Downloaded
advertisement
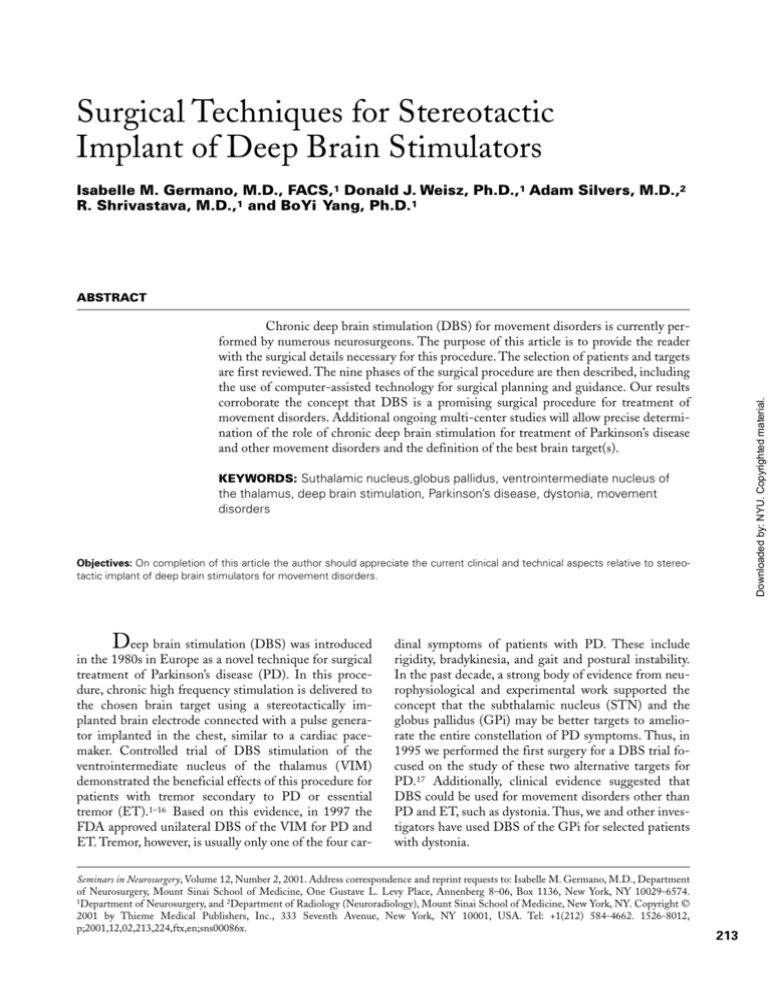
Surgical Techniques for Stereotactic Implant of Deep Brain Stimulators Isabelle M. Germano, M.D., FACS,1 Donald J. Weisz, Ph.D.,1 Adam Silvers, M.D.,2 R. Shrivastava, M.D.,1 and BoYi Yang, Ph.D.1 ABSTRACT Downloaded by: NYU. Copyrighted material. Chronic deep brain stimulation (DBS) for movement disorders is currently performed by numerous neurosurgeons. The purpose of this article is to provide the reader with the surgical details necessary for this procedure. The selection of patients and targets are first reviewed. The nine phases of the surgical procedure are then described, including the use of computer-assisted technology for surgical planning and guidance. Our results corroborate the concept that DBS is a promising surgical procedure for treatment of movement disorders. Additional ongoing multi-center studies will allow precise determination of the role of chronic deep brain stimulation for treatment of Parkinson’s disease and other movement disorders and the definition of the best brain target(s). KEYWORDS: Suthalamic nucleus,globus pallidus, ventrointermediate nucleus of the thalamus, deep brain stimulation, Parkinson’s disease, dystonia, movement disorders Objectives: On completion of this article the author should appreciate the current clinical and technical aspects relative to stereotactic implant of deep brain stimulators for movement disorders. D eep brain stimulation (DBS) was introduced in the 1980s in Europe as a novel technique for surgical treatment of Parkinson’s disease (PD). In this procedure, chronic high frequency stimulation is delivered to the chosen brain target using a stereotactically implanted brain electrode connected with a pulse generator implanted in the chest, similar to a cardiac pacemaker. Controlled trial of DBS stimulation of the ventrointermediate nucleus of the thalamus (VIM) demonstrated the beneficial effects of this procedure for patients with tremor secondary to PD or essential tremor (ET).1–16 Based on this evidence, in 1997 the FDA approved unilateral DBS of the VIM for PD and ET. Tremor, however, is usually only one of the four car- dinal symptoms of patients with PD. These include rigidity, bradykinesia, and gait and postural instability. In the past decade, a strong body of evidence from neurophysiological and experimental work supported the concept that the subthalamic nucleus (STN) and the globus pallidus (GPi) may be better targets to ameliorate the entire constellation of PD symptoms. Thus, in 1995 we performed the first surgery for a DBS trial focused on the study of these two alternative targets for PD.17 Additionally, clinical evidence suggested that DBS could be used for movement disorders other than PD and ET, such as dystonia. Thus, we and other investigators have used DBS of the GPi for selected patients with dystonia. Seminars in Neurosurgery, Volume 12, Number 2, 2001. Address correspondence and reprint requests to: Isabelle M. Germano, M.D., Department of Neurosurgery, Mount Sinai School of Medicine, One Gustave L. Levy Place, Annenberg 8–06, Box 1136, New York, NY 10029-6574. 1Department of Neurosurgery, and 2Department of Radiology (Neuroradiology), Mount Sinai School of Medicine, New York, NY. Copyright © 2001 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA. Tel: +1(212) 584-4662. 1526-8012, p;2001,12,02,213,224,ftx,en;sns00086x. 213 SEMINARS IN NEUROSURGERY/VOLUME 12, NUMBER 2 2001 This article reviews the technical details of the surgical procedure for DBS. At our Institution, DBS surgeries other than VIM for PD and ET are performed with Investigation Review Board (IRB) and Food and Drug Administration (FDA) Investigation Device (IDE) approval. PATIENT SELECTION One of the most important factors for successful surgical outcome is patient selection based on accurate diagnosis. Patients who are given the diagnosis of PD may have Parkinsonism or Parkinson’s plus syndromes. These are also known as “multiple system atrophy” (MSA). In either case, these syndromes respond poorly to surgery presumably because the underlying pathophysiology is not the same as for idiopathic PD. A history of good responsiveness to levodopa upon presentation of the symptoms is a good indicator that the diagnosis of PD is correct. Prior to consideration for surgery, all patients should have an adequate trial of medical therapy. Because of the fluctuating nature of the disease, “on” medication and “off ” medication neurological examinations should be performed by an experienced neurologist using standardized evaluation scales, such as the United Parkinson’s Disease Rating Scale (UPDRS) and Hoehn and Yahr scale. Most surgeons would agree that patients with a grade 5 Hoehn and Yahr score are so disabled that symptomatic improvement secondary to the surgery might not result in functional improvement. Thus, they are not good surgical candidates. Dementia and excessive brain atrophy are also considered contraindications for DBS. Contraindications for conventional stereotactic neurosurgical procedures are also contraindications to surgery for DBS. Normal preoperative coagulation studies are mandatory to rule out coagulopathy. Patients on chronic intake of oral anticoagulants are not considered good candidates for this procedure. Patients must stop the intake of acetylsalicilic acid and any other medication with antiplatelet effects at least 2 weeks prior to surgery. Uncontrolled hypertension, particularly intraoperative hypertension, is a contraindication since it increases the risk of intraoperative hemorrhage. Typically the patient is admitted to the hospital the morning of the procedure. The day prior to surgery the patient is loaded with Dilantin (1000 mg). Oral intake and medications, except for antihypertensive medications, are discontinued at midnight prior to surgery. Anti-Parkinson’s medications are discontinued to avoid drug-induced dyskinesias that can interfere with stereotactic frame placement and proper imaging studies for target determination. There is also concern that dyskinesias could apply enough force on the frame to reduce accuracy of stereotactic localization during the surgery. Additionally, discontinuation of anti-Parkinson’s medication facilitates the immediate feedback on the effects of the intraoperative stimulation (see below). TARGET SELECTION After the appropriate neurological diagnosis is confirmed and all contraindications are ruled out, a patient with medically refractory movement disorder(s) becomes a candidate for DBS. At this point it is crucial to decide the best brain target. The choice of target is based on the diagnosis and symptoms. There is unanimous consensus that the VIM is the best target for ET. For patients with advanced PD where tremor is only one of the symptoms we prefer to use the STN. Patients with dystonia are implanted in the GPi. Although these are currently our target selection criteria, there have been no studies to clearly document that these are the best choices, as discussed below. In most cases, patients have bilateral symptoms. Although we used to perform simultaneous bilateral procedures, we now prefer to stage them. Therefore, we select as the first side the brain target opposite to the patient’s worse symptoms. OPERATIVE PROCEDURE The operative procedure is divided into nine stages summarized in Table 1. The first eight phases of the procedure are done under local anesthesia with neuroleptic analgesia. Placement of the pulse generator is done under general anesthesia. We perform all stages in the same day. The duration of the entire procedure is 6 to 8 hours. Postoperatively the pulse generator is turned “on” the day of the patient’s discharge from the hospital, that is, 48 to 72 hours after the surgery. Typically, the patients require additional visits on an outpatient basis to determine the optimal stimulation contacts and electrical parameters. Table 1 Operative Procedure for Deep Brain Stimulation Implant 1. Fixation of the stereotactic frame 2. Imaging for target localization 3. Preoperative planning and virtual surgery 4. Placement of recording electrode 5. Intraoperative microrecording 6. Placement of permanent electrode 7. Intraoperative macrostimulation 8. Intraoperative imaging 9. Placement of pulse generator Downloaded by: NYU. Copyrighted material. 214 STEREOTACTIC IMPLANT OF DBS/GERMANO, ET AL Imaging for Target Localization The head MR localizer is then placed on the frame. The fiducial channels of the localizer must be completely filled with water to eliminate air bubbles that could cause artifacts. The patient is scanned in the supine position with the frame in the head coil. We use a Signa 1.5 Tesla scan (General Electric, Milwaukee, WI) and special sequences for target determination (Table 2). These sequences have the advantage of reducing spatial distortion with the T1-weighted images and excellent anatomical depiction of the GPi, the optic tract, the internal capsule, the red nucleus, the substantia nigra, and the STN with the T2-weighted images. We also acquire a T1-weighted sequence to be used for computer-assisted image-guided planning (see below). We obtain the first set of stereotactic coordinates using conventional stereotactic measurement and image Table 2 Magnetic Resonance Imaging Sequences for Target Localization Series Type Purpose Sagittal localizer Axial images Coronal images Contiguous axial T1W T1W T2W T1W Define AC-PC plane Obtain target coordinates Anatomical verification of target Computer-assisted planning acquisition protocol. First, the AC-PC line is identified on the sagittal localizer images. Axial 2-mm contiguous T1- and T2-weighted images are then obtained parallel to the AC-PC line. On T1-weighted axial images, the slice that simultaneously depicts AC and PC is identified. The superior-inferior and lateral distance of the desired target is then calculated. The axial slice with the appropriate superior-inferior distance to the AC-PC is then selected and the stereotactic coordinates of the target are chosen on that slice (Fig. 1). Additionally the “x” and “y” coordinates of the nine fiducials are calculated on the same axial slice. For targeting of the GPi and STN, T2-weighted images are then used to visualize anatomical landmarks, such as the external (GPe) and internal (GPi) pallidal segments, the internal capsule, the optic tract, the substantia nigra, and the red nucleus. The cursor used to define the target and fiducials on the T1-weighted images is positioned in the same location on the T2-weighted image to assess its relationship with the above anatomical landmarks. If necessary, adjustments based on visual anatomical landmarks are made in the anterior-posterior, lateral, and vertical coordinates. The last set of MR images is acquired according to our protocol for image-guided computer-assisted guidance. Preoperative Planning and Virtual Surgery The MRI obtained with the computer-assisted imageguided protocol is then loaded in the StealthStation Frame-Link software (Medtronic SNT, Louisville, CO). This allows for display of triplanar and 3D images. Additionally, after the fiducials of the stereotactic frame are entered in the computer together with the AC-PC and midline points, the computer provides real-time readout of AC-PC and CRW (or Leksell) coordinates (Fig. 2). Finally, a scalable Shaltenbrand atlas can be overlapped to the reformatted images. This allows anatomical and neurophysiological data to display simultaneously and it is very helpful in the refinement of the target choice. A second set of coordinates is, therefore, obtained with this software and compared to the previous set. In case of discrepancy, each coordinate (AP, lateral, vertical) can be visualized on the screen and corrected using visual anatomical landmarks. When the coordinates of the target are satisfactory, an entry point is selected. The entry point is chosen Downloaded by: NYU. Copyrighted material. Fixation of the Stereotactic Frame We use the Cosman-Roberts-Wells (CRW) stereotactic frame. This is fixed to the patient’s head on the morning of surgery. An intravenous infusion is secured to the patient’s arm ipsilateral to the deep brain implant for administration of neuroleptic analgesia. Approximately 30 minutes before placement of the frame, the patient is sedated with Valium (5 to 10 mg) and morphine (4 to 6 mg) while (s)he is monitored on a pulse oxymeter. With the patient in a wheelchair, the CRW MR-compatible ring is placed over the patient’s head as parallel as possible to the anterior-posterior commissure (AC-PC) line. In order to parallel the AC-PC line in the sagittal plane, the frame is positioned 15 degrees to a line that joins the lower canthus to the ipsilateral external auditory meatus and is inclined 6 degrees from the horizontal plane with the anterior half of the ring being higher than the posterior half. This is roughly achieved by having an assistant lightly supporting the frame below the external meatus with two hands and by allowing the frame to rest on a fingertip placed on the patient’s nose. Correct positioning of the stereotactic ring along the AC-PC line is much more important when placing the Leksell frame as with this stereotactic system the target is localized relative to the center of the frame. The scalp is then infiltrated to the periosteum with local anesthetic solution of 1.0% lidocaine; approximately 2 to 4 ml is injected through each of the pinholes using a 25-gauge needle. The stereotactic frame is then fixed to the patient’s head using four MR-compatible screws of the appropriate lengths. The diagonally opposed screws are advanced simultaneously and symmetrically, alternating between left and right opposing screws. In this fashion, all screws are advanced to similar depth to avoid rotation of the frame. 215 SEMINARS IN NEUROSURGERY/VOLUME 12, NUMBER 2 2001 A B C D Figure 1 MR images of a 70-year-old woman with ET used for target localization of the left VIM. (A) Sagittal T1-weighted localizer image depicting the AC and PC. (B) Sagittal image showing the position of the axial slices shown below and acquired parallel to the AC-PC line. (C) Axial image used to determine the location of the target. First, the length of the intercommisural line (IC, labeled 1, 26 mm). The crossing of the lines indicates the AP target calculated using conventional coordinates.17a From this point the lateral coordinate is calculated at 14 mm from the midline (labeled 2). (D) The vertical coordinate is 3 mm above the AC-PC plane. anterior to the coronal suture and approximately 3 cm lateral to midline. Great care is taken to ensure that the entry point is on a gyrus and not on a sulcus to avoid cortical hemorrhages. After the entry point is chosen, the computer displays the planned trajectory and the anteriorposterior and lateral arc coordinates for the frame. At this point additional computer-reformatted images can be displayed to allow performance of virtual surgery (Fig. 2). In particular the “probe eye’s view” reformatted image allows us to follow the planned path of the electrode through the brain. It is very important to assure that the planned path does not interfere with the sulci, the ventricular system, and the internal capsule. If the planned trajectory is not satisfactory, the entry point is changed and new trajectories can be displayed until the optimal one is found. Additionally, performance of virtual surgery with three-dimensional and triplanar images is an excellent teaching tool for residents in training. Placement of the Recording Electrode Although preoperative imaging studies are required to allow localization of the target, proper target localization is confirmed by intraoperative microrecording and macrostimulation. In the operating room, the patient lies supine on the operating room table with the frame fixed to the Mayfield head clamp adapter. The patient receives intravenous antibiotics (cefuroxime 1 gr) and steroids (dexamethasone 10 mg). The blood-pressure cuff and the oxygen saturation monitor are placed on the arm ipsilateral to the side of the deep brain stimulator implant to allow free neurological testing of the contralateral limbs during surgery. The patient’s hair is shaved anterior to the coronal suture. The entry point is marked using the frameless equipment. Lidocane 1% 1:200,000 with epinephrine is injected at the entry point. The patient’s head is draped with a transparent drape (Apuzzo drape, Downloaded by: NYU. Copyrighted material. 216 Figure 2 Preoperative planning and virtual surgery. Intraoperative photograph of the computer screen displaying axial and reformatted coronal, sagittal, and 3D images while planning the target, entry point, and trajectory for a left STN DBS. (A) After the fiducials, AC, PC, and midline points are entered in the computer, a reformatted patient’s scaled Schaltenbrand atlas is overlapped to the triplanar images. By clicking on the reformatted images (the dot on the images represents the chosen STN) the computer allows for real-time reading of the CRW coordinates in the dialog box (right-hand side). (B). After the target is selected, the entry point is chosen (see text) and the trajectory displayed as a line on the triplanar images. Virtual surgery can be performed by scrolling the bar in the dialog box and visualizing the planned path on computer reformatted images (right lower quadrant). This allows to optimization of the trajectory if necessary (see text). Radionics, Burlington, MA). This allows the patient’s face to be seen during the stimulation. Sedatives are administered intravenously by the anesthesiologist as needed. These are short lasting and are meant to sedate the patient during the placement of the burr hole only. The patient’s full cooperation during the remainder of the surgery is desirable. Blood pressure should be kept under strict control at all times, using intravenous antihypertensive medications if necessary. The CRW stereotactic arc is adjusted with the stereotactic coordinates obtained as described above. This is then mounted on a rigid CRW phantom to validate the accuracy of the hardware and then is assembled into the patient’s frame. A stereotactic guided linear skin incision, approximately 4 cm long, is made centered on the entry point and parallel to midline. A 14-mm burr hole is then made with a craniotome using a disposable burr (Acrucat, Codman, Philadelphia, PA). A burr hole ring is placed around the hole to allow fixation of the permanent electrode at the end of the procedure. The dura is cauterized with the bipolar and kept closed. A guiding cannula is then mounted on the CRW arc held by a digital microdrive (Radionics, Burlington, MA). A brain cannula is then inserted trough the dura bluntly and advanced to 20 mm above the target. A large piece of gelfoam is packed around the cannula on the dura to prevent CSF leak during the recording. Intraoperative Microrecording We utilize monopolar tungsten electrodes with a tip diameter of 0.25 micron and impedance of 500k ohms at 1k Hz (FHC, Brunswick, ME). After the cannula stylet 217 Downloaded by: NYU. Copyrighted material. STEREOTACTIC IMPLANT OF DBS/GERMANO, ET AL SEMINARS IN NEUROSURGERY/VOLUME 12, NUMBER 2 2001 is removed, the microelectrode is inserted through the brain cannula. The tip of the microelectrode is then advanced though the brain cannula. This extends 10 mm beyond the brain cannula. At this point the microelectrode impedance is verified. Electrodes are replaced if the impedance is less than 200k ohms or greater than 500k ohms. The microelectrode is further advanced in micrometer increments, using a digital microdrive. After waiting for 2 to 3 minutes for the brain to stabilize in position relative to the recording electrode, the tip is slowly advanced until extra cellular spikes are seen and heard from the recordings. The microelectrode recordings are amplified (gain = 5000) and bandpass filtered (300 to 10,000 Hz). The output of the amplifier is sent to a storage oscilloscope, an audioamplifier, a window discriminator, an analogto-digital converter connected to a personal computer, and a digital tape drive (for archival storage). Additional details of the microrecording equipment are reported elsewhere.18 Identification of the target structure through microelectrode recordings is accomplished by analyzing the characteristics of the neuronal recordings. As the microelectrode enters the STN, there is a sudden increase in the number of spikes being recorded because cells in the STN are much more densely packed and tonically active than are cells immediately above the structure. Single cells are isolated in order to obtain additional information about the neuronal firing patterns and rates. It is our experience that these cells can be more difficult to isolate than are cells in surrounding areas because of the STN’s higher cell density. As an aid in isolating single cells from a recording that contains two or more cells we also use template-matching spike sorting software. In our recordings most STN cells have shown an irregular firing pattern with periods of bursts and pauses (Fig. 3A). We have also observed tremor-related patterns of activity in patients who were exhibiting tremor at the time of the recordings. The cell density (high), pattern of activity (bursts of spikes and irregular firing patterns or tremor-related activity), firing rate (10 to 80 spikes/sec), and spike morphology (0.5 to 0.8 msec width) are our main criteria for STN localization. When placing a DBS in the GPi, typically the microrecording starts in the GPe. Cells in the GPe normally exhibit one or two patterns of firing, neither of which is regular. One pattern consists of rapid bursts lasting greater than 500 msec that are separated by very low rates of discharge or silence that can last for more than 0.5 msec. The second pattern consists of very slow firing interspersed with occasional short bursts of spikes. As the electrode moves to the GPi there is a brief silence and reduced background activity, indicating that the tip is probably in the internal medullary lamina. Unlike the GPe, the GPi cells exhibit continuous discharge without periods of silence. Firing rates of the GPI cells range from 10 spikes/sec to over 100 spikes/sec (Fig. 3B). As the electrode reaches the ventral part of the GPi, the background activity decreases. This indicates the presence of white matter, possibly the optic tract. At this point microstimulation (less than 20 mA) of the electrode is performed to evoke visual sensation. If electrical stimulation fails to elicit visual sensation, we record visual evoked responses from the same electrode. Recordings are made in correspondence to a flashing light that is computer controlled. Generally 20 to 50 stimuli are averaged and analyzed. Typical microelectrode recording of the VIM reveals noisy, high-voltage spontaneous activity (Fig. 3C), albeit less than that observed in the ventrocaudal (VC) thalamus. Additionally, in the VIM, kinesthetic neurons respond to deep (not superficial) movements of the joints. There is a topographic orientation, with the lower limb dorsolateral, upper limb ventromedial, and face most medial. Finally, single-cell recording of the VIM shows cells that discharge at tremor frequency and cease firing when the tremor is arrested. These are also known as “tremor cells.” Responses of single unit discharges to passive movements of the contralateral or ipsilateral limbs are also detected intraoperatively by analyzing the corresponding changes in neuronal firing rates and patterns as visualized on the oscilloscope, heard on the audiomonitor, and analyzed by computer software. Placement of the Permanent Electrode After adequate localization of the target is performed by microelectrode recording, the microelectrode and cannula are withdrawn. A larger cannula is then placed up to 10 mm above the target and the permanent electrode is passed into the cannula to reach the target. The permanent electrode is a 1.2 mm-diameter, tetrapolar electrode with four contacts, each 1.5 mm long at 1.5-mm distance from each other [Model 3387, Medtronic, Minneapolis, MN]. The most distant contact, known as contact “0,” is placed at “target.” The target for the permanent electrode is defined intraoperatively by the stereotactic coordinates of the track where the neurophysiological characteristics of the specific target were seen with the largest millimetric range. Intraoperative Macrostimulation The permanent electrode is then connected to a test stimulator. Macrostimulation is performed at high frequency greater than 100 Hz, to check for benefit, and low frequency less than 100 Hz, to rule out side effects. Typically, resolution of the tremor and improvement of rigidity are seen at high frequency. Motor effects, including tetanic contractions, seen at low voltage, suggest proximity to the internal capsule. When targeting the Downloaded by: NYU. Copyrighted material. 218 STEREOTACTIC IMPLANT OF DBS/GERMANO, ET AL 219 Downloaded by: NYU. Copyrighted material. A B C Figure 3 Oscilloscope tracings of intraoperative microelectrode recordings. Five seconds of activity are shown in each tracing (x-axis). Representative samples of the firing pattern, as described in the text, of a cell in (A) the STN; (B) the GPi; and (C) the VIM. STN, oculomotor effects, including mydriasis, indicate too-far medial location of the electrode. In the thalamus, speech disturbances, such as anomia, indicate proximity to the anterior nuclei, speech arrest to the medial nuclei, sensory disturbances, including paresthesias, to the posterolateral nuclei. Upon completion of the macrostimulation, the stylet is then removed from the electrode and the cannula is withdrawn from the brain. The electrode is secured to the burr hole ring with the burr hole cap. The skin is closed with nylon. Intraoperative Imaging The patient is then brought to the MR scanner to confirm correct positioning of the electrode and rule out presence of intracerebral hemorrhage (Fig. 4). This could be a contraindication to proceeding with the last phase of the surgery, that is, placement of the pulse gen- erator. After the MR images are acquired, the stereotactic frame is removed and the patient returned to the operating room. Placement of the Pulse Generator This stage of the surgical procedure is most readily accomplished under general anesthesia. The patient is positioned prone on the operating room table with the head in a donut holder rotated to the side opposite the implant. The head, neck, and superior half of the chest are prepped and draped. A linear skin incision is made below and parallel to the clavicle after infiltration with lidocaine 1:200,000 with epinephrine. A subcutaneous pocket over the muscle fascia is then dissected similar to that used for a cardiac pacemaker. The pocket should be big enough to accommodate the entire pulse generator and to avoid having the skin incision positioned over it. SEMINARS IN NEUROSURGERY/VOLUME 12, NUMBER 2 2001 Figure 4 Postoperative axial MR image of the same patient shown in Figure 1, confirming the location of the deep brain electrode in the left VIM. The electrode contact is seen in the left VIM as a signal void. Postoperatively, the patient had complete control of her essential tremor in the right upper extremity. The incision over the head is then reopened and the distal part of the electrode externalized. A tunneling device is then used to pass the connecting wire under the skin. This is then connected to the electrode proximally and to the pulse generator distally. The connecting wire is inserted in the distal part of the electrode and held in place by four screws. These are tightened with a hex wrench to achieve a finger-tight fit. The connection is then covered with a silicon boot. It is important that the connection not be placed over the parietal boss to avoid skin erosion. We place it toward the convexity; alternatively it could be placed behind the ear. The distal part of the connecting wire has two pins. These are inserted in the pulse generator and fixed by four screws closed with the hex wrench to achieve a finger-tight fit. Excess cable is carefully positioned behind the pulse generator. The pulse generator is then placed in the subcutaneous pocket with great care to position the engraved part of the stimulator toward the skin. If this is positioned toward the chest wall, percutaneous telemetry may be difficult to accomplish. The incisions are then closed in anatomical layers and dressed in the usual sterile fashion. RESULTS We participated in a multicenter trial that evaluated 96 patients and 38 patients who underwent bilateral STN and GPi DBS, respectively. These were followed for 6 months, with a double-blind, cross-over assess- ment at 3 months. Significant benefits of stimulation were observed with stimulation in both “off ” and “on” states. Stimulation for the “off ” state provided significant improvement of all the cardinal features of PD. Benefits were confirmed in the double-blind, cross-over study and approximated to those obtained with L-dopa, but with a decrease in motor fluctuations, increased “on” time without dyskinesia, and reduced “off ” period severity. The L-dopa dose was reduced by approximately 30% in these patients. In this trial, patients were not randomized to STN or GPi, so the study was not directed to compare these two targets. The detailed results of our patients, including improvement of UPDRS scores, have been published elsewhere.18a DISCUSSION Intraoperative stimulation at high frequency (greater than 100 Hz) of the motor thalamus has long been performed during ablative surgery for movement disorders to provide electrophysiological confirmation of the target location prior to lesioning.19–22 Chronic stimulation of the motor thalamus is very effective for medically refractory ET and PD tremor. In a series of 80 PD, Benabid found that 88% had complete or near complete resolution at the longest follow-up ranging from 6 months to 8 years.4 Similar efficacy has been noted in open trials.11,12 Bilateral thalamic DBS has been reported to be more effective than unilateral DBS in controlling bilat- Downloaded by: NYU. Copyrighted material. 220 STEREOTACTIC IMPLANT OF DBS/GERMANO, ET AL animal and human studies suggests that neurotransmitter and fiber activation also may be an important mechanism for DBS. Long-term effects of DBS in the brain are not known. DBS offers several theoretical advantages when compared to ablative procedures. First, the stimulation parameters can be adjusted at any time in an attempt to maximize efficacy and minimize adverse events. Second, since a destructive lesion is not performed, DBS does not preclude the opportunity to employ neuroprotective or restorative therapies when and if they become available. On the other hand, DBS has some disadvantages. First, the use of a mechanical device implies that malfunction or infection of the equipment could occur at any given time throughout the patient’s life. Second, since the lifespan of the pulse generator battery is restricted (2 to 5 years) additional surgery is necessary to replace it. Third, the DBS system is costly. Finally, the stimulator adjustments require frequent and prolonged out-patient visits to optimize the stimulation. CONCLUSIONS As is true of ablative procedures, high-frequency chronic DBS is a technically challenging procedure that requires stereotactic skills and excellent knowledge of the anatomy and physiology of the basal ganglia. Although DBS may have theoretical advantages over ablative procedures, further clinical experience with longterm follow up is necessary to establish if these advantages are real. Thus, at the present time the decision to treat a PD patient with an ablative procedure or DBS rests solely on the patient-physician’s decision. Additional multicenter studies are necessary to allow precise determination of the role of chronic DBS for treatment of PD and other movement disorders and to define the best brain target(s). REFERENCES 1. Alesch F, Pinter MM, Helscher RJ, et al. Stimulation of the ventral intermediate thalamic nucleus in tremor dominated Parkinson’s disease and essential tremor. Acta Neurochir 1995; 136:75–81 2. Benabid AL, Pollak P, Louveau A, Henry S, de Rougemont J. Combined (thalamotomy and stimulation) stereotactic surgery of the VIM thalamic nucleus for bilateral Parkinson disease. Appl Neurophysiol 1987;50:334–346 3. Benabid A, Pollak P, Cervason C, et al. Long-term suppression of tremor by chronic stimulation of the ventral intermediate thalamic nucleus. Lancet 1991;337:403–406 4. Benabid AL, Pollak P, Gao D, et al. Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders. J Neurosurg 1996;84: 203–214 Downloaded by: NYU. Copyrighted material. eral appendicular and midline tremor.23 In a randomized trial, DBS resulted in similar high level of tremor relief with significantly fewer complications than VIM thalamotomy.24 Relief of rigidity, bradykinesia, and gait and postural instability is, however, reportedly unaffected by VIM stimulation. Thus, alternative targets are investigated, namely the STN and GPi. An increasing number of reports describe the effects of chronic unilateral or bilateral pallidal stimulation for PD.25–33 Improvements in UPDRS motor scores during stimulation were highly variable, ranging from statistically insignificant25 to significant changes of 11 to 70% in other reports.26–31 Similarly to pallidotomy, pallidal stimulation improves contralateral tremor, rigidity, bradykinesia, and L-dopa–induced dyskinesias. Improvement in axial symptoms and gait and postural stability has been reported; however, this is not a unanimous finding.25–33 Multiple factors can contribute to the variability of improvements after GPi DBS. These factors include surgical technique, small sample size, and location of the permanent electrode. Efforts to proceed with larger prospective and controlled studies are in progress. Benabid and colleagues34–36 pioneered bilateral STN DBS in PD patients. In their experience, UPDRS motor scores and activity of daily living (ADL) scores improved by 42 to 82% 3 months after the surgery. All PD symptoms improved in the “off ”state with akinesia and rigidity improving the most. More than with any other procedure, the “on” state symptoms that are L-dopa–resistant are improved.35 Additionally, after STN DBS, patients were able to significantly decrease their L-dopa intake. Thus, drug-induced dyskinesias are improved after STN DBS. Numerous other clinical reports confirmed these findings.34–44 The exact mechanisms by which chronic electrical stimulation is efficacious are complex and still poorly understood. It is well known that the effects of stimulation are only seen while the stimulation occurs and they stop within seconds of stopping the stimulation. It seems clear that DBS simulates the effects of a lesion without the need to make a brain lesion. At typical stimulation parameters, tissue within 2 to 3 mm of the stimulating electrode is likely to be affected, but could vary greatly depending on the stimulation parameters. Stimulation could directly activate cells or axons by depolarization, but could also inactivate cells or axons by depolarization blockade. Furthermore, electrical stimulation can activate adjacent long tract white matter fibers either orthodromically or antidromically. Activation of cells or fibers could have similar behavioral effects as inactivation by increasing release of inhibitory neurotransmitters, overriding abnormally patterned activity, with a constant frequency signal, or by numerous other hypothetical mechanisms.35 Although there is evidence for local neuronal blockade, other evidence from 221 SEMINARS IN NEUROSURGERY/VOLUME 12, NUMBER 2 2001 5. Blond S, Siegfried J. Thalamic stimulation for the treatment of tremor and other movement disorders. Acta Neurochir Suppl 1991;52:109–111 6. Blond S, Caparros-Lefebvre D, Parker F, et al. Control of tremor and involuntary movement disorders by chronic stereotactic stimulation of the ventral intermediate thalamic nucleus. J Neurosurg 1992;77:62–68 7. Burleigh AL, Horak FB, Burchiel KJ, et al. Effects of thalamic stimulation on tremor, balance, and step initiation: a single subject study. Mov Disord 1993;8:519–524 8. Caparros-Lefebvre D, Ruchoux MM, Blond S, Petit H, Percheron G. Long-term thalamic stimulation in Parkinson’s disease: postmortem anatomoclinical study. Neurology 1994; 44:1856–1860 9. Deiber MP, Pollak P, Passinghan R, et al. Thalamic stimulation and suppression of parkinsonian tremor: evidence of a cerebellar deactivation using positron emission tomography. Brain 1993;116:267–279 10. Hassler R. The influence of stimulations and coagulations in the human thalamus on the tremor at rest and its physiopathologic mechanism. Excerpta Media Foundation 1955; 2:637–642 11. Hubble JP, Busenbar KL, Wilkinson S, et al. Effects of thalamic deep brain stimulation based on tremor type of diagnosis. Mov Disord 1997;12(3):337–341 12. Koller W, Pahwa R, Busenbark K, et al. High-frequency unilateral thalamic stimulation in the treatment of essential and parkinsonian tremor. Ann Neurol 1997;42:292–299 13. Ondo W, Jankovic J, Schwartz K, Almaguer M, Simpson RK. Unilateral thalamic deep brain stimulation for refractory essential tremor and Parkinson’s disease tremor. Neurology 1998;51:1063–1069 14. Siegfried J and Lippitz B. Bilateral chronic electrostimulation of ventroposterolateral pallidum: a new therapeutic approach for alleviating all Parkinsonian symptoms. Neurosurgery 1994;35:1126–1130 15. Tasker RR. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg Neurol 1998;49:145–153 16. Andy DJ. Thalamic stimulation for control of movement disorders. Appl Neurophysiol 1983;46:107–111 17. Olanow CW, Germano IM, Brin MF, Swope D, Weisz D. Deep brain stimulation of the subthalamic nucleus for Parkinson’s disease. Mov Disord 1996;11(5):598–599 17a.Kelly PJ. Therapy of Parkinson’s Disease. New York: Marcel Dekker; 1990 18. Weisz D and Yang B. Intraoperative electrophysiological recording techniques. In: Germano IM, ed. Neurosurgical Treatment of Movement Disorders. Park Ridge, IL: AANS Publication Committee, 1998:207–218 18a.Olanow CW, Brin MF, Obeso JA. The role of deep brain stimulation as a surgical treatment of Parkinson’s disease. Neurology 200;55(S60-S66) 19. Hassler R, Riechert T, Munginger F, Umbach W, Ganglberger JA. Physiological observations in stereotaxic operations in extrapyramidal motor disturbances. Brain 1960;83: 337–350 20. Bertrand G, Jasper H, Wong A, Mathews G. Microelectrode recording using stereotactic surgery. Clin Neurosurg 1966; 16:328–356 21. Hirai T, Miyazaki M, Nakajima H, Shibazaki T, Ohye C. The correlation between tremor characteristics and the predicted volume of effective lesions in stereotaxic nucleus ventralis intermedius thalamotomy. Brain 1983;106:1001–1018 22. Tasker RR, Organ LW, Hawrylyshyn P. Investigation of the surgical target for alleviation of involuntary movement disorders. Appl Neurophysiol 1982;45:261–274 23. Ondo W, Almaguer M, Jankovic J, Simpson R. Thalamic deep brain stimulation: comparison between unilateral and bilateral placement. Arch Neurol 2001;58:218–222 24. Schuurman PR, Bosch DA, Bossuty PMM, et al. A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med 2000;342: 461–468 25. Tronnier VM, Fogel W, Kronenbuerger M, Steinvorth S. Pallidal stimulation: an alternative to pallidotomy? J Neurosurg 1997;87:700–705 26. Burchiel KJ, Anderson VC, Favre J, Hammerstad JP. Comparison of pallidal and subthalamic nucleus deep brain stimulation for advanced Parkinson’s disease: results of a randomized, blinded pilot study. Neurosurgery 1999;45:1375– 1384 27. Durif F, Lemaire JJ, Debilly B, Dordain G. Acute and chronic effects of anteromedial globus pallidus stimulation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1999;67: 315– 322 28. Gálvez-Jiménez N, Lozano A, Tasker R, Duff J, Hutchison W, Lange AE. Pallidal stimulation in Parkinson’s disease patients with a prior unilateral pallidotomy. Can J Neurol Sci 1998;25:300–305 29. Ghika J, Villemure JG, Fankhauser H, et al. Efficiency and safety of bilateral contemporaneous pallidal stimulation (deep brain stimulation) in levodopa-responsive patients with Parkinson’s disease with severe motor fluctuations: a 2-year follow-up review. J Neurosurg 1998;89:713–718 30. Gross C, Rougier A, Guehl D, Boraud T, Julien J, Bioulac B. High-frequency stimulation of the globus pallidus internalis in Parkinson’s disease: a study of seven cases. J Neurosurg 1997;87:491–498 31. Troster AI, Fields JA, Wilkinson SB, et al. Unilateral pallidal stimulation for Parkinson’s disease: neurobehavioral functioning before and 3 months after electrode implantation. Neurology 1999;49:1078–1083 32. Vingerhoets G, van der Linden C, Lanno E, et al. Cognitive outcome after unilateral pallidal stimulation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1999;66:297–304 33. Hristova A, Lyons K, Troster A, Pahwa R, Wilkinson S, Koller W. Effect and time course of deep brain stimulation of the globus pallidus and subthalamus on motor features of Parkinson’s disease. Clin Neuropharmacol 2000;23(4): 208–211 34. Limousin P, Pollak P, Hoffman D, Benazzouz A, Perret JE, Benabid AL. Abnormal involuntary movements induced by subthalamic nucleus stimulation in parkinsonian patients. Mov Disord 1996;11:231–235 35. Limousin P, Krack P, Pollak P, et al. Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 1998;339:1105–1111 36. Limousin PL, Pollak P, Benazzouz A, et al. Effect on parkinsonian signs and symptoms of bilateral subthalamic nucleus stimulation. Lancet 1995;345:91–95 37. Krack P, Pollack P, Limousin P, et al. Subthalamic nucleus or internal pallidal stimulation in young onset Parkinson’s disease. Brain 1998;121:451–457 38. Krack P, Benazzouz A, Pollak P, et al. Treatment of tremor in Parkinson’s disease by subthalamic nucleus stimulation. Mov Disord 1998;13:907–914 Downloaded by: NYU. Copyrighted material. 222 STEREOTACTIC IMPLANT OF DBS/GERMANO, ET AL 43. Pinter MM, Alesch F, Murg M, Seiwald M, Helscher RJ, Binder H. Deep brain stimulation of the subthalamic nucleus for control of extrapyramidal features in advanced idiopathic Parkinson’s disease: one-year follow-up. J Neural Transm 1999;106:693–709 44. Rodriguez-Oroz MC, Gorospe A, Guridi J, et al. Bilateral deep brain stimulation of the subthalamic nucleus in Parkinson’s disease. Neurology 2000;55(Suppl 6):S45–S51 Downloaded by: NYU. Copyrighted material. 39. Kumar R, Lozano AM, Kim YJ, et al. Double-blind evaluation of subthalamic nucleus deep brain stimulation in advanced Parkinson’s disease. Neurology 1998;51:850–855 40. Molinuevo J, Valldeoriola F, Tolosa E, et al. Levodopa withdrawal after bilateral subthalamic nucleus stimulation in advanced Parkinson’s disease. Arch Neurol 2000;57:983–988 41. Moro E, Scerrati M, Romito LM, Roselli R, Tonali P, Albanese A. Chronic subthalamic nucleus stimulation reduces medication requirements in Parkinson’s disease. Neurology 1999;53:85–90 42. Pillon B, Ardouin C, Damier P, et al. Neuropsychological changes between “off ” and “on” STN or GPi stimulation in Parkinson’s disease. Neurology 2000;55:411–418 223 Downloaded by: NYU. Copyrighted material.