 1990; Rosenberg et al 1990; Staudenmayer and Selner 1990). For example, some studies (Black et al 1990; Simon et al 1990), but not all (Davidoff 1991; Kipen and Fiedler 199!), have noted past histories of depression in more MCS patients than in normal controls. No studies have presented data on central nervous system responses to acute chemical exposures in MCS. Although immunological or even allergic mechanisms have been proposed, no consistent findings have been demonstrated. Despite the intense debate, only one such study in the literature has presented e.ny data on the effects of laboratory chemical challenges on MCS patients. Doty et al (1988) reported that MCS patients had higher levels of nasal resistance and faster respiratory rates before and after low level exposures to two common chemicals (phenyl ethyl alcohol and methyl ethyl ketone) in comparison with normal controls. Why is it important to go beyond labeling MCS as merely a variant of "standard" psychiatric syndromes? In the first place, psychiatric diagnoses in DSM-III-R are simply descriptive labels for symptom patterns; as such, they provide no etiological explanation of the phenomenology and do not imply a simple "psychogenic" cause for most disorders (Davidoff et al 1991). Nonpsychogenic precipitants of depression can include drugs, other chemical agents, and medical illnesses (Stoudemire 1987). Recent studies in neurological disorders such as stroke (Catapano and Galderisi 1990) and Parkinson's disease (Ehmann et al 1989) have indicated that biological factors in the brain, more than psychological reactions to disability, account for the depression that often accompanies these conditions. Investigations of MCS may provide etiological clues for still other subtypes of affective disorders. Second, no group studies on the central nervous system effects c~ environmental chemicals in MCS patients have yet been published. MCS patients have significant objective baseline impairments in verbal and visual memory function (Kipen and Fielder 1991). Occupational investigations of wo~-kers overexposed to solvents, pest:,c:~des, or diesel fuel have shown multiple neuropsychologicai deficits (Morrow et ai 1990; Molhave 1991; Rosenstock et al 1991; Schwartz et al 1991), asymmetric bleed flow on single photon emission computed tomography (SPECT) and positron emission tomography (PET) scans especially in frontal and temporal regions (Callender 1991; Morrow et ai 1991), and affective symptomatology that persists long after an acute exposure event (Kilburn et al 1989; Morrow et al 1989, 1990). Third, subsensory (not consciously detectable) 220 BIOLPSYCHIATRY I.R. Bell et al 1992;32:2 i 8--242 Environmental Chemicals > NEUROBIOLOGICAL EVENTS 1 ~ A I I Psychosocial Stressors Symptoms 2 Figure 1. Interactive biopsychosocial model for multiple chemical sensitivity. 'Chemical kindling of olfactory bulb, amygdala, piriform cortex, and/or hippocampus is the major neurobiological event that would initiate MCS. Genetic vulnerability to affective disorders, trait shyness, and female gender may increase kindling risk. 2Low levels of chemicals and/or psychosocial stressors induce neurobiological events that would activate the already kindled limbic system in chronic MCS and perpetuate affective, cognitive, and/or somatic symptoms. levels of certain chemicals in normal human subjects reduce performance on attentional tasks, alter electrophysiological electroencephalographic (EEG) patterns, and lower mood (Lorig 1989). Fourth, finding affective disorders in MCS does not rule out other, concomitant illness processes. Sampling biases, disability status, and chronicity of illness could favor finding affective spectrum disorders in a high percentage of selected MCS patients, just as many studies of more traditional chronic medical illnesses have also noted (e.g. depression .in approximately 20% and up to 45% of patients with cancer, heart disease, rheumatoid arthritis, diabetes) (Katon and Sullivan 1990). Thus, depression cannot be a diagnosis of exclusion in clinical practice. Concomitant depression might predispose some patients to enter the medical care system and further to enroll in MCS research studies more readily and/or to complain of worse illness severity in comparison with MCS patients without depression (Parmelee et al 1991). Our own survey data showed that 66% of 643 healthy young adult college students rated the smell of at least one common environmental chemical and 15% rated 4 to 5 of five chemical odors as capable of making them ill. Although depression explained 27% of the variance in total symptom scores, neither depression, anxiety, sense of control, nor repression accounted for any of the variance in the total chemical sensitivity scores (Bell et al 1992b). Such findings suggest a major public health problem whose core derives much more from biological than psychological factors. Fifth, a large body of animal literature indicates that low levels of various environmental chemicals exert acute and chronic effects both on behavior and on neurophysiological function, including limbic kindling (Burchfiel and Duffy 1982; Joy 1982; Gilbert 1992a). The Kindling and Sensitization Model These data suggest an integrative hypothesis that synthesizes the literature in biological psychiatry (Post 1980; Post et al 1984; Adamec and Stark-Adamec 1983; Adamec 1990, 991; Adamec and Stark-Adamec 1986; Anteiman 1988; Hudson and Pope 1990) with that of neur~'.cxicology (Joy 1982; Gilbert 1992a; Ashford and Miller 1991; Bell 1975, 1982, 1992a). That is, many environmental chemicals gain access to the central nervous system via the olfactory (Cain 1974; Shipley 1985; Cheng et al 1988; Ryan et al 1988; Ghantous et al 1990) and limbic pathways (Gilbert and Mack 1989), induce lasting changes in limbic neuronal activity (Bokina et al 1976) and overall cortical arousal levels (Lorig et al 1988), and thereby alter a broad spectrum of behavioral and physiological functions to produce clinical MCS syodrnmes (Figure 1). The lack of a blood-brain barrier in the Limbic Kindlingand ChemicalSensitivity BIOLPSYCHIATRY 1992;32:218-242 221 olfactory system permits direct access via the nasal mucosa to the olfactory bulb for a wide range of environmental chemicals, including aromatic hydrocarbon solvents (Ghantous et al 1990), aluminum (Peri and Good 1987), and cadmium (Hastings and Evans 1991). Macromolecular substances can move transneuronal!y from the primary sensory neurons in the nose not only to the olfactory bulb, but also to the olfactory tubercle, piriform cortex, periamygdalar and entorhinal cortex, anterior hippocampus, locus coeruleus, raphe nuclei, and diagonal band (Shipley 1985). The olfactory pathways are particularly susceptible to electrical and chemical kindling (Sato et al 1990). Kindling is a special type of time-dependent sensitization of olfactorylimbic neurons (Antelman 1988; Post 1980). It involves the ability of a repeated, intermittent stimulus (e.g. daily, high-frequency electrical stimulation) that is initially incapable of eliciting a response eventually to induce a motor seizure from later applications of the same stimulus. Limbic structures such as the amygdala are especially vulnerable to kindling. More generally, time-dependent sensitization (TDS) is a phenomenon of amplification of subsequent responses to a novel, foreign, and potentially threatening stimulus by the passage of time between the first and later stimuli (typically 7-14 days) (Antelman 1988). As in kindling, TDS can develop during repeated, noncontinuous exposures to a given drug or nondrug stressor, whose intensity can be mild or marked. The direction of later responses in TDS depends in part on the intensity of the original stressor and on the reactivity of the individual (Anteiman et al 1991). Kindling and TDS are not identical phenomena (Kalivas and Barnes 1988). For example, even though the same agent, for example, cocaine, can cause either kindling or sensitization, dependcht on dose and timing schedules, kindling is distinguished by a convulsive or subconvulsive endpoint in limbic structures, whereas sensitization can involve a broader range of behaviors and functions in various physiological systems (Antelman 1988; Antelman et al 1990; Kalivas and Barnes 1988). In the present model, subconvulsive chemical kindling in olfactory bulb, amygdala, and piriform cortex, as well as in hippocampus, would be the neurobiological mechanism that serves as amplifier for reactivity to low level chemical exposures and as an initial common pathway for a range of clinical phenomenology, including cognitive and affective dysfunctions (Dager et al 1987; Ashford and Miller 1991; Bell 1992a). Derivative mechanisms would encompass neurophy~iological (especially frontal and temporal ciysfunctions), autonomic, endocrine, and immune pathways regulated by the limbic system and connected structures (Mesulam 1985). For the present discussion, the term "kindling" in nonepileptic human subjects refers to permanent increases in limbic neuronal excitability and associated behaviors via repeated subthreshold stimulation, that is, partial kindling (Adamec and Stark-Adamec 1983; Adamec 1990; Post et al 1984). The resultant subconvulsive endpoint could involve a range of persistent phenomena, such as long-term potentiation with plastic changes in excitatory amino acid receptors (Huang et al 1992), changes in dopaminergic pathways and benzodiazepine receptor numbers, and/or failure of GABAergic inhibitory function under the stress of stimulation (Ade,mec and StarkAdamec 1983; Adamec 1990); behaviorally, it might manifest with irritability, anxiety, mood lability, and social withdrawal, parallel to Adamc~'~ obserJati¢;ns in cars (Adamec and Stark-Adamec 1983; Adamec 1990). Post et M (1984) have previously proposed that limbic kindling and sensitization underlie the long-term course of affective disorders; and the anticonvulsant drugs that block kindling (Sato et al 1990) have been found clinically useful in a subset of affective syndromes (Adamec 1990). In addition to the endogenous events proposed by Post, many environmental chemicals, including pesticides (Joy 1982; 222 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 Table I. Kindling Model for Initiation and Perpetuation of Multiple Chemical Sensitivity Affective status Normal Depl~ss~d b Normal Depressed b Duration of exposure" Initiating dose Perpetuating dose acute acute chronic chronic high medium medium low low low low low "Time-dose factors th~.t contribute to kindling-like phenomena may include a single dose at toxic levels or intermittent doses at subtoxic levels (see text), ~"Depressed" affcctive status means a lower endogenous threshold for kindling-like phenomena that environmental chemicals can then ix~tentiatein limbic neurons, Such status can occur in individuals vulnerable to affective spectrum disorders, including but not limited to bi~lar disorder or inborn trait shyness (see text), Joy et al 1983; Gilbert and Mack 1989; Gilbert 1992a; Gilbert 1992b; Gilbert 1992c), flame retardants (Tilson et al 1990), formaldehyde, acetone, benzene, and ozone (Bokina et al 1976), can also induce or accelerate seizares and/or kindling phenomena in limbic structures. Notably, most environmental chemical exposures in daily life are intermittent, which would favor kindling and sensitization (of. Post 1980). Consequently, we hypothesize that a range of environmental chemicals can also trigger and/or perpetuate affective and cognitive disorders as well as related somatic dysfunctions in vulnerable individuals via kindling mechanisms (Ashford and Miller 1991; Bell 1992a). Lipid-soluble chemicals with convulsant properties such as certain pesticides (Gilbert 1992a) v,ould be the strongest candidates for inaia~ingolfactory-limbic kindling and core central nervous system (CNS) symptoms of MCS. Other agents could induce TDS amplification of their own nonconvulsant activns in other pathways (Antelman 1988; Antelman et ai 1987, 1991) and thus perpetuatethe illness in a variety of target organs (e.g. central nervous, endocrine, and immune systems). The individuals who would be most vulnerable to kindling and related phenomena from low levels of environmental chemicals could be those genetically predisposed to certain affective spectrum disorders such as bipol~u' disorder, major depression (Rosenthal and Cameron 1991), and panic disorder (Dager et al ! 987). Psychiatrically healthy persons without an inherent loading for affective illness could also develop chemically induced syndromes, but only from higher concentrations or longer exposure periods (Table I). As Post et al (1984) and Adamec (1990) have emphasized (see above), kindling can be partial; a full clinical seizure disorder need not develop, Given the relative lack of research in MCS, it should be noted that the present discussion offers an argument for the possibility of kindling, but that no systematic data on kindling in MCS patients has yet been collected to test these hypotheses. The most relevant, albeit indirect, human evidence is that inhalation of room air through the nose, as opposed to the mouth, mote readily activates epileptiform activity in patients with temporal lobe epilepsy (Servit et al 1977), the type of seizure disorder most closely related to kindling (Sato et al 1990). IEy analogy, some MCS patients anecdotally claim more severe responses during nose versu~ mouth breathing in polluted environments. Clinical Phenomenology of Multiple Chemical Sensitivity Syndrome MCS symptoms can include: fatigue, concentration and/or memory difficulties, irritability, nervous tension, depression, daytime drowsiness, food cravings, insomnia, headaches, nasal congestion, arthralgias, myalgias, tinnitus, gastrointestinal distress, palpitations, vasculitis (Rea 1977, 1978; Jones et al 1982; Little et al 1983; Egger et al 1983, 1989; Limbic Kindlingand ChemicalSensitivity BIOLPSYCHIATRY 1992;32:218-242 223 Weiss et al 1980; Egger et al 1985; Steward and Raskin 1985; Kaplan et al 1989; Simon et al 1990; Ro:~enthaland Cameron 1991), and perhaps certain seizure disorders (Crayton et al 1981; Egger et al 1989). Early clinical observers of MCS patients anecdotally described bipolar symptom patterns for acute chemical responses, beginning with mild irritability and ranging up to panic or even mania, and followed by a period oi"depression, fatigue, and somatic symptoms such as headache, rhinitis, or hives (Randolph 1978). Patients then were reported to plateau chronically at a stimulated or depressed level, around which they would fluctuate depending on their level of adaptation to the triggering exposures. Women outnumbered men in clinical series (Rowe 1950; Ashford and Miller 1991), but no systematic epidemiologic studies are available. Patients often trace the onset of the MCS to an initial high-dose exposure such as a chemical spill or repeated, lower level exposures from a move to a new home or office building, or home pesticide treatment, for example, chlorinated hydrocarbons or organophosphates (Ashford and Miller 199 I; Rosenthal and Cameron 1991). Central nervous system symptoms are prominent and perhaps the most common feature Gf the illness in the otherwise diverse clinical symptomatology of MCS patients (Randolph 1978; Ashford and Miller 1991; Bell et al 1992a). Once the syndrome has been initiated, a "spreading phcr.omenon' reportedly occurs, in which sensitivity generalizes from the original agent to low doses of multiple, chemically unrelated substances, such as perfume, tobacco smoke, auto exhaust, and newsprint. A majority of patients also report new sensitivities to common foods, alcoholic beverages, and often previously tolerated medications (Randolph 1978; Boyles 1985), a cross-sensitization that parallels the phenomenology of TDS. Once initiated, heightened susceptibility to chemicals and foods (which are themselves mixtures of organic chemicals [Bell 1982]) persists indefinitely, with gradual symptomatic improvement following long-term avoidance of triggering substances. However, resumption of frequent, intermittent exposure can reactivate symptoms at any time, as in kindling and sensitization (Kalivas and Barnes 1988). Adaptation of symptom expression can occur with very frequent or continuous chemical or food exposures and can occur during the sensitizing process (Randolph 1978), again similar to findings with time.dependent sensitization (Post 1980; Kalivas and Barnes 1988). The most severely affected patients become chronically disabled, with high individual and societal costs in terms of lost productivity, social isolation, financial setbacks, and health care requirements (Bell 1987). Much controversy has surrounded various diagnostic methods and treatments offered to these patients, including a procedure called provocation-neutralization (King 1988; Jewett et al 1990), detoxification procedures (Kilburn et al 1989), and physician-directed avoidance of all chemical exposures (Brodsky 1983; Bell 1987). Chemically sensitive groups can overlap in clinical symptomatology, but differ in demographics, types of initiating chemical exposures, and dose levels. Ashford and Miller (1991) have delineated four different groups of chemically sensitive patients: (1) the individual MCS patients described above, with heterogeneous work and home chemical exposures, generally at low levels; (2) tight building occupants (white collar office workers; primarily female, whose symptoms began in the workplace), with off~,assing from construction materials and office equipment, perfume, and tobacco smoke as major e~posures; (3) industrial workers (blue collar workers; primarily male), with higher level acute and chronic industrial chemical exposures; and (4) members of contaminated communities (all ages and both sexes), with exposures from air and water contamination by toxic waste sites, pesticide spraying, or industrial dumping, at varying levels. For all of the groups above, the implicated exposure levels are frequently below 224 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 allowable regulatory limits, do not trigger known allergic or immunologic mechanisms, and are therefore controversial. The time pattern of MCS initiation most closely parallels kindling or partial kindling when it involves repeated, intermittent exposures to subtoxic levels of environmental chemicals with convulsant properties, such as might occur in monthly, routine pesticide spraying at home or in daily office chemical exposures at the workplace. The time patterning of MCS initiation parallels the more general phenomenon of t,.'me-dependent sensitization in the central nervous system (TDS) (Antelman 1988) when it involves a single, high dose or even toxic exposure that is or is perceived as very foreign or life-threatening by the individual, followed by subtoxic levels of the same or cross-sensitized chemicals thereafter, such as might occur in an industrial chemical spill accident (Simon et al 1990; Morrow et al 1991). Either long-term low dose, intermittent or short-term, high-dose exposures can result in clinically indistinguishable MCS syndromes. By analogy, certain environmental chemicals (Bokina et al 1976) and corticotropin-releasing hormone (Weiss et al 1986) can produce kindled-like neuronal firing in the amygdala after only one, relatively higher dose, as opposed to repeated intermittent low doses of the given agent. Moreover, either I0 nontoxic weekly doses or one toxic dose of an organophosphate pesticide can lead to the same increase in EEG beta activity of mt,,keys (Burchfiel and Duffy 1982). Although certain more classically toxic exposures can produce lasting structural damage and/or irreversible impairments, hallmarks of MCS are the persistent sensitivity to environmental chemicals and the fluctuating symptoms from day to day with variations in exposures (Randolph 1978). Partial kindling (Adamec and Stark-Adamec 1983) and time-dependent sensitization (Antelman 1988; Antelman et al 1991) can manifest with altered function of the central nervous system that could result in such behavioral and affective changes, without structural lesions or simple pharrnacokinetic relationships. Human Studies Cognitive and EEG Findings. Preliminary data indicate that MCS patients have attention and concentr~.tion as well as memory deficits. For example, Bell et al (1992a) observed both a higher prevalence of subjecti Je difficulty concentrating and poorer objective performance on a 2-rain serial subtraction task in patients with food and chemical sensitivi,ies than in normal controls. Molhave's group in Scandinavia (Molhave et al 1986, 1991; Kjaergaard et al 1991; Molhave 199 !) has challenged office workers reporting symptoms of sick building syndrome (SBS) and normals with an airborne mixture of 22 volatile organic substances, primarily solvents, commonly released indoors by building materials. Sick building syndrome refers to a complex of symptoms reported by office workers in certain modern office buildings. A wide range of causative factors may be involved, including inadequate ventilation, indoor air pollutants (e.g., smoke, formaldehyde, various solvents), ergonomic factors, crowding, and work stresses (Kreiss 1989). Symptoms associated with SBS include sensory irritation of mucous membranes, headache, sluggishness, difficulty concentrating or remembering, dizziness, nausea and vomiting, skin irritation, nonspecific symptoms, and changes in olfactory or gustatory sensations (Molhave 1991). During chemical exposures, Kjaergaard et al (1991) found irritation of the eyes, nose, and throat to be the most common symptoms, as well as less improvement between sessions on the same day in concentration task performance (e.g., graphic continuous performance test and the digit symbol test) of SBS workers and normals exposed to Limbic Kindlingand ChemicalSensitivity BIOLPSYCHIATRY 1992:32:2i8-242 225 mixtures of the organic chemicals in comparison with subjects from both groups who received no chemicals at either session. Molhave et al (1986) had earlier noted decreased digit span test performance in otherwise healthy subjects reporting SBS symptoms given the same chemical mixture. Apart from attention deficits, Kipen and Fiedler (1991) have presented preliminary findings of impaired performance on the California Verbal Learning Test and the Continuous Visual Memory Test in MCS patients relative to control patients with chronic fatigue syndrome (CFS). The greater memory deficits in MCS are particularly notable because they were found in comparison with controls who also report cognitive difficulties; like MCS, CFS has also often been compared with major depression (K~zpp et al 1991). The occurrence of attentional deficits in chemically sensitive patients is consistent with the known neuroanatomical links between the olfactory system and frontal cortex (Mesulam 1985; Lorig 1989). Risberg and Ingvar (1973) have shown the greatest changes in regional cerebral blood flow occur in frontal-prefrontal regions of normals during performance of the digit span task; and Mesulam has commented that frontal areas appear to regulate attentional tone. Attention and concentration difficulties consistent with frontal impairments are common in major depression (Gruzelier et al 1988). Conceivably, such cognitive findings in MCS could derive from low level chemical exposures via olfactorylimbic pathways, depression, or both factors. The relative contribution of each factor could range from none to 100%, depending on the individual and the setting. The visual memory dysfunctions in MCS also suggest the possibility of chemical kindling or other chemically induced neuronal dysfunction such as impaired long-term potentiation in the hippocampus (Da Silva et al 1986; Cain 1989; Tilson et al 1990; Gilbert 1992a) of some MCS patients. In the occupational health literature, Rosenstock et al (1991) found that 36 men with a history of acute organophosphate pesticide poisoning were more likely to manifest chronic neuropsychological deficits 2 years after the incident in comparison with normal matched controls. Notably, a number of MCS patients have attributed onset of their conditions to organophosphate exposures (Ashford and Miller 1991). In addition, Kilburn et al (1989) reported that 14 firemen exposed to polychlorinated biphenyls (PCBs) during a transformer fire exhibited worse cognitive performance in memory for stories and visual images and in concentration for digit span backwards and Trails A and B on testing 6 months later, in comparison with matched firemen controls not exposed in the fire. The PCB-exposed firemen also reported significantly more anger, depression, and fatigue, as well as persistent headaches, muscle weakness, and aching joints. Numerous studies in the Scandinavian occupational health lite~:~urehave documented neuropsychological impairments in industrial workers exposed to various chemicals, including toluene, styrene, xylene, trichlorethylene, mixed solvents, paint, and jet fuel (Riihimaki and Savolainen 1980; Flodin et al 1984; kegren and Gamberale 1990). The types of tasks in which the exposed workers show greater deficits than do controls are attention, short-term memory, sensorimotor, and visuoconstructive tests. However, interpretation of much of this research is limited by the retrospective nature of the studies, issues of demographic mismatching between exposed and unexposed worker cohorts, lack of historical exposure data, and lack of direct laboratory challenges with chemicals. Olfactory sensory dysfunction, cognitive impairments, affective symptoms, and somatic discomforts may derive from neuroanatomically proximate structures, but they do not necessarily develop to comparable degrees within the same individual. One group has shown that objective deficits in olfactory stimulus identification per se were not well 226 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 correlated with sere: ity of cognitive deficits in solvent-exposed workers (Schwartz et al 1991). On the other Land, Ryan et al (1988; Morrow et al 1990) have demonstrated that a history of cacosmi:~, the subjective sense of altered olfactory function together with feelings of illness from a chemical odor, predicted poorer performance in solvent-exposed workers on a battery of neu~'opsychological tests. In addition, affective syndromes, which were more common in their" chemically exposed workers than in controls, also correlated poorly with degree of cognitive impairment. Despite finding higher nasal resistances and faster respiratory rates in an MCS group, Doty et al (1988) noted no difference between the MCS patients and normal controls on olfactory sensory function tests. Thus, a history of feeling ill from the odor of chemicals may predict cognitive impairment, but the latter may not correlate with degree of olfactory impairment or degree of affective dysfunction in the same individual. Although exposure levels in solvent-exposed workers, office workers in a sick building, and MCS patients may be quantitatively different, all of these cohorts report cacosmia. A recent Environmental Protection Agency survey of workers in several different Federal office buildings found that approximately 1/3 considered themselves "especially sensitive" to indoor air pollutants (Atmospheric Research and Exposure Assessment Laboratory 1991). In our own research mentioned above (Bell et al 1992b), 2/3 of over 640 college students reported feeling ill whenever they smell one or more of five different environmental chemicals (i.e., pesticide, car exhaust, paint, new carpet, perfume); 28% rated an average of at least three chemicals as causing illness. The most chemically sensitive subgroup also had higher symptom and depression rating scores than did students with the lowest degree of self-rated cacosmia. As in the clinical setting, the most chemically sensitive cohort contained significantly more women than did the nonsensitive cohort. Even after the contribution of depression was controlled as a significant covariate, women overall still had significantly higher cacosmia scores than did men. However, although depression accounted for almost a third of the variance in symptom scores overall, it explained none of the variance in the cacosmia score. The correlation between degree of self-rated illness from chemical odors and depression over the whole sample was extremely weak (r - 0.16). Thus, depression may relate to self-reported severity of symptoms, but not to degree of sensitivity to chemical odors or to objective measures of chemically induced cognitive dysfunction. The student survey findings are remarkably similar to those for patients with MCS, but without the confour~ds from chronic illness, treatments, disability, and litigation. In normal persons, nasal inhalation of room air itself produces changes in the EEG different from those with mouth breathing (Lorig 1989). Laboratory studies with dependent measures highly sensitive to attentional deficits indicate that low level chemical exposures increase arousal levels but disrupt attention, even in normais. Lorig and colleagues have published a series of studies on the effects of several essential oil odorants and of a common perfume constituent, gala×elide. Overall they have found that electrophysiological responses in EEG are greater than perceptual changes noted consciously by normal subjects during odorant exposures. SFeci~,:ally, they observed that (1) the anterior-posterior distribution of beta activity on period analysis differed between subsensory odorants and no odorant conditions even when subjects reported no detection of the presence of a chemical exposure; (2) mood was less happy during exposure to undetected odors as well; (3) undetected levels of galaxolide doubled the amount of time needed to solve a visual search task; and (4) undetected levels of galaxolide produced changes ~n the P200 auditory evoked potentials (Lorig and Schwartz 1988; Lorig et al 1988; Lorig et al 1990; Limbic Kindling and Chemical Sensitivity toOLPSYCHIATRY 199?:32:218-242 227 Lorig et al 1991). Schwartz et al (1992a, b, c) have found that normal adult human subjects of both sexes and various ages show significant increases in topographic EEG alpha blocking during brief exposures to a variety of subsensory olfactory stimuli (e.g., isoamyl acetate, androstenone) as compared with a water control. In addition, Bokina et al (1976) investigated the effects of carbon bisulfide on human subjects; they demonstrated that repeated inhalation of this chemical at subsensory (not consciously detected) levels produced impaired performance of motor coordination tasks. Such findings suggest that extremely low levels of environmental chemicals below conscious awareness may have a significant impact on the behavior of normal humans, especially on arousal levels and attention. It is plausible that some individuals could possess an accentuated responsivity to chemicals (Dory et al 1988). MCS patients have higher levels of resting parietal beta activity on EEG spectral analysis (Staudenmayer and Selner 1990), a nonspecific finding consistent with increased arousal. However, no studies comparing MCS patients and normals on spectral EEG or SPECT scans responses during chemical exposures have been reported. Callender (1991) recently presented a case series of chemically exposed workers with MCS-like features of whom 85% showed SPECT scan abnormalities, especially in the temporal and frontal regions. A recent case report described a patient with acute tetrabromine solvent poisoning who developed chronic affective and cognitive dysfunction (Morrow et al 1991). His PET scan demonstrated decreased glucose uptake in the left amygdala, left superior, and left posterior medial frontal regions, among several sites; topographic EEG showed asymmetric slowing (higher activity in all frequency bands over the left posterior temporal region); and cognitive testing revealed impaired performance on tests of learning and memory, attention, and psychomotor speed. This patient had been misdiagnosed after the initial chemical exposure with major depression without, an organic component. Of note, the diagnosis of somatization disorder provides a label for patients with polysymptomatic somatic syndromes for which traditional medical evaluations provide no etiological explanation (Liskow et ai 1986; Orenstein 1989). Even in somatization disorder--without assessment for chemical sensitivity--brain electrophysiological function is abnormal. One group has examined evoked potentials and regional cerebral blood flow in patients with somatization disorder. They found that the somatization patients had more difficulty with selective attention to relevant versus irrelevant stimuli, showed parallel changes in auditory evoked potentials, and experienced a higher right to left hemisphere blood flow ratio as well as slightly greater posterior to anterior blood flow ratio than did normal controls (James et al 1987). It is unknown whether or not a subset of somatization patients also have MCS with attentional deficits, although Simon et al's (1990) data suggest an overlap. Affective Spectrum Disorder Findings. Dory et al (1988) reported higher Beck Depression Inventory scores in chemically sensitive patients than in normal controls. Simon et al (1990) similarly found higher scores on the SLC-90R depression subscale and greater frequency of history of past depressive disorders and ill-defined medical, complaints for the MCS patients than for occupationally matched controls. Pearson et ai (1983; Rix et al 1984) noted marked symptom overlap between self-reported British food "allergies" and a mixed sample of psychiatric outpatients. Black et al (1990) observed that 39% of MCS patients exhibited major depression or dysthymia versus only 13% of normal controls. Unfortunately, none of these studies used an appropriate control group of chronically medically ill patients with more traditional diagnoses. The prevalence of concomitant 228 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 depression in chronic illnesses overall averages 20%, with a range from 5%-45% in different studies (Katon and Sullivan 1990). A recent report indicates that 65%-71% of depressed persons seen in either general medical or specialty mental health settings concomitantly have any of eight chronic medical diagnoses (e.g., arthritis, hypertension, gastrointestinal disorder) (Wells et al 1991). Thus, depression and somatic preoccupation in MCS patients could be an epiphenomenon of being chronically ill, regardless of etiology. Furthermore, patients in all of the MCS investigations were drawn from selected clinical samples rather than from the general population; if sampling procedures favored selection of the most depressed MCS patients, overestimation of the prevalence of affective illness among chemically sensitive persons could result. At the same time, the phenomenology of the core central nervous system symptoms in many MCS patients involves zffective lability, mixed bipolar-like, depressive, and panic-like pictures. On neurobiolog!cal and behavioral bases, at least one inborn temperamental type, trait shyness, coald be associated with vulnerability to enhanced chemical sensitivity. Children with trait shyness and behavioral inhibition show an inborn psychophysiological pattern of hyperreactivity to nonchemical stimuli. In our student survey above, trait shyness scores accounted for 6% of the variance in cacosmia over the whole sample; differences in levels of depression between cacosmia groups were no longer significant, once shyness was covaried. The psychophysiology of shyness includes distress and avoidance in response to novel stimuli, chronic sympathetic nervous system activation and cortisol elevation, higher ratings of depression and fearfulness, increased parental histories of panic and agorophobia with depressive disorders, and increased personal and familial histories of hay fever (Kagan et al 1987, 1988, 1991; Bell et al 1990; Bell et al 1992c; Biederman et al 1990; Rosenbaum et al 1988). Kagan has previously proposed that extremely shy or behaviorally inhibited individuals have hyperreactive limbic systems (Kagan et al 1987o IORR~ U,~ bases this suggestion, in part, on work in the cat. It has been reported that behaviorally defensive (avoidant, "shy") cats exhibit stronger neuronal firing in the amygdala and ventromedial hypothalamus (cf. "eating center" Bell 1975) than do nondefensive cats (Adamec and Stark-Adamec 1983, 1986; Adamec 1991). Partial kindling of the amygdala increases defensive behaviors in both defensive and nonde~'er~ive eats (Adamec and StarkAdamec 1986). The corticomedial amygdala, which recei~,es olfactory system afferents, also regulates agonistic and social learning behaviors such as fear and avoidance of dominant animals (Luiten et al 1985). Because the amygdala receives heavy input from the olfactory system and exhibits a low threshold for kindling from both environmental chemicals (Bokina et al i976) and from numerous other stimuli (Post et al 1984; Cain 1989; Gilbert 1992a), humans and animals with the neurophysiology and neurochemistry of shyness, i.e., inborn avoidant temperaments, might be expected to have the strongest reactions to environmental chemicals. As in the case of solvent-exposed workers, olfactory detection thresholds may not differentiate cacosmic from noncacosmic shy persons; still, olfactory thresholds are somewhat lower in extremely shy than in extremely outgoing men (Herbener et al 1989). Taken together, the data suggest that before they ever present clinically, a subset of persons who are extremely shy may be at increased risk of feeling ill when they smell common environmental chemicals. This vulnerability may be due in part to an inherent neurophysiological susceptibility to partial kindling by such chemicals. Animal studies in neurotoxicology reviewed below support this hypothesis. Limbic Kindling and Chemical Sensitivity BIOLPSYCHIATRY 1992;32:218-242 229 Animal Studies A large number of industrial chemicals that offgas from home and office building materials or are added to indoor environments have neurotoxic properties, including convulsant and affective dysfunction effects (Gilbert 1992a). Generally, Federal regulations attempt to limit exposure to such agents in the workplace to levels so low that the majority of the working population notice either minor physical or no ill effects (Molhave 1991). However, such standards are based on average healthy workers and often only on men (Parkinson et al 1990). No regulatory agency has addressed a more subtle problem of neurotoxicity--that is, chemical kindling, the capacity of the central nervous system to amplify its responsivity to exogenous stimuli on a lasting basis (Joy 1982; Dager et al 1987; Gilbert 1992a). Notably, kindling produces behavioral changes in primates that are more similar to partial complex than to the grand real seizures seen in lower animals (Gilbert 1992a; Wada and Osawa 1976). Drugs and othe,r agents such as physostigmine, cocaine, lidocaine, glutamate, corticotropin releasing factor, and beta-endorphin call all cause or facilitate amygdala kindling from repeated administrations (Girgis 1981; Post et al 1984; Cain and Coreoran 1985; Weiss et al 1986; Mori and Wada 1987; Cain et al 1988; Gilbert 1988; Gilbert 1992a). More. recent research in neurotoxicology has documented the ability of chlorinated hydrocarbon pesticides such as lindane or dieldrin and other pesticides to induce chemical kindling and potentiate electrical kindling as well (Joy 1982; Joy et al 1983; Gilbert and Mack 1989; Gilbert 1992a,b,c). Joy 0982) has shown that the chlorinated hydrocarbon pesticides intensify synaptic activity of both excitatory and inhibitory pathways by increasing presynaptic neurotransmitter release. Once lindane increases the rate at which electrical kindling develops, subsequent exposures have relatively less effect on the now permanent vulnerability to seizure activity. This observation raises the possibility that illness in MCS resulting from an initial chemical kindling may not always show clearcut relationships to later exposures. Post (1980) has also noted that the timing of exposures to drugs, ethanol, and electrical stimuli is crucial to their effects; continuous exposures favor adaptation whereas intermittent exposures, especially once every 24 hr, facilitate kindling. Both animal and human studies have shown marked variability in the effects of substances such as nitrogen dioxide (Coffin et al 1977) and xylene (Riihimaki and Savolainvn 1980), dependent on exposure schedules, Thus, it is essential to consider time factors in research on kindling in the induction and maintenance of chemical sensitivity as well as in the manifestation of symptoms. Organophosphate pesticides such as satin, which are cholinesterase inhibitors, may also exert lasting effects on electrophysiological activity of the brain in monkeys and humans. Burchfiel and Duffy (1982) injected both single higher and multiple lower doses of the pesticide in monkeys and measured EEG responses twice--the day after the final dose and one year later. The single higher doses (5 Ixg/kg) produced classic acute toxic reactions, but ten lower doses (l Ixg/kg) repeated weekly generated no signs of acute toxicity. Nonetheless, compared with controls receiving vehicle only injections, EEG spectral analysis showed that both high and low dose satin regimens caused significant increases in temporal lobe EEG beta activity at both 1 day and 1 year later. These data suggest the same sensitized outcome from either a single toxic dose or repeated, intermittent subthreshold doses of this pesticide (cf. time-dependent sensitization and kindling). Consistent with individual differences in susceptibility, a subset, but not 230 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 all, of the satin-exposed human workers studied by the same group showed greater amounts of EEG beta activity and increases in rapid-eye movement sleep. In combination with Staudenmayer and Selner's finding of greater parietal beta activity in MCS patients (1990), these findings suggest that certain chemicals could induce permanent changes in EEG activity and associated behaviors in vulnerable individuals. In view of Simon et al's (1990) report that more of the industrial workers who went on to claim chronic problems with MCS after an initial toxic spill had prior psychiatric histories (usually of depr¢ssion, anxiety, or somatizatio~ disorders) than did those without MCS, the data support the notion of interactions between chemical exposures and inherent neurophysiological vulnerabilities to produce MCS, by kindling or by a related neurophysiological mechanism. It should be noted that the present model interprets data from Staudenmayer and Selner (1990), Simon et al (1990), and Black et al (1990) with a more neurobiological emphasis than did the original investigators, most of whom inferred a psychogenic etiology for MCS from the same findings. We refer the reader to the introduction and conclusion sections of this paper for our considerations in reconciling these differing points of view. The ability to cause lasting changes and/or low dose reactivity in nervous system activity may extend beyond pesticides to other environmental chemicals. Earlier Bokina et al (1976) studied the effects of acet¢ne, benzene, ammonia, formaldehyde, and ozone on the electrophysiological responses of the olfactory bulb, corticomedial amygdala, and other brain structures in rabbits. They found that 10-sec chemical exposures to relatively higher doses produced orienting behaviors, increased neocortical activity, and increased respiration rates without changes in olfactory system firing. With 20-rain exposures to lower doses, however, they noted the same chemicals induced a persisting stress rhythm in both cortex and reticular system. When they gave a sequence of an initially higher and then lower concentration of these chemicals, the low doses now triggered epileptoid activity in the olfactory bulb and corticomedial amygOala during concomitant flickering light stimulation. In the latter study, the environmental pollutants differed markedly in structure and chemical properties, but induced similar effects on the central nervous system, paralleling observations in MCS (cf. Egger et al 1985, 1989). Single high doses of other agents, such as corticotropin-releasing factor (CRF), can also trigger kindlinglike seizure activity in the amygdala, whereas repeated CRF doses accelerate onset of electrical kindling (Weiss et al 1986). Limbic structures other than the amygdala are also vulnerable to environmental chemicals. Tilson et al (1990) observed in female rats that a single dose of the organophosphate flame-retardant tris(2-chloroethyl)phosphate (TRCP), which is widely used in synthetic fibers and plastics (over 100,000 pounds manufactured per year), produced acute seizures, permanent damage to hippocampai neurons, and persistent impairment in learni~,g a spatial memory task. Female rats were used in the latter study on the basis of prior evidence that females were more sensitive to hippocampai damage from TRCP than were males (Matthews et al 1990). This effect might overlap both traditional toxicology and kindlingsensitization effects. Some environmental chemicals may exert acute behavioral effects in addition to kindling. For example, acute low levels of lindane produce increases in anxious behaviors that are blocked by gamma aminobuty~c acid (GABA) agonist drugs in a rat model of anxiety (Llorens et al 1990). In addition, low dose dieldrin, a related chlorinated hydrocarbon pesticide, combined wi~ the stress of a learned helplessness footshock paradigm (an animal model of depression--Porsolt et al 1977) to produce task performance deficits Limbic Kindlingand ChemicalSe,si6.vity BXOLPSYCHIATRY 1992;32:218-242 231 not seen with the chemical or the learned helplessness condition alone (Carlson and Rosellini 1987). Escapable shock combined with the dieldrin did not produce comparable performance impairments. The data suggest that acute low ievel chemical exposures might interact with the neurophysiology of the affective state to generate additional behavioral symptomatology in the subset of MCS patients who are already depressed or anxious at the time of a given chemical exposure. On the one hand, these phenomena might occur with neurochemical mechanisms distinct from kindled events. On the other hand, several animal models of depression, including reserpine-induced depletion of catecholamines, physostigmine-induced elevation of acetylcholine, and olfactory bulbectomy, themselves facilitate acquisition of amygdala kindling (Girgis 1986; Jesberger and Richardson 1988; van Riesen and Leonard 1990). Thus, environmental chemicals could act synergistically with the neurochemistry of depression or of strong emotional experience to augment limbic kindling. In this situation, the same limbic neural circuitry would be impacted by two distinct sources that would otherwise have no immediate relationship to each other, that is, environmental chemical effects and depression. Such interactions between different classes of stressors are well-established for TDS (Antelman 1988) and are implicit in Post et al's (1984) model for the course of bipolar disorder. Conclusions Taken together, the human and animal literature suggests that MCS could be a multifactorial, unanticipated field experiment on susceptible human subjects demonstrating the ability of low levels of environmental chemicals to alter central nervous system activity, behavior, and associated physiological functions. Both persons with predisposed nervous systems, such as those with genetic loading for affective spectrum disorders, and normals can show adverse ,;entral nervous system effects of chemicals, but the former may be more apt to be kindled by lower exposure levels. The higher levels encountered in some industrial and occasional nonindustrial exposures may affect individuals who were neuropsychiatrically and neurophysiologically normal at baseline. Lower level chemical ex. posures would produce only functional kindled lesions, whereas higher levels cot:!d cause both structural and functional lesions in the limbic system. If partial limbic kindling ~ underlies MCS, the resultant electrophysiological lesion may become permanent and ultimately independent of further cumulative exposure to chemicals. In parallel with the nature of kindling, the present model would apply best to patients in whom a major chemical exposure event preceding a marked decrement in health can be identified. The original exposure need not have persisted, once the presumptive kindling process was mobilized. Thereafter, lower levels of chemicals should be capable of eliciting neurobiological dysfunction. These hypotheses further imply that objective laboratory tests for the hypothesized central nervous system dysfunctions in MCS are available. The neuroscience tools that have already proved useful in this research may also prove valuable for clinical diagnosis. These include spectral and period analysis of EEG (Benignus 1984; Lorig 1989), topographic EEG (Morrow et al 1991), auditory evoked potentials (Lorig 1989), all-night sleep recordings (Burchfiel and Duffy 1982), functional brain imaging scans (Morrow et al 1991; Callender 1991), and neuropsychological tests for attention, concentration, and memory (Ryan et al 1988; Kipen and Fielder 1991; Kjaergaard et al 1991; Rosenstock et al 1991). To reconstruct the remainder of the clinical presentation, psychological complications that can influence limbic function such as low sens~ of control over life stressors (cf. learned helplessness) and/or affectively charged psychological 232 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 trauma (Morrow et al 1989) can be evaluated. For example, animal behavioral studies indicate that a low sense of control over stress, perhaps including preexisting depression, may interact with acute chemical exposures to increase performance deficits over those from the depression alone (Carlson and Rosellini 1987). Psychological versus Biological Issues in MCS Although proponents and detractors of MCS present their arguments in either purely biological or purely psychogenic terms, the human and animal data suggest the likelihood that exogenous chemical exposures, genotype, gender, and psychosocial factors interact to produce the clinical phenomena (Schwartz 1981, 1982). The relative contribution of each factor in individual cases may range widely. The most important psychological factors may be (a) perception of inescapable stress either from other life circumstances or from the chronic illness itself, and (b) the novelty or unfamiliarity of the setting in which chemical exposures occur. Numerous animal and human studies have shown that inescapable stress and unfamiliar environments interact with drugs and other chemical exposures to accentuate adverse effects beyond those from the agent alone; endpoints range from more severe panic attacks in humans to greater tumor growth or even more drug-induced deaths in animals (Sklar and Anisman 1979; Natelson et al 1980; Natelson and Cagin 1981; Siegel et al 1982; Sanderson et a1 1989; Kiecolt-Glaser and Glaser 1991). Depressed patients who perceive themselves as helpless or extremely shy persons who react with fear to novel stimuli would be prime candidates for such biopsychosoeial interactions. Novelty, foreignness, and perceived threat are key properties of stimuli that can induce time-dependent sensitization to a wide range of stressors, including psychological (e,g., shock, needle jab, immobilization) and pharmacological (e.g. ethanol, amphetamine, clonidine, amitriptyline, haloperidol, diazepam, estrogen, immunosuppressants) factors; and, as noted above, several studies have demonstrated cross-sensitization between different classes of stressor (Antelman 1988). Thus, the nature of sensitization means that a previous acute toxic chemical exposure or an emotionally traumatic event could initiate or increase vulnerability to MCS (of. Black et al 1990). Thereafter, low-level chemicals might cross-sensitize and produce symptoms to differing degrees, depending on the individual. Conditioning factors must be considered as well (Wood 1978; Russell et al 1984). Bolla-Wilson et al (1988) have previously postulated that these play a role in some adverse chemical reactions; Post et al (1984) have also suggested conditioning factors in an interplay with kindling and sensitization phenomena in the longitudinal course of affective disorders. However, even in classical conditioning, the initial unconditioned stimulus must be capable of inducing a biological response that can then pair with the biologically inactive conditioned stimulus. Furthermore, a conditioned response is not always a reliable replication of the biologically induced response. As with drugs such as insulin, atropine, and ethanol, conditioned reactions to some environmental chemicals could manifest opposite in d~rection to the direct biological effects (unconditioned responses) of the chemicals. For example, although high-dose ethanol biologically causes a decrease in body temperature, the conditioned response is an increase in body temperature (Eikelboom and Stewart 1982). Contrary to inferences by certain skeptics of MCS (Selner 1988), the ability to treat the clinical phenomenology of a multifactorial illness with a psychological approach Limbic Kindling and Chemical Sensitivity BIOLPSYCHIATRY 1992~32:218-242 233 neither proves nor disproves the role of biology or psychology in the etiology of the illness (Post et al 1984; Schwartz 1981, 1982). Post et al (1984) have pointed out that interventions with cognitive-behavioral desensitization may be useful for the psychological treatment component of clinical care in kindled individuals, in part because neurobiological events in the brain mediate psychosociai experiences (Figure 1). Biological and psychosociai factors coexist in all clinical disorders, regardless of the medical or psychiatric realm in which the diagnosis may fall (Schwartz 1981, 1982). Therefore, a history of early childhood abuse, previous depression, or the presence of some classically conditioned and even misattributed chemical reactions (Selner 1988) in no way rules out a major contribution of environmental chemical kindling of the limbic system to the etiology of MCS. Similar limbic cross-reactivity on a neurochemical basis (e.g. excitatory amino acids) between strong affective experiences and environmental chemical kindlingsensitization is quite feasible (cf. Carlson and Rosellini 1987). Gender Differences Had MCS patients not already been identified, the neurotoxicology, psychopharmacology, and psychophysiology literatures suggest that MCS ought to exist, and that biological psychiatrists ought to be ale~ to the possibility that there may be individuals whose illnesses involve both environmental chemical initiation and perpetuation of overt symptomatology. Useful history in such cases might include the timing and circumstances of illness onset in relationship to concomitant chemical exposures at home or work. Examination of gender differences in chemical susceptibility may also prove important, given (a) our data in normals (Bell et al 1992b) and that of Molhave's group in SBS patients (Molhave et al 1991) suggesting that women may be more cacosmic than their male peers; (b) neurotoxicology studies finding female rats more vulnerable than males to hippocampal damage frora at least one common organophosphate, TRCP (Tilson et al 1990); (c) evidence demonstrating that women have lower olfactory detection and identification thresholds than men across the lifespan (prepubertal through postmenopausal ages) and that seizure threshc, ld~ may vary in parallel with olfactory thresholds (Doty et ai 1984; Dory 1986); (d) ba~;ic studies finding female and castrated male rats more susceptible than intact males to time-dependent sensitization from both drug and nondrug stressors (Robinson and Becker !986; Antel,nan 1988). The reasons for such gender differences are not clear, but are likely to be multifactorial. In the first place, chemical kindling tends to occur for substances that are convuisants (Gilbert 1992a,b,c). It follows that persons with lower seizure thresholds might be more readily kindled when they encounter such chemicals. Estrogen, but not testosterone, lowers seizure threshold in numerous species (Newmark and Penry 1980). In addition, other endocrine factors such as elevated adrenocorticotropic hormone (ACTH) or cortisol, stimulated by estrogen or a variety of other stressors, appear to contribute to gender differences in olfactory thresholds (Doty et al 1981; Dory 1986). Testosterone may attenuate pituitary-adrenal responsivity (Robinson and Becker 1986). Furthermore, TDS occurs more readily in both intact females and castrated males in comparison with intact males (Kalivas and Barnes 1988). Athough ovariectomy causes little change in sensitization of adult females, removal of the testes accentuates sensitization in male animals (Robinson and Becket 1986). Thus, testosterone or another testicular hormone may protect males against sensitization processes (Robinson and Becker 1986). Similar hormonal factors might be involved in cacosmia and/or MCS as well. 234 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 Testing the Model The current model lends itself readily to testing in animal models drawn from previous toxicology research in which both biological and psychological variables, as well as time and dose factors, can be systematically manipulated to assess their relative contributions to changes in electrophysiology, functional brain imaging, behavioral measures, and task performance from baseline. The triggering ability of solvents and pesticides at dose levels comparable to those implicated by MCS patients in the initiation of their illness can be tested in animals with chemical kindling (Joy 1982) and TDS (Antelman et al 1991) protocols; both behavior and electrophysiological activity in limbic neurons during subsequent low-dose exposures can be measured. Because animal models for anxiety (e.g., plus-maze performance [Llorens et al 1990]), depression (e.g., inescapable stress; re. :;erpine; olfactory bulbectomy [Jesberger and Richardson 1988]), and avoidance behaviors (Adamec 1991) exist, it should be feasible to perform tests of environmental chemical kindling and/or time-dependent sensitization in combination with these preparations as well. Ethical considerations would preclude experimental attempts to induce chemical kindling in patients or normals. Tests of the kindling hypothesis in existing MCS patients may he indirect and limited to (a) PET and SPECT imaging and surface electrophysiological studies as well as cognitive tests during double-blind low-dose chemical exposures at different points in their illnesses; (b) studies of long-term clinical course in MCS, looking for an acceleration of frequency and severity of chemical reactions with increasingly lower chemical doses necessary to trigger reactions over time, similar to that described by Post et al (1984) in their kindling model of bipolar disorder; (c) doubleblind, placebo-controlled clinical trials of antikindling or anticonvulsant drugs such as cionidine, valproic acid, or carbamazepine (Sate et al 1990) in MCS patients. The latter protocol may require creative solutions to the generalized intolerance of medications that MCS patients often report, for example, avoiding synthetic capsule dyes or even administering the medication and placebo treatment on a time-dependent sensitization schedule of once a week (Antelman 1988; Antelman et al 1987) rather than daily, to amplify the antikindling effects but avoid a crescendo of side effects and resultant noncompliance. Furthermore, case-control, prospective studies of workers new to a particular industry or a particular tight building and of homeowners new to pesticide treatment of their homes might permit identification of risk factors in initiation of MCS cases. This approach would allow assessment of premorbid medical, psychiatric, and social histories, as well as repeated air samplc measurements of the test environment and PET or SPECT brain imaging, spectral and/or topographic EEG, neuropsychological batteries, and self-report measures of biopsychosocial stressors in the cases and controls at baseline and at regular intervals (e.g., 1-3 months for 1-3 years) after starting the job or treating the home. Additional clinical studies might include chemical test exposures using identical doses at baseline and follow-up evaluations, with levels typical of customary indoor air, but well below those that might initiate MCS (Ashford and Miller 1991). Acute reactivity to the test doses could be assessed with PET, spectral EEG, and autonomic monitoring during nose versus mouth breathing. Individuals kindled or sensitized by their work or home exposures would be expected to show progressively stronger objective and subjective responses, including affective lability, to the same low-test doses over time as compared with nonkindled persons. Furthermore, nasal, as opposed to mouth, inhalation of chemicals should activate abnormal EEG and/or brain metabolic patterns more readily in Limbic Kindling and Chemical Sensitivity etOLPSYCHIATRY 1992;32:218-242 235 sensitized individuals. Proper experimental designs to elicit kindling or sensitization may require (a) use of repeated, intermittent, rather than one-time or continuous, chemical exposures; and (b) careful attention to use of familiar versus unfamiliar settings for testing in view of the context-dependence versus independence of TDS, a feature which relates to dose size and number of sensitizing exposures (Kalivas and Barnes 1988). In conclusion, it was an allergist who first observed patients with MCS forty years ago and later emphasized the phenomenology of altered reactivity and the role of time factors as core features of the syndrome (Randolph 1970, 1974, 1978). However, with the dicovery of immunoglobulin E in 1967 and the corresponding redefinition of allergy in immunologic terms, certain groups have emphasized that evidence does not support an immunologic basis for MCS (California Medical Association 1986; Terr 1986). On the one hand, several studies have shown a higher prevalence of atopic allergies (Nasr et ai 1981; Matussek et al 1983; Bell et al 1991), immediate skin test reactivity (Ossofsky 1976), and/or elevated antibody titers to foods and pollens (Sugerman et al 1982) in depression per se. No compelling hypothesis has emerged to relate atopy and depression causally, other than cholinergic (Marshall 1989) or perhaps beta-endorphin factors (Bell 1992b). On the other hand, regardless of the presence or absence of atopy, limbic kindling offers a plausible, data-based hypothesis for heightened reactivity to low levels of environmental chemicals in MCS patients and for the apparent overlaps between MCS and a subset of affective spectrum disorders. Extensive clinical and basic research to test this hypothesis is now needed. References Adamec RE (1990): Does kindling model anything clinically relevant? Biol Psychiawy 27:249279. AdamecRE (1991): individualdifferences in temporallobe sensoryprocessingof threatening stimuli in the cat. Physiol Behav 49:455-464. Adamec RE, Stark-Adamec C (1983): Limbic kindling and animal behavior--implications for human psychopathologyassociated with complex partial seizures. Biol Psychiatry 18:269-293. Adamec RE, Stark-AdamecC (1986): Limbic hypeffunction, limbic epilepsy, and interictal behavior. In Doane BK, Livingston KE (eds), The Limbic System. Functional Organization and Clinical Disorders. New York: Raven Press, pp 129-145. Antelman SM (1988): Time-dependent sensitization as the cornerstone for a new approach to pharmacotherapy: drugs as foreign/stressfulstimuli. Drug Dev Res 14:1-30. Antelman SM, Caggiula AR, Kocan D, et al (1991): One experience with 'lower' or 'higher' intensitystressors respectivelyenhances or diminishesresponsivenessto haloperidolweeks later: implications for understandingdrug variability. Brain Res 566:276-283. Antelman SM, Cunnick JE, Lysle DT, et al (1990): Immobilization 12 days (but not one hour) earlier enhanced 2-deoxy-d-glucose-inducedimmunosuppression:Evidencefor stressor-induced time-dependent sensitization of the immune system. Prog Neuropsychopharmacol Biol Psychiatry 14:579-590. Antelman SM, Kocan D, Edwards DJ, Knopf S (1987): A single injection of diazepam induces long-lasting sensitization. Psychopharmacol Bull 23:430-434. Ashford NA, Miller CS (1991): Chemical Exposures. Low Levels and High Stakes. New York: Van Nostrand Reinhold. AtmosphericResearchand Exposure AssessmentLaboratory, US EnvironmentalProtection Agency (June, 1991): Indoor air quality and work environmentstudy: EPA headquarters buildings. Vol. IV. Multivariatestatistical analysis of health, comfort, and odor perceptionsas related to personal and workplace characteristics. Administrationand Resources ManagementPM-273, 21M-3004. 236 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 Bell IR (1975): A kinin model of mediation for food and chemical sensitivities: biobehavioral implications. Ann Allergy 35:206-215. Bell IR (1982): Clinical Ecology. A New Medical Approach to Environmental Illness. Bolinas, CA: Common Knowledge Press. Bell IR (1987): Environmental illness and health: The controversy and challenge of clinical ecology for mind-body health. Advances: J lnstit Advancement Health 4(3):45-55. Bell IR (1992a): Neuropsychiatric and biopsychosocial mechanisms in multiple chemical sensitivity: An olfactory-limbic system model. In National Research Council Report: Multiple Chemical Sensitivities. Addendum to Biologic Markers in immunotoxicology. Washington, De: National Academy Press, pp 89-108. Bell IR (1992b): Allergens, physical irritants, depression, and shyness. J Appl Dev Psycho113:125133. Bell IR, Jasnoski ML, Kagan J, King DS (1990): Is allergic rhinitis more frequent in young adults with extreme shyness? A preliminary survey. Psychosom Med 52:517-525. Bell IR, Jasnoski ML, Kagan J, King DS (1991): Depression and allergies: survey of a nonclinical population. Psychother Psychosom 55:24-31. Bell IR, Markley EJ, King DS, et al (1992a): Polysymptomatic syndromes and autonomic reactivity in individuals with self-reported adverse food reactions. Submitted for publication. Bell IR, Schwartz GE, Peterson JM, Amend D (1992b): Self-reported illness from chemical odors in young adults without clinical syndromes or occupational exposures. Arch Envir Health, in press. Bell IR, Martino GM, Meredith KE, Schwartz (3E, Siani MM, Morrow FD (1992c): Vascular disease risk factors, urinary free cortisol, and health histories in older adults: shyness and gender interactions. Biol Psychol, in press, Benignus VA (I 984): EEG as a cross species indicator of neurotoxicity. Neurobehav Toxicol Teratol 6:473-483. Biederman J, Rosenbaum .IF, Hirshfeld DR, et al (1990): Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Arch Gen Psy. chiatry 47:21-26, Black DW, Rathe A, Gold~,.teinRB (1990): Environmental illness. A controlled study of 26 subjects with '20th century disease'. JAMA 264:3166-3170. Bokina AI, Eksler ND, Semenenko AD, Merkuryeva RV (1976): Investigation of the mechanism of action of atmospheric pollutants on the central nervous system and comparative evaluation of methods of study. Environ Health Perspect 13:37-42. Bolla-Wilson K, Wilson R, Blceckcr ML (1988): Conditioning of physical symptoms after neurotoxic exposure. J Occup Med 30:684--686. Boyles JH (1985): Chemical sensitivity. Diagnosis and treatment. Otolaryngol Ciin North Am 18:787-795. Brodsky CM (1983): 'Allergic to everything': a medical subculture. Psychosomatics 24:731-742. Burchfiel JL, Duffy FH (1982): Organophosphate neurotoxicity: Chronic effects of sarin on the electroencephalogram of monkey and man. Neurobehav Toxicol Teratol 4:767-778. Cain DP (1974): The rele of the olfactory bulb in limbic mechanisms. Psychol Bull 8 i :654-67 I. Cain DP (1989): Long-term potentiation and kindling: how similar are the mechanisms? Trends Neurosci 12:6--10. Cain DP, Corcoran ME ( 1985): Epileptiform effects of met-enkephalin, B-endorphin, and morphine: kindling of generalized seizures and potentiation of epileptiform effects by handling. Brain Res 338:32'7-336. Cain DP, Desborough KA, McKitrick DJ (1988): Retardation of amygdala kindling by antagonism of NMD-aspartate and muscarinic cholinergic receptors: Evidence for the summation of excitatory mechanisms in kindling. Exp Neurol 100:179-187. California Medical Association Scientific Board Task Force on Clinical Ecology (1986): Clinical ecology--a critical appraisal. West J Med 144:239-245. Limbic Kindling and Chemical Sensitivity BIOLPSYCHIATRY 1992;32:218-242 237 Callender TJ (1991): Metabolic brain imaging abnormalities in chemically exposed individuals who developed multiple chemical sensitivity syndrome or chronic fatigue syndrome. Presented at the 119th Annual Meeting of the American Public Health Association, Atlanta, Georgia, November 10o14, 1991. Carlson JN0 RoseUini RA (1987): Exposure to low doses of the environmental chemical dieldrin causes behavioral deficits in animals prevented from coping with stress. Psychopharmacology 91:122-126. Catapano F, Galderisi S (1990): Depression and cerebral stroke. J Clin Psychiatry 51 (9 Suppl):912. Chang YS, Yamada Y, Yeh HC, Swift D (1988): Diffusional deposition of ultrafine aerosols in a human nasal cast. J Aerosol Sci 19:741-751. Coffin DL, Gardner DE, Sidorenko GI, Pinigin MA (1977): Role of time as a factor in the toxicity of chemical compounds in intermittent and continuous exposures. Part I1. Effects of intermittent exposure. J Toxicol Environ Health 3:821-828. Crayton JW, Stone T, Stein G (1981): Epilepsy precipitated by food sensitivity: report of a case with double-blind placebo-controlled assessment. Clin Electroencephalogr 12:192-197. Dager SR, Holland JP, Cowley DS, Dunner DL (1987): Panic disorder precipitated by exposure to organic solvents in the work place. Am J Psychiatry 144:i056-1058. DaSilva FHL, Goiter JA, Wadman WJ (1986): Kindling of the hippocampus induces spatial memory deficits in the rat. Neurosci Len 63:115-120. Davidoff LL (1991): Multiple chemical sensitivities: Research on psychiatric/psychosocial issues. Presented at the 119th Annual Meeting of the American Public Health Association, Atlanta, Georgia, November 10-14, 1991. Davidoff LL, Callender TJ, Morrow LS, Ziem G (1991): Letters to editor re Staudenmayer and Selner (below). J Psychosom Res 35: !-3. Doty RL (1986): Gender and endocrine-related influeaces on human olfactory perception. In Meiselman HL, Rivlin RS (eds), Clinical Measurement of Taste and Smell. New York: MacMillar, pp 377-413. Doty RL, Snyder PJ, Huggins GR, Lowry LD (! 98 I): Endocrine, cardiovascular, and psychological correlates of olfactory sensitivity changes during t.~e human menstrual cycle. J Comp Physiol Psychol 95:45-60. Doty RL, Shaman P, Applebaum SL, Giberson R, Siksorski L, Rosenberg L (1984): Smell identification ability: Changes with age. Science 226:!441-1443. Dory RL, Deems DA, Frye RE, Pelberg R, Shapiro A (1988): Olfactory sensitivity, nasal resistance, and autonomic function in patients with multiple chemical sensitivities. Arch Otolaryngol Head Neck Surg 114:1422-1427. Egger J, Carter CM, Wilson J, Turner MW, Soothill JF (1983): Is migraine a food allergy? Lancet 2:865-869. Egger J, Carter CM, Graham PJ, Gumley D, Soothill JF (1985): Controlled trial of oligoantigenic treatment in the hyperkinetic syndrome. Lancet 1:5400545. Egger J, Carter CM, Soothill .IF, Wilson J (1989): Oligoantigenic diet treatment of children with epilepsy and migraine. J Pediatr 114:51-58. Ehmann TS, Beninger RJ, Gawel MJ, Riopelle RJ (1989): Depressive symptoms in Parkinson's disease: A comparison with disabled control subjects. J Geriatr Psychiatry Neurol 2:3-9. Eikelboom R, Stewart J (1982): Conditioning of drug-induced physiological responses. Psychol Rev 89:507-528. Flodin U, Edling C, Axelson O (1984): Clinical studies of psychoorganic syndromes among workers with exposure to solvents. Am J Indust Med 5:287-295. Ghantous H, Dencker L, Gabrielsson J, Danielsson BRG, Bergman K (1990): Accumulation and turnover of metabolites of toluene and xylene in nasal mucosa and olfactory bulb in the mouse. Pharmacol Toxicol 66:87-92. Gilbert ME (1988): The NMDA-receptor antagonist, MK-801, suppresses limbic kindling and kindled seizures. Brain Res 463:90-99. Gilbert ME (1992a): Neurotoxicants and limbic kindling. In lsaacson RL, Jensen KF (eds), The 238 BIOL PSYCHIATRY I.R. Bell et al 1992;32:218-242 Vulnerable Brain and Environmental Risks. Vo!. 1: Malnutrition and Hazard Assessment. New York: Plenum, in press. Gilbert ME(1992b): Proconvulsant activity of endosulfan in amygdala kindling. Neurotoxicol Teratol 14:143-149. Gilbert ME (t992c): A characterization of chemical kindling with the pesticide endosulfan. Neurotoxicol Teratol 14:151-158. Gilbert ME, Mack CM (1989): Enhanced susceptibility to kindling by chlordimeform may be mediated by a local anesthetic action. Psychopharmacology 99:163-167. Girgis M ( 198 I): Elect¢ al versus cholinergic kindling. Electroenceph Clin Neurophysiol 5 ! :417425, Girgis M (1986): Biochemical patterns in limbic system circuitry: biochemical-electrophysiological interactions displayed by chemitrode techniques. In Doane BK, Livingston KE (eds), The Limbic System: Functional Organization and Clinical Disorders. New York: Raven Press,.pp 55--65. Gruzclier J, Seymour K, Wilson L, Jolley A, Hirsch S (1988): Impairments on neuropsychologie tests of temporohippocampal and frontohippocampal functions and word fluency in remitting schizophrenia and affective disorders. Arch Gen Psychiatry 45:623-629. Hastings L, Evans JE (1991): Olfactory primary neurons as a route of entry for toxic agents into the CNS. Neurotoxicology 12:707-714. Herbener ES, Kagan J, Cohen M (1989): Shyness and olfactory threshold. Person Individ Diff 10:1159-1163. Huang YY, Colino A, Selig DK, Malenka RC (1992): The influence of prior synaptic activity on the induction of long-term potentiation. Science 255:730-733. Hudson Jl, Pope HG (1990): Affective spectrum disorder: does antidepressant response identify a family of disorders with a common pathophysiology? Am J Psychiatry 147:552-564. Iregren A, Gamberalc F (1990): Human behavioral toxicology. Central nervous effects of low-dose exposure to neurotoxic substances in the work environment. Scand J Work Environ Health 16(Suppl I): 17-25. James L, Singer A, Zurynski Y, et al (1987): Evoked response potentials and regional cerebral blood flow in somatization disorder. Psychother Psychosom 47:190-196. Jesberger JA, Richardson JS (1988): Brain output dysregulation induced by olfactory bulbectomy: An approximation in the rat of major depressive disorder in humans. IntJ Neurosci 1988;38:241265. Jewett DL, Fein 13, 13reenberg MH (1990): A double-blind study of symptom provocation to determine food sensitivity. N Engl J Med 323:429-433. Jones VA, McLaughlan P, Shorthouse M, Workman E, Hunter JO (1982): Food intolerance: a major factor in the pathogenesis of irritable bowel syndrome. Lancet 2:1115-1117. Joy RM (1982): Mode of action of lindane, dieldrin, and related insecticides in the central nervous system, Neurobehav Toxicol Teratol 4:813-823. Joy RM, Stark LG, Albertson TE (1983): Proconvulsant actions of lindane: Effects on afterdischarge thresholds and durations during amygdaloid kindling in rats. Neurotoxicology 4:211-220. Kagan J, Reznick JS, Snidman N (1987): The physiology and psychology of behavioral inhibition in children. Child Dev 58:1459-1473. Kagan J, Reznick JS, Snidman N ( 1988): Biological bases of childhood shyness. Science 240:167171, Kagan J, Snidman N, Julia-SellersM, Johnson M O O991): Temperament and allergicsymptoms, Psychosom Med 53:332-340, Kalivas PW, Barnes CD (eds) (1988): Sensitization in the Nervous System. Caldwell, NJ: Telford Press, Kaplan BJ, McNicol J, Conte RA, Moghadam HK (1989): Dietary replacement in preschool-aged hyperactive boys, Pediatrics 83:7-17. Limbic Kindling and Chemical Sensitivity BIOLPSYCHIATRY 1992;32:218-242 239 Katon W, Sullivan MD (1990): Depression and chronic medical illness. J Clin Psychiatry 51(6, Suppl):3-1 I. Kiecolt-Glaser J. Glaser R (1991): Stress and immune function in humans. In Ader R (ed), Psychoneuroimmunology, 2nd ed. New York: Academic Press, pp 849-867. Kilbum KH, Warsaw RH, Shields MG (1989): Neurobehavioral dysfunction in firemen exposed to polychlorinated biphenyls (PCBs): possible improvement after detoxification. Arch Environ Health 44:345-350. King DS (1988): The reliability and validity of provocative food testing: A critical review. Med Hypotheses 25:7-16. Kipen HM, Fiedler N (199 I): Psychological and immunological evaluation of patients with multiple chemical sensitivities. Presented at the 119th Annual Meeting of the American Public Health Association, Atlanta, Georgia, November 10-14, 1991. Kjaergaatd SK, Molhave L, Pedersen OF (1991): Human reactions to a mixture of indoor air volatile organic compounds. Atmospheric Environ 25A: 1417-1426. Kreiss K (1989): The epidemiology of building-related complaints and illness. Occup Med 4:575592, Krupp LB, Mendelson WB, Friedman R (1991): An overview of chronic fatigue syndrome. J Clin Psychiatry 52:403-410. Liskow B, Othmer E, Penick EC, DeSouza D, Gabrielli W (1986): Is Briquet's syndrome a heterogeneous disorder? Am J Psychiauy 143:626-629. Little CH, Stewart AG, Fennessy MR (1983): Platelet serotonin release in rheumatoid arthritis: A study in food-intolerant patients. Lancet 2:297-299. Llorens J, Tusell JM, Sunol C, Rodriguez-Farre E (1990): O~ the effects of lindane on the plusm~ze model of anxiety. Neurotoxicol Teratol 12:643-647. Lorig TS (1989): Human EEG and odor response. Prog Neurobiol 33:387-398. Lorig "iS, Schwartz GE (1988): Brain and odor: I. Alteration of human EEG by odor administration. Psychobiology 16:281-284. Lorig TS, Schwartz GE, Herman KB, Lane RD (1988): Brain and odor I1. EEG activity during nose and mouth breathing. Psychobiology 16:285-287. Lorig "IS, Herman KB, Schwartz GE (1990): EEG activity during administration of low-concentration odors. Bull Psychosom Soc 28:405-408. Lorig TS, Huffman E, DeMartino A, DeMarco J (1991): The effects of low concentration odors on EEG activity and behavior. J Psychophysiol 5:69-77. Luiten PGM, Koolhaas JM, deBoer S, Koopmans SJ (1985): The cortico-medial amygdala in the central nervous system organization of agonistic behavior. Brain Res 332:283-297. Marshall P (1989): Attention deficit disorder and allergy: A neurochemical model of the relation between the illnesses. Psychol Bull 106:434-446. Matthews HB, Dixon D, Herr DW, Tilson HA (1990): Subchronic toxicity studies indicate that ttis(2-chloroethyl)phosphate administration results in lesions in the rat hippocampus. Toxicol lndust Health 6:1-15. Matussek P, Agerer D, Seibt G (1983): Allergic disorders in depressive patients. Compr Psychiatry 24:25-34. Mesulam MM (1985): Principles of Behavioral Neurology. Philadelphia: FA Davis. Molhave L (1991): Indoor climate, air pollution, and human comfort. J Expos Anal Environ Epidemiol 1:63-81. Molhave L, Bach B, Pedersen OF (1986): Human reactions to low concentrations of volatile organic compounds. Environ lnt 12:167-175. Mohave L, Jensen JG, Larsen S (1991): Subjective reactions to volatile organic compounds as air pollutants. Atmos Environ 25A: 1283-1293. Mori N, Wada JA (1987): Bidirectional transfer between kindling induced by excitatory amino acids and electrical stimulation. Brain Res 425:45-48. Morrow LA, Ryan CM, Goldstein G, Hodgson MJ (1989): A distinct pattern of personality disturbance following exposure to mixtures of organic solvents. J Occup Med 31:743-746. 240 BIOLPSYCHIATRY I.R. Bell et al 1992;32:218-242 Morrow LA, Ryan CM, Hodgson MJ, Robin N (1990): Alterations in cognitive and psychological functioning after organic solvent exposure. J Occup Med 32:444-450. Morrow LA, Callender TJ, Lottenberg S, Buchsbaum MS, Hodgson MJ, Robin N (1991): PET and neurobehavioral evidence of tetrahromine encephalopathy. J Neuropsychiatry Clin Neurosci 2:431-435. Nasr S, Altman EG, Meltzer HY (1981): Concordance of atopic and affective disorders. JAffective Disord 3:291-296. Natelson BH, Cagin NA (1981): The role of shock predictability during aversive conditioning in producing psychosomatic digitalis toxicity. Psychosom Med 43:191-197. Natelson BH, Hoffman SL, Cagin NA (1980): A role for environmental factors in the production of digitalis toxicity. Pharmacol Biochem Behav 12:235-237. Newmark ME, Penry JK (1980): Catamenial epilepsy: A review. Epilepsia 21:281-300. Orenstein H (1989): Briquet's syndrome in association with depression and panic: A reconceptualization of Briquet's syndrome. Am J Psychiatry 146:334-338. Ossofsky JH (1976): Affective and atopic disorders and cyclic AMP. Compr Psychiatry 17:335346. Parkinson DK, Bromet EJ, Cohen S, Dunn LO, Dew MA, Ryan C, Schwartz JE (1990): Health effects of long-term solvent exposure among women in blue-collar occupations. Am J Indust Med 17:661-675. Parmclee PA, Katz IR, Lawton MP (1991): The relation of pain to depression among institutionalized aged. J Gerontol 46:P13-21. Pearson DJ, Rix KJB, Ber,tley SJ (1983): Food allergy: how much in the mind? A clinical and psychiatric study of suspected food hypersensitivity. Lancet 1:1259-1261. Perl DP, Good PF (1987): Uptake of aluminum into central nervous system along nasal-olfactory pathways. Lancet 1:1028. Porsolt RD, LePichon M, Jalfre M (1977): Depression: a new animal model sensitive to antidepressant treatment. Nature 206:730-732. Post RM (1980): Minirevicw. Intermittent versus continuous stimulation: Effect of time interval on the development of sensitization or tolerance, Life Sci 26:1275-1282. Post RM, Rubinow DR, Ballenger JC (1984): Conditioning, sensitization, and kindling: Implications for the course of affective illness, in Post R, Ballenger.l (eds), Neurobiology of Mood Disorders. Baltimore: Williams and Wilkins, pp 432-466. Randolph TG (1970): Domiciliary chemical air pollution in the etiology of ecologic mental illness. lnt J Soc Psychiatry 16:243-265. Randolph TG (1974): The history of ecologic mental illness. In Frazier CA (ed), Annual Review of Allergy 1973. Flushing, NY: Medical Exam. Pub. Co. Randolph TG (1978): Specilic adaptation. Ann Allergy 40:333-345. Rea WJ (1977): Environmentally-triggered small vessel vasculitis. Ann Allergy 38:245-251. Rea WJ (1978): Environmentally-triggered cardiac disease. Ann Allergy 40:243-251. Riihimaki V, Savolainen K (1980): Human exposure to m-xylene, Kinetics and acute effects on the central nervous system. Ann Occup Hyg 23:411-422. Risberg J, lngvar DH ( 1973): Patterns of activation in the grey matter of the dominant hemisphere during memorizing and reasoning---a study of regional cerebral blood flow changes during psychological testing in a greup of neurologically normal patients. Brain 96:737-756. Rix KJB, Pearson DJ, Bentley SJ (1984): A psychiatric study of patients with supposed food allergy. Br J Psychiatry 145:121-126. Robinson TE, Becker JB (1986): Enduring changes in brain and behavior produced by chronic amphetamine administration: a review and evaluation of animal models of amphetamine psychosis. Brain Res Rev 11:157-198. Limbic Kindling and Chemical Sensitivity BIOL PSYCHIATRY 1992;32:218-242 241 Rosenbaum JF, Biederman J, Gersten M, et al (1988): Behavioral inhibition in children of parents with panic disorder and agoraphobia: a controlled study. Arch Gen Psychiatry 45:463-470. Rosenberg SJ, Freedman MR, Schmaling KB, Rose C (1990): Personality styles of patients asserting environmental illness. J Occup Med 32:678-681. Rosenstock L, Keifer M, Daniell WE, McConnell R, Claypoole K (1991): Chronic central nervous system effects of acute organophosphate pesticide intoxication. Lancet 338:223-227. Rosenthal NE, Cameron CL (1991): Exaggerated sensitivity to an organophosphate pesticide. Am J Psychiatry 148:270. Rowe AH (1950): Allergic toxemia and fatigue. Ann Allergy 8:72-79,84. Russell M, Dark KA, Cummins RW, Ellman G, Callaway E, Peeke HVS (1984): Learned histamine release. Science 225:733-734. Ryan CM, Morrow LA, Hodgson M. (1988): Cacosmia and neurobehavioraldysfunction associated with occupational exposure to mixtures of organic solvents. Am J Psychiatry 145:1442-1445. Sanderson WC, Rapee RM, Barlow DH (1989): The influence of an illusion of control on panic attacks induced via inhalationof 5.5% carbon dioxide-enrichedair. Arch Gen Psychiatry 46:157162. Sato M, Racine RJ, Mclntyre DC (1990): Kindling: basic mechanisms and clinical validity. Electroencephalogr Clin Neurophysiol 76:459-472. Schwartz GE (1981): A systems analysis of psychobiology and beha~,~iortherapy. Implications for behavioral medicine. Psychother Psychosom 36:159-184. Schwartz GE (1982): Testing the biopsychosocial model: the ultimate challenge facing behavioral medicine? J Consult Clin Psychol 50:1040-1053. Schwartz BS, Ford P, Bolla KI, Aguew J, Bleecker ML (1991): Solvent-associated olfactory dysfunction: Not a predictor of deficits in learning and memory. Am J Psychiatry 148:751-756. Schwartz GE, Wright KP, Polak EH, Kline JP, Dikman Z (1992a): Topographic EEG mapping of conscious and unconscious odors. Chem Senses, in press. Schwartz GE, Wright KP, Polak EH, Schwartz JI (1992b): Conscious and unconscious odor registration in the elderly. Chemical Senses, in press. ~chwartzGE, Kling JP, Dikman Z, Wright KP, Polak EH (I 992c): EEG registrationof androstenone in androstenone anosmic subjects. Chem Senses, in press. Selner JC (1988): Chemical sensitivity. In Lichtenstein LM, Fauci AS (eds), Current Therapy in Allergy, Immunology, and Rheumatology.3. Philadelphia: BC Decker, pp 48-52. Servit A, Kristof M, Kolinova M (1977): Activation of epileptic electroencephalographic activity in the human by nasal airflow. Physiol Bohemoslov 26:499-506. Shipley MT (1985): Transport of molecules from nose to brain: transneuronal anterograde and retrograde labeling in the rat olfactory system by wheat germ agglutin-horseradish peroxidase applied to the nasal epithelium. Brain Res Bull 15:129-142. Siegel S, Hinson RE, Krank MD, McCully J (1982): Heroin overdose death: Contribution of drugassociated environmental cues. Science 216:436-437. Simon GE, Katon WJ, Sparks PJ (1990): Allergic to life: psychological factors in environmental illness. Am J Psychiatry 147:901-906. Sklar LS, Anisman H (1979): Stress and coping factors influence tumor growth. Science 205:513515. StaudenmayerH, Camazine M ( 1989): Sensing type ~ o n a l i t y , projection, and universal "allergic" reactivity. J Psychol Type 18:59--62. Staudenmayer H, Selner JC (1990): Neuropsychophysiologyduring relaxation in generalized, universal 'allergic' reactivity to the environment: A comparison study. J Psychosom Res 34:259270. Stewart DE, Raskin J (1985): Psychiatric assessment of patients with '120th century disease" ("total allergy syndrome"). Can Med Assoc J 133:!001-1006. 242 aiOL PSYCHIATRY I.R. Bell et al 1992;32:218-242 Stoudemire GA (1987): Selected organic mental disorders. In Hales RE, Yudofsky SC (eds), Textbook of Neuropsychiatry. Washington, DC: American Psychiatric Association Press, pp 125-139. Sugennan AA, Southern DL, Curran JF (1982): A study of antibody levels in alcoholic, depressive, and schizophrenic patients. Ann Allergy 48:166-171. Terr AI (1986): Environmental illness. A clinical ~'eview of 50 cases. Arch Intern Med 146:145149. Tilson HA, Veronesi B, McLamb RL, Mathews HB (1990): Acute exposure to tris(2-chloroethyl)phosphate produces hippocampal neuronal loss and impairs learning in rats. Toxicol Appl Pharmacol 106:254-269, van Riesen H, Leonard BE (1990): Effects of psychotropic drugs on the behavior and neurochemistry of olfactory bulbectomized rats. Pharacol Ther 47:21-34. Wada JA, Osawa T (1976): Spontaneous recurrent seizure state induced by daily electric amygdaloid stimulation in Senegalese baboons (Papio papio). Neurology 26:273-286. Weiss B, Williams JH, Margen S, et al (1980): Behavioral responses to artificial food colors. Science 207:1487-1488. Weiss SRB, Post RM, Gold PW, et al (1986): CRF-induced seizures and behavior: interaction with amygdala kindling. Brain Res 372:345-351. Wells KB, Rogers W, Bumam A, Greenfield S, Ware JE (1991): How the medical comorbidity of depressed patients differs across health care settings: Results from the medical outcomes study. Am J Psychiatry 148:1688-1696. Wood RW (1978): Stimulus properties of inhaled substances. Environ Health Perspect 26:69-76.