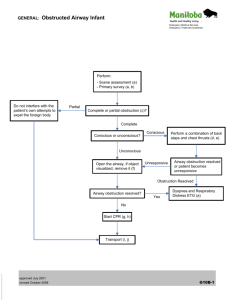
A- Infant Obstructed Airway
advertisement

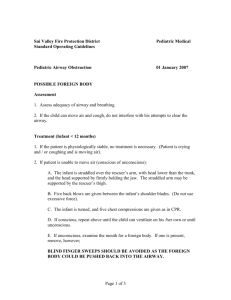
EMS SKILL AIRWAY EMERGENCY: AIRWAY OBSTRUCTION INFANT PERFORMANCE OBJECTIVES Demonstrate competency in recognizing and managing an airway obstruction in an infant who is choking. CONDITION Recognize and manage an airway obstruction in an infant who is found choking. Necessary equipment will be adjacent to the manikin or brought to the field setting. EQUIPMENT Infant manikin, infant bag-valve-mask device, O2 connecting tubing, oxygen source with flow regulator, pediatric resuscitation tape, goggles, various masks, gown, gloves, timing device. PERFORMANCE CRITERIA Items designated by a diamond () must be performed successfully to demonstrate skill competency. Items identified by double asterisks (**) indicate actions required, if indicated. Items identified by the symbol (§) should be practiced. Ventilations and compressions must be performed at the minimum rate required. PREPARATION Skill Component Key Concepts Take body substance isolation precautions Mandatory (minimal) personal protective equipment – gloves Assess scene safety/scene size-up If unknown as to possible trauma, manage as trauma (determined by environment and information obtained from bystanders). If spinal immobilization is required, an additional rescuer is needed to maintain in-line axial stabilization. ** Consider spinal immobilization - if indicated Evaluate need for additional BSI precautions Situational - goggles, mask, gown Approach the infant and introduce yourself to the infant, family or caregiver – if circumstance, time and resources allow Use age appropriate techniques to introduce yourself to infant. The caregiver should hold the infant during the assessment if the infant is in distress and responsive. RESPONSIVE INFANT PROCEDURE Skill Component Key Concepts Establish that the infant is choking: ** Call for additional resources – if needed Mild Obstruction: - adequate air exchange - coughing - gagging - stridor/wheezing Severe Obstruction: - poor or no air exchange - increased respiratory distress - weak, ineffective cough or no cough - stridor (high-pitched noise while inhaling) or no noise - unable to make noise (cry) - cyanosis - decreasing level of consciousness Signs and symptoms of airway obstruction may be caused by a foreign body or infection of the upper airway such as epiglottitis and croup. Infection should be suspected if the infant has a fever and is congested, hoarse, or drooling. Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 1 of 6 Skill Component Key Concepts DO NOT interfere if infant has an effective cough. Attempt to remove foreign body obstruction: Mild obstruction – Do not interfere with infant’s attempt to relieve the obstruction Only attempt to remove an obstruction caused by a foreign body. An obstruction caused by an infection will not clear with obstruction maneuvers and the infant must be transported immediately to an Emergency Department Approved for Pediatrics (EDAP). Severe obstruction – Perform up to 5 back slaps - Place infant prone on forearm Keep head lower than the body Support jaw and face Use heel of hand Deliver slaps, using the heel of the hand, between the shoulder blades DO NOT perform a blind finger sweep. This may force object further down the distal airway structures. Only perform finger sweep if object is visible. Place infant on forearm with head lower than the chest while supporting the head. Hold the jaw and face with fingers extended. DO NOT cover mouth or compress the soft tissue of the neck. Use the heel of the hand to deliver slaps to the back between the shoulder blades. Each slap should be of sufficient force to dislodge the object. Turn the infant by: Place infant face up (supine) Turn infant onto the opposite arm Maintain support of the head and neck - placing the free hand on the occiput and back, cradling the infant between both hands and arms - turning the body as one unit - maintain control of head and neck at all times - keep the head slightly lower than the body throughout the procedure (keep head lower than the body) Perform up to 5 chest thrusts: Find lower 1/2 of sternum (1 finger width below nipple line) Use 2 finger pads Compress at a depth of at least 1/3 - 1/2 of chest diameter Rate 1 thrust per second Technique for chest thrusts is the same as for chest compressions when performing CPR. DO NOT use upward compressions. - Lower half of sternum - 2 finger pads of either index & middle finger or middle & ring finger of one hand - Depth 1/3 - 1/2 the anterior/posterior diameter of the infant - Rate 1 thrust per second to simulate an “artificial cough” In children, the most common cause of cardiac arrest is an inadequate airway. Attempt removal of obstruction for 2 minutes before leaving the infant to call for other resources. Call for ALS - if obstruction is not relieved after 2 minutes or infant becomes unresponsive ** If responsive but still obstructed – continue series of back slaps and chest trusts until obstruction is relieved or the infant becomes unresponsive. Signs of inadequate breathing include: respiratory distress, fast/slow respirations, bradycardia, stridor, cyanosis, poor perfusion, and altered LOC (agitation, irritable cry, nonresponsive to caregivers, etc.). Manage ventilations after removal of obstruction: If breathing is restored and adequate: - trauma - initiate spinal immobilization If breathing is absent or inadequate: - perform rescue breathing of 12-20 per minute (1 breath every 3-5 seconds) with BVM or barrier device Supplemental oxygen should always be used after spontaneous breathing has resumed. When ventilating only use enough force to allow for adequate chest rise. Over-inflation causes gastric distention that will affect tidal volume by elevating the diaphragm. Use of a BVM by a single rescuer can result in an inadequate seal on the face and may not be as effective as a barrier device. When using an infant BVM device, occlude the pop-off-valve if unable to achieve adequate chest rise since higher pressures may be necessary. If the airway is open and it is difficult to compress the bag and air leaks around the seal, an airway obstruction may still be present. Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 2 of 6 UNRESPONSIVE INFANT PROCEDURE (Infants who were previously responsive may have the obstruction relieved when muscles relax) Key Concepts Skill Component Establish unresponsiveness Tap bottom of feet or gently shake and shout. ** Activate the emergency response system or call for additional EMS personnel - if not called for previously Assess for adequate breathing 5-10 seconds: Apnea Abnormal breathing Gasping Look at chest for adequate tidal volume and rate. Check breathing for at least 5 seconds and no more than 10 seconds. Palpate for brachial/femoral pulse 5-10 seconds unless history of chocking Palpate the pulse for at least 5 seconds and no more than 10 seconds. Check for other signs of circulation - breathing, coughing or movement in response to rescue breaths. This is done in conjunction with palpating for a pulse. An agonal gasp is not a breath, but may be present for several minutes. Gasps may sound like a snort, snore, or groan. Palpate brachial pulse on same side as the rescuer, inside of the upper arm and between the elbow and shoulder. An alternative to Palpating the brachial pulse is Palpating a femoral pulse in neonates and infants or at the base of the umbilical cord in the newborn. Start compressions (C-A-B sequence) Complete 30 compressions Open airway: Medical - head-tilt/chin-lift The tongue is the most common cause of airway obstruction due to decreased muscle tone. Trauma - jaw-thrust - neutral position (tragus of ear should be level with top of shoulder) The tongue and epiglottis may obstruct the entrance of the trachea due to inspiratory efforts creating negative pressure in the airway. Move the infant no more than necessary to maintain an open airway. A second rescuer is needed to maintain in-line axial stabilization if spinal immobilization is required. ** Clear/suction airway - if indicated If the infant is found in a prone position with suspected trauma, the infant should be turned using the log-roll method to avoid flexion or twisting of the neck and back. Look in mouth for foreign body: Attempt to remove foreign body obstruction - if visualized Always look in mouth for foreign body prior to giving breaths In children, the most common cause of cardiac arrest is an inadequate airway. DO NOT perform a blind finger sweep, this may force object further down the trachea. Perform finger sweep only if object is visible. The airway is easily obstructed by mucus, blood, pus, edema, external compression and hyperextension. To remove foreign body: - insert the index finger inside the cheek and into the throat to the base of the tongue. - use a hook like motion to grasp the foreign body and maneuver it into the mouth so it can be removed. Attempt 2 breaths with BVM or mouth-to-barrier-device (1 second/breath) Repositions head and attempt 2 ventilation is unsuccessful nd ventilation – if 1 st **- If object is not visible – continue CPR, starting with compressions ** Clear/suction airway - if indicated Continue CPR until foreign body obstruction is relieved Five (5) compression cycles should take approximately 2 minutes. ** Call for additional resources - If not called for previously Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 3 of 6 Skill Component Key Concepts Reassess infant after obstruction is relieved - If a pulse is present and the infant is not breathing adequately, start BVM ventilations. Look for: Responsiveness to stimulus Breathing Pulse Vital signs An infant who is not altered should be placed in a position of comfort. An infant who is altered should be placed in a position to protect the airway, reduce the chances of the airway being occluded by the tongue, and protected from aspiration of mucus or vomit. ** Start compressions - if heart rate is less than 60/minute with signs of poor perfusion [begin with compressions] REASSESSMENT (Ongoing Assessment) Skill Component Key Concepts Reassess the infant at least every 60 seconds once the infant has return of spontaneous respirations and circulation (ROSC): This is a priority infant and the heart rate must be re-evaluated every 60 seconds or sooner. Respirations and circulation continuously Initial assessment Relevant portion of the secondary assessment Vital signs Evaluate response to treatment Infants must be re-evaluated at least every 5 minutes if any treatment was initiated or medication administered. Evaluate results of reassessment and compare to baseline condition and vital signs Evaluating and comparing results assists in recognizing if the child is improving, responding to treatment or condition is deteriorating. **Manage the infant’s condition as indicated. § Explain the care being delivered and the transport destination to the child/caregivers Communication is important when dealing with the child, family or caregiver. This is a very critical and frightening time for all involved and providing information helps in decreasing the stress they are experiencing. PATIENT REPORT AND DOCUMENTATION Skill Component Key Concepts § Give patient report to equal or higher level of care personnel Report should consist of all pertinent information regarding the assessment finding, treatment rendered and infant’s response to care provided. § Verbalize/Document: Reassessment of airway includes: - chest rise and fall - skin color - airway patency Event leading up to the obstruction Cause of obstruction – type of obstruction/foreign body Observed or reported signs of obstruction: - skin signs - absent or inadequate respirations Response to obstruction maneuver Reassessment of airway Additional treatment provided Developed: 10/01 Documentation must be on either the Los Angeles County EMS Report or departmental Patient Care Record form. Revises: 6/06, 11/07, 1/08, 4/09, 1/13 Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 4 of 6 AIRWAY EMERGENCY: AIRWAY OBSTRUCTION INFANT Supplemental Information INDICATIONS: Infants who are choking with signs of mild or severe airway obstruction CAUSES: Intrinsic cause - tongue (most common), infection and swollen air passages Extrinsic cause - foreign body, facial injuries, vomitus, etc CONTRAINDICATIONS: None when above conditions apply. COMPLICATIONS: Gastric distention Rib fractures Sternal fractures Separation of ribs from sternum Laceration of liver or spleen Pneumothorax Hemothorax Lung and heart contusion Fat emboli Other internal injuries Recognizing Choking in the Responsive Infant Mild Airway Obstruction Signs Severe Airway Obstruction Signs • Adequate air exchange • Responsive and able to cough forcefully • May wheeze between coughs • • • • • • • Poor or no air exchange Weak, ineffective cough or no cough Stridor (high-pitched noise while inhaling) or no noise Increased respiratory difficulty Possible cyanosis Unable to make noise(cry) Decreasing level of consciousness Rescuer Actions Mild Airway Obstruction Severe Airway Obstruction • Encourage infant to continue coughing and attempt to breathe as long as there is adequate air exchange. • Activate ALS response • If responsive, perform chest thrusts • DO NOT interfere with the infant’s attempts to expel the foreign body. Monitor his/her condition. • If unresponsive, to stimuli start chest compressions • Activate ALS response if mild obstruction persists. NOTES: Infant is defined as a neonate to 1 year of age (12 months). Some signs of inadequate breathing are: respiratory distress, fast/slow respirations, bradycardia, stridor, cyanosis, poor perfusion, and altered LOC. Obstruction may have been relieved prior to EMS arrival. Patient should be transported for medical evaluation. DO NOT perform a blind finger sweep. This may force object further down trachea. Perform finger sweep only if object is visible. Supplemental oxygen should always be used after spontaneous breathing has resumed. An infant who is altered should be placed in a position to protect the airway to reduce the chance of the airway being occluded by the tongue and protected from aspiration of mucus or vomit. The tongue is the most common cause of airway obstruction due to decreased muscle tone. Intrinsic causes of an obstruction include infection and swollen air passages. Extrinsic causes include foreign body, facial injuries, vomitus, etc. The tongue and epiglottis may obstruct the entrance of the trachea due to inspiratory efforts creating negative pressure in t he airway. Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 5 of 6 AIRWAY EMERGENCY: AIRWAY OBSTRUCTION INFANT Supplemental Information Any infant who received chest thrusts must be evaluated medically to ensure there are no complications, injuries or retained foreign body fragments. DO NOT hyperventilate. Hyperventilation reduces the success of survival due to cerebral vasoconstriction resulting in decreased cerebral perfusion. In addition, hyperventilation increases intrathoracic pressure and decreases venous return to the heart resulting in diminished cardiac output. Rescuers have a tendency to ventilate too rapidly. Priority patients are patients who have abnormal vital signs, signs/symptoms of poor perfusion, or if there is a suspicion that the patient’s condition may deteriorate. Airway Emergency: Infant Airway Obstruction © 2013, 2009, 2008, 2007, 2006, 2001 Page 6 of 6