Neurophysiologic Reflexes of postural Regulation
advertisement

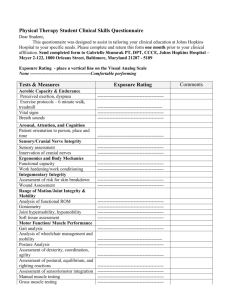
Neurophysiologic Reflexes of postural Regulation Laura Hanson, D.C., D.I.C.C.P., NDT www.originaldevelopment.org Posture Development • Postural reflexes • Milestones • Locomotion Environment • Free style vs restrained style • Learning to roll and sitting up requires using the abdominal muscles – the beginning of posture Sitting Posture • Around 7 to 8 months • Do not leave to sway unsteadily • Muscles of the abdomen, back Balancing Upright • Muscles of the abdomen • Muscles of the buttock • Muscles of the shoulders and upper back • Muscles holding the feet in the correct position The Walking Child Shoulder and neck hold the chest up and chin in Buttock muscles help the lower spine from hollowing Lower Abs pull in by 5 years of age The Feet in Good Balance • The child’s weight is on the balls of the feet and the outer sides • The toes point forward and the inner sides of the feet are parallel with each other Muscular Imbalances • Child’s weight falls on the inner sides of his feet • Toes shift outward • Long arch of the foot flattens • Poor balance Entertaining baby holders teach the child to walk on the inner parts of the feet with the legs spread apart and maintains the baby in one posture for long periods of time causing fatigue. Use or Lose It! Biomechanical Relationship Compression: push Tension: Shear: pull slide Torsion: rotate or twist • Gravity and tone create rhythm • Gravity and rhythm increase tone • Tone, rhythm, and gravity create movement Cognitive System Emotional System Movement System Reflexive Control • Central generators neural networks that can endogenously (i.e., without rhythmic sensory or central input) produce rhythmic patterned outputs“ • “Neural circuits that generate periodic motor commands for rhythmic movements such as locomotion.“ • CPGs have been shown to produce rhythmic outputs resembling normal "rhythmic motor pattern production" even in isolation from motor and sensory feedback from limbs and other muscle targets Postural Reflexes • • • • • Visual Righting Reflexes Labyrinthine Righting Reflexes Neck Righting Reflexes Body on Head Righting Reflexes Body on Body Righting Reflexes Gravity Location of Center of Gravity in Human Body Shapes Red X marks the Spot • The human body responds to this constant force • From the time the infant lifts the head to mature gait • Gravity as the main reference point • Postural reflexes serves as the neuromotor impetus for this adaptive response Outcome • Constant barrage of afferent input into the NS, causing a hypersensitive state within the neuronal receptor pool • Pools are made largely from interneurons, allowing sensory input to be conveyed to a higher spinal and cortical centers • Simultaneously providing input for spinal reflexive control of various functions Visual Input • Pathway optic nerve, optic chiasm, optic tracts • Projecting to 3 subcortical areas: pretectum, superior colliculus, lateral geniculate body Vision and Posture • Visual input for postural control helps to fixate the position of the head and upper trunk in space • Maintaining the center of mass of the trunk balanced over the arches of the feet • Studies involving patients with visual vertigo – visual distortion markedly reduced postural control • Visual disorders correlated with postural deformity as seen in scoliosis Vision • A role in the regulation of upright posture • Maintaining the head in space • Alterations in head posture may develop secondarily to visual changes • Studies show people wearing glasses may demonstrate a change in head position • People who wear multifocal lenses tend to exaggerate forward head posture to use the lenses • Refraction problems (vision) – sensorial exteroception of the eye – convergence problems (proprioception) – Refraction disorders • myopia, astigmatism, hypermetropia which are generally recognised and treated • convergence disorders are very rarely diagnosed. • Remove head tilt • Child is instructed to look up and down for approximately 1520 seconds • If head tilt continue move on….. • Identify tropia – Deviation of the eye from the normal position HYPO Note the weak eye A convergence defect never corrects itself, it generates a new body image which functions with the defect and the postural disorder that accompanies it. If one has a convergence defect, in the absence of treatment, it is for life! • Asymmetrical oculomotor tension leads to asymmetrical muscular tension cervical spine • Lack of ROM of the neck • Neurological link between the muscles of the eye (III, IV, VI) and the cranial nerve XI • They connect via the sensory division of the V: upper trapezius and SCM are related and dependent on the eye • Neuro link between the first cervical nerve and the XI, the sub occipitals are involved. IN CHILDREN; · Easily fatigued; · Diminished intellectual abilities; · Difficulties at school (lazy or turbulent children); · Dysgraphia; · Spelling difficulties; · Difficulties in learning to read; · Poor performance in sports activities; · Short legs in children. • Examiner identifies depression or elevation of eye movements ABD ADD D E D E • Note horizontal deviations: • Intorsion – top of the eye turns inward – Superior Oblique • Extorsion – top of the eye turns out – Inferior Oblique Visual Input • Neuronal relay is based upon relative perception • Higher cortical functions are necessary to differentiate between a fixed person within a moving environment, or a moving person within a fixed environment • Postural corrections are made in the direction of visual stimulation • Afferent stimulation differentiates who is moving or what is moving • Even small changes in posture can occur resulting from changes in light or subconscious threshold • Real-time posture does not receive much contribution from higher-level processes • Infants learn to assume a sitting position in response to visual cues in their environment • Repetitive practice of sitting and heighten sense to visual variables develops visuomotor coordination Oculomotor Proprioception • Dual-control system is responsible for afferent input into the oculomotor nuclei • One pathway serves to generate eye rotations • Second pathway provides sensory information regarding eye alignment and stabilization • Proprioception passes through the optic tract nucleus, rostral portion of the superior colliculus Superior Colliculus • Essential role in head and eye orientation and coordination • Important in the integration centers for the extraocular proprioceptive pathways and the trigeminal nucleus • Extensive reciprocal feedback pathway with the reticular formation • The trigeminal nerve provides sensation to the face and contains both sensory and motor aspects. • The sensory component provides tactile, proprioception and Nociception afference of the face and mouth. The motor component is for biting, chewing, and swallowing. • A complete sensory map of the face and mouth converge and communicate through CN V, VII, IX and X. The counter parts of the dorsal horn and dorsal column nuclei contain a complete sensory map of the rest of the body. Face Tapping Fixing the Head and Trunk in Space • Stabilizes the visual field for gaze stabilization • Stabilizes the center of mass of the head and trunk within feet support • Minimizes the external stress acting upon head and trunk Vestibular Input • Provides sensory input about sustained postural stimulation • Components utricle, saccule (linear translations), 3 semicircular canals (rotations) • Utricle (head tilts) and saccule (head position relative to visual field) provide head position relative to gravity • Utricle and saccule transmit to brainstem and cerebellum Transmission • Afferent information is transmitted along the vestibular nerve • Vestibular nuclei receives from the vestibular nerve, the cerebellum and the optic tract • Vestibular nuclei projects to the thalamus, superior colliculus, reticular formation, cerebellar flocculus, and lower vestibular nuclei • Of special interest is the lateral vestibular nucleus or Deiter’s nucleus projects to the vestibulospinal tract • Heel-to-toe test – Age 6 years hold posture for at least 7 seconds – Observe arm position – Observe feet for navigation • Start with dominant leg eyes open and eyes closed – 6 year old should be able to stand in EC posture for 10 seconds • Repeat to the other side • Examines the length of time nystagmus last following rotation of the child • Child in chair, head flexed, 10 spins in 20 seconds • Normal: lasts 7-14 seconds • <7=hypo • >14=hyper • Neurological system cannot regulate the amount of information bombarding the CNS • Sensory overload • Brain unable to ignore all the vestibular information • After playing children may complain of an upset stomach or dizziness • Does not receive or correctly process information about movement, changes in direction, and relationship to gravity • The child will have a difficult time determining if they are up or down • Low muscle tone • Poor equilibrium • Hyper – Slow swinging – Rocking – Slow linear movements – Jumping – Directional change – Linear walking – Linear movement • Hypo – Spinning – Swinging – Jumping – Accelerating decelerating – Changing directions quickly Vision and Vestibular • Constantly interact for upright posture and tone • Reflexive modulation – Vestibulo-ocular reflex • Tract modulation – Vestibulospinal tract – Dorsal and ventral spinocerebellar tract Vestibulo-ocular Reflex (VOR) • Compensates for head rotations or accelerations • 3 components – VOR detects rotations through semicircular canals – VOR detects linear acceleration of the head via the utricle and saccule – Ocular counter-rolling response or optokinetic reflex adapting eye position during head tilting and rotation The Key is Integration • The integration of the head and eyes for body posture is the VOR • The cerebellar flocculus is responsible for integrating and executing the efferent corrections of the VOR Cerebellum Development • Characterization of the cerebellar territory at the midbrain-hindbrain boundary • Formation of two compartments for cell proliferation: first, the Purkinje cells and the deep cerebellar nuclei arise from the ventricular zone of the metencephalic alar plate; second, granule cell precursors are formed from a second compartment of proliferation, i. e. the upper rhombic lip (6 to 8 weeks gestation) • Inward migration of the granule cells: granule precursor cells form the external granular layer, from which (continuing into the first postnatal year) granule cells migrate inwards to their definite position in the internal granular layer • Formation of cerebellar circuitry and further differentiation Purkinje Cells • Largest neurons in the human brain • Large number of dendritic spines • Parallel fibers make relatively weaker excitatory synapses to spines in the Purkinje cell dendrite, whereas climbing fibers originating from the Inf Olivary Nuc in the Medulla provide very powerful excitatory input to the proximal dendrites and cell • Send inhibitory projections to the deep cerebellar nuclei, and constitute the sole output of all motor coordination in the cerebellar cortex. Medial and Lateral Vestibulospinal Tracts • Efferent equivalents of the VOR • Modulating motor to the axial and appendicular muscles for rapid postural adaptations • The cerebellum where afferent input from visual through the vestibular nerve and cervical mechanoreceptors is collected • Compensation is made by the trunk and extremities to the head position Vestibulospinal Tract • Reflexive correction to sudden perturbations in static upright posture • Visual is responding to constant postural adatations • The vestibular apparatus through the vestibulospinal tract is quicker to respond to slight postural disruptions, allowing for a faster response from the skeletal postural muscles Dorsal and Ventral Spinocerebellar Tracts • Sensory signals to the cerebellum • Through joint, skin, muscle spindles and GTO afferents • Mapping position sense of the lower extremity • Coordination for locomotion • Spinal interneurons between thoracic 1 and lumbar 2 Trouble in Development Cervical Mechanoreceptors • Head on neck position – – – – Facet joints Capsule Spinal ligaments Proprioceptive input from cervical muscles Chiropractic Cervical facets contribute to postural orientation, injury may produce postural symptoms like vertigo and dizziness • Facets MR provide afferent postural input to trochlear, abducens, spinal trigeminal, central and lateral cervical and vestibular nuclei, cerebellar flocculus and vermis Posterior Longitudinal Ligament • Extensive sensory input for postural control • Provided by Pacinian and Ruffini corpuscles • Afferent connections with the gracilis and cunneatus, vestibular nuclei, thalamus, sympathetics, and muscle spindles Cervical Muscles • The upper cervical spine contains a higher density of muscle spindles than in any other spinal region • Affected by visual field and vestibular apparatus Cervical Torticollis • Responding to 15 min of cervical vibration • Muscle spasm may be associated with aberrant afferent input relaying head position to the CNS • Cervical input plays a major role during locomotion and less in coordinated static posture Visual and the Cervical Spine • Cervico-ocular reflex • Cervicocollic Reflex • Vestibulocollic Cervico-ocular Reflex • Orient eye movements to changes in neck and trunk positions • The trunk, cognitive interpretation, retinal information contribute to the plasticity of the COR • Intact optokinetic reflex Cervicocollic Reflex • Orient the position of the head in relation to disturbed trunk posture • Like a stretch reflex • Reflexive correction of cervical spine position through co-contraction of specific cervical muscles by activating muscle spindles • Communication between CC and VCR Vestibulocollic • Evaluate through perturbations of the head in the horizontal plane. • Dissociated from the vestibulospinal reflex which orients the extremities to the position of the head and neck • Reflex based on stimulation of cervical afferents directly • Globally through the reticular formation for interpretation throughout the CNS and sensitivity Development of Postural Control • Infant’s orientation at 2 months is dependent on visual cues for head and trunk 4 to 6 Months • Postural reflexive mechanisms such as crawling begin to incorporate joint MR and the vestibular system Head Control Head position relative to gravity trunk and lower extremity control can be learned using a fixed reference point Pelvo-ocular reflex • Neuromotor responses are coordinated in the lower extremities before trunk and upper extremities • Serves to orient the body region in response to head position and anticipatory visual reference cues 8 – 14 Months • Infants can process multiple postural sensory stimulation Biomechanical Development • Structural and functional development of the spine appears to result from upright posture in gravity • Sagittal curves allow for balance between strength and flexibility • Microgravity to gravity • Forces experienced a birth develop the muscle bone lever system • Balance of tone Progression of Curves Network of Postural Control • • • • Head upright Stand upright Stabilizing trunk, pelvic, lower extremities Global posture and spine balancing head, neck, trunk over the base of support = feet Ossification • Active muscular stabilization increases the stress on musculotendinous junctions and osseous attachments for bone development • Standing repeatively coordinates neuromotor control of the lower extremities and spine integrating head and neck with the cerebellum Center of Mass • • • • Tone Body Image Balance Performance Abdominal Tone Center of Mass Glute Max Abdominals Hamstring Quadratus Lumborum Piriformis TFL Upper Traps SCM Problems w/ Core • • • • Visceroptosis Back pain Poor diet/lifestyle Exercising on machines Spine Vol 30(21), 1 November 2005, pp2388-2392 • Spinal Kyphosis Causes Demyelination and Neuronal Loss in the Spinal Cord • Conclusions: Progressive kyphosis of the cervical spine resulted in demyelination of nerve fibers in the funiculi and neuronal loss in the anterior horn due to chronic compression of the spinal cord. These histologic changes seem to be associated with both continous mechanical compression and vascular changes in the spinal cord. Single-Leg Stance BalanceTest • Maintain balance EC for 30 seconds • Repeat four times to reach peak performance • • • • 20-49yrs/24-28 sec. 50-59 yrs/21 sec. 60-69 yrs/10 sec. 70-79 yrs/4 sec. Short Foot Lever • Balance training begins with careful attention to formation of a good arch in your foot without bending your toes (BullockSaxton, et al., 1993, Janda, Va'vrova' 1990;Janda, Va'vrova' 1996) Sensory Motor Training Stabilization From the Ground Up!