Nursing Documentation Changes and Reminders
advertisement

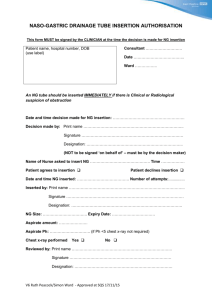
Nursing Documentation Changes and Reminders CCTC Nursing Documentation Change #1 Standard pH range changed to match new RRT documentation Change #2 Clarification for documentation standards for IV solutions. Change #2 Record each central and peripheral site: R IJ Introducer R IJ Double lumen Brown White Blue L forehand #18 peripheral Document legibly the following 3 pieces of information for each central and peripheral IV LUMEN: 1. Side of body 2. Insertion site 3. Type of catheter Change #2 Clarification for documentation standards for IV solutions. R IJ Introducer R IJ Triple lumen: Brown White Blue L forehand #18 peripheral 0.9% normal saline CVP 0.9% normal saline with 1,000 units heparin TPN Levophed in D5W Saline lock Record ONLY the SOLUTION and MEDICATION ADDED. This documentation identifies where solutions are running. If you change either the site, solution or medication, you must make a DAR entry to indicate the change. DO NOT record the rate or drug dose; this is already documented on the graphic record. If you document the rate or dose here, you must make a DAR note any time the rate or dose is changed. Change #3 Confirm each shift by a checkmark that the Admission and NEW Daily checklist for a pregnant patient have been activated and reviewed (obtain under “P” from Protocol Link of CCTC Website). Change #4 Confirm each shift by a checkmark that the NEW Postpartum Admission and Q shift checklists have been activated and reviewed (obtain under “P” from Protocol Link of CCTC Website). Reminder: Remember that this should be completed for any female patient of childbearing years, not just patients with obstetrical diagnosis. “No” should be confirmed by a pregnancy test or prior hysterectomy. If confirmed by reason other than pregnancy test, a * and DAR note should be completed with the initial documentation of “No”. This assessment is a reminder to rule out pregnancy in all females of child bearing years. Most females admitted via ED are screened prior to CCTC admission; check in Power Chart for results. For any appropriate patient who has not been screened, the need for screening should be raised during rounds, and the discussion/decision documented. Change #5 Confirm at the start of each shift that patients have a current blood transfusion sample on hand. If blood is no longer required, you can enter “not required” on the line for “Expires”. All patients require an initial sample and completion of transfusion consent process. Note that all patients at risk for bleeding or who may require any blood product should have a current sample. Important Blood Sampling Reminder: NEVER draw the confirmation sample at the same time as the initial Blood Transfusion Lab sample…this is a very serious POLICY VIOLATION that can lead to FATAL transfusion errors. The confirmation sample is required any time a patient does not have prior Blood Transfusion Lab history and must be obtained during a completely separate blood draw event. The confirmation sample is collected to “confirm” that the blood group identified during the initial sample is the same as during the confirmation sample. If either sample was drawn from the wrong patient, a mismatch will alert the lab. The error could be the original sample (which could have been drawn many years earlier) or the confirmation sample. Drawing both samples at the same time places patients at serious risk….mislabelling of blood transfusion samples DOES happen in CCTC! Fatal transfusion reactions can occur following administration of only a few mls of the wrong blood group. CCTC 24 Hour Flowsheet: Reminders and Future Updates Reminders Re Line Documentation on CCTC Flowsheet Be sure to enter the date of insertion. Be sure that the location of line insertion (e.g., CCTC, ED, OR, IR, other) is documented at the time of admission/line insertion on the line tracking record (the next revision of the flowsheet will eliminate the need for the line tracking record). The best time to obtain ACCURATE information about lines inserted pre-CCTC is from the admitting team. It should be assumed that lines inserted in the ED or the OR when a patient is hemorrhaging or unstable will need to be changed, unless there is clear documentation by the physician who inserted the line of the technique. Reminders Re Line Documentation on Flowsheet Remember to document when dressings are changed and if there are issues with any line (e.g., positional, blocked, dressing adherence). All line issues require a DAR note and should be reported during rounds. The issue, discussion and plan must be documented in the DAR. If an emergency line does not get changed following the initial discussion, this should be documented and passed on to subsequent shifts. Remember, if there is no documentation that line issues were reported in rounds, it means the discussion didn’t take place. FUTURE changes with next revision to CCTC Flowsheet: • • • • • A column will be added to identify location of insertion (e.g., by CCTC, OR, ED, IR or “other”) Columns will be added to identify whether there is documentation that insertion bundle requirements were MET or unknown/unmet When the revised flow sheet is available (several months away), the existing line tracking sheet that records line insertion details will be eliminated Until that time, please ensure that the line insertion location and circumstances are documented correctly and the line tracking sheet is up-to-date Any lines where insertion circumstances are unknown/unmet should be changed as soon as possible, and within 48 hours. Be sure to document the issue, discussion and plan from rounds. Future changes in next graphic revision: Inserted by: CCTC, OR, ED, IR, Other Insertion bundle Documented Unknown /unmet List all central and peripheral venous and arterial lines