VIEW PDF - Cataract & Refractive Surgery Today Europe
advertisement

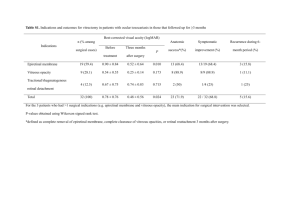
Today’s PRactice Bonus Feature The Vitreomacular Interface After LASIK Epiretinal membranes and macular holes may occur, although rarely, after refractive surgery. By Hugo Quiroz-Mercado, MD; and Miguel Paciuc-Beja, MD C omplications from refractive surgery are related mostly to refractive outcomes. Retinal complications after LASIK can include retinal tears, retinal detachment, choroidal neovascularization, subretinal hemorrhage, epiretinal membrane, and macular hole. Fortunately, such complications are rare; the incidence of vitreoretinal complications after LASIK has been estimated to be between 0.06% and 0.36%.1 It is not easy to relate vitreomacular pathology directly to LASIK surgery. When we perform LASIK, we do not typically think about its potential effect on the vitreomacular interface (VMI). Additionally, there may be weeks or even months between the time LASIK is performed and the occurrence of vitreomacular symptoms. It is difficult to know whether the LASIK surgery or the patient’s myopia is the root cause; the aforementioned complications, although uncommon, occur at a higher incidence in patients with myopia—the majority of patients undergoing LASIK. POSTERIOR VITREOUS DETACHMENT Availability of optical coherence tomography (OCT) has changed the way we visualize the retina, the vitreous, and the VMI, in the same way that corneal topography and pachymetry changed the way we see the cornea. Vitreomacular complications observed after LASIK share a common pathophysiology: posterior vitreous detachment (PVD). With the help of OCT and ultrasonography, we can see that the incidence of PVD is higher in patients who have undergone LASIK compared with the expected incidence in patients with similar characteristics in whom the procedure was not performed. That is to say, there is a cause-and-effect relationship between LASIK and PVD. Ultrasonography has shown that, after myopic microkeratome-assisted LASIK, 14% of eyes had PVD. Another study showed an incidence of post-LASIK PVD of 9.5%, and B-scan ultrasonography demonstrated that 16% of eyes had PVD 48 hours after LASIK in which a femtosecond laser was used to create the 30 Cataract & Refractive Surgery Today Europe January 2014 Figure 1. Case No. 1: Color fundus photograph of the left eye. The macular region shows macular folds and distortion of the normal architecture of the juxtafoveal vessels. Nasal and inferior to the fovea, there is evidence of epiretinal fibrous tissue, which is likely due to the presence of an epiretinal membrane. flap. Numerous studies are consistent with an incidence of post-LASIK PVD of greater than 10%.2-4 According to autopsy studies, PVD is present in less than 10% of individuals younger than 50 years.5 It has been suggested that post-LASIK PVD may be caused either by deformation of the eye secondary to increased intraocular pressure (IOP) with the application of the corneal suction ring or by trauma as a result of the shockwave induced by the excimer laser. Deformation of the eye theoretically occurs when the suction ring induces an increase in IOP, which can rise above 80 mm Hg. The suction and the increase in IOP could elongate the eye along the anteroposterior axis and, in turn, cause a contraction in the horizontal axis. This combination of events may push the lens anteriorly and cause vitreoretinal traction at the vitreous base and the posterior pole, facilitating PVD. Today’s PRactice Bonus Feature A B Figure 2. Case No. 1: Time-domain OCT of the left eye shows complete distortion of internal and external architecture of the retina nasal and inferior to the fovea. Over the retina, there is a highly reflective membrane, which makes contact with the retina in the central part of the projection. The nerve fiber layer shows a characteristic saw-like configuration. There is a substantial increase in retinal thickness. Could trauma caused by the excimer laser shockwave induce PVD? Stress wave amplitudes of up to 100 atm, 6.2 to 7.3 mm behind the endothelium, have been measured during experimental LASIK. At the retinal plane, 23 mm behind the endothelium, the stress wave amplitude fell to approximately 10 atm, which seems to be insufficient to cause a significant retinal lesion.6 PVD has been widely associated with the occurrence of epiretinal membrane (ERM). Separation of the vitreous from the inner retinal surface usually occurs due to the aging process and is more common in myopic eyes. It may also occur as a consequence of trauma or inflammation at any age. PVD has been shown to cause small breaks in the internal limiting membrane, through which glial cells may grow and proliferate on the retinal surface. With PVD progression, residual vitreous is often left on the inner retinal surface. Residual vitreous remains on the surface of the retina in nearly half of eyes with PVD.7 This is called vitreoschisis. ERMs are composed of Take-Home Message • Vitreomacular complications observed after LASIK share the common pathophysiology of PVD. • PVD, which occurs in about 10% of patients after LASIK, can cause vitreomacular traction. • Macular OCT is advisable in patients with unexplained visual symptoms after LASIK. Figure 3. Case No. 2: Seven months after successful LASIK, a 21-year-old woman presented with sudden onset of metamorphopsia. OCT showed an inner segment ellipsoid band loss at the subfoveal area in the patient’s right eye (A). One month later, OCT revealed a stage 3 macular hole (B). glial cells that attach to vitreous cortex remnants on the inner retinal surface. CASE REPORT NO. 1 A 29-year-old man underwent uneventful LASIK in both eyes. Cycloplegic refraction was -2.50 D sphere in each eye. Corneal pachymetry was 549 µm in the right eye and 530 µm in the left. Dilated funduscopy was unremarkable, and no PVD was noted. LASIK was performed using the Hansatome microkeratome (Basuch + Lomb) with a 160-µm flap and the Visx Star S4 excimer laser (now Abbott Medical Optics Inc.). Visual acuity was 20/20 OU after 6 months. Dilated funduscopy revealed PVD in both eyes. Eighteen months after surgery, visual acuity remained 20/20 OU, but the patient complained of metamorphopsia in his left eye. In this eye, funduscopy revealed an ERM with thin macular folds (Figure 1). Stratus OCT (Carl Zeiss Meditec) of the macula showed a hyperreflective line partially in contact with the retinal surface, folds in the interior layers of the retina, retinal thickening, and distortion of the normal retinal architecture (Figure 2). (Continued on page 37) January 2014 Cataract & Refractive Surgery Today Europe 31 Today’s PRactice Bonus Feature (Continued from page 31) CASE REPORT NO. 2 A 21-year-old woman was seen in our retina clinic because of sudden onset of metamorphopsia in her right eye. Visual acuity was 20/25 OD and 20/20 OS. The patient had no history of trauma or ocular inflammation. She reported having undergone successful LASIK 7 months earlier. Fundus examination of the right eye showed PVD, Amsler grid testing showed a central area of metamorphopsia, and Spectralis OCT (Heidelberg Engineering) showed loss in the inner segment ellipsoid band at the subfoveal area (Figure 3A). There were no abnormal findings in the left eye. One month later, she complained of a sudden decrease in visual acuity in her right eye and a large central scotoma. Her BCVA was 20/200 OD and 20/20 OS. Funduscopy showed a full-thickness macular hole, and OCT revealed a stage 3 macular hole (Figure 3B). CONCLUSION Excessive traction on the macula can lead to anatomic changes in the contour of the foveal surface. OCT and ultrasonography suggest that macular holes are caused by tractional forces related to perifoveal vitreous detachment. Idiopathic macular holes can be viewed as a complication of early stages of PVD. In theory, a PVD caused by vitreoretinal traction could lead to a macular hole. Retinal complications, although uncommon, can occur after LASIK. PVD occurs in about 10% of patients after LASIK and can cause vitreomacular traction. Macular OCT is therefore necessary to investigate unexplained visual symptoms after LASIK. n Hugo Quiroz-Mercado, MD, is a Professor at the University of Colorado School of Medicine. Dr. QuirozMercado states that he has no relevant financial interests to disclose. Miguel Paciuc-Beja, MD, is an Associate Professor at the University of Colorado School of Medicine. Dr. PaciucBeja states that he has no relevant financial interests to disclose. He may be reached at tel: +303 602 8574; e-mail: miguel.paciuc@dhha.org. 1. Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149(3):371-382. 2. Luna JD, Artal MN, Reviglio VE, Pelizzari M, Diaz H, Juarez CP. Vitreoretinal alterations following laser in situ keratomileusis: clinical and experimental studies. Graefes Arch Clin Exp Ophthalmol. 2001;239(6):416-423. 3. Mirshahi A, Schopfer D, Gerhardt D, Terzi E, Kasper T, Kohnen T. Incidence of posterior vitreous detachment after laser in situ keratomileusis. Graefes Arch Clin Exp Ophthalmol. 2006;244(2):149-153. 4. Gavrilov JC, Gaujoux T, Sellam M, Laroche L, Borderie V. Occurrence of posterior vitreous detachment after femtosecond laser in situ keratomileusis: ultrasound evaluation. J Cataract Refract Surg. 2011;37(7):1300-1304. 5. Foos RY, Wheeler NC. Vitreoretinal juncture: synchysis senilis and posterior vitreous detachment. Ophthalmology. 1982;89:1502-1512. 6. Krueger RR, Seiler T, Gruchman T, Mrochen M, Berlin MS. Stress wave amplitudes during laser surgery of the cornea. Ophthalmology. 2001;108:1070-1074. 7. Duker J, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611-2619. January 2014 Cataract & Refractive Surgery Today Europe 37