Journal of Cardiac Failure Vol. 13 No. 7 2007
Review Articles
Systolic and Diastolic Heart Failure: Differences and Similarities
KANU CHATTERJEE, MB, FRCP, FCCP, FACC, FAHA, MACP,1 AND BARRY MASSIE, MD, FACC2
San Francisco, California
ABSTRACT
Background: Diastolic heart failure (DHF) and systolic heart failure (SHF) are 2 clinical subsets of the
syndrome of chronic heart failure that are most commonly encountered in clinical practice.
Methods and Results: The clinically overt DHF and SHF appear to be 2 separate syndromes with
distinctive morphologic and functional changes although signs, symptoms, and prognosis are very similar.
In DHF, the left ventricle is not dilated and the ejection fraction is preserved. In contrast in SHF, it is
dilated and the ejection fraction is reduced. The neurohormonal abnormalities in DHF and SHF appear
to be similar. The stimuli and the signals that ultimately produce these 2 different phenotypes of chronic
heart failure remain, presently, largely unknown.
Conclusions: Although there has been considerable progress in the management of SHF, the management
of DHF remains mostly empirical because of lack of knowledge of the molecular and biochemical mechanisms which produce myocardial structural and functional changes in this syndrome. Further research
and investigations are urgently required. (J Cardiac Fail 2007;13:569e576)
Key Words: Systolic heart failure, diastolic heart failure, remodeling, function.
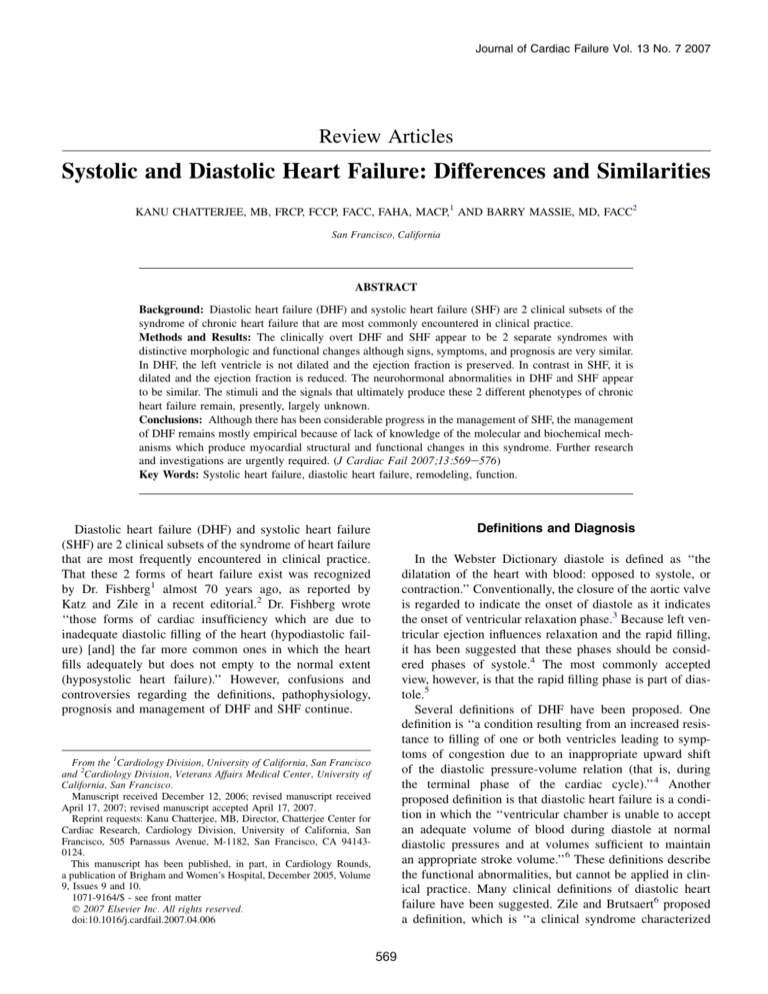
Definitions and Diagnosis
Diastolic heart failure (DHF) and systolic heart failure
(SHF) are 2 clinical subsets of the syndrome of heart failure
that are most frequently encountered in clinical practice.
That these 2 forms of heart failure exist was recognized
by Dr. Fishberg1 almost 70 years ago, as reported by
Katz and Zile in a recent editorial.2 Dr. Fishberg wrote
‘‘those forms of cardiac insufficiency which are due to
inadequate diastolic filling of the heart (hypodiastolic failure) [and] the far more common ones in which the heart
fills adequately but does not empty to the normal extent
(hyposystolic heart failure).’’ However, confusions and
controversies regarding the definitions, pathophysiology,
prognosis and management of DHF and SHF continue.
In the Webster Dictionary diastole is defined as ‘‘the
dilatation of the heart with blood: opposed to systole, or
contraction.’’ Conventionally, the closure of the aortic valve
is regarded to indicate the onset of diastole as it indicates
the onset of ventricular relaxation phase.3 Because left ventricular ejection influences relaxation and the rapid filling,
it has been suggested that these phases should be considered phases of systole.4 The most commonly accepted
view, however, is that the rapid filling phase is part of diastole.5
Several definitions of DHF have been proposed. One
definition is ‘‘a condition resulting from an increased resistance to filling of one or both ventricles leading to symptoms of congestion due to an inappropriate upward shift
of the diastolic pressure-volume relation (that is, during
the terminal phase of the cardiac cycle).’’4 Another
proposed definition is that diastolic heart failure is a condition in which the ‘‘ventricular chamber is unable to accept
an adequate volume of blood during diastole at normal
diastolic pressures and at volumes sufficient to maintain
an appropriate stroke volume.’’6 These definitions describe
the functional abnormalities, but cannot be applied in clinical practice. Many clinical definitions of diastolic heart
failure have been suggested. Zile and Brutsaert6 proposed
a definition, which is ‘‘a clinical syndrome characterized
From the 1Cardiology Division, University of California, San Francisco
and 2Cardiology Division, Veterans Affairs Medical Center, University of
California, San Francisco.
Manuscript received December 12, 2006; revised manuscript received
April 17, 2007; revised manuscript accepted April 17, 2007.
Reprint requests: Kanu Chatterjee, MB, Director, Chatterjee Center for
Cardiac Research, Cardiology Division, University of California, San
Francisco, 505 Parnassus Avenue, M-1182, San Francisco, CA 941430124.
This manuscript has been published, in part, in Cardiology Rounds,
a publication of Brigham and Women’s Hospital, December 2005, Volume
9, Issues 9 and 10.
1071-9164/$ - see front matter
Ó 2007 Elsevier Inc. All rights reserved.
doi:10.1016/j.cardfail.2007.04.006
569
570 Journal of Cardiac Failure Vol. 13 No. 7 September 2007
by the symptoms and signs of heart failure, a preserved
ejection fraction (EF), and abnormal diastolic function.’’
Other definitions such as ‘‘heart failure with preserved systolic function’’ or ‘‘heart failure with normal or near normal
ejection fraction’’ have also been used.
Several definitions of systolic heart failure also exist. In
1933, Sir Thomas Lewis defined heart failure as ‘‘a condition in which the heart fails to discharge its contents adequately.’’7 In 1980, Dr. Braunwald described heart failure
as ‘‘a pathophysiological state in which an abnormality of
cardiac function is responsible for the failure of the heart
to pump blood at a rate commensurate with the requirements of the metabolizing tissues.’’8 Although these definitions describe the pathologic mechanisms, it is difficult to
employ in clinical practice. Thus it is preferable to use
the terms ‘‘diastolic’’ and ‘‘systolic’’ heart failure as these
definitions describe the principal mechanisms.
Systolic and Diastolic Dysfunction and Clinical
Heart Failure
Systolic dysfunction from impaired contractile or pump
function and diastolic dysfunction from impaired ventricular relaxation, compliance or filling are not always associated with clinical heart failure characterized by signs and
symptoms of low cardiac output or of congestion. Furthermore, in SHF, diastolic dysfunction as assessed by changes
in the ventricular filling features is common, particularly in
advanced heart failure. In diastolic heart failure, left ventricular systolic performance, function and contractility in
general, remain normal.9 In some studies, long-axis systolic
dysfunction has been observed.10
Diagnosis
Based on the proposed definitions, it appears that for
establishing the diagnosis of DHF or SHF, it is only necessary to measure left ventricular ejection fraction after
confirming the presence of heart failure. If ejection fraction
is preserved it is DHF, and if reduced it is SHF. It is highly
desirable to establish the normal range of ejection fraction
for any technique employed, preferably under similar loading conditions. It should be appreciated that signs and
symptoms, radiologic and electrocardiographic findings
and neurohormonal profile cannot distinguish between
DHF and SHF.6,11
Is Cardiac Catheterization Necessary?
Coronary angiography is occasionally indicated when
myocardial ischemia is strongly suspected, irrespective of
type of heart failure. Similarly, endomyocardial biopsy is
rarely necessary to establish the etiology of heart failure.
Cardiac catheterization is not necessary to assess ejection
fraction, contractile function, or diastolic functions.
Incidence, Prevalence, and Prognosis
The incidence and prevalence of both SHF and DHF is
considerable and increasing.12,13 The recent epidemic
increase in heart failure in older population appears to be
related both to increase in the incidence and improved survival.14 The incidence of systolic and diastolic heart failure
has been reported to be 61% to 68% and 16% to 39%,
respectively.15 The cross-sectional population echocardiographic studies have reported that of patients diagnosed
with heart failure, 40% to 71% have DHF.15
Natural History of Asymptomatic Systolic and Diastolic
Dysfunction
Asymptomatic left ventricular systolic dysfunction constitutes Stage B systolic heart failure.16 The prevalence of
Stage B systolic heart failure in the community is between
3% and 6%.17 The risk of development of symptomatic
heart failure is reported to be between 5.1% and
10.5%.17e21
The echo-Doppler studies have reported that patients
with asymptomatic left ventricular diastolic dysfunction
have a higher incidence of all-case mortality adjusted for
age, sex, and ejection fraction.12 Mild diastolic dysfunction
was associated with 8.3-fold, and moderate-to-severe
dysfunction with 10.2-fold increased risk of mortality.12
Natural History in Symptomatic Patients
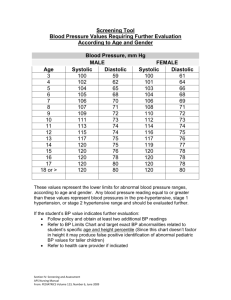
The overall mortality of symptomatic patients with DHF
or SHF is very similar22,23 and is related to the functional
class. In patients with New York Heart Association Class
II and III DHF, an annual mortality rate of 3.8% was
observed.24 In patients who required hospital admissions
for treatment, 1-year all cause death was 27% in DHF
and 36% in SHF25 (Fig. 1).
Mode of Death
In systolic heart failure approximately 50% of deaths are
sudden and the rate of sudden death in systolic heart failure
is 6 to 9 times higher compared with that in the general
population.26 Interestingly, with the increased severity of
systolic heart failure (New York Heart Association IV), incidence of sudden cardiac death decreases.27 The absolute
rates of pump failure death and sudden cardiac death
increases with decreasing left ventricular ejection
fraction.28 However, it has been reported that the risk of
sudden cardiac death is better correlated to left ventricular
mass than to the ejection fraction.29 The left ventricular
mass is increased considerably in both DHF and SHF;
thus, the risk assessment for sudden cardiac death based
on ejection fraction alone may not be appropriate. In a recent report, the risk of sudden cardiac death was found to be
only 7% among 2314 patients, compared with death from
other causes, which was 93%.30
Systolic and Diastolic Heart Failure
Chatterjee and Massie
571
Fig. 1. One-year mortality morbidity in patients with severe systolic (open bar) and diastolic (closed bar) heart failure. Although the mortality morbidity rate in patients with preserved systolic function is lower than that of patients with reduced systolic function, the mortality
rate in both groups with severe heart failure was high. (Published with permission of Dauterman KW, Go AS, Rowell R, Gebretsadik T,
Gettner S, Massie BM. Congestive heart failure with preserved systolic function in a statewide sample of community hospitals. J Card
Failure 2001;7:221e8.25)
Risk Factors
Older age, hypertension, diabetes, obesity, and coronary
artery disease are risk factors for both DHF and SHF. Although DHF is more common in elderly females, diastolic
dysfunction is more common in elderly males.31 In DHF,
hypertension is a more common risk factor.12 However,
a substantial proportion of patients with SHF have a history
of hypertension. In SHF, ischemic heart disease is the most
common etiology, but many patients with DHF have coronary artery disease. In decompensated heart failure, 63% of
patients with systolic and 54% of patients with diastolic
heart failure have coronary artery disease.32 Thus, for prevention, modification of the same risk factors should be
employed in both DHF and SHF.
Remodeling
The distinctive features of remodeling in DHF and SHF
are summarized in Table 1 and illustrated in Fig. 2.33,34 In
SHF, the left ventricular cavity size is increased with an
increase in both end-diastolic and end-systolic volumes,
Table 1. Morphologic and Functional Changes in Diastolic
vs Systolic Heart Failure
Parameters
Left ventricular
cavity size
Left ventricular mass
Mass/cavity
Wall thickness
End-diastolic stress
End-systolic stress
End-diastolic volume
End-systolic volume
Ejection fraction
Mechanical
dyssynchrony
Left ventricular
shape and geometry
Diastolic Heart
Failure
Systolic Heart
Failure
Normal or decreased
Increased
Increased
Increased
Increased
Increased
Normal
Normal
Normal or decreased
Normal
May be present
Increased
Normal or decreased
Decreased
Increased
Increased
Increased
Increased
Decreased
May be present
Usually remains
unchanged
Spherical
decreased or unchanged wall thickness, increased wall
stress, and reduced ejection fraction. The mass is increased,
but the mass/cavity ratio remains unchanged or is decreased. In SHF, there is an alteration in ventricular shape
and geometry with a greater increase in transverse than in
long axis, and mechanical dyssynchrony with or without
electrical dyssynchrony occur in a substantial number of
patients.35 In DHF, the cavity size remains unchanged or
may even decrease, and the end-diastolic and end-systolic
volumes remain normal or decrease. In DHF, there is usually an increase in wall thickness and mass; however,
mass/cavity ratio is substantially increased. In DHF, enddiastolic wall stress is increased and systolic wall stress
remains normal and ejection fraction remains normal or
may even be higher than normal.9,34 In DHF, significant alteration in ventricular shape and geometry is uncommon;
however, mechanical dyssynchrony may occur even without electrical dyssynchrony.35,36 The left ventricular morphologic and functional changes in DHF and SHF
compared to controls as evaluated by echocardiographic
studies are summarized in Table 2.11
The differences in the structural changes in systolic and
diastolic heart failure are summarized in Table 3 and illustrated in Fig. 3. In SHF there is myocyte lengthening and an
increase in myocyte length/width ratio. The sarcomeres are
replicated in parallel. In DHF there is an increase in the myocyte cross-sectional area with little or no change in its
length/width ratio. The sarcomeres are replicated in parallel. The abnormality in calcium regulation occurs in both
types of heart failure. Increased collagen volume and fibrosis occur in both but the character and degree of fibrosis
appear to be different. In animal models, in SHF, there is
degradation and disruption of fibrillar collagen; in contrast,
in the pressure-overloaded hypertrophy which is associated
with diastolic failure, there is an increase in collagen with
increased width and continuity of the fibrillar collagen.34
The collagen cross links are decreased in SHF and
increased in DHF. In general the matrix metalloproteinases
572 Journal of Cardiac Failure Vol. 13 No. 7 September 2007
Fig. 2. Ventricular remodeling in systolic and diastolic heart failure. (Left) Autopsy examples; (right) cross-sectional 2-dimensional echocardiographic views of systolic and diastolic heart failures compared with normals are illustrated. In systolic heart failure, the left ventricular cavity is markedly dilated and wall thickness is not increased. In diastolic heart failure, the cavity size is normal or decreased and wall
thickness is markedly increased. (Reprinted with permission.33)
are increased in SHF and decreased in DHF. In contrast,
their endogenous tissue inhibitors tend to decrease in
SHF and increase in DHF.37,38 Other biochemical evidences
for abnormal collagen metabolism such as increased circulating levels of amino-terminal propeptide of Type III procollagen have been reported in systolic heart failure.39 The
titin isoforms N2BA/N2B ratio is decreased in systolic failure and it is increased in diastolic failure.2 Left ventricular
endomyocardial biopsy studies have reported an increase in
myocyte diameter and less decrease in myocyte volume in
Table 2. Echocardiographic Left Ventricular Morphologic
and Functional Characteristics in Primary Systolic and
Diastolic Heart Failure Compared With Controls
Controls
LVEDV (mL) 102 6 12
LVESV (mL) 46 6 11
LVEF %
54 6 2
LV mass (g) 125 6 12
LV mass/
1.49 6 0.17
volume
NE pg/mL
169
BNP pg/mL
3
Systolic Heart
Failure
192
137
31
232
1.22
6
6
6
6
6
10*
9*
2*
9*
0.14
287
28
DHF compared with SHF, whereas collagen volume
fractions increased in both types.40
The initiating stimuli for remodeling in SHF and DHF
have not been clearly delineated. In SHF, after acute myocardial infarction, the extent of myocardial injury and the
magnitude of left ventricular systolic dysfunction appear
to be the major determinants. A small infarct and relatively
preserved ejection fraction is not usually associated with
ventricular remodeling.41,42 Abnormal neurohormonal activation has also been implicated as a major mechanism for
progressive remodeling in systolic heart failure.43
In DHF, the stimuli for ventricular remodeling remain
unclear. The pressure overload resulting from hypertension
Diastolic Heart
Failure
Table 3. Diastolic and Systolic Heart Failure Remodeling:
Myocyte and Matrix Changes
6
6
6
6
6
Systolic Heart
Failure
Diastolic Heart
Failure
þ
þ
þ
þ
e
þ
e
e
þ
þ
þ
þ
e
e
þ
þ
87
37
60
160
2.12
10
9
2y
9y
0.14z
306; P 5 .007
56; P 5 .02
Adapted from Kitzman DW, et al. JAMA 2002;288:2144e50.11
LVEDV, left ventricular end-diastolic volume; LVESV, left ventricular
end-systolic volume; LVEF, left ventricular ejection fraction; LV, left
ventricle; NE, norepinephrine; BNP, B-type natriuretic peptide.
*Systolic heart failure vs. controls, P ! .001.
y
Diastolic heart failure vs. controls, P ! .001.
z
Diastolic heart failure vs. controls, P ! .002.
Myocyte
Hypertrophy
Apoptosis
Necrosis
Myocardial fibrosis
Calcium regulation
MMPs/TIMPs
Collagen cross-links
Titin isoforms N2BA/
N2B
þ, increased; e, decreased or impaired; MMPs, matrix metalloproteinases; TIMPs, tissue inhibitors of metalloproteinases.
Systolic and Diastolic Heart Failure
Chatterjee and Massie
573
Fig. 3. Changes in myocytes (left) and in extracellular matrix (right) in systolic heart failure resulting from dilated cardiomyopathy, and
diastolic heart failure resulting from pressure over load compared with normals in animal models. In systolic heart failure, the myocyte
length is increased without any change in the cross-sectional area; in diastolic heart failure, the cross-sectional area of the myocyte is increased without a significant change in its length. In systolic heart failure, collagen degradation and disruption occur; in diastolic heart
failure, there is increased width and continuity of fibrillar collagen. (Reprinted with permission.34)
and obesity associated with concentric hypertrophy is likely
to be an important contributing factor. Neurohormonal abnormalities, similar to those observed in systolic heart failure, occur in DHF.11 Thus neurohormonal abnormalities do
not explain differences in ventricular remodeling in DHF
and SHF. It is possible that neurohormonal abnormalities
produce different substrate response in DHF and SHF.
Functional Changes
In SHF, impaired contractile function is the principal
functional derangement and is the major mechanism for reduced ejection fraction (Fig. 3).34,44 The other mechanism
for reduced ejection fraction in SHF is increased wall
stress. Diastolic function, as assessed by echo-Doppler
studies, is frequently abnormal in patients with overt SHF.
Impaired left ventricular relaxation and increased passive
stiffness is the principal functional derangement in DHF.34
The pressure-volume relation during diastole shifts upward
and to the left (Fig. 4); as a result there is a disproportionately greater increase in diastolic pressure for any increase
in volume.45
The hemodynamic profile may be similar in SHF and
DHF. In SHF, reduced ejection fraction results in a decrease
in stroke volume and cardiac output. Increased left ventricular end-diastolic volumes and often associated abnormal
Fig. 4. Schematic diagram of pressure-volume relations in normals, systolic and diastolic heart failure. In systolic heart failure, a downward
and rightward shift of the end-systolic pressure-volume line indicates decreased contractile function, which is the principal cause of reduced
ejection fraction and forward stroke volume. In primary diastolic heart failure, diastolic pressure-volume relation (dashed line) shifts upward and to the left, indicating a disproportionate and a greater increase in diastolic pressure for any increase in diastolic volumes. If there
is also a decrease in end-diastolic volume, then a decrease in stroke volume also occurs. (Reprinted with permission.44)
574 Journal of Cardiac Failure Vol. 13 No. 7 September 2007
Fig. 5. The changes in the diastolic pressure-volume relation in patients with overt diastolic heart failure, illustrating its shifts upward and to
the left. (Reprinted with permission.45)
diastolic filling result in increased left ventricular diastolic
pressure, a passive increase in left atrial and pulmonary
venous pressure, and postcapillary pulmonary arterial
hypertension. Right ventricular failure and systemic venous
hypertension and its hemodynamic and clinical consequences occur.
In DHF, because of the disproportionate increase in left
ventricular diastolic pressure, there is an increase in left
atrial and pulmonary venous pressure that is associated
with symptoms and signs of pulmonary venous congestion
(Fig. 5).45 Postcapillary pulmonary hypertension resulting
from increased pulmonary venous pressure may precipitate
right heart failure. Left ventricular stroke volume and cardiac output may also decline because of decreased enddiastolic volume (preload dependent). Chronic elevation
of pulmonary venous pressure may be associated with
increased pulmonary vascular resistance from secondary
pulmonary vasoconstriction, which may occur in both
SHF and DHF.
Does Left Ventricle Dilate in Diastolic Heart Failure?
Left ventricular dilation always occurs in SHF. In DHF,
however, left ventricular dilation does not appear to occur
without an additional insult such as myocardial infarction.
In some patients with DHF without coronary artery disease,
serial assessment of ventricular volumes and pressures and
stiffness have been performed; end-diastolic volumes and
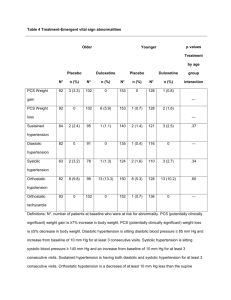
Table 4. Changes in Left Ventricular End Diastolic
Volumes (LVEDVI) and Pressures (LVEDP), Ejection
Fraction (LVEF), and Left Ventricular Stiffness Modulus
(Stiff-Mod) During 64 6 9 Months in Patients With DHF
Initial
LVEDVI mL/m2
LVEF %
LVEDP mm Hg
Stiff-Mod kN/m2
68
67
14
3.4
Published with permission.46
*P ! .05 follow-up vs. initial.
6
6
6
6
9
3
3
0.6
End of Follow-up
76
60
26
6.3
6
6
6
6
8
4
2*
0.9*
ejection fraction remain unchanged, but end-diastolic pressure and stiffness index increase, suggesting that in DHF
ventricular dilatation does not occur and worsening
diastolic function is the mechanism for development and
progression of heart failure (Table 4).46,47 Thus left ventricle size remains unchanged and it does not dilate without an
ischemic insult.
Differences in Therapeutic Options
Although there have been considerable advances in the
treatment of SHF, very little progress has been made in
the management of DHF. The improvement in prognosis
in SHF is most likely related to the therapeutic discoveries
that have been observed to attenuate adverse remodeling
and improve hemodynamic abnormalities. The neurohormonal modulators such as renin-angiotensin-aldosterone
and adrenergic antagonists clearly improve symptoms and
quality of life and decrease mortality. So far no such therapies have been discovered for improving prognosis in
patients with DHF. Angiotensin receptor blocking agents
have the potential for decreasing morbidity but not mortality.24 It has been reported that statin therapy has the potential to decrease mortality of patients with DHF.48 Statin
therapy is also associated with lower mortality in SHF.49
Chronic resynchronization therapy with or without
implantable cardioverter defibrillator improves prognosis
of patients with SHF. However, chronic resynchronization
therapy has not been shown to produce beneficial effects
in DHF. Cardiac transplantation is likely to benefit selected
patients either with SHF or DHF.
Conclusion
Established clinical systolic and diastolic heart failure
appear to be 2 distinct syndromes of chronic heart failure.
The myocardial structural and primary functional derangements are distinctive in these 2 syndromes, although hemodynamic consequences, clinical presentations, signs and
symptoms, and prognosis are similar. The neurohormonal
abnormalities are also similar in both of these syndromes.
Although there have been considerable advances in the
Systolic and Diastolic Heart Failure
management of systolic heart failure, the management of
DHF remains primarily to relieve symptoms. Because of inadequate knowledge of the molecular and biochemical
mechanisms of the structural remodeling and principal
functional derangement in diastolic heart failure, treatments
to improve prognosis have not evolved. Thus further basic
science and clinical research is urgently required. However,
potential exists for discovery of therapeutic agents to
improve fundamental abnormalities of the cytoskeleton
and myocardial architecture and thereby decrease myocardial stiffnessdthe principal functional derangement in
diastolic heart failure. Until then the treatment of diastolic
heart failure will remain empirical.
17.
18.
19.
20.
Acknowledgment
21.
The authors are grateful to Marci Yellin for her invaluable assistance in preparing the manuscript.
22.
References
23.
1. Fishberg AM. Heart failure. Philadelphia: Lea & Febiger; 1937.
2. Katz AM, Zile MR. New molecular mechanism in diastolic heart
failure. Circulation 2006;113:1922e5.
3. Wiggers CJ. Studies on the consecutive phase of the cardiac cycle.
1. The duration of the consecutive phases of the cardiac cycle and
the criteria for their precise determination. Am J Physiol 1921;56:415.
4. Brutsaert DL, Sys SU, Gillebert TC. Diastolic failure: pathophysiology and therapeutic implications. J Am Coll Cardiol 1993;22:318e25.
5. Wiggers CJ. Studies on the consecutive phases of the cardiac cycle II.
The laws governing the relative durations of ventricular systole and
diastole. Am J Physiol 1921;56:439e59.
6. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and
diastolic heart failure: part I: diagnosis, prognosis, and measurements
of diastolic function. Circulation 2002;105:1387e93.
7. Lewis T. Diseases of the heart. London, UK: MacMillan; 1933.
8. Braunwald E. Clinical manifestations of heart failure. In:
Braunwald E, editor. Heart disease: a textbook of cardiovascular medicine. 1st ed. Philadelphia: WB Saunders; 1980. p. 493.
9. Baicu CF, Zile MR, Aurigemma GP, Gaasch WH. Left ventricular systolic performance, function and contractility in patients with diastolic
heart failure. Circulation 2005;111:2306e12.
10. Vinereanu D, Nicolaides E, Tweddel AC, Fraser AG. ‘‘Pure’’ diastolic
dysfunction is associated with long-axis systolic dysfunction. Implications for the diagnosis and classification of heart failure. Eur J Heart
Fail 2005;7:820e8.
11. Kitzman DW, Little WC, Brubaker PH, et al. Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic
heart failure. JAMA 2002;288:2144e50.
12. Redfield MM, Jacobson SJ, Burnett JC, et al. Burden of systolic and
diastolic ventricular dysfunction in the community: appreciating the
scope of the heart failure epidemic. JAMA 2003;289:194e202.
13. McMurray JV, Pfeffer M. Heart failure. Lancet 2005;365:1877e89.
14. Barker WH, Mulloly JP, Getchell W. Changing incidence and survival
for heart failure in a well-defined older population, 1970e1974 and
1990e1994. Circulation 2006;113:799e805.
15. Hogg K, Swedberg K, McMurray J. Heart failure with preserved left
ventricular systolic function; epidemiology, clinical characteristics,
and prognosis. J Am Coll Cardiol 2004;43:317e27.
16. Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the
evaluation and management of chronic heart failure in the adult:
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
Chatterjee and Massie
575
executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines
(Committee to revise the 1995 Guidelines for the Evaluation and
Management of Heart Failure). J Am Coll Cardiol 2001;38:
2101e13.
Wang TJ, Levy D, Benjamin EJ, Vasan RS. The epidemiology of
‘‘asymptomatic’’ left ventricular systolic dysfunction: implications
for screening. Ann Intern Med 2003;138:907e16.
Effect of enalapril on mortality and the development of heart failure in
asymptomatic patients with reduced left ventricular ejection fractions.
The SOLVD Investigators. N Engl J Med 1992;327:685e91.
Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on
mortality and morbidity in patients with left ventricular dysfunction
after myocardial infarction. Results of the survival and ventricular
enlargement trial. The SAVE Investigators. N Engl J Med 1992;
327:669e77.
Sharpe N, Murphy J, Smith H, Hanan S. Preventive treatment of
asymptomatic left ventricular dysfunction following myocardial
infarction. Eur Heart J 1990;11(Suppl B):147e56.
Kober L, Torp-Pedersen C, Carlsen JE, et al. A clinical trial of the
angiotensin-converting-enzyme inhibitor trandolapril in patients with
left ventricular dysfunction after myocardial infarction. Trandolapril
Cardiac Evaluation (TRACE) Study Group. N Engl J Med 1995;333:
1670e6.
Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med
2006;355:251e9.
Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med
2006;355:260e9.
Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in
patients with chronic heart failure and preserved left-ventricular
ejection fraction: The CHARM-Preserved Trial. Lancet 2003;362:
777e81.
Dauterman KW, Go AS, Rowell R, et al. Congestive heart failure with
preserved systolic function in a statewide sample of community
hospitals. J Card Fail 2001;7:221e8.
American Heart Association. Heart disease and stroke statisticsd2003
update. Dallas, TX: American Heart Association; 2002.
MERIT-HF Investigators. Effect of metoprolol CR/XL in chronic heart
failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-CF). Lancet 1999;353:2001e7.
Solomon S, Olofsson B, Finn P, et al. Causes of death across full spectrum of ventricular function in patients with heart failure: The Charm
Study:[abstract]. J Am Coll Cardiol 2004;45:180A.
Turakhia M, Ali S, Schiller NB, et al. Left ventricular mass predicts
death and sudden death in patients with CAD regardless of ejection
fraction: data from the Heart and Soul Study. Circulation 2006;114:
II-400.
Al-Khatib SM, Shaw L, O’Connor CM, et al. Sudden cardiac death in
patients with diastolic heart failure. Circulation 2006;114:II-404.
Fischer M, Baessler A, Hense HW, et al. Prevalence of left ventricular
diastolic dysfunction in the community. Results from a Doppler echocardiographic-based survey of a population sample. Eur Heart J 2003;
24:320e8.
Fonarow GC, ADHERE Scientific Advisory Committee. The Acute
Decompensated Heart Failure National Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure:[review]. Rev Cardiovasc Med 2003;4(Suppl 7):
S21e30.
Konstam MA. Systolic and diastolic dysfunction in heart failure? Time
for a new paradigm. J Cardiac Failure 2003;9:1e3.
Aurigemma GP, Zile MR, Gasch WH. Contractile behavior of the left
ventricle in diastolic heart failure. Circulation 2006;113:296e304.
Wang J, Kurrelmeyer KM, Torre-Amione N, Nagueh SF. Systolic
and diastolic dyssynchrony in patients with diastolic heart failure
and the effect of medical therapy. J Am Coll Cardiol 2007;49:
88e96.
576 Journal of Cardiac Failure Vol. 13 No. 7 September 2007
36. Chatterjee K. Diastolic and systolic heart failuredsimilarities and
differencesdpart I. Cardiol Rounds 2005;9:9.
37. Spinale FG. Matrix metalloproteinases: regulation and dysregulation
in the failing heart. Circ Res 2002;90:520e30.
38. Ahmed SH, Clark LL, Pennington WR, et al. Matrix metalloproteinases/tissue inhibitors of metalloproteinases: relationship between
changes in proteolytic determinants of matrix composition and structural, functional, and clinical manifestations of hypertensive heart
disease. Circulation 2006;113:2089e96.
39. Rossi A, Cicoira M, Golia G, et al. Amino-terminal propeptide of type
III procollagen is associated with restrictive mitral filling pattern in patients with dilated cardiomyopathy: a possible link between diastolic
dysfunction and prognosis. Heart 2004;90:650e4.
40. Heerbeek LV, Borbe’ly A, Hans WM, et al. Myocardial structure and
function differ in systolic and diastolic heart failure. Circulation 2006;
113:1966e73.
41. Pfeffer MA, Janice M. Pfeffer memorial lecture. J Card Fail 2002;
8(Suppl 6):S248e52.
42. Bolognese I, Neskovic AN, Parodi G, et al. Left ventricular remodeling after primary coronary angioplasty: patterns of left ventricular
dilation and long-term prognostic implications. Circulation 2002;
106:2351e7.
43. Chatterjee K, De Marco T, McGlothlin D. Remodeling in systolic
heart failuredeffects of neurohormonal modulators: basis for current
pharmacotherapy. Cardiology Today 2005;9:270e7.
44. Aurigemma GP, Gaasch WH. Diastolic heart failure. N Engl J Med
2004;35:1097e1105.
45. Zile MR, Baicu CF, Gaasch WH. Diastolic heart failuredabnormalities in active relaxation and passive stiffness of the left ventricle.
N Engl J Med 2004;350:1953e9.
46. Handoko ML, Heerbeek LV, et al. Does diastolic heart failure evolve
to systolic heart failure?:[abstract]. Circulation 2006;114(Suppl II):
816.
47. Melenovsky V, Borlaug BA, Rosen B, et al. Cardiovascular features of
heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol
2007;49:198e207.
48. Fukuta H, Sane DC, Brucks S, Little WC. Statin therapy may be associated with lower mortality in patients with diastolic heart failure:
a preliminary report. Circulation 2005;112:357e63.
49. Mozaffarian D, Nye R, Levy WC. Statin therapy is associated with
lower mortality among patients with severe heart failure. Am J Cardiol
2004;93:1124e9.