Bone 41 (2007) 437 – 445
www.elsevier.com/locate/bone
Fracture repair: Modulation of fracture-callus and mechanical properties by
sequential application of IL-6 following PTH 1–34 or PTH 28–48
Nimrod Rozen a,b,1 , Dina Lewinson a,b,⁎, Tova Bick b , Zvi C. Jacob a,c ,
Haim Stein c , Michael Soudry b,c
a
Department of Anatomy and Cell Biology, The Rappaport Family Faculty of Medicine, Technion-Israel Institute of Technology, PO Box 9649, Haifa 31096, Israel
b
Institute for Research of Bone Repair, Department of Orthopaedic Surgery A, Rambam Medical Center, 8 Ha'aliya str., PO Box 9602, Haifa 31096, Israel
c
Division of Orthopaedics, Rambam Medical Center, 8 Ha'aliya str., PO Box 9602, Haifa 31096, Israel
Received 24 January 2007; revised 19 April 2007; accepted 19 April 2007
Available online 8 May 2007
Abstract
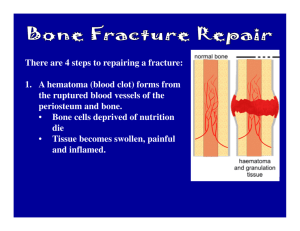
Fracture healing presents a sequence of three major stages: inflammation and granulation tissue formation, callus formation and remodeling.
Our working hypothesis was that fracture-repair might be enhanced by stimulating proliferation of chondrocytes and osteoblasts in the early stages
of fracture healing followed by sequential acceleration of the remodeling process. In the present study we employed a novel device developed by
us implementing a standardized fracture in rat tibiae. We investigated the effect of PTH 28–48 or PTH 1–34 alone or in sequence combination
with IL-6 together with its soluble receptor (IL-6sR) on fracture repair. PTH 28–48 or PTH 1–34 was applied locally into the hematoma of
fractures on days 4, 5 and 6 and IL-6+ its soluble receptor on days 7, 9, and 11. Post-fracture callus volume as measured 14 days post-fracture was
increased significantly only by PTH 1–34 (20%; P b 0.01). When one of the PTH fragments and IL-6 + IL-6sR were applied sequentially callus
volume was increased significantly (33%; P b 0.01). X-rays radiography at 5 weeks post-fracture showed enlarged callus volume following
treatment by either PTH fragments alone, and complete union following the sequential injection of both PTH fragments and IL-6 + IL-6sR, only.
Only the combination of one of the PTH fragments with IL-6 + IL-6sR, as measured 6 weeks post-fracture by three point bending, changed
dramatically the quality of the regenerating bone as presented by a 300% increase in mechanical resistance when PTH 1–34 was combined and
200% when PTH 28–48 was combined relative to vehicle-treated fractured bones. We conclude that the sequential application of IL-6 + IL-6sR
with both PTH fragments has the potential of enhancing fracture healing in long bones and should be further explored in preclinical and in clinical
studies.
© 2007 Elsevier Inc. All rights reserved.
Keywords: Fracture repair; Bone; IL-6; PTH 1–34; PTH 28–48
Introduction
Fracture healing after injury in a long bone is a well regulated
multi-step process; however, 5–10% of the fractures are
associated with non-union or delayed healing [1]. The interest
in the clinical applications of growth factors and other peptides
as enhancers of bone repair has stimulated several studies
⁎ Corresponding author. Institute for Research of Bone Repair, Orthopaedic
Surgery A, Rambam Medical Center, 8, Ha'aliya st., Haifa 31096, Israel.
Fax: +972 48543606.
E-mail address: dinal@tx.technion.ac.il (D. Lewinson).
1
Present address: Department of Orthopaedic Surgery, Ha'Emek Medical
Center, Afula 18101, Israel.
8756-3282/$ - see front matter © 2007 Elsevier Inc. All rights reserved.
doi:10.1016/j.bone.2007.04.193
resulting in as yet no definitive conclusion and pragmatic
recommendations [2]. One of the agents studied intensively on
its potential effect on fracture healing is the parathyroid hormone
(PTH) and specifically its amino terminal fragment PTH 1–34.
PTH has two opposite effects on bone if administered in different
ways. While continuous administration causes bone loss, intermittent injection increases bone volume and bone density [3–5].
The primary target of PTH in bone is the osteoblast which
expresses a single PTH receptor (PTH1R), which is a common
receptor also to the hypercalcemia associated peptide PTHrelated protein (PTHrP) [6]. The complexity of PTH skeletal
actions, catabolic as well as anabolic has made their evaluation
for the most part difficult to interpret. However, these ambiguous
actions of PTH on bone suggest its effect as a bone turnover
438
N. Rozen et al. / Bone 41 (2007) 437–445
Fig. 1. Fracture scheme demonstrating the four sites (marked as bold squares),
that were chosen for the histomorphometric analysis. Sections that displayed a
fracture gap between 4 cortices were chosen for analysis. Two of them were
located under the periosteum proximal and distal to the fracture gap and the
other two adjacent to the cortices at the fracture gap. Four Alcian blue-H&Estained sections from each callus, approximately 50–100 μm apart, were
analyzed histomorphometrically. Surface areas occupied by fibrous tissue,
cartilage, and cancellous bone were analyzed. Mean values ± SEM of areas of
each type of tissue were calculated separately.
modulator in fracture repair. Experiments in animal models have
used intermittent application of various doses of PTH 1–34 in
different orthopaedic applications. In a study in parathyroidectomized rats, PTH administration was shown to enhance early
fracture-healing [7]. In a number of recent reports, doses ranging
from 10 to 200 μg/kg in rat models of fracture-healing were
found to be associated with substantial increases in both mechanical and histological properties [8–11]. Nakajima et al. [9]
observed stimulation of osteoprogenitor cells as revealed by
PCNA immunostaining in day 2 post-fracture in the periosteum
of fractured rats treated daily with 10 μg/kg PTH. They also
reported increased levels of mRNA expression of collagen typeI, osteonectin, alkaline phosphatase, and osteocalcin, all markers
of differentiated osteoblasts during the early stages of the healing
cascade and in a later stage (4–21 days post-fracture). In other
studies, in which models of impaired bone metabolism were
used, PTH analogs were shown to reverse the inhibition of bonehealing in ovariectomized rats and in rabbits treated with
corticosteroids. In one report, PTH 1–34 was shown to increase
bone in-growth and pullout strength in porous metallic implants
[12–14]. Despite its promising potential in enhancing fracture
repair, no results of trials have yet been published on the use of
PTH 1–34 (Teriparatide) in clinical setting.
Our laboratory studied the effect of the synthetic mid-region
fragment of PTH, PTH 28–48, and confirmed in newborn mice
previous in vitro observations, that it exerts anabolic effects on
cartilage in vivo as well [15–20]. These effects are probably
mediated through binding to the common PTH/PTHrP receptor
and transduction of the signal by means of the protein kinase C
pathway [21–23]. Moreover, It has been shown that PTH 28–48
up-regulates 1,25-dihydroxyvitamin D3 receptors in rat growth
cartilages by the same pathway [24]. Interleukin-6 (IL-6) is a
multifunctional cytokine that regulates pleiotropic biological
activities in immune regulation, inflammation, hematopoiesis,
and oncogenesis. Its effects are shared by other cytokines of the
IL-6 family, such as leukemia inhibitory factor and oncostatin M
[25,26]. It is also known as a stimulator of bone resorption [27].
IL-6 exerts its biological activities through interaction with
specific receptors expressed on the surface of target cells. The
receptor complex mediating the biological activities consists of
two distinct membrane-bound glycoproteins: IL-6 receptor and
gp 130, which is a signal transduction non-ligand binding
component. Upon binding of IL-6 to the receptor, gp130 is
homodimerized and is subsequently involved in down-stream
signal processes binding tyrosine kinases and activating STAT1
and STAT3 transcriptional factors. Both IL-6R and gp130 also
occur in soluble form in biological fluids and have been purified
from human serum and urine [28]. Our group has previously
demonstrated that systemic injection of IL-6 to nude (athymic
mutant) mice enhances bone remodeling up to the point that the
petrotic bone of the nude mice resembles that of a normal mice
[29]. Therefore we decided to study the metabolic effect of IL-6
on bone remodeling during fracture repair and to explore whether
its sequential combination with PTH fragments will benefit the
fracture healing process without compromising the quality of the
regenerated bone. Recently we have described the fracture
healing cascade high-lightening important cross roads in which
epigenetic intervention might enhance the healing process [1].
The present study presents an example applying this approach.
Materials and methods
Rat fracture model
Wistar female rats (200–250 g) were used. Animals were maintained and
sacrificed in a manner approved by the Institutional Committee for Animal Care
Fig. 2. Histomorphometric analysis of 8 days (upper panel) and 14 days (lower
panel) old fracture calluses. Sections from five rats were analyzed for each
group. The histogram demonstrates surface areas ± SEM occupied by cartilage,
woven bone and fibrous tissue. *P b 0.02 vs. control.
N. Rozen et al. / Bone 41 (2007) 437–445
and Experiments of the Technion. Rats were anesthetized with intraperitoneal
injections of sodium phenobarbital (4 mg/100 g body weight) (Rhöne Merieux
Limited, Harlow, Essex, UK). A hollow wire pin (French 25) was introduced
through the medial aspect of the tibia in the area of the ring of Ranvier until the
middle of the medullary canal. Then, fracture was induced by the “Rozen
device”, which was developed in our laboratory, to the mid-shaft of the tibia
[30]. With this device the left tibia is clamped by two flexible screws proximally
and distally to the mid-shaft and a closed fracture is induced by a direct external
blow by means of a pendulum. The device administers controlled blows that
produce anatomically uniform fractures. Following fracture the pin was pushed
further until it reached the ankle joint. The right tibia remained untouched and
served as an unfractured control for the same rat. Post operatively the fractured
tibiae were immersed in an antiseptic solution in order to avoid infections. The
rats were free to move in their cages with full weight bearing throughout the
experimental period. All rats received the same Purina diet. Rats were divided
randomly into experimental groups. Each experimental group contained 5–10
animals.
Local application of PTH fragments and IL-6
On days 4, 5, and 6 post-fracture, at 11.00 AM, a volume of 0.2 ml was
applied directly by injection under the skin above the fracture site. This volume
439
contained either a low dose of 0.2 μg hPTH 28–48 (Sigma-Aldrich Corporation,
St. Louis, Missouri, USA), a high dose of 1.0 μg hPTH 28–48, 1.0 μg rat PTH
1–34 (Sigma-Aldrich Corporation, St. Louis, Missouri, USA), or vehicle (0.4%
BSA in 0.01 mol/l acetic acid).
hIL-6 (Sigma-Aldrich Corporation, St. Louis, Missouri, USA) was locally
applied in the same conditions solely or in combination with it soluble receptor
(hIL-6sR; Sigma-Aldrich Corporation, St. Louis, Missouri, USA) on days 7, 9,
and 11 post-fracture. The following concentrations were applied: 8, 20, and 40
ng/0.2 ml of IL-6 and 20, 50, and 100 ng/0.2 ml of IL-6sR, respectively. Rats
were euthenized by a lethal intraperitoneal injection of sodium phenobarbital on
day 8, 14, or 6 weeks post-fracture.
Processing for histology and histomorphometry
Fractured left tibiae were removed by dislocation from the knee and ankle
joints, and following removal of the pins were stripped of skin and carefully
cleaned from surrounding soft tissue, keeping the periosteum intact as possible.
Those that were removed from rats killed after 8 and 14 days were immersed in
neutral buffered formalin solution for 48 h. Tibiae were then decalcified in 10%
EDTA (in 0.1M Tris buffer) solution for 8 weeks. Following decalcification the
tibiae were embedded in paraffin. Six micrometer thick sections were stained
with Alcian blue (pH 2.5) and counterstained with H&E.
Fig. 3. Representative sections of 14 days old callusses following injections on days 7, 9 and 11 of vehicle (A), 40 ng IL-6 (B), 8 ng IL-6 + 20 ng IL-6sR (C), 20 ng IL-6 +
50 ng IL-6sR (D), and 40 ng IL-6 + 100 ng IL-6sR (E). No differences were observed between vehicle-treated (A), IL-6 alone (B), and low doses of IL-6 + IL-6sR (C).
Both combinations with the higher doses showed marked modulation of cartilage remodeling into bone (D&E). Alcian-blue-H&E staining.
440
N. Rozen et al. / Bone 41 (2007) 437–445
Sections that displayed a fracture gap between 4 cortices were chosen for
analysis. Four Alcian blue-H&E-stained sections from each callus, approximately
50–100 μm apart, were analyzed morphometrically using an Olympus™ Image
Analysis System (Cue-2 morphometry software of Galai Corporation, Migdal
Haemek, Israel). Using a grid frame and tracing device, the surface area of 9 squares
(3×3) of the grid in ×10 magnification (300 μm2) in 4 specific locations under the
periosteum and adjacent to the cortices at the fracture gap (Fig. 1) was measured and
surface areas occupied by fibrous tissue, cartilage, and cancellous bone were analyzed. Mean values ±SEM of areas of each type of tissue were calculated separately.
Tibia volume measurement
Before being exposed to the demineralization procedure and further
processing for the histological observations, the 14 days treated tibiae from all
experimental groups were subjected to calluses measurements by the principle
of Archimedes. The left cleaned tibiae, which contained the fracture callus and
periosteum and the corresponding right, similarly cleaned but not fractured
tibiae, were immersed in 5 ml of distilled water in a 10 ml grading cylinder. The
volume created by the immersed bones was measured and the additional
volume, calculated by reducing the volume of the non-fractured from the
fractured bone of the same rat represents callus volume.
Mechanical testing
Six weeks post-fracture calluses were immediately frozen in liquid nitrogen
and kept frozen in −70 °C until the day of the mechanical testing. The night
before testing, they were left to thaw in a refrigerator. The next day, all soft tissue
was carefully removed. The mechanical strength of the healing fractures was
measured by a 3-point bending procedure that was applied using a materials
testing machine (Instron 1195, Instron Corporation, Canton, Massachusetts,
USA). A small chamber containing three bars was tailor made for this purpose.
The fractured bone was placed on two rounded bars (spaced 15 mm apart) with
the fracture line between the bars. Deflection was performed by lowering
another bar onto the fracture line using a constant speed of 1 mm/min. All bones
were placed in the same position so that the force was applied from the anterior
to the posterior surface of the bone—convex side was under pressure of the
descending bar. Transducers recorded load and deflection continuously. The
signal was fed to an x–y recorder, and the load–deflection curves obtained were
read by a graphic tablet into a PC computer using Analog to Digital card
(National Semiconductor, Santa Clara, California, USA). The parameters
calculated were: maximum load to failure, absorptive energy, and stroke at
breaking point. The stroke (mm) was defined as the length of deflection at
maximum loading. Results were normalized and calculated with respect to the 2
diameters in the anterior-posterior and lateral directions of the tibia.
analyzed by quantitative histomorphometry. Measurements of
surface areas occupied by cartilage, intramembranous bone, and
fibrous tissue revealed that by 8 days post-fracture (Fig. 2, upper
panel) all 3 parameters increased when compared with vehicletreated fractures, but only cartilage and fibrous tissue increments
caused by the local application of high dose PTH 28–48 were
statistically significant: 2.8 (P b 0.02) and 1.7 (P b 0.02) -folds,
respectively. By 14 days post-fracture (Fig. 2, lower panel), the
increased cartilage surface area was maintained, but only the
higher dose was statistically significant (1.8-folds, P b 0.02). As
a consequence of these results, the dose of 1.0 μg was chosen for
future experiments.
IL-6 and IL-6 + IL-6sR dose response
On days 7, 9, and 11 post-fracture 3 doses of IL-6 (8, 20 and
40 ng/0.2 ml) were injected solely or in combination with IL6sR (20, 50, and 100 ng/0.2 ml, respectively) and compared
with vehicle-injected rats on the same days. All rats were
sacrificed 14 days post-fracture, and their tibiae were processed
for histological evaluation. All 3 doses of IL-6 tested showed a
similar histological picture, namely quite a lot of cartilage
Statistical analysis
Histomorphometric and callus volume values are expressed as mean ± SEM.
Statistical analysis of data was carried out using One-way Analysis of Variance
(ANOVA), using t-test for means comparison between treated and control
groups. Data were summed and calculated using SPSS statistics program.
Results were regarded as significant at P b 0.05.
Results
Establishment of an effective dose of PTH 28–48 by differential
histomorphometric analysis
Fractures were implemented in the left tibiae of rats using the
“Rozen Device”. On days 4, 5, and 6 post-fracture, all rats were
injected locally, into the hematoma with vehicle, a low (0.2 μg;
n = 10), and a high (1.0 μg; n = 10) dose of PTH 28–48. Five
randomly selected rats from each group were sacrificed 8 days
post-fracture and the rest on the 14th day. Paraffin sections were
Fig. 4. Tibia volume measurements of 14 days old fractured and unfractured bones
treated with vehicle (control), 40 ng IL-6+ 100 ng IL-6sR, 1.0 μg PTH 1–34,
1.0 μg PTH 28–48 and combinations. Results are means± SEM of 5 bones per
group. *P b 0.0005—left (fractured) vs. right (unfractured); +P b 0.01—left
(fractured) of an experimental rat vs. left (fractured) of vehicle treated control rat
#P b 0.02—right (unfractured) of an experimental rat vs. right (unfractured) of
vehicle treated control rat.
N. Rozen et al. / Bone 41 (2007) 437–445
441
Fig. 5. Representative sections of 14 days old callusses: A—vehicle; B—increased amounts of cartilage following treatment with 1.0 μg PTH 28–48; C—mostly
intramembranous bone in fractures that received the combination of 1.0 μg PTH 28–48 with 40 ng IL-6 + 100 ng IL-6sR. ca—cartilage, ct—cortex, eb—endosteal
bone, pib—periosteal intramembranous bone, rf—resorption front. Alcian-blue-H&E staining.
surrounding the fractured cortices, similar to vehicle-treated
fractures (Figs. 3A and B). A gradual shift from cartilage to
intramembranous bone was observed when IL-6 was combined
with its soluble receptor. Although the combination with the
low doses still resembled the vehicle-treated or IL-6 alone
(Fig. 3C), both higher doses combinations showed marked
modulation of cartilage remodeling into bone (Figs. 3D and E).
As a consequence of these results, the combination of 40 ng
IL-6 was chosen to combine with 100 ng of its soluble receptor
for future experiments.
Fig. 6. X-rays radiographs of fractured tibiae taken 5 weeks post-fracture. A—control; B—1.0 μg PTH 28–48; C—1.0 μg PTH 1–34; D—40 ng IL-6 followed by
100 ng IL-6sR; E—1.0 μg PTH 28–48 + 40 ng IL-6 + 100 ng IL-6sR; F—1.0 μg PTH 1–34 + 40 ng followed by IL-6 + 100 ng IL-6sR. Arrow—site of fracture.
442
N. Rozen et al. / Bone 41 (2007) 437–445
but not when compared to vehicle-treated fractured bones (Fig. 4).
However both PTH fragments when combined with the later
application of IL-6 + IL-6sR brought about a significant increase
in tibia volume when compared both to their own unfractured
tibiae controls and to vehicle-treated fractures (Fig. 4). Interestingly, a systemic effect on the unfractured right tibiae was exerted
by the sequential application of PTH 1–34 followed by IL-6 +
IL-6sR (Fig. 4, upper panel). Calculating the callus volume by
deducting the volume of the unfractured tibiae from the fractured
tibiae it can be appreciated that when PTH 1–34 was combined
with IL-6 + IL-6sR, the ▵ increased by about 2.4-folds when
compared with vehicle-treated rats (Fig. 4, upper panel) and by
3-folds when PTH 28–48 was combined with IL-6 + IL-6sR
(Fig. 4, lower panel), probably because the increased cartilage
area that was stimulated by PTH 28–48 served as infrastructure
for its remodeling into bone. Indeed, comparison of the histology
of 14 days old callusses showed increased amounts of cartilage
following treatment with PTH 28–48 (Fig. 5B) when compared
with vehicle-treated (Fig. 5A) and mostly intramembranous bone
in fractures that received the combination of PTH 28–48 with
IL-6 + IL-6sR (Fig. 5C). We concluded that IL-6 + IL-6sR
accelerated the remodeling of cartilage into bone.
X-rays radiography
Fig. 7. Mechanical resistance as expressed by power to failure measurements
(MPa) of 6 weeks old fractured and unfractured bones treated with vehicle
(control), 1.0 μg PTH 1–34, 1.0 μg PTH 28–48 and combinations. Results are
means ± SEM of 5 bones per group. *P b 0.0001 and b0.03—left (fractured) vs.
right (unfractured) for PTH 1–34 + IL-6 + IL-6sR and PTH 28–48 + IL-6 +
IL-6sR, respectively. +P b 0.0001 and b0.005—left (fractured) of an experimental rat vs. left (fractured) of vehicle treated control rat for PTH 1–34 + IL-6 +
IL-6sR and PTH 28–48 + IL-6 + IL-6sR, respectively.
X-rays radiographs that were taken by 5 weeks post-fracture
showed that treatment of fractures with either of the PTH
fragments resulted in enlarged calluses around the fracture site,
Sequential application of PTH fragments and IL-6 + IL-6sR
Following the results obtained by application of the mid
fragment of PTH, PTH 28–48, and by application of IL-6 +
IL-6sR, we decided to evaluate the sequential application of
these factors on the fracture healing process. In addition we
analyzed whether the known accelerating effect of the amino
terminal fragment of PTH, PTH 1–34, is further enhanced by
sequential application of IL-6 + IL-6sR. In order to be able to
compare between both PTH fragments we applied also PTH
1–34 in the dose of 1.0 μg. The various factors were applied at
the same temporal conditions as described in the former
experiments. Two parameters were chosen for evaluation:
measurement of tibia volume by 14 days post-fracture and
analyzing mechanical resistance at 6 weeks post-fracture.
Tibia volume
PTH 1–34 was the only factor that increased tibia volume
significantly when applied alone to fractured bones, but only
when compared to the unfractured bones of the rats in its group
Fig. 8. Graphs of the application of strength from representative control and
experimental fractured bones.
N. Rozen et al. / Bone 41 (2007) 437–445
while only fractures treated by sequential applications of either
of the PTH fragments with IL-6 + IL-6sR demonstrated full
healing (Fig. 6).
Mechanical testing
Fig. 7 demonstrates that both PTH fragments, when applied
during the early stages of the healing process did not confer more
resistance to 6 weeks healing bones, as measured using the 3
point-bending technique. However, a combination of both PTH
fragments with IL-6 and its soluble receptor increased dramatically the fractures' resistance, 200% (P b 0.05) when PTH28–48
was combined and 300% (P b 0.0001) when PTH1–34 was
combined. Moreover the resistance of the broken bones of the
combination groups was similarly increased when compared with
their own right unfractured bones (P b 0.03 and P b 0.00001,
respectively, Fig. 7). Bones treated with IL-6 + IL-6sR were not
measurable as these bones where easily broken during handling.
Analysis of representative bones is presented in Fig. 8. In this
figure it can be seen that as we have shown in Fig. 7, the
mechanical load needed for callus break in both PTH fragments
treated fractures did not differ from those treated with vehicle.
In contrast, combination of both PTH fragments with IL-6 and
its soluble receptor increased the plasticity of the bones as
expressed in the increased load to failure needed to break the
bones, in their energy absorptive capacity and in lengthening of
the displacement parameter.
Discussion
Our working hypothesis was that the fracture healing process
could be accelerated not only by the use of growth factors known to
be anabolic to cartilage and bone, but also by factors that affect the
remodeling of cartilage to bone in particular and bone turnover in
general [1]. Therefore we opted to apply anabolic and remodeling
accelerating agents in sequence at particular time points of the
chondrogenic and cartilage to bone remodeling phases (4–6 and
7–11 days post-fracture, respectively) of the regeneration process.
Our concept was to increase cartilage that will serve as an
infrastructure for the newly formed bone and then to accelerate its
remodeling into bone by endochondral ossification. PTH 1–34 and
PTH 28–48 were chosen to stimulate the chondrogenic phase as
they are known to be growth factors to skeletal cells [15,16,31,32].
In addition, on the basis of our previous studies that demonstrated
activation of osteoclasts in nude mice by IL-6 + IL-6sR, we have
chosen to use this cytokine as a cartilage to bone remodeling
accelerator during fracture repair [29]. Preliminary experiments
were performed in order to determine the dosage of local
application of IL-6 into the hematoma and whether the addition
of IL-6sR in order to improve its availability will be beneficial. Our
results (shown in Fig. 5) demonstrate that remodeling was
enhanced only when the soluble receptor for IL-6 was combined
to the cytokine. In effect, it is well documented that the number of
IL-6 receptors might be a limiting factor for its biological effect and
that IL-6sR is a key factor for the effects of IL-6 in bone [25–28].
As a result of these experiments we decided to inject 40 ng IL-6
+ 100 ng of the soluble receptor.
443
While the effects of the active amino-terminal fragment PTH
1–34 on fracture repair have been extensively studied [8,9,33–36],
no data are available concerning its synthetic mid-region fragment,
PTH 28–48.
During the early stage of fracture healing the callus develops in
order to stabilize the fractured bone fragments so that cortical
union might proceed. As the main goal for intervention is
acceleration of the healing process, we analyzed the effects of the
PTH 28–48 peptide on callus components following its local
application during the early stages of fracture healing. Due to the
short half-life of this PTH fragment, we presumed that systemic
administration would have little effect and opted to apply the
fragment locally and directly to the encapsulated hematoma at the
fracture site. This approach has been adopted by several authors,
especially for the application of recombinant proteins with or
without carriers, in order to circumvent undesired side effects that
might accompany a systemic administration [2,37–41]. Our
working hypothesis was that PTH 28–48 might be effective as an
accelerating agent for fracture healing, as it has been proved by
our group and others to induce chondrogenesis in mice and rats
and also to exert mitogenic stimulation for osteoblastic cell lines
[15–20]. Histomorphometric analysis of low-dose (0.2 μg) and
high-dose (1.0 μg) injections demonstrated that by 8 days postfracture only cartilage and fibrous tissue increased significantly.
However, by 14 days post-fracture only the increased cartilage
surface area was maintained and only by the higher dose. As a
consequence of these results, the dose of 1.0 μg was chosen for the
following experiments. In summary, PTH 28–48, when injected
directly into the callus area, stimulated all the components of the
healing process but the fibrous tissue (that includes mainly
mesenchynal progenitors) filling the gap and cartilage components were most profoundly stimulated. We suggest that the main
effect of PTH 28–48 is to stimulate the proliferation of progenitor
cells and orient their differentiation towards chondrogenesis.
Concomitantly, it should be emphasized that woven bone
formation was not compromised and proceeded undisturbed.
Contrary to most studies that followed long-term daily systemic applications of different growth factors, we chose short-term
local applications in accordance with specific biological stages of
the healing process [1]. Thus, PTH fragments were injected solely
on days 4, 5, and 6 in order to stimulate chondrogenesis, whereas
IL-6 + IL-6sR were applied on days 7, 9, and 11 in order to
accelerate cartilage and woven bone remodeling. Our results
demonstrated that although both PTH fragments when applied
during the early stages of the healing process enhanced callus
formation by 14 days, this increased callus formation was not
translated into greater resistance of the healing bone as measured
6 weeks post-fracture. On the other hand, a combination of each of
the PTH fragments with IL-6 + IL-6sR increased not only the
callus volume and accelerated the healing process as demonstrated
by radiography, but also modified dramatically the quality of the
bone, as presented by an increase of 300% in mechanical
resistance when PTH 1–34 was combined and of 200% when
PTH 28–48 was combined, when compared with vehicle-treated
fractured bone. Interestingly, the mechanical strength of the
contralateral unfractured bones of both experimental groups in
which the PTH fragments combined with IL-6 + IL-6sR were
444
N. Rozen et al. / Bone 41 (2007) 437–445
injected to the callus was reduced compared to control unfractured
bones. The probable explanation is that there is a systemic effect of
the locally injected agents that increases remodeling of intact
bones resulting in higher porosity and fragility.
Several other agents and growth factors have been tested for
their ability to accelerate fracture healing. Amongst them are the
proteins of the BMP and TGF-β family. Increased callus volume
in rat fractures that were locally treated with either BMP-2 or TGFβ were reported to be associated with only moderate increases in
strength and stiffness [37,40], while in other studies in rabbits and
rats treated with BMP-2, a temporal enhancement in the healing
time was noted that was also accompanied with marked improvement of biomechanical properties [42–44]. Local application of
TGF-β as a coating in poly (D,L-lactide)-coated titanium Kirschner
wires resulted in less cartilage in the periosteal callus and increased
mineralization and biomechanical strength [45], and BMP-2 when
applied in a calcium phosphate paste enhanced temporal bridging
and mineralized callus [46], exemplifying that the mode of
application and the dosage have fundamental effects on the
variation in the results. Exploring TGF-β effects when directly
applied to the fracture site resulted in conflicting results. So, for
example, no increase in callus volume under unstable fixation
conditions, while some increase under stable conditions was
reported in one study [37], while increase in the strength of tibial
fractures was reported by others [39]. Applying one injection of
100 μg bFGF directly to the fracture site in rats had similar effects
as PTH 28–48, namely enlargement of the cartilaginous callus
with no induction of rapid healing [47], while doubling the dose
stimulated bone remodeling and increased bone mineral content in
a tibial fracture model in beagle dogs [48]. Perhaps the most
promising results were achieved by intermittent application of
PTH 1–34 throughout the healing process, probably by enhancing
both proliferation and differentiation of osteoprogenitor cells and
by increasing bone mineral content and osteoclastogenesis [8,9].
Similarly, a PTHrP analog had effective effects on impaired bone
healing in rabbits that were on corticosteroid therapy [13].
As approximately 5–10% of fractures are associated with
delayed or non-union healing, it is obvious that the search for
agents that will be able to promote the healing process will
continue. As of now no one specific factor has yet proved to gain
clinical use, and may be in the future combinations of several
factors will have to be explored [2,49]. Adopting this attitude PTH
fragments carry promise for the future especially if combined with
a factor that will concomitantly enhance the remodeling of the
stimulated cartilage into a well-mineralized bone tissue.
In conclusion the present study demonstrated that sequential
application of anabolic PTH fragments with the remodeling
accelerator IL-6 that stimulates chondro/osteoclasts function
[50–51], results in a synergistic fracture healing enhancement.
Further studies are needed as to how to integrate these findings
into a potential for treating and accelerating fractures in the
clinical setting.
Acknowledgments
We are grateful to Prof. Elazar Gutmanes from the Faculty of
Materials and Engineering of the Technion for helping with the
mechanical tests. This work was supported by the Research
Foundation of Rambam Medical Center and by The Technion
V.P.R. Fund.
References
[1] Rozen N, Lewinson D, Bick D, Meretyk S, Soudry M. Role of bone
regeneration and turnover modulators in control of fracture. Crit Rev
Eukaryot Gene Expr 2007;17(3):197–214.
[2] Lieberman JR, Daluiski A, Einhorn TA. The role of growth factors in the
repair of bone. J Bone Joint Surg 2002;84-A:1032–44.
[3] Tam CS, Heersche JN, Murray TM, Parsons JA. Parathyroid hormone
stimulates the bone apposition rate independently of its resorptive action:
differential effects of intermittent and continuous administration. Endocrinology 1982;110:506–12.
[4] Schiller PC, D'Ippolito G, Roos BA, Howard GA. Anabolic or
catabolic responses of MC3T3-E1 osteoblastic cells to parathyroid
hormone depend on time and duration of treatment. J Bone Miner Res
1999;14:1504–12.
[5] Dobnig H, Turner RT. Evidence that intermittent treatment with
parathyroid hormone increases bone formation in adult rats by activation
of bone lining cells. Endocrinology 1995;136:3632–8.
[6] Juppner H, Abou-Samra AB, Freeman M, Kong XF, Schipani E, Richards
J, et al. A G protein-linked receptor for parathyroid hormone and
parathyroid hormone-related peptide. Science 1991;254:1024–6.
[7] Fukuhara H, Mizuno K. The influence of parathyroid hormone on the process
of fracture healing. Nippon Seikeigeka Gakkai Zasshi 1989;63:100–15.
[8] Andreassen TT, Ejersted C, Oxlund H. Intermittent parathyroid hormone
(1–34) treatment increases callus formation and mechanical strength of
healing rat fractures. J Bone Miner Res 1999;14(6):960–8.
[9] Nakajima A, Shimoji N, Shiomi K, Shimizu S, Moriya H, Einhorn TA, et al.
Mechanisms for the enhancement of fracture healing in rats treated with
intermittent low-dose human parathyroid hormone (1–34). J Bone Miner
Res 2002;17(11):2038–47.
[10] Vortkamp A, Lee K, Lanske B, Segre GV, Kronenberg HM, Tabin CJ.
Regulation of rate of cartilage differentiation by Indian hedgehog and
PTH-related protein. Science 1996;273:613–22.
[11] Holzer G, Majeska RJ, Lundy MW, Hartke JR, Einhorn TA. Parathyroid
hormone enhances fracture healing. A preliminary report. Clin Orthop
1999;366:258–63.
[12] Kim HW, Jahng JS. Effect of intermittent administration of parathyroid
hormone on fracture healing in ovariectomized rats. Iowa Orthop J 1999;19:
71–7.
[13] Bostrom MP, Gamradt SC, Asnis P, Vickery BH, Hill E, Avnur Z, et al.
Parathyroid hormone-related protein analog RS-66271 is an effective
therapy for impaired bone healing in rabbits on corticosteroid therapy.
Bone 2000;26:437–42.
[14] Skripitz R, Andreassen TT, Aspenberg P. Parathyroid hormone (1–34)
increases the density of rat cancellous bone in a bone chamber. A dose–
response study. J Bone Joint Surg Br 2000;82:138–41.
[15] Kim TY, Vargas V, Mayer H, Somjen D, Kaye AM. Selective anabolic
effects of muteins of mid-region PTH fragments on skeletal tissues of
prepubertal rats. Bone 2002;30:78–84.
[16] Rihani-Bisharat S, Maor G, Lewinson D. In vivo anabolic effects of
parathyroid hormone (PTH) 28–48 and N-terminal fragments of PTH and
PTH-related protein on neonatal mouse bones. Endocrinology 1998;193:
974–80.
[17] Schlüter K-D, Hellstren H, Wingender E, Mayer H. The central part of the
parathyroid hormone stimulates thymidine incorporation of chondrocytes.
J Biol Chem 1989;264:1087–92.
[18] Somjen D, Binderman I, Schluter K-D, Wingender E, Mayer H, Kaye AM.
Stimulation by defined parathyroid hormone fragments of cell proliferation
in skeletal-derived cell cultures. Biochem J 1990;272:781–5.
[19] Somjen D, Schluter K-D, Wingender E, Mayer H, Kaye AM. Stimulation
of cell proliferation in skeletal tissues of the rat by defined parathyroid
hormone fragments. Biochem J 1991;277:863–7.
N. Rozen et al. / Bone 41 (2007) 437–445
[20] Shurtz-Swirski R, Lewinson D, Schenzer P, Mayer H, Silbermann M.
Effects of parathyroid hormones fragments on the growth of murine
mandibular condylar cartilage in vitro. Acta Endocrinol (Copenh)
1990;122:217–26.
[21] Civitelli R, Reid IR, Wedtbrook S, Avioli LV, Hruska KA. PTH elevates
inositol polyphosphates and diacylglicerol in a rat osteoblast-like cell line.
Am J Physiol 1988;255:E660–7.
[22] Fujimori A, Cheng S-L, Avioli LV, Civitelli R. Structure-function
relationship of parathyroid hormone: activation of phospholipase-C,
protein kinase-A and -C in osteosarcoma cells. Endocrinology 1992;130:
29–36.
[23] Sabatini M, Lesur C, Pacherie M, Pastoureau P, Kucharczyk N, Fauchere JL,
et al. Effects of parathyroid hormone and agonists of the adenylyl cyclase and
protein kinase C pathways on bone prolifiration. Bone 1996;18:59–65.
[24] Klaos G, Eichel Bv, May T, Hügel U, Mayer H, Ritz E, et al. Synergistic
effects of parathyroid hormone and 1,25-dihydroxyvitamin D3 on
proliferation and vitamin D receptor expression of rat growth cartilage
cells. Endocrinology 1994;135:1307–15.
[25] Naka T, Nishimoto N, Kishimoto T. The paradigm of IL-6: from basic
science to medicine. Arthritis Res 2002;4(Suppl 3):S233–42.
[26] Kishimoto T. Interleukin-6: discovery of a pleiotropic cytokine. Arthritis
Res Ther 2006;8(Suppl 2):S2.
[27] Roodman GD. Regulation of osteoclast differentiation. Ann N Y Acad Sci
2006;1068:100–9.
[28] Liu XH, Kirschenbaum A, Yao S, Levine AC. The role of the interleukin6/gp130 signaling pathway in bone metabolism. Vitam Horm 2006;74:
341–55.
[29] Rozen N, Ish-Shalom S, Rachmiel A, Stein H, Lewinson D. Interleukin-6
modulates trabecular and endochondral bone turnover in the nude mouse
by stimulating osteoclast differentiation. Bone 2000;26(5):469–74.
[30] Rozen N, Rachmiel A, Jacob ZC, Stein H, Lewinson D. Development of a
standardized closed fracture instrument in the rat tibia. Bone 2003:S108
[Suppl].
[31] Tashjian Jr AH, Gagel RF. Teriparatide [human PTH(1–34)]: 2.5 years of
experience on the use and safety of the drug for the treatment of
osteoporosis. J Bone Miner Res 2006;21(3):354–65.
[32] Martin TJ, Quinn JM, Gillespie MT, Ng KW, Karsdal MA, Sims NA.
Mechanisms involved in skeletal anabolic therapies. Ann N Y Acad Sci
2006;1068:458–70.
[33] Andreassen TT, Fledelius C, Ejersted C, Oxlund H. Increases in callus
formation and mechanical strength of healing fractures in old rats treated
with parathyroid hormone. Acta Orthop Scand 2001;72(3):304–7.
[34] Andreassen TT, Willick GE, Morley P, Whitfield JF. Treatment with
parathyroid hormone hPTH(1–34), hPTH(1–31), and monocyclic hPTH
(1–31) enhances fracture strength and callus amount after withdrawal
fracture strength and callus mechanical quality continue to increase. Calcif
Tissue Int 2004;74(4):351–6.
[35] Nakazawa T, Nakajima A, Shiomi K, Moriya H, Einhorn TA, Yamazaki M.
Effects of low-dose, intermittent treatment with recombinant human
parathyroid hormone (1–34) on chondrogenesis in a model of experimental fracture healing. Bone 2005;37(5):711–9.
[36] Alkhiary YM, Gerstenfeld LC, Krall E, Westmore M, Sato M, Mitlak BH,
et al. Enhancement of experimental fracture-healing by systemic
administration of recombinant human parathyroid hormone (PTH 1–34).
J Bone Joint Surg Am 2005;87(4):731–41.
445
[37] Crichtlow MA, Bland YS, Ashhurst DE. The effect of exogenous
transforming growth factor-β2 on healing fractures in the rabbit. Bone
1995;16:521–7.
[38] Kawaguchi H, Kurokawa T, Hanada K, Hiyama Y, Tamura M, Ogata E, et al.
Stimulation of fracture repair by recombinant human basic fibroblast growth
factor in normal and streptozotocin-diabetic rats. Endocrinology
1994;135:774–81.
[39] Nielsen HM, Andreassen TT, Ledet T, Oxlund H. Local injection of TGFbeta increases strength of tibial fractures in the rat. Acta Orthop Scand
1994;65:37–41.
[40] Welch RD, Jones AL, Bucholz RW, Reinert CM, Tjia JS, Pierce WA, et al.
Effect of recombinant human bone morphogenetic protein-2 on fracture
healing in a goat tibial fracture model. J Bone Miner Res 1998;13:
1483–90.
[41] Yasko AW, Lane JM, Fellinger EJ, Rosen V, Wozney JM. The healing of
segmental bone defects by recombinant human bone morphogenetic
protein (rhBMP-2): a radiographic, histological, and biomechanical study
in rats. J Bone Joint Surg 1990;74A:659–70.
[42] Bostrom M, Lane JM, Tomin E, Browne M, Berberian W, Turek T, et al.
Use of bone morphogenetic protein-2 in the rabbit ulnar non-union model.
Clin Orthop Relat Res 1996;327:272–82.
[43] Bouxsein ML, Turek TJ, Blake CA, D'Augusta D, Li X, Stevens M, et al.
Recombinant human bone morphogenetic protein-2 accelerates healing in
a rabbit ulnar osteotomy model. J Bone Joint Surg Am 2001;83-A
(8):1219–30.
[44] Einhorn TA, Majeska RJ, Mohaideen A, Kagel EM, Bouxsein ML, Turek
TJ, et al. A single percutaneous injection of recombinant human bone
morphogenetic protein-2 accelerates fracture repair. J Bone Joint Surg Am
2003;85-A:1425–35.
[45] Schmidmaier G, Wildemann B, Bail H, Lucke M, Fuchs T, Stemberger A,
et al. Local application of growth factors (insulin-like growth factor and
transforming growth factor-beta 1) from a biodegradeable poly(D,L-lactide)
coating of ostesynthetic implants accelerate fracture healing in rats. Bone
2000;28:341–50.
[46] Li RH, Bouxstein ML, D'Augusta D, Kim H, Wozney JM, Seeherman HJ.
rhBMP-2 injected in a calcium phosphate paste (alpha-BSM) accelerates
healing in the rabbit ulnar osteotomy model. J Orthop Res 2003;21:
997–1004.
[47] Makajima F, Ogasawara A, Goto K, Moriya H, Einhorn TA, Yamazaki M.
Spatial and temporal gene expression in chondrogenesis during fracture
healing and the effects of basic fibroblast growth factor. J Orthop Res
2001;19:935–44.
[48] Nakamura T, Hara Y, Tagawa M, Tamura M, Yuge T, Fukuda H, et al.
Recombinant human basic fibroblast growth factor accelerates fracture
healing by enhancing callus remodeling in experimental dog tibial fracture.
J Bone Miner Res 1998;13:942–9.
[49] Schmidmeir G, Wildemann B, Cromme F, Kandziora F, Haas NP, Rashke
M. Bone morphogenetic protein-2 coating of titanium implants increases
biomechanical strength and accelerates bone remodelling in fracture
treatment: a biomechanical and histological study. Bone 2002;30:816–22.
[50] Guillén C, de Gortázar AR, Esbrit P. The interleukin-6/soluble interleukin6 receptor system induces parathyroid hormone-related protein in human
osteoclastic cells. Calcif Tissue Int 2004;75:153–9.
[51] Franchimont N, Wertz S, Malaise M. Interleukin-6: an osteotropic factor
influencing bone formation? Bone 2005;37:601–6.