Clinical Psychology Review 26 (2006) 679 – 694
The social zeitgeber theory, circadian rhythms, and mood disorders:
Review and evaluation
Louisa D. Grandin a,⁎, Lauren B. Alloy a , Lyn Y. Abramson b
b
a
Temple University, Weiss Hall, 6th Floor, 1701 N. 13th St., Phila. PA 19122, United States
University of Wisconsin, 410 Brogden Hall, 1202 West Johnson Street, Madison WI 53706, United States
Received 21 February 2006; received in revised form 24 June 2006; accepted 6 July 2006
Abstract
The social zeitgeber theory [Ehlers, C. L., Frank, E., & Kupfer, D. J. (1988). Social zeitgebers and biological rhythms. Archives
of General Psychiatry, 45, 948–952] offers an explanation of how life events trigger depressive episodes. According to this theory,
life stress leads to mood episodes by causing disruptions in individuals' social routines and, in turn, their biological circadian
rhythms. In this article, we review the literature pertaining to the social zeitgeber theory, as well as evidence that this theory may be
applied to (hypo)manic episodes. Given the limited data supporting the social zeitgeber theory to date, we also evaluate whether
circadian rhythm disruptions are triggered by an internal mechanism, such as an abnormality in one's pacemaker (the
suprachiasmatic nucleus; SCN). We review these two theories in an attempt to understand the potential causes of circadian rhythm
disruptions and affective episodes in individuals with unipolar and bipolar disorders. We also propose several areas of future
research.
© 2006 Elsevier Ltd. All rights reserved.
Contents
1.
2.
3.
4.
Introduction . . . . . . . . . . . . . . . . . . .
1.1. Mood disorders . . . . . . . . . . . . . .
1.2. Life events . . . . . . . . . . . . . . . .
1.3. Social zeitgebers and social rhythms . . .
1.4. Biological rhythms . . . . . . . . . . . .
Life events, social rhythms, and mood . . . . . .
2.1. Life events and mood . . . . . . . . . . .
2.2. Life events, social zeitgebers and rhythms
2.3. Summary . . . . . . . . . . . . . . . . .
Social zeitgebers and biological rhythms. . . . .
3.1. Summary . . . . . . . . . . . . . . . . .
Circadian rhythms and mood. . . . . . . . . . .
4.1. Social rhythms and mood . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
⁎ Corresponding author. Tel.: +1 617 855 3389; fax: +1 215 204 5539.
E-mail address: lgrandin@temple.edu (L.D. Grandin).
0272-7358/$ - see front matter © 2006 Elsevier Ltd. All rights reserved.
doi:10.1016/j.cpr.2006.07.001
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
680
681
681
682
683
683
684
684
685
686
687
688
688
680
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
4.2. Psychotherapy and mood: Implications for the social
4.3. Summary. . . . . . . . . . . . . . . . . . . . . . .
5. Summary of limitations and directions for future research .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . .
zeitgeber
. . . . .
. . . . .
. . . . .
theory
. . . .
. . . .
. . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
689
689
690
691
1. Introduction
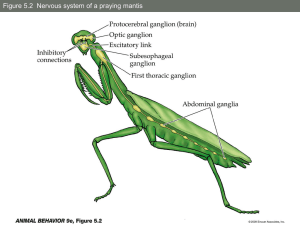
Ehlers, Frank, and Kupfer (1988) proposed that depressive episodes arise as a consequence of life events
disturbing social zeitgebers (external cues that function to entrain biological rhythms) which, in turn, derail social
and biological rhythms. According to this theory, disruptions in these rhythms influence somatic symptoms (e.g.,
sleep propensity) that in vulnerable individuals leads to a major depressive episode (see Fig. 1). This theory was, in
part, derived from the substantial evidence that depressed individuals have irregular biological rhythms, such as
sleep–wake cycles, temperature, melatonin, and cortisol rhythms (Howland & Thase, 1999). Recent evidence
suggests that the social zeitgeber theory may also explain (hypo)manic episodes of individuals with bipolar disorder
(Frank et al., 2005; Malkoff-Schwartz et al., 2000, 1998).
In this review, we elaborate on the associations proposed by the social zeitgeber theory, including its relevance to
hypo(manic) episodes. Second, we focus on possible causes of circadian rhythm disruptions in unipolar and bipolar
individuals. Consistent with the social zeitgeber theory, we will review studies suggesting that life events (external
triggers) may trigger circadian rhythm disruptions and, consequently, affective episodes in vulnerable individuals (see
Fig. 1). Alternatively, we will also discuss studies that suggest these circadian rhythm disruptions are due to a stable,
trait-like, dysfunction in vulnerable individuals. We suggest that this stable dysfunction may be a biological
abnormality in unipolar and bipolar individuals' pacemakers. For reasons of parsimony, we term this theory the
“internal trigger” theory, referring to an abnormality within the body, such as a genetic mutation. The “internal trigger”
hypothesis is contrasted with the social zeitgeber theory, an “external trigger” hypothesis (see Fig. 1). In this review, we
use the social zeitgeber theory interchangeably with the external trigger hypothesis.
Evidence for each proposed causal link of the social zeitgeber theory, or the five associations numbered in Fig. 1, is
discussed in turn. First, we review the association of life events, social zeitgebers and rhythms, and mood (see Fig. 1).
Next, we discuss the association of social and biological rhythm disruptions (pathway 3 in Fig. 1). We then review the
Fig. 1. Description of the internal trigger and external trigger theories.
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
681
association of biological rhythm disruptions and mood (pathways 4 and 5 in Fig. 1). In each section, we specifically
discuss how the findings pertain to the internal or external trigger hypotheses, or both. We begin by providing
necessary background on the definition and assessment of mood disorders, life events, social zeitgebers, social
rhythms, and biological rhythms in this literature.
1.1. Mood disorders
A major depressive episode is diagnosed when an individual experiences five or more depressive symptoms for two
weeks (for symptoms see Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision (DSM
IV-TR), American Psychiatric Association [APA], 2000). It is also possible that individuals may experience less severe
episodes, or minor depressive episodes, which require fewer symptoms as well as a shorter duration and less
persistence of these symptoms (see Research Diagnostic Criteria; Spitzer, Endicott, & Robins, 1978). The majority of
the studies reviewed only included individuals who had experienced major depressive episodes in their study groups;
however, some studies did not make a distinction between participants who experienced minor or major depression. We
will make this distinction whenever possible in reviewing the studies, as some studies did find differences between
these subtypes (e.g., Brown et al., 1996). We also distinguish between individuals with clinical depression (e.g.,
individuals who have experienced a major or minor depressive episode) and individuals who have experienced only
depressive symptoms. In short, we categorize individuals who have experienced a major or minor depressive episode
(but not a manic or hypomanic episode) as unipolar depressed.
Individuals with bipolar disorder experience hypomanic or manic episodes as well as depressive episodes (although
a depressive episode is not necessary for a bipolar diagnosis). Individuals diagnosed with bipolar I disorder experience
at least one manic episode (and typically, at least one major depressive episode as well). Individuals diagnosed with
bipolar II disorder experience at least one hypomanic episode, which is less severe and persistent than mania (see APA,
2000). In this review, bipolar disorder refers to individuals with bipolar I disorder unless otherwise specified.
Most studies utilize the Structured Clinical Interview for DSM version III-R (SCID; Spitzer, Williams, Gibbon, &
First, 1990) or the Schedule for Affective Disorders and Schizophrenia-Lifetime version (SADS-L; Endicott & Spitzer,
1978) to diagnosis individuals with bipolar or unipolar disorder. Several studies have examined the reliability and
validity of the SCID diagnoses (Segal, Kabacoff, Hersen, Van Hasselt, & Ryan, 1995; Skre, Onstad, Torgerson, &
Kringlen, 1991; Williams et al., 1992; Zanarini & Frankenburg, 2001). In general, the kappas from these studies for
diagnoses range from 0.5 to 1.0. In regards to its validity, several studies have used the SCID as the “gold standard” in
determining the accuracy of clinical diagnoses (e.g., Shear et al., 2000; Steiner, Tebes, Sledge, & Walker, 1995).
Studies also have found high reliability coefficients for the SADS-L interview, particularly for current and past
diagnoses of mood disorders (Alloy & Abramson, 1999; Alloy et al., 2000; Hammen, 1991; Reilly-Harrington, Alloy,
Fresco, & Whitehouse, 1999).
1.2. Life events
Dohrenwend and Dohrenwend (1981) suggested that stressful life events are “those that are proximate to, rather than
remote from, the onset of the disorder. For example, this category includes the recent death of a friend or relative but not
the fact that an adult's father died when he was a child. The latter event is not irrelevant to life stress but is subsumed
under personal dispositions, since we assume that an early death of a parent can affect an adult's behavior only insofar
as its impact was internalized (p.131).” These authors make the point that events that occurred awhile ago, or when an
individual was a young child, are not considered life events, because it is ‘life stress’ that is most likely incorporated
into an individual's personality style, cognitive vulnerability, or other trait-like characteristics. Thus, the ‘proximity’ of
a life event to the onset of a disorder is vital in order to assume its association with the onset, and particularly, as the
trigger of a mood episode.
Cobb (1974) and Brown and Harris (1978) pioneered the idea that one's environment may influence the impact of a
stressful event on an affective episode. Specifically, these investigators highlighted the need to understand an
individual's current life situation, the nature of social supports available to the person, personal characteristics, and the
attitudes of peers when examining the impact of a life event. In support of such a contextual model, recent research has
suggested that social support, personality, and other psychosocial variables may act as third variables in the relationship
of life stress and affective disorders (Leskelä et al., 2004; Panzarella, Alloy, & Whitehouse, in press; Paykel, 2001).
682
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
Although such potential variables are not a focus of this review, it is important to acknowledge that contextual factors
are important in understanding the complicated association of life events and mood episodes, as well as the impact of a
life event.
Further, life events are different from chronic stress. Ezquiaga, Gutierrez, and López (1987) define life events as
“circumstances punctually situated in time that induce stress and require the individual to use adaptation mechanisms”
and chronic stress as “adverse circumstances that act uninterruptedly over a prolonged time (p. 136).” Thus, life events
entail a change or readjustment by an individual. For this reason, many of the research designs in this review only
examined events that had a moderate or severe impact on the participant.
The assessment of life events has improved substantially from earlier studies. One such improvement is a change
from the use of self-report forms, or checklists of life events, to life event interviews conducted by highly trained
interviewers based on the contextual model established by Brown and Harris (1978). For example, many studies utilize
the Bedford Life Events and Difficulties Schedule (LEDS; Brown & Harris, 1979), or variants of this interview (Alloy
& Abramson, 1999; Hammen, Marks, Mayol, & DeMayo, 1985), particularly studies examining social rhythm
disruption, life events, and mood (Frank, Anderson, Reynolds, Ritenour, & Kupfer, 1994; Malkoff-Schwartz et al.,
1998, 2000). These interview-based assessments are similar in that they utilize the contextual threat methods of Brown
and Harris and, thus, elicit objective impact ratings for each event (Brown & Harris, 1978). Further, these life event
interviews utilize similar procedures of assessment and possess good psychometric properties (Alloy & Abramson,
1999; Daley et al., 1997; Hammen, 1991; Hammen, Henry, & Daley, 2000; Johnson & Miller, 1997; Malkoff-Schwartz
et al., 2000; Simons, Angell, Monroe, & Thase, 1993).
1.3. Social zeitgebers and social rhythms
The term “zeitgeber,” German for “time-giver,” is used to describe environmental, or external, time cues that entrain
human circadian rhythms. For example, research has found that in free running environments, circadian rhythms, such
as the sleep–wake cycle, have a period of approximately 25 h (Refinetti and Menaker, 1992; Wehr et al., 1985; Wever,
1975). Thus, circadian rhythms are likely entrained by zeitgebers in our environment in order to yield a period of
almost exactly 24 h, even though the inherent, free running cycle is 25 h (Moore-Ede, Czeisler, & Richardson, 1983;
Panda, Hogenesch, & Kay, 2002; Wever, 1979). These data are consistent with the social zeitgeber theory; however,
they do not rule out the possibility of an internal trigger as well. Moreover, do changes in zeitgebers cause severe
enough disruptions to trigger affective episodes? We will review the evidence relevant to this question in the following
sections.
Social zeitgebers are usually derived from social contact with other individuals, but solitary activities can also be
social zeitgebers for the circadian clock. For example, many activities may occur alone or with others, such as,
commuting to work, having meals, bedtimes, and watching television (Monk, Kupfer, Frank, & Ritenour, 1991). In
Ehlers, Kupfer, Frank and Monk (1993) the social zeitgeber theory was amended to include physical zeitgebers in
addition to social zeitgebers. For example, light is a physical zeitgeber (or “zeitstörer”) that can entrain and regulate the
circadian rhythms of hormonal, metabolic, and physical activity, which has also been shown to have clinical
implications for mood disorders (Panda et al., 2002; Wever, 1979; Wirz-Justice, 2006). In this review, we focus
specifically on the effects of social zeitgebers, but it is important to remember that other types of zeitgebers, or
zeitstörers, affect one's circadian rhythms and mood as well.
The Social Rhythm Metric (SRM) is intended to capture an individual's “social rhythm,” or the frequency with
which daily activities are performed and the level of regularity and social contact associated with these activities
(Monk, Flaherty, Frank, Hoskinson, & Kupfer, 1990). The measure is completed in the evening before going to bed and
tracks the timing of 15 specific and 2 write-in, or individualized, activities. The timing of these activities (i.e., waking
up, eating meals) is thought to contribute to the stability of an individual's daily routine or constitute their social
rhythm. If the time an activity occurs on a given day is within 45 min of the average time, it is considered a “hit.” Social
rhythm regularity is defined by the number of activities that had three or more hits in one week (possible range = 0–17
activities). Average frequency of activities also often is calculated by averaging the frequencies of all items that had
been endorsed as regular (possible range = 3–7 times) (Monk et al., 1991). The SRM was found to be moderately
consistent (i.e., r = 0.44, p < .001 between SRM scores in weeks 1 and 2) and valid (e.g., participants on vacation have
considerably lower SRM scores) in a group of 50 healthy controls (Monk et al., 1990, 1991). Other evidence for the
conceptual validity of the SRM is derived from studies that found SRM scores are correlated positively with other
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
683
indices of social rhythm stability (Brown et al., 1996; Monk et al., 1991; Monk, Petrie, Hayes, & Kupfer, 1994; Stetler,
Dickerson, & Miller, 2004; Szuba, Yager, Guze, Allen, & Baxter, 1992).
Frank and colleagues developed the first standardized assessment of social rhythm disruption (SRD) events based
on the LEDS interview (Frank, Malkoff-Schwartz, Sherrill, & Anderson, 1999). These ratings are determined “by a
consensus panel and are guided by clearly delineated criteria and a ‘dictionary' of examples (p. 1008, MalkoffSchwartz et al., 2000).” The SRD rating scale relies on the degree of disruption in one's sleep–wake cycle brought
about by a life event (Frank, Malkoff-Schwartz et al., 1999; Malkoff-Schwartz et al., 2000, 1998). For example, a high
SRD rating would be given to life events that contribute to sleep disruption (e.g., overseas travel) or to a substantial
desynchronization in one's routine that would likely change one's sleep–wake pattern or promote sleep disruption
(e.g., marital separation, ending or beginning a full-time job; Malkoff-Schwartz et al., 2000). One study conducted two
reliability assessments of this rating system for social rhythm disruption events and found high inter-rater agreement
(kappa = 0.94 and 0.87; Malkoff-Schwartz et al., 2000).
1.4. Biological rhythms
A biological process of the human body that repeats itself approximately every 24 h is considered to have a daily
rhythm. Such rhythms are defined as “circadian” if they persist with the same period in the absence of external time
cues, or are endogenously driven (Refinetti & Menaker, 1992). Circadian rhythms are described quantitatively as
having a “mean,” or the level at which the oscillation takes place, a “period,” or the time to complete one cycle, an
“amplitude,” or the distance between the mean and peak of the cycle's oscillation, and an “acrophase” or time of the
peak of the circadian rhythm's phase (Minors & Waterhouse, 1985).
The suprachiasmatic nucleus (SCN), or internal pacemaker, in the anterior hypothalamus of the brain is suspected of
regulating human biological rhythms. The SCN can function autonomously, without the need for external zeitgebers
(“free running state”), but it can also be entrained by zeitgebers (“entrained state”) (Cermakian & Boivin, 2003; Wever,
1979). For example, the core of the SCN receives photic input from the retina, which triggers a response initiated by
various genes and chromatin remodeling within the SCN neurons. The SCN also receives non-photic input from
different parts of the brain (Cermakian & Boivin, 2003). The tightly packed neurons in the SCN are believed to
integrate these photic and nonphotic zeitgebers and then produce an output signal that regulates the circadian rhythms
in the body. These data suggest that a combination of internal and external triggers may affect individuals' pacemakers,
but it is unclear which source of cues, internal or external, predominantly influences affective episodes. Preliminary
evidence in this area will be reviewed.
Studies that attempt to measure the free running, or endogenous, component of the SCN must remove or minimize
potential external zeitgebers, such as noise, light, and clocks. These studies are interested in observing as many
oscillations, or consecutive cycles, of the circadian rhythms as possible to understand the quantitative aspects of the
rhythms. Participants in these studies are isolated from their normal environments for usually 10 to 30 d, although some
studies may only isolate participants for a few days, particularly if a sleep manipulation is imposed (Minors &
Waterhouse, 1985). Participants' body temperature, sleep, and activity levels are usually monitored continuously with
blood drawn approximately every hour to assess levels of plasma melatonin, cortisol, thyroid stimulating hormone
(TSH), and other hormones suspected of having a circadian rhythm.
2. Life events, social rhythms, and mood
According to the social zeitgeber theory, life events begin the causal chain of processes that lead to major depressive
episodes (Ehlers et al., 1988). Thus, we begin by very briefly reviewing the extensive evidence that life events are
associated with affective episodes and symptomatology. It is important to note that there are several theories, other than
the social zeitgeber theory, which also attempt to explain the association between life events and depression. These
theories will not be discussed, as they are outside the scope of this review (see Ellicott, Hammen, Gitlin, Brown, &
Jamison, 1990; Hammen, 1991; Johnson & Roberts, 1995; Monroe & Handjiyannakis, 2002; Safford, Crossfield,
Alloy, & Abramson, in press).
In this section, we will also review findings that may explain how life events influence mood. Specifically, we
review the evidence that life events may be associated with mood because they affect social zeitgebers (i.e., meal times,
exercise, clocks) (pathway 1 in Fig. 1), which then disrupt an individual's social rhythm (i.e., daily activities, social
684
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
interactions) (pathway 2 in Fig. 1). We will also discuss the limitations of the literature and offer an alternative
interpretation of the findings based on the internal trigger hypothesis.
2.1. Life events and mood
The social zeitgeber theory describes a potential pathway by which life stress may influence mood. This theory was
based originally on the finding that life events are associated with depressive symptoms (Paykel, 2001), but is also
supported by research suggesting that life events are associated with (hypo)manic symptoms (Dunner, Patrick, & Fieve,
1979), as well as precede bipolar episodes or relapse (Glassner & Haldipur, 1983; Joffe, MacDonald, & Kutcher, 1989;
Kennedy, Thompson, Stancer, Roy, & Persad, 1983). However, it is important to note that some studies using
structured life event interviews (e.g., LEDS) did not find a significant association of life events and (hypo)manic
episodes (Chung, Langeluddecke, & Tennant, 1986; Sclare & Creed, 1990). These inconsistent findings in bipolar
samples are likely due to these studies relying on long-term recall (e.g., 10 years) of events, using different time frames,
utilizing different inclusion criteria, using hospital admission as the criterion for relapse (this is problematic given that
events may occur between onset of episode and admission), and having insufficient power to detect meaningful group
differences (see Alloy et al., 2005; Johnson, 2005; Johnson & Roberts, 1995).
In the last 15 years, the literature has improved considerably on these limitations and replicated earlier findings that
life events are associated with bipolar episodes (Christensen et al., 2003; Ellicott et al., 1990; Hammen & Gitlin, 1997;
Hunt, Jones, & Silverstone, 1992; Pardoen et al., 1996). For example, one particularly well-designed study found that
life events are associated with the course of bipolar disorder or the time to recovery after a bipolar episode (Johnson &
Miller, 1997). In short, extensive evidence suggests that life events precede depressive as well as (hypo)manic
symptoms and episodes (Alloy et al., 2005; Johnson, 2005; Johnson & Roberts, 1995).
2.2. Life events, social zeitgebers and rhythms
The first study to examine whether life events are associated with social zeitgebers and rhythm disruption (pathways
1 and 2 in Fig. 1) assessed 87 individuals after the loss of a spouse (Flaherty, Frank, Hoskinson, Richman, & Kupfer,
1987). This study concluded that social rhythm disruptions were associated with the loss of a spouse (a severe negative,
social rhythm disruption event), as well as with an increase in depressive symptomatology. In contrast, Prigerson et al.
(1994) did not find a relationship between a spouse's death and social rhythm disruption in an elderly (aged 60 to
80 years) sample. Perhaps these participants' preservation of regular social rhythms, after the death of their spouse,
buffered them from the development of bereavement-related depression. These studies are limited by their correlational
design as well as their utilization of a community sample, which increases the generalizability of these results, but does
not add to our understanding of how these events affect individuals with bipolar or unipolar mood disorders. Further,
Prigerson et al. (1994) had a long time interval (e.g., 9 to 12 months) between the severe life event and assessment of
social rhythm disruption and symptomatology. In short, we cannot determine from these studies whether social rhythm
disruptions are due to the loss of a zeitgeber, the occurrence of an event, or a biological abnormality (e.g., in one's
pacemaker) in vulnerable individuals (see Fig. 1).
To improve upon these limitations, Brown et al. (1996) conducted a follow-up study to the Prigerson et al. (1994)
study in which 43 elderly, spousally bereaved individuals and 15 elderly, nonbereaved individuals were added to their
original sample. This study found that individuals currently in a major depressive episode, but not a minor depressive
episode, had significantly lower social rhythm stability and activity levels than the nonbereaved controls (Brown et al.,
1996). In the major depressive group, social rhythm stability was also inversely related to subjective sleep quality (i.e.,
sleep impairment increased as stability of social rhythm decreased) and severity of depression (i.e., less social rhythm
regularity was associated with more depressive symptoms).
Similar to the early studies, this study had a cross-sectional design and, thus, we cannot determine whether it was the
death, or loss of a zeitgeber, that impacted the individuals with major depression (external trigger hypothesis) or
whether they had a more trait-like social rhythm irregularity present even prior to the spouse's death (internal trigger
hypothesis). The latter explanation is consistent with findings from the sleep literature that individuals with unipolar
and bipolar disorders have disrupted sleep cycles, suggesting that they have a more permanent abnormality in their
circadian rhythm pacemakers (Wehr & Wirz-Justice, 1982; Wu & Bunney, 1990). Future studies need to assess the
temporal relationship of zeitgebers, circadian rhythm disruptions, and symptoms. However, this study did improve
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
685
upon the Prigerson et al. (1994) study by finding an association of social rhythm stability, sleep, and depressive
symptoms in individuals experiencing a major depressive episode. Thus, the null findings from the Prigerson et al.
(1994) study may be explained by their lumping of individuals with varying levels of vulnerability (i.e., intensity of
depressive symptoms).
Two other studies have examined the association of life events and social rhythm regularity in a clinical sample
(Malkoff-Schwartz et al., 2000, 1998). These studies utilized the LEDS to assess life events. As described above, the
level of social rhythm disruption (SRD) of events was rated by a consensus panel and ranged from 1 (marked) to 4
(little/no disruption) (Frank, Malkoff-Schwartz et al., 1999). An event was considered disruptive if it received a score of
1, 2, or 3 (Malkoff-Schwartz et al., 1998). These studies primarily focused on the association of events and episode
onsets; however, they also recognized that life events are associated with SRD (pathways 1 and 2 in Fig. 1) (MalkoffSchwartz et al., 1998).
Malkoff-Schwartz et al. (1998) found that twice as many bipolar participants experienced a SRD event during an
eight week pre-onset period compared to an eight week control period. Further, the proportion of participants with at
least one SRD event was significantly greater during the pre-onset than control periods for manic participants, but not
for depressed participants (55% versus 10%, respectively). Between-group comparisons illustrated that the association
of SRD events and episode onsets was unique to manic episodes. It is possible that the eight week window in this study
may have been ample time for SRD to trigger mania, but not depression (Malkoff-Schwartz et al., 1998). Alternatively,
the group differences could be attributed to the small sample sizes or to manic participants experiencing more than
twice as many total events than the depressed participants (81% and 38%, respectively), allowing for a greater chance
for these events to be associated with SRD (Malkoff-Schwartz et al., 1998). Finally, it is possible that SRD events do
not impact depressive symptoms as much because depression is manifested as a result of a more trait-like abnormality
in the pacemaker (i.e., internal trigger hypothesis), whereas manic symptoms may be associated more with disruptions
in zeitgebers (as proposed by the social zeitgeber theory) (see Fig. 1).
To examine these theories, the same authors conducted a similar study, but with 8- and 20-week pre-onset periods
and episode-free control periods from the year prior to each participant's mood episode onset (Malkoff-Schwartz et al.,
2000). Participants with bipolar and unipolar mood disorders were divided into four groups: bipolar manic (n = 21),
bipolar depressed (n = 21), bipolar rapid cycling (n = 24), and unipolar depressed (n = 44). Between-group comparisons
illustrated that bipolar manic participants experienced more SRD events in the pre-onset periods than their control
periods compared to the other three groups. The only significant within-subject comparison, as also found in the
previous study, was that the manic participants experienced more SRD events in the 8-week pre-onset period compared
to the 8-week control period. This supports Malkoff-Schwartz et al.'s (1998) earlier presumption that bipolar manic
participants are especially susceptible to SRD events, particularly given the added comparison groups (i.e., unipolar
depressed, bipolar cycling). Additionally, the null findings for the 20-week pre-onset period suggest that there were no
delayed effects of SRD events on depressive episodes. Thus, bipolar individuals experiencing manic symptoms appear
to be influenced by zeitgebers; although, it is still unclear whether these individuals also have trait-like abnormalities in
their pacemakers as suggested by disruptions in their sleep (Sack, Nurnberger, Rosenthal, Ashburn, & Wehr, 1985;
Wehr, Wirz-Justice, Goodwin, Duncan, & Gitlin, 1979) and the internal trigger hypothesis (see Fig. 1).
2.3. Summary
Research suggests that life events precede the onset of unipolar and bipolar episodes. Further, consistent with the
social zeitgeber theory, there is some evidence that life events are associated with social rhythm disruptions which, in
turn, may trigger affective symptoms (Malkoff-Schwartz et al., 2000, 1998). For example, life events that disrupt
individuals' social rhythms are significantly associated with onsets of manic episodes (Malkoff-Schwartz et al., 2000,
1998). However, this conclusion must be considered preliminary, given that these studies have small sample sizes and
lack a non-psychiatric control group.
It is unclear from these studies whether social rhythm disruptions preceded depressive symptoms (Brown et al.,
1996; Flaherty et al., 1987). Moreover, several studies did not find an association between depressive symptoms and
socially disruptive events (Malkoff-Schwartz et al., 2000, 1998; Prigerson et al., 1994). The lack of an association
between depressive symptoms and SRD events may suggest that individuals with mood disorders, particularly major
depression, have trait-like social rhythm irregularities that contribute to their symptoms as suggested by the internal
trigger theory (see Fig. 1) as opposed to disruptions due to changes in zeitgebers. Given the limitations of these
686
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
studies, these data do not clarify the mechanism underlying depressive symptoms for unipolar and bipolar
individuals.
Despite the null findings with depressive symptoms, these findings offer preliminary support for the social zeitgeber
theory, particularly given the recent Malkoff-Schwartz et al. (1998, 2000) findings with manic episodes. Future
research should examine why SRD events may affect depressive and hypo(manic) episodes differently, as well as
whether social rhythm regularity changes from before to after a SRD event. Future research is also needed to examine
whether external zeitgebers or internal cues are more effective in influencing circadian disruptions and, ultimately,
affective symptoms. Thus, longitudinal studies, assessing the temporal associations of zeitgebers, mood, and biological
circadian rhythms are needed to test the validity of the social zeitgeber theory.
3. Social zeitgebers and biological rhythms
Ehlers et al. (1988) proposed that the “primary path” of the social zeitgeber theory consisted of a “chain of events in
which instability of social rhythms can lead to an instability in specific biological rhythms, particularly sleep (p. 950).”
Thus, social zeitgebers, such as personal relationships, meals, exercise, or social demands (i.e., school, work) are tasks
that serve to entrain biological rhythms, such as temperature, hormone levels, and sleep (Monk et al., 1990, 1991).
According to the social zeitgeber theory, depressive symptoms are the result of changes in social zeitgebers disrupting
social and biological rhythms (pathways 2 and 3 in Fig. 1).
There has been very little research on the association of social zeitgebers and biological rhythms in patient
populations (pathway 3 in Fig. 1); however, researchers have acknowledged for centuries that healthy humans are able
to adapt their circadian rhythms to environmental zeitgebers (Elmore, Betrus, & Burr, 1994). For example, researchers
have identified the entrainment effects of the light-dark cycle, social contact/interaction, time of meals, and ambient
temperature on human circadian rhythms (Aschoff et al., 1971; Eastman, 1987; Sack, Lewy, Blood, Keith, & Nakagwa,
1992; Wever, 1989). More specifically, Aschoff et al. (1971) were among the first investigators to identify that social
zeitgebers (i.e., meals, sleep propensity) can entrain the circadian rhythms of body temperature, cortisol,
catecholamines, and sodium in individuals under constant darkness. Moreover, two small, but well designed studies
found that the presence of others in a group was responsible for a significant phase shift in these rhythms and that the
rate of cortisol phase shift was heavily influenced by social interactions (Vernikos-Danellis & Winget, 1979; Winget,
Vernikos-Danellis, & Beljan, 1975).
More recently, a review concluded that changes in daily activity patterns and social contacts, whether natural or
brought about by an experimental manipulation, a religious observance, or long-term travel, are associated with
changes in biological rhythms (Stetler et al., 2004). Thus, preliminary research in community samples suggests that
zeitgebers influence circadian rhythms (as suggested by the social zeitgeber theory); however, these studies are limited
in that they do not utilize bipolar or unipolar samples, have small sample sizes, and do not ascertain the directionality of
these relationships. It is unclear from these studies whether changes in external cues disrupt circadian rhythms to the
extent that they may cause affective symptoms.
Stetler et al. (2004) examined social rhythm regularity and biological rhythms, specifically daily cortisol levels, in
50 unipolar depressed participants who were matched on age, sex, and ethnicity to 50 non-depressed, control
participants. Similar to previous studies, this study found that control participants exhibited a decline in cortisol levels
on days in which they performed more regular activities (Aschoff et al., 1971; Vernikos-Danellis & Winget, 1979;
Winget et al., 1975). This relationship was not found for participants with unipolar depression (Stetler et al., 2004).
Further, control participants had a significantly greater normative decline in cortisol levels on days in which they
performed more regular activities with other people than on days in which they engaged in fewer regular activities with
other people. The unipolar depressed group exhibited a similar, but nonsignificant, trend for regular activities
conducted with others. Thus, regular activities carried out when other people are present may be an important factor in
whether these activities influence the circadian rhythm of cortisol. This conclusion is supported by the finding that
nonsocial, regular activities were not related to diurnal cortisol patterns in either group (Stetler et al., 2004).
This study is consistent with previous findings that healthy individuals' social zeitgebers and rhythms are associated
with their biological rhythms. The lack of such an association in unipolar depressed individuals may be due to the
inability of social zeitgebers to entrain their biological rhythms. It is possible that a biological abnormality in depressed
individuals' pacemakers may make it difficult for them to entrain to their social environments, perhaps explaining the
observed desynchrony of circadian rhythms in depressed individuals (Wehr & Wirz-Justice, 1982; Wu & Bunney,
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
687
1990). This is supported by the finding that unipolar depressed individuals in Stetler et al.'s (2004) study experienced
the same number of social zeitgebers as the normal controls. The absence of a social zeitgeber–circadian rhythm
association in unipolar depressed individuals in the Stetler et al.'s (2004) study contradicts the social zeitgeber theory
and some of the evidence previously reviewed illustrating that external zeitgebers (i.e., life events) do influence
individuals' lifestyle or social regularity. Specifically, the social zeitgeber theory suggests that depressed individuals'
social zeitgebers have the ability to entrain their biological rhythms. According to this theory, it is the irregularity of
social zeitgebers (i.e., by loss or change in zeitgebers) that leads to a disruption in biological rhythms and eventually
depressive symptoms (see Fig. 1) (Ehlers et al., 1988).
Another possible explanation for Stetler et al.'s (2004) findings is that unipolar depressed individuals may require
stronger or more frequent social zeitgebers than nondepressed individuals to influence their biological rhythms, due to
an abnormality in their circadian pacemakers or SCN. This “attenuation theory” suggests that depressive symptoms
may be related to the strength of circadian rhythms, as measured by the amplitude of their phases, as well as the
precision of the circadian rhythms (Czeisler, Kronauer, Mooney, Anderson, & Allan, 1987; Schulz & Lund, 1983).
Preliminary evidence suggests that individuals with unipolar depression have weaker circadian rhythms compared to
normal controls (Vogel, Vogel, McAbee, & Thurmond, 1980). This explanation is congruent with both theories
proposed in Fig. 1 (represented by the dotted arrow in Fig. 1); the extent to which vulnerable individuals' circadian
rhythms are disrupted is a function of both (1) the zeitgeber's strength in entraining the rhythm (the social zeitgeber or
external trigger theory) and (2) a biological abnormality of the pacemaker causing it to be less responsive to its
environment (the internal trigger theory).
Congruent with the attenuation theory, research has found that unipolar depressed individuals find their social
interactions to be less enjoyable and less intimate compared to normal controls (Nezlek, Hampton, & Shean, 2000).
Thus, it is possible that a higher frequency or a stronger intensity of social interactions are needed to act as zeitgebers
for depressed individuals than are needed by normal controls. In sum, the impact of a zeitgeber on a biological rhythm
can be “modulated by protective and vulnerability factors from both the psychosocial and the psychobiological spheres
(p. 950, Ehlers et al., 1988),” perhaps a biological abnormality of the pacemaker. Thus, future research should examine
the relationship of the type, quantity/intensity, and frequency of social zeitgebers and depression and (hypo)mania, and
specifically, how individuals with these symptoms experience or interpret their social interactions.
Unfortunately, given the correlational nature of the Stetler et al. (2004) study, the causal direction of these
associations cannot be determined. Thus, it is also possible that changes in cortisol levels could influence regularity and
frequency of daily activities (the opposite directionality proposed by the social zeitgeber theory, see Fig. 1). Other
limitations to this study include assessment of social rhythm regularity over only four days, in contrast to the typical
two to six weeks (Monk et al., 1991). Yet, this study did report SRM scores that were quite stable across four days for
both groups (for controls, α = .72, for depressed, α = .84) (Stetler et al., 2004). This study also only assessed one
biological rhythm. Future research should address the relationship of social zeitgebers and other biological rhythms
such as body temperature, sleep, and other hormones. Finally, this study was restricted to same-day analyses, given that
the data collection days were not consecutive days. Thus, it is impossible to assess possible time lag effects of social
rhythm regularity and cortisol levels.
3.1. Summary
There is preliminary evidence that social zeitgebers may influence circadian rhythms in community samples,
supporting pathway 3 of the social zeitgeber theory (see Fig. 1). One study did not find such an association between
social zeitgebers and the cortisol circadian rhythm in a sample of unipolar depressed individuals (Stetler et al., 2004).
Although this finding contradicts the social zeitgeber theory, several possible explanations for these results were
discussed. There are currently no studies that have addressed this relationship in a bipolar sample. Thus, future research
is greatly needed in this area, particularly to give the social zeitgeber theory credence, as it is a necessary pathway in
this model (or pathway 3 in Fig. 1).
Future research should also examine the critical components of social zeitgebers needed to entrain circadian
rhythms. Specifically, particular types or intensities of social zeitgebers may be required to influence circadian rhythms
as suggested by the attenuation theory. Likewise, as mentioned, an understanding of how the pacemaker (SCN) may
interpret zeitgebers is needed. Alternatively, given the lack of evidence that social zeitgebers entrain biological rhythms
in individuals with unipolar and bipolar disorder, it should be considered that a biological abnormality in the pacemaker
688
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
is responsible for their symptoms as opposed to disruptions in external cues (see Fig. 1). In short, future work should
address whether various characteristics of zeitgebers, such as the degree to which they entail social interactions,
differentially impact circadian rhythms. Such research investigating how social zeitgebers influence biological rhythms
is needed to gain further support for the external trigger hypothesis.
4. Circadian rhythms and mood
The last pathways of the social zeitgeber theory presume that circadian rhythm disruption creates the somatic
symptoms of depression, leading to a major depressive episode in vulnerable individuals (see Fig. 1) (Ehlers et al.,
1988). Again, we also review evidence pertinent to (hypo)manic symptoms. First, we review the association of bipolar
and unipolar individuals' social rhythm regularity and mood episodes. Next, we review preliminary evidence from
treatment studies that suggests efforts to regularize, or improve social rhythm regularity, are associated with improved
mood. The effectiveness of these psychotherapies, although questionable, yields preliminary support for the social
zeitgeber theory.
4.1. Social rhythms and mood
The most discouraging results for the social zeitgeber theory are from an early study that found no differences in
SRM scores between 20 individuals with unipolar depression and 15 day-working normal controls over a 12-week
period (Monk et al., 1990). However, the depressed individuals had more intrasubject variability in their SRM scores
than controls and required more weeks of sampling to achieve a stable measure of their social rhythm regularity (Monk
et al., 1991). These results suggest that individuals with unipolar depression have more difficulty maintaining social
rhythm regularity from day to day; however, this may be a result of either an external force acting on depressed
individuals (e.g., life events acting as social rhythm disrupters as postulated by the social zeitgeber theory) or an
internal component of the depressed individuals (e.g., cognitive vulnerability, personality style, abnormal circadian
pacemaker) (see Fig. 1). Further, these results, as most other studies conducted with patient populations, are limited by
the unstandardized medication regimes of participants with mood disorders, given that medications have been shown to
affect circadian rhythms (Bendetti et al., 2001).
Given that participants in the Monk et al. (1991) study were in remission, it is possible that the lack of group
differences was due to the patient group not being currently depressed. As a result, Szuba et al. (1992) examined the
daily SRM scores of individuals with bipolar and unipolar depression1 (n = 19) in an inpatient psychiatric hospital
compared to a control group of full-time, day-shift employees of the hospital. In contrast to Monk et al. (1991), this
study found that less social rhythm regularity was correlated with a higher report of depressive symptoms and the
depressed group had lower overall SRM scores (less regular social rhythms) than the control group (Szuba et al., 1992).
Thus, even in highly structured environments, there was enough variability in SRM scores to yield a significant
difference between groups. However, this study is limited in that pre-hospitalization social rhythm and activity levels
were not assessed. Similar to Monk et al.'s (1991) study, it is unclear from these data why depressed individuals have
less regular schedules (i.e., life events, abnormal pacemakers), but it appears that their schedules are associated with
their depressive symptoms.
More recently, two other studies have obtained the finding that bipolar individuals have significantly lower social
rhythm regularity scores (as measured by the SRM) compared to sex- and age-matched control participants (Ashman et
al., 1999; Jones, Hare, & Evershed, 2005). Unfortunately for the social zeitgeber theory, these studies also found that
lower social rhythm regularity scores did not vary systematically with mood state; however, a power analysis revealed
that these studies did not have enough participants to demonstrate a significant effect (Ashman et al., 1999).
Nonetheless, these results suggest that circadian rhythm regularity may be a trait marker (internal trigger theory) as
opposed to a consequence of clinical state (external trigger theory) (see Fig. 1). This is supported by post-hoc analyses
in the Ashman et al. (1999) study that morning activities (but not evening activities) were significantly phase delayed
(i.e., occurred later) during periods of depressed mood compared to (hypo)manic and euthymic mood states, suggesting
that there may be a biological abnormality with these individuals' pacemakers. Such an abnormality may create a trait1
Diagnoses were made by two psychiatrists without using structured interviews. However, given that this study was conducted in a psychiatric
hospital, it is likely that the participants were exhibiting severe psychopathology which may have facilitated diagnosis.
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
689
like phase delay of their social rhythms which, in turn, could trigger their symptoms (i.e., internal trigger hypothesis).
However, without assessing these individuals' daily exposure to zeitgebers, we cannot rule out that these seemingly,
trait-like social rhythm disruptions could also be due to external events as suggested by the social zeitgeber theory and
indicated by the dotted line in Fig. 1.
Congruent with this theory, a recent study found that individuals with bipolar spectrum disorders2 had lower traitlike social rhythm regularity scores (as defined by a modified version of the SRM) than demographically matched
normal controls (Chang, Alloy, & Abramson, 2003). Moreover, further analyses with a larger sample from the same
study showed that lower regularity scores prospectively predicted depressive and (hypo)manic episodes (Shen, Alloy,
Abramson, & Grandin, submitted for publication). These data are consistent with the theory that individuals with
affective disorders have less regular daily routines as a result of a more stable trait, such as an abnormality in their
pacemakers. However, zeitgebers may also affect the pacemakers' rhythm or worsen these individuals' lifestyle
regularity (as indicated by the dotted line in Fig. 1).
4.2. Psychotherapy and mood: Implications for the social zeitgeber theory
Interpersonal and Social Rhythm Therapy (IPSRT) was specifically designed to maintain regular daily rhythms as
well as identify and manage potential precipitants of rhythm dysregulation (Frank, Holly, & Kupfer, 2000). The central
tenet of IPSRT, similar to the social zeitgeber theory, is that circadian rhythm disruptions are the primary underlying
mechanism in bipolar disorder. Thus, IPSRT is presumed to alter the underlying neuronal circuitry that is associated
with bipolar symptomatology by regularizing circadian rhythms, particularly the sleep-wake cycle (Frank et al., 2000).
One longitudinal study has addressed the effectiveness of IPSRT for bipolar individuals. Specifically, bipolar
participants with an acute depressive or (hypo)manic episode were randomized to either IPSRT (n = 18) or to a standard
medication clinic treatment condition, Clinical Status and Symptom Review Treatment (CSSRT; n = 20) (Frank et al.,
1997). Participants completed the SRM everyday and symptom measures every few weeks for up to 52 weeks
(M = 24.8 ± 13.8 and M = 26.7 ± 15.0 for the IPSRT and CSSRT groups, respectively). In the first publication of their
findings, the authors reported that the IPSRT group increased their number of regular activities over time faster than the
CSSRT group, but the two groups did not differ in their number of bipolar symptoms (Frank et al., 1997). These results
did not provide support for the social zeitgeber theory in that increasing bipolar individuals' social rhythm regularity
did not appear to improve their mood.
These findings were replicated in a second publication, as the authors found no difference in the outcomes between
four, randomized groups after two years of follow up: (1) acute IPSRT followed by preventative IPSRT, (2) acute
IPSRT followed by preventative clinical management (CM), (3) acute CM followed by preventative CM, or (4) acute
CM followed by preventative IPSRT (Frank, Swartz et al., 1999). However, the most recent findings from this
longitudinal study, indicated that participants treated with IPSRT, as opposed to CM, in the acute phase experienced
longer episode-free periods and were more likely to remain well in the two year preventive maintenance phase (Frank et
al., 2005). Further, this association was mediated by increased social rhythm regularity for participants receiving
IPSRT. These data suggest that social rhythm disruptions may cause affective episodes. These findings provide
stronger support for the social zeitgeber theory than for the internal trigger theory, given that stable, trait-like rhythms
probably would be less likely to show such improvements or changes over a relatively short time period than rhythms
triggered by external events (see Fig. 1).
4.3. Summary
Research is needed to determine whether disruptions in social rhythms are associated with bipolar episodes.
Although preliminary findings suggest this association exists, the results are mixed and, thus, require replication. In
addition, several of the studies examining this association have been limited by small sample sizes, short assessment
2
Bipolar spectrum disorders are considered categories of bipolar disorder and include bipolar II, cyclothymic, and bipolar not otherwise specified
(NOS) diagnoses. Cyclothymia involves at least two years of numerous hypomanic and depressive episodes that do not meet criteria for mania or
major depression and occur without a symptom-free period of two months (APA, 2000). A diagnosis of bipolar NOS entails recurrent hypomanic
episodes without depressive episodes, or a cyclothymic pattern but with hypomanic and depressive periods that do not meet minimum duration
criteria for hypomanic and depressive episodes, or hypomanic and depressive periods that were too infrequent to qualify for a cyclothymic
diagnosis.
690
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
periods, heterogeneous patient populations, and not assessing the direction of their findings. Further, the SRM may
not adequately capture social rhythm regularity, given that it relies on participants' ability to accurately assess the
timing of activities that they often do habitually. Alternatively, given the high frequency of these activities,
participants are likely to be accurate reporters of their timing, which is supported by the sound psychometric
properties of the SRM.
It is possible that subtypes of bipolar disorder may respond differently to particular interventions (Jones, 2004).
There are very few studies examining the manipulation of social rhythm regularity, but there have been none to date
that have attempted such an intervention in bipolar NOS, cyclothymic, or bipolar II individuals. This is particularly
important because reduced social rhythm regularity in bipolar spectrum individuals prospectively predicted time to the
onset of their (hypo)manic and depressive episodes (Shen et al., submitted for publication). Further, given the
preliminary, but promising, findings for IPSRT, future research should address the effects on mood of manipulating
social rhythm regularity in a bipolar sample, particularly for individuals with specific subtypes of the disorder.
These findings also offer preliminary evidence that circadian rhythm regularity is trait-like as opposed to a
consequence of symptomatology in bipolar samples (Ashman et al., 1999; Chang et al., 2003; Jones et al., 2005). Given
that even remitted bipolar individuals are likely to experience symptoms, future research should examine a trait
hypothesis in at-risk healthy participants (e.g., offspring of bipolar parents). Another consideration includes examining
differences between bipolar and control groups that may confound the interpretation of social rhythm and circadian
rhythm differences between the groups. As mentioned, bipolar samples differ from normal controls in their medication
regimes. Specifically, lithium, a popular mood stabilizer for bipolar individuals, has been shown to have circadianstabilizing effects (Bendetti et al., 2001). Further, studies have found lifestyle differences between bipolar samples and
control groups that are not accounted for in their study design, such as employment, marital status, and personality
characteristics (Jones et al., 2005; Swendsen, Hammen, Heller, & Gitlin, 1995). Future studies should be wary of these
individual and group differences and how they may affect the study design and interpretation of results.
Taken together, the studies reviewed in this section illustrate that vulnerable individuals have less social rhythm
stability and that this may lead to their affective episodes (Chang et al., 2003; Shen et al., submitted for publication).
Further, this research indicates that regularizing social rhythms in bipolar samples could be an effective intervention
(Frank et al., 2005).
5. Summary of limitations and directions for future research
This review highlighted several limitations of the social zeitgeber theory, as well as the studies conducted to test this
theory to date. A general comment is that there is not enough prospective, longitudinal research, particularly with
unipolar and bipolar samples, to fully evaluate the merits of the social zeitgeber theory. At best, this review highlighted
several associations that suggest circadian rhythm disruptions may contribute to the symptoms experienced by
individuals with bipolar and unipolar mood disorders. It is still unclear whether external cues (the social zeitgeber
theory), internal cues (the internal trigger theory), or both influence circadian rhythm disruptions and whether these
disruptions are associated with changes in mood (see Fig. 1). These clarifications are necessary to determine the
validity of the social zeitgeber theory. Consequently, we briefly highlight specific limitations and suggestions for future
research.
Evidence suggests that life events precede affective symptoms. Thus, it is likely that events trigger mood
symptoms, consistent with the external trigger, or social zeitgeber theory, illustrated in Fig. 1. However, it is unclear
whether bipolar and unipolar individuals are more vulnerable to life events or zeitgebers because they have an
abnormally functioning pacemaker. It is also ambiguous whether social rhythm disruptions act as the mechanism by
which events affect symptoms. For example, many studies did not assess social rhythms prior to life events, assess
life events and social rhythms in close proximity to one another, and group individuals with potentially different
vulnerabilities (i.e., bipolar vs. unipolar individuals). Longitudinal studies to determine the temporal association of
circadian rhythm regularity, life events, and symptoms would eliminate several of these limitations. Further,
standardized interviews (i.e., SADS-L, SCID) should be utilized to identify diagnostic groups and current mood
state, or level of vulnerability, in community samples. This is particularly important as research suggests that social
rhythm disruption events may be more likely to precipitate mania than depression (Malkoff-Schwartz et al., 2000,
1998). Utilizing larger sample sizes will also become important if comparing several groups. Such studies would
allow a detailed examination of the consequences of life events, such as disruptions of social rhythms, and whether
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
691
such consequences vary depending on the mood state (i.e., depressed, manic, mixed) and/or the diagnosis (i.e.,
unipolar, bipolar) of an individual (Chang et al., 2003).
Several studies found that social and physical zeitgebers (i.e., people, meals, noise, room temperature, light) affect
biological rhythms (i.e., cortisol, body temperature, sodium, sleep, heart rate) in community samples; however, there
has been only one study conducted with a unipolar depressed sample and none with a bipolar sample. The lack of
research in this area may be because it is time consuming and expensive research to conduct. For example, it is very
difficult to assess biological rhythms, such as body temperature and hormone levels, outside of a laboratory. Further,
such methodology interrupts participants' lifestyles and, thus, is difficult to do for more than a few days and requires
considerable compensation to participants. Recent advances in noninvasive methods of measuring biological rhythms
in one's natural environment, such as with actigraphy, may further research in this area (Jones et al., 2005). Specifically,
future research should examine the effects of various zeitgebers, and the characteristics of these cues (i.e., intensity,
frequency), on biological rhythms in bipolar and unipolar samples to determine whether social zeitgebers are
responsible for biological circadian rhythm disruptions. If the data fail to support this link, it would undermine the
social zeitgeber theory and suggest that further attention needs to be paid to the influence of the pacemaker on these
rhythms (see Fig. 1).
This review also highlighted the finding that bipolar and unipolar samples may have less social rhythm regularity,
but that this was not associated with their current mood state; however, therapy regularizing social rhythms did improve
mood in a bipolar sample (Frank et al., 2005). Additional research is needed to determine whether social and circadian
rhythm regularity are prospectively predictive of bipolar episodes to lend credence to both theories in Fig. 1.
Improvements upon earlier studies would include utilizing larger and more homogenous samples, assessing social and
circadian rhythm regularity and mood daily for at least two weeks, and utilizing objective measures of circadian activity
(e.g., actigraphy). Preferably, future research would also stabilize participants' medications prior to assessing circadian
rhythm regularity, as medications can alter circadian activity.
In summary, the social zeitgeber theory is an attractive explanation of affective episodes, given that it attempts to
understand how external triggers (e.g., social zeitgebers) may affect mood. However, it is unclear from the literature
whether it accurately reflects the chain of events that culminate in affective episodes. Although the social zeitgeber
theory is an excellent working model, we encourage other investigators to consider and test alternative explanations,
such as the internal trigger theory, or more specifically, vulnerability linked to genetic factors (i.e., serotonin transporter
gene) (for review, see Alda, 2001). Investigators should also consider other explanatory theories of affective episodes,
such as the influence of individual or personality traits (Swendsen et al., 1995), behavioral sensitization to stress (i.e.,
kindling model; Post & Weiss, 1997), for example, due to early trauma (Benes, 1994; Pine, 2003), and dysregulation
due to one's behavioral activation systems (for review, see Johnson, 2005; Johnson & Roberts, 1995; Power, 2005).
The importance of this research is highlighted by the numerous implications of elucidating an accurate model of
affective disorders. For example, it would give treatment teams, families, and patients a framework in which to
understand the mood disorders, as well as aid in their prevention and intervention. Thus, we hope that the issues raised
in this review will stimulate future research that may ultimately lead to a more complete understanding of a causal
pathway to unipolar and bipolar mood episodes.
References
Alda, M. (2001). Genetic factors and treatment of mood disorders. Bipolar Disorders, 3, 318−324.
Alloy, L. B., & Abramson, L. Y. (1999). The Temple–Wisconsin Cognitive Vulnerability to Depression (CVD) Project: Conceptual background,
design, and methods. Journal of Cognitive Psychotherapy: An International Quarterly, 13, 227−262.
Alloy, L. B, Abramson, L. Y, Hogan, M. E., Whitehouse, W. G., Rose, D. T., Robinson, M. S., et al. (2000). The Temple–Wisconsin Cognitive
Vulnerability to Depression (CVD) Project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for
depression. Journal of Abnormal Psychology, 109, 403−418.
Alloy, L. B., Abramson, L. Y., Urosevic, S., Walshaw, P. D., Nusslock, R., & Neeren, A. M. (2005). The psychosocial context of bipolar disorder:
Environmental, cognitive, and developmental risk factors. Clinical Psychology Review, 25, 1043−1075.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th Ed.-Text Rev). Washington DC: American
Psychiatric Association.
Aschoff, J., Fatranska, M., Giedke, H., Doerr, P., Stamm, D., & Wiser, H. (1971). Human circadian rhythms in continuous darkness: Entrainment by
social cues. Science, 171, 213−215.
Ashman, S. B., Monk, T. H., Kupfer, D. J., Clark, A. H., Myers, F. S., Frank, E., et al. (1999). Relationship between social rhythms and mood in
patients with rapid cycling bipolar disorder. Psychiatry Research, 86, 1−8.
692
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
Benes, F. M. (1994). Developmental changes in stress adaptation in relation to psychopathology. Development and Psychopathology, 6, 123−139.
Bendetti, F., Barbini, B., Campori, E., Fulgosi, M. C., Pontiggia, A., & Colombo, C. (2001). Sleep phase advance and lithium to sustain the
antidepressant effect if total sleep deprivation in bipolar depression: New findings supporting the internal coincidence model? Journal of
Psychiatric Research, 35, 323−329.
Brown, G. W., & Harris, T. O. (1978). Social origins of depression. London: Free Press.
Brown, G. W., & Harris, T. O. (1979). The Bedford College Life-Events and Difficulty Schedule: Directory of severity for long-term difficulties.
London: Bedford College, University of London.
Brown, L. F., Reynolds, C. F., Monk, T. H., Prigerson, H. G., Dew, M. A., Houck, P. R., et al. (1996). Social rhythm stability following late-life
spousal bereavement: Associations with depression and sleep impairment. Psychiatry Research, 62, 161−169.
Cermakian, N., & Boivin, B. (2003). A molecular perspective of human circadian rhythm disorders. Brain Research Reviews, 42, 204−220.
Chang, G. H., Alloy, L. B., & Abramson, L. Y. (2003). Examining social rhythm regularity to predict affective episodes in bipolar spectrum
individuals. Bipolar Disorder, 5(Suppl. 1), 39−40.
Christensen, E. M., Gjerris, A., Larsen, J. K., Bendtsen, B. B., Larsen, B. H., Rolff, H., et al. (2003). Life events and onset of a new phase in bipolar
affective disorder. Bipolar Disorders, 5, 356−361.
Chung, R. K., Langeluddecke, P., & Tennant, C. (1986). Threatening life events in the onset of schizophrenia, schizophreniform psychosis and
hypomania. British Journal of Psychiatry, 148, 680−685.
Cobb, S. (1974). A model for life events and their consequences. In B. S. Dohrenwend, & B. P. Dohrenwend (Eds.), Stressful life events: Their nature
and effects. New York: John Wiley & Sons.
Czeisler, C. A., Kronauer, R. E., Mooney, J. J., Anderson, J. L., & Allan, J. S. (1987). Biological rhythm disorders, depression, and phototherapy: A
new hypothesis. In M. K. Erman (Ed.), The psychiatric clinics of North America. Sleep disorders (pp. 687−709). Philadelphia, PA: W. B. Sanders.
Daley, S. E., Hammen, C., Burge, D., Davila, J., Paley, B., Lindberg, N., et al. (1997). Predictors of the generation of episodic stress: A longitudinal
study of late adolescent women. Journal of Abnormal Psychology, 104, 251−259.
Dohrenwend, B. S., & Dohrenwend, B. P. (1981). Life stress and psychopathology. In D. A. Regier, & G. Allen (Eds.), Risk factor research in the
major mental disorders. DHHS Pub. No. (ADM) 81-1068. Washington D.C.: Supt. of Docs, U.S. Govt. Print Off.
Dunner, D. L., Patrick, A., & Fieve, R. R. (1979). Life events at the onset of bipolar affective illness. American Journal of Psychiatry, 136, 508−511.
Eastman, C. I. (1987). The circadian rhythm of temperature in humans during a 26-hour sleep–wake schedule. Physiology and Behavior, 40, 17−23.
Ehlers, C. L., Frank, E., & Kupfer, D. J. (1988). Social zeitgebers and biological rhythms. Archives of General Psychiatry, 45, 948−952.
Ehlers, C. L., Kupfer, D. J., Frank, E., & Monk, T. H. (1993). Biological rhythms and depression: The role of zeitgebers and zeitstörers. Depression,
1, 285−293.
Ellicott, A., Hammen, C., Gitlin, M., Brown, G., & Jamison, K. (1990). Life events and the course of bipolar disorder. American Journal of
Psychiatry, 147, 1194−1198.
Elmore, S. K., Betrus, P. A., & Burr, R. (1994). Light, social zeitgebers, and the sleep–wake cycle in the entrainment of human circadian rhythms.
Research in Nursing and Health, 17, 471−478.
Endicott, J., & Spitzer, R. L. (1978). A diagnostic interview: The schedule for affective disorders and schizophrenia. Archives of General Psychiatry,
35, 837−844.
Ezquiaga, E., Gutierrez, J., & López, A. (1987). Psychosocial factors and episode number in depression. Journal of Affective Disorders, 12,
135−138.
Flaherty, J., Frank, E., Hoskinson, K., Richman, J., & Kupfer, D. (1987). Social zeitgebers and bereavement. Paper presented at the 140th Annual
Meeting of the American Psychiatric Association, Chicago.
Frank, E., Anderson, B., Reynolds, C. F., Ritenour, A., & Kupfer, D. J. (1994). Life events and the research diagnostic criteria endogenous subtype: A
confirmation of the distinction using the Bedford College methods. Archives of General Psychiatry, 51, 519−524.
Frank, E., Hlastala, S., Ritenour, A., Houck, P., Tu, X. M., Monk, T. H., et al. (1997). Inducing lifestyle regularity in recovering bipolar disorder
patients: Results from the maintenance therapies in bipolar disorder protocol. Biological Psychiatry, 41, 1165−1173.
Frank, E., Holly, S. A., & Kupfer, D. J. (2000). Interpersonal and social rhythm therapy: Managing the chaos of bipolar disorder. Biological
Psychiatry, 48, 593−604.
Frank, E., Kupfer, D. J., Thase, M. E., Mallinger, A. G., Swartz, H. A., Fagiolini, A. M., et al. (2005). Two-year outcomes for interpersonal and social
rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry, 62, 996−1004.
Frank, E., Malkoff-Schwartz, S., Sherrill, J. T., & Anderson, B. (1999). Social Rhythm Disruption (SRD) criteria. Pittsburgh: Western Psychiatric
Institute and Clinic.
Frank, E., Swartz, H. A., Mallinger, A. G., Thase, M. E., Weaver, E. V., & Kupfer, D. J. (1999). Adjunctive psychotherapy for bipolar disorder:
Effects of changing treatment modality. Journal of Abnormal Psychology, 108, 579−587.
Glassner, B., & Haldipur, C. V. (1983). Life events and early and late onset of bipolar disorder. American Journal of Psychiatry, 140, 215−217.
Hammen, C. (1991). Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology, 100, 555−561.
Hammen, C., & Gitlin, M. (1997). Stress reactivity in bipolar patients and its relation to prior history of disorder. American Journal of Psychiatry,
154, 856−857.
Hammen, C., Henry, R., & Daley, S. E. (2000). Depression and sensitization to stressors among young women as a function of childhood adversity.
Journal of Consulting and Clinical Psychology, 68, 782−787.
Hammen, C., Marks, T., Mayol, A., & DeMayo, R. (1985). Depressive self-schemas, life stress, and vulnerability to depression. Journal of Abnormal
Psychology, 94, 308−319.
Howland, R. H., & Thase, M. E. (1999). Affective disorders: Biological aspects. In T. Millon, P. H. Blaney, & R. D. Davis (Eds.), Oxford textbook of
psychopathology (pp. 166−202). London: Oxford University Press.
Hunt, N., Jones, W. B., & Silverstone, T. (1992). Life events and relapse in bipolar affective disorder. Journal of Affective Disorders, 25, 13−20.
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
693
Joffe, R. T., MacDonald, C. M., & Kutcher, S. P. (1989). Life events and mania: A case-controlled study. Psychiatry Research, 30, 213−216.
Johnson, S. L. (2005). Life events in bipolar disorder: Towards more specific models. Clinical Psychology Review, 25, 1008−1027.
Johnson, S. L., & Miller, I. (1997). Negative life events and time to recovery from episodes of bipolar disorder. Journal of Abnormal Psychology,
106, 449−457.
Johnson, S. L., & Roberts, J. E. (1995). Life events and bipolar disorder: Implications from biological theories. Psychological Bulletin, 117,
434−449.
Jones, S. E. (2004). Psychotherapy of bipolar disorder: A review. Journal of Affective Disorders, 80, 101−114.
Jones, S. E., Hare, D. J., & Evershed, K. (2005). Actigraphic assessment if circadian activity and sleep patterns in bipolar disorder. Bipolar Disorders,
7, 1−11.
Kennedy, S., Thompson, R., Stancer, H. C., Roy, A., & Persad, E. (1983). Life events precipitating mania. British Journal of Psychiatry, 142,
398−403.
Leskelä, U. S., Melarin, T. K., Lestelä-Mielonen, P. S., Rytsälä, H. J., Sokero, T. P., Heikkinen, M. E., et al. (2004). Life events, social support, and
onset of major depressive episode in Finnish patients. The Journal of Nervous and Mental Disease, 192, 373−381.
Malkoff-Schwartz, S., Frank, E., Anderson, B. P, Hlastala, S. A., Luther, J. F., Sherril, J. T., et al. (2000). Social rhythm disruption and stressful life
events in the onset of bipolar and unipolar episodes. Psychological Medicine, 30, 1005−1016.
Malkoff-Schwartz, S., Frank, E., Anderson, B., Sherril, J. T., Siegel, L., Patterson, D., et al. (1998). Stressful life events and social rhythm disruption
in the onset of manic and depressive bipolar episode. Archives of General Psychiatry, 55, 702−707.
Minors, D. S., & Waterhouse, J. M. (1985). Introduction to circadian rhythms. In S. Folkard, & T. H. Monk (Eds.), Hours of work: Temporal factors
in work-scheduling (pp. 1−14). New York, NY: John Wiley & Sons, Ltd.
Monk, T. H., Flaherty, J. F., Frank, E., Hoskinson, K., & Kupfer, D. J. (1990). The Social Rhythm Metric: An instrument to quantify the daily rhythms
of life. Journal of Nervous and Mental Disease, 178, 120−126.
Monk, T. H., Kupfer, D. J., Frank, E., & Ritenour, A. M. (1991). The Social Rhythm Metric (SRM): Measuring daily social rhythms over 12 weeks.
Psychiatry Research, 36, 195−207.
Monk, T. H., Petrie, S. R., Hayes, A. J., & Kupfer, D. J. (1994). Regularity of daily life in relation to personality, age, gender, sleep quality, and
circadian rhythms. Journal of Sleep Research, 3, 196−205.
Monroe, S. M., & Handjiyannakis, K. (2002). The social environment and depression: Focusing on severe life stress. In I. H. Gotlib, & C. L. Hammen
(Eds.), Handbook of depression. New York, NY: Guilford Press.
Moore-Ede, M. C., Czeisler, C. A., & Richardson, G. S. (1983). Circadian timekeeping in health and disease: Part 1. Basic properties of circadian
pacemakers. New England Journal of Medicine, 309, 469−476.
Nezlek, J. B., Hampton, C. P., & Shean, G. D. (2000). Clinical depression and day-to-day social interaction in a community sample. Journal of
Abnormal Psychology, 109, 11−19.
Panda, S., Hogenesch, J. B., & Kay, S. A. (2002). Circadian rhythms from flies to humans. Nature, 417, 329−335.
Panzarella, C., Alloy, L. B., & Whitehouse, W. (in press). Expanded hopelessness theory of depression: On the mechanisms by which social support
protects against depression. Cognitive Therapy and Research.
Pardoen, D., Bauwens, F., Dramaix, M., Tracy, A., Genevrois, G., Staner, L., et al. (1996). Life events and primary affective disorders: A one year
prospective study. The British Journal of Psychiatry, 169, 160−166.
Paykel, E. S. (2001). The evolution of life events research in psychiatry. Journal of Affective Disorders, 62, 141−149.
Pine, D. S. (2003). Developmental psychobiology and response to threats: Relevance to trauma in children and adolescents. Biological Psychiatry,
53, 796−808.
Post, R. M., & Weiss, S. R. D. (1997). Kindling and stress sensitization. In L. T. Young, & R. T. Joffe (Eds.), Bipolar disorder: Biological models and
their clinical applications (pp. 93−126). New York: Marcel Dekker.
Power, M. J. (2005). Psychological approaches to bipolar disorders: A theoretical critique. Clinical Psychology Review, 25, 1101−1122.
Prigerson, H. G., Reynolds, C. F., Frank, E., Kupfer, D. J., George, C. J., & Houck, P. R. (1994). Stressful life events, social rhythms, and depressive
symptoms among the elderly: An examination of hypothesized causal linkages. Psychiatry Research, 51, 33−49.
Refinetti, R., & Menaker, M. (1992). The circadian rhythm of body temperature. Physiology and Behavior, 51, 613−637.
Reilly-Harrington, N. A., Alloy, L. B., Fresco, D. M., & Whitehouse, W. G. (1999). Cognitive styles and life events interact to predict bipolar and
unipolar symptomatology. Journal of Abnormal Psychology, 108, 1−12.
Sack, R. L., Lewy, A. J., Blood, M. L., Keith, L. D., & Nakagwa, H. (1992). Circadian rhythm abnormalities in totally blind people: Incidence and
clinical significance. Journal of Clinical Endocrinology and Metabolism, 75, 127−134.
Sack, D. A., Nurnberger, J., Rosenthal, N. E., Ashburn, E., & Wehr, T. A. (1985). Potentiation of antidepressant medications by the phase advance of
the sleep–wake cycle. American Journal of Psychiatry, 142, 606−608.
Safford, S. M., Crossfield, A. G., Alloy, L. B., & Abramson, L. Y. (in press). Negative cognitive style, depression, and the reporting of negative life
events: Stress generation, reporting bias, or harsh environment. Journal of Affective Disorders.
Schulz, H., & Lund, R. (1983). Sleep onset REM episodes are associated with circadian parameters of body temperature: A study of depressed
patients and normal controls. Biological Psychiatry, 18, 1411−1426.
Sclare, P., & Creed, F. (1990). Life events and the onset of mania. British Journal of Psychiatry, 156, 508−514.
Segal, D. L., Kabacoff, R. I., Hersen, M., Van Hasselt, V. B., & Ryan, C. F. (1995). Update on the reliability of diagnosis in older psychiatric
outpatients using the structured clinical interview for DSM-III-R. Journal of Clinical Geropsychology, 1, 313−321.
Shear, M. K., Greeno, C., Kang, J., Ludwig, D., Frank, E., Swartz, H., et al. (2000). Diagnosis of nonpsychotic patients in community clinics.
American Journal of Psychiatry, 157, 581−587.
Shen, G. C., Alloy, L. B., Abramson, L. Y., & Grandin, L. D. (submitted for publication). Social rhythm regularity and the onset of affective episodes
in bipolar spectrum individuals.
694
L.D. Grandin et al. / Clinical Psychology Review 26 (2006) 679–694
Simons, A. D., Angell, K. L., Monroe, S. M., & Thase, M. E. (1993). Cognition and life stress in depression: Cognitive factors and the definition,
rating, and generation of negative life events. Journal of Abnormal Psychology, 102, 584−591.
Skre, I., Onstad, S., Torgersen, S., & Kringlen, E. (1991). High interrater reliability for the Structured Clinical Interview for DSM-III-R Axis I
(SCID-I). Acta Psychiatrica Scandanavia, 84, 167−173.
Spitzer, R. L., Endicott, J., & Robins, E. (1978). Research diagnostic criteria: Rationale and reliability. Archives of General Psychiatry, 35, 773−782.
Spitzer, R. L., Williams, J., Gibbon, M., & First, M. B. (1990). Structured clinical interview for DSM-III-R, patient edition/non-patient edition (SCIDP/SCID-NP). Washington, D.C.: American Psychiatric Press, Inc.
Steiner, J. L., Tebes, J. K., Sledge, W. H, & Walker, M. L. (1995). A comparison of the structured clinical interview for DSM-III-R and clinical
diagnoses. Journal of Nervous and Mental Disorders, 183, 365−369.
Stetler, C., Dickerson, S. S., & Miller, G. E. (2004). Uncoupling of social zeitgebers and diurnal cortisol secretion in clinical depression. Psychoneuroendocrinology, 29, 1250−1259.
Swendsen, J., Hammen, C., Heller, T., & Gitlin, M. (1995). Correlates of stress reactivity in patients with bipolar disorder. American Journal of
Psychiatry, 152, 795−797.
Szuba, M. P., Yager, A., Guze, B. H., Allen, E. M., & Baxter, L. R. (1992). Disruption of social circadian rhythms in major depression: A preliminary
report. Psychiatry Research, 42, 221−230.
Vernikos-Danellis, J., & Winget, C. M. (1979). The importance of light, postural and social cues in the regulation of the plasma cortisol rhythm in
man. Chronopharmacology; proceedings of the Satellite Symposium of the 7th International Congress of Pharmacology (pp. 101−106). Paris.
Vogel, G. W., Vogel, F., McAbee, R. S., & Thurmond, A. J. (1980). Improvement of depression by REM sleep deprivation. Archives of General
Psychiatry, 37, 247−253.
Wehr, T. A., Sack, D. A., Duncan, W. C., Mendelson, W. B., Rosenthal, N. E., Gillin, J. C., et al. (1985). Sleep and circadian rhythms in affective
patients isolated from external time cues. Psychiatry Research, 15, 327−339.
Wehr, T. A., & Wirz-Justice, A. (1982). Circadian rhythm mechanisms in affective illness and in antidepressant drug action. Pharmacopsychiatry, 15,
31−39.
Wehr, T. A., Wirz-Justice, A., Goodwin, F. K., Duncan, W., & Gillin, J. C. (1979). Phase advance of the circadian sleep–wake cycle as an
antidepressant. Science, 206, 710−713.
Wever, R. A. (1975). Autonomous circadian rhythms in man: Singly versus collectively isolated subjects. Naturwissenschaften, 62, 443−444.
Wever, R. A. (1979). The circadian system of man: Results from experiments under temporal isolation. New York, NY: Springer Verlag.
Wever, R. A. (1989). Light effects on human circadian rhythms: A review of recent experiments. Journal of Biological Rhythms, 4, 161−185.
Williams, J. B. W., Gibbon, M., First, M. B., Spitzer, R. L., Davies, M., Borus, J., et al. (1992). The Structured Clinical Interview for DSM-III-R
(SCID). II. Multi-site test–retest reliability. Archives of General Psychiatry, 49, 630−636.
Winget, C. M., Vernikos-Danellis, J., & Beljan, J. R. (1975). Synchrony of physiological rhythms is regulated by social zeitgebers. The Physiologist,
18, 1025.
Wirz-Justice, A. (2006). Biological rhythm disturbances in mood disorders. International Clinical Psychopharmacology, Suppl 1, S11−S15.
Wu, J. C., & Bunney, W. E. (1990). The biological basis of an antidepressant response to sleep deprivation and relapse: A review and hypothesis.
American Journal of Psychiatry, 147, 14−21.
Zanarini, M. C., & Frankenburg, F. R. (2001). Attainment and maintenance of reliability of axis I and axis II disorders over the course of a
longitudinal study. Comprehensive Psychology, 42, 369−374.