Proprioceptive Neuromuscular Facilitation for the
advertisement

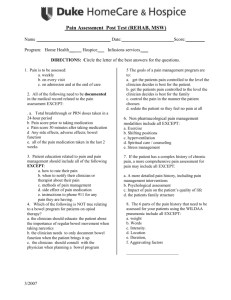
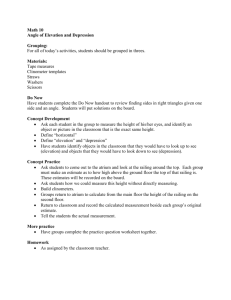
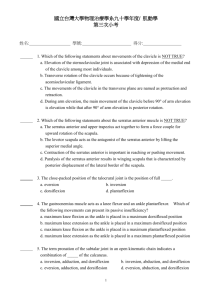
FUNCTIONAL REHABILITATION R. Barry Dale, PhD, PT, ATC, CSCS, Column Editor Proprioceptive Neuromuscular Facilitation for the Scapula, Part 2: Diagonal 2 T HIS COLUMN DESCRIBES the general principles of applying proprioceptive neuromuscular facilitation (PNF) to the scapula and is a continuation from the March Functional Rehabilitation column, which addressed Diagonal Pattern 1 (D1) for the scapula. The basic principles discussed in the previous column remain the same with respect to the athlete’s position and the clinician’s hand placement and body position. Similar to D1, the second scapular diagonal (D2) consists of two positions from which movement begins or ends. These two positions are anterior depression and posterior elevation, and the athlete may move from either position as a starting point.1 Table 1 presents a summary of hand placements and movements in both diagonals. Positioning the Athlete The side-lying position is perhaps best for the athlete because it allows the clinician to control the involved scapula with relative ease. The athlete should lie on the unaffected side with pillows between the knees and supporting the head and involved upper extremity. The athlete’s body segments should be in a neutral position; for example, the head properly aligned with the trunk (watch for excessive cervical flexion) and the trunk not rotated or laterally flexed. Observe the scapula and pelvis for neutrality, with particular attention to protraction and retraction. D2 Movements in this diagonal relate well to scapular movement during many sport-specific activities, and the clinician should consider concentric and eccentric muscle actions and their relationship to sport specificity. The following discussion relates to a clinician treating an athlete’s right scapula. Concentric Movement From Anterior Depression to Posterior Elevation The athlete’s scapula begins in a position of protraction and depression (anterior depression). Movement into elevation and retraction occurs as the scapular elevators and retractors act concentrically. The clinician’s right hand should be on the spine of the scapula while the left hand contacts the acromion (Figure 1). Only the heel of each hand should contact the athlete during this movement to avoid facilitation of antagonistic muscle groups. The clinician’s body should face the athlete’s right lower extremity to adequately resist scapular elevation and retraction. Eccentric Movement From Posterior Elevation to Anterior Depression Eccentric activity of the scapular elevators and retractors occurs as the athlete resists the clinician moving the scapula into protraction and depression from a retracted and elevated position. The clinician’s hand placement does not change during this phase if it follows the concentric movement. Rather, the movement direction reverses as the athlete slowly resists the clinician providing the movement force. Concentric Movement From Posterior Elevation to Anterior Depression Although body positions for both the athlete and the clinician remain the same for concentric movement from posterior elevation to anterior depression, the © 2005 Human Kinetics • ATT 10(3), pp. 51-53 ATHLETIC THERAPY TODAY MAY 2005 51 Table 1. Scapula Positions and Clinician Hand Placements for Proprioceptive-Neuromuscular-Facilitation Diagonals1 Procedure AE (D1) concentric eccentric PD (D1) concentric eccentric AD (D2) concentric eccentric PE (D2) concentric eccentric Position Verbal Command Scapula begins in posterior depression. Both of the clinician’s hands are placed over the anterior acromion. Scapula begins in anterior elevation, moves to posterior depression. Clinician’s hands remain the same. Pull your shoulder blade up and forward, toward your nose. Allow your shoulder to move slowly as I pull your shoulder blade down and back. Scapula begins in anterior elevation. The left hand contacts the spine of the scapula, whereas the right hand frames the inferior border with the thumb and index finger. Scapula begins in posterior depression, moves to anterior elevation. Clinician’s hands remain the same as for concentric movement. Push your shoulder blade down and back. Scapula begins in posterior elevation. Clinician’s left hand contacts the anterior axilla, whereas the right hand contacts the posterior axilla, with the fingers of both hands providing resistance to protraction and depression. Scapula begins in anterior depression. Clinician’s hands remain the same as for concentric anterior depression. Pull your shoulder blade forward and down. Scapula begins in anterior depression. Clinician’s hand placement is similar to that during anterior depression except that the fingers are extended to avoid contact with the axilla as the heels of both hands contact the acromion and spine of the scapula. Scapula begins in posterior elevation. Clinician’s hand placement is identical to that for concentric movement. Push your shoulder blade up and back. Allow your shoulder to move slowly as I push your shoulder blade up and back. Allow your shoulder to move slowly as I pull your shoulder blade up and back. Allow your shoulder to move slowly as I push your shoulder blade forward and down. Note. The table uses the athlete’s right scapula as reference. AE = protraction combined with elevation; D1 = Diagonal 1; PD = retraction combined with depression; AD = protraction combined with depression; D2 = Diagonal 2; PE = retraction combined with elevation. Figure 1 Athlete’s position and clinician’s hand placement for concentric movement from anterior depression into posterior elevation. 52 MAY 2005 clinician’s hand placement must shift to resist concentric activity of the scapular protractors and depressors. Clinician hand placement changes to allow proprioceptive input and resistance to the scapular depressors and protractors. The hand that was previously on the spine of the scapula now contacts the posterior axilla while the hand formerly on the acromion shifts to the anterior axilla (Figure 2). The hand placements in this diagonal are easier than those in the first diagonal, especially when performing concentric or eccentric reversals between posterior elevation and anterior depression. Once the proper hand position is attained, the clinician places the athlete’s scapula in retraction and ATHLETIC THERAPY TODAY Figure 2 Athlete’s position and clinician’s hand placement for concentric movement from posterior elevation into anterior depression. elevation and then instructs the athlete to move the shoulder downward and forward. Again, it is helpful to allow several practice movements, which can be passive or active. Eccentric Movement From Anterior Depression to Posterior Elevation The athlete’s scapula begins in anterior depression and resists the force of the clinician’s hands, slowly allowing the scapula to move into posterior elevation. This requires eccentric control of the anterior depressors and posterior elevators. Again, the clinician’s hand placements do not change when switching between concentric and eccentric movements. Reversals Reversals require the clinician to change hand placement at the end of a given movement in order to begin the antagonistic movement. Whereas it was beneficial to leave one hand in place when performing reversals ATHLETIC THERAPY TODAY in D1, D2 hand placements are such that the clinician’s hands can easily shift positions to provide adequate resistance in the appropriate direction. In an example movement from concentric posterior elevation with a reversal into concentric anterior depression, the athlete begins in protraction and depression with the clinician’s hands over the scapular spine and anterior acromion. Next, the clinician instructs the athlete to move the scapula upward and back while providing adequate resistance. As the athlete achieves scapular retraction and elevation, the clinician shifts his or her hands downward and forward to contact the anterior and posterior portions of the axilla while instructing the athlete to move the shoulder downward and forward. Summary Applying PNF to the scapula assists muscle recruitment and reeducation and enables functional movement. This column presented D2; the one in the March 2005 issue presented D1. Acknowledgment Special thanks to Jonathon Shaw and Dr. Dennis Fell for their assistance in preparing the photographic elements. References 1. Adler SS, Beckers D, Buck M. The scapula and pelvis. In: Adler SS, Beckers D, Buck M. PNF in Practice: An Illustrated Guide. 2nd ed. New York, NY: Springer; 2000:63-74. Barry Dale is an assistant professor at the University of South Alabama. His areas of interest include orthopedics, neurology, and exercise physiology. MAY 2005 53