Upper Cervical Ligament Testing in a Patient With Os
advertisement

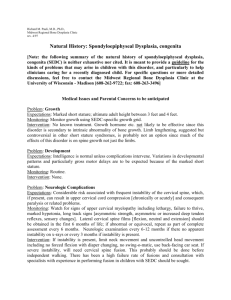
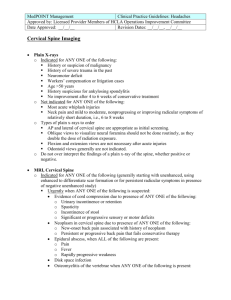
[ RESIDENT’S CASE PROBLEM ] PAUL E. MINTKEN, PT, DPT1,2B?I7C;JH?9A"PT, DPT²J?CEJ>O<BODD"PT, PhD3 Upper Cervical Ligament Testing in a Patient With Os Odontoideum Presenting With Headaches P hysical therapists play an important role in the screening of patients with cervical spine conditions. Headaches are commonly treated by physical therapists, 9,10,19,20,25, 35, 36, 38,48, 96 and a thorough differential diagnosis is often needed to determine if the headaches are of musculoskeletal origin.56 The lifetime prevalence of headache (encompassing all headache types) has been estimated to be 93% to 98%, and up to 17.8% of individuals with headaches meet the International Headache Society classification criteria for cervicogenic headache.65 Physical therapy is often considered a first-line treatment for these patients.10 Jull and colleagues36 have demonstrated that a combined program of cervical spine manipulative therapy (thrust and nonthrust) and exercise can reduce the symptoms of cervicogenic headache. However, the risk of adverse events following cervical spine thrust manipulation is higher than for other re- gions of the spine,6 and the role of testing the integrity of the cervical spine for potential contraindications to manual therapy is not clearly defined.12,46,69 SUPPLEMENTAL VIDEO ONLINE TIJK:O:;I?=D0 Resident’s case problem. T879A=HEKD:0 The role of premanipulative testing of the cervical spine is an area of controversy, and there are very few data to inform and guide practitioners on the use of ligamentous stability tests when assessing the upper cervical spine. T:?7=DEI?I0 A 23-year-old female was referred to physical therapy by a neurologist for the management of intractable headaches of possible musculoskeletal origin. Her Neck Disability Index score was 54% and she rated her headache pain as varying from 3/10 to 9/10 on a numerical pain rating scale. She reported a 2-year history of intermittent lower extremity paresthesias without a known mechanism or current symptoms. She was treated in physical therapy for 11 visits with improvements in cervical range of motion, strength, and intensity of her headaches, but noted no change in the frequency of headaches. She was subsequently referred to the primary author for a second opinion and potential manual therapy interventions. Initial neurological screening examination for upper and lower motor neuron lesions was unremarkable. Assessment of the transverse ligament, using the anterior shear test in supine, brought on paresthesias in both feet and her toes. The paresthesias continued after the cessation of the test. The Cervical instability has been reported in patients with conditions commonly treated in physical therapy.13,17,36,41,62,80,89 The role of premanipulative testing of the Sharp-Purser test performed in sitting, immediately after the transverse ligament test, abolished the paresthesias. She was then referred back to her primary care physician for further evaluation. Subsequent radiographs and magnetic resonance imaging revealed that the patient had a C2-C3 Klippel-Feil congenital fusion and os odontoideum. The patient was examined by a neurosurgeon who concluded that she was not a surgical candidate. Her neurological symptoms completely resolved, but she continued to have headaches. T:?I9KII?ED0 Os odontoideum is a clinically important condition, given that the mobile dens may render the transverse ligament incompetent, leading to atlantoaxial instability. Both the role and sequencing of upper cervical ligamentous testing is controversial. The results of this case report suggest that physical therapists should be cognizant of this condition and consider screening the upper cervical ligaments prior to manual or mechanical interventions to this region. TB;L;BE<;L?:;D9;0 Diagnosis, level 4. J Orthop Sports Phys Ther 2008;38(8):465-475. doi:10.2519/jospt.2008.2747 TA;OMEH:I0 Klippel-Feil syndrome, manual therapy, neck, transverse ligament, upper cervical instability 1 Assistant Professor, University of Colorado at Denver and Health Sciences Center, School of Medicine, Department of Physical Therapy, Denver, CO; Fellow in the Regis University Manual Therapy Fellowship, Regis University, Department of Physical Therapy, Denver, CO. 2 Physical Therapist, Wardenburg Health Center at the University of Colorado, Boulder, CO. 3 Associate Professor and Manual Therapy Fellowship Coordinator, Regis University, School of Physical Therapy, Denver, CO. The individual in this case gave consent to use her medical information and images as part of this publication. Address correspondence to Dr Paul Mintken, Education 2 South, Bldg L28, Room 3128, 13121 E 17th Avenue, PO Box 6508, Aurora, CO 80045. E-mail: paul.mintken@uchsc.edu journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 465 [ RESIDENT ’ S CASE PROBLEM <?=KH;'$Schematic illustration showing ligaments of the upper cervical spine seen from the posterior view. Modified with permission from Barrow Neurological Institute, copyright 2008. cervical spine is an area of controversy, particularly in the area of vertebrobasilar insufficiency.12,14,26,27,42-44,52,54,67,80 Additionally, there are very little data supporting or refuting the role of screening the ligaments of the upper cervical spine to determine the presence or absence of instability.11,49,50,63,80,89 Cook et al13 stated that clinical cervical spine instability is difficult to diagnose, involves subtle clinical features, and few valid, reliable clinical tests exist to aid in differential diagnosis. Numerous clinical tests for cervical spine instability are currently in use in clinical practice, and most are intended to assess the integrity of the alar and transverse ligaments (<?=KH;'). Most of these tests have not been validated in patients with neck pain and headaches and the level of reliability of the tests varies.11,13,58,60 Uitvlugt and Indenbaum89 reported that the Sharp-Purser test was moderately sensitive (88%) and highly specific (96%) in detecting atlantoaxial instability in individuals with rheumatoid arthritis. Cattryse et al11 reported moderate to substantial interobserver reliability (L = 0.50-1.0) for the upper cervical flexion test for 3 of 4 investigators and poor to substantial interobserver reliability (L = 0.0-0.67) with the lateral displacement test and the Sharp-Purser test when performed on 11 children with Down’s syndrome. The transverse ligament test (also known as the anterior shear test) is commonly taught in professional level physical therapist programs; however, its validity has not been established.63 Meadows50 argues that the above tests take little time and should be done on every patient with neck pain. However, Swinkels and Oostendorp,80 who have identified 5 upper cervical instability tests, including a version of the anterior shear test, argue that it is essential to determine the reliability and validity of these tests to determine their clinical usefulness. Os odontoideum and Klippel-Feil ] syndrome (KFS) can cause cervical instability. Os odontoideum is described as a condition in which the dens is separated from the body of the axis.16 The incidence of os odontoideum is unknown; but Sankar et al75 reported that 3.1% of 519 patients with abnormal cervical spine radiographs had os odontoideum. KFS is a congenital disorder characterized by abnormal fusion of some of the cervical vertebrae and the incidence has been reported to range from 1 in 100 to 1 in 42 000 births.22,23,32 KFS has been associated with C1-C2 hypermobility and instability,7,66,71,76 as well as numerous other organ system abnormalities.85 It is important for therapists to screen patients for potential cervical instability arising from traumatic, systemic, or congenital conditions. The purpose of this case report is to describe the clinical examination, evaluation, and decision-making process involved in the management of an individual presenting with chronic headaches and signs and symptoms suggestive of upper cervical instability from an underlying undiagnosed condition. 97I;:;I9H?FJ?ED FWj_[dj>_ijeho A 23-year-old female was referred to physical therapy with intractable headaches that were deemed to be of possible musculoskeletal origin. During the history intake, the patient stated that she began having daily severe right-sided headaches in October 2006 which she rated as 10/10 on a numerical pain rating scale (NPRS), where 0 represents no pain and 10 represents the worst pain imaginable.31 Within a month, she saw her primary care physician, who treated her initially with Imitrex. This offered some symptomatic relief but did not change the frequency of her incapacitating headaches. A week after seeing her primary care physician, she was referred to a neurologist, who diagnosed her with classic migraines with aura, with concomitant musculoskeletal headaches.2 The diagnosis of concomitant musculoskeletal 466 | august 2008 | volume 38 | number 8 | journal of orthopaedic & sports physical therapy headaches was based on the presence of a unilateral headache with paracervical muscle hypertonicity and reproduction of familiar headache symptoms with cervical muscle palpation.78 Amiri et al3 reported that it is common for patients to present with 2 or more concurrent headache types but that, unfortunately, isolated features of physical impairment were not helpful in differentiating cervicogenic headaches. The neurologist prescribed a low dose of Trazadone along with Midrin. These medications had no effect on her symptoms. No musculoskeletal imaging was done at that time. The neurologist referred the patient to physical therapy, with the intent to seek magnetic resonance imaging (MRI) if the symptoms did not improve. At her initial physical therapy examination on November 14th, 2006, her Neck Disability Index score was 54%, which indicated severe disability.90 The patient stated that her daily headache symptoms ranged from 3/10 (best) to 9/10 (worst) on the NPRS. Her headaches were typically worse at the end of the day and aggravated by stress and neck movements, particularly extension. On her intake form she reported a 2-year history of intermittent lower extremity paresthesias. Upon further questioning she described tingling sensations in her toes bilaterally as well as the left foot through the ball and dorsum of the foot. She had a recollection of the occurrence of these symptoms but could not recall any provoking incidents or other associated symptoms and denied current symptoms. During her initial physical therapy examination, further questioning about her headaches revealed a history of migraines that began 2 years before, with infrequent occurrence and lasting for up to 2 days. She had been headache free for 9 months prior to the most recent onset in October 2006 and stated that her typical symptoms would start with a visual aura of colors and swirls lasting up to 2 hours. This was followed by a headache that would begin in a focal point of pain at the base of the skull/upper neck on the right, which she characterized as “feeling like a tent stake is being pounded into my head.” These symptoms would dissipate somewhat with time to a generalized right-sided headache, with a sensation of intense pressure that was made worse with stress and movement of the neck. By the time she saw the neurologist in November 2006, she was having daily intractable, incapacitating headaches that would peak in the afternoon. The initial physical therapy examination included screening for upper quarter (cervical and thoracic spine, shoulder, elbow, wrist, and hand) range of motion (ROM), myotomal strength, and deep tendon reflexes deficits.50 The results of the screen were considered unremarkable. Further examination revealed moderate limitations in cervical spine extension and side bending, increased tone in the upper trapezius and suboccipital muscles bilaterally, tight pectoralis minors, weak deep neck flexors and scapular retractors, and a stiff upper thoracic spine. Sensory testing and cranial nerve testing were not performed but were reported as normal in the examination performed 2 weeks earlier by the neurologist. She was treated in physical therapy for 11 visits over a period of 2 months. Treatments included gentle soft tissue massage to the upper trapezius and suboccipital musculature, instruction in a home exercise program to address postural strengthening of scapular retractors and deep neck flexors, and stretches for the upper trapezius and anterior chest wall musculature.48 She made clinical improvements in strength, cervical ROM, and the intensity of her headaches, as her pain decreased to 1/10 to 2/10, but she continued to have daily headaches. She was then (end of January 2007) referred to the primary author for a second opinion and possible manual therapy interventions. CWdkWbF^oi_YWbJ^[hWf_ijÊi;nWc_dWj_ed The history and the previous physical therapist’s notes were reviewed. Additional questioning revealed that the headaches were daily and constant, she was unable to find any interventions, medication or otherwise, that gave her relief. Her Neck Disability Index that day was 44%, indicating moderate disability. 90 She stated that her headaches seemed to be related to neck movements, particularly looking up, and she reported feeling tired all the time. When questioned regarding the symptoms of fatigue, she stated that she had always had trouble sleeping, and this was exacerbated by her constant headaches. She did not relate any other medical conditions that might be contributing to feeling tired, and stated that her general health was good except for a history of a ruptured ovarian cyst. A neurological screening examination, which included deep tendon reflexes of the upper and lower extremities, a myotomal screen, and tests for upper motor neuron signs (Hoffman’s sign), was unremarkable.50 As she was not reporting any recent or current sensory disturbances, a sensory examination was not performed. On observation, the patient presented with decreased kyphosis in the mid thoracic spine, increased kyphosis at the cervicothoracic junction, and forward shoulders.39 No frontal plane postural deviations were noted. She rated her headache at the time of the evaluation at 2/10. Cervical ROM was measured using a single inclinometer.30 Intraclass correlation coefficients (ICCs) for interexaminer and intraexaminer reliability of measuring cervical ROM with a single inclinometer has been reported to be 0.84 and 0.94 for flexion and extension and 0.82 and 0.92 for side bending, respectively.30 The patient was asked to nod her head slowly and bring her chin to her chest. Cervical flexion measured 50° and did not reproduce any symptoms. Gentle overpressure in end range flexion did not cause any change in her symptoms. Cervical extension measured 40° and increased her headache to a 4/10. When her symptoms increased with active ROM testing, overpressure was not introduced. Upon returning to an upright posture, the headache returned to the baseline 2/10, suggesting minimal irritability.47 Left side journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 467 [ TABLE J[ij RESIDENT ’ S CASE PROBLEM ] Description of Upper Cervical Ligamentous Testing 50,63 :[iYh_fj_ed H[ikbj Alar ligament stress test (<?=KH;( and EDB?D;L?:;E) Patient is supine and the therapist grips and stabilizes the No excessive motion was noted and the end feel spinous process of the axis. The head and atlas are then was capsular side bent around the coronal axis of the atlantoaxial joint. Ipsilateral rotation of the axis is prevented by the stabilization of the axis. The end feel and the amount of motion are assessed. If the alar ligament is intact, little to no side bending can occur and the end feel should be capsular. The test is then repeated with rotation of the head and atlas on the axis and the end feel is assessed Transverse ligament test or anterior shear test (<?=KH; 3 and EDB?D; L?:;E) Patient supine with the head supported by a pillow in the Positive for bilateral lower neutral position. The therapist supports the occiput in extremity paresthesias the palms of the hands and the third, fourth, and fifth fingers while the 2 index fingers are placed in the space between the occiput and the C2 spinous process, thus overlying the neural arch of the atlas. The head and C1 are then lifted (sheared) anteriorly together, while the head is maintained in its neutral position and gravity fixes the rest of the neck. The patient is instructed to report any symptoms other than local pain and soreness. The sensation of a lump in the throat or the presence of cardinal signs or symptoms indicates a positive test50,63 Sharp-Purser test (<?=KH;* and EDB?D;L?:;E) Relieved lower extremThe palm of one hand is placed on the patient’s forehead ity paresthesias. No and the spinous process of the axis is then gently fixed excessive motion was by a pinch grip of the thumb and fingertip pads of the noted and no sense of other hand. The head and neck are then gently flexed. sliding or “clunking” Through palmar pressure on the forehead, the occiput was noted and atlas are translated posteriorly. The unique feature of this test is that the stress component is intended to relieve the symptoms rather than aggravate them. It has also been reported that a clunk may be noted as the atlas reduces on the axis bending was 50° and right side bending 42°, and symptoms did not increase at end range with overpressure. Cervical rotation was measured using a goniometer. Youdas et al95 reported that goniometric measurements of active ROM of the cervical spine made by the same physical therapist had ICCs greater than 0.80. Rotation to the right measured 82°, and reproduced her headache at a 4/10 on the NPRS. Her headache returned to 2/10 when she returned her head to midline. Left rotation was 90° and symptoms did not change with gentle overpressure. The examination then focused on the upper cervical spine, as it has been reported that the presence of painful upper cervical joint dysfunction is a diagnostic criterion for cervicogenic headache.4,34,37,78 The occipitoatlantal joints were assessed in supine, as described by Greenman.24 The head/occiput is grasped by the physical therapist and passive upper cervical flexion and extension, with the axis of motion through the external auditory meatus, was performed. Motion is then assessed by introducing side bending/ translation, while maintaining end range flexion or extension. As the upper cervical spine was flexed, the patient reported moderate paresthesias into her toes bilaterally. Upon release of upper cervical flexion, the symptoms disappeared. These symptoms have been described as cardinal symptoms of upper cervical instability11 and cervical cord compession.63 Pettman63 defined “cardinal symptoms” as any of the following signs or symptoms <?=KH;($Alar ligament stress testing. Spinous process of the axis is stabilized while the head and the atlas are side bent or rotated to assess for excessive movement. (A) Start position; (B) sidebending stress; (C) rotation stress. that are reproduced by active or passive movements of the head or neck: an overt loss of balance (drop attacks), facial or lip paresthesias, bilateral or quadrilateral limb paresthesias, or nystagmus. Upper cervical instability was suspected, so craniovertebral ligamentous stress tests were performed (TABLE 1). As the patient was already supine and did not have any symptoms, the alar ligament stress tests were performed as described by Pettman (<?=KH; ( and EDB?D; L?:;E).63 A normal capsular end feel was appreciated with no excessive movement, and these tests were not painful and did not reproduce any paresthesias. As the patient continued to be symptom free, the transverse 468 | august 2008 | volume 38 | number 8 | journal of orthopaedic & sports physical therapy <?=KH;)$Transverse ligament or anterior shear test. The therapist supports the occiput, while the 2 index fingers are placed in the space between the occiput and the C2 spinous process. The head and C1 are then moved anteriorly as a unit on the cervical spine. (A) Start position; (B) end position. <?=KH;+$Lateral radiograph. Arrow points to Klippel-Feil fusion at C2-C3. The parallel lines outline the anterior atlantodental interval (AADI). No increased motion is noted in the AADI in neutral, flexion, or extension. The measurement landmarks for the AADI are the posterior surface of the anterior tubercle of C1 and the anterior surface of the odontoid.95 <?=KH;*$Sharp-Purser test. The palm of one hand is placed on the patient’s forehead while the spinous process of the axis is held by a pinch grip of the opposite hand. Then the head and neck are the gently flexed. Through palmar pressure on the forehead, the occiput and atlas are translated posteriorly. ligament was assessed using the anterior shear test as described by Meadows (<?=KH;) and EDB?D;L?:;E)50: “The patient lies supine with the head supported by a pillow in the neutral position. The therapist supports the occiput in the palms of the hands and the third, fourth, and fifth fingers, while the 2 index fingers are placed in the space between the occiput and the C2 spinous process, thus overlying the neural arch of the atlas (C1). The head and C1 are then translated anteriorly as a unit with the head maintained in its neutral position while gravity maintains the remainder of the cervical spine/neck against the table. The patient is instructed to report any symptoms other than local pain and soreness.” In this case, the patient reported the return of moderate paresthesias into her toes, which continued after the cessation of the test. She was then carefully assisted to a sitting position and the Sharp-Purser test (<?=KH;* and EDB?D; L?:;E), as described by Pettman,63 was performed, which abolished the paresthesias. No “clunk” was noted with the test and there was no perceived excessive motion. Upon re- lease of the force applied during the test the patient had a return of paresthesia in 1 lower extremity that she described as very mild and similar to the symptoms she had described during the intake history. Pettman63 stated that the reduction of symptoms with the Sharp-Purser test is suggestive of upper cervical instability. An assessment of the deep tendon reflexes of the lower extremities was repeated and deemed normal. The patient was scheduled to see her primary care physician in the same building approximately 90 minutes after her physical therapy appointment that day, and a message was left for her physician explaining the concerns of upper cervical instability. She saw her physician later that day but no information regarding journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 469 [ RESIDENT ’ S CASE PROBLEM ] physical examination was recorded in the physician’s note. :_W]deij_Y?cW]_d] The primary care physician referred the patient for diagnostic imaging, including flexion/extension radiographs of the cervical spine. Radiographs revealed that the patient had a type I C2-C3 KlippelFeil congenital fusion74 (<?=KH;I+#.). Samartzis et al74 define a type I Klippel-Feil as a single congenitally fused cervical segment. During the 6 days following the physical therapy examination and the physician’s visit, the patient stated that her toes tingled while lying in supine or when she brought her head into cervical flexion. She also reported intermittent dizziness, ataxia, and 2 episodes of falling down. Based on the results of the radiographs and the neurological symptoms, the patient underwent MRI of the cervical spine 6 days after the physical therapy examination. An os odontoideum was identified on a sagittal image of the MRI (<?=KH;I/ and 10). Os odontoideum describes a condition in which a portion of the odontoid process is separated from the body of the axis,51 potentially rendering the transverse ligament unable to stabilize the atlas on the axis.18,73 The imaging was subsequently interpreted by 3 radiologists, who all concurred that the imaging most likely represented an os odontoideum. The anterior atlantodental interval (AADI)94 was deemed to be normal on the radiographs (<?=KH;I+#-), but this could be a result of muscle guarding. On the MRI (<?=KH;I / and 10), the dens fragment appears to have sclerotic margins, suggesting a longstanding entity. This is supported by the lack of edema on the sagittal T2 MRI (<?=KH;'&). One radiologist commented that the os odontoideum was larger and less irregular than a typical case, and that it involved a larger amount of the dens than is typically seen. This could explain the instability under stress, as the transverse ligament and alar ligaments may stabilize the os fragment and pull it anteriorly with C1 during the anterior shear test, with re- <?=KH;,$Flexion radiograph. Arrow points to Klippel-Feil fusion at C2-C3. The parallel lines outline the anterior atlantodental interval (AADI). No atlantoaxial subluxation was noted. sultant motion occurring between the os fragment and the C2 vertebra. This could be confirmed with axial or coronal MRI through the foramen magnum (which were not performed in this case). Also noted was a synchondrosis of the base of the dens with the body of C2 and partial fusion of C2 with the underlying C3. No cord signal changes were noted, but an area of narrowing was identified that was probably long-standing (<?=KH;'&). The patient was referred to a neurosurgeon 9 days after the physical therapy examination, who completed a thorough neurological examination, including sensation, strength testing, cranial nerve examination, and testing for both upper and lower motor neuron problems. The examination was deemed unremarkable. Cervical spine ROM was not assessed. The neurosurgeon told the patient that both os odontoideum and KPS are congenital conditions that do not warrant surgical intervention in the absence of progressing neurological symptoms. Her symptoms of lower extremity paresthesias had resolved within 7 days, and she was no longer reporting dizziness, ataxia, or falling down. She continued to have daily incapacitating headaches and she subsequently withdrew from the univer- <?=KH;-$Extension radiograph. Arrow points to Klippel-Feil fusion at C2-C3. The parallel lines outline the anterior atlantodental interval (AADI). No atlantoaxial subluxation was noted. <?=KH;.$Open-mouth view. No abnormalities were noted. sity and no longer had health insurance. The patient was contacted 6 months later, and she continued to have headaches but did not report having had any neurological signs or symptoms during that time. :?I9KII?ED T he prevalence of upper cervical instability is unknown, as it may be present in asymptomatic individuals.28 KFS, characterized by congenital fusion of 2 or more cervical vertebrae, is present in up to 1% of the population and has been associated with craniocervical abnormalities that can lead to spontaneous and progressive neurological sequelae after relatively minor neck trauma.23,79 470 | august 2008 | volume 38 | number 8 | journal of orthopaedic & sports physical therapy <?=KH;/$Sagittal T1-weighted magnetic resonance image. Arrows point to area of os odontoideum and KlippelFeil fusion of C2-C3. KFS has also been associated with genitourinary tract abnormalities (65%),53 scoliosis (60%),82,84,93 facial asymmetries and torticollis (45%),84 hearing loss (38%),85 Sprengel’s deformity (36%),84 spinal cord abnormalities (syringomyelia 15%),88 spina bifida,59 cervical stenosis,68 cleft palate,85 congenital upper extremity abnormalities,83 cervical ribs,87 and cardiovascular anomalies.61 The prevalence of os odontoideum is unknown.86 Os odontoideum was initially thought to be due to a congenital failure of fusion of the dens to the remainder of the axis.29 Sankar et al75 reported that 2 separate etiologies may explain os odontoideum: posttraumatic and congenital. Verska et al91 reported on a set of identical twins in which 1 twin presented with an os odontoideum after trauma and the other twin had a normal cervical spine and no history of trauma. Crockard and Stevens15 state that os odontoideum may be the product of excessive movement at the time of ossification of the cartilaginous dens, and that the presentation is similar to an unfused Type II odontoid fracture. In this case, the Klippel-Feil fusion at C2-C3 may have lead to excessive motion at C1-C2 resulting in an os odontoideum. Several authors have reported that os odontoideum often accompanies Klippel-Feil fusions, particularly when present at C2-C3,7,55,76 and Morgan et al55 suggested there may be a pattern of autosomal dominant familial inheritance for this combination. Os odontoideum is clinically important because an insufficient dens may render the transverse ligament incapable of restraining the atlas on the axis.18,73 With increased motion, upper cervical cord or vertebral artery impingement may occur.33,40,51,72,77,81,92 Michaels et al51 reported on a 35-year-old taxi driver who was involved in a lowspeed head-on motor vehicle collision who died 4 days later. Autopsy revealed an os odontoideum that had compressed the spinal cord on flexion of the head. Sherk and Dawoud76 report a case of an individual with os odontoideum with KFS who developed quadriplegia and ultimately died after falling and hitting his head. Although Galli et al21 reported on a patient with os odontoideum presenting with cervical vertigo, the role of os odontoideum and upper cervical instability in headaches and other cervical complaints is unclear. Upper cervical spine instability can be a benign condition that goes unnoticed for years. Nagashima et al57 report the case of a 42-year-old woman presenting with KFS and severe hypermobility of the upper cervical spine that showed no signs of neurological involvement. Morgan et al55 reported on an asymptomatic 16-year-old boy with familial os odontoideum and a Klippel-Feil fusion of C2-C3. While upper cervical instability can and does exist in asymptomatic individuals, it journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 471 [ RESIDENT ’ S CASE PROBLEM <?=KH;'&$Sagittal T2-weighted magnetic resonance image. The left arrow points to the area of os odontoideum. The dens fragment appears to have sclerotic margins with no evidence of edema, indicating a long-standing entity. The black arrow points to a potential area of narrowing of the cervical spinal cord. can lead to serious neurological sequelae in others. Pizzutillo et al64 suggest that individuals with KFS with hypermobility of the upper cervical segment are at risk for neurologic sequelae. The role of screening the upper cervical spine is an area of controversy, particularly in regard to the vertebral artery.1,8,46,49,69,70 The role of craniocervical ligamentous testing in screening for cervical instability has received much less attention. Numerous clinical tests have been developed to assess the stability of the upper cervical spine.11,13,49,50,63,89 Un- fortunately, no consensus exists regarding which tests, if any, are appropriate, and there is no clear guidance on an appropriate sequence to testing the ligamentous structures of the upper cervical spine. In a study investigating the reliability of 3 commonly used tests for upper cervical instability in children with Down’s syndrome, the sequence of the testing was chosen at random.11 In retrospect, the sequencing of the upper cervical ligament testing in this case may not have been ideal. In our subsequent literature review, the author of 1 ] article described a “reasoned” approach to assessing upper cervical ligamentous stability. Aspinall5 suggests that if upper cervical instability is suspected, the Sharp-Purser test should be performed first before any of the other ligamentous tests. If, and only if, the Sharp-Purser is negative, Aspinall then suggests that, in the absence of neurological symptoms, a test that passively moves the atlas on the axis be used to assess for laxity of the transverse ligament. In this case, it would have potentially been safer to perform the Sharp-Purser first, which is considered a relocation or “alleviation” test, to assess for instability. The Sharp-Purser test is not without controversy, as Pettman63 stated that this test is intended to relieve neurological symptoms, while Meadows49 called the use of the Sharp-Purser in the presence of neurological symptoms an “exercise in futility and risk.” In this particular case, it is the authors’ opinion that the Sharp-Purser would have been negative if performed first, as the results of the test that was ultimately performed did not reveal excessive motion and the patient had no symptoms to be relieved prior to the application of the anterior shear test. The positive finding of the Sharp-Purser performed in this case was the relief of paresthesia, which was elicited by the initial application of the anterior shear test. Had the SharpPurser test been performed first, it would have been considered negative (no perception of instability or symptoms to be relieved), leading to the performance of the anterior shear test and likely the same results. While the sequencing of the examination was possibly less than optimal, it is the authors’ opinion that it required a provocation of the symptoms for the clinical exam to suggest the presence of upper cervical instability in this patient. The anterior shear test should be viewed as a provocative test, one in which cardinal signs may be elicited in an unstable upper cervical spine. While this is clearly an area that requires more research, the findings in this case report combined with previously published expert opinions 472 | august 2008 | volume 38 | number 8 | journal of orthopaedic & sports physical therapy suggest that, in the presence of cardinal signs or symptoms, the Sharp-Purser test, which is aimed at alleviating symptoms, should be performed first. In the absence of symptoms, tests designed to alleviate symptoms should still be performed first in an attempt to identify excessive mobility. This should be followed by provocative tests only if no symptoms were produced and no excessive mobility is perceived. Provocative tests are not recommended in the presence of symptoms, suggesting neurological compromise. It could also be argued that the patient should have been sent back to the physician following the onset of bilateral lower extremity paresthesias with passive upper cervical flexion, as this motion has been described as a test to identify upper cervical instability.11 Indeed, the primary author had previously referred patients back to physicians based on the suspicion of upper cervical instability based on the results of the clinical examination, only to be accused of what Pettman63 refers to as “craniovertebral hysteria.” The timing, necessity, and threshold for medical referral is unclear. In a previously published case report involving suspected upper cervical instability (no imaging was ever taken), a Sharp-Purser test was performed in which a “large amount of movement was appreciated” and the patient had a reduction in her right-sided face, ear, neck, and shoulder pain.45 Despite these findings, and a history of dizziness and bilateral blurred vision, the patient was not referred back to the physician for further examination. The patient was diagnosed with clinical instability of the cervical spine and subsequently treated successfully with manual therapy. One could argue that this patient should have been referred for further diagnostic workup. Despite the relative rarity of os odontoideum and the controversy surrounding clinical testing of upper cervical instability, failure of a physical therapist to recognize this condition could result in severe patient injury when manual physical therapy procedures or end range mobility exercises are performed. We have described a case where the physical therapist examination of the upper cervical spine was highly suggestive of a potentially serious condition that required further medical referral. Even with limited information on the diagnostic utility of the physical examination tests to determine the presence or absence of cervical spine instability, and the sequence in which they should be performed, it is our opinion that in this patient the results of these tests represented an absolute contraindication to any further examination or treatment to the cervical region until further diagnostic workup was performed. *$ +$ ,$ -$ .$ 9ED9BKI?ED /$ E s odontoideum is a clinically important condition given that the mobile dens may render the transverse ligament incompetent, leading to atlantoaxial instability. This can have potentially devastating consequences to the spinal cord or vertebral arteries.33,40,51,72,76, 77,81,92 The results of this case report suggest that physical therapists should be cognizant of this condition and consider screening the upper cervical spine prior to manual or mechanical interventions to this region. At this time no consensus exists regarding which tests, if any, are appropriate, and there is no clear guidance on an appropriate sequence to testing the ligamentous structures of the upper cervical spine. Clearly, further research and dialogue are needed in this area. T 10. 11. 12. 13. '*$ '+$ H;<;H;D9;I 1. AJP Forum: pre-manipulative testing of the cervical spine. Aust J Physiother. 2001;47:163-167. 2. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia. 1988;8 Suppl 7:1-96. 3. Amiri M, Jull G, Bullock-Saxton J, Darnell R, Lander C. Cervical musculoskeletal impairment in frequent intermittent headache. Part 2: subjects with concurrent headache types. ',$ '-$ '.$ '/$ Cephalalgia. 2007;27:891-898. http://dx.doi. org/10.1111/j.1468-2982.2007.01346.x Antonaci F, Bono G, Mauri M, Drottning M, Buscone S. Concepts leading to the definition of the term cervicogenic headache: a historical overview. J Headache Pain. 2005;6:462-466. http://dx.doi.org/10.1007/s10194-005-0250-6 Aspinall W. Clinical testing for the craniovertebral hypermobility syndrome. J Orthop Sports Phys Ther. 1990;12:47-54. Assendelft WJ, Bouter LM, Knipschild PG. Complications of spinal manipulation: a comprehensive review of the literature. J Fam Pract. 1996;42:475-480. Baba H, Maezawa Y, Furusawa N, Chen Q, Imura S, Tomita K. The cervical spine in the KlippelFeil syndrome. A report of 57 cases. Int Orthop. 1995;19:204-208. Barker S, Kesson M, Ashmore J, Turner G, Conway J, Stevens D. Professional issue. Guidance for pre-manipulative testing of the cervical spine. Man Ther. 2000;5:37-40. http://dx.doi. org/10.1054/math.1999.0230 Beeton K, Jull G. Effectiveness of manipulative physiotherapy in the management of cervicogenic headache: a single case study. Physiother. 1994;80:417-423. Bronfort G, Nilsson N, Haas M, et al. Noninvasive physical treatments for chronic/ recurrent headache. Cochrane Database Syst Rev. 2004;CD001878. http://dx.doi. org/10.1002/14651858.CD001878.pub2 Cattrysse E, Swinkels RA, Oostendorp RA, Duquet W. Upper cervical instability: are clinical tests reliable? Man Ther. 1997;2:91-97. http:// dx.doi.org/10.1054/math.1997.0290 Childs JD, Flynn TW, Fritz JM, et al. Screening for vertebrobasilar insufficiency in patients with neck pain: manual therapy decision-making in the presence of uncertainty. J Orthop Sports Phys Ther. 2005;35:300-306. http://dx.doi. org/10.2519/jospt.2005.1312 Cook C, Brismee JM, Fleming R, Sizer PS, Jr. Identifiers suggestive of clinical cervical spine instability: a Delphi study of physical therapists. Phys Ther. 2005;85:895-906. Cote P. Rotation: a valid premanipulative dizziness test? Does it predict safe manipulation? J Manipulative Physiol Ther. 1994;17:413-414. Crockard HA, Stevens JM. Craniovertebral junction anomalies in inherited disorders: part of the syndrome or caused by the disorder? Eur J Pediatr. 1995;154:504-512. Dai L, Yuan W, Ni B, Jia L. Os odontoideum: etiology, diagnosis, and management. Surg Neurol. 2000;53:106-108; discussion 108-109. Dobbs A. Manual therapy assessment of cervical instability. Orthop Phys Ther Clin N Am. 2001;10:431-454. Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6:452-461. http://dx.doi.org/10.1002/ jor.1100060317 Edeling J. Manual therapy rounds. Cervicogenic, journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 473 [ 20. 21. 22. 23. (*$ (+$ (,$ (-$ (.$ (/$ 30. 31. 32. 33. )*$ )+$ ),$ RESIDENT ’ S CASE PROBLEM tension-type headache with migraine: a case study. J Man Manip Ther. 1997;5:33-38. Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page JC. Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headache. J Orthop Sports Phys Ther. 2006;36:160-169. http://dx.doi.org/10.2519/ jospt.2006.2126 Galli J, Tartaglione T, Calo L, Ottaviani F. Os odontoideum in a patient with cervical vertigo: a case report. Am J Otolaryngol. 2001;22:371-373. http://dx.doi.org/10.1053/ajot.2001.26503 Gjorup PA, Gjorup L. Klippel-Feil’s Syndrome. Dan Med Bull. 1964;11:50-53. Gluck GS, Mawn SV. The Klippel-Feil syndrome: implications for Naval service. Mil Med. 1992;157:318-322. Greenman PE. Principles of Manual Medicine. 2nd ed. Baltimore, MD: Williams & Wilkins; 1996. Hanten WP, Olson SL, Lindsay WA, Lounsberry KA, Stewart JK. The effect of manual therapy and a home exercise program on cervicogenic headaches: a case report. J Man Manip Ther. 2005;13:35-43. Haynes MJ. Doppler studies comparing the effects of cervical rotation and lateral flexion on vertebral artery blood flow. J Manipulative Physiol Ther. 1996;19:378-384. Haynes MJ, Cala LA, Melsom A, Mastaglia FL, Milne N, McGeachie JK. Vertebral arteries and cervical rotation: modeling and magnetic resonance angiography studies. J Manipulative Physiol Ther. 2002;25:370-383. Henderson S, Henderson D. Os odontoideum with associated multidirectional atlantoaxial instability: imaging and clinical considerations. JCCA J Can Chiropr Assoc. 2006;50:111-117. Hensinger RN, Fielding JW, Hawkins RJ. Congenital anomalies of the odontoid process. Orthop Clin North Am. 1978;9:901-912. Hole DE, Cook JM, Bolton JE. Reliability and concurrent validity of two instruments for measuring cervical range of motion: effects of age and gender. Man Ther. 1995;1:36-42. http:// dx.doi.org/10.1054/math.1995.0248 Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117-126. Juberg RC, Gershanik JJ. Cervical vertebral fusion (Klippel-Feil) syndrome with consanguineous parents. J Med Genet. 1976;13:246-249. Juhl M, Seerup KK. Os odontoideum. A cause of atlanto-axial instability. Acta Orthop Scand. 1983;54:113-118. Jull G. Characterization of cervicogenic headache. Phys Ther Rev. 1998;3:95-105. Jull G. Management of cervical headache. Man Ther. 1997;2:182-190. http://dx.doi.org/10.1054/ math.1997.0298 Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835-1843; discussion 1843. )-$ Jull G, Zito G, Trott P, Potter H, Shirley D. Interexaminer reliability to detect painful upper cervical joint dysfunction. Aust J Physiother. 1997;43:125-129. ).$ Jull GA, Stanton WR. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-108. http://dx.doi. org/10.1111/j.1468-2982.2004.00811.x )/$ Kendall FP, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore, MD: Williams & Wilkins; 1993. *&$ Kikuchi K, Nakagawa H, Watanabe K, Kowada M. Bilateral vertebral artery occlusion secondary to atlantoaxial dislocation with os odontoideum: implication for prophylactic cervical stabilization by fusion--case report. Neurol Med Chir (Tokyo). 1993;33:769-773. *'$ Kristjansson E, Dall’Alba P, Jull G. A study of five cervicocephalic relocation tests in three different subject groups. Clin Rehabil. 2003;17:768774. *($ Licht PB, Christensen HW, Hoilund-Carlsen PF. Carotid artery blood flow during premanipulative testing. J Manipulative Physiol Ther. 2002;25:568-572. http://dx.doi.org/10.1067/ mmt.2002.128367 *)$ Licht PB, Christensen HW, Hoilund-Carlsen PF. Is there a role for premanipulative testing before cervical manipulation? J Manipulative Physiol Ther. 2000;23:175-179. **$ Licht PB, Christensen HW, Svendensen P, Hoilund-Carlsen PF. Vertebral artery flow and cervical manipulation: an experimental study. J Manipulative Physiol Ther. 1999;22:431-435. *+$ Lincoln J. Case report. Clinical instability of the upper cervical spine. Man Ther. 2000;5:41-46. http://dx.doi.org/10.1054/math.1999.0219 *,$ Magarey ME, Rebbeck T, Coughlan B, Grimmer K, Rivett DA, Refshauge K. Pre-manipulative testing of the cervical spine review, revision and new clinical guidelines. Man Ther. 2004;9:95-108. http://dx.doi.org/10.1016/j. math.2003.12.002 *-$ Maitland G. Vertebral Manipulation. 5th ed. Sydney, New South Wales, Australia: Butterworths; 1986. *.$ McDonnell MK, Sahrmann SA, Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2005;35:3-15. http://dx.doi.org/10.2519/ jospt.2005.1441 */$ Meadows J. Manual therapy rounds. The SharpPurser test: a useful clinical tool or an exercise in futility and risk? J Man Manip Ther. 1998;6:97100. +&$ Meadows J. Orthopedic Differential Diagnosis in Physical Therapy: A Case Study Approach. New York, NY: McGraw-Hill; 1999. +'$ Michaels L, Prevost MJ, Crang DF. Pathological changes in a case of os odontoideum (separate odontoid process). J Bone Joint Surg Am. 1969;51:965-972. ] +($ Mitchell J, Keene D, Dyson C, Harvey L, Pruvey C, Phillips R. Is cervical spine rotation, as used in the standard vertebrobasilar insufficiency test, associated with a measureable change in intracranial vertebral artery blood flow? Man Ther. 2004;9:220-227. http://dx.doi. org/10.1016/j.math.2004.03.005 +)$ Moore WB, Matthews TJ, Rabinowitz R. Genitourinary anomalies associated with Klippel-Feil syndrome. J Bone Joint Surg Am. 1975;57:355357. +*$ Moran R, Mullany A. What is the clinical utility of the cervical extension rotation test as routinely applied in the premanipulative screening process? J Osteopath Med. 2003;6:24-29. ++$ Morgan MK, Onofrio BM, Bender CE. Familial os odontoideum. Case report. J Neurosurg. 1989;70:636-639. +,$ Mueller L. Cervicogenic Headache: A Diagnostic and Therapeutic Dilemma. Headache & Pain: Diagnostic Challenges, Current Therapy. 2003;14:29-37. +-$ Nagashima H, Morio Y, Teshima R. No neurological involvement for more than 40 years in Klippel-Feil syndrome with severe hypermobility of the upper cervical spine. Arch Orthop Trauma Surg. 2001;121:99-101. +.$ Olson K, Paris S, Spohr C, Gorniak G. Radiographic assessment and reliability study of the craniovertebral side bending test. J Man Manip Ther. 1998;6:87-96. +/$ Paksoy Y, M SE, Kalkan E. Klippel-Feil syndrome associated with persistent trigeminal artery. Spine. 2004;29:E193-196. ,&$ Panjabi MM, Nibu K, Cholewicki J. Whiplash injuries and the potential for mechanical instability. Eur Spine J. 1998;7:484-492. ,'$ Paul I, Badmanaban B, Campalani G. Patients with Klippel-Feil syndrome should have imaging of the subclavian artery and its branches prior to coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2007;6:403-404. http:// dx.doi.org/10.1510/icvts.2006.141994 ,($ Petersen SM. Articular and muscular impairments in cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2003;33:21-30; discussion 30-22. ,)$ Pettman E. Stress tests of the craniovertebral joints. In: Boyling J, Palastanga N, eds. Grieve’s Modern Manual Therapy: The Vertebral Column. Edinburgh, UK: Churchill Livingstone; 1994:529538. ,*$ Pizzutillo PD, Woods M, Nicholson L, MacEwen GD. Risk factors in Klippel-Feil syndrome. Spine. 1994;19:2110-2116. ,+$ Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population--a prevalence study. J Clin Epidemiol. 1991;44:1147-1157. ,,$ Rea GL, Mullin BB, Mervis LJ, Miller CL. Occipitocervical fixation in nontraumatic upper cervical spine instability. Surg Neurol. 1993;40:255-261. ,-$ Refshauge KM. Rotation: a valid premanipulative dizziness test? Does it predict safe manipula- 474 | august 2008 | volume 38 | number 8 | journal of orthopaedic & sports physical therapy tion? J Manipulative Physiol Ther. 1994;17:15-19. ,.$ Ritterbusch JF, McGinty LD, Spar J, Orrison WW. Magnetic resonance imaging for stenosis and subluxation in Klippel-Feil syndrome. Spine. 1991;16:S539-541. ,/$ Rivett DA. A valid pre-manipulative screening tool is needed. Aust J Physiother. 2001;47:166. -&$ Rivett DA, Thomas L, Bolton P. Pre-manipulative testing: where do we go from here? NZ J Physiother. 2005;33:78-83. -'$ Roach JW, Duncan D, Wenger DR, Maravilla A, Maravilla K. Atlanto-axial instability and spinal cord compression in children--diagnosis by computerized tomography. J Bone Joint Surg Am. 1984;66:708-714. -($ Ruiz Torres B, Zaldibar Barinaga B, Jarne Esparcia MA, Rios Gomez C. Lhermitte’s sign and paresthesia of the hands as an initial manifestation of os odontoideum at an advanced age [Spanish]. Rehabilitacion. 2004;38:30-32. -)$ Saldinger P, Dvorak J, Rahn BA, Perren SM. Histology of the alar and transverse ligaments. Spine. 1990;15:257-261. -*$ Samartzis DD, Herman J, Lubicky JP, Shen FH. Classification of congenitally fused cervical patterns in Klippel-Feil patients: epidemiology and role in the development of cervical spine-related symptoms. Spine. 2006;31:E798804. http://dx.doi.org/10.1097/01. brs.0000239222.36505.46 -+$ Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: the case for a multifactorial etiology. Spine. 2006;31:979-984. http://dx.doi.org/10.1097/01. brs.0000214935.70868.1c -,$ Sherk HH, Dawoud S. Congenital os odontoideum with Klippel-Feil anomaly and fatal atlanto-axial instability. Report of a case. Spine. 1981;6:42-45. --$ Shirasaki N, Okada K, Oka S, Hosono N, Yonenobu K, Ono K. Os odontoideum with posterior atlantoaxial instability. Spine. 1991;16:706-715. -.$ Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 1998;38:442-445. -/$ Smith BA, Griffin C. Klippel-Feil syndrome. Ann Emerg Med. 1992;21:876-879. .&$ Swinkels RA, Oostendorp RA. Upper cervical instability: fact or fiction? J Manipulative Physiol Ther. 1996;19:185-194. .'$ Takakuwa T, Hiroi S, Hasegawa H, Hurukawa K, Endo S, Shimamura T. Os odontoideum with vertebral artery occlusion. Spine. 1994;19:460-462. .($ Theiss SM, Smith MD, Winter RB. The long-term follow-up of patients with Klippel-Feil syndrome and congenital scoliosis. Spine. 1997;22:12191222. .)$ Thomsen M, Krober M, Schneider U, Carstens C. Congenital limb deficiences associated with Klippel-Feil syndrome: a survey of 57 subjects. Acta Orthop Scand. 2000;71:461-464. http:// dx.doi.org/10.1080/000164700317381135 .*$ Thomsen MN, Schneider U, Weber M, Johannisson R, Niethard FU. Scoliosis and congenital anomalies associated with Klippel-Feil syndrome types I-III. Spine. 1997;22:396-401. .+$ Tracy MR, Dormans JP, Kusumi K. Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin Orthop Relat Res. 2004;183-190. .,$ Tsou HK, Shen CC, Wang YC. Os odontoideum: a case report and review. Zhonghua Yi Xue Za Zhi (Taipei). 1998;61:741-747. .-$ Tubbs RS, Salter EG, Oakes WJ. Klippel-Feil anomaly with associated rudimentary cervical ribs in a human skeleton: case report and review of the literature. Folia Morphol (Warsz). 2006;65:92-94. ..$ Tubbs RS, Wellons JC, 3rd, Oakes WJ. Lumbar split cord malformation and Klippel-Feil syndrome. Pediatr Neurosurg. 2003;39:305-308. http://dx.doi.org/10.1159/000075258 ./$ Uitvlugt G, Indenbaum S. Clinical assessment of atlantoaxial instability using the Sharp-Purser test. Arthritis Rheum. 1988;31:918-922. /&$ Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409-415. /'$ Verska JM, Anderson PA. Os odontoideum. A case report of one identical twin. Spine. 1997;22:706-709. /($ Watanabe M, Toyama Y, Fujimura Y. Atlantoaxial instability in os odontoideum with myelopathy. Spine. 1996;21:1435-1439. /)$ Winter RB, Moe JH, Lonstein JE. The incidence of Klippel-Feil syndrome in patients with congenital scoliosis and kyphosis. Spine. 1984;9:363-366. /*$ Yamashita Y, Takahashi M, Sakamoto Y, Kojima R. Atlantoaxial subluxation. Radiography and magnetic resonance imaging correlated to myelopathy. Acta Radiol. 1989;30:135-140. /+$ Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion--comparison of three methods. Phys Ther. 1991;71:98-104; discussion 105-106. /,$ Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006;11:118-129. http://dx.doi.org/10.1016/j.math.2005.04.007 @ CEH;?D<EHC7J?ED WWW.JOSPT.ORG journal of orthopaedic & sports physical therapy | volume 38 | number 8 | august 2008 | 475