OXYCODONE CONTROLLED RELEASE MEDICATION
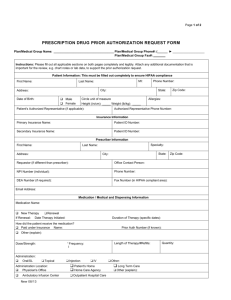
advertisement

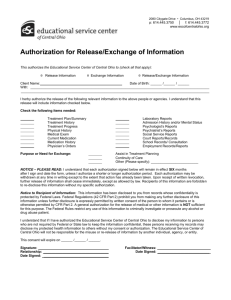
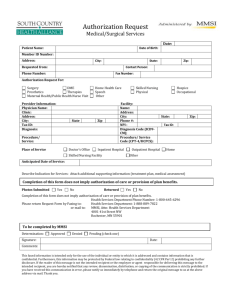
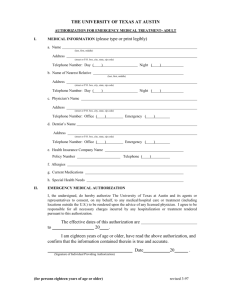
MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES PROCEDURES TO REQUEST PRIOR AUTHORIZATION ON CONTROLLED RELEASE OXYCODONE/OXYCONTIN® CONTENTS I. PAGE Procedures to Request Prior Authorization for Controlled Release Oxycodone/OxyContin® A. B. C. D. E. A-23 Effective Date of Prior Authorization Thresholds for Prior Authorization Emergency Supplies Early Fills Initiating the Prior Authorization Request 1. Who May Initiate the Request 2. Where and When to Call 3. Information to Be Available for the Prior Authorization Review and Documented Within the Medical Record F. Review Process 1. Use of Medical Necessity Review Criteria 2. Timeliness of the Review 3. Approval/Prior Authorization Number 4. Long Term Therapy 5. Peer Review A-23 A-23 A-24 A-24 A-24 A-24 A-24 II. Dispensing Considerations A-26 III. Clinical Criteria for the Medical Necessity Review of Controlled Release Oxycodone/OxyContin® A. Brand Name B. Generic Name C. Oral Tablet Strengths/Generic Codes D. FDA Indication E. Criteria Elements F. Expert Panel review and Approval G. Literature References A-26 A-26 A-26 A-26 A-26 A-26 A-27 A-27 A-21 A-24 A-25 A-25 A-25 A-25 A-25 A-25 December 2001 MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES THIS PAGE IS INTENTIONALLY BLANK A-22 December 2001 MEDICAL ASSISTANCE HANDBOOK I. PHYSICIANS’ SERVICES Procedures to Request Prior Authorization of Prescriptions for Controlled Release Oxycodone/Oxycontin® The procedures outlined within this section of the Physicians’ Services Handbook relate to the requirements for prior authorization of certain prescriptions for OxyContin® under the Medical Assistance (MA) Program, fee-for-service component. Many of the HealthChoices managed care organizations (MCOs) also have requirements for prior authorization of OxyContin®. Prescribers are referred to the procedures defined by the applicable MCO for managed care prior authorization requests. A. Implementation Date for Prior Authorization OxyContin® prescriptions meeting the thresholds outlined below, dispensed on and after January 7, 2002, will require prior authorization. B. Thresholds for Prior Authorization The Department will require prior authorization for prescriptions for OxyContin® that meet either or both of two (2) conditions: 1) Prescriptions that exceed doses of greater than three (3) tablets per day of any single strength of OxyContin®. The number of tablets per day is determined by the prescriber within the prescribed directions for use. Directions for use are required on all Medical Assistance prescriptions (see Physicians’ Services MA Handbook, Section I, General Information, page I-9). However, upon dispensing the medication, the pharmacist plays a key role in transmitting accurate information to the Department. The pharmacist enters the “days’ supply” which in turn drives the automated system alerts for prior authorization. The tablets per day value is system calculated by dividing the quantity dispensed by the days supply. Pharmacists need to appreciate the need for entering accurate information within the days’ supply field as this element is key to an accurate alert for prior authorization for OxyContin®. A shortening of the days’ supply to avoid a later early refill alert can inaccurately increase the calculated tablets per day and trigger a prior authorization that may not be necessary. 2) Prescriptions for more than two (2) different strengths of OxyContin® that are taken concurrently. Regardless of whether the third, or any subsequent, strength is actually being taken concurrently, the Electronic Claims Management (ECM) pointof-sale on-line claims adjudication system may recognize the medication as taken concurrently depending on the amount of time elapsing between prescriptions. Accordingly, where the prescriber is aware that a third, or additional, strengths are prescribed within the same timeframe that the A-23 December 2001 MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES earlier strengths would have covered, the prescriber should request a prior authorization. Note: It is possible for a physician to prescribe up to six (6) tablets per day of OxyContin®, i.e., three (3) tablets for each of up to two (2) strengths without prior authorization. C. Emergency Supplies The Department does not consider a delay in the receipt of OxyContin® to present a life threatening emergency and, therefore, will NOT cover emergency supplies of OxyContin® pending approval of a request for prior authorization. Temporary alternative methods of pain relief may be necessary. D. Early Fills Additionally, early fills, i.e., dispensing an OxyContin® prescription when more than 25% of an earlier dispensed supply remains, will not be approved and prior authorization will not be granted for any exceptions. E. Initiating the Prior Authorization Request 1. Who May Initiate the Request The prescriber must request the prior authorization. 2. Where and When to Call Prior authorization requests will be accepted by the MA Fee-for-Service Program Prior Authorization Unit at 1-800-558-2660 between the hours of 8:00 AM and 4:00 PM, Monday through Friday. 3. Information To Be Available for the Prior Authorization Review and Documented Within the Medical Record The information required at the time of a prior authorization review includes the name and ACCESS card number of the recipient, the prescriber’s license number and what is being prescribed, i.e.,: drug, strength, quantity, directions/days’ supply. Additionally, clinical information to apply the medical necessity criteria for OxyContin® will be necessary. (The criteria are provided in Section III. of these procedures.) Using criterion element number one (1) as an example, a description of the etiology, severity, nature/type of pain and any effect on the performance of the activities of daily living (ADL) will need to be provided.) The clinical information, provided during the course of the review, must also be verifiable within the patient’s medical record. Upon retrospective review, the Department may seek restitution for the cost of the A-24 December 2001 MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES prescription and any applicable restitution penalties from the prescriber, if the medical record does not support the medical necessity for the prescription. (Reference 55 Pa. Code § 1101.83 (b)). F. Review Process 1. Use of Medical Necessity Review Criteria Department nurse reviewers will accept the prior authorization request and apply review criteria to assess the medical necessity of the drug and the dosage level. These criteria are included in section III on page A-26. 2. Timeliness of Review The Department will respond to prior authorization review requests within twenty-four (24) hours. 3. Approval/Prior Authorization Number If the Department approves the request, a ten (10)-digit prior authorization number will be issued. This number should be documented on the prescription and within the medical record in the event that the prescriber needs to reference the number for the patient/pharmacy. 4. Long Term Therapy The Department will consider requests to authorize multiple prescriptions for a recipient during the prior authorization review when, in the professional judgment of the reviewer, the condition producing the pain reasonably can be expected to continue for longer than thirty (30) days. The reviewer will approve multiple prescriptions consistent with the expected duration of the pain/therapy, but not to exceed six (6) prescriptions or six (6) months. When multiple prescriptions are approved during a review, both the prescriber and the recipient will receive written confirmation of the prior authorization numbers and related prescription information. Note: Authorization for multiple months does not waive the requirement for original prescriptions for each month approved. 5. Peer Review If the criteria are not met, the prior authorization request will be referred to the physician review level for a determination. A-25 December 2001 MEDICAL ASSISTANCE HANDBOOK II. PHYSICIANS’ SERVICES D ispensing Considerations The prescriber should also be aware that the MA ECM point-of-sale on-line claims pharmacy system is being modified to assist in the monitoring of the requirements for controlled release oxycodone/OxyContin®. The on-line system may detect a need for prior authorization not previously known to the prescriber. For example, if a consumer is receiving prescriptions from multiple prescribers unknown to each other and the system detects multiple strengths or an excessive tablet supply, prior authorization will be required. The pharmacist should contact the prescriber to alert the prescriber that the prescription has tripped the threshold level and prior authorization is now required. The prescriber should not ask the pharmacist to call for the prior authorization number. Prior authorization numbers will be provided only to the prescribing physician. III. Clinical Criteria for the Medical Necessity Review of Controlled Release Oxycodone/OxyContin® A. Brand Name OxyContin® B. Generic Name Controlled Release Oxycodone C. Oral Tablet Strengths/Generic Codes 10mg/16282 20mg/16283 40mg/16284 80mg/16286 160mg/92459 (not currently available from manufacturer) D. FDA Indication The controlled release oral form of oxycodone/OxyContin® is indicated for the management of moderate to severe pain when a continuous, around-the-clock opioid analgesic is needed for an extended period of time. OxyContin® is not intended for use as a PRN (“as needed”) analgesic or for acute, short-term pain relief. E. Criteria Elements All three (3) of the following medical necessity criteria elements must be met in the professional judgment of the reviewer, for verification of medical necessity and approval of prior authorization at a non-physician review level. Situations not meeting one or more of the following criteria will be considered on a case-by case basis by a physician reviewer to determine the medical necessity. A-26 December 2001 MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES 1. There is a documented history of pain that includes all of the following: • • • • Pain arises from a chronic condition; AND Pain is moderate to severe in nature; AND Pain is sustained and persistent rather than brief and intermittent; AND Pain interferes with the activities of daily living (ADL) such as work, mobility, sleep, eating, personal hygiene and social functioning. 2. A narcotic pain reliever is the most appropriate treatment option as documented by one or more of the following elements: • Pain is inadequately controlled by non-narcotic pain relievers, including non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen (APAP), and aspirin (ASA); OR • Recipient exhibits contraindications to non-narcotic pain relievers, such as allergy, drug-disease interaction, drug-drug interaction, history of adverse reaction; OR • There is documentation regarding an earlier episode of the same pain etiology and nature where management with non-narcotic medication was inadequate; OR • The pain is so severe that it would be appropriate to initiate pain management with opioids such as pain resulting from metastatic disease or severe orthopedic trauma. 3. The proposed dosage is the minimum effective dosage. For doses and dosing intervals that exceed the FDA-approved starting dose of 10 mg. every twelve (12) hours, there is documentation demonstrating an appropriate upward titration of Oxycontin® or an appropriate conversion from other opioidcontaining medications. F. Expert Panel Review and Approval These criteria have been reviewed and approved by an independent panel of experts including multiple physician specialties, pharmacists and a consumer representative. The physician specialties represented included anesthesiology, addiction medicine, hematology, oncology, pain management and family practice. Additionally, the panel included pharmacists from the University of Maryland, School of Pharmacy’s Center on Drugs and Public Policy and staff from the Pennsylvania Medical Society’s Center for Professional Drug Education. G. Literature References References included, but were not limited to: Jacox A, Carr DB, Payne E, et al. Management of cancer pain. Clinical practice guideline no. 9, AHCPR Publication No. 94-0592. Agency for Health Care Policy A-27 December 2001 MEDICAL ASSISTANCE HANDBOOK PHYSICIANS’ SERVICES and Research, U.S. Department of Health and Human Services, Public Health Service. Rockville, MD. 1994. Model guidelines for the use of controlled substances for the treatment of pain. Federation of State Medical Boards of the United States, Inc. May 2, 1998. Purdue Pharma LP. Product Information: OxyContin®; July 2001. A-28 December 2001