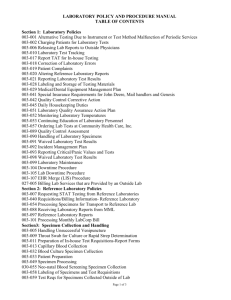
Laboratory Services Manual - Regina Qu'Appelle Health Region
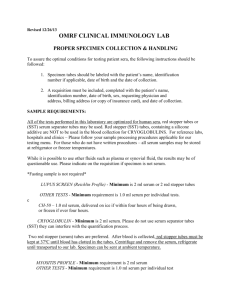
advertisement

LABORATORY SERVICES MANUAL AND TEST COMPENDIUM TABLE OF CONTENTS I LABRegOP7900 GENERAL INFORMATION I Laboratory Services at RQHR Sites............................................................1 II Hours of Operation .....................................................................................2 III Laboratory Administration..........................................................................2 IV Phlebotomy Services ...................................................................................3 V Laboratory Requisitions ..............................................................................4 VI Test Priority.................................................................................................5 VII Test Order Entry..........................................................................................6 VIII Requisition Test Add-Ons or Changes........................................................7 IX Specimen Requirements.............................................................................. 7 X Specimen Collection 1. Client Identification.............................................................................8 2. Typenex Red Arm Bands ....................................................................8 3. Collection of Blood Specimens...........................................................9 4. Specimen Labelling...........................................................................10 XI Transporting Specimens to the lab ............................................................ 10 XII Specimen Rejection................................................................................... 11 XIII Laboratory Information System ................................................................11 XIV Results Reporting ......................................................................................12 XV Types of Reports .......................................................................................13 XVI Requests for Results .................................................................................13 XVII Availability of Tests “After Hours” ..........................................................13 XVIII Laboratory Tests Available on 24 Hour Basis ..........................................14 XIX Turn Around Time ....................................................................................14 XX Critical Values ..........................................................................................15 XXI Laboratory Abbreviations .........................................................................15 APPENDIXES LABRegOP7109 Laboratory Specimen Portering Competency LABRegOP7109A1 Instructions for Portering Laboratory Specimens LABRegOP7109A2 Portering Laboratory Specimens Competency Quiz LABRegOp7109A3 Portering Laboratory Specimens Competency Quiz Answers LABPhlbOP7009A1 Sending Patient Specimens using the Pneumatic Tube Critical Values: LABChemOP8200T1 Chemistry Critical Values LABHemaOP7019T1 Hematology Critical Values LABMicOP8000A1 Microbiology Critical Values LABTranOP7001W3Transfusions Critical Values LABHistOP1000T1 Anatomic Pathology Critical Results LABCytoOP7047 Communication of Cytopathology Critical Results LABRlabOP7900A2 Rural Lab Critical Results LABRegOP7901T.2.6 Table of Contents Lab Services Manual Laboratory Services, Regina Qu’Appelle Health Region Page 1 of 5 Last printed 7/4/2013 3:15 PM Turn Around Times: LABChemOP8202C1 Chemistry Tests LABHemaOP7031C1 Guidelines for Expected TAT in Hematology LABMicOP8000A2 Anticipated TAT for Microbiology Tests LABTranOP7001W2 TAT for Transfusions SDCL Requisition Completion Instructions LABRlabOP7900A3 Tests Performed at Rural RQHR sites II LABChemOP7269 CHEMISTRY Purpose ........................................................................................................ 1 Procedure..................................................................................................... 1 Blood Specimens......................................................................................... 2 Rapid ACTH Test (Cortrosyn) ......................................................... 2 Blood Ethanol ................................................................................... 2 Blood Gases ...................................................................................... 2 Dexamethasone Suppression Test .................................................... 3 Glucose Tolerance ............................................................................ 3 Growth Hormone Suppression Test.................................................. 4 Insulin ............................................................................................... 4 Xylose Test ....................................................................................... 5 Urine Specimens ......................................................................................... 5 Specimen Collection ......................................................................... 5 Urine Testing Notes .......................................................................... 6 Feces Specimens ......................................................................................... 6 Feces Tests........................................................................................ 6 CSF Specimens ........................................................................................... 7 Toxicology Specimens ................................................................................ 7 Fluid Specimens .......................................................................................... 8 Specimen Collection ......................................................................... 8 Tests Performed ................................................................................ 8 Fluid Notes........................................................................................ 8 Therapeutic Drug Testing...........................................................................9-11 LABChemOP7352A1 ACTH Stimulation Test LABChemOP7317A1 75 Gm Maternal Glucose Tolerance III LABAccnOP7200 CYTOGENETICS I General Information .................................................................................... 1 II Blood Chromosome Studies........................................................................ 2 III Bone Marrow Studies.................................................................................. 2 IV Aminotic Fluid Analysis ............................................................................. 2 LABRegOP7901T.2.6 Table of Contents Lab Services Manual Laboratory Services, Regina Qu’Appelle Health Region Page 2 of 5 Last printed 7/4/2013 3:15 PM V VI VII VIII IV V Products of Conception Analysis ................................................................ 3 Cord Blood Studies ..................................................................................... 3 Buccal Smears for Sex Chromatin Studies ................................................. 3 Out Patient Services .................................................................................... 3 LABCytoOP7000 CYTOLOGY I Purpose ........................................................................................................ 1 II Specimens – Types, Collection Methods, Identification and Labelling ..... 1 III Specimen Submission and Transportation .................................................. 2 IV Cytology Requisitions ................................................................................. 2 V Specimen Rejection Criteria........................................................................ 3 VI RQHR Cytology Laboratory Address and Hours of Operation .................. 3 VII General Techniques A. Pap Smears .................................................................................... 4 B. Sputum ............................................................................................ 5 C. Bronchial Brushings ...................................................................... 6 D. Bronchial Washings ...................................................................... 6 E. Urine Specimens/Bladder Washings ............................................. 6 F. Serous Effusions (Pleural, Peritoneal, Pericardial Fluids) ............ 7 G. Cerebrospinal Fluids ..................................................................... 7 H. Abdominal and Pelvic Washings .................................................. 8 I. Gastrointestinal, Esophageal and Gastroesophageal Brushings...... 8 J. Breast Secretions (Nipple Discharges) .......................................... 8 K. Joint Fluids .................................................................................... 9 L. Cyst Fluids ..................................................................................... 9 M. Ocular Specimens .......................................................................... 9 N. Guided Fine Needle Aspiration Biopsies (Cat Scan, Ultrasound) Adequacy Check ......................................................................... 10 O. Fine Needle Aspiration Clinic, Pasqua Hospital........................... 11 LABHemaOP7001 HEMATOLOGY Hematology I General Information .................................................................................. 1 II Requisition Forms ..................................................................................... 1 III Collection of Specimens.............................................................................. 2 IV Bone Marrow Examinations ...................................................................... 2 V List of Tests Provided in Hematology ....................................................... 3-4 VI Blood Required for Laboratory Tests ........................................................ 5 VII Normal (Reference) Ranges ...................................................................... 6-9 LABHemaOP7037 Flowcytometry General Information .................................................................................... 1 Collection of Specimens.............................................................................. 1 List of Tests provided in Flowcytometry .................................................... 2 LABRegOP7901T.2.6 Table of Contents Lab Services Manual Laboratory Services, Regina Qu’Appelle Health Region Page 3 of 5 Last printed 7/4/2013 3:15 PM VI VII LABHistOP1000 HISTOPATHOLOGY Hours of Operation.................................................................................................. 1 I Submission of Tissues for Examination .................................................... 1 1. Routine Pathological Examination.................................................. 1 2. Urgent or Overnight Reports ......................................................... 1 3. Tissues for Microbiological Examination Prior to Pathological Examination .................................................................................. 1 4. Tissues for Quick Section ............................................................. 2 5. Tissue for Electron Microscopy .................................................... 2 6. Photography ................................................................................... 2 7. Immunofluorescence for Bound Immunoglobulin ........................ 2 8. Lymph Nodes and Open Lung Biopsies ....................................... 3 9. Testicular Biopsies ........................................................................ 3 10. Amputated Limbs .......................................................................... 3 11. Specimens Sent to Lab After 1630 Hours ..................................... 3 12. Muscle Biopsies for Enzyme Histochemistry ............................... 3 13. Nerve Biopsies .............................................................................. 3 14. Flow Cytometry ............................................................................. 4 15. Chromosome Studies ..................................................................... 4 16. Kidney Biopsies ............................................................................ 4 II Autopsies ................................................................................................... 4 1. Coroner’s Cases............................................................................... 4 2. Hospital Autopsies .......................................................................... 5 3. Courtesy Autopsies ......................................................................... 5 Consent for Autopsy........................................................................ 5 LABMicOP7204 MICROBIOLOGY Hours of Operation...................................................................................... 1 Scope of Service.......................................................................................... 1 Specimens for Microbiology....................................................................... 2 Reporting Results ........................................................................................ 3 APPENDIXES LABMicOp7204A1 Specimen Containers for Microbiology LABMicOP7204A2 Microbiology Collection and Test Compendium LABMicOP7204A3 Sputum Collection LABMicOP7204A4 Stool Collection LABMicOP7204A5 Urine Collection LABMicOP7204A6 Pinworm Collection LABMicOP7204T1 Criteria for Rejection of Microbiology Specimens LABMicOP7021 Collection of Blood Cultures LABRegOP7901T.2.6 Table of Contents Lab Services Manual Laboratory Services, Regina Qu’Appelle Health Region Page 4 of 5 Last printed 7/4/2013 3:15 PM VIII LABTranOP7001 TRANSFUSIONS I Legal Responsibility.................................................................................... 1 II Supply of Blood .......................................................................................... 1 III Ordering Blood Transfusions ...................................................................... 1 IV Issue of Blood.............................................................................................. 3 V Patient Notification ..................................................................................... 3 VI Blood Infusion............................................................................................. 3 VII Canceling Blood.......................................................................................... 4 VIII Shortages of Blood ...................................................................................... 4 IX Emergent and Routine Transfusions ........................................................... 4 X Confirmatory Blood Group ......................................................................... 5 XI Crossmatches for Surgery ........................................................................... 5 XII Cord Blood .................................................................................................. 5 XIII Exchange Transfusion ................................................................................. 5 XIV Neonate Transfusion ................................................................................... 6 XV Autologous and Directed Donations ........................................................... 6 XVI Blood Required for Laboratory Tests.......................................................... 6 XVII Adverse Effects of Transfusions ................................................................7-10 XVIII Product Information .................................................................................. 10 APPENDIXES • LABTranOP7011 Use of the Typenex Red Arm Band • LABTranOP7001W4 Canadian Blood Services CIRCULAR OF INFORMATION IX LABLisOP8007F2 TEST COMPENDIUM LABRegOP7901T.2.6 Table of Contents Lab Services Manual Laboratory Services, Regina Qu’Appelle Health Region Page 5 of 5 Last printed 7/4/2013 3:15 PM Subject/Title: LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATION Last Approved Time: 7/4/2013 2:24:13 PM Revision: 3.4 Approving Authority and Contact for Interpretation: Assistant Manager Laboratory Services Regulatory Affairs Phone: (306) 766-4470 Current Version on Print Date Policy Process Control Purpose The purpose of this procedure is to provide specific instructions for the proper collection and handling of laboratory specimens. These instructions have been developed for those collecting specimens to be submitted to Regina Qu’Appelle Health Region (RQHR) laboratories for analysis. Procedure I Laboratory Services at Regina Qu’Appelle Health Region (RQHR) Sites The laboratory at the Wascana Rehabilitation Centre functions as a specimen collection service only. All specimens are referred to other laboratories for processing. The laboratory at the Pasqua Hospital consists of a: Centralized Histopathology Laboratory Centralized Cytopathology Laboratory Autopsy Suite Rapid Response Lab which offers stat service for a limited test menu in clinical pathology (Chemistry, Haematology and Transfusions) Phlebotomy service Accession service The laboratory at the Regina General Hospital consists of a: Centralized clinical pathology service (Chemistry, Haematology, Transfusions, Microbiology, Chemistry Specialized Testing) Satellite Cytopathology service Satellite Histopathology service which performs quick sections only on surgical specimens Autopsy suite Phlebotomy service Accession service LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 1 of 18 Last printed 7/4/2013 2:24 PM II Hours of Operation The Wascana Rehabilitation Centre laboratory operates from 0730 to 1600 hours, Monday to Friday. It is closed on weekends and statutory holidays. The Regina General Hospital and Pasqua Hospital laboratories operate 24 hours a day, seven days a week. Full services are available Monday to Friday, 0730 1600 hours (there may be some variation in hours from one lab discipline to another), while a limited test menu is available outside of regular hours. Laboratory services must not be abused. Routine work, whenever possible should be requested during the day shift. The staffing level during evenings, nights and weekends is greatly reduced and cannot accommodate excessive routine requests without jeopardizing the laboratory’s ability to respond to emergencies in a timely fashion. III Laboratory Administration The Medical Head, Laboratory Services and the Director-Operations, Laboratory Services are ultimately responsible for the overall operation of laboratory services in the RQHR. The Director-Operations, Laboratory Services is responsible for the operation of the Laboratory Services financial management and human resources for laboratory services within the RQHR in Regina and is responsible for the regulatory and safety requirements for all laboratories within the RQHR. The Manager, Laboratory Information System, with the assistance of one supervisor, is responsible for management of the Laboratory Information System at all sites. The Assistant Manager, Regulatory Affairs, Laboratory Services, with the assistance of one supervisor, is responsible for all issues related to quality assurance, safety and regulatory requirements at all sites. The Assistant Manager, Finance and Human Resources/Labour Relations, Laboratory Services is responsible for all issues related to financial management and human resources/labour relations of all Regina laboratory sites of the RQHR. There are six Unit Managers. Responsibility for each laboratory discipline is assigned to the Unit Managers as follows: Unit Manager, Chemistry, with the assistance of two supervisors, is responsible for Chemistry, Specialized Chemistry and Point of Care Testing at all sites. Unit Manager, Haematology/Transfusions, with the assistance of two supervisors, is responsible for Haematology and Transfusions services at all sites. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 2 of 18 Last printed 7/4/2013 2:24 PM Unit Manager, Histopathology/Cytopathology, with the assistance of two supervisors, is responsible for Histopathology and Cytopathology services at all sites. Unit Manager, Microbiology, with the assistance of one supervisor, is responsible for Microbiology services at all sites. Unit Manager, Laboratory Support Services, with the assistance of two supervisors, is responsible for Phlebotomy, Accessioning and other support personnel and services at the RGH and Pasqua sites. Unit Manager, Rural and Inter-Regional Support is responsible for Laboratory Services at the rural sites. Each laboratory discipline is also under the direction of a Medical Section Head that is a medically qualified specialist in his/her field of laboratory medicine. All issues and concerns related to specific disciplines or services should be directed to the Unit Manager or supervisor responsible. Physicians should direct their concerns to the Medical Section Head of the specific laboratory discipline or the Medical Head, Laboratory Services. IV Phlebotomy Services Wascana Rehabilitation Centre Collections begin at 0730 hours each morning on days the laboratory is in operation. Fastings are collected first, followed by the remainder of the requests. Additional requests that arise during the day should be phoned to the laboratory. Regina General Hospital Daily collection rounds are as follows: 0630 hours - all routine collections for which requisitions have been received are collected. 1030 hours - any routine orders that have accumulated between 0630 and 1030 hours will be collected during this round. 1300 hours - any routine orders that have accumulated between 1030 and 1300 hours will be collected during this round. Timed requests will be collected at the times specified throughout the day. STAT and URGENT requests will be collected throughout the day as the need arises. Phlebotomy staff will respond STAT to Trauma, MI (Myocardial Infarction) and Stroke alerts. All routine orders will be batched according to the above schedule unless instructions to the contrary are communicated to the phlebotomists. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 3 of 18 Last printed 7/4/2013 2:24 PM Pasqua Hospital 0630 hours - all routine collections for which requisitions have been received are collected. 0900 hours and hourly until 2200 hours - all routine collections for which requisitions have been received in the laboratory are collected on each collection round. Timed requests will be collected at the times specified throughout the day. STAT and URGENT requests will be collected throughout the day as the need arises. Phlebotomy staff will respond STAT to Trauma, MI (Myocardial Infarction) and Stroke alerts. All routine orders are batched according to the above schedule unless instructions to the contrary are communicated to the phlebotomists. V Laboratory Requisitions 1. Laboratory requisitions serve as a mechanism for placing a client test order in the Laboratory Information System (LIS). The following requisitions are available: Biochemistry / Haematology Microbiology Transfusions Flow Cytometry Surgical Pathology Consultation Gastrointestinal Biopsy Prostate Biopsy Women’s Health Centre Pathology Cytopathology – Non Gynecologic Cytopathology - Gynecologic Biochemistry EIA Cytogenetics Saskatchewan Disease Control Laboratory Ova & Parasite Examination Community green white pink salmon cream yellow cream cream canary mauve canary white (Royal Columbian requisition) Choose the appropriate requisition Green (full page form) blue 2. A supply of requisitions is available from the RQHR Print Shop. Copies of the Royal Columbian Cytogenetics requisition may be obtained from the Accession department. Canadian Blood Services requisitions for HLA Typing may be obtained from the Accession Department, Laboratory Services. 3. Orders for tests, which are referred to Saskatchewan Disease Control Laboratory, must be submitted on the appropriate SDCL requisition. Do not use RQHR requisitions. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 4 of 18 Last printed 7/4/2013 2:24 PM 4. VI When completing requisitions: stamp the top right-hand corner of RQHR requisitions with the client’s addressograph. In the absence of an addressograph, print legibly the required information. Be sure to include all of the following information: first and last name date of birth (day/month/year) MRN / HSN Stay Number gender name of ordering physician, including the first name or initial in-patient location, or physician address for out-patients and referred-in specimens indicate “copy to” physician, if required. Clearly indicate this physician’s first name or initial and location. indicate the priority, i.e. stat, urgent, routine or timed indicate date and time to be collected (when required) indicate the diagnosis and other relevant information such as anticoagulant therapy, antibiotic therapy, therapeutic drug dosage or client’s height and weight. indicate tests required. If test order is uncommon or unclear, verify test order for accuracy. For unusual test requests refer to the Laboratory Specimen Requirements in the Test Compendium on the RQHR Intranet or on the RQHR internet website. For tests not listed in the test compendium, contact the SDCL for client preparation and specimen collection requirements. all changes made to a requisition must be authorized and initialled by the nursing staff making the change. Test Priority The terms STAT, Urgent, Routine and Timed Collection will be used consistently when ordering laboratory tests. STAT - refers to life threatening medical emergencies. Laboratory staff gives top priority to STAT requests at the expense of other orders, therefore this priority should only be used when absolutely necessary. Urgent - refers to tests that are required as soon as possible but are not involved in life threatening medical emergencies. Routine – these specimens are processed after STATs and Urgent collections. Timed - used when specimens are to be collected at specified times of the day. Timed collections are ordered in the following instances only: - pre-op bloodwork - special procedures (eg: angioplasty, ACTH stimulation tests) - TPN bloodwork - timed drug levels - INR - timed due to medication adjustment - CK, Troponin ordered as per physician request for CCU protocol LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 5 of 18 Last printed 7/4/2013 2:24 PM VII Test Order Entry At the RGH and Pasqua sites, laboratory test orders must be data entered (accessioned) into the Laboratory Information System (LIS) before the blood specimen is collected by the phlebotomist. The patient identification will be confirmed at the time of collection using the SoftID electronic identification system. It is the responsibility of the client service area to ensure that requisitions for routine, timed and urgent blood tests are sent to the laboratory well in advance of the required time of collection. Requisitions should be in the laboratory no later than 2100 hours the day prior to collection to facilitate processing the AM blood work. Requisitions received after 2100 hours may not be entered in time for collection on the first A.M. collection run. Occasional exceptions may occur for critical care areas. Requisitions for blood work on new admission patients should be delivered to the lab. When this is not possible due to work load during the night shift, mark the requisition with “New Admission” and FAX it to the lab to be data entered into the LIS for the Morning Collection. The requisitions for next day collections are accessioned into the LIS throughout the day and evening. A daily log of patients entered into the LIS is printed each morning at 4:00 AM. This daily log is faxed to the nursing units so that they can confirm which requisitions have been sent to the lab for the AM Collection run (morning swarm). This daily log can be used to avoid sending duplicate requisitions for patient collection, thus avoiding patients being collected twice for the same order. Urines and Microbiology swabs will be entered into the LIS post-Collection. For STAT collections: 1. First - FAX all STAT requisitions to the Lab for data entry into the LIS. RGH FAX 766-4307 Pasqua FAX 766-2223 2. Second - Call the STAT phone number to notify the Phlebotomist of the STAT collection. RGH phone 766-1658 Pasqua phone 766-8412 The phlebotomist will always confirm that the STAT requisition has been faxed to lab for data entry into the Laboratory Information System. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 6 of 18 Last printed 7/4/2013 2:24 PM VIII Requisition Test Add-Ons or Changes Call the Laboratory, as indicated below, with any additions or changes to tests on a requisition that has already been sent to the laboratory. These additions must be data entered into the LIS before collection, if additional specimen tubes are required. At the RGH, For Add-On tests: BEFORE the specimen has been collected, call Accession at 4495 AFTER the specimen has been collected, call Chemistry at 4490, or Hematology at 4477 At the PASQUA, For ALL Add-On tests, call Chemistry at 2256. Tests Which May be Added On Chemistry tests can be added onto previous chemistry orders, in most circumstances. However, Ammonia and Blood Gases cannot be added on. Blood Cultures cannot be added onto previously collected test requests. Coagulation tests (INR, APTT, D-Dimer) cannot be added onto an order already collected. Previously collected Coagulation tubes may have a D-Dimer added, if collected within the last 4 hours. Hematology tests may be added onto a previously collected hematology EDTA tube within the last 24 hours. RQHR Lab Specimen Requirements – see link below http://www.rqhealth.ca/programs/lab/pdf_files/rqhr_lab_specimen_requirements.p df Use the SEARCH button to quickly find the test you are requesting. IX Specimen Requirements The type of specimen required for each test is listed in the Test Compendium. The Test Compendium is available for viewing on the RQHR Intranet and may be accessed from the Home Page by choosing “Departments”, then “Laboratory” and “RQHR Lab Specimen Requirements”. Use the SEARCH button to quickly find the required test. Detailed, pre-test preparation required for tests is listed in the appropriate section (laboratory department) of this manual. Take particular care to use the correct specimen container (e.g. stool collection container with SAF for parasite investigation). LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 7 of 18 Last printed 7/4/2013 2:24 PM X Specimen Collection 1. Client Identification Client identification must be confirmed using two client identifiers by all physicians and staff prior to the collection of all laboratory specimens. Client identification is a process that includes confirmation of at least two client identifiers through observation of documented identifiers, then requesting the client to recite their first and last name and date of birth when the client is able to participate in the identification process. Best practice for client identification is to actively involve the client. Two client identifiers include of the first and last name, and unique identifying number. The unique identifying number consists of the Health Services Number (HSN) or Medical Record Number (MRN). For Transfusions specimens also check the client’s date of birth as a third identifier. Confirm the client’s identity by checking the first and last name and the MRN (or HSN) on the requisition against the first and last name and MRN (or HSN) on the client’s armband. The client’s room or bed number may not be used as an identifier. Clients presenting to a Specimen Collection area without an armband, must present their pink form completed by SWADD or HSN card to confirm their first and last name and HSN. Ensure the identifiers match the corresponding identifiers on the requisition. WRC residents without an armband must be positively identified by a staff member who is familiar with the client. Identification must be documented by a signature of the identifier on the requisition prior to specimen collection. Requisitions signed only by the specimen collector will denote responsibility for both identification and specimen collection. 2. Typenex (Red) Arm bands A Typenex Red Arm band must be used when a group and antibody screen is ordered on a patient who is not staying in the hospital (pre-admission, outpatient transfusion, Emergency, Wascana Rehab Centre) or on a patient who may be transferred to another facility for diagnostic procedures. For instructions on using the Typenex Arm band, refer to the procedure LABTranOP7011Use of the Typenex Red Arm Band System found in the Transfusions section of this Manual. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 8 of 18 Last printed 7/4/2013 2:24 PM 3. Collection of Blood Specimens When drawing blood from indwelling line (e.g. arterial, PICC, Hickman, etc.), discard at least the first 7 ml of blood in the case of an adult and 3 ml of blood in the case of a child. It will often be contaminated with heparin, which will interfere with many analyses. To ensure that specimen integrity is maintained collect the specimen tubes in the following order: Blood cultures (Aerobic then Anaerobic) Blue top tube with citrate for coagulation (completely fill the tube) Serum tube with or without clot activator, with or without gelYellow Serum Separator Tube (SST) with gel, or Red top tube, or Orange Rapid Serum Tube (RST) Green top tube with heparin Mauve top tube with EDTA Tube with other additives (e.g. grey top tube) Gently invert all the tubes 5 times to mix the blood with the additives. To invert turn the filled tube upside-down and then return it to an upright position. When drawing blood using a winged collection set (e.g. butterfly), consideration must be given to the air space of the tubing when it is connected to an evacuated blood collection tube, as less blood will enter the evacuated tube than with the usual venipuncture technique. Prior to drawing the coagulation Blue top tube, a partially filled discard tube or a serum tube for other laboratory tests must be collected first. If blood is to be drawn into a syringe and transferred into a vacutainer tube, the transfer should occur immediately following phlebotomy. If there is a delay, the specimen will begin to clot or cellular elements will begin to separate from the plasma leading to erroneous results. Use the BD Blood Transfer Device (female luer adapter). Collect the blood into the syringe and ensure that the safety mechanism has been activated. Disconnect the syringe from the needle and discard the needle. Attach the Transfer Device to the syringe. With the syringe tip facing down, insert the vacutainer tubes into the transfer device. Allow the blood to transfer from the syringe to the tube using the tube’s vacuum. Do not depress the plunger of the syringe. Do not unthread syringe from the transfer device after use. Dispose of the syringe and transfer device as one piece in a sharps container. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 9 of 18 Last printed 7/4/2013 2:24 PM 4. Specimen Labelling Do not pre-label the tubes. Label all specimens in the immediate presence of the client at the time of collection. a) Blood samples: Label tubes from the armband / requisition with the client’s first and last name and the MRN (or HSN). Specimens for crossmatches, group and reserve serum or group and Rh must also be labelled with the client’s date of birth and the date of collection. The signature of the person collecting the specimen, and the date and time of collection must be recorded on each requisition available at the time of collection. For Pink Transfusion requisitions, the person performing the phlebotomy MUST sign the requisition with the date and time of collection. Record on the requisition if the specimen was collected from a “line”. b) Cord blood specimens: Label cord blood gases with the mother’s last name and the mother’s MRN. Label cord blood specimens with the baby’s last name and the baby’s MRN. Record the date and time of collection on the requisition. c) Blood gases, urines, swabs, blood cultures, stools and body fluids are collected in containers that do not lend themselves to easy labelling. These specimens will be accepted if labelled with the numbered tear-off requisition label and the client’s first and last name and MRN is recorded on the label. Record the date and time of collection and the initials of the person collecting the specimen on the requisition. d) Tissue specimens for histology examination must be labelled with name of client, MRN, HSN, surgeon, nursing unit, nature of specimen and date of surgery. Indicate nature of specimen on Cytopathology and Histopathology requisitions. Cytopathology and Histopathology requisitions MUST be legibly signed by physician performing procedure. XI Transporting Specimens to the Lab All laboratory specimens and containers should be considered contaminated. Ensure that all containers with screw on lids have the lid placed on securely. Biohazard bags are not necessary for transport of specimens; however, personal protective equipment must be used (i.e. gloves). Gross contamination of specimen containers must be removed prior to transport (i.e. wipe visible contamination from specimen container with cotton ball soaked in 0.5% hypochlorite solution or Virox 5 working solution or use an alcohol swab). For further information concerning the delivery of specimens to the laboratory, refer to the appendix for LABRegOP7109 Instructions for Portering Laboratory Specimens. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 10 of 18 Last printed 7/4/2013 2:24 PM XII Specimen Rejection Specimens that are not labelled correctly will be assessed according to the Lab Services Specimen Rejection protocol. The specimen may be rejected and a repeat draw requested. This decision is made based on the type of error, the nature of the specimen, and the degree of difficulty in obtaining a repeat specimen. XIII Laboratory Information System Laboratory Services has a Laboratory Information System (LIS) in place. The LIS is a vital component to laboratory consolidation in the city of Regina and allows Laboratory Services to centralise clinical pathology at the Regina General Hospital and anatomic pathology at the Pasqua Hospital. The LIS is being implemented in the RQHR rural laboratories, beginning with Moosomin and Indian Head. The use of bar code labels reduces the risk of specimen identification errors. The process of ordering laboratory tests is simplified through the use of standardized requisitions that combine many tests into fewer forms. The Regina General Hospital and Pasqua Hospital laboratories are fully computerized. Specimens referred to either site from the community, centres outside of Regina, or other hospitals will be processed in a computerised environment. Therefore, standardized requisitions should be used to order tests and users can expect to see test results on computer generated reports. Many physicians in RQHR are receiving laboratory results by EMR (Electronic Medical Record). Glossary of Terms LIS - Laboratory Information System Accession - the process whereby an order is entered into the laboratory computer system and assigned an Order Number. This is a function performed by laboratory staff. The Order Number will appear on reports. MRN / HIN - clients are given a seven digit Hospital Identification Number (HIN) when they enter a hospital in the Regina Qu’Appelle Health Region. In the LIS, all references to the HIN are noted as MRN (Medical Record Number). These terms are used interchangeably. Stay Number - is an eight-digit number generated by RQHR hospital computer systems (Admission/Discharge/Transfer systems) and is unique to each client stay in the hospital. Interim Report - contains partial results from a single order. Biochemistry/Haematology reports will be flagged in the top right-hand corner as LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 11 of 18 Last printed 7/4/2013 2:24 PM “INTERIM”. In the case of Microbiology reports, each individual test result will be identified as “INTERIM” or “FINAL”. Final Report - contains all results from a single order. It contains all of the information that has been previously reported on an Interim Report. It is flagged with “FINAL” in the top right-hand corner of the report. All new results that have not previously been reported will be flagged with an asterisk (*). HSN – is a nine digit Provincial Health Services Number XIV Results Reporting Printers are in place on most nursing units at the Regina General Hospital, Pasqua Hospital, Wascana Rehabilitation Centre and some physician offices. Results print directly to the nursing unit in these locations. Any location not having a printer will have reports delivered via the Mail Messenger service or pneumatic tube system. Results from STAT, Urgent and Routine requests print as soon as they are available. 1. Biochemistry/Haematology Report Biochemistry and Haematology results are combined on the same report. The reference range for each test will be shown in the right-hand column of the report. The range shown is appropriate for the age and sex of the client. Abnormal results are flagged with abnormal codes such as “C”, “L” or “H”. A key at the bottom of the report explains each code. 2. Microbiology Report When a specimen culture yields a pathogenic organism, a list of antibiotics to which the organism is sensitive is recorded at the bottom of the report. Note: The recommended dosage shown will not necessarily be appropriate to the client’s age. The dosage shown will always be a standard adult dosage. Adjustments must be made for other age groups. Each individual test on a Microbiology report will be flagged as “interim” or “Final”. 3. Transfusion Report Transfusion Reports are cumulative in nature for a given order. A list of blood products which are available, issued or transfused is recorded. A pink slip of paper called a “Transfusion Record” is issued with each blood product. The Record is permanently filed in the client’s Health Record by attaching it to a “Laboratory Reports” form. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 12 of 18 Last printed 7/4/2013 2:24 PM XV Types of Reports The LIS prints the following four types of reports; Interim, Final, Cumulative and Discharge Report. The type of report will be indicated in the top-right corner of the report. Interim - contains partial results of an order. It can be discarded when the Final Report is received. Final - contains all results for an order (except tests referred to Sask. Disease Control Laboratory). Results not previously printed are flagged with an asterisk (*). Cumulative Report - available upon request only. This is a report, which is formatted in four columns containing results of the last four orders on a client. Discharge Report - prints upon discharge. This report prints in Health Records only and is a summary of all Chemistry and Haematology tests done during a client stay. New results obtained after discharge will be reported and sent to the physician and Health Records on a report called “New Results After Discharge”. XVI Requests For Results Laboratory test results are printed as soon as available. Check the “Lab Results Viewer” if available. Do not phone for results unless there is an unusual delay in receiving a report. When it is necessary to phone for: clinical pathology (Chemistry, Haematology, Microbiology, Transfusions) results call the Inquiry Centre at local 4915 anatomic pathology results call local 2245 XVII Availability of Tests “After Hours” The laboratory is staffed continuously seven days a week. The staff covering the period 1600 - 0015 hours is considerably fewer in number than the daytime staff and after 0015 hours only two technologists are on duty. IT IS IN EVERYONE'S INTEREST TO RESTRICT TESTING AFTER HOURS TO ESSENTIAL WORK ONLY. Clinicians gain by getting improved turn round times on urgent tests; the laboratory gains by increased efficiency. There is a list of tests, which are available on a 24-hour basis. Several points should be noted when ordering tests from this list during the evening and night shifts. 1. The tests listed should only be used when the performance is necessary for the diagnosis or therapy at the time the request is made. 2. From time to time there may be an urgent need for tests not on the list. When this is the case, the clinician in charge should phone the pathologist or professional on call for the relevant laboratory section. If the test is LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 13 of 18 Last printed 7/4/2013 2:24 PM needed and can be performed he/she will then authorize the technologist to perform the test. It will be understood that this provision must be used sparingly. The name and pager number for the individual on call can be obtained from laboratory staff. 3. When it is possible to predict that an esoteric test will be required out-ofhours, advance warning should be given to the professional head of the laboratory division concerned. XVIII Laboratory Tests Available On 24-Hour Basis A. Chemistry Refer to “CHEMISTRY TESTS” in the appendix for 24 hr. test availability. B. Hematology Refer to “GUIDELINES FOR EXPECTED TURN AROUND TIMES IN HEMATOLOGY” in the appendix for 24 hr test availability. C. Transfusions 1. 2. D. Microbiology 1. 2. XIX Group and screens Direct antiglobulin test Stat Gram stain and culture of the following: - all aspirated fluids including CSF - all tissues - other specimens on physician’s request Collection of blood cultures Turn Around Time (TAT) TAT for the purpose of this document and unless otherwise indicated is defined as the interval between the time the specimen is collected by phlebotomy to reporting of the test result. Lab services will strive to meet this target for at least 90% of STAT orders. The reader must be aware that circumstances will occasionally arise that will limit the ability to meet these deadlines i.e. equipment failure, excessive volume of STAT orders, limited staff coverage on certain shifts. The expected Turn Around Times for the Chemistry, Hematology, Microbiology and Transfusions departments are listed in the appendix to this procedure. These TAT are for in hospital clients. For clinic or referred in specimens, the routine TAT is 24-72 hours. LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 14 of 18 Last printed 7/4/2013 2:24 PM XX Critical Values When results fall within ranges identified as “Critical”, laboratory staff will telephone verified results to the nurse on the unit concerned or to the physician, or in the case of out-patient or referred-in specimens to the clinic or physician’s office to communicate the results. A statement will be made to the effect that the result is seriously abnormal and that the attending physician should be notified immediately. Each critical value communicated verbally or by phone will be verified by having the listener read back each result to confirm the accuracy of the transmission. When critical results are sent electronically through the LIS or by FAX, the laboratory will telephone to confirm receipt of the critical result. For critical values listed by department, please refer to the appendix. XXI Laboratory Abbreviations When ordering laboratory tests, use accepted abbreviations only or, if in doubt, write the name out in full. Refer to the following list of abbreviations: a1AT ABO ACTH ADH AFB AFP AGBMAb ALA ALG AMA ANA Anti-HB Anti-HC ASMA AS0 or ASOT ATP BCG HCG BT CBC CEA CO2 CK CMV CRP C&S CSF CT CVI DAT Alpha-1-Antitrypsin Main blood group system Adrenocorticotrophic hormone Antidiuretic hormone Acid fast bacilli Alpha-fetoprotein Antiglomerular Basement Membrane Antibodies Amino levulinic acid Anti-lymphocyte globulin Antimitochondrial Antibodies Anti-nuclear antibody Hepatitis B Antibody Hepatitis C Antibody Antismooth Muscle Antibodies Antistreptolysin "O" Adenosine triphosphate Bacilli- Calmette Guerin Vaccine Beta Human Chorionic Gonadotropin (serum or urine) Bleeding Time Complete Blood Count Carcinoembryonic Antigen Carbon Dioxide Content Creatine Kinase (Enzyme) Cytomegalovirus C-Reactive Protein Culture and Sensitivity Cerebrospinal Fluid Clotting Time Cell Volume Index Direct Antiglobulin Test LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 15 of 18 Last printed 7/4/2013 2:24 PM Diff DNA ECF ECHO EDTA ERA ESR FBS FSH FTA-ABS FVIIIR:Ag GC GFR GGT G-6-PD GSM GTT Hct Hb or Hgb HbF HBsAg HBcAg HBeAg HGH 5-HIAA Hp IFE IgA IgD IgE IgG IgM IVIgG K 17-KS 17-KGS L LDH LE LH MCD MCH MCHC MCT MCV MPV N Na 02 OPL Differential Deoxyribonucleic Acid Extra Cellular Fluid Enteric Cytopathogenic Orphan (Virus) Ethylene-diamine tetra acetate (anticoagulant for blood specimens) Estradiol receptor assay Erythrocyte Sedimentation Rate Fasting Blood Sugar Follicle Stimulating Hormone Fluorescent Treponemal Antibody Absorption Test Factor VIII Related Antigen Gonococcus (N. gonorrhoeae) Glomerular Filtration Rate Gamma Glutamyl Transferase Glucose-6-phosphate dehydrogenase Group and Screen Crossmatch Glucose Tolerance Test Hematocrit Haemoglobin Haemoglobin F Hepatitis B Surface Antigen Hepatitis B Core Antigen Hepatitis B Envelope Antigen Human growth hormone 5-Hydroxyindole Acetic Acid Haptoglobin Immunofixation electrophoresis Immunoglobulin A Immunoglobulin D Immunoglobulin E Immunoglobulin G Immunoglobulin M Intravenous Immune Globulin Potassium 17-Ketosteroids 17-Ketogenic steroids Litre Lactate Dehydrogenase Lupus Erythematosus Luteinizing Hormone Mean Cell Diameter Mean Corpuscular Haemoglobin Mean Corpuscular Haemoglobin Concentration Mean Cell Thickness Mean Corpuscular Volume Mean Platelet Volume Nitrogen Sodium Oxygen Out-Client Live LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 16 of 18 Last printed 7/4/2013 2:24 PM OPS OT PCV PCO2 PE pH PKU Plt PO2 PPL0 PSA PT PTH PTT or APTT RA Factor RDW RF RBC Rh RNA RSV RST AST (SGOT) ALT (SGPT) Sp.Gr. SED OR ESR SST TBG TIBC Tr TRH TSH TPI TT TWBC VDRL VMA WBC WR Out-Client Specimen Old Tuberculin Packed Cell Volume Partial Pressure Carbon Dioxide Protein Electrophoresis Hydrogen Ion Concentration Phenylketonuria Platelets Partial Pressure Oxygen Pleuropneumonia-like Organism Prostate Specific Antigen Prothrombin Time Parathyroid Hormone Partial Thromboplastin Time Rheumatoid Arthritis Factor Red Cell Distribution Width Rheumatoid Factor Red Blood Cell Count Rhesus Factor Ribonucleic Acid Respiratory Syncitial Virus Rapid Serum Tube (orange top blood collection tube) Glutamic Oxalacetic Transaminase Glutamic Pyruvate Transaminase Specific Gravity Erythrocyte Sedimentation Rate Serum Separator Tube (yellow top tube containing gel) Thyroxine-binding Globulin Total Iron Binding Capacity Transferrin Thyrotrophin Releasing Hormone Thyroid Stimulating Hormone Treponema Pallidum Immobilization Thrombin Time Total White Blood Count Flocculation Test for Syphilis Vanillylmandelic Acid White Blood Cell Count Wasserman Reaction Related documents 1. 2. 3. 4. LABRegOP2109 Review and Distribution of Lab Services Manual LABRegOP7950 Laboratory Services Manual for Physician Offices LABRegOP3651 Triage and Treatment Manual LABPhlbOP7017 Protocol for Performing a Venipuncture Appendixes LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 17 of 18 Last printed 7/4/2013 2:24 PM 1. LABRegOP7109 Laboratory Specimen Portering Competency 2. LABRegOP7109A1 Instructions for Portering Laboratory Specimens 3. LABRegOP7109A2 Portering Laboratory Specimens Competency Quiz 4. LABRegOP7109A3 Portering Laboratory Specimens Competency Quiz Answers 5. LABPhlbOP7009A1.2 Sending Patient Specimens using the Pneumatic Tube 6. LABChemOP8200T1 Chemistry Critical Values 7. LABHemaOP7019T1 Hematology Critical Values 8. LABMicOP8000A1 Microbiology Critical Values 9. LABTranOP7001W3 Transfusions Critical Values 10. LABHistOP1000T1 Anatomic Pathology Critical Results 11. LABCytoOP7047 Communication and Documentation of Cytopathology Critical Results 12. LABRlabOP7900A2 Rural Laboratories Critical Results 13. LABChemOP8202C1 Chemistry Tests (Tests, Turn Around Times, 24 hr Availability and testing site) 14. LABHemaOP7031C1 Guidelines for Expected Turn Around Times in Hematology (Tests, Turn Around Times, 24 hr Availability and testing site) 15. LABMicOP8000A2 Anticipated Turn Around Times for Microbiology Tests 16. LABTranOP7001W2 Turn Around Time (TAT) for Transfusions 17. LABRlabOP7900A3 Tests Performed by Rural Laboratories Revision History Found in SoftTech Health Lab QMS™ Document Management System Author J. Hill, MLT, ART L. Engel MLT revised LABRegOP7900.3.4 LABORATORY SERVICES MANUAL GENERAL INFORMATIO Laboratory Services Regina QuAppelle Health Region Page 18 of 18 Last printed 7/4/2013 2:24 PM Subject/Title: LABRegOP7109.1.1 Laboratory Specimen Portering Competency Last Approved Time: 4/6/2010 11:40:41 AM Revision: 1.1 Approving Authority and Contact for Interpretation: Assistant Manager Laboratory Services Regulatory Affairs Phone: (306) 766-4470 Current Version on Print Date Policy Process Control Purpose This procedure provides instruction for competency assessment of portering staff members who are transporting patient specimens to the laboratory. All RQHR staff that transport patient specimens to the laboratory must read the instruction sheets for Portering Specimens and Sending Patient Samples using the Pneumatic Tube, then complete the quiz. Procedure STEP 1. 2. 3. ACTION Read LABRegOP7109A1 Instructions for Portering Laboratory Specimens Read LABPhlbOP7009A1 Sending Patient Samples in Using the Pneumatic Tube Complete LABRegOP7109A2 Portering Laboratory Specimens Competency Quiz using the e-Quiz function of the Intranet. Log onto RQHR Intranet e-Quiz/Attendance. Related documents 1. 2. LABPhlbOP7009 Operation of Pneumatic Tube LABPhlbOP7009A1 Sending Patient Samples Using the Pneumatic Tube Appendixes (charts, form, job aids, labels, logs, tables, tags, worksheets) 1. 2. 3. LABRegOP7109 A1 Instructions for Portering Laboratory Specimens LABRegOP7109 A2 Portering Laboratory Specimens Competency Quiz LABRegOP7109 A3 Portering Laboratory Specimens Competency Quiz Answers LABRegOP7109.1.1 Laboratory Specimen Portering Competency Laboratory Services Regina Qu'Appelle Health Region Page 1 of 2 Last printed 4/6/2010 11:40 AM Revision History Found in Softtech Health Lab QMS™ Document Management System Author Marsh, Virginia, MLT, CAdmin, CCE Page 2 of 2 Last printed 4/6/2010 11:40 AM Instructions for Portering Laboratory Specimens Proper transportation of laboratory specimens is a vital link in providing RQHR patients with timely accurate test results. This document provides instruction on the safe transportation of laboratory specimens from the various departments and wards to the laboratory. Precautions Confidentiality of patient information on specimens must be maintained during transport. (i.e. name should not be visible) All laboratory specimens and containers are considered contaminated. Prior to transport ensure that all specimen containers with screw tops and caps are securely fastened to prevent leaking. Grossly contaminated specimen containers or requisitions should not be accepted for transport. Gloves (personal protective equipment) must be worn to deliver laboratory specimens. Use Isagel or wash hands after removal of gloves. Transport Transport patient specimens directly to the laboratory. Refer to the Lab Services Manual for specific specimen transport storage and time requirements. Drop off all laboratory specimens at the Accession counter. Exceptions include: o Blood gas specimens should be delivered directly to the chemistry department and a technologist notified of their arrival. o Pathology specimens which are delivered to the Histopathology / Cytology department. o STAT specimens physically handed over to a person within the laboratory. Transport via pneumatic tube following the instructions Sending Patient Samples Using the Pneumatic Tube. All specimens must be accompanied by an appropriately completed requisition. LABRegOP7109A1.1.2 Instructions for Portering Lab Specimens Laboratory Services Regina Qu'Appelle Health Region Page 1 of 2 Last printed 7/4/2013 9:27 AM After Hours RGH - After day shift hours, deliver specimens to the Accession desk in Laboratory Services. If you do not have card access and the lab staff are unavailable, the Pass-Through specimen box will be unlocked to enable specimen drop off. Pasqua - After day shift hours, continue to deliver specimens to the Accession desk in Laboratory Services. If you do not have card access and the lab staff are unavailable, please call 2256 or 2200. Or if you need to contact the lab staff STAT please page 2564 or 4803. RQHR staff that frequent the lab, are encouraged to obtain card access. Transport via pneumatic tube following the instructions LABPhlbOP7009A1.2 Sending Patient Specimens using the Pneumatic Tube. Compromised Specimens When a laboratory specimen is dropped and broken, or damaged during transport: o Alert the next RQHR Employee passing by to contact housekeeping. Do not leave the damaged specimen unattended. o Immediately notify the department or ward to recollect the specimen. o Fill out an Employee Report of Incident/Hazard and an Incident Investigation with your supervisor. Submit to Employee Health. Note: It is important for laboratory specimens to be delivered in a timely manner to ensure specimen integrity, viability and prompt turn around times. LABRegOP7109A1.1.2 Instructions for Portering Lab Specimens Laboratory Services Regina Qu'Appelle Health Region Page 2 of 2 Last printed 7/4/2013 9:27 AM Portering Laboratory Specimens Competency Quiz Name: __________________________ Contact Number: _____________________ 1. Are gloves required to transport patient specimens to the laboratory? a. Yes b. No 2. What is the importance of delivering patient specimens directly to the laboratory? a. Assurance of specimen integrity and viability. b. Prompt turn around times of testing results. c. Ensure specimens are not misplaced and confidentiality compromised. d. Biohazard material is not accessible in public or designated clean areas. e. All of the above. 3. Where are patient specimens delivered during the day shift? a. Accession area of the laboratory, except Blood gases, Pathology and STAT specimens. b. To the Out-patient collection laboratory. 4. Is it acceptable practice to leave patient specimens in public areas such as hallways, elevator foyers, waiting rooms, etc? a. No b. Yes 5. If a patient specimen is dropped, broken and spilled on route to the laboratory, what should be done? a. Carry on with your deliveries, leaving the broken specimen in the corridor. b. Alert the next RQHR Employee passing by to contact housekeeping. Do not leave the damaged specimen unattended. Immediately notify the department or ward to recollect the specimen. c. Recover the specimen remains and deliver to the laboratory. LABRegOP7109A2.1.2 Portering Lab Specimens Competency Quiz Laboratory Services Regina Qu'Appelle Health Region Page 1 of 1 Last printed 7/4/2013 9:27 AM Portering Laboratory Specimens Competency Quiz Answers 1. Are gloves required to transport patient specimens to the laboratory? a. Yes Rational: All laboratory specimens and containers are considered a potential source of infection. 2. What is the importance of delivering patient specimens directly to the laboratory? a. Assurance of specimen integrity and viability. b. Prompt turn around times of testing results. c. Ensure specimens are not misplaced and confidentiality compromised. d. Biohazard material is not accessible in public or designated clean areas. e. All of the above. Rational: Patient specimens must be delivered promptly to the laboratory to ensure specimens do not deteriorate. The accuracy of the patient test results depends on the specimen reliability. 3. Where are patient specimens delivered during the day shift? a. Accession area of the laboratory, except Blood gases, Pathology and STAT specimens. Rational: It is important to deliver laboratory specimens to the appropriate receiving area, so that specimens are not misplaced or lost. STAT specimens should be physically handed to a person in the laboratory to allow priority processing. 4. Is it acceptable practice to leave patient specimens in public areas such as hallways, elevator foyers, waiting rooms, etc? a. No Rational: It is unacceptable to leave patient specimens in public areas due to considerations such as: breach of confidentiality, accessible biohazardous material, and misplaced or lost specimens. LABRegOP7109A3.1.2 Portering Lab Specimens Competency Quiz Answers Laboratory Services Regina Qu'Appelle Health Region Page 1 of 2 Last printed 7/4/2013 9:28 AM 5. If a patient specimen is dropped, broken and spilled on route to the laboratory, what should be done? b. Alert the next RQHR Employee passing by to contact housekeeping. Do not leave the damaged specimen unattended. Immediately notify the department or ward to recollect the specimen. Rational: To ensure patient, staff and visitor safety, it would be unacceptable to leave the biohazardous spill unattended. Safe work practices would be ensured by contacting appropriately trained staff with safety equipment specific to the task to clean up a biohazardous spill. LABRegOP7109A3.1.2 Portering Lab Specimens Competency Quiz Answers Laboratory Services Regina Qu'Appelle Health Region Page 2 of 2 Last printed 7/4/2013 9:28 AM Subject/Title: LABChemOP8200T1.3.2 Chemistry Critical Values Last Approved Time: 1/6/2014 2:32:50 PM Revision: 3.2 Approving Authority: Medical Biochemist Contact for Information: Chemistry Phone: (306) 766-4490 Current Version on Print Date CHEMISTRY CRITICAL VALUES TEST (Blood) Sodium Potassium Potassium (newborn) Bicarbonate Calcium (total – check corrected value) Glucose Glucose (newborn) Magnesium Phosphorus Iron (< 14 years) pH pCO2 pO2 Acetaminophen Amikacin LOW HIGH UNITS 120 2.8 2.5 10 1.8 155 6.0 7.0 2.2 1.7 <0.50 0.30 25 17 > 2.10 7.20 20 40 Carbamazepine Digoxin Gentamicin Lithium Phenytoin Phenobarbital Salicylate Theophylline Tobramycin Vancomycin HIV Hepatitis C Antibody LABChemOP8200T1.3.2 Chemistry Critical Values Laboratory Services Regina QuAppelle Health Region 3.0 > 50.0 7.60 70 600 >10 mg/L (Pre) >30 mg/L (Post) 63 ≥ 3.0 ≥ 2.0 (Pre) ≥ 15.0 (Post) ≥ 2.0 ≥ 119 ≥ 200 2.3 >110 ≥ 2.0 (Pre) ≥ 15.0 (Post) ≥ 21.0 (Pre) ≥ 60.0 (Post) Reactive* Reactive* mmol/L mmol/L mmol/L mmol/L mmol/L mmol/L mmol/L mmol/L mmol/L umol/L mmHg mmHg umol/L mg/L umol/L nmol/L mg/L mmol/L umol/L umol/L mmol/L umol/L mg/L mg/L Hepatitis B Surface Antigen HTLV Reactive* Reactive* *Indicate to ward that sample is being referred to SDCL for confirmation LABChemOP8200T1.3.2 Chemistry Critical Values Laboratory Services Regina QuAppelle Health Region LABChemOP8200T1 Chemistry Critical Results Laboratory Services, Regina Qu’Appelle Health Region Page 2 of 2 Last printed 1/6/2014 2:32 PM JOB AID LABHemaOP7019T1 HEMATOLOGY CRITICAL VALUES Any critical/ urgent value where the Physician can not be notified must be paged to the Hematologist on call and an occurrence report initiated. (Refer to the time notification for paging Hematologist) Any new critical finding must have a HEMR ordered and a slide sent to the Hematologist on a separate tray Test Name Critical Value Alert/Urgent Value (called to the Physician immediately) (Physician notified within 24 hours) Platelet ≤ 20 x 109 /L (new case) ≤ 50 x 109 /L (out-patient/community) ≤ 70 x 109 /L (patient bleeding) ≤ 100 x 109 /L PAC, DS, DAS ≤ 100 x 109 /L (neo) Hemoglobin ≤ 60 g/L (new case) ≥ 200 g/L adult male ≥ 220 g/L (new born) ≥ 180 g/L adult female ≤ 90 g /L PAC, DS, DAS Malaria Positive WBC ≥ 30 x 109 /L (inpatients-new case) ≤ 1.5 x 109 /L (new case) Monotest Positive: if reflexed from lab PT INR > 6.0 PTT ≥ 100 sec. Fibrinogen ≤ 1.0 g/L D-Dimer CSF ≥ 20 x 109 /L outpatients ≥ 5000 μg/L ASAP INR ≥ 1.5 pre-op patients or first time on none ASAP ≥ 39 sec pre-op patients or first time on none Call all Referred In D-Dimers-(including Rural labs: G, H, I, J, L, M, and N Depots) TNC ≥ 10 Any test result that the technologist feels is significant should be called Test Name Abnormal blood films Brown Plasma Critical Value (Notify the Hematologist on call immediately) 1. New Leukemia 2. Schistocytes-Any with platelets ≤ 50 x 109 /L and/or hgb drop ≥ 30 g/L (except hemodialysis patients) 3. Spherocytes- 2 + with anemia-new case 4. Sickle cells-Any new case 5. Positive Malaria When plasma sample has severe hemolysis (not from difficult poke) Order: CBC, scan, Hemr, renal, & liver panel, LD, plasma hgb, methemalbumin, PT, PTT, Fib, DDimer and DAT-if not done previously within 6 hr. Kleihauer Urgent Value (Hematologist notified within 24 hrs) 1. Marked Rouleaux- new or significant change. 2. 3+ Agglutination - new. 3. ANEUT ≤ 0.5 x 109 /L (first time) Positive with an actual ml bleed (Blood Bank notified ASAP) Note: New Leukemias-First time Blasts(add comment: refer to Hematologist’s review for verification) Fluid/CSF cell counts and differentials should be called to physician/ward when the LIS is down. LABHemaOP7019T1 Hematology Critical Values Laboratory Services Regina QuAppelle Health Region Page 1 of 1 Last printed 7/4/2013 9:26 AM LABMicOP8000.A.1.6 Microbiology Critical Values~~000010012.doc Microbiology Critical and Significant Values When results fall within "Critical" ranges, results should be verified, and then within 1 hour the Ward, or Physician concerned must be notified. This notification may be a phone call, with read back, followed by a hard copy of the report sent to their printer, or it may be a phone call notifying them you are sending a report, followed by confirmation that they have received the report. All calls must be documented. The following are considered Critical Values in Microbiology: Gram Smears Cultures Test Critical Value Notification to: Blood Culture Any new positive on In Patients or Emergency Patients. Immediate call & send report to appropriate ward. CSF Any positive Gram smear. Immediate call & send report to appropriate ward. STAT All Gram smear results. Immediate call & send report to appropriate ward. OR specimens All Gram smear results if marked STAT Any positive Gram smear CSF culture Any new positive result. Group A Streptococcus isolated from sterile sites, patients with history of necrotising fascitis, and/or deep wounds. Any new positive result. Sterile body fluids and tissue specimens E. coli 0157 LABMicOP8000.A.1 Microbiology Critical Values Laboratory Services Regina Qu'Appelle Health Region Any new positive result. Page 1 of 3 Last printed 6/11/2013 2:52 PM Immediate call & send report to appropriate OR. Immediate call & send report to appropriate ward. Immediate call & send report to Public Health (Regina 766-7789). After Hours call MHO on call. Regina 766-7773 Other Health Regions – refer to call list. Immediate call & send report to Infection Control for isolates from In Patients, Nursing Homes, and WRC. LABMicOP8000.A.1.6 Microbiology Critical Values~~000010012.doc When results fall within “Significant” ranges, the Ward, Clinic, or Physician concerned should be notified. Depending on the specimen and the result, notification may require a phone call or it may just be the electronic sending of the report. Notification should occur within that day. All calls must be documented. The following are considered Significant Values in Microbiology: Gram Smears Calcofluor White AFB Smears Test Protocol Blood Culture Call & send report for any new positive on patients from Referred In or Clinics. Sterile body fluids and tissues (NOT STAT or OR) Just send results, no call required. Pneumocystis Positive Just send results, no call required. Acid fast bacilli seen on initial smear. Call & send report of new positives to Ward / Clinic, & Infection Control. Call SDCL to notify them that a positive is coming. Tech 2’s will send electronic report during regular hours to Public Health. Immediate call & send report to Infection Control Clostridium difficile New positives Toxin Positive (regardless of method) In Patient (including Rural), Emerg., Nursing Home, - Call & send report to Ward, & Infection Control. Out Patient or Clinic: Just send results to location. No calls required. Public Health does not need to be notified. Non-culture Influenzae Screen Positive RSV Positive Norovirus Positive Mycology Growth of dimorphic or pathogenic fungi (Blastomyces, Coccidiodes, Histoplasma, Paracoccidioides). Call & send report of new positives to Ward. If In patient notify Infection Control. Tech 2’s will send electronic report during regular hours to Public Health. (Public Health does not need to be notified about positive RSV’s) Call & send interim report on new positives to Ward, & Notify Microbiologist. Dialysis Waters Call & send report to Clinical Engineering for any positive result that falls outside the acceptable limits for Dialysis Waters. Laboratory Waters No action required. Water sterility LABMicOP8000.A.1 Microbiology Critical Values Laboratory Services Regina Qu'Appelle Health Region Page 2 of 3 Last printed 6/11/2013 2:52 PM LABMicOP8000.A.1.6 Microbiology Critical Values~~000010012.doc Test Bioterrorism Agent Blood culture growth report Body fluid, & Tissues Enteric Pathogens (Campylobacter sp., Salmonella, Shigella, Yersinia, Aeromonas, Plesiomonas , Vibrio cholerae). Listeria MRSA Screen Positive VRE Screen Positive ESBL Positive Organism Cultures Neisseria gonorrhoeae Neisseria meningitidis (sterile site) Protocol Call all confirmed or highly suspicious organisms to Ward or Clinic, SDCL, & Infection Control. Just send results, no call required. Just send results, no call required. Call & send report of new positives to Ward / Clinic. If In patient notify Infection Control. Tech 2’s will send electronic report during regular hours to Public Health. Just send results, no call required. Interim reports on new RQHR In patient positive – Call & send report to Ward. If In patient notify Infection Control. If Out Patient no notification required. Final reports - Just send results, no calls required. Tech 2’s will send electronic report during regular hours to Public Health. (Only notify Public Health of ESBL from sterile sites) Send report of new positives to Ward / Clinic if isolate is from non-genital source. If genital culture, no call required. Tech 2’s will send electronic report during regular hours to Public Health. NEVER notify Infection Control Immediate call & send report to Public Health (Regina 766-7789). After Hours call MHO on call. Regina 766-7773 Other Health Regions – refer to call list. Immediate call & send report to Infection Control for isolates from In Patients, Nursing Homes, and WRC. Tech 2’s will send electronic report during regular hours to Public Health. Streptococcus agalactiae (Group B) Isolated from children <4weeks of age Parasitology Positive for: Amoebiasis, Cryptosporidia Entamoeba histolytica Giardia, Cyclospora LABMicOP8000.A.1 Microbiology Critical Values Laboratory Services Regina Qu'Appelle Health Region Immediate call & send report to Infection Control for isolates from In Patients, Nursing Homes, and WRC. Tech 2’s will send electronic report during regular hours to Public Health. Send printed report to Infection Control for isolates from In Patients, Nursing Homes, and WRC. Page 3 of 3 Last printed 6/11/2013 2:52 PM LABTranOP7001W3 Transfusions Critical Values Undue delay in filling crossmatch request for any reason. Inability to crossmatch with compatible blood. Inability to procure blood or blood products LABTranOP7001W3 Transfusion Critical Values Laboratory Services Regina Qu'Appelle Health Region Page 1 of 1 Last printed 5/7/2010 4:25 PM ANATOMIC PATHOLOGY CRITICAL RESULTS Significant or unexpected surgical pathology findings are to be promptly communicated to the patient’s physician by telephone. Documentation of the date and time of notification and name of the recipient of the notification are to be included in the pathology report. Significant or unexpected surgical pathology findings include but are not limited to the following: 1. Malignancy in an uncommon location or specimen type (e.g. hernia sac, intervertebral disk material, tonsil, etc.). 2. Absence of chorionic villi when clinically expected (potential ectopic pregnancy). 3. Change of a frozen section diagnosis after review of permanent sections. 4. Mycobacterial, fungal or other significant organisms identified on special stains. The pathologist will document the name of the physician notified and the date and time of the call on the surgical report. LABHistOP1000T1.1.2 Anatomic Pathology Critical Results Laboratory Services Regina Qu'Appelle Health Region Page 1 of 1 Last printed 11/06/2013 2:50 PM Subject/Title: LABCytoOP7047 Communication and Documentation of Cytopathology Critical Results Last Approved Time: 10/15/2012 10:01:01 AM Revision: 1 Approving Authority: Cytopathologist Phone: (306) 766-2641 Contact for Interpretation: Cytology Current Version on Print Date Policy Process Control Purpose There are certain cytopathology diagnoses that may be considered particularly significant and unexpected. There are no consensus guidelines developed on Critical Values in cytology, so we will address the type of cases that the RQHR Cytopathology Department has designated as Critical Results. It is important to have prompt communication and documentation of these particular diagnoses. Procedure Cytology Critical Value (CV) cases: Bacteria or fungi in cerebrospinal fluid Pneumocystis, fungi, or viral cytopathic changes in BAL, wash, or brush Bacteria in FNA Fungi in FNA Acid-fast bacilli in any specimen Completely unexpected malignancy (malignancy in a fluid with a negative history and no clinical suspicion) Malignancy (suspected or not) in critical places (sup.vena cava synd., risk of spinal cord injury) 1. The Cytotechnologist screening the case, will identify the Critical Result and will take it immediately to the pathologist reporting the case. 2. The pathologist will promptly communicate the significant or unexpected findings to the patient’s physician or other clinical personnel responsible for patient care by telephone. 3. The pathologist will document the date and time of notification and name of the recipient of the notification on the cytology report. 4. If after 3 tries, a physician cannot be reached by telephone, the report will be faxed to the physician / ward within 24 hours. LABCytoOP7047 Communication and Documentation of Cytopathology Critical Results Laboratory Services Regina QuAppelle Health Region Page 1 of 2 Last printed 10/15/2012 10:01 AM References Diagnostic Cytopathology, Vol 34, No 6, “Critical Values in Cytology” Related documents RQHR Quality Manual, LABRegOP8101 Timely Communication of Critical Values and New Diagnosis LABRegOP7900 Laboratory Services Manual General Information Appendixes (charts, form, job aids, labels, logs, tables, tags, worksheets) Revision History Found in SoftTech Health Lab QMS™ Document Management System Author Ronald Angeles, MD, FRCPC, PATHOLOGIST, L. Kozak, MLT Page 2 of 2 Last printed 10/15/2012 10:01 AM RURAL LAB CRITICAL RESULTS CHEMISTRY TEST (Blood) Sodium Potassium Potassium (newborn) Bicarbonate Bilirubin (newborn) Calcium (total – check corrected value) Glucose Glucose (newborn) Magnesium Phosphorus PH PCO2 PO2 Acetaminophen Digoxin Salicylate Phenytoin LOW HIGH 120 2.8 2.5 10 1.8 2.2 1.7 <0.50 0.30 < 7.20 ≤ 20 ≤ 40 UNITS 155 6.0 7.0 280 3.0 25 17 > 2.10 > 7.60 ≥ 70 600 ≥ 3.0 2.3 119 mmol/L mmol/L mmol/L mmol/L umol/L mmol/L mmol/L mmol/L mmol/L mmol/L mmHg mmHg umol/L nmol/L mmol/L umol/L HEMATOLOGY Any new critical finding must have a HEMR (Hematologist Review) ordered. Send 2 unstained slides and CBC report to RGH hematology. Test Name Critical Value Alert/Urgent Value (called to the Physician immediately) (Physician notified within 24 hours) Platelet ≤ 20 x 109 /L (new case) ≤ 50 x 109 /L (out-patient/community) 9 ≤ 70 x 10 /L (patient bleeding) ≤ 100 x 109 /L Pre-Op 9 ≤ 100 x 10 /L (neo) Hemoglobin ≤ 60 g/L (new case) ≥ 200 g/L adult male ≥ 220 g/L (new born) ≥ 180 g/L adult female ≤ 90 g /L Pre-Op Malaria Positive WBC ≥ 30 x 109 /L (inpatients-new case) ≤ 1.5 x 109 /L (new case) Monotest LABRlabOP7900A2.1.2 Rural Lab Critical Result Appendix Laboratory Services, Regina Qu’Appelle Health Region ≥ 20 x 109 /L outpatients Positive: if reflexed from lab Page 1 of 2 Last printed 7/4/2013 2:04 PM RURAL LAB CRITICAL RESULTS PT INR > 5.0 ASAP INR ≥ 1.5 pre-op patients or first time on none PTT ≥ 100 sec. ASAP ≥ 39 sec pre-op patients or first time on none Any test result that the technologist feels is significant should be called Test Name Abnormal blood films Brown Plasma Critical Value (Notify the Hematologist on call immediately) Send unstained slides (2) along with CBC report to RGH for HEMR) 1. New Leukemia 2. Schistocytes-Any with platelets ≤ 50 x 109 /L and/or hgb drop ≥ 30 g/L (except hemodialysis patients) 3. Spherocytes- 2 + with anemia-new case 4. Sickle cells-Any new case 5. Positive Malaria When plasma sample has severe hemolysis (not from difficult poke) Order: CBC, scan, Hemr, renal, & liver panel, LD, PT, PTT, (some tests may not be available on site. Refer those tests to RGH for testing.) Urgent Value (Hematologist notified within 24 hrs) 1. 2. 3. Marked Rouleaux- new or significant change. 3+ Agglutination - new. Absolute Neutrophil < 0.5 x 109 /L-first time Note: New Leukemias-First time Blasts(add comment: refer to Hematologist’s review for verification) TRANSFUSION The laboratory will call whenever there will be a delay in filling the crossmatch request – detailing the reason for the delay. MICROBIOLOGY All POSITIVE blood culture results will be phoned. NOTES 1. 2. 3. Any result that the technologist feels is significant should be phoned, especially if there is a change from a previous result. Critical results telephoned from the testing facility should be telephoned to the inpatient ward, office/clinic or directly to the ordering physician. Any critical/ urgent value where the Physician can not be notified must be paged to the Medical Section professional “on call” and an occurrence report initiated. a. Page the appropriate medical section. To locate the medical section personnel on call, go to the “intranet” →choose “on call lists”→ choose either “clinical chemistry” for chemistry personnel on call or choose “hematology and transfusion lab consult” for hematology and transfusions section personnel on call. Please ensure you have the patient’s phone number prior to prior to initiating the page. The “on call” profession requires the patient phone number. LABRlabOP7900A2.1.2 Rural Lab Critical Result Appendix Laboratory Services, Regina Qu’Appelle Health Region Page 2 of 2 Last printed 7/4/2013 2:04 PM CHEMISTRY TESTS TEST Acetaminophen AFP (alpha fetoprotein) Albumin (serum/fluid) Alcohol (Ethanol) Alkaline Phosphatase ALT Amikacin Ammonia (plasma) Amylase (serum/urine/fluid) AST B12 B2 Microglobulin BhCG - Quantitative Bilirubin-total and direct (serum/fluid) Blood and Body Fluid Exposure Blood Gases BNP (plasma) CA125 Calcium (serum/urine) Carbamazepine Carbon Dioxide (CO2) Carboxyhemoglobin (whole blood) CEA Chloride (serum/urine) Cholesterol (serum/fluid) CK CKMB Mass CMV Creatinine (serum/urine/fluid) CRP CSF Glucose CSF Protein Cyclosporine (whole blood) Digoxin Dilantin (Phenytoin) Estradiol Ferritin Folates (serum and rbc) Free PSA Free T3 Free T4 LABChemOP8202C1 Chemistry Tests Laboratory Services, Regina Qu’Appelle Health Region STAT TAT (in minutes) 70 24 hr Availability * 70 70 70 70 70 70 70 70 * * * * * * * * 70 70 * * 2.5 hours 10 70 * * * 70 70 70 30 * * * * * * * * * * * * * * * * * * * * * 70 70 70 70 70 70 70 4 hours 70 70 70 * * * * * * Test Site RGH / PH * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * Page 1 of 4 Last printed 6/12/2013 11:43 AM CHEMISTRY TESTS FSH Gentamicin GGT Glucose Glucose Tolerances HDL / LDL Cholesterol Hemoglobin – fetal (APT test) Iron Ketones Lactate LD LH Lithium Magnesium (serum/urine) Methotrexate Microalbumin (urine) Occult Blood (feces/gastric) Osmolality (serum/urine) Phenobarbital Phosphorus (serum/urine) Potassium (serum/urine) Pregnancy test (serum/urine) Prolactin Protein (serum/urine/fluid) PSA PTH Salicylate Sirolimus Sodium (serum/urine) Tacrolimus Theophylline TIBC Tobramycin Triage (urine) Triglyceride (serum/fluid) Troponin I TSH Urea (serum/urine/fluid) Uric Acid (serum/urine/fluid) Urinalysis Valproic Acid Vancomycin 70 70 70 70 70 60 70 - plasma 60 – whole blood 70 LABChemOP8202C1 Chemistry Tests Laboratory Services, Regina Qu’Appelle Health Region 70 70 2 hours * * * * * * * * * * * * 70 70 70 70 60 * * * * * 70 * 70 70 4 hours 70 4 hours 70 * * 70 60 70 70 70 70 60 70 70 * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * Page 2 of 4 Last printed 6/12/2013 11:43 AM CHEMISTRY TESTS Chemistry Specialized Testing Chemistry Specialized Testing is staffed Monday to Friday 0730 – 1600 @ RGH Limited testing is available on the weekend. Call back may be required for some stat tests. TEST α-1 antitrypsin Acid Glycerol Lysis Time AGBMA Alkaline Phosphatase Isoenzymes AMA Amino Levulinic Acid Amniotic Fluid Scan ANA Screen Anti-dsDNA Anti-RNP/SM Anti-Scl 70 Anti-Smith Anti-SSA Anti-SSB ASMA Barbiturate Quantitation (Pentobarbital) Bence Jones Protein – Urine C3 – C4 Cryoglobulin / Cryofibrinogen Free Light Chains Galactose (serum/urine) Glucose 6 Phosphate Dehydrogenase Haptoglobin Hemoglobin A1C Hemoglobin A2 Hemoglobin F Hemoglobin Electrophoresis Hemoglobin in Plasma H-pylori IgG IFE with Quant Immunoglobulins Methemalbumin Methemoglobin/Sulfhemoglobin Oligoclonal Bands in CSF PE with IFE – Quant Immunoglobulins Porphobilinogen LABChemOP8202C1 Chemistry Tests Laboratory Services, Regina Qu’Appelle Health Region STAT TAT 4 hours 2 hours 2 hours 2 hours 2 hours 2 hours ROUTINE TAT 3 days 3 days 14 days 3 days 14 days 1 week 2 hours 14 days 21 days 21 days 21 days 21 days 21 days 21 days 14 days 8 hours 10 days 3 days 14 days *batch runs – 30 days 1 week 5 days 3 days 3 days 2 weeks 2 weeks 2 weeks 24 hours 7 days 10 days 24 hours 2 days 1 week 10 days 1 week Page 3 of 4 Last printed 6/12/2013 11:43 AM CHEMISTRY TESTS Porphyrin Screen, Urine or Stool Protein Electrophoresis – Serum Protein Electrophoresis – Urine Pseudocholinesterase/Dibucaine # Pyrogens Quant Immunoglobulins RF Sugar Chromatography Sweat Chloride Transferrin 2 hours 4 hours 2 hours 3 days 5 days 10 days 4 days 3 days 3 days 3 days 1 week 3 days 3 days All testing performed is approved by Health Canada regulations. LABChemOP8202C1 Chemistry Tests Laboratory Services, Regina Qu’Appelle Health Region Page 4 of 4 Last printed 6/12/2013 11:43 AM GUIDELINES FOR EXPECTED TURN AROUND TIMES IN HEMATOLOGY TEST CBC STAT “ TAT” 24 HR AVAILABILITY I HR * CBC DIFFERENTIAL 90 MINS * MALARIA SCREEN 90 MINS * 1 HR * 1 HR * 1 HR * 3 HR * 1 HR * 2 HR * 2 HR * 2 HR * 90 MINS * APTT PT FIBRINOGEN D-DIMER CSF CSF DIFFERENTIAL PERITONEAL FLUID & DIFFERENTIAL ESR MONOTEST KLEIHAUER BONE MARROWS FLOWCYTOMETRY 90 MINS NOTIFICATION SAME DAY 12HRS-(VERBAL RESULT BY PHONE) LABHemaOP7031C1.1.3 Guidelines for Expected Turn Around Times in Hematology Laboratory Services, Regina Qu’Appelle Health Region TEST PERFORMED RGH PASQUA * * * * * * * * * * * * * * * * * * * * * * * * * * Page 1 of 4 Last printed 6/12/2013 11:44 AM GUIDELINES FOR EXPECTED TURN AROUND TIMES IN HEMATOLOGY TEST ROUTINE CBC 6 HRS DIFFERENTIALS 24 HRS * * APTT 4 HRS * * PT 4 HRS * * FIBRINOGEN 4 HRS * * OTHER FLUIDS 4 HRS * * ESR 6 HRS * * RETICS 24 HRS * * MONOTEST 6 HRS * * KLEIHAUER 24 HRS * SEMEN ANALYSIS 48 HRS * BONE MARROWS 72 HRS * FLOWCYTOMETRY 48 HRS * CD4/CD8 24 HRS * LABHemaOP7031C1.1.3 Guidelines for Expected Turn Around Times in Hematology Laboratory Services, Regina Qu’Appelle Health Region TEST PERFORMED RGH PASQUA * * * Page 2 of 4 Last printed 6/12/2013 11:44 AM GUIDELINES FOR EXPECTED TURN AROUND TIMES IN HEMATOLOGY The following tests are available but they are to be approved by the hematologist mainly because: a) These tests are time consuming. b) These tests are difficult to interpret. TEST RGH SERUM VISCOSITY * SICKLE CELL TEST * HEINZ BODY TEST * SUCROSE LYSIS TEST * HAM’S TEST * LEUKOCYTE ALKALINE PHOSPHATASE * NBT TEST * MYELOPEROXIDASE STAIN * COMBINED ESTERASE STAIN * IRON STAIN * SUDAN BLACK STAIN * LEUKOCYTE ACID PHOSPHATASE * MALARIA IDENTIFICATION * LABHemaOP7031C1.1.3 Guidelines for Expected Turn Around Times in Hematology Laboratory Services, Regina Qu’Appelle Health Region Page 3 of 4 Last printed 6/12/2013 11:44 AM GUIDELINES FOR EXPECTED TURN AROUND TIMES IN HEMATOLOGY The following special coagulation tests have to be approved by the Hematologist. These tests are time consuming and difficult to interpret. The TAT for these tests is 8-12 weeks. BLEEDING TIME TEST RGH * FACTOR ASSAYS * RISTOCETIN * FACTOR VIII RELATED ANTIGEN * PLATELET AGGREGATION STUDY * PROTEIN S * PROTEIN C * ANTITHROMBIN III * APC RESISTANCE RATIO * ANTICARDIOLIPIN ANTIBODIES * DRVVT * THROMBIN TIME * EUGLOBULIN LYSIS * FACTOR XIII * HEPARIN ASSAY * INHIBITOR STUDIES * HIT TEST * PFA * LABHemaOP7031C1.1.3 Guidelines for Expected Turn Around Times in Hematology Laboratory Services, Regina Qu’Appelle Health Region Page 4 of 4 Last printed 6/12/2013 11:44 AM Anticipated Turn Around Times for Microbiology Tests Turn-around time (TAT) for Microbiology specimens is from the time of receipt of specimen in the laboratory to the time of generation of the final report. Specimen Initial Processing Final culture Comments Negative Positive Abscess Microscopy performed 72 hours 24 – 48 hours Mixed cultures, with Aspirate and reported. after isolation anaerobic organisms Body fluids Specimen cultured of organism. may require longer Deep Wound time. Blood Cultures Bottles are placed in an 5 days 24 – 48 hours Mixed cultures may automated system for after isolation require longer time. continuous monitoring. of organism. Bottles that are flagged as **Fungal blood positive are subcultured cultures are incubated immediately, and Gram for 5 days. stains are called STAT. **If extended incubation is requested, & approved by MOC: Blood culture bottles will be monitored on the automated system for 5 days. If negative after 5 days, terminal subculture will be performed. ≤ 24 hours ≤ 24 hours Appropriate ward and C. difficile Toxin Test the Infection Control department are notified of all positive results. Eyes / Ears Microscopy performed 48 hours 48 – 72 hours **Conjunctiva and reported. specimens must Specimen cultured include swabs from both the infected and the uninfected eyes LABMicOP8000.A.2 Anticipated Turn Around Times For Microcioloby Tests Laboratory Services Regina Qu'Appelle Health Region Page 1 of 4 Last printed 6/12/2013 11:46 AM Anticipated Turn Around Times for Microbiology Tests Specimen Rapid FLU Test Fungal cultures Genital Initial Processing In house testing only performed on In Patients. Specimens from out patients are referred to Reference Laboratory for testing. Preliminary report is issued at 7 days. Microscopy performed and reported. Specimen cultured Final culture Negative Positive ≤ 2 hours ≤ 2 hours 4 weeks 4 weeks 48 hours for Candida 48 – 72 hours 72 hours for GC MRSA Screen RSV Skin (superficial) Sputum PCR negative test results are released. PCR positive test results are confirmed by culture. Presumptive positive results should be reported as soon as mauve colonies grow on MRSA Select agar & test positive with the slide coagulase test. In house testing only performed on In Patients. Specimens from out patients are referred to Reference Laboratory for testing. Microscopy performed and reported. Specimen cultured 24 hours 72 – 96 hours ≤ 2 hours ≤ 2 hours 48 hours 48 – 72 hours Microscopy performed and reported. Specimen cultured. 48 hours 48 – 72 hours LABMicOP8000.A.2 Anticipated Turn Around Times For Microcioloby Tests Laboratory Services Regina Qu'Appelle Health Region Comments *Testing only performed at RQHR during Flu season. ** All suspected isolates of N. gonorrhoeae are referred to Reference laboratory for confirmation. Ward and Infection control notified immediately when MRSA is isolated. **If salivary specimen, ward will be notified and asked to recollect. Page 2 of 4 Last printed 6/12/2013 11:46 AM Anticipated Turn Around Times for Microbiology Tests Specimen Initial Processing Final culture Negative Positive 24 - 48 hours 24 – 48 hours Throat GenProbe DNA probe assay. Throat culture (Non-routine Throat) Specimen cultured 48 hours 48 – 72 hours Stool Culture: Urine VRE Screen Specimen cultured 72 hours 24 hours ≤ 72 hours 72 – 96 hours 48 – 72 hours ≤ 96 hours Specimen cultured Comments Testing not performed on Weekends. Throat swabs on children received on Fridays are cultured Antimicrobial susceptibility testing performed only upon request. Ward and Infection control notified immediately when VRE is confirmed. Microscopy Results Turn-around time (TAT) for Microbiology specimens is from the time of receipt of specimen in the laboratory to the time of generation of the final report. Test STAT Routine Gram Stain 1 hour Same day Auramine O (ZN) In Patients 2 hour 24 hours PCP 2 hour 24 hours Parasitology (O&P) LABMicOP8000.A.2 Anticipated Turn Around Times For Microcioloby Tests Laboratory Services Regina Qu'Appelle Health Region 48 – 72 hours Page 3 of 4 Last printed 6/12/2013 11:46 AM Anticipated Turn Around Times for Microbiology Tests Notes: 1. Additional interim reports are sent when delays in identification and / or susceptibility testing occur, as with fastidious organisms and mixed cultures. All positive cultures will have interim reports issued within 48 hours. Prompt and updated reports aid the physician in appropriate clinical interventions and proper patient management. 2. If these TAT limits cannot be met because of problems within the laboratory such as equipment, media, or reagents, the client will be notified (physician / ward), and if necessary, testing at an alternate site will be arranged. 3. Audits of TAT’s for interim and final reports is performed on a quarterly basis, evaluating different specimen types each quarter. The goal for interim reports is 100% of reports issued in ≤ 48 hours. LABMicOP8000.A.2 Anticipated Turn Around Times For Microcioloby Tests Laboratory Services Regina Qu'Appelle Health Region Page 4 of 4 Last printed 6/12/2013 11:46 AM Turn Around Time (TAT) – for Transfusions The following is the expected time frames for commonly requested blood products: Test Requested TAT Group O Uncrossmatched Packed cells 10 minutes Group-specific Uncrossmatched Packed Cells 15 minutes from sample receipt in Lab Fully Crossmatched Packed Cells 45 minutes from sample receipt in Lab (assuming no serological problems) Frozen Plasma 25 minutes (product must be thawed) (need a current admission blood group or issue universal donor group) Platelets (if available on site) 10 minutes (need a current admission blood group) Cryoprecipitate (need a current admission blood group or issue universal donor group) 25 minutes (product must be pooled and thawed) Blood Group – Stat 15 minutes from sample receipt in Lab- Blood Group - Routine 24 hours Group and Screen – Stat 45 minutes Group and Screen – Routine 4 hours Cold Agglutinin test 24 hours Direct Antiglobulin Test – Stat 30 minutes Direct Antiglodulin Test - Routine 24 hours NOTE: The Pasqua Hospital does not do serological testing. All serological testing is completed at the Regina General Hospital, therefore for the group-specific uncrossmatched packed cells and the fully crossmatched packed cells the TAT is from when sample is received at the Regina General Hospital. Laboratory Services, Regina Qu’Appelle Health Region Page 1 of 1 Last printed 6/12/2013 11:47 AM APPENDIX Tests Referred to Saskatchewan Disease Control Laboratory Orders for tests, which are referred to the Saskatchewan Disease Control Laboratory, must be submitted on the appropriate SDCL requisition. Do not use RQHR requisitions. The following is a list of the more common tests referred to the Saskatchewan Disease Control Laboratory: Aldosterone ASOT Catecholamine Chlamydia Cortisol DHEA-SO4 Fructosamine (Glycosylated Protein) HBsAg HCV Hepatitis A,B, and C screen HIV Insulin Metanephrines Mycobacterium Culture PKU Progesterone PTH Testosterone Thyroid Antibody Urine Drug Screen VDRL Viral Culture Viral Serology – Rubella, Torch screen, Cytomegalovirus (CMV) Herpes, Legionella, Epstein-Barr virus LABRegOP7900A1.1.1 Tests Referred to SDCL Laboratory Services Regina Qu'Appelle Health Region Page 1 of 1 Last printed 5/7/2010 4:22 PM Specimen & Requisition Reminders: Please help SDCL reduce turnaround time and thus improve patient care by accurately submitting specimens and requisitions. Saskatchewan Ministry of Health Saskatchewan Disease Control Laboratory Patient Demographics MUST: - Include the complete last name and first names - Include the patient’s address for all MHO reportable test orders. Place Saskatchewan Disease Control Laboratory number sticker here Chemistry Requisition Patient's Name & Address (required - print clearly) Patient PHN XXX XXX XXX Last Name, First Name 123 City Street Regina, SK S4X 4C2 Birthdate D 12 / 01 M Gender Male / 2011 Y Female Sending Location Phone # Requisitions/packing slips MUST contain the patient’s Personal Health Number (PHN) and Birthdate Hospital ID, Ward or Room # Patient Type In Diagnosis Collection Date Medication Collection Time Physician name (include initials) Physician MCIB# D / H Physician’s Last Name, First Name or Initials MUST be included on all requisitions. - Include Physician’s MCIB # -Indicate if out of province physician Please do not use: - Interns or residents - Abbreviated last names or ‘Nick’ names for physicians To ensure results are sent to the correct location, include complete return address Note: All specimens must have two unique identifiers: - Patient Last & First Names - PHN - Birthdate Clearly mark off all tests on the requisitions or list them on the packing slips Out M / / Y M Dr. First Name OR Initials, Last Name XXXX Return Address (Doctor/Clinic/Hospital) In addition to mail/courier, please copy to: Mail* or Fax (_____) _____- _________ Dr.'s Name Phone report (_____) _____ - _________ Please ensure that requisitions and specimens are properly labeled. Specimen Type Serum Urine Plasma Blood CSF Gastric Other (specify) _________________________________________ Additional Information If this is 24 hr. urine collection, enter volume ________ (Liters/day) Body wt. _________ kg Timed series: number of tubes _____. Indicate collection time on tube(s) and requisition. ________ Tests (Compendium of tests contains additional information) Estradiol DHEA-SO4 Progesterone Phenylalanine Prolactin Cholinesterase (Pseudo) Testosterone Lipase SHBG/FAI Oxalate LH & FSH Catecholamine B12 VMA Ferritin Metanephrines Iron Studies UFC (iron, Transferrin, Ferritin) Drugs of Abuse – Urine – 5 Panel Amphetamines Benzodiazepines Cannabinoids Cocaine Opiates Drugs of Abuse: (other) ________________________ ________________________ ________________________ Magnesium 5HIAA Cortisol HVA Toxicology Tests 17-OHP Porphyrins Reason for Request HGH* Primidone PTH (Intact)* Quinidine ACTH* Ethosuximide C-Peptide* NAPA/Procainamide Therapeutic Overdose Other Drugs suspected (specify) Lead* Gastrin* Insulin RBC Folate ** (Hematocrit __________) * See Test in compendium for special handling ** CBC result required for RBC folates Health 13 126 09/09 Other tests requested (specify) Chemistry Please use "Thyroid Function" requisition if only thyroid tests are requested. SUBMISSION OF SPECIMENS Attention to the following points will ensure useful results on submitted specimens: 1. Collect specimen properly and complete the requisition carefully. 2. Send sufficient specimen for tests requested. 3. For tests not listed, consult SDCL Laboratory Test Compendium, enquire by mail or telephone. (The laboratory offers many additional chemical tests whose frequency does not warrant inclusion on the standard form). CLOTTED BLOOD OR SERUM 1. If possible, collect fasting blood. Turbidity or lactescences of postprandial specimens may interfere with many tests. 2. Complete requisition and record any concurrent medications. 3. a) Avoid hemolysis,. Constituents such as potassium, phosphates, and most enzymes are unequally distributed between the cellular elements and extracellular plasma. b) Use a 20 or 22 gauge needle (smaller lumens may rupture erythrocyte membranes in the vacuum draw). c) Avoid excessive stasis. (After 5 minutes of venous occlusion, many enzymatic activities are increased 20-25%). 4. Separate serum wherever possible. Submission of serum free of r.b.c. eliminates risk of leakage from cellular elements and risk of hemolysis enroute to the laboratory. 5. a) Store specimen in refrigerator until transporting. b) Pack to avoid breakage. 6. The following must be frozen and received frozen: ACTH C-peptide Gastrin Specimen Volume Required (See Compendium) Serum (double the volume stated if sending clotted blood) Serum Separator Vacutainer (SST) should be avoided in therapeutic drug and hormone testing. Please centrifuge whole blood and submit plasma or serum as per compendium. URINE CHEMISTRY Record 24hr volume and body weight on requisition. Send required aliquot for testing. Specimen Volume Required 1. Catchecholamines .............................................. 25 mL 5 HIAA ................................................................. 25 mL VMA .................................................................... 25 mL MET .................................................................... 25 mL HVA .................................................................... 25 mL Oxalates ............................................................. 25 mL On above tests, check pH which should be 2-4. Add 6N HCl if necessary. 2. 17 - Ketosteroids ................................................ 25 mL Adjust pH to less than 5 with glacial acetic acid or send frozen. 3. Urine "drugs of abuse" screen..............................20 mL random urine and/or urine "drugs of abuse (other)" Submission of Specimens Alcohol(s) .................................. Barbiturates ........................... Carbon Monoxide .................. Clobazam ................................. Ibuprofen ................................. Tricyclic Antidepressants ....... Other specific drugs .............. Lead .................................... 3 mL whole blood (grey top) 2 mL serum 2 mL whole blood 4 mL serum 2 mL serum 4 mL serum 4 mL serum 2 mL whole blood For a more complete list of laboratory tests and specimen requirements, refer to the SDCL Compendium of Laboratory Tests on-line (www.health.gov.sk.ca/compendium). For further information, please phone: For after hour STAT testing please phone: For interpretation, please phone: 787-3193 787-3197 536-4653 787-7900 Chemistry Toxicology Cell phone Dr. Denis Lehotay Laboratory Test Menu-Rural Facilities Wolseley **On Call Fort Qu'Appelle **On Call √ √ Bilirubin - Total √ √ √ √ √ √ Bilirubin - Conjugated √ Bilirubin - Total (Neo-Natal) √ Blood Gases √ Calcium √ Cholesterol (total) √ √ Cholesterol HDL √ √ Cholesterol LDL √ √ Carbon Dioxide (C02) √ Creatinine √ √ √ Chloride √ √ √ Sodium √ √ √ √ √ √ Potassium √ √ √ √ √ Glucose √ √ √ √ Glucose Tolerance Collection √ √ √ √ Magnesium √ √ √ Phosphorus √ √ √ Protein, Total - Serum √ √ Triglyceride √ √ Urea √ Uric Acid √ Alkaline Phosphatase √ √ √ √ √ √ Alanine Transaminase √ √ √ √ √ √ Amylase √ √ √ √ √ √ Aspartate Transaminase √ Creatine Kinase √ TROPONIN T √ Gamma Glutamyl Transferase (GGT) √ Lestock Indian Head ** On Call √ Whitewood √ Montmartre √ Imperial √ Grenfell Broadview ** On Call Albumin Cupar Test Balcarres ** On Call Sites testing Available 24 hours Moosomin ** On call STAT Testing Turn Around Time: 70 minutes √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ LABRlabOP7900A3.1.3 Laboratory Services Regina Qu'Appelle Health Region √ √ √ √ √ 1 Fort Qu'Appelle **On Call Indian Head ** On Call Broadview ** On Call Urinalysis - Microscopic √ √ √ √ √ √ √ √ √ √ √ Urinalysis - Dipstick Only √ √ √ √ √ √ √ √ √ √ √ Occult Blood - Feces (STAT only) √ √ √ √ Icotest √ √ √ √ Acetaminophen (Tylenol) √ Salicylate √ Lestock √ Wolseley **On Call Pregnancy Test - Serum Whitewood √ Montmartre Pregnancy Test - Urine Imperial √ Grenfell √ Lactate Dehydrogenase Cupar Moosomin ** On call Lactate Balcarres Test √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ Digoxin √ Phenytoin √ Drugs of Abuse √ √ HIV - POCT √ √ CBC √ √ √ √ √ √ √ √ √ √ √ Automated Differential √ √ √ √ √ √ √ √ √ √ √ Manual Differential √ √ √ √ √ √ √ √ √ √ √ Cell Morphology √ √ √ √ √ √ √ √ √ √ √ ESR √ √ √ √ √ √ √ √ √ √ √ Semen Analysis - Post vasectomy APTT √ √ √ √ Prothrombin Time (INR reported) √ √ √ ABO Forward and Reverse √ Rh typing √ Direct Antiglobulin Test √ Antibody Detection Screen √ Crossmatching Units of Blood √ Issue of packed cells / blood products √ Wet Prep (Hanging Drop) √ Monotest √ ECG √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ LABRlabOP7900A3.1.3 Laboratory Services Regina Qu'Appelle Health Region √ √ √ √ 2 Subject/Title: LABChemOP7269 Chemistry Lab Services Last Approved Time: 5/6/2013 2:47:39 PM Revision: 5.1 Approving Authority: Medical Biochemist Contact for Information: Chemistry Phone: (306) 766-4490 Current Version on Print Date Policy Process Control Purpose The purpose of this procedure is to provide information about the services provided by the Chemistry department at the Regina General Hospital and the Pasqua Hospital. The department is operational 24 hours a day to provide essential diagnostic testing. Routine and specialized testing is performed Monday to Friday from 0730 – 1600. Evening and night shifts are staffed to handle essential coverage only. A Biochemist is always on call to handle any unusual issues or problems that may arise. Procedure The Chemistry department has two sections, Routine Chemistry (RGH and Pasqua) and the Specialized Testing section at the RGH. The testing profile of the Chemistry department is quite extensive. Requirements for all tests are listed on the RQHR Intranet – Department / Laboratory / RQHR Lab Specimen Requirements. Critical result list is found in an appendix in the General Lab Services procedure. Test availability and turn-around-time is found in an appendix in the General Lab Services procedure. The following tables provide extra information regarding specimen collection that may be needed by the nursing unit. The tables are separated by specimen type. There are two additional tables regarding toxicology and therapeutic drug monitoring. LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 1 of 12 Last printed 5/6/2013 2:47 PM Blood Specimens Rapid ACTH Test (Cortrosyn) Blood Ethanol Blood Gases This test is used as a screening test for adrenocortical function Cortrosyn is a synthetic 1-24 ACTH. Baseline Cortisol is collected 250 ug of cortrosyn is injected intravenously by the ward 30 min Cortisol is collected 60 min Cortisol is collected See attached Appendix for specific ordering and collection instructions Chemistry only tests ethanol for medical purposes The legal driving limit of 0.08 is equal to 17.4 mmol/L Plasma ethanol results are about 7% higher than whole blood Capillary Ward notifies the Chemistry department that a capillary blood gas is needed Chemistry staff will inform ward to warm the foot or the hand (this depends on the size and age of the patient) The site is usually warmed with a wet cloth and then wrapped up with something to hold the heat in (for example wrapping a diaper around the cloth). The temperature should not exceed 45° C The site is ideally warmed for 3 – 4 minutes prior to the collection Arterial Arterial samples are drawn by a Respiratory Therapist or may be collected from an arterial line by a RN It is of utmost importance that the sample be correctly labeled (2 identifiers) The time of collection should also be indicated on the requisition. If the time is not stated, the technologist will default the entry to the time received in the laboratory. When dropping off specimens in Chemistry or when sending them through the pneumatic tube LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 2 of 12 Last printed 5/6/2013 2:47 PM Dexamethasone Suppression Test Glucose Tolerance system, it is EXTREMELY important the staff know that there is a sample to run Staff should be paged or phoned if no one was present in the department when the sample was dropped off Blood gas samples should not be left in the porthole at the RGH but should be brought directly to the department Blood gases are always analyzed STAT Report will print to ward immediately Screen for Cushing’s syndrome Baseline Cortisol levels are drawn at 0800 and 2000 hrs 1.0 mg of dexamethasone is given at 2300 hr A 0800 (post dose) Cortisol is drawn the next morning Patient should have been on a diet that contained adequate carbohydrates (150 g) for three days prior to testing Patient must fast for 10 hours prior to test (not required for gestational screen – see below) The commercially prepared glucose drink is obtained from the Chemistry department For patients that may be allergic to the dye in the orange drink, an alternative drink is available but the lab must be notified by the physician’s office so alternative drink can be ordered. Non-Pregnant Adult Glucose Tolerance (75 g) Fasting glucose sample is collected 75 g drink (296 ml) is given Patient should consume drink within 5 minutes 2 hour glucose sample is collected Gestational Diabetes Screen (50 g) Women are tested between their 24th and 32nd weeks of gestation Patient does not have to be fasting 50 g drink (296 ml) is given 1 hour glucose sample is collected Gestational Diabetes Tolerance (75 g) Test is done when woman has an elevated LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 3 of 12 Last printed 5/6/2013 2:47 PM result with the screening test Fasting glucose sample is collected 75 g drink (296 ml) is given Patient should consume drink within 5 minutes 1 and 2 hour glucose samples are collected See attached Appendix for specific ordering and collection instructions Children Dosage of drink must be calculated based on patient’s weight (not to exceed 75g of glucose) Calculation will be performed by a Chemistry technologist Fasting glucose sample is collected Drink is given Patient should consume drink within 5 minutes 2 hour glucose sample is collected Calculation of drink volume patient’s weight (kg) X 1.75 = #gm of drink #gm X 3.95 = # mLs of drink LIS test code GLMLS will calculate # mLs when patient weight (kg) is entered Growth Hormone Suppression Test Insulin Hypoglycemic Screen ( 5hr GTT) Approval by Medical Biochemist/Clinical Chemist should be sought prior to ordering this test as poor correlation with symptoms are typically seen Fasting glucose sample is collected 75 g drink is given Blood samples are drawn at 0.5, 1, 1.5, 2, 3, 4, 5 hour times Patient fasts overnight Fasting blood sample drawn for Growth Hormone 75 g glucose drink (296 mL) given Blood samples are drawn for Growth Hormone at the intervals requested by the physician Insulinoma is a rare condition that can cause organic hypoglycemia Measure blood glucose when symptoms of hypoglycemia are exhibited (glucose should be <2.5 mmol/L) LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 4 of 12 Last printed 5/6/2013 2:47 PM Toxicology Therapeutic Drug Monitoring Xylose Test Insulin levels should then be requested Measurement of glucose, insulin and C-peptide may be indicated if administration of exogenous insulin is suspected See separate section See separate section Children Food and fluids are withheld from patient for at least 8 hours prior to the test Patient is asked to void and specimen is discarded Pharmacy will prepare xylose drink based on 1 g of xylose per kilogram of body weight in a 10% solution (need weight of child in kg) Drink is given to patient followed by equal amount of water Patient is kept at rest and is given nothing by mouth for the next 5 hours All urine passed in the 5 hour period is collected and pooled for testing Adult Food and fluids are withheld from patient for at least 8 hours prior to the test Fasting blood sample is taken (pre drink level) 25 g of xylose dissolved in 250 mL of water is given to patient – followed by an extra 250 mL of water Patient is kept at rest and is given nothing by mouth for the next hour 1 hour sample is taken (1 hour post drink level) Urine Specimens Specimen Collection All specimens received must be labeled following standard laboratory labeling practice (2 identifiers) All specimens are accessioned into the LIS 1st morning urine specimen ideal specimen for testing as most concentrated patient voids first morning sample into a clean 80 mL sterile container or a graduated urine LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 5 of 12 Last printed 5/6/2013 2:47 PM tube, specimen is labeled and sent to lab Urine Testing Notes Feces Specimens Feces Tests Random urine specimen specimen collected at any time of day patient voids into a clean 80 mL sterile container or a graduated urine tube, specimen is labeled and sent to laboratory 24 hour urine specimen Disposable 24 hour urine container are used for collection It is important to have a complete and accurate specimen collected for valid results Patient empties bladder in a.m. (do not save this sample) Record start time and date For the next 24 hour collect all urine specimens that are voided during the day and night Last sample should be when patient empties bladder the next morning at the same time as start time Record stop time and date Label specimen and send to laboratory If possible specimen should be kept cool during collection The testing requirements can all be found on the Intranet Specimens should NOT be collected in containers containing boric acid for tests performed by the Chemistry department The collection for metals requires a special acid washed container – Obtain from the Chemistry department prior to beginning the 24 hour collection Required preservatives are added by the Chemistry staff after the 24 hour collection is completed Occult Blood Tests for the presence of blood Label specimens with two identifiers Specimen to be collected in sterile plastic container (be careful not to contaminate the LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 6 of 12 Last printed 5/6/2013 2:47 PM outside of the container with specimen) Fecal Fat Test requires the approval of SDCL prior to testing (contact Dr Lehotay or Jeff Eichhorst 787-3284) Test requires a 72 hour stool collection Pre-weighed containers, instruction for collection and shipping are provided by SDCL Start test after bowel movement. Discard this sample. Record start time and date Collect all stool passed in the next 72 hours Record stop time and date Specimen should be kept cold and entire specimen delivered to lab when complete Patient should not have any procedures that could alter the stool specimen (ie enema) CSF Specimens Routine Chemistry Protein, Glucose, LD, Lactic Acid, Chloride IgG Index Requires a CSF and a serum sample in order to calculate the IgG Index If physician writes order with the CSF tests, the ward MUST also order a blood collection on the patient CSF – IgG and albumin Serum - IgG Make sure patient has the blood test before being discharged Oligoclonal Bands Requires at least 2 mL CSF specimen If possible a serum sample is collected and run simultaneously with the CSF sample Toxicology Specimens Quantitative measurement is available on a 24 hour basis for: Acetaminophen, Ethanol, Salicylate on blood samples LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 7 of 12 Last printed 5/6/2013 2:47 PM Fluid Specimens Specimen Collection Tests Performed Fluid Notes Stat Qualitative testing for Drugs of Abuse is available on urine specimens on a 24 hour basis by ordering a Urine Triage – Acetaminophen/Paracetamol, Amphetamines, Methamphetamines, Barbiturates, Benzodiazepines, Cocaine, Methadone, Opiates, Phencyclidine, THC, Tricyclic Antidepressants Methanol and Isopropanol levels are measured by SDCL – call back required if after normal business day Routine urine drug screens are sent to SDCL for testing Suspected overdose of Therapeutic Drugs can be tested on a 24 hour basis for those drugs that are performed by the Chemistry department Specimens are collected by ward Specimens must be labeled with 2 identifiers Specimens for pH must be collected in a syringe or a green top tube – Specimen must be on ice and brought down immediately or pH will be rejected All other Chemistry tests should be collected in a red top tube or in a sterile C&S container Pleural Fluid Protein, Amylase, LD, Cholesterol, Triglyceride, pH, Glucose, Chylomicrons Peritoneal Fluid (ascites fluid) Protein, Amylase, Creatinine, Bilirubin, pH, Albumin Synovial Fluid Glucose, Uric Acid, Cholesterol, Triglyceride Pericardial Fluid pH, Amylase, LD, Protein, Dialysate Glucose, Creatinine, Protein, Urea, Volume Pancreatic Cyst Fluid CEA The matrix of fluids is different than serum samples and therefore may affect results The testing of fluids for many tests is not LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 8 of 12 Last printed 5/6/2013 2:47 PM indicated as there are no reference values for comparison Testing is often done to determine if specimen is a transudate or an exudate Transudate – low protein, no cells present Exudate – high protein, cells present Therapeutic Drug Testing For TDM to be effective, it is essential that the requisition is completed with the drug dosage regimen and administration time Separate requisitions are required for pre and post samples Ideal sampling times are indicated below – guidelines from the Pharmacy and Therapeutics Committee Test Amikacin Ideal sampling time Pre level – 30 minutes before dose Post level – 30-60 minutes after dose Carbamazepine Digoxin Ethosuximide Gentamicin Once daily – 6-14 hours after dose Pre level – 0 – 1 hour before dose Pre level – 0 – 1 hour before dose Pre level – 0 – 1 hour before dose Pre dose 0 – 30 minutes before dose Post dose 30 minutes after dose Lidocaine Once daily Gentamicin – 6 – 14 hours after dose 12 hours should elapse before collecting level Test notes Just before 3rd regular dose or as ordered by pharmacy After 3rd regular dose or as ordered by pharmacy After 3rd dose Steady state reached on day 7 of dosing regime Post load dose – done on day 2 Maintenance dose – done on day 5 (do not collect if less than 6 hours after dose) Steady state reached on day 7 of dosing regime Just before 3rd regular dose or as ordered by pharmacy After 3rd regular dose or as ordered by pharmacy After 1st or 2nd dose Pre level not recommended Indication for collection - when toxicity is suspected LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 9 of 12 Last printed 5/6/2013 2:47 PM - when ventricular arrhythmias occur despite lidocaine administration Lithium Post level – Collect 12 hours after evening dose Phenobarbital Pre level – 0 – 1 hour before dose Phenytoin (Dilantin) Pre level – 0 – 1 hour before dose Pre level – 0 – 1 hour before dose IV Loading levels 1) Immediately after loading infusion 2) 2 hours post infusion 3) 24 hours post infusion Primidone Procainamide / NAcetylprocainamide Quinidine Salicylate (therapeutic) Theophylline (Aminophylline) Maintenance levels Pre level – 0 – 60 minutes before dose Post level – 75 minutes after oral dose Pre level – 0 – 1 hour before dose Post level – 1 – 3 hours after dose Infusion Collect level any time Intermittent (IV or po) Pre level – 0 – 30 minutes before dose Post level – regular release – 2 hours slow release – 3 – 5 hours Steady state reached on day 4 of dosing regime (do not collect before 8 hours post dose) IV loading – no restrictions Maintenance – day 3 Steady state – Children/Infant – day 8 Adult/Adolescent – day 10 Maintenance – day 3 Steady state – day 7 Steady state reached on day 3 of dosing regime Maintenance – 24 hours Peak level may not occur until 2-4 hrs following dose in some patients Steady state reached on day 2 of dosing regime Steady state reached on day 3 of dosing regime Steady state – 24 – 48 hours Steady state – day 2 (do not collect pre dose greater than 60 minutes before dose) LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 10 of 12 Last printed 5/6/2013 2:47 PM Tobramycin Pre level – 0 – 30 minutes before dose Just before 3rd regular dose or as ordered by pharmacy Post level – 30 – 60 minutes after dose After 3rd regular dose or as ordered by pharmacy (collections times must be followed for accurate interpretation of result) Vancomycin Pre level – 0 – 30 minutes before dose Just before 3rd regular dose or as ordered by pharmacy Post level – 60 - 90 minutes after dose After 3rd regular dose or as ordered by pharmacy (collections times must be followed for accurate interpretation of result) References A Handbook of Routine Urinalysis, Sister Laurine Graff Saskatchewan Disease Control Laboratory Test Compendium Pharmacy and Therapeutics Committee Related documents Lab Services Manual General Information LABRegOP7900 Revision History Found in Softtech Health Lab QMS™ Document Management System Author Tammy Ottenbreit, MLT, ART LABChemOP7269 Chemistry Lab Services Laboratory Services Regina QuAppelle Health Region Page 11 of 12 Last printed 5/6/2013 2:47 PM Appendix LABChemOP7352A1 ACTH Stimulation Test Ward - stamp 3 SDCL requisitions with patient addressograph - Requisition 1 – write ACTH Stimulation Test – BASELINE CORTISOL. (state required time for baseline collection. ie 0700 hrs – patient must be fasting) - Requisition 2 – write ACTH Stimulation Test – 30 MINUTE CORTISOL - Requisition 3 – write ACTH Stimulation Test – 60 MINUTE CORTISOL For Phlebotomy Draw - staple requisitions together before sending to Laboratory. - requisitions must be in the Laboratory before 2100 hrs to ensure test is ordered in LIS and phlebotomy is prepared for collection in a.m. - testing (fasting collection or injection) should not be started before 0700 hrs. - phlebotomy will collect the baseline sample - DO NOT give injection until phlebotomy informs you that baseline sample has been collected - immediately after patient has been given the injection, phone 4527 (RGH) or 8412 (PH) and say “patient name” has been given injection for ACTH Stimulation Test - phlebotomy will return at 30 minute and 60 minute intervals to collect cortisol samples For Ward /Arterial line draw - ward is responsible for following protocol - yellow top tube is required for cortisol level - patients first and last name and MRN must be written on each tube - exact collection time must be noted on each requisition - baseline/ 30 minute/60 minute must be written on tube and matched to requisition to ensure specimens are processed correctly Accession - test is accessioned with LIS code – RACTH - it will ask for date and collection time - time marked is for the baseline collection - collection times for 30 minute and 60 minute collections will automatically fill in Phlebotomy - PDA will display collection for the ACTH stimulation test - patient order will have 3 labels with timed collections - collect baseline sample and print label - mark other 2 collections as “no” so labels are not printed - inform the ward that the baseline sample has been collected and that the injection can be given - the ward will call 4527 (RGH) or 8412 (PH) and say when the injection has been given LABChemOP7352A1 ACTH Stimulation Test Lab Services Regina Qu’Appelle Health Region Page 1 of 2 Last printed 6/12/2013 3:11 PM - phlebotomist that receives the call will go into patient order in the LIS and modify the collection times EXAMPLE 1. ward will say injection has been given at 0900 hrs 2. 30 minute will be 0930 hrs and 60 minute will be 1000 hrs 3. go into patient order 4. specimen tab 5. place cursor on collection to be modified (ie 30S for 30 minute) 6. select “Specimen” from top tool bar 7. select “Modify Specimen” 8. enter in the correct time for collection (ie 0930 hrs) 9. repeat for 60 minute specimen 10. save order - collections will now appear in the PDA’s with the proper collection time and all phlebotomists will be aware LABChemOP7352A1 ACTH Stimulation Test Lab Services Regina Qu’Appelle Health Region Page 2 of 2 Last printed 6/12/2013 3:11 PM Appendix LABChemOP7317A1 75 gm Maternal Glucose Tolerance Ward - stamp a green requisition with patient’s addressograph order MAT 75gm 2 hr only (do not mark fasting glucose) enter collection time for fasting sample (ie 0700) ensure requisition is received in laboratory the day before test is required phlebotomy will collect fasting sample DO NOT give drink until phlebotomist informs you that fasting sample has been collected when patient has finished drink, call 4527 and say “patient name” has finished drink at _____ time. phlebotomy will return at the 1 and 2 hour interval to collect glucose sample Accession - requisition is accession with LIS code - GTTGE - it will ask for date and collection time - time marked is for the fasting collection - collection times for 1 and 2 hour will automatically fill in Phlebotomy - PDA will display collection for the tolerance - patient order will have 3 labels with timed collections - collect fasting sample and print this label - mark other 2 collection as ‘no’ so labels are not printed - inform the ward that the fasting sample has been collected and that the drink can be given - the ward will call 4527 and will say when patient has finished the drink (or they will leave message) - phlebotomist that receives call will go into patient order in the LIS and modify the collection times EXAMPLE 1. ward says drink complete at 0830 2. 1 hr will be at 0930 and 2 hr will be at 1030 3. go into patient order 4. Specimen tab 5. place curser on collection to be modified (ie CHEM1 CH1 for 1 hr) 6. select ‘Specimen’ from top tool bar 7. select ‘Modify Specimen’ 8. enter in the correct time for collection (ie 0930) 9. repeat for 2 hr specimen 10. save order - collections will now appear in the PDAs with the proper collection time and all phlebotomists will be aware LABChemOP7317A1 Lab Services Regina Qu’Appelle Health Region Page 1 of 1 Last printed 6/12/2013 3:12 PM - phlebotomist that receives the call will go into patient order in the LIS and modify the collection times EXAMPLE 1. ward will say injection has been given at 0900 hrs 2. 30 minute will be 0930 hrs and 60 minute will be 1000 hrs 3. go into patient order 4. specimen tab 5. place cursor on collection to be modified (ie 30S for 30 minute) 6. select “Specimen” from top tool bar 7. select “Modify Specimen” 8. enter in the correct time for collection (ie 0930 hrs) 9. repeat for 60 minute specimen 10. save order - collections will now appear in the PDA’s with the proper collection time and all phlebotomists will be aware LABChemOP7352A1 ACTH Stimulation Test Lab Services Regina Qu’Appelle Health Region Page 2 of 2 Last printed 6/12/2013 3:11 PM Subject/Title: LABAccnOP7200 Cytogenetics Last Approved Time: 4/16/2010 1:55:25 PM Revision: 1 Approving Authority Manager of Support Services Contact for Interpretation: Accession Phone: (306) 766-4495 Current Version on Print Date CYTOGENETICS I GENERAL INFORMATION Specimens for cytogenetic (chromosome) and DNA studies are sent to a referral laboratory for testing. Specimens are to be collected MONDAY THROUGH THURSDAY ONLY AND MUST BE RECEIVED IN THE LABORATORY BEFORE NOON ON THE DAY OF COLLECTION. NOTE: Specimens are NOT to be collected or sent on a statutory holiday or on Thursday when Friday is a statutory holiday. Chromosome studies may be performed on blood, amniotic fluid, bone marrow or skin/tissue. No prior approval is required. Different specimens require different treatment and methodology. Therefore it is important to check the Test Compendium for type of vacutainer to use when collecting blood samples for chromosome studies. DNA studies MUST receive prior approval from Dr. E. Alport @ 766-2778 before collection. Specimen(s) must be kept at room temperature at all times. Specimen(s) must be received at RGH by noon. Specimens will be processed immediately and be ready for FED-EX pick-up by 1400 hr the same day of collection. Requisitions must be carefully completed with particular emphasis on relevant cytogenetic information ie: suspected chromosome abnormality or indication for request. Testing for specific abnormalities (e.g. Fragile X) must be specifically requested as they are not part of routine testing. LABAccnOP7200 Cytogenetics Laboratory Services Regina Qu'Appelle Health Region Page 1 of 3 Last printed 4/19/2010 10:24 AM II BLOOD CHROMOSOME STUDIES 1. Routine – determines constitutional karyotype. Check test compendium for type of specimen container required for collection. Special Studies (e.g. Fragile-X, high-resolution studies) - Special arrangements must be made with the referral lab. Hemochromatosis - Approval to order this test is to be obtained from the Hematologist, Dr. Devaraj. He may be contacted by telephone at 766 - 4464 (pager # 4230) 2. For Hematological Disorders For patients who have a high WBC count and more than 10 percent circulating immature myeloid cells (myelocytes or younger), peripheral blood may be examined for acquired chromosome abnormalities. III BONE MARROW STUDIES (i) Marrow is the tissue of choice for the detection of chromosome abnormalities in hematological malignancies. (ii) Can be set up mornings only Monday to Thursday. (iii) Please notify the Hematology lab well before the marrow tap is begun so that the necessary preparations may be made. IV AMNIOTIC FLUID Fluid should be collected at 13+ weeks gestation. (a) Use plastic syringes and sterile tubes Approximately 20 - 30 ml of fluid is required. Withdraw 2 - 3 ml and DISCARD. This minimizes contamination with maternal macrophages. (b) The next 10-12 ml of fluid drawn is gently inserted into a sterile tube. (c) Using a NEW SYRINGE withdraw another 10-12 ml of fluid and insert into a second sterile tube. (d) Approximately 5ml in a third tube are required for Alpha -fetoprotein. Page 2 of 3 Last printed 4/19/2010 10:24 AM V PRODUCTS OF CONCEPTION Products-of-conception tissue is not routinely submitted for cytogenetic studies. However if the testing is requested be sure to: VI VII 1. Collect spontaneous abortion material in its entirety into sterile containers. To keep specimen from drying out, cover with sterile saline-soaked gauze and deliver to the lab as soon as possible. The sample should be kept at room temperature if it is delivered the same working day. Samples that cannot be delivered the same day should be refrigerated. 2. Therapeutic abortion material (larger fetuses) should be kept from drying out by covering with sterile saline/water-soaked gauze or adding a small amount of sterile water or saline to the container and bring to the lab as soon as possible. CORD BLOOD 1. Collect into heparinized tube (green top), mix thoroughly and bring to laboratory. 2. May be kept refrigerated if necessary until morning. BUCCAL SMEARS FOR SEX CHROMATIN STUDIES This test is no longer performed. VIII OUT-PATIENT SERVICE Patient reports to the Specimen Collection Laboratory before Noon Monday to Thursday except statutory holidays. Physician’s Name, Address and Telephone number must be clearly marked on the requisition. Specimens must be delivered to the RGH Laboratory by NOON on day of collection. Note: Specimens are not collected or shipped on a Thursday when Friday is a statutory holiday. Revision History Found in SoftTech Health Lab QMS™ Document Management System Author D. Fox, ART Page 3 of 3 Last printed 4/19/2010 10:24 AM Subject/Title: LABCytoOP7000 Diagnostic Cytology Lab Services Manual and Testing Compendium Last Approved Time: 7/15/2011 3:50:11 PM Revision: 2.1 Approving Authority: Cytopathologist Phone: (306) 766-2641 Contact for Interpretation: Cytology Current Version on Print Date Diagnostic Cytology Laboratory Services Manual and Testing Compendium I. PURPOSE The primary purpose of this manual is to provide a guideline for clinical specimen collection, and handling that are submitted for cytological diagnosis. II. SPECIMEN A. Types: 1. Endocervix 2. Exocervix 3. Vaginal wall 4. Vulva 5. Cerebrospinal fluids 6. Joint fluids (synovial) 7. Ocular fluids 8. Serous effusions - pleural, pericardial, peritoneal 9. Urine 10.Respiratory 11.Skin 12.Various lesions - superficial, deep-seated B. Collection Methods: 1. Scrapings 2. Brushings 3. Lavages 4. Drainage 5. Washings 6. Fine needle aspiration biopsies 7. Aspirations 8. Secretions C. Specimen Identification and Labeling: LABCytoOP7000 Diagnostic Cytology Lab Services Manual and Testing Compendium Laboratory Services Regina QuAppelle Health Region Page 1 of 12 Last printed 1/10/2012 3:19 PM Inadequately identified specimens will not be accepted. 1. Containers must be labeled with 2 identifiers at the time of collection. Examples of acceptable identifiers are: patient name, date of birth, HSN (Health Services Number), MRN (Medical Record Number). 2. Submitted slides may be labeled with a single identifier, but two identifiers are preferred. Specimen Slides are to be labeled with a lead pencil on the frosted end with the patient’s full name. Please do not use pen-type inks because ink tends to run during cytology processing. 3. If more than one site is sampled on the same patient, the specific source/site must be indicated on each specimen submitted, as well as, indicated on individual cytology requisitions. III. SPECIMEN SUBMISSION & TRANSPORTATION A. Prepared Slide Submission: all slides must be labeled with patient’s first and last name a completed cytology requisition must accompany the slide(s) all prefixed smears/slides are allowed to dry prior to transportation slides are packaged within a blue plastic slide mailer to prevent slide breakage. (Note: Patient identification on the blue mailer is not acceptable; must be on specimen slides. The Regina Qu’Appelle Health Region Cytology Laboratory will supply mailers upon request) B. Fresh (Liquid) Specimen Submission: fresh specimens are submitted in a separate clearly labeled, secure, leakproof container. Do not transport specimen in a syringe or other collectable device. the specimen container is placed within a secondary container. Examples are a sealable plastic bag or a secondary leakproof container. cytology requisitions must accompany the specimen, and should not be placed within the secondary container. IV. CYTOLOGY REQUISITION FORM: 1. The requisition form must accompany the labeled cytology specimen. 2. The requisition must provide identifying information: patient’s full name provincial hospitalization number date of birth and/or age ordering physician’s name and address (copy to physician’s name and address) date of specimen collection Page 2 of 12 Last printed 1/10/2012 3:19 PM source and site of specimen type of collection method relevant clinical information and history The Gyne requisition order # is RQHR 694. The NonGyne requisition order # is RQHR 220 (NOTE: The RQHR Cytology Laboratory will supply requisitions upon request.) V. SPECIMEN REJECTION CRITERIA 1. Specimen Container/Slide improperly labeled or unlabeled 2. Discrepancy of information between specimen and requisition form 3. Slide(s) broken beyond repair 4. Specimen received without accompanying requisition or vise versa 5. Inadequate preservation of specimen 6. Specimen container broken or leaking 7. Specimen received from an unauthorized source 8. Requisition lacking pertinent information on: patient’s full name patient demographics ordering physician source/site of specimen VI. RQHR CYTOLOGY LABORATORY ADDRESS & HOURS of OPERATION RQHR Diagnostic Cytology Division, Anatomical Pathology Laboratory Pasqua Hospital 4101 Dewdney Avenue Regina, SK S4T 1A5 1-306-766-2641 - Cytology Supervisor 1-306-766-2642 - Microscopy Area 1-306-766-2519 - Cytopreparatory Area 1-306-766-2752 - Fax Hours of operation: 0730-1600 hours Monday-Friday Page 3 of 12 Last printed 1/10/2012 3:19 PM The Satellite Cytology service is located at the: RQHR Regina General Hospital Satellite Cytology Laboratory 1440 14th Avenue Regina, SK 1-306-766-4488 - Cytotechnologist 1-306-766-4772 - FAX Hours of operation: 0730-1530 Monday-Friday The Fine Needle Aspiration Clinic is located at the: RQHR Pasqua Hospital Ambulatory Clinic 4101 Dewdney Avenue Bookings: Regina, Sask. S4T 1A1 1-306-766-2240 Hours of Operation: Wednesday: 0900-1200 NOTE: The Cytology laboratories are not staffed on Saturdays, Sunday or Statuary Holidays. VII. GENERAL TECHNIQUES A. PAP SMEAR PROCEDURE The objective of an adequate Pap smear is to provide a sampling of the squamocolumnar junction between the ectocervix and endocervix (Transformation Zone). Combinations of various types of sampling are possible and can vary. Please note that use of cotton-tip applicator is NOT recommended. Sampling devices are available from the RQHR Cytology laboratory and can be ordered directly on the requisition. The Pap smear is considered a screening test only and has been demonstrated to produce false negative rates however it is still considered to be a highly effective tool for detecting cancerous and precancerous cervical lesions 1. Complete cytology requisition. Include all pertinent information, including the clinical information section, the reason for the Pap smear, age, LMP date, hormone replacement therapy, post menopause history, and the sampling tools used. 2. Prepare slide by writing the patient’s name on the frosted end of the slide. 3. Wooden Spatula: Transformation Zone Scrape (and vaginal pool sample, if indicated) Page 4 of 12 Last printed 1/10/2012 3:19 PM insert and rotate one full turn spread material over top-half of slide spray immediately with fixative, holding spray bottle 3-4 inches away from slide pump 5-6 times or until saturated the spray will contact the bottom half of the slide. This will not jeopardize the remainder of the procedure Cytobrush: endocervix sampling gently insert cytobrush into the endocervix rotate slowly one turn remove cytobrush spread material on the bottom-half of the slide by rolling and twisting the cytobrush spray immediately as described above. There is no need to direct spray away from material already on the slide. Additional spray will not alter the specimen. 4. Place slide in slide holder, leaving open until dry 5. When completely dry, close folder. Wrap the requisition around the holder and secure with rubber band 6. Mail or deliver to the RQHR Pasqua Hospital Cytology division. PRECAUTIONS: USE OF CYTOBRUSH Manufacturers of cytobrush suggest these precautions: You may want to inform your patients that due to thorough sampling of the endocervical canal by the Cytobrush, there may become minor painless spotting for a day or two following the Pap test. B. SPUTUM 1. Specimen the first morning sputum is generally considered to be the most representative for cytological examination 2. Specimen Collection the patient receives a labeled specimen container the night before, and is instructed how to expectorate sputum upon awakening the next morning, the patient is to rinse his/her mouth, clean his/her throat with a gentle cough, and deep cough from the diaphragm and expectorate all sputum into an appropriate seal proof specimen container the procedure should be repeated once a day for three days 3. Submission the cup should be collected by early morning and immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated. An equal volume of 50% ethyl alcohol should be added to the specimen if there will be a delay in reaching the laboratory (more than one day). The addition of alcohol should be noted on the requisition and specimen container Page 5 of 12 Last printed 1/10/2012 3:19 PM 4. Limitations If pulmonary macrophages are not seen, the specimen will be reported as unsatisfactory C. BRONCHIAL BRUSHING 1. Specimen bronchial brushings is a selective brushing of the bronchial tree, and is performed by the physician during fiberoptic bronchoscopy brushings are usually taken and immersed in a balanced salt solution 2. Specimen Collection bronchial brushing is performed by the physician the brush is immersed in a seal proof specimen collection tube that contains saline or Cytolyt (preservative) 3. Submission the specimen is to be immediately taken to the laboratory the specimen collected after hours or on the weekend should be refrigerated, making sure preservative of Cytolyt or 50% ethyl alcohol has been added D. BRONCHIAL WASHINGS 1. Specimen bronchial washings selectively washes a specific area of the bronchial tree, and is performed by the physician during fiberoptic bronchoscopy washings are usually taken using a balanced salt solution 2. Specimen Collection the distal airways are rinsed with normal saline the fluid is collected via suction the specimen is collected within an appropriate seal proof container 3. Submission the specimen is to be immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated an equal volume of Cytolyt or 50% ethyl alcohol should be added to the specimen if there will be a delay in reaching the laboratory (more than one day). The addition of alcohol should be noted on the requisition and specimen container. E. 1. 2. URINE SPECIMENS/BLADDER WASHINGS Specimen voided or catheterized urine specimens; bladder washings Specimen Collection voided urine: the patient is hydrated and the subsequent midstream voided urine is collected in a labeled container bladder washing: is usually done at cystoscopy by irrigating the bladder with normal saline catheterized urine: is collected through the catheter and is transferred into a labeled container Page 6 of 12 Last printed 1/10/2012 3:19 PM 3. 4. F. 1. 2. 3. renal pelvis and ureters: hydrate patient one glass water every 15 minutes for 2 hours. Patient should void and discard urine. Catheterize ureter below level of suspected lesion and collect urine for ½ hour. Other ureter catheterized as control. Same for renal pelvis with or without saline irrigation. Submission the specimen is immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated. if the specimen cannot be refrigerated, the addition of equal volume of 50% alcohol should be added. This addition should be noted on the requisition form, and on the specimen container Limitations Low grade papillary urethelial carcinoma may not be diagnosed by cytologic examination alone as recent instrumentation or calculi may produce similar atypical changes in the urothelial cells SEROUS EFFUSIONS Specimen pleural (thoracic) fluids, peritoneal (ascites) fluids, pericardial fluids Specimen Collection serous effusions collections are performed by a physician fluid is withdrawn from the serous body cavity fluid is collected in a clearly labeled, screw-top leakproof container if possible patient should be moved into several positions in order to well suspend the cellular material prior to collection Submission the specimen is immediately taken to the laboratory fluids should be submitted fresh the size of the fluid sample should not exceed 200 ml. If the amount is greater than 200 ml., the fluid should be well mixed and the specimen should be centrifuged in a few tubes to obtain a button of cells. Decant the supernatant and add 50% ethyl alcohol to the button. Resuspend the cells. Place the entire resuspended specimen (with added 50% ethyl alcohol) into a leakproof container the practice of salvaging large amounts of fluids is not recommended fluids collected after hours or on the weekend should be refrigerated. the addition of an equal volume of 50% ethyl alcohol should be added if the specimen will be delayed in reaching the laboratory (more than one day). This addition must be noted on the requisition and the specimen container G. CEREBROSPINAL FLUID 1. Specimen cerebrospinal fluid specimens 2. Specimen Collection the specimen is obtained by the physician while performing a lumbar puncture fluid is collected in a clearly labeled, leakproof tube 3. Submission Page 7 of 12 Last printed 1/10/2012 3:19 PM the specimen is to be immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated. if the specimen cannot be refrigerated, the addition of equal volume of Cytolyt or 50% alcohol should be added. This addition must be noted on the requisition form, and on the specimen container *NOTE: Please indicate on the requisition if lymphoma/leukemia is suspected H. ABDOMINAL and PELVIC WASHINGS 1. Specimen abdominal and pelvic washings 2. Specimen Collection abdominal and pelvic washings are performed by a physician washings are usually collected in balanced salt solution washings are collected in a clearly labeled, screw-top leak proof container 3. Submission the specimen is immediately taken to the laboratory fluids should be sent fresh and unfixed if at all possible fluids collected after hours or on the weekend should be refrigerated if the specimen cannot be refrigerated, the addition of equal volume of Cytolyt or 50% alcohol should be added. This addition must be noted on the requisition form, and on the specimen container I. GASTROINTESTINAL, ESOPHAGEAL, and GASTROESOPHAGEAL BRUSHINGS 1. Specimen brushings from the gastrointestinal, esophageal, and gastroesophageal sites 2. Specimen Collection the gastroenterologist performs the brushing after the brushing technique is completed, the brush is cut with wire cutters from the flexible wire leaving approximately 1 inch of wire the brush is dropped immediately into a test tube filled with Cytolyt or 50% alcohol 3. Submission the specimen is to be immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated. J. 1. 2. BREAST SECRETIONS (NIPPLE DISCHARGES) Specimen nipple discharges Specimen Collection slide is labeled with patient’s name secretion is expressed by gently squeezing the areolar area between the thumb and index finger the secretion is smeared across a glass slide Page 8 of 12 Last printed 1/10/2012 3:19 PM 3. the smear is immediately sprayed with fixative if secretion is thick, place another labeled glass slide on top and gently pull apart slide; fix with spray fixative prepare as many slides as there is secretion Submission allow slides to dry and place in slide mailer requisition is attached to slide mailing container specimen is immediately delivered to the laboratory K. JOINT FLUIDS (SYNOVIAL FLUIDS) 1. Specimen synovial fluids, joint fluids 2. Specimen Collection the physician aspirates the fluid from the joint the synovial fluid is aspirated into a sterile test tube do not add fixative (alcohol) 3. Submission the synovial fluid is transported immediately to the cytology laboratory the requisition must indicate if the test is for the presence of crystals L. 1. 2. 3. 4. CYST FLUIDS Specimen cellular material extracted from suspected cysts Specimen Collection the clinician aspirates the contents of the cyst, and samples the wall and adjacent tissue by means of fine needle aspiration the aspirated material may be submitted in a clean leak proof container Submission the specimen is immediately taken to the laboratory specimens collected after hours or on the weekend should be refrigerated if the specimen cannot be refrigerated, the addition of equal volume of Cytolyt or 50% alcohol should be added. This addition must be noted on the requisition form, and the specimen container Limitations improper fixation, failure to include pertinent history specimens lacking representative cyst lining will be considered unsatisfactory M. OCULAR SPECIMENS 1. Specimen ocular discharges, secretions, conjunctival lesion, corneal lesions 2. Specimen Collection mucoid discharges are collected with a sterile cotton swab pre-moistened with sterile saline conjunctiva scrapings are collected with a rounded spatula or instrument to avoid abrasion Page 9 of 12 Last printed 1/10/2012 3:19 PM 3. material is gently smeared on a glass slide and is immediately immersed in 95% alcohol or is sprayed with fixative the scraping tool may be rinsed in a sterile saline and the solution is submitted for cytology intra-ocular aspiration for fluid cytology should be treated like a FNAB Submission any fluid, secretion or scraping is immediately transported to the laboratory fresh specimens collected after hours or on the weekend should be refrigerated specimens are fixed immediately in 95% alcohol or sprayed with fixative N. GUIDED FINE NEEDLE ASPIRATION BIOPSIES ( CT SCAN, ULTRASOUND, ETC): ADEQUACY CHECK Introduction: The Cytotechnologist will assist the clinician in the fine needle aspiration biopsy procedure of deep-seated lesions. You may contact the cytology lab at one of the following numbers: Pasqua site……………..ext. 2519 or 2642 Regina General site……ext. 4488 the cytology lab is notified at the hospital site where the procedure is being performed adequacy check will be provided on all aspirated specimens by the cytotechnologist, and a pathologist can be contacted if necessary 1. 2. Specimen radiologically guided fine needle aspiration of a deep-seated lesion Collection & Procedure the cytotechnologist prepares an area for FNAB preparation upon arrival. He confirms the patient and site with the radiology staff, and labels slides and a preservative- filled falcon tube following the aspiration technique, the cytotechnologist assists the clinician in the preparation of the specimen. Adequacy of specimen and difficulty of biopsy being performed determine the number of direct smears the clinician expels material on the slide the cytotechnologist makes pull-apart smears. Both air-dried and spray fixed smears are made. Air-dried smears are stained for adequacy using Diff Quick stain if at any time during the aspiration, the needle appears to be a dry tap, draw up a little preservative into the hub of the needle and then expel material on a slide the cytotechnologist views the stained smears (Diff Quick) with a light microscope, and indicates whether the sample contains representative cellular material of the aspirated lesion *this preliminary assessment of adequacy is documented on the back of the requisition and in the cytopathology report after an adequate number of smears are prepared, the needle is rinsed in the appropriate preservative tube for further testing Page 10 of 12 Last printed 1/10/2012 3:19 PM the cytotechnologist makes sure that each prepared slide is labeled separately and that patient identifiers are placed on any specimen container with collected material (including different sites, if warranted) NOTE: It is very important that the cytology requisition is properly filled-out, including relevant clinical history, clinical suspicions, and if STAT diagnosis is required 3. Transportation the cytotechnologist transports the specimen to the cytology laboratory and the specimen is immediately processed O. FINE NEEDLE ASPIRATION CLINIC, PASQUA HOSPITAL Introduction: The Regina Qu’Appelle Health Region has a Fine Needle Aspiration Clinic within the Pasqua Hospital, Ambulatory Care, Level 1. The Aspiration Clinic is run by the Pasqua Hospital Pathology Department. A Pathologist performs the aspiration and interprets the specimen for adequate sampling. A Cytotechnologist is also present to assist the Pathologist. Address and Bookings: Regina Qu’Appelle Health Region- Pathology Department Fine Needle Aspiration Clinic Pasqua Hospital, 5’th level 4101 Dewdney Avenue Regina, Sask S4T 1A5 Appointment Booking: (306) 766-2240 or 2245 Fax number: (306) 766-2752 Hours of Operation: Wednesday 0900-1200 1. 2. Specimen head and neck lesions (thyroid, lymph nodes, salivary glands) breast lesions miscellaneous (superficial soft tissue) Collection and Procedure the cytotechnologist prepares the area for fine needle aspiration upon the patient’s arrival. He checks the name band on the patient to make sure it matches the name on the requisition the pathologist discusses the fine needle aspiration procedure with the patient, including FNA site and any relevant clinical history. The patient is asked to provide written consent before the procedure begins upon patient consent, the patient is then prepared for the procedure. The cytotechnologist labels slides and a preservative-filled falcon tube Page 11 of 12 Last printed 1/10/2012 3:19 PM 3. the pathologist performs the fine needle aspiration. The number of direct smears will be determined by the adequacy of the specimen and difficulty of the biopsy being performed the pathologist expels material onto glass slides pull- apart smears are made. Both air-dried and spray fixed smears are made. Air dried smears are stained for adequacy using Diff Quik stain. the pathologist views the Diff Quik smears using a light microscope and indicates whether the sample contains representative cellular material of the aspirated lesion. after an adequate number of smears are prepared, the needle is rinsed in the appropriate preservative tube for further processing. *the cytotechnologist makes sure that each prepared slide is labeled separately and that patient identifiers are placed on any specimen container with collected material (including different sites, if warranted). Transportation the cytotechnologist makes sure the specimen is transported to the cytology laboratory for immediate processing and reporting Revision History Found in SoftTech Health Lab QMS™ Document Management System Author Y. Shelley Taylor, ART (CSMLS) / H. Budinski, MLT / L. Kozak, MLT Page 12 of 12 Last printed 1/10/2012 3:19 PM Subject/Title: LABHemaOP7001.2 Hematology Last Approved Time: 10/27/2014 8:49:10 AM Revision: 2.5 Approving Authority: Medical Hematopathologist Contact for Interpretation:Hematology Phone: (306) 766-4477 Current Version on Print Date HEMATOLOGY I GENERAL INFORMATION The laboratory provides a comprehensive series of hematology tests, and processes hundreds of specimens per day. A department with such a large volume of work requires a degree of organization and rostering of procedures to achieve maximal efficiency. This means that certain tests are not constantly available. Whenever investigations are urgently required for medical reasons, the laboratory staff will be pleased to be of service as quickly and as completely as possible. Out-of-hours tests are restricted to those on the STAT list unless authorization is obtained by the physician of record from the hematologist. The laboratory hematologist will be pleased to discuss problems at any time. II REQUISITION FORMS These should be accompanied by relevant information like anticoagulant therapy or diagnosis, particularly in those tests outside the routine work of the laboratory. All test requests for PT and APTT must have specific anticoagulant therapy, if any, stated on the requisition. If information is incomplete, laboratory staff will phone the ward for this information before the test results will be released. 1. BIOCHEMISTRY/HEMATOLOGY Form (green): for CBC, PT/INR, APTT, MONO and other tests not listed. This form is used for requests from the hospital wards. 2. COMMUNITY LAB REQUISITION Form (blue): for CBC, PT/INR, APTT, MONO and other tests ordered from the physician offices. LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 1 of 9 Laboratory Services Regina Qu'Appelle Health Region III COLLECTION OF SPECIMENS Usually a phlebotomist or technologist is available to take blood specimens, but medical staff may need to take blood in emergencies, or when the laboratory staff find it impossible to obtain blood. The following vacutainer specimen tubes are used: Mauve top (EDTA) - CBC, platelets, ESR Blue top (citrate) - Coagulation tests Red top (clotted blood) – Monotest, H.I.T. For coagulation tests it is essential that an unhemolyzed specimen without frothing is taken as rapidly as possible. Therefore, choose a large vein and aspirate with a large bore needle without undue delay. The collection of a frothy, hemolyzed and slowly taken specimen will initiate the early stages of the coagulation system and invalidate results. It is always worth remembering that a syringe is often more useful in taking blood from "difficult" patients. Also, a full tube of blood is required for all coagulation testing. IV BONE MARROW EXAMINATIONS A. Requests These should be booked (Monday – Friday) 24 hours in advance whenever possible and will normally be done only before 1300 hours in order to facilitate histology processing. Marrows with chromosome studies (or other genetic testing) must be collected Monday – Thursday to facilitate shipping procedures and referral laboratories. When a marrow examination is urgently required outside normal hours, this may be arranged on consultation with the laboratory hematologist. All requests for bone marrow examination must be accompanied by relevant clinical information. B. Collection of Specimen A good marrow specimen needs a meticulous method of aspiration. Only the first 0.5 ml of aspirate contains a good concentration of particles and this should be drawn out as rapidly as possible since marrow, being rich in thromboplastic substances, clots rapidly. If more marrow is required, i.e. chromosome analysis, flow cytometry, culture, etc., use a second syringe. If the first aspiration fails, use a new needle at a different site. LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 2 of 9 Last printed 10/27/2014 12:57 PM V LIST OF TESTS PROVIDED IN HEMATOLOGY A. General Hematology: 1. 2. 3. 4. 5. 6. 7. CBC: This gives print out of Hemoglobin, Hematocrit, WBC, RBC, platelets, MCV, MCHC, MCH, MPV, RDW and five-part differential count. ACT DIFF 2: This back-up analyzer provides hemoglobin, hematocrit, WBC, RBC, platelets, MCV, MCH, MCHC and a three part differential count. Reticulocyte count Erythrocyte sedimentation rate (ESR). Monotest Serum Viscosity Kleihauer test Malaria Identification B. The following tests are available but they are to be approved by the hematologist mainly because: (i) these tests are time consuming and (ii) they are difficult to interpret 1. Sickle cell test 2. Heinz body test 3. Hb electrophoresis 4. Test for Hb 'H' 5. Sucrose lysis test 6. Hams test 7. Acid Glycerol Lysis Test (previously Osmotic fragility) 8. Plasma Hb 9. Methemalbumin 10. Urinary hemosiderin 11. NBT Test 12. Myeloperoxidase Stain 13. Combined Esterase Stain 14. Iron stain 15. Sudan Black Stain 16. Leukocyte Acid Phosphatase C. Coagulation Tests: Coagulation Screen includes the following tests: 1. 2. 3. 4. Prothrombin Time Activated partial thromboplastin time Fibrinogen D-Dimer LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 3 of 9 Last printed 10/27/2014 12:57 PM The following special coagulation tests have to be approved by Hematologist: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 14. 15. 16. 17. 18. 19. D. Bleeding Time Factor Assays Ristocetin Cofactor von Willebrand Factor Antigen Platelet Aggregation Study Protein C Protein S Antithrombin APC Resistance Ratio Anticardiolipin Antibodies DRVVT/KCT Thrombin Time Euglobulin Lysis Factor XIII Heparin/Anti Xa Assay Inhibitor Studies HIT test PFA Body Fluids: Cell counts are done on CSF, pleural, peritoneal, synovial fluid, dialysate and bronchial washings. E. Semen Analysis: 1. Sperm count is done on post vasectomy. 2. Semen Analysis is done on specimens for fertility studies. (Semen analysis for fertility study or post vasectomy are done weekdays only from 08:00 – 14:45 except statuary holidays.) LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 4 of 9 Last printed 10/27/2014 12:57 PM VI BLOOD REQUIRED FOR LABORATORY TESTS TEST TYPE VOL. OF BLOOD ANTICOAGULANT VACUTAINER CBC (hemoglobin WBC, RBC) Min. 2 mL EDTA mauve Fibrinogen 2.7 mL 1.8 mL 3.2% Na Citrate 3.2% Na Citrate adult blue pediatric blue Partial Thromboplastin Time 2.7 mL 1.8 mL 3.2% Na Citrate 3.2% Na Citrate adult blue pediatric blue Prothrombin Time 2.7 mL 1.8 mL 3.2% Na Citrate 3.2% Na Citrate adult blue pediatric blue Sedimentation Rate Min. 2 mL EDTA mauve Monotest Min. 2 mL Min. 2 mL (preferred) EDTA none (serum) mauve red Kleihauer Min. 2 mL Viscosity Min. 5 mL EDTA mauve none (serum) red CSF none red Pleural, peritoneal, synovial, dialysate fluids, and bronchial washings EDTA mauve NOTE: When an analysis is required for which capillary blood is required, the Laboratory Technologist will obtain the specimen. KEY TO VACUTAINERS RED No anticoagulant for clotted blood GREY Potassium oxalate for chemistry GREY T.S.Thymol/Sodium Fluoride for chemistry (lactic acid) MAUVE EDTA for Hematology GREEN Heparin for pH, Carboxyhemoglobin, "Stat" Electrolytes only, Flowcytometry LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 5 of 9 Last printed 10/27/2014 12:57 PM BLUE VII Liquid Sodium Citrate for Prothrombin Time, P.T.T. and other coagulation tests ESTABLISHED NORMAL (REFERENCE) RANGES A. CBC (12 years or older) WBC 4 - 10 x 109/L RBC Men Women 4.3 - 5.4 x 1012/L 3.7 - 5.1 x 1012/L Hb Men Women 140 - 180 g/L 120 - 160 g/L Hct Men Women 0.400 - 0.500 L/L 0.370 - 0.470 L/L MCV 82 - 97 fL MCH 27 - 32 pg MCHC 320 - 360 G/L RDW 11.5 - 14.5 Platelet 150 - 400 x 109/L MPV 7.4 - 10.4 fl LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 6 of 9 Last printed 10/27/2014 12:57 PM CBC reference ranges (under 12 years old) Test 0 - 3 Day 4 Day-3 Mo 3 – 12 Mo 12 Mo-3 Yr 3 - 6 Yr 6 - 12 Yr WBC 10.0 - 30.0 10.0 - 26.0 6.0 – 18.0 6.0 - 18.0 5.0 - 15.0 4.5 - 13.5 RBC 4.00 - 6.00 4.00 - 6.00 3.20 - 4.80 3.60 - 5.20 4.10 - 5.50 4.00 - 5.40 x 1012/L Hgb 135 – 195 135 - 195 96 – 126 110 – 130 120 - 140 Hct .440 - .640 .440 - .640 .320 - .440 .360 - .440 .370 - .450 .370 - .450 L/L MCV 98.0 - 114.0 98.0 - 114.0 87.0 - 103.0 70.0 - 86.0 77.0 - 91.0 77.0 - 91.0 fL MCH 24.0 - 34.0 24.0 - 34.0 24.0 - 34.0 23.0 - 31.0 24.0 - 30.0 24.0 - 30.0 pg MCHC 320 – 360 320 - 360 320 - 360 320 – 360 320 - 360 RDW 11.5 - 14.5 11.5 - 14.5 11.5 - 14.5 11.5 - 14.5 11.5 - 14.5 11.5 - 14.5 Platelet 150 – 400 150 - 400 150 - 400 150 – 400 150 - 400 150 - 400 MPV 7.4 – 10.4 7.4 - 10.4 7.4 – 10.4 7.4 – 10.4 7.4 - 10.4 7.4 - 10.4 Neutrophil 5.0 – 13.0 5.0 - 13.0 2.0 – 6.0 2.0 – 6.0 2.0 - 6.0 2.0 - 6.0 x 109/L Lymph 3.5 - 8.3 3.5 - 8.3 5.5 – 8.5 5.5 – 8.5 5.5 - 8.5 5.5 - 8.5 x 109/L Monocyte 0.5 - 1.5 0.5 - 1.5 0.7 – 1.5 0.7 – 1.5 0.7 - 1.5 0.7 - 1.5 x 109/L Eosinophil 0.1 - 2.5 0.1 - 2.5 0.3 – 0.8 0.3 – 0.8 0.3 - 0.8 0.3 - 0.8 x 109/L Basophil 0.0 - 0.1 0.0 – 0.1 0.0 – 0.1 0.0 - 0.1 0.0 - 0.1 x 109/L 0.0 - 0.1 B. 115 - 145 320 - 360 WBC Differential Counts (12 years or older) Absolute Neutrophils: 1.5 - 6.5 x 109/L Absolute Lymphocytes: 1.2 - 3.4 x 109/L Absolute Monocytes Count: 0.2 - 0.8 x 10 9/L Absolute Eosinophil Count: 0.0 - 0.4 x 109/L Absolute Basophil Count: 0.0 - 0.2 x 109/L Neutrophil Lymphocytes Monocytes Eosinophils Basophils 42.2 - 75.2% 20.5 - 51.1% 1.7 - 7.6% 0.0 - 5.0% 0.0 - 0.8% % % % % % - LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 7 of 9 Last printed 10/27/2014 12:57 PM x 109/L g/L g/L x 109/L C. D. E. Coagulation 1. INR: 0.9 – 1.3 Therapeutic Range INR: 2. Activated Partial Thromboplastin Time: 25 - 38 sec. Therapeutic Range: 55 - 80 seconds. 3. Fibrinogen: 1.8 – 3.5 g/L 4. D-Dimer: less than 500 ug/L FEU DVT 2.0 - 3.0 Recurrent P.E. 2.5 - 3.5 Chromogenic Assays and Special Coagulation Tests 1. Anti-Thrombin: 80% - 120% 2. Protein C: 70% - 130% of normal 3. Women Men Protein S Free 50 - 130% 70 -150% Functional Protein S 67 – 132% 4. APC Resistance 2.0 – 5.0 5. Anticardiolipin IgM Anticardiolipin IgG Anticardiolipin IgA 0 – 10 MPL/ml 0 – 22 GPL/ml 0 – 21 APL/ml 6. DRVVT Ratio 0.0 – 1.3 KCT Ratio 0.0 – 1.2 7. Bleeding Time 2 - 9 ½ minutes 8. VW Factor Antigen 50-200% of normal Lower Limit of normal is 40% for blood Group O individuals 9. Ristocetin CoFactor 50-200% of normal 10. Factor XII Assay 0.45 – 1.50 units/mL 11. Factor Assays (V,VII,VIII,IX,X,XI) 0.50 – 1.50 units/mL Erythrocyte Sedimentation Rate (ESR) 0 - 20 mm/hr LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 8 of 9 Last printed 10/27/2014 12:57 PM F. Body Fluids CSF: Clear, colorless RBC - 0 WBC - adults 0 - 5 x 106/L neonates 0 - 30 x 106/L Differential Lymphocytes Monocytes Neutrophils Eosinophils Adults 60% + 20% 30% + 15% 2% + 4% less than 1% Neonates 20% + 15% 70% + 20% 4% + 4% less than 1% Pleural, synovial fluids Clear, pale yellow WBC: Pleural 0 - 1.0 x 109/L Synovial 0 - 0.2 x 109/L RBC: 0 x 1012/L Differential - less than 25% neutrophils Peritoneal fluids Clear, pale yellow WBC: 0 - 300 per mm3 Dialysate fluids Clear, colorless WBC: 0.0 – 0.10 x 109/L RBC: 0 x 1012/L G. Lamellar Bodies < 15,000 /µL 15,000 – 49,000 /µL ≥ 50,000 /µL Immature Transitional Mature Revision History Found in Softtech Health Lab QMS™ Document Management System Author: Revised by Joan Isaak LABHemaOP7001.2 Hematology Laboratory Services Regina QuAppelle Health Region Page 9 of 9 Last printed 10/27/2014 12:57 PM Subject/Title: LABHemaOP7037.1.1 Flowcytometry Last Approved Time: 5/22/2013 9:08:05 AM Revision: 1.3 Approving Authority: Pathologist Contact for Interpretation:Flowcytometry Phone: (306) 766-6191 Current Version on Print Date Policy General Information Technical staff is available weekdays 0730 to 1630 hours (except statutory holidays). Specimens should be received at Pasqua laboratory by 1400 hours to facilitate processing. Out of hours tests are restricted unless authorization is obtained by physician of record from the Pathologist. Collection of Specimens Specimen Whole Blood for Flowcytometry Requirement 5 ml EDTA or Sodium Heparin (green). ACD is acceptable but Lithium Heparin is not. Whole Blood for 3-5 ml EDTA (mauve). CD4/CD8 1 microtainer EDTA (minimum of 250ul) Whole Blood for PNH 5 ml EDTA (mauve) or (Paroxysmal nocturnal 10 ml ACD (Yellow) hemoglobinuria) Bone Marrow Body Fluids Tissue specimen Fine Needle Aspirates (FNA) 1-3 ml collected in heparinized syringe and then placed in EDTA or Sodium Heparin tube Minimum of 40 ml in container with RPMI preservative and without any anticoagulant. Between 0.5 and 3.0 cm in RPMI preservation media. Place in 10ml RPMI preservation media. Additional Information Store and transport at room temperature. Specimen must be processed within 24 hrs of collection. Keep at room temperature. Specimen must be processed within 24 hrs of collection. Keep specimens at room temperature. EDTA specimen must be processed within 8 hrs of collection. ACD specimen must be processed within 24 hrs of collection Store and transport at room temperature. Specimens must be processed within 24 hrs of collection. Freshly collected and sent immediately. Store and transport at 4°C. Must be processed within 24 hrs of collection. Store and transport at 4°C. Specimens must be processed within 24 hrs of collection. DO NOT FREEZE. Store and transport at 4°C. Must be processed within 24 hrs of collection. LABHemaOP7037.1.1 Flowcytometry Laboratory Services Regina QuAppelle Health Region Page 1 of 2 Last printed 5/22/2013 9:08 AM List of Tests provided in Flowcytometry 1. 2. 3. 4. CD4/CD8 Leukemia Immunophenotyping Lymphocyte/Lymphoma Phenotyping PHN Testing (Paroxysmal nocturnal hemoglobinuria) Revision History Found in Softtech Health Lab QMS™ Document Management System Author Joan Isaak, MLT LABHemaOP7037.1.1 Flowcytometry Laboratory Services Regina QuAppelle Health Region Page 2 of 2 Last printed 5/22/2013 9:08 AM Subject/Title: LABHistOP1000 Histopathology Clinical Support Services Man Last Approved Time: 5/6/2013 8:14:15 AM Revision: 3.3 Approving Authority: Medical Pathologist Contact for Interpretation: Histology Phone: (306) 766-2075 Current Version on Print Date HISTOPATHOLOGY CLINICAL SUPPORT SERVICES MANUAL Hours of Operation: Technical Staff are available Monday to Friday, 0600 to 1530 hours. Non-technical staff are available Monday to Friday, until 1700 hours. Saturdays, Sundays and Statutory Holidays are not worked. I. SUBMISSION OF TISSUES FOR PATHOLOGICAL EXAMINATION 1. For routine pathological examination, the requirements are: Tissues should be immersed in 10% neutral buffered formalin immediately after removal. Volume of the 10% neutral buffered formalin should be at least 10 times the volume of the specimen. Tissues should not be squashed into small containers. 10% neutral buffered formalin for the nursing units and operating room is available from Histopathology at the Pasqua Hospital or the laboratory at the Regina General Hospital. affix gummed label to each specimen jar clearly indicating name of patient, HIN, HSN, surgeon, nursing unit, nature of specimen and date of surgery. the attending physician must complete and legibly sign the Histopathology request form and provide relevant clinical history, nature of specimen and date of surgery (include operative findings and details of previous surgery with dates). Where relevant provide obstetrical and gynaecological history. THIS IS A STATUTORY REQUIREMENT. 2. URGENT or over-night reports on tissue These tissues must be submitted to Histopathology no later than 1500 hours; only small biopsies can be processed this quickly. If it is considered that fixation is not complete; the specimen will not be processed: every effort will be made to notify the clinician. 3. Tissues for Microbiological Culture and subsequent Pathological Examination. These tissues should be submitted in a sterile container and should be sent immediately to Microbiology at the RGH in the fresh state with no formalin added. LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region Page 1 of 7 Last printed 5/6/2013 8:14 AM - The requisition should state clearly that a culture is required and, wherever possible, what organism is suspected. If pathologic examination is also required, a pathology requisition must also be completed. 4. Tissues for Quick Section This is routinely available Monday through Friday (except statutory holidays) and available at other times by direct arrangement between the physician of record and the pathologist on call. The equipment to perform Quick Sections is kept in the Histopathology laboratory and specimens should be sent by pneumatic tube or special messenger to Histopathology without delay. A pathologist should be informed before the specimen leaves the operating room. Call local 2228 at PH or use Phillips intercom system to call the Histology Lab. At RGH, call the pathologist at 4466 or page on pathologist’s pager 6290. The tissue should be fresh with no added formalin. 5. Tissue for Electron Microscopy If electron microscopy on tissue is required, Histopathology should be notified a day in advance so the proper solutions can be made. Phone local 2228 at PH. Dispatch the tissue immediately to the Histopathology laboratory in the fresh state with NO added solution. The requisition should state clearly that ELECTRON MICROSCOPY is required. A full clinical history must be supplied. For specimens originating from the RGH, notify the onsite pathologist at local 4466. Tests for Electron Microscopy are referred outside the region. 6. Tissues requiring photography with subsequent pathological examination. These should be sent immediately to the laboratory in the fresh state with no formalin added (Monday to Friday only). The requisition should state clearly that a photograph is required and also indicate what features are to be demonstrated. The pathologist on call must be notified for specimens procured out of normal working hours. 7. Immunofluorescence for bound immunoglobulin Tests ordered on renal biopsies are referred to Saskatoon City Hospital Pathology Department for testing. Pediatric (0-16 yr) renal biopsies are referred to Winnipeg Health Sciences Centre for testing. Testing of skin and oral mucosa biopsies is performed by Histopathology on a weekly basis. Tissues should be placed in Michel's fixative without refrigeration or freezing. Michel's fixative is available from Histopathology (local 2228). LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 2 of 7 Last printed 5/6/2013 8:14 AM 8. Tissue for conventional light microscopy should be submitted at the same time. Lymph Nodes and Open Lung Biopsies At PH Notify the Histology department (local 2228). Send immediately by special messenger to Histopathology, in the fresh state with NO added formalin. After 1700 h, special arrangements must be made with the pathologist on call. - At RGH Notify the on-site pathologist (local 4466). Send immediately by special messenger to the Laboratory, in the fresh state with NO added formalin. After 1700 h, special arrangements must be made with the pathologist on call. 9. Testicular Biopsies: Bouin's fixative is available from Histopathology upon request (local 2228). Notify a day in advance. 10. Amputated limbs Limbs which do not require pathological examination should be accompanied by a requisition clearly marked FOR DISPOSAL and should be placed in a vault in the Autopsy suite for later disposal. 11. After 1630 hours Specimens without fixative (i.e. fresh specimens) must not be left in the Histopathology Laboratory. For lymph node biopsies, kidney biopsies, thoracic biopsies, flow cytometry and other urgent specimens, contact the on call pathologist. 12. Muscle Biopsies: Processing and reporting of all muscle biopsies is performed by an external reference laboratory. The Histology laboratory requires 48 hours notice of the intent to perform a muscle biopsy. It is essential that the on-call pathologist receives notification of intent to do a muscle biopsy. Liquid nitrogen is not stored in the laboratory and can only be delivered Tuesdays and Thursdays, effectively restricting our ability to offer the service to Wednesday, Thursday and Friday. 13. Nerve biopsies: Processing and reporting of all nerve biopsies is performed by an external reference laboratory. It is essential that the Histopathology Laboratory (local 2228), receive 24 hour notification of the intent to perform a nerve biopsy so that the proper solutions can be made. LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 3 of 7 Last printed 5/6/2013 8:14 AM - II. Prior to commencement of the procedure, the pathologist on call must be notified so that they may ensure that proper protocol is followed. 14. Flow Cytometry: This is routinely available Monday through Friday (except statutory holidays) and available at other times by direct arrangement between the physician of record and the pathologist on call. Tissue submitted for Flow Cytometry must be submitted in RPMI medium and delivered immediately to the laboratory. 15. Chromosome Studies: Tissues submitted for chromosome studies are sent to an external reference laboratory for testing. Tissues submitted should be fresh with no added formalin and delivered immediately to the laboratory. The pathologist on call should be notified that a specimen has been sent for chromosome studies 16. Kidney Biopsies: Notify the pathologist on call prior to performing the biopsy. Ideal specimen: two kidney needle core biopsies each measuring 1-1.5 cm in length. These biopsies are placed between two pieces of filter paper that have been dampened with normal saline. Dispatch the tissue immediately to the Histopathology laboratory. A full clinical history must be supplied Kidney Biopsies are sent to Saskatoon City Hospital for testing. Pediatric (0-16 yr) cases are sent to Winnipeg Health Sciences Centre for testing. AUTOPSIES 1. CORONER'S AUTOPSIES: “Warrant for Post-Mortem or Other Examination” (Form C) must be completed by the coroner. This form is provided by the coroner. A coroner’s autopsy differs from a hospital autopsy in that the coroner’s order to perform an autopsy constitutes a legal consent and does not require the consent of the decedent’s family. The coroner should be notified in all cases of death due to: Homicide Suicide Accident Unusual circumstances which require investigation falling under the general category of “misadventure” NOTE: A Coroner should be called in those cases in which death is due to so-called “natural conditions” such as infection, renal failure, LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 4 of 7 Last printed 5/6/2013 8:14 AM pneumonia, etc., when those conditions are thought to be a consequence of an injury even when death occurs months or years following the initial incident. In doubtful cases it is advisable to discuss the case with the Coroner. 2. 3. HOSPITAL AUTOPSIES: All hospital autopsies require a completed and signed “Consent for Autopsy” (Form RQHR 064) before an autopsy can be performed. For the order of those who may give legal consent for a hospital autopsy - see list below The request for autopsy shall be made by the attending or consulting physician or his designate. A resident or house physician may request an autopsy after consulting with the attending or consulting physician. Nursing or Admitting personnel may obtain and witness the consent signature. If consent/permission is sought by telephone, the person obtaining permission and a witness to the telephone conversation must both sign the “Consent for Autopsy” (RQHR 064) form. There are no legal requirements making a hospital autopsy mandatory. COURTESY AUTOPSIES: A request must be made to the Director or pathologist on call. The following documentation is required: Valid consent from the legal next of kin. It is acceptable to use their own form or the “Consent for Autopsy” (Form RQHR 064) will be provided. Adequate legible or type-written clinical history (must not be photocopy of hospital chart) Referring agency to pay for transportation Courtesy autopsies are performed Monday through Friday subject to time constraints. They are not performed on weekends/holidays except in rare instances. THE FOLLOWING MAY GIVE CONSENT FOR AUTOPSY: 4.3 The Coroner The legal next of kin (in certain circumstances the executor or person lawfully in possession of the body). See list below. In the case of common-law relationship, the Pathologist must contact Risk Management (766-4979) for verification. Please refer to the following procedure - RHD Procedure No: 1.1.7 (Page 13) 4.3 Consent to Autopsy. Consent to Autopsy LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 5 of 7 Last printed 5/6/2013 8:14 AM The attending physician is responsible for ensuring that the individual providing the consent is aware of the nature, purpose, and effect of the consent. A Medical Resident may be appointed by the attending physician to explain the nature, purpose, and effect of the autopsy to the substitute decision maker or person lawfully in possession of the body. An autopsy requires a written consent using the Consent for Autopsy Form. When obtaining consent, the next-of-kin who may authorize autopsy are listed in order below. All except the spouse must be at least eighteen years of age: spouse (unless living separate immediately prior to the death or illness) children of the person either parent brother or sister any other next-of-kin the person lawfully in possession of the body other than the RHD, the Minister of Justice, or a funeral director When permission is obtained from a person other than the person or persons listed on the hierarchical list, the reasons should be documented on the health record. When the extent of autopsy is not indicated on the consent form, authorization for the complete autopsy is assumed. Under those circumstances which warrant a coroner’s investigation, no autopsy shall be performed unless and until authorized by the coroner. The completed “Consent for Autopsy” form and patient chart are to accompany the body to the Laboratory. The patient chart and “Consent for Autopsy” form must be left in the “Autopsy Permission Box” by the accession area at RGH or in the “Autopsy Permission Box” on the wall at Pasqua. Note: Under no circumstances should the “Consent for Autopsy” form and patient chart be sent to Health Records. References 4.3 Consent to Autopsy - Page 13 of RHD Procedure No: 1.1.7 (this can be found on the RQHR Intranet) Revision History Found in SoftTech Health Lab QMS™ Document Management System Author D. McHardy, MLT LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 6 of 7 Last printed 5/6/2013 8:14 AM LABHistOP1000 Histopathology Clinical Support Services Man Laboratory Services Regina QuAppelle Health Region LABHistOP1000.3.3 Histopathology Clinical Support Services Manual Page 7 of 7 Last printed 5/6/2013 8:14 AM Subject/Title: LABMicOP7204 MICROBIOLOGY LABORATORY SERVICES Last Approved Time: 4/15/2010 11:03:52 AM Revision: 2 Approving Authority:Medical Microbiologist Contact for Interpretation: Microbiology Phone: (306) 766-4481 Current Version on Print Date Policy Process Control Purpose This procedure provides information on the hours of operation and the scope of services provided by the Microbiology laboratory. It also provides guidelines for the collection and transportation of specimens for Microbiology. Hours of Operation Technical staff is available Monday to Friday, 0645 to 0000 hours. Saturday and Sunday technical staff is available 0745 to 1615 hours. Outside these hours, technical staff is on call. Scope of Service Bacteriology: - Bacterial culture - Organism identification - Drug susceptibility testing Mycobacteriology (Microscopy only. Culture will be sent to the Provincial Laboratory) Mycology Parasitology Virology (Limited viral screens are performed on In Patient specimens. All specimens are referred to the Provincial Laboratory for viral cultures) Clostridium difficile cytotoxin testing Trichomonas culture LABMicOP7204 MICROBIOLOGY LABORATORY SERVICES Laboratory Services Regina Qu'Appelle Health Region Page 1 of 3 Last printed 4/15/2010 11:03 AM Procedure Step Action Complete a Microbiology 1 requisition. Additional Information These are white or blue in colour. The white requisition is used by the Hospitals and Nursing Homes. The blue requisition is used by the community laboratories. Each form has a set of perforated numbers at the bottom. Removal of the tape enables the numbers to be firmly affixed to each specimen submitted for bacteriological examination. In the case of swabs, the labels should be applied along the length of the tube. Each number sticker must have name, MRN/HSN, specimen type and date filled in. The appropriate spaces at the top half of the requisition should be filled in by the Nursing Unit or Clinic, with all the pertinent information requested, including the diagnosis and antibiotic therapy. This information is important in the correct identification of the specimen, and also in determining the culture method to be used. 2 Collect specimen and transport specimens to laboratory. Refer to Appendix 1 for Specimen Containers for Microbiology. Refer to Appendix 2 for Microbiology Collection and Test Compendium. Refer to Table 1 for the Criteria for Rejection of Microbiology Specimens. Procedure notes All specimens and containers should be considered contaminated. Biohazard bags are not necessary for transport of specimens; however, personal protective equipment must be used. ie. Gloves. Gross contamination of specimen containers must be removed prior to transport (wipe visible contamination from specimen container with cotton ball soaked in 0.5% hypochloride solution or use an alcohol swab). Page 2 of 3 Last printed 4/15/2010 11:03 AM Reporting Results A direct gram smear will be performed and reported on all appropriate specimens. These results will be sent to the appropriate ward when results have been completed. STAT gram smears will be performed and results called within 30 minutes. When a specimen culture yields a pathogenic organism, the organism will be reported along with a list of antibiotics to which the organism is susceptible with standard adult dosage. Dosage adjustments must be made for other age groups, and for patients with underlying disease. eg. renal failure. Qualitative tests such as Clostridium difficile cytotoxin testing will be reported as “positive” or “negative”. Each individual test on a Microbiology report will be flagged as an “interim” or a “final” report. When results fall within ranges identified as “Critical”, Laboratory staff will telephone results to the nurse on the unit concerned or to the physician, or in the case of out-patient or referred in specimens to the clinic or physician’s office. Refer to Microbiology Critical Values. Related documents LABMicOP7202.T.1 Criteria for Rejection of Microbiology Specimens LABMicOP8000.A.3 Microbiology Critical Values Appendixes LABMicOP7204.A.1 Specimen Containers for Microbiology LABMicOP7204.A.2 Microbiology Collection and Testing Compendium LABMicOP7204.T.1 Criteria for Rejection of Microbiology Specimens Revision History Found in Softtech Health Lab QMS™ Document Management System Author Carol Barth, MLT. Page 3 of 3 Last printed 4/15/2010 11:03 AM Specimen Containers for Microbiology Used for transport of sterile tissue as well as skin and nail scrapings and hair for fungal culture. Supply stored at 4°C Swabs Transport Stool A B C A) SAF - Parasites (O&P) B) Sterile container without preservative - CD toxin, Viral C) Cary Blair w/indicator - Routine Culture (C&S) Urine Urine culture container with Boric Acid preservative minimum fill 5ml. Blood Cultures A e-Swab is used for all routine specimens when aerobic and/or anaerobic organisms are suspected including Neisseria gonorrhea, Trichomonas and Candida species. B C Cultures A) FA- Plus - Aerobic B) FN- Plus - Anaerobic C) PF- Plus - Pediatric **Vials for Mycobacterium available from Microbiology **For Complete instructions on Specimen collection and Transportation / Storage refer to the Microbiology compendium. 6914-15-MMS-ddh Viral Transport Sterile Container RQHR Microbiology Test Compendium The Regina Qu’Appelle Health Region (RQHR) Division of Microbiology, within the Department of Laboratory Medicine provides amalgamated service to all patients and providers within RQHR. The laboratory is staffed 24 hours a day, 365 days per year, with medical consultation available 24/7. Contact us: Laboratory Services, Microbiology Regina General Hospital 1440 – 14 Ave Regina, SK S4P 0W5 Phone: 306-766-4481 Fax: 306-766-4640 The Medical Microbiologist on-call can be reached through the hospital switchboards at 306-766-4444 or 306-766-2222. General Specimen Collection and Submission Requirements All specimens must be labeled and submitted with a completed requisition (see Laboratory Services Manual - General Information for further details). Specimens may be rejected if: they are improperly labeled or not accompanied by a completed requisition submitted in inappropriate container, received in leaking or otherwise compromised container Insufficient quantity of specimen, inappropriate specimen type for test requested, duplicate specimens, or if integrity of specimen has been compromised (e.g. lack of temperature control, delays in transit) Whenever possible, specimens for microbiologic detection should be collected before antibiotics are given. Care must be taken to avoid contamination of specimens with organisms of the normal flora or environment. Specimens should be delivered to the laboratory soon after they are collected. Delays in transport can lead to incorrect, invalid, or misleading results. The date and time of specimen collection should be recorded on the requisition in order to identify these delays and aid in results interpretation. Providing relevant clinical information will ensure specimens are processed and reported appropriately. This compendium describes routine testing performed. For special requests or additional information, please contact the Microbiology laboratory or Medical Microbiologist on-call. Last revised October 2015 Compendium of Tests TEST ON REQUISITION BLOOD & STERILE FLUIDS Blood Cultures SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES [See LABMicOP7021 Collection of Blood Cultures procedure for details] Bottles are incubated on an automated instrument with continuous monitoring until growth is detected, or for 5 days if negative. Positive gram stains are considered CRITICAL RESULTS and are phoned to submitting location immediately upon detection 24 hours per day. Once growth is detected, Gram stain is performed STAT and bottles are sub-cultured. Identification and susceptibility results are usually available 24 – 48 hours after organism is isolated. Adult blood culture bottles must be filled to the appropriate volume in order to achieve optimal dilution of ingredients. Over-filling or under-filling bottles will reduce the sensitivity of detection. Adults (≥16 years) set: 1 aerobic + 1 anaerobic bottle; 8 – 10 mL each Child (1 – 15 years) set: Collect approximately 1mL per year of age total. Divide total volume into multiple bottles as indicated. 1 – 4 years: 1 pediatric bottle 5 – 8 years: 2 pediatric bottles 9 – 15 years: 1 pediatric + 1 aerobic adult bottle Infant (0 – 12 months) set: 1 pediatric bottle (1 – 2 mL) For all adult collections, 2 sets collected from 2 separate sites will always be performed. One set should always be collected from a peripheral venipuncture. Label sites of collection. Reports of no growth are sent at 24 hours and 5 days, if applicable. Label bottles and provide information on requisition to identify the source of each blood culture set (e.g. sets labeled #1, #2; requisition indicates #1 venipuncture, #2 PICC line). Pediatric blood cultures will be drawn as a single set unless specifically ordered as 2 sets. Pediatric blood cultures will not include anaerobic culture bottles unless specifically requested. Transport at room temperature, as soon as possible and <24 hours. Do not freeze or refrigerate. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES CSF (Cerebrospinal fluid) Lumbar puncture Extraventricular drain Indwelling shunt Collect using sterile technique into sterile screw capped containers. Gram stain and culture for bacteria and yeast is performed routinely. Cultures are incubated for 7 days. Positive gram stains are considered CRITICAL RESULTS and are phoned to submitting location immediately upon detection 24 hours per day. Avoid sending first tube collected for microbiology testing due to increased risk of specimen contamination. Minimum volumes: Bacterial/yeast culture ≥1 mL Fungal culture ≥2 mL Transport at room temperature, as soon as possible and <2 hours. Do not freeze or refrigerate. Sterile Fluids Pleural fluid Peritoneal fluid Pericardial fluid Synovial fluid Bone marrow Collect using sterile technique into sterile screw capped container. Alternatively, collect 2 mL into a sterile screw capped container for Gram stain preparation, then inoculate aerobic and anaerobic blood culture bottles with 6 – 8 mL each. Transport at room temperature, as soon as possible and <24 hours. Do not freeze or refrigerate. Filamentous fungal cultures performed if ordered on requisition. Cultures are incubated for 4 weeks. All CSF specimens requesting filamentous fungal culture will have a qualitative Cryptococcal Antigen lateral flow assay (CrAg LFA) performed. Positive specimens will undergo semiquantitative titration. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 7 days. Identification and susceptibility results are usually available 24 – 48 hours after organism is isolated. Reports of no growth are sent at 24 and 72 hours, if applicable. Positive gram stains are considered CRITICAL RESULTS and are phoned to submitting location immediately upon detection 24 hours per day. If ordering additional testing from reference laboratory, ensure adequate volume is submitted: ≥2 mL for Mycobacterial culture, ≥1mL for viral isolation, and approximately 1mL per additional special request Swabs of sterile fluid are inappropriate specimens. This significantly compromises the sensitivity of organism detection. Filamentous fungal cultures performed if ordered on requisition. Cultures are incubated for 4 weeks. Reports of no growth are sent at 24 and 72 hours, if applicable. Specimens submitted in blood culture bottles will have negative Specimens submitted in blood reports sent at 24 hours and 5 culture bottles are incubated days. on an automated instrument with continuous monitoring until growth is detected, or for 5 days if negative. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Intravascular Catheter tip Disinfect surrounding skin before removal. Aseptically remove catheter and cut 1-2” of distal end into sterile container. Intravascular catheter tips are processed by a semiquantitative roll method, and incubated aerobically. If neonate or TPN, culture for Malassezia spp. is performed. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. Submit intravascular catheter tips only if there are signs of infection. If an intravascular line infection is suspected, blood cultures should be collected simultaneously. Collect 1 set from suspected intravascular line before removal, and collect 1 set from a peripheral venipuncture. Label sites of collection. CSF shunt and peritoneal dialysis catheter tips are flushed and vortexed with broth, which is then cultured semi-quantitatively. Reports of no growth are sent at 24 and 96 hours, if applicable. Tips from Foley catheters, chest tubes, and other drains are not accepted. Cultures are incubated aerobically for 4 days. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. WOUNDS/SURGICAL Superficial wound swab Clean wound thoroughly before swabbing affected areas. Avoid touching surrounding skin. Use liquid-based E-swab collection system (preferred) or M-40 Transystem swabs. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Gram stain and culture for aerobic bacteria and yeast is performed routinely. Cultures are incubated for 48 hours. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. Reports of no growth are sent at 24 and 48 hours, if applicable. If aspiration of wound is possible, this is preferred as it will more accurately identify pathogens and minimize isolation of colonizing organisms. Note: swabs from decubitus ulcers and pressure sores cannot distinguish infecting pathogens from colonizing organisms and are not routinely processed. Please submit tissue or aspirate specimens. Note: swabs are not appropriate for isolation of filamentous fungi Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Deep wound swab Clean wound thoroughly before swabbing affected areas. Avoid touching surrounding skin. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 72 hours. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. If aspiration of wound or tissue biopsy is possible, this will be preferred as it will more accurately identify pathogens and minimize isolation of colonizing organisms. Use liquid-based E-swab collection system (preferred) or M-40 Transystem swabs. Reports of no growth are sent at 24 and 72 hours, if applicable. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Note: swabs from decubitus ulcers and pressure sores cannot distinguish infecting pathogens from colonizing organisms and are not routinely processed. Please submit tissue or aspirate specimens. Note: swabs are not appropriate for isolation of filamentous fungi Aspirate/fluid/drainage Clean and decontaminate surface before collecting specimen. Aspirate ≥1 mL of specimen using sterile technique. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 72 hours. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. Specimen can be submitted to lab in a sterile screw capped container, or in capped syringe with needle removed. Filamentous fungal cultures performed if ordered on requisition. Cultures are incubated for 4 weeks. Reports of no growth are sent at 24 and 72 hours, if applicable. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. If Actinomycosis is suspected, please indicate under ‘Other/Special Requests’. Cultures will be incubated for 10 days. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING Tissue/biopsy Collect using sterile technique, into sterile screw capped container. You may add a small amount of sterile saline to keep tissue from drying out. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 7 days. Positive gram stains are considered CRITICAL RESULTS and are phoned to submitting location immediately upon detection 24 hours per day. Filamentous fungal cultures performed if ordered on requisition. Cultures are incubated for 4 weeks. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Bone Chip Collect using sterile technique, and place into sterile screw capped container. Bone bank products may be directly placed into tube of Thioglycollate broth. Transport at room temperature, as soon as possible. Do not freeze or refrigerate. If Actinomycosis is suspected, please indicate under ‘Other/Special Requests’. Cultures will be incubated for 10 days. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 7 days. Bone bank products are incubated in submitted Thioglycollate broth for 7 days. NOTES Reports of no growth are sent at 24 hours and 7 days, if applicable. Positive gram stains or detection of growth from bone bank specimens are considered CRITICAL RESULTS and are phoned to submitting location immediately upon detection 24 hours per day. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. Reports of no growth are sent at 24 hours and 7 days, if applicable. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Foreign body/implant Collect using sterile technique, and place into sterile screw capped container. Gram stain and culture for aerobic and anaerobic bacteria, and yeast is performed routinely. Cultures are incubated for 7 days. Identification and susceptibility results are usually available 24 – 48 hours after an organism is isolated. For unusual specimens or special requests, contact the Microbiologist on-call before submitting to laboratory. Transport at room temperature, as soon as possible. Do not freeze or refrigerate. ARO SCREENS MRSA (Methicillin-Resistant Staphylococcus aureus) Nares: insert into nostril 2-3 cm and roll swab 5 times. Insert same swab into second nostril and repeat. Groin: roll swab from top to bottom of inguinal area 5 times. Repeat using same swab on opposite side. Use liquid-based E-swab collection system (preferred) or M-40 Transystem swabs. Reports of no growth are sent at 24 hours and 7 days, if applicable. Real Time Polymerase Chain Reaction (RT-PCR) testing performed routinely. Newly identified colonization is confirmed with culture. Turnaround time ≤24 hours. Newly identified colonization confirmation available at 72 hours. Inpatient wards and Infection Control notified immediately of new positive results. New positive cases are reported to Public Health. Submit screens from nares, groins, invasive devices in place ≥1 month (e.g. tracheostomy, catheters), and open wounds. Only 1 requisition per patient is needed for all MRSA screening specimens. Repeat specimens received <7 days after a negative screen or <30 days after a positive screen will not be processed. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES VRE (Vancomycin-Resistant Enterococcus) Rectal swab: insert into rectum 2-3 cm and rotate 5 times Chromogenic screening cultures are performed routinely Turnaround time 48 – 72 hours. Repeat specimens received <7 days after a negative screen or <30 days after a positive screen will not be processed. Inpatient wards and Infection Control notified immediately of new positive results. New positive cases are reported to Public Health. Use liquid-based E-swab collection system (preferred) or M-40 Transystem swabs. Stool: collect 1g (~size of a hazelnut) of freshly passed stool into sterile container with no preservative (White top). ESBL/CRE (Extended Spectrum BetaLactamase / Carbapenemase Resistant Enterobacteriaceae) Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Rectal swab: insert into rectum 2-3 cm and rotate 5 times Use liquid-based E-swab collection system (preferred) or M-40 Transystem swabs. Stool: collect 1g (~size of a hazelnut) of freshly passed stool into sterile container with no preservative (White top). Chromogenic screening cultures are performed routinely Turnaround time 48 – 72 hours. Inpatient wards and Infection Control notified immediately of new positive results. New positive cases are reported to Public Health. Repeat specimens received <7 days after a negative screen or <30 days after a positive screen will not be processed. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Last revised October 2015 TEST ON REQUISITION URINE C&S only if positive urinalysis or C&S SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Midstream: hold labia apart (female) or retract foreskin (male), begin voiding and discard first several mL urine. Without stopping flow of urine, collect 5 – 10mL midstream specimen into wide-mouth sterile container. Urinalysis screening performed. Urinalysis results will be reported within 24 hours. If urinalysis is positive for leukocyte esterase (LE) or nitrites, specimen will undergo quantitative culture for uropathogenic bacteria. Cultures are incubated 24-48 hours. If specimen is cultured, organism identification is usually available 24 – 48 hours after it is isolated. If submitting urine for diagnosis of urinary tract infection (UTI), please order “C&S only if positive urinalysis”. A negative urinalysis has high specificity to rule out UTI. If urinalysis is positive for nitrites or leukocyte esterase culture will be performed routinely. Straight Catheter: thoroughly clean urethral area with mild soap and water. Aseptically insert catheter into bladder. Discard initial several mL urine, collect 5 – 10 mL. Indwelling Catheter: disinfect catheter collection port with 70% alcohol. Use needle and syringe to aseptically collect 5 – 10 mL of urine. Supra-pubic aspirate or Cystoscopy collection: collect 5 – 10 mL using aseptic technique. Transfer urine into tube containing Boric acid preservative and fill to indicator line. Sterile containers may be submitted if processed <2 hours after collection. If urinalysis is negative, this predicts the absence of a urinary tract infection. Specimen will not be cultured. If C&S is ordered, urine will be cultured without a urinalysis performed. Reports of no growth are sent at 24 hours, if applicable. Urine from pregnant women or individuals undergoing GU surgery/manipulation should order a regular urine C&S to ensure appropriate processing. Urine collected or received in non-sterile containers is unacceptable for culture. Catheter bags are not suitable for culture. Specimens collected in pediatric urine bags should be aseptically transferred into sterile container and tube containing Boric acid preservative. Repeat specimens received within 3 days will not be processed. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Culture for Salmonella spp., Shigella spp., Campylobacter spp., Shiga toxin producing E.coli (STEC), Aeromonas spp., and Pleisiomonas spp. performed routinely. Cultures are incubated 72 hours. Organism identification is usually available 24 – 48 hours after it is isolated. Repeat specimens received within 5 days will not be processed. If ordering “C&S only if positive urinalysis”, submit urine in both sterile container and preservative. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. STOOL Bacterial C&S Collect freshly passed stool into clean, dry container. Transfer to enteric transport media container (Cary Blair). Fill to line marked on container. There should be no contaminating material. E.g. urine, tissue paper. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Report of no pathogens Stool cultures are not detected is sent at 72 hours, if performed on patients who applicable. have been in hospital >3 days. Consider C.difficile testing in hospitalized patients with new onset diarrhea. Susceptibility testing is not routinely performed on enteric pathogens from patients without known risk factors. If antibiotic therapy is indicated, please contact the Microbiology lab at 766-4481. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING NOTES Clostridium difficile Collect 1g (~size of a hazelnut) of freshly passed stool into sterile container with no preservative. There should be no contaminating material. E.g. urine, tissue paper. All stools are initially tested for GDH and Toxin A/B using an enzyme immunoassay (EIA). Specimens with concordant results (i.e. GDH+/Toxin+ or GDH-/Toxin-) are reported immediately. Specimens with discordant results (i.e. GDH+/Toxin-) undergo PCR testing, and results of the PCR assay are reported. Turnaround time 24 hours. The rate of asymptomatic carriage of C.difficile in young children is high (up to 50% <3 years; up to 74% <1 year). Specimens from children <1 year will not be processed. Positive results in children <3 years should be interpreted with caution. Transport at room temperature, as soon as possible. If delay is anticipated, keep specimen at 4°C. Repeat specimens from patients with previously positive C.difficile <2 weeks will not be tested. Formed stools are not routinely processed. If patient is suspected of C.difficilerelated ileus, please clearly indicate on requisition or contact the Microbiology lab at 766-4481. Giardia/Cryptosporidium Collect freshly passed stool into clean, dry container. Transfer to container with SAF preservative. Fill to line marked on container and mix well. There should be no contaminating material. E.g. urine, tissue paper. Transport at room temperature, as soon as possible. Do not freeze. Specimens are tested by enzyme immunoassay (EIA) for detection of Giardia or Cryptosporidium antigens. Positive EIA results are confirmed with direct microscopy. Turnaround time 2 – 7 days Positive reports are sent to Public Health. Antibiotics, mineral oil, bismuth, kaolin, or barium will interfere with parasite detection. Delay specimen collection a minimum of 7 days after administration of these substances. Stool for Giardia/ Cryptosporidium is not performed on patients who have been in hospital >3 days. Consider C.difficile testing in hospitalized patients with new onset diarrhea. Last revised October 2015 TEST ON REQUISITION SPECIMEN COLLECTION & TRANSPORT TESTING PERFORMED TURNAROUND TIME & REPORTING Pinworm (Scotch Tape Test) Collection kits are available from Laboratory Stores. Direct microscopy is performed routinely Turnaround time 24 – 72 hours Direct examination and microscopy are performed routinely Specimens undergo direct examination for evidence of pathogenic stool parasites. Turnaround time 24 – 72 hours NOTES Collect specimen from the skin of the perianal area first thing in the morning before the patient has bathed or used the toilet. Remove screw cap with pinworm paddle, press sticky side to perianal area. Replace cap with paddle and tighten cap. Parasite Identification Full O&P exam Transport at room temperature, as soon as possible Transport suspected parasite to laboratory in leak-proof, wide mouth container. Collect freshly passed stool into clean, dry container. Transfer to container with SAF preservative. Fill to line marked on container and mix well. There should be no contaminating material. E.g. urine, tissue paper. Transport at room temperature, as soon as possible. Do not freeze. Turnaround time 7 - 14 days Positive reports may be sent to Public Health. Antibiotics, mineral oil, bismuth, kaolin, or barium will interfere with parasite detection. Delay specimen collection a minimum of 7 days after administration of these substances. Indicate on requisition risk factors warranting Full O&P. Specimens submitted without relevant history will be tested for Giardia/Cryptosporidium only. Last revised October 2015 Patient Instructions for Sputum Specimen Collection A sputum specimen collected first thing in the morning is the best specimen. At least 5mL (1 teaspoon) of specimen is required. 1. Label the specimen container with: i. The patient’s full name (last and first) ii. The date of collection iii. The patient’s Provincial Health Number 2. Gargle and rinse your mouth with water. This helps to eliminate accumulated cells and normal bacteria that may interfere with your test results. 3. Inhale deeply several times and exhale with an explosive cough. This should produce mucus from the lungs. Saliva (spit) from the mouth is not an acceptable specimen. 4. Cough specimen into the specimen container. 5. Replace lid and tighten securely so sample will not leak. 6. Transport the specimen with the requisition to the laboratory or collection site as soon as possible. If there is a delay of more than 2 hours in transporting, the specimen should be refrigerated. Notes: • An early morning specimen, collected before eating, drinking, or brushing teeth, is the preferred sample. • The specimen should be collected before starting antibiotics. • Saliva (spit) has a clear color. This is not a suitable specimen and will not be processed by the laboratory. • Specimen MUST be labeled with a first and last name, and a Provincial Health Number (HSN). If you do not have an HSN, please label specimen with patient’s first and last name, and date of birth. • Some tests require more than one specimen. If multiple specimens are requested, they must be collected first thing in the morning for 3 consecutive days. LABMicOP7204.A.3 Sputum COLLECTION.doc Patient Instructions for Stool Specimen Collection - Prior to collecting the samples (at least 48 hours), the patient should not take antacids (Rolaids, Tums), oily laxatives, or antidiarrheal medication (Kaopetate). Radiology examinations using bismuth, or barium should also be avoided if ova & parasite testing is requested. Collect one specimen for each test requested unless otherwise instructed. Collection of specimens from multiple days is usually not required. 1. Label the specimen container with: i. The patient’s full name (last and first) ii. The date of collection iii. The patient’s Provincial Health Number 2. Wash hands before beginning collection and after collection. 3. Urinate prior to stool collection, to avoid contaminating the specimen. 4. Pass stool directly into a clean, dry, wide mouth container, such as a plastic or Styrofoam cup or plate, or other plastic container, or plastic bag, or clean diaper. 5. Carefully open the specimen container and place on a table or counter. If it contains a fluid, do not discard it. This fluid is a preservative for the sample. These fluids are poisonous and must be kept away from children. If more than 1 specimen vial is required, fill only one vial at a time and replace the lid onto the same vial it came from. 6. Using the spoon attached to the lid of the specimen vial, add spoonfuls of stool to each vial so that the liquid reaches the “fill line” located on the label of the vial. If the vial does not have a “fill line”, then only add enough specimen to half fill the container. If the specimen is runny it may be poured directly into the specimen vial. It is important to take areas of the specimen which appear bloody, slimy, or watery. Hard stools are not acceptable for most testing. 7. Replace the lid and tighten securely so samples will not leak, and mix vial well. Proceed to the next container if more than 1 vial is requested. 8. Transport the specimen with the requisition to the laboratory or collection site as soon as possible. If there is a delay of more than 2 hours in transporting, the specimens for C&S and C. difficile Toxin testing must be refrigerated. Stools for O&P should be stored at room temperature. LABMicOP7200.A.4 Stool Collection Patient Instructions for Midstream Urine Collection 1. Label the specimen container with: i. The patient’s full name (last and first) ii. The date of collection iii. The patient’s Provincial Health Number 2. Wash hands with soap and water. 3. Use the sterile screw-capped container provided to you for collection. Open the container, and set the lid aside. Do not to touch the inside or the rim of the container. 4. Cleanse the entire genital area if you have been provided with a towellete. Discard towellete in to waste container. Thorough cleansing is very important in children, but is not imperative for specimens from female patients. 5. Urinate a small amount of urine into the toilet. This washes away some of the contaminating bacteria that normally reside on the urethra. 6. Continue urinating, then midway through move the container into the stream of urine and fill half to two thirds full. 7. Replace lid and tighten securely so sample will not leak. 8. Wash hands with soap and water. 9. If specimen was collected, on site, give to Clinic personnel. If specimen was collected at home, transport the specimen with the requisition to the laboratory or collection site as soon as possible. If there is a delay of more than 2 hours in transporting, the specimen should be refrigerated. LABMicOP7204.A.5 Urine Collection INSTRUCTIONS FOR PINWORM COLLECTION A. Laboratory Instructions Send patient home with a collection kit in a resealable bag. Collection kit will contain: i. A pinworm paddle ii. An instruction sheet iii. A requisition B. Patient Instructions 1. Collect specimen in the morning before taking a bath or going to the bathroom. (6:00am is the best time) 2. Label the container with: i. The patient’s full name (last and first) ii. The date of collection iii. The patient’s Provincial Health Number 3. Carefully remove the screw cap with the paddle 4. The paddle has one side labeled “Sticky Side” 5. Press the sticky side to the perianal area. The adhesive material on the sticky side will collect any pinworm eggs present 6. Avoid touching the sticky side with your fingers or hands 7. Place the pinworm collection container back into the resealable plastic bag. The collection kit can be stored at room temperature, and does not need to be placed in the refrigerator. 8. Return the requisition and the collection kit to the laboratory or Physician’s offices as soon as possible. If further assistance is required, please call the Microbiology Laboratory at (306)-766-4481. . Table 1: Criteria for Rejection of Microbiology Specimens Bronchial Washings Rule Exception - Washings are not processed for C&S, but are processed for AFB and Fungus Mini BAL will be processed only for tests requested - C&S is done on washings from ICU patients, or Dr. Jones, Dr. Dewar patients. - C&S is done on NICU patients, even if only 1 swab is received. ICU patients can have one sputum specimen for C&S daily. Specimen type Eye - Conjunctiva swabs are processed for C&S only when swabs from both eyes are received. MRSA Screens - Axilla swabs are not processd. Duplicate specimens for MRSA screening from the same patient within a 5 day period should be approved before they are processed. Sputum C&S - Sputum specimens for C&S from the same patient within a 3 day period are not processed. - Stool C&S - Stool specimens for C&S from the same patient within a 5 day period are not processed. Stool specimens for C&S on patients after 3 days hospitalization are not processed. - Additional testing may be required if clinical conditions indicate, but must be approved by the Microbiologist. Stool C. diff Toxin - - More than two stool specimens for C. diff Toxin from the same patient within a 5 day period, if the first one is positive, are not processed. Formed stool specimens are not processed. Stool O&P - Stool specimens for O&P on patients after 3 days hospitalization are not processed. - Additional testing may be required if clinical conditions indicate, but must be approved by the Microbiologist Throat Grp A Screen - Throat swabs from the same patient within a 24 hour period are not processed. - If susceptibility testing is required culture will be performed on the repeat specimen. Tips - All Central Venous Line tips are processed - All “other” tips must be approved before processing. Urine C&S - Duplicate urine specimens on the same patient in a 3 day period will not be processed. - Check previous culture result before canceling. VRE Screens - Only VRE screens from rectal swabs, or stool will be processed. * Rectal swabs must be stool stained to be acceptable. - All “other” sites must be approved by Microbiologist before processing. LABMicOP7204.T.1 Criteria for Rejection of Microbiology Specimens Laboratory Services Regina Qu'Appelle Health Region Page 1 of 2 Last printed 6/17/2013 2:58 PM Table 1: Specimen Problem Criteria for Rejection of Microbiology Specimens Rule Exception - Saliva, breast milk, 24 hour urine specimens, foley catheter tips, vomitus, gastric aspirate, and placenta swabs are all inappropriate specimens. (**Placenta tissue collected surgically is acceptable for culture.) Swabs of decubitis ulcers, such as coccyx, sacral, or ischial rectal. - Specimens from these sites are of limited value as they are colonized by organisms which will grow on culture but may not be the infecting agent. - Multiple Specimens - Multiple specimens from the same patient and the same source collected on the same day will not be processed. (eg. Urine, stool, sputum) - Inappropriate specimens - - LABMicOP7204.T.1 Criteria for Rejection of Microbiology Specimens Laboratory Services Regina Qu'Appelle Health Region Swabs of rectal abscesses are acceptable for culture. A biopsy is the preferred specimen. Exceptions: AFB requests, blood cultures, and specimens collected by invasive procedures. If multiple specimens from similar sources (swabs) are received, consult Microbiologist. Page 2 of 2 Last printed 6/17/2013 2:58 PM Subject/Title: LABMicOP7021 Collection of Blood Cultures Last Approved Time: 7/4/2012 7:35:06 AM Revision: 4.1 Approving Authority:Medical Microbiologist Contact for Interpretation: Microbiology Phone: (306) 766-4481 Current Version on Print Date Purpose This procedure provides instruction for collecting blood culture specimens. Blood cultures are critical in the diagnosis of bacteraemias and fungaemias, which are life threatening conditions. Strict adherence to the accepted methods for collection of blood cultures ie. timing, volumes, and numbers, are essential in the detection of pathogenic organisms. Failure to recognize bacteraemia and fungaemia leads to delay or lack of treatment. Also of importance is the use of aseptic technique in blood culture collection. Failure to do so can result in a contaminated specimen, ie. false positive culture, resulting in the inappropriate use of antibiotics. Collection and Timing 1. Collect blood aseptically by venipuncture. 2. The number of blood culture bottles taken during a single venipuncture defines a “set” of blood cultures. 3. Optimal collection of blood cultures is as follows: Bottles / Set Volume / Number Timing Bottle of sets 1 aerobic + 8 – 10 mL 2 Adult 1 anaerobic 8 – 10 mL (>12 yrs) Child Simultaneous 1 pediatric + 1 – 3 mL 2 (6 – 12 yrs) Or 20 to 30 1 anaerobic 8 – 10 mL minutes apart (1 – 6 yrs) 1 pediatric 1 – 3 mL 2 1 pediatric 1 – 3 mL 1 Neonate – 1 ** yr. **For infants and young children the volume drawn must not exceed 1% of the patient’s total blood volume. Reagents Blood Culture vials Supplies BD Push Button Blood Collection Set, alcohol swabs, cotton balls, Band-Aid, tourniquet, vacutainer holder Special Safety Precautions Universal body substance precautions. Refer to the Safety Manual for general safety requirements. LABMicOP7021 Collection of Blood Cultures Laboratory Services Regina QuAppelle Health Region Page 1 of 3 Laboratory Services Regina Qu'Appelle Health Region @BCL@C00BA06F.doc Procedure STEP ACTION Place required equipment within easy reach 1 Mark 8 to 10mL level on the aerobic and anaerobic vials. Mark the 1 to 3mL 2 level on the pediatric vial. Remove flip caps from blood culture vials and clean vial tops with alcohol swab; 3 do not use iodine or disinfectants to swab rubber caps on vials. Select vein and prepare arm using a double application of 70% alcohol starting at 4 the centre of the site and swabbing concentrically for 1 minute. Allow the venipuncture site to dry. Do not touch the venipuncture site after 5 preparation or prior to phlebotomy. Screw a vacutainer holder onto the needle farthest from the butterfly. Remove sleeve from needle closest to butterfly. 6 Perform venipuncture 7 Tape tube to arm just below the butterfly 8 Insert multi sample needle into blood culture bottle. The multi sample needle 9 must be held in place in the vial. Remove the needle from the aerobic vial and insert the needle into the anaerobic 10 vial. Remember to hold the needle in place. Fill vial to the level you previously marked on the vial. 11 Proceed to collect required vacutainer tubes following the regular venipuncture 12 procedure. Release tourniquet and remove needle from vial. 13 Cover puncture site with gauze/cotton, then activate the safety device. 14 Remove needle from arm and apply pressure to cotton swab on venipuncture site. 15 Place butterfly needle unit into needle disposal container by placing sharp edge of 16 both needles together and insert sharp edges first. Time, date and initial requisition 17 Locate bar code on side of bottle. DO NOT mark it or cover it in any way. 18 Write the patient’s name on the bottle. 19 Blood cultures should not be refrigerated, but delivered to the Microbiology 20 laboratory immediately. If collected at Pasqua, leave bottles at room temperature until they can be transported to RGH. Procedure Notes 1. A solitary blood culture is not acceptable except in neonates. Blood cultures from two separate venipunctures are required. If a blood culture is required and only one requisition is supplied, request a second requisition for the second collection. Two sets of cultures increase the chances of detecting bacteraemias, and aids in the differentiating contamination from true episodes of bacteraemia. 2. Drawing blood through indwelling intravenous or intra-arterial catheters should be avoided as they are associated with higher rates of contamination. If blood is drawn via an indwelling catheter it must be accompanied by a culture drawn from a peripheral venipuncture. Page 2 of 3 Last printed 7/4/2012 @BCL@C00BA06F.doc 3. 4. 5. 6. 7. The volume of blood is critical because the concentration of organisms in the majority of bacteremias is low, especially if the patient is on antimicrobial therapy. Culture of larger volumes of blood increases the recovery of pathogens and also decreases the time to detection. Three blood cultures are the maximum number required to diagnose an episode of septicemia. If bacterial endocarditis is suspected, 3 to 5 cultures may be collected over a 48 hour period. Collect 3 cultures initially, and if these are negative at 24 hours, a further 2 may be collected. When orders for more blood cultures are received, contact the Microbiologist. The recommended blood to broth ratio is 1:5 to 1:10. Dilutions beyond 1:10 occur by necessity in blood cultures of infants and small children. Extended incubation of blood cultures from patients with suspected SBE is not required. Caution must be taken if you are using the BacT/Alert Blood Collection Adapter Caps in combination with a third-party blood collection set. Some blood collection sets have incompatible threads and the blood collection, even when the needle is screwed all the way down, the threads do not firmly connect, and the luer needle could back out of the adapter cap during use. To reduce the chance of this happening, maintain control of the luer connector by securing it between the thumb and forefinger during the venipuncture. References 1) Isenberg, HD., Clinical Microbiology Procedure Handbook, ASM Press, 2004 2) Baron, EJ. et al, Blood Cultures IV, Cumitech, 1C, 2000. 3) Clinical and Laboratory Standards Institute (CLSI) M47-P. Principles and Procedures for Blood Cultures ; Proposed Guidelines. Revision History Found in Softtech Health Lab QMS™ Document Management System Author Carol Barth, MLT. Page 3 of 3 Last printed 7/4/2012 Subject/Title: LABTranOP7001.6.1 Transfusions Laboratory Service Manual Last Approved Time: 1/31/2013 1:45:06 PM Revision: 6.1 Approving Authority : Medical Hematopathologist Contact for Interpretation: Transfusion Supervisor Phone: (306) 766-4474 Current Version on Print Date TRANSFUSIONS I LEGAL RESPONSIBILITY A. Physician/ Authorized Practitioner: The ordering physician is responsible for using clinical judgement to determine that the benefits to be obtained from transfusion outweigh the risks. They are also responsible to obtain informed consent for the transfusion and to ensure that the necessary clinical information is available to the laboratory. B. Medical and/or Nursing Staff or Perfusionist: The Medical and/or Nursing Staff or Perfusionist are responsible for ensuring that blood administered to the patient is the blood crossmatched for the patient, as identified by its labelling and it is administered in a safe manner. C. Laboratory: The laboratory is responsible for maintaining adequate blood product within the limits of the national supply, maintaining satisfactory blood storage conditions and using safe testing techniques. II SUPPLY OF BLOOD Every effort will be made to supply blood at the time requested. If sufficient advance notice is given, inability to fill an order will be unusual. III ORDERING BLOOD TRANSFUSIONS A. Blood Specimens: The sample required for an ABO Group, Rh type and cross match (compatibility testing) is 2 x 3mL two mauve top Vacutainer tubes. Ensure that the patient armband is legible and affixed to the patient. (Phlebotomy staff and technologists are instructed that a specimen must not be taken unless these conditions are met.) In the case of unconscious LABTranOP7001.6.1 Transfusions Laboratory Service Manual Laboratory Services Regina QuAppelle Health Region Page 1 of 10 Last printed 1/31/2013 1:45 PM patients who have not yet been identified, an unidentified number is assigned; it is vital that the armband bearing this identification is not removed prematurely. Patients who are leaving the hospital and returning for transfusion (i.e. pre-surgical, outpatients and patient transfers) must be identified by a red armband attached at the time of collection. This armband must be affixed to the patient when they return for transfusion. Confirm the patient's identity by checking - first and last name - medical record number and - date of birth on the wristband against the requisition before taking the specimen. Label the specimen tubes with the patient's first and last name, hospital identification number, red armband number, date of birth and the date of collection. Technologists are instructed to reject specimens that are inadequately labelled or unsatisfactory in quality or amount. Specimens are stored for 35 days and may be used up to 14 days for crossmatch providing the patient has not been pregnant or transfused in the last three months. Specimens from patients who have been pregnant or transfused within the last three months samples may be used up to 96 hours. Neonatal specimens may be used for up to 4 months from the date of birth, regardless of previous transfusions. If more than 96 hours have elapsed since a transfusion, a new specimen must be sent for further crossmatching in case new clinically significant allo-antibodies have developed. B. Blood Transfusion Requisition: The information requested on the form is essential in aiding the laboratory staff. The following must be given: 1) The name and date of birth of the patient 2) Medical Record Number 3) Patient location 4) Date of order 5) Blood Product type and amount required 6) Diagnosis 7) Date of surgery or transfusion if applicable 8) History of previous transfusions, blood group, antibodies and pregnancy 9) Ordering physician Technologists are instructed not to accept incomplete or illegible requisitions. C. Blood Products Transferred with Out of Town Patients: All transported blood products that arrive in the hospital must be left in the sealed container, and delivered immediately to the Transfusions Department. Breaking the seal will result in wastage of transported products. Page 2 of 10 Last printed 1/31/2013 1:45 PM IV ISSUE OF BLOOD When the testing has been completed a computer-generated report is printed on the Unit. The report contains the patient's ABO and Rh type and results of the antibody screen. Affix this form to the patient's chart. When the blood is required, present a slip of paper indicating the patient's first and last name, hospital identification number, date of birth and the type of blood product required to the Transfusion technologist. If the patient’s has a red armband, the unique identification number is required. In order to maintain the integrity of the blood product, only one unit of blood will be issued at a time except in circumstances where the product will be infused quickly. A two part pink tag is attached to the donor unit containing the patient name, donor unit number, patient and donor blood group and compatibility status. The technologist performs a verbal check with the portering personnel for transport to the ward. The porter name is recorded and the person receiving the product and the technologist sign the crossmatch tag. V PATIENT NOTIFICATION All patients who receive human blood products are given a “Notification of the Administration of Blood and Blood Products” form. This form is given with the first product transfused in each patient stay. Upon discharge the nurse must review this information with the patient and have the patient sign the form. VI BLOOD INFUSION All transfused patients must have provided informed consent prior to transfusion. The patient shall be informed with a description of the blood component, the associated and benefits, including life-threatening risks and alternatives to transfusion. This consent shall be documented on the patient Health Record chart. 1. Check the information on the pink crossmatch tags, and Blood Bank Report. Check that the patient's name, medical record number, date of birth and ABO Group and Rh. Check that the donor ABO Group, Rh and unit number on the pink tag is the same as on the label of the blood pack. Sign with date and time the white and pink tags to indicate that the information has been verified. Remove the pink copy of the crossmatch tag and attach to the chart. NOTE: Do not remove the white tag from the unit until the infusion is complete. NOTE: It is not necessary to verify the unit numbers against the Blood Bank Report. 2. Check the identity of the patient carefully by comparing the wristband with the white tag of the blood pack. Check the patient's first name, last name, medical record number and date of birth. This must be done in full. Failure to do this is the major cause of transfusion accidents. 3. Check the patient vital signs as per the nursing protocol Page 3 of 10 Last printed 1/31/2013 1:45 PM 4. Transfusions must be started within 30 minutes of product issue. Return units to Transfusions if unable to hang immediately. Do not put blood in nursing unit refrigerator. 5. Infusion rate is as prescribed by physician / authorized practitioner. 6. Infusion must be completed within 4 hours of blood issue. 7. Infuse blood slowly during the first 15 minutes as the signs of a severe transfusion reactions often appear early in the transfusion. 8. Blood must be warmed using approved blood warming apparatus only. Serious hemolysis may occur with over-warming. 9. Do not add any medication to the blood product. 10. For additional information on the administration of blood and blood products, see the Circulars of Information found in on the Intranet. 11. Return all empty blood bags (used, unused, partially used) to the laboratory the same day. Package each empty pack individually in a plastic bag with the tag outside of the bag and secure with tape or a twist tie. DO NOT leave needles attached. If there is blood left in bag, please close off the port before placing in plastic bag to prevent leakage while being transported to the lab. 12. Certain wards do not return the blood pack to the lab unless there is a transfusion reaction. Remove the white tag at the completion of the transfusion and return to the lab. All empty bags must be kept on the ward for 4 hours post transfusion prior to discard. VII CANCELING BLOOD To assist the Laboratory in making the most efficient use of the donor blood inventory, notify the Laboratory immediately when blood is no longer required for a patient. VIII SHORTAGES OF BLOOD Due to variation in supply and demand, shortages of blood occur from time to time. One consequence of this may be an acute shortage of a particular group (most commonly O Rh Negative). It may be necessary on occasion to issue blood of a different group than the patient. This will be done based on established protocols, or in consultation with the Transfusion Medicine Physician. IX EMERGENT AND ROUTINE TRANSFUSIONS A. EMERGENT Transfusions: An emergent request for transfusion should be made when blood is required to preserve life. Page 4 of 10 Last printed 1/31/2013 1:45 PM In such situations, uncrossmatched O Negative blood, or uncrossmatched blood of the patient's group, may be issued on the responsibility of the ordering physician. Group-specific blood takes a short time (approximately 10 minutes) to obtain and is preferred to O Negative blood (due to limited supply). “STAT” crossmatch requests will be processed as soon as possible. Note: Refer to the General Lab section for a complete list of turnaround times B. ROUTINE Transfusions: Requests for blood should, whenever possible, be made before 1400 hours on the day before the blood is needed. Elective transfusions should not be requested on evenings or nights to ensure adequate ward staff is available to properly observe the patient and manage any adverse reactions. X CONFIRMATORY BLOOD GROUP A second blood group test will be requested and collected on all non-emergent patients who do not have a historical blood group on file. The confirmatory blood group protocol was implemented as a risk reduction system. Patient misidentification occurs at sample collection in approximately one out of every 1,000 samples. XI CROSSMATCHES FOR SURGERY Patients who are likely to need transfusion during surgery should have their blood group determined and screened for antibodies prior to surgery. XII CORD BLOOD All newly delivered infants have a specimen of umbilical cord blood taken as soon after delivery as possible from the placental end of the cut cord. Draw the specimen into 1 x 7 mL red top tube (clotted blood) and 1 x 3 mL mauve top tube (EDTA anticoagulant). Label the tubes clearly with the infant's surname and medical record number. If infant and mother’s surnames are different, label tubes with both names. Send the sample with a properly completed maternal requisition to the Transfusion Laboratory. Laboratory testing will be performed if required. If the baby has a positive Direct Antiglobulin Test, additional testing will be performed as indicated. XIII EXCHANGE TRANSFUSION Exchange transfusion is used as a treatment for severe hyperbilirubinemia secondary to hemolytic disease of the newborn. Removing the infant's plasma both reduces the load of bilirubin and the amount of unbound antibody. Antibody-coated cells, whose destruction would further raise the bilirubin load, are removed and replaced with red cells compatible with the maternal antibody. Page 5 of 10 Last printed 1/31/2013 1:45 PM Specialized blood products are required for neonatal transfusions. XIV NEONATAL TRANSFUSION The Transfusion Laboratory aliquots a unit of packed cells for small volume transfusions. This unit will be used until outdate for the assigned baby. XV AUTOLOGOUS AND DIRECTED DONATIONS Canadian Blood Services will collect units of blood for a patient’s own use if requested by the attending physician. These units are specially labeled and can only be used for the donor. The patient will bring a portion of the autologous label and a letter for the ward explaining that autologous units are available along with a letter explaining the process to the ward on admission. Place the green tags on the Health Records chart along with the letter. The patient’s own blood must be used prior to any other units. Canadian Blood Service also operates a directed donation program for parents donating to children under the age of 17. Please contact the Transfusions Lab for information on this program. XVI BLOOD REQUIRED FOR LABORATORY TESTS Test requested Group and Rh Only (including confirmatory blood group) Specimen required 1 x 4 mL mauve Antibody Screen Cross match Group and Reserve Serum 2 x 4 mL mauve Direct Antiglobulin Test 1 x 4 mL mauve Cold Agglutinin testing 2 x 6 mL red top 1 x 4mL mauve top (must be maintained at 37°C) 1 x 6mL red 1 x 4mL mauve Cord Blood Testing Vacutainer Key RED MAUVE No anticoagulant for clotted blood. Do not use the serum separator tubes (SST) EDTA Anticoagulant Page 6 of 10 Last printed 1/31/2013 1:45 PM XVII ADVERSE EFFECTS OF TRANSFUSION Notify the Physician and report all adverse reactions to the laboratory immediately. Return the unit of blood to the Transfusion department as soon as possible accompanied by the tag. The back of the tag should be completed with all pertinent information. 1. Febrile Non-Hemolytic Reaction A febrile reaction is suspected if the patient has one of more of the following; a fever (>38°C and a change of ≥ 1°C from pretransfusion value), chills, sensation of cold or rigors. These signs and symptoms may be observed during the transfusion or within 4-6 hours of its completion without any other apparent cause. A fever can have many causes unrelated to blood transfusion; therefore, a blood transfusion is not necessarily discontinued if a fever develops. Most febrile transfusion reactions are mild and may be treated or prevented by the administration of antipyretics such as acetaminophen prior to the transfusion. Severe febrile symptoms may indicate a more serious reaction, such as acute hemolytic reaction or bacterial contamination. 2. Allergic Reactions - Minor Symptoms include transient urticarial or other skin rash with pruritus associated with the transfusion. This may be associated with fever. The cause of urticaria is thought to be a reaction to a soluble antigen in the donor plasma. Mild urticaria is usually harmless and should be treated with antihistamines. It is not necessary to discontinue the transfusion as long as serious symptoms (below) are not present. 3. Allergic Reactions – Severe/Anaphylactic Signs and symptoms of a severe allergic reaction can include rash greater than 2/3 BSA, respiratory symptoms (tightness in throat, cough, hoarseness, dyspnea, wheeze, hypoxemia) and unstable vital signs (hypotension, tachycardia). The reaction may progress to respiratory failure and circulatory collapse. Anaphylactic reactions occur in individuals who are IgA deficient and who have developed antibodies to IgA. These antibodies react with IgA in transfused plasma. It should be noted that it is possible for reactions to occur even during the first transfusion. Stop the transfusion immediately, keep the I.V. open with normal saline to allow for the administration of medications as ordered by the physician. 4. Hemolytic Transfusion Reactions Page 7 of 10 Last printed 1/31/2013 1:45 PM Signs and symptoms include fever, chills, nausea, hypotension, chest or back pain, shock, generalized bleeding, hemoglobinuria, oliguria or anuria within 24 hours of the receipt of the transfusion. Hemolytic transfusion reactions are caused by the intravascular destruction of red blood cells. This usually follows the transfusion of ABO incompatible blood given to a patient that has been improperly identified. Hemolytic reactions may also occur following the transfusion of blood that has outdated, is bacterially contaminated or that has been damaged by freezing or heating. Action to take if an Acute Hemolytic Transfusion Reaction is suspected: a) b) c) d) e) f) g) h) i) Stop transfusion and maintain the IV line with normal saline. Check patient’s vital signs and commence oxygen if required. Notify physician and the laboratory immediately and request an investigation. Check patient identification against blood and sign on the back of the pink tag to confirm that the clerical check was done. Note the nature and severity of the reaction on the back of the pink tag. Send the remaining donor blood to the laboratory for investigation. Collect the first urine passed following the reaction. Send to the laboratory for a routine urinalysis and free hemoglobin. Monitor the urine output. Have a post reaction serum bilirubin done. Treatment of a hemolytic reaction is determined by the specific symptoms. Treat hypotension with fluid replacement. Induce and maintain urinary flow by fluid replacement and diuretics. Dialysis may be required. If the patient has symptoms of a hemostatic disorder laboratory tests will determine if platelets or specific coagulation factors should be given. 5. Delayed Hemolytic Transfusion Reaction Delayed Hemolytic Transfusion reactions may occur 3 days to 2 weeks after transfusion. The patient typically presents with hemolytic anemia (low haemoglobin, high bilirubin, reticulocytosis, spherocytosis, high LDH), a positive antibody screen, and a positive direct antiglobulin test (i.e., DAT, Coombs’ test). Most are benign, but life-threatening hemolysis with severe anemia and renal failure may occur. Notify physician and Transfusion Laboratory immediately. 6. Bacterial Contamination- Acute reaction Despite the observance of aseptic technique during collection and processing, the possibility of bacterial contamination (usually by normal skin flora) still exists. This contamination does not usually cause clinical problems because the products are stored at temperatures that inhibit bacterial growth. However, when the storage or administration of a blood product does not meet accepted standards, proliferation of bacteria may occur and cause serious harm to the patient. Page 8 of 10 Last printed 1/31/2013 1:45 PM Symptoms of a reaction include high fever, hypotension, shock, hemoglobinuria, DIC and renal failure. Stop the transfusion immediately and notify the Transfusion Laboratory. Send the product to the laboratory for Gram stain and culture. Blood cultures on the patient are also recommended to help establish that the blood product was the cause of any infection. Treatment includes supportive care, including appropriate antibiotics. 7. Disease Transmission – Delayed reaction Infectious diseases may be transmitted in spite of careful selection of donors and testing of blood. Donor selection criteria are designed to screen out individuals who are at high risk for viral infections, including HIV, hepatitis B and C, and HTLV. Testing is also performed on all units prior to release. For a complete listing of tests, see the Canadian Blood Services Circular of Information. 9. Circulatory Overload Pulmonary edema may develop rapidly in a patient who has received too much or too rapid an intravenous infusion, particularly in patients with renal failure, heart failure or severe chronic anemia. The symptoms include dyspnea, cyanosis, orthopnea, severe headache, hypertension or congestive heart failure during or soon after the receipt of a transfusion Be circumspect in transfusing such patients. It is wise to limit the patient to no more than 2 units of packed cells per 24 hours, watching carefully for signs of heart failure. If circulatory overload occurs, treat with elevation of head of the bed, diuretics, etc. 12. Transfusion Associated Graft Versus Host Disease (TA-GVHD) Blood products are routinely irradiated to prevent GVHD for high risk populations. TA-GVHD is extremely rare and most commonly occurs in immunocompromised recipients who do not receive irradiated blood products. Symptoms of TA-GVHD include fever, skin rash (which often starts on the palms, the soles of the feet and the ear lobes), elevated liver enzymes (ALT and AST, Alkaline phosphatase) and bilirubin, pancytopenia and diarrhea. The reaction is very severe and results in death in over 90% of the cases. 13. Transfusion Related Acute Lung Injury TRALI is suspected if the recipient experiences acute pulmonary edema in the absence of cardiac failure within 6 hours of the receipt of a transfusion. Symptoms include dyspnea, cyanosis, chills, fever and hypotension. Page 9 of 10 Last printed 1/31/2013 1:45 PM 14. Other Complications Other rare adverse events such as iron overload, Post Transfusion Purpura, hypotensive reactions and Aseptic Meningitis have been associated with transfusion. The Transfusion Medicine Physician on call should be contacted if any of these are suspected. XVIII PRODUCT INFORMATION Information on blood and blood products can be found in Appendix A of this procedure, the Canadian Blood Services Circular of Information (a copy is found with this manual) and package inserts from the fractionated blood products. The Clinical Guide to Transfusion supplied by Canadian Blood Services and the Bloody Easy book sponsored by Ontario are both excellent, informative books available for information on transfusion medicine. Additional information can be obtained from the technologists in the Transfusions Department, or the Transfusion Medicine physician on call. References 1. American Association of Blood Banks, Technical Manual, 16th ed., 2008 2. Canadian Society for Transfusion Medicine Standards for Hospital Transfusion Services Version 3- February 2011 3. Canadian Blood Services Circular of Information 4. Public Health Agency of Canada Adverse Event Definitions User’s Manual Version 3.0 November 2007 5. Clinical Guide to Transfusion, fourth edition, CBS, July 2006. Related Documents 1. 2. 3. 4. Appendix A – Blood Product Insert – LABTranOP7001W1.1 Turn Around Time – LABTranOP7001W2.1 Transfusions Critical Values – LABTranOP7001W3.1 Laboratory Service Manual – General Information Revision History Refer to Document Control Log Author: Renee Masters-Guest MLT Judy Hoff ART, MLT Paula Van Vliet ART, MLT Page 10 of 10 Last printed 1/31/2013 1:45 PM Subject/Title: LABTranOP7011 Use of the Typenex Red Arm Band System Last Approved Time: 6/27/2012 8:39:23 AM Revision: 2.2 Approving Authority : Medical Hematopathologist Contact for Interpretation: Transfusion Supervisor Phone: (306) 766-4474 Current Version on Print Date Purpose This procedure provides instruction for use of Typenex stickers on red armbands and RQHR bar-coded armbands for continuity of patient identification. Sample Information Typenex armbands ensure the continuity of identification for patients who require blood group and antibody screen and are not staying in the hospital such as surgical assessment patients, outpatient transfusions or patients being transferred to another facility for diagnostic procedures. RQHR bar-coded arm bands are given to patients on hospital admission through Emergency, Day Surgery or direct ward admission. Cardiac surgery or angioplasty patients must have 2 armbands, one applied to each arm. The Transfusion requisition may be marked as either one of the following: OHS, CAD, CABG, AVR, MVR, Heart surgery, Angio, Bentalls procedure or PTCA. Supplies Completed Transfusion Requisition with the following information: o First and last name o Date of birth o MRN or HSN o Patient location o Order date o Product required o Diagnosis o Transfusion and/or pregnancy history o Surgery or transfusion date o Ordering physician Red number sheets with barcode Typenex arm bands, cardboard inserts/or RQHR bar-coded patient arm bands 2 mauve EDTA tubes LABTranOP7011 Use of the Typenex Red Arm Band System Laboratory Services Regina QuAppelle Health Region Page 1 of 4 Last printed 6/27/2012 8:39 AM Special Safety Precautions Refer to the Safety Manual for general safety requirements. Note Two arm band processes are used within the RQHR for patient identification dependant on patient location, the Typenex red arm band and the RQHR bar-coded arm band. Procedure for Red Typenex arm bands STEP 1. 2. 3. 4. 5. 6. 7. 9. 10. 11. ACTION If the patient is wearing an armband with a red number, STOP and phone Transfusions to verify the need for a crossmatch or directions on how to proceed. On the cardboard insert, write legibly or attach a label prepared by LIS, which contains the following information: First and last name date of birth MRN or HSN if available Insert the cardboard into the red plastic armband. Seal the open end of the card slot. Remove the long sticker from the right side of the red number sheet and wrap it around that end of the Typenex arm band covering the card slot. Securely fasten the red armband to the patient’s arm. In the case of cardiac surgery / angioplasty patients please fasten the red armband to both arms. See Sample Information for a list of diagnosis. Perform collection as per LABPhlbOP7017 Protocol for Performing a Venipuncture Attach one red sticker to: Each properly labeled blood sample making sure not to cover the patient identification or the barcode. Transfusion requisition Explain to the patient the importance of leaving the band on. If it is removed for any reason: The sample will have to be redrawn The surgery or procedure may be delayed Attach the additional stickers to the requisition. When accessioning the sample in the LIS ensure that the Typenex (red) number is entered. Procedure for RQHR bar-coded arm bands 1. If the patient is wearing a armband with a red number, STOP and phone Transfusions to verify the need for a cross match or directions on how to proceed Page 2 of 4 Last printed 6/27/2012 8:39 AM 2. The RQHR barcoded band is printed with patient’s admitting information and barcodes on the waterproof arm band. Remove the long sticker from the right side of the red number sheet and wrap it around the right side of the arm band away from the barcodes, making sure the red number is on the same side as patient’s information. Securely fasten the RQHR armband to the patient’s arm. In the case of cardiac surgery / angioplasty patients please fasten an armband to both arms, a red armband can be used for the second band. See Sample Information for a list of diagnosis. Perform collection as per LABPhlbOP7017 Protocol for Performing a Venipuncture. Attach one red sticker to: Each properly labeled blood sample making sure not to cover the patient identification or the barcode. Transfusion requisition Explain to the patient the importance of leaving the band on. If it is removed for any reason: The sample will have to be redrawn The surgery or procedure may be delayed 3. 4. 5. 6. 7. 8. 9. Attach the additional stickers to the requisition. When accessioning the sample in the LIS ensure that the Typenex (red) number is entered. NOTE Once the patient has been admitted they can be identified using regular hospital armband procedure. The Typenex red number is unique and the same number cannot be used twice. If an error occurs, attach another armband and discard the other numbers. ISSUING BLOOD PRODUCTS USING TYPENEX SYSTEM The following information must be supplied by the ward prior to issue of blood products: A) patient’s name (last and first) B) date of birth C) Typenex red identification number (i.e. RHK7732) NOTE - If the Typenex number is not supplied, the blood product CANNOT be issued. Typenex system is not required for re-crossmatch once the patient has been admitted. Page 3 of 4 Last printed 6/27/2012 8:39 AM References 1. CSTM Standards for Hospital Transfusion Services Version 3 February 2011 #5.2.2.2 2. CSA Z902.10 Blood and Blood Components #10.2.4 Related documents LABTranOP7011J1 Typenex Label Position LABPhlbOP7017 Protocol for Performing a Venipuncture Revision History Found in SoftTech Health Lab QMS™ Document Management System Author Paula Van Vliet MLT, ART Judy Hoff MLT, ART Page 4 of 4 Last printed 6/27/2012 8:39 AM APPENDIX LABTranOP7001W4 Canadian Blood Services Circular of Information The Circular of Information provided by Canadian Blood Services provides information about blood products such as component composition, packaging, storage and handling, indications, warnings and precautions, adverse events, dose and administration etc. The table below provides a list of the contents of the Circular of Information. February 2011 Edition (English Versions) Red blood cells LR SAGM added PDF Pooled platelets LR CPD, apheresis platelets PDF June 2011 Edition (English Versions) Plasma components (FFPA, FP CPD, Cryosupernatant CPD, Cryoprecipitate CPD) PDF Visit the Canadian Blood Services website for the current version of this document by using the following link: http://www.bloodservices.ca/CentreApps/Internet/UW_V502_MainEngine.nsf/page/ E_COI LABTranOP7001W4.1.1 CBS Circular of Information Laboratory Services Regina Qu'Appelle Health Region Page 1 of 1 Last printed 8/1/2012 This compendium is the responsibility of Regulatory Affairs, Lab Services. All revisions to this document must go through Regulatory Affairs. Note: Occasionally specimen collection (type of specimen, type of container required, etc.) and specimen transport instructions may change following the print date of this handbook. Therefore, it is recommended that the use of the LIS “Ctrl-T” key function be performed in Order Entry, prior to specimen collection. ** For serological evidence, two blood specimens are desirable whenever possible. The first should be collected within 5 days of onset, the second collected 5 -10 days later. Separate the serum from the clot and send only cell-free serum to avoid the danger of hemolysis of the clot. It is essential that the clinical history accompany the specimens for serological investigations in order to select the appropriate viral antigens for testing. Microbiology tests (complete Micro testing available in Lab Services Manual). Tests referred to Saskatchewan Disease Control Laboratory (SDCL) previously Provincial Laboratories (*) must be recorded on the appropriate SDCL Requisition. Effective date: June 12, 2015 Test Name Highlighted information denotes changes for this version Specimen Container Volume Specimen Requirements Reference Range **5 Disease Blood See Parvovirus B19. *ACE Blood *ACE CSF th 1 Red 2 mL serum 0.5 mL Aliquot + freeze ASAP. Freeze Acetaminophen Blood (Tylenol) N.B. Treatment chart should be consulted before beginning therapy. 1 SST or 1 Green 1 mL serum or plasma *Acetazolamide Blood 2 Red *Acetone (Quantitative) Blood 1 Grey 3 mL Aliquot serum 3 mL whole Do not use alcohol swab. blood Do not open tube. Record time of collection on tube and requisition. Acetone (Qualitative) Blood 1 SST or 1 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum or plasma Units Peak Concentration: 66-199 Toxic Levels: Hours after ingestion: 4 hr: 1325 16 hr: 150 8 hr: 600 20 hr. 75 12 hr: 300 Hepatic damage may occur if >790 at 4 hr Do not use alcohol swab. Do not open tube. μmol/L Normal: negative <0.34 mmol/L Occupational exposure: <0.34-1.72 Ketoacidosis: 1.72-12.04 Panic value: >8 Toxic: >3.40 Negative Testing Site LIS Code SDCL - Hamilton TAT: 3 weeks SDCL - Hamilton ACE Chem - RGH & PH ACECF ACET SDCL - Mayo AZOLA SDCL Routine = 24 hr Emergency = 2 hr ACETO Chem - RGH & PH KETON 2 Test Name Specimen Container Volume Specimen Requirements Reference Range *Acetylcholine Receptor Antibodies Blood Units Testing Site LIS Code 1 SST 1 mL serum Frozen Aliquot and freeze serum. Ship frozen. SDCL - Hamilton ABACR *Acetylcholinesterase Blood Pre-arrange with SDCL 4 Mauve 3 mL EDTA whole blood & 3 mL plasma Stable for only 48 hr. Store and send COLD. Send Hematocrit result with specimen. SDCL - Toronto ACHOL Acid Elution (Kleihauer) Blood 1 Mauve Acid Glycerol Lysis Test Blood *Acid Phosphatase *ACTH Blood Note: Patient does not need to be fasting *ACTH Stimulation Test (Cortrosyn) (Rapid Screen) Activated Protein C (APC) *Acyclovir Blood Can use same tube as CBC 1 Mauve or 0.5 mL Green whole blood 1 Mauve (chilled) 2 mL plasma 1-SST at 3 1 mL separate serum for times each collection Hematology - RGH KLEIH Refrigerate ASAP after Sperocytosis = <150 seconds. At collection. least 60% lysis Collect Monday-Friday occurs before scan only. is leveled. Keep cool and send to Normal = >150 seconds. Scan Special Chem within 12 should level off before hours. 60% lysis occurs. Not available Collect on ice between 0-11 0800 and 1000. Collect at any time for endocrinologists Mohammed and Mann. Return to lab immediately. Spin and separate within 15 minutes. Freeze and send frozen. Submit as separate sample. Collect cortisol before injection and at 30 and 60 minutes after injection. pmol/L Special Chem RGH AGLT SDCL TAT – 7 days ACTH SDCL TAT = 3 days Order Timed Cortisols SDCL - California ACYCL See Hypercoag Blood 1 SST 2 mL serum Acylcarnitine (for Blood PKU Card NICU) *ADH Blood 2 Mauve or 3 mL Anti-Diuretic 2 Green plasma L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Aliquot and freeze Collect in pre-chilled tubes, on ice. Aliquot and freeze SDCL – Toronto TAT = 4 weeks Print Date: June 12, 2015 ADH 3 Test Name Hormone (Vasopressin) Water Deprivation Test To measure basal level, collect after 12 hr fast with patient in Recumbent position for 1 hr prior to collection. *Adenosine Deaminase *Adenovirus *Adrenal Antibodies Adrenal tissue Ab Specimen Container Volume (chilled tubes) Blood or CSF or Fluid 1 SST Nasopharyngeal Aspirate, Washes Throat Blood 1 SST Units Testing Site LIS Code SDCL - Mayo ADEAM immediately. Must be frozen within 24 hr. Cannot be refrozen. Aliquot plasma equally into 2 pre-chilled plastic vials. 1 mL serum or CSF or fluid (min. 0.5 ml) Aliquot. Must Be Frozen. Specimen must be received with 7 days of collection. See Respiratory Virus Isolation or Detection. 1 mL serum frozen *Adrenalin AFP AGBMA (AntiGlomerular Capillary Basement Membrane Antibodies) ALA Albumin Blood Blood 1 SST Albumin Alcohol, Ethyl Fluid Blood 1 Red 1 mL fluid 1 SST or 1 mL 1 Green or serum or Blood Specimen Requirements Reference Range See Throat Virus Isolation or Detection. Freeze and send frozen. SDCL – Hospital in ABAD Common TAT = 3 weeks See Catecholamines See Alpha-fetoprotein 1 SST 1 mL serum Immunology - RGH AGBMS See Aminolevulinic Acid L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum < 1 yr. 32-48 1 – 2 yrs. 37-57 2 – 3 yrs. 33-58 > 3 yrs 35-50 None available Do not open tube. g/L Chem - RGH & PH ALB g/L Chem - RGH & PH Chem - RGH & PH ALBFL ALC Print Date: June 12, 2015 4 Test Name Specimen Container Volume 1 Grey *Aldosterone Blood *Aldosterone 24 hr Urine 24 hr Urine 10 mL container aliquot Alkaline Phosphatase Blood (ALP) 1 SST or 1 Green 2 mL plasma 1 mL serum or plasma Alkaline Phosphatase Fluid (ALP) Alkaline Phosphatase Blood Fractionation (Isoenzymes) Testing will be performed only on specimens with elevated alkaline phosphatase. *Allergy Test (RAST) Blood (Food screen or inhalant screen) Please fill out special sheet Alpha-1-Antitrypsin Blood 1 SST 2 mL serum 1 SST 100 µL serum per test 1 SST 1 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Testing Site LIS Code plasma *Aldolase 1 EDTA Specimen Requirements Reference Range No longer available. Recommend CK Aliquot and freeze. Requires separate aliquot when ordered with other tests. If ordered with Renin can be the same specimen and requisition. Keep cool during 15-70 collection. Freeze aliquot. Record collection data and 24 hr volume on requisition. <30 d: 76-300 1-23 mo: 112-396 2-11 yr: 90-300 12-14 yr (F): 40-270 12-14 yr (M): 76-400 15-17 yr (F): 32-200 15-17 yr (M): 63-270 Adult (>17 yr): 40-135 No Longer Available None available ALDOL pmol/L SDCL ALDOS nmol/d SDCL – Hamilton TAT = 4 weeks ALDOU U/L Chemistry - RGH & ALP PH ALPFL Heat stable fraction: <20% implies bone source >25% and <55% implies liver and/or intestinal source 100 µL is required for each test ordered. Special sheet must accompany specimen. 0.91-3.07 g/L Special Chem RGH APISO SDCL - Saskatoon TAT = 2 weeks RAST Immunology - RGH A1AT Print Date: June 12, 2015 5 Test Name Specimen Container Volume Specimen Requirements Reference Range *Alpha-1-Antitrypsin Feces Special 24 hour container feces from Mayo collection *Alpha-1-Antitrypsin Phenotyping Only done if alpha-1-antitrypsin is low. *Alpha-2Macroglobulin Alpha-Fetoprotein (AFP) Tumour Marker *Alpha-Fetoprotein (AFP) Blood 1 SST 1 mL serum Blood 1 SST Blood 1 SST 1 mL serum 1 mL serum Amniotic Fld. 1 mL Amniotic Fluid 1 mL amniotic fluid 1 SST 1 mL serum 3 Sodium or Lithium Heparin 10 mL whole blood 3 Sodium or Lithium Heparin 10 mL whole blood *Alpha-Fetoprotein Blood (AFP) Maternal Screen Fill out special form with all relevant info. *Alpha Galactosidase Blood *Alpha Glucosidase Blood *Alpha-Hydroxy L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Testing Site LIS Code Freeze SDCL TAT = 7 days ATTRF Freeze serum within 24 hr of collection. Send copy of the alpha-1-antitrypsin results with specimen. SDCL - Toronto A1PHT SDCL - Hamilton A2MAC Chemistry - RGH AFPO Refrigerate at 2-8º C and transport on ice packs, within 24 hr of collection. Complete Maternal Serum Screen requisition. Accurate gestational age and all relevant information needed for interpretation of results. SDCL TAT = 1 day AFMAT SDCL MSS Send whole blood. Keep at room temperature. Refer ASAP. Collected Mon-Thurs early morning. Must be at SDCL same morning. (Sample must be received by Saskatoon within 24 hrs of collection) Send whole blood. Keep at room temperature. Refer ASAP. Collected Mon-Thurs early morning. Must be at SDCL same morning. (Sample must be received by Saskatoon within 24 hrs of collection See 17- SDCL - Saskatoon ALGAL 0-9 Units μg/L SDCL – Saskatoon ALGLU Print Date: June 12, 2015 6 Test Name Specimen Container Volume Progesterone *Alprazolam (Xanax) Blood 1 Red ALT Blood 1 SST or Green ALT *Aluminum Fluid Blood Urine Amikacin (Amikin) Blood Trough and Peak NOTE: Record pre or post along with exact date and time of last doses and exact date and time of collection *Amino Acid Blood Chromatography (Can be done micro 2 small green. Spin and freeze plasma.) *Amino Acid Units Testing Site LIS Code Therapeutic: 2-120 nmol/L SDCL ALPRA 4 - 55 U/L Chem - RGH & PH ALT No Longer Available None available Separate plasma from red cells ASAP. Put plasma or serum in polypropylene tube. Indicate on requisition that specimen is EDTA plasma. Place in polypropylene container. Record on requisition: collection date, total 24 hr volume if submitted or random urine. U/L Chem - RGH & PH SDCL – Toronto TAT = 10 days ALTFL ALUM SDCL – Toronto TAT = 10 days ALUMU Trough – usually drawn ½ hr before drug is administered. Peak – usually drawn 1 hr after drug is administered, but physician may vary. Daily – 6 to 14 hrs after dose. Separate ASAP, freeze mg/L Chemistry- RGH AMIPR (trough) AMIP (peak) AMIKN (random) SDCL - Saskatoon AACID SDCL - Saskatoon AARUR hydroxyprogesterone 1 mL serum 1 mL serum or plasma 3 mL 1 – 7 mL Royal Blue plasma EDTA) BD368381 *Aluminum Specimen Requirements Reference Range Urine 24-hr urine container acidwashed or random urine collected in acidwashed container. 1 EDTA 10-15 mL aliquot of 24 hr urine or 10-15 mL of random urine 1 GREEN (preferred) or 1 EDTA (full) NICU: 2 mL venous blood in pediatric green top Random or 1 mL plasma NICU: 0.6 mL plasma L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL plasma 10 mL urine Freeze. Record collection Trough: 1-8 Peak: 20-30 Toxic Trough: > 10 Toxic Peak: > 30 Print Date: June 12, 2015 7 Test Name Chromatography State collection period Aminolevulinic Acid (ALA) State collection period Specimen Container Volume Urine 24 hr urine. Aliquot. 24 hr brown urine container 20 mL aliquot of 24 hr urine in dark container or wrap in tin foil Specimen Requirements Reference Range date 24 hr volume if submitted or random urine on requisition. Collect into brown bottle. 0-45 Freeze aliquot ASAP in dark container or wrap in tin foil Aminophylline (Theophylline) Blood *Amiodarone (Cordarone) Collect trough specimen prior to administration of next dose) dose. *Amitriptyline (Elavil) Blood 2 SST 3 mL serum Blood 2 Red or Green 4 mL serum Do not use SST tubes or plasma Ammonia Blood 1 Green (full) 2 mL Place specimen on ice heparinized immediately after plasma collection and bring ASAP to lab. Patient not to clench hand during collection. Outpatient collections to come to RGH or PH. If shipping freeze plasma aliquot and send on dry ice. 10 mL Keep specimen in the dark amniotic at all times. fluid 3 mL serum Aliquot. Amniotic Fluid Scan Amniotic (A450) Fluid (OD Rise) *Amoebasis Serology Blood Units μmol/d Testing Site LIS Code TAT = 1 week (random) AA24 (24 hr) ALA24 Special Chem RGH See Theophylline 1 SST (Entamoeba) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Therapeutic: Minimum: 220-600 Maximum: 650-1100 Toxic: >1700 12-47 nmol/L μmol/L SDCL – Toronto TAT = 2 weeks AMIOD SDCL TAT:Emerg = 4 hr Routine = 3 days Chem - RGH & PH AMIT AMMO Special Chem RGH A450 SDCL - Montreal TAT = 4 weeks AMOES Print Date: June 12, 2015 8 Test Name Specimen Container Volume *Amoxapine (Asendin) Blood 2 Red or 2 Green 4 mL serum Do not use SST tubes or plasma *Amphetamines Urine AMA (AntiMitochondrial Antibodies) Amylase Amylase Amylase Blood Plastic urine container 1 SST 20 mL NOTE: Blood unsuitable. random Refrigerate samples. urine 1 mL serum 1 SST Blood Fluid Urine Specimen Requirements Reference Range Therapeutic: 600-1200 Toxic: >1200 – but CNS effects including seizures, convulsions, lethargy and coma are important indicators Negative Units Testing Site LIS Code nmol/L SDCL TAT: Emerg = 4 hr Routine = 3 days AMOXA SDCL TAT = 2 days AMPH Immunology - RGH AMAS Amylase Isoenzymes Blood 1 SST 1 mL serum 1 mL fluid 5 mL urine 24 hr urine amylase no longer available. 1 mL serum No Longer Available ANA or ANF (Anti-Nuclear Antibody or AntiNuclear Factor) *Anafranil (Clomipramine) *ANCA Blood 1 SST 1 mL serum No hemolysis Immunology - RGH ANA Blood 2 Red 4 mL serum SDCL CLOMI 1 SST or 1 Green See Anti-Neutrophil Cytoplasmic Antibodies See Testosterone 1 mL serum Record date/time of or plasma collection on tube and requisition. Aliquot and freeze. Must have own specimen and req. SDCL TAT = 14 days ADION *Androgen *Androstenedione Blood (A2) Draw in AM preferred but can be done at other times. Random *Angiotensin I *Angiotensin Converting Enzyme *ANNA-1 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 20-110 None available 32-641 U/L U/L U/L Total: 20-110 Pancreatic: 43-67 Salivary: 38-56 U/L % % Infants and children: Decreased from 10.1 during the first week to 1.7 in prepuberty At puberty: 0.3-8.4 Female: Normal: 1.6-9.4 Menopausal: <3.5 Male: 2.0-9.4 nmol/L Chem - RGH & PH Chem - RGH & PH Chem - RGH & PH See Renin See ACE See Anti-Hu Print Date: June 12, 2015 AMYL AMYFL AMYRA (random) 9 Test Name *Anti-Adrenal Antibodies *CC1 Esterase Inhibitor Anticardiolipin and (Anticardiolipin Antibodies to Nonspecific Antigen) *Anti-Centromere Antibodies *Anti-Chlamydia pnemoniae *Anti-Cyclic Citrullinated Peptide (Anti-CCP) *Anti-Diuretic Hormone Anti-DNA or dsDNA (Anti-Nucleic Acid) Performed only if ANA screen positive *Anti-DNASE B Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Immunology-RGH CENTR SDCL CCPAB See Adrenal Antibodies See C1 Esterase Inhibitor Blood 3 Blue and 1 Red Blood 1 SST See LUPWS 1 mL serum Blood Blood See Chlamydophilia pneumoniae IgM and IgG. 1 SST 1 mL serum Only done if ANCA screen is positive. See ADH Blood 1 SST 1 mL serum RHD specimens only Immunology - RGH DSDNA Blood 1 SST SDCL - MAYO ABDNS *Anti-Endomysial Antibodies *Anti-GAD65 Blood 1 SST SDCL ABEND *Anti-Gastric Antibodies (Anti GP Cell Ab) Anti-Glomerular Capillary Basement Membrane Antibody (AGCBM Ab) *Anti-Gliadin Antibody (Identifies IgA & IgG) Anti-Glutamic Decarboxylase Ab *Anti-Gluten Antibodies Blood 1 SST 0.5 mL Refrigerate – preferred serum (Can be frozen). 1 mL serum Keep specimen cool. Send on ice packs. See Anti-Glutamic Decarboxylase Ab 2 mL serum Send last B12 result with specimen SDCL - Saskatoon ABGA Blood 1 SST 1 mL serum Immunology - RGH AGBMS Blood 1 SST 1 mL serum Blood 1 SST 2 mL serum Separate immediately and Freeze Order Celiac Disease Profile and write on req. SDCL TAT = 3 weeks SDCL-Toronto L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 ABGLI ABGAD CDP Print Date: June 12, 2015 10 Test Name Specimen Container Volume *Anti-HAV IgM and/or IgG Hepatitis A *Anti-HAV – Total Ab *Anti-HBc *Anti-Hbe Blood 1 SST Blood Blood Blood 1 SST 1 SST 1 SST *Anti-HBs *Anti-HCV *Anti-HDV Only done if HBV positive *Anti-HEV *Anti-HFV *Anti-HGV *Anti-Histone *Anti-Hu (ANNA-1) Blood Blood Blood Blood Blood Blood Blood Blood Testing Site LIS Code 2 mL serum SDCL HEAAB SDCL SDCL SDCL - test done weekly HEATO HEBCO HEBEB 1 SST 1 SST 1 SST 2 mL serum 2 mL serum 2 mL serum Performed on patients with Negative history of being HbsAg positive 2 mL serum 2 mL serum 2 mL serum SDCL SDCL SDCL HEBAB HECAB HEDAB 1 SST 1 SST 1 SST 1 SST 1 SST 2 mL serum 2 mL serum 2 mL serum 1 mL serum Freeze 1 mL serum Freeze ASAP HEEAB HEFAG HEGAB HISAB HU Blood 1 SST See Insulin Antibodies 1 mL serum Separate and freeze ASAP *Anti-Intrinsic Factor Ab Blood 2 SST 3 mL serum Avoid administration of B12 for 48 h before collection SDCL SDCL SDCL SDCL - Ontario SDCL – Mitogen Diagnostics, Calgary SDCL SDCL – Toronto TAT = 3 weeks SDCL Anti-Jo-1 Anti-La *Anti-Liver & AntiKidney Ab (Anti-KLM or Anti-LKM) *Anti-Mag Assay (Anti-Myelin Associated Glycoprotein Assay) *Anti-Microsomal Blood 1 SST 2 mL serum SDCL ABJO Blood 1 SST See Anti-SSB 2 mL serum Keep cool. Send on ice pack. SDCL - Toronto ABKLM Blood 1 RED SDCL AMAG SDCL ABMIC *Anti-Insulin Ab *Anti-Islet Cell Ab *Anti-Mitochondrial Specimen Requirements Reference Range 1 mL serum Patient should be fasting. Freeze serum See Anti-Thyroid Peroxidase Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Units ABINS ABISC ABINF Immunology - RGH AMAS Print Date: June 12, 2015 11 Test Name Specimen Container Volume Ab (AMA) *Anti-Mullerian Hormone *Anti-Musk Blood 1 SST 1 mL serum Send frozen Blood 1 RED Do not use SST 1 SST See spec. requirement 1 SST 1 SST 2 mL serum Freeze. Must be approved (SDCL 787-3131 ext 4) 1 mL serum 2mL serum Separate ASAP in aliquot. Must specify perinuclear or cytoplasmic staining. 2 mL serum If ANCA positive a p-ANCA 2 mL serum will be performed. 1 SST 1 mL serum *Anti-Myocardial *Anti-Neutrophil Cytoplasmic (ANCA) Blood Blood p-ANCA c-ANCA Syn: Vasculitis Panel or Vasculitis Screen Anti-Nuclear Ab *Anti-Ovarian Ab Anti-Pancreatic Islet Ab *Anti-Parietal Cell Ab Anti-Phospholipid Ab Blood Blood *Anti-Reticulin Ab Blood *Anti-Ri Blood Specimen Requirements Reference Range Units Testing Site LIS Code SDCL – Hospital in MULLH Commons,Toronto SDCL – California MUSKA SDCL - Toronto ABMYO SDCL – Saskatoon PANCA CANCA See ANA Blood SDCL - Toronto ABOVA See Anti-Islet Cell Ab Anti-RNP Blood Performed only if ANA screen is positive Anti-Ro Anti-Scleroderma-70 Blood Ab (Anti-Scl-70) Performed only if ANA screen positive Anti-Skeletal Ab 1 SST 2 mL serum 3 Blue & 1 4 mL Order as LUPWS. Double Red plasma spin plasma and separate 2 mL serum into 4 tubes, freeze all plasma and serum tubes. 1 SST 1 mL serum Aliquot & send specimen on ice packs 1 SST 1 mL serum Freeze ASAP SDCL ABPAR Special Coag Hematology - RGH SDCL - Toronto ABRET 1 SST 1 mL serum RHD only SDCL – Mitogen RI Diagnostics, Calgary Immunology - RGH RNPSM 1 SST See Anti-SSA 1 mL serum RHD only Immunology - RGH SCL70 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Anti-Striated Muscle Print Date: June 12, 2015 12 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Ab *Anti-Skin Ab Blood 1 SST 1 mL serum SDCL - Saskatoon ABSKI TAT = 2 weeks Immunology - RGH ASMAS Anti-Smooth Muscle Ab (ASMA) *Anti-Sperm Ab Anti-SSA Ab Anti-SSB Ab (Anti-La) Anti-Smith Ab (SM) Performed only if ANA Screen positive *Anti-Streptolysin Blood 1 SST 1 mL serum Blood Blood 1 Red 1 SST 2 mL serum Freeze 2 mL serum RHD only SDCL - Mayo Lab ABSPE Immunology – RGH SSA SSB SM Blood 1 SST 2 mL serum SDCL ASLT *Anti-Striated Muscle Ab *Anti-Techoic Acid Anti-Thrombin III Blood 1 SST 2 ml serum SDCL - Toronto ABSTM *Anti-Thyroglobulin Blood 1 SST 2 mL serum *Anti-Thyroid Microsomal *Anti-Thyroid Peroxidase Anti-Thyrotropin Ab Blood 1 SST 1 mL serum Special Coag Hematology - RGH SDCL ABTHY TAT = 2-3 days SDCL ABMIC Blood 1 SST 1 mL serum SDCL PEROX SDCL ABTTG SDCL – Mitogen Diagnostics, Calgary YO (ASO) (Streptozyme) See Techoic Acid. See Hypercoag (order as HCOAG) Anti-Topoisomerase AntiBlood Transglutaminase Ab Anti-Trypsin Anti - Xa *Anti-Yo (Purkinje Cyto Ab) Blood <100 IU/mL See Thyrotropin Binding Inhibitory Immunoglobulin See Anti-SCL-70 1 SST See Alpha-1-Antitrypsin See Heparin Assay 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Freeze ASAP Print Date: June 12, 2015 13 Test Name Specimen Container Volume Specimen Requirements Reference Range *Apolipoprotein A1 Collect after 14 hr fast *Apolipoprotein B Not required to be fasting. *Apo-E Lipoprotein Must be fasting 14 hr. A letter submitted by the ordering physician outliniing the reason for requesting this test must accompany the sample. APT (Alkaline Denaturation Test) Bring to lab ASAP Blood 1 Mauve 1 mL plasma Blood 1 Mauve 1 mL plasma Blood 4 Mauve *Arbovirus Serology Feces, vomitus or gastric content Blood *Arsenic Blood For non-dietary exposure within 48 hr *Arsenic Urine Information on patient's diet should be included 1 SST Testing Site LIS Code Separate from cells within 4 hr of collection SDCL – Toronto APOA1 Separate from cells within 4 hr of collection. Freeze and send frozen Minimum of Separate within 4 hrs of 6 mL EDTA collection. Store and ship plasma at 4 degrees. SDCL – Toronto APOLI SDCL APOLE 1 g or 1 mL Give to Chemistry ASAP Chemistry - RGH APT 2 mL serum SDCL ARBOS No substitute is acceptable *24 hr urine is specimen of choice. SDCL - Edmonton ARSB 24 hr urine is specimen of choice. For non-dietary exposure within 48 hr, send EDTA whole blood. Send in polypropylene container. Record collection date, 24 hr volume if submitted or random urine on req. Room Temp Collect Mon-Fri mornings only. Send to SDCL ASAP See Salicylate Protect from light with foil 45-85 or use light sensitive SDCL – Toronto TAT = 3 weeks ARSU SDCL - Saskatoon ARYLS SDCL TAT = 3 days VITAC Whole 1 – 7 mL Royal Blue blood EDTA) Units BD368381 24 hr or random urine container acidwashed 1 mL of 24 hr urine or 10 mL random urine *Arylsulfatase A Blood 1 Na Heparin (Full) 3 mL Whole Blood ASA *Ascorbic Acid (Vitamin C) Blood 1 SST 1 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 μmol/L Print Date: June 12, 2015 14 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code SDCL AMOXA Chem - RGH & PH AST SDCL - Edmonton TAT = 3 weeks ASPGS LOR HEBAG aliquot tube. Separate and freeze immediately. Send frozen on dry ice. *Asendin (Amoxapine) ASMA *ASO Blood 2 Red or 2 Green 4 mL serum or plasma Blood AST (SGOT) Blood 1 SST 1 mL serum *Aspergillus Serology Blood 1 SST 3 mL serum Anti-Smooth Muscle Ab See Anti-Streptolysin (ASO). <6 mo: 63-81 6 mo-5 yr: 46-63 >5 yr: 5-35 (Farmer’s Lung, Galactomannin) Atenolol (Ternormen, Tenolin) *Ativan (Lorazepam) Blood *Australian Antigen Blood (HBsAg) *Auto Antibodies Blood Test Not Available 2 Red 1 SST 5 mL serum 1 mL serum SDCL SDCL 1 Mauve Full Transfusions - RGH *DANT *Auto Immune Muscle Disease Profile *Aventyl (Nortriptyline) B12 B12 & Folates (RBC) Note: If B12 or RBC folate decreased, serum folate reflexed. *B12 Binding Protein *Babesiosis Serology Blood 1 SST & 1 Mauve Blood 1 SST *Bacterial Meningitis Blood 1 RED Blood 2 Red Blood Blood Tubes must be labelled with name, DOB, and PHN or MRN 1 mL serum Freeze within 4 hours of Includes Jo1, Mi2, PL-7, PL-12, collection PM/Scl, Ku, Ro52, SRP. 4 mL serum Do not use SST See Vitamin B12 1 ml serum Needs hematocrit run in & 1 mL Hematology first whole blood See Transcobalamine 3 mL serum Aliquot. SDCL to Calgary AIMDP SDCL NORTR Chemistry - RGH B12FO SDCL – Montreal TAT = 4 weeks BABES Special Chem - BARBQ See Encephalitis (Bacterial). (Hemophilus influenzae, CSF Neisseria meningitidis, Strept. pneumoniae) *Barbiturates U/L 1 Red or L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 3 mL serum Do not use Seraclear - See individual tests for reference Print Date: June 12, 2015 15 Test Name Specimen Container Volume 2 Green (full) NOT SST *Barbiturate (Urine Drug Screen) *Bartonella henselae Urine (random) Blood 1 SST or plasma Specimen Requirements Reference Range Units ranges RGH Refrigerate sample Negative SDCL TAT = 2 days SDCL – Winnipeg BARTS TAT = 3 weeks Immunology - RGH IFEU 2 mL serum Bence Jones Protein Urine or Blood 24 hr urine 100 mL of or 1 SST 24 hr urine or 1 mL serum *Benzitropine (Cogentin) *Benzodiazepines Blood 2 Red 4 mL serum Urine Random 20 mL urine Refrigerate Blood 1 Red 1 mL serum Refrigerate Blood Urine 1 SST 1 mL serum Blood 1 SST Beta 2 (B2) Transferrin Bilirubin Fluid Blood 1 SST or 1 Green LIS Code false positive (Cat Scratch Fever) *Beta 2 Glycoprotein1 AB Beta 2 Microglobulin Beta 2 Microglobulin Beta-Hydroxbutyrate Bicarbonate *Bile Acid Concentration (Bile Acid Assay) Testing Site 24 hr urine collection is preferred Record Collection Time, Date and Volume on req. Rural sites: Send aliquot frozen Not available See B-OH Butyric Acid See CO2 2 mL serum Aliquot & Freeze Preferred: Collect after overnight fast or postprandial. (will accept non-fasting specimens ) 0.5 mL Freeze in plastic. Must be frozen before shipping. 1 mL serum Negative 0-3.4 Cord: 18-52 Direct: 0-9 Total: 2-20 mg/L µmol/L SDCL BENZI SDCL TAT = 2 days SDCL to Mayo BENZO B2GLY Immunology - RGH B2MGB SDCL - Edmonton BCONC SDCL – referred out - Mayo Chem - RGH & PH B2TFE BILCD (cord) BILTD (total and direct) BILIT (total) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 16 Test Name Specimen Container Volume Specimen Requirements Reference Range Bilirubin – Neonate Blood 1 Microcontainer Bilirubin *Biotinidase Fluid Blood ß-hCG (Qualitative) (Pregnancy Test) State pregnancy test on req ß-hCG (Quantitative) Tumour Marker ß-hCG (Quantitative) Maternal Screen Fill out special form with all relevant information *ß-OH-Butyric Acid Urine or Blood 1 mL fluid 1 SST or 2 mL serum Freeze ASAP 1 Green or plasma Random or 1 mL urine 1 SST or 1 mL serum 0.2 mL Protect from light serum or heparinized plasma Full term: 24 hr: 36-104 48 hr: 103-120 3-5 d: 68-103 Premature: 24 hr: 17-103 48 hr: 103-137 3-5 d: 171-205 None available 0-6 Units Testing Site LIS Code µmol/L Chem - RGH BILIN µmol/L Chem - RGH & PH SDCL to Winnipeg BILFL BIOTD Chem - RGH & PH Chemistry - RGH PREGU (urine) SPREG (serum) BHCGR Blood 1 SST 2 mL serum Blood 1 SST 2 mL serum Accurate gestation age needed SDCL MSS Blood 1 SST 1 mL serum Freeze ASAP BOHBU *BK Virus – Plasma PCR Blood 1 Mauve *BK Virus CSF BK Virus PCR CSF *BK Virus Urine BK Virus PCR Urine SDCL - Toronto Hospital in Comons SDLC – Toronto Hospitals in Common SDLC – Toronto Hospitals in Common SDCL –Toronto Hospitals in Common *Blastomycosis Serology Bleeding Time Must be approved by Hematologist Bleeding Disorder Blood SDCL - Edmonton TAT = 3 weeks Hem - RGH & PH BLASS 2 mL EDTA Freeze plasma ASAP. plasma If specimen thaws , it is unsuitable for analysis. Sterile leak 1 mL CSF Freeze CSF ASAP. proof tube If specimen thaws , it is unsuitable for analysis. Sterile 20 ml urine Freeze urine ASAP. plastic (random) If specimen thaws , it is urine unsuitable for analysis. container. 1 SST 3 mL serum Done on patient's arm by Hematology Tech Blood IU/L 3 Blue L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 4 mL Double spin plasma and 2-9.5 Minute Spec. Coag. Print Date: June 12, 2015 BKVIR BKVIC BKVIU BT BLDWS 17 Test Name Specimen Container Volume Investigation (BLDWS) Blood Culture Fungal Blood Blood Culture Pediatric Blood Culture Routine Blood *Blood Culture TB (Mycobacterium) Blood Culture Blood/Bone Marrow Blood Gases Blood Gases Blood Gases Blood Dialysis Fluid Arterial (full) citrated plasma Aerobic and Anaerobic Vials Pediatric Vial Aerobic and Anaerobic Vials Myco/FLytic vial 8-10 mL blood/vial Syringe (electrolyte balanced dry heparin) Units Testing Site LIS Code separate into 4 tubes. Freeze and send frozen on dry ice. Transport to Microbiology Lab immediately and place in BacTAlert. Hem – RGH & PH 2-4 mL blood/vial 8-10 mL blood/vial A single blood culture is acceptable for infants. Transport to Microbiology Lab immediately and place in BacTAlert. Microbiology - RGH BCUL 1-5 mL blood/vial Send at room temp ASAP. Do not refrigerate or freeze See Microbiology Compendium Anaerobic technique. PH <2 mo: 7.30-7.47 Brought to lab ASAP. 2 mo-2 yr: 7.34-7.46 >2 yr: 7.35-7.45 pCO2 < 2mo: 27-40 2 mo-2 yr: 26-41 2yr: 33-45 pO2 < 2 mo: 55-80 2 mo-2 yr: 65-100 >2 yr: 75-100 HCO3 <2 yr: 16-24 >2 yr: 22-26 Base Excess <2 mo: -10 - -2 2 mo-2 yr: -4-2 >2 y: -2.5-2.5 O2 Saturation: 95-98 1.5 mL (adults) 0.6 mL (neonates) Cord Arterial Syringe (lithium or sodium heparin) 1.5 mL Cord Venous Syringe (lithium or sodium 1.5 mL L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Anaerobic technique. Brought to lab ASAP. Microbiology - RGH BCUL Microbiology - RGH BCUL pH …….…7.23-7.33 pCO2 …….…. 41-58 pO2 ……….… 12-24 HCO3 …….… 20-25 Base Excess pH …7.30-7.40 pCO2 …33-44 pO2 … 23-35 SDCL. TB/BC Microbiology - RGH Chem - RGH & PH BGA Chem - RGH & PH BGCA Chemi - RGH & PH BGCV mmHg mmHg mmol/L mmol/L % mmHg mmHg mmol/L mmol/L mmHg mmHg Print Date: June 12, 2015 18 Test Name Specimen Container Volume Specimen Requirements Reference Range heparin) Blood Gases Blood Gases Blood Gases Micro Venous Venous Blood Group Blood Blood Parasite for ______ Blood BNP Blood (N-Terminal Pro Brain Natriuetic Peptide) Capillary tubes Electrolyte balanced heparin Syringe 2 x 125µL Anaerobic technique. Brought to lab in ice water ASAP. pH …….…7.32-7.42 pCO2 ………. 40-50 pO2 ………… 25-47 HCO3 …….… 22-29 Base Excess 1 FULL Anaerobic technique. . pH …….…7.32-7.42 Green Place on ice and deliver to pCO2 ………. 40-50 Vacutainer Chemistry lab within 15 HCO3 …….… 22-29 minutes. Base Excess 1 Mauve Tubes must be labelled with full name, DOB, MRN OR HSN 1 Mauve Can use same tube as CBC, enter name of parasite in LIS 1 EDTA 1 mL Remove plasma from cells ASAP and run immediately 400uL- 1 or Freeze. full EDTA Stability: 4 hrs at room microtainer temp or 24 hrs frozen. For Neonatals can be collected using EDTA microtainers. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Anaerobic technique. No ice required if brought to lab ASAP. HCO3 … 16-24 Base Excess pH <2 mo: 7.30-7.47 2 mo-2 yr: 7.34-7.46 >2 yr: 7.35-7.45 pCO2 < 2 mo: 27-40 2 mo-2 yr: 26-41 >2yr: 33-45 pO2 <2 mo: 55-80 2 mo-2 yr: 65-100 >2 yr: 75-100 HCO3 <2 yr: 16-24 >2 yr: 22-26 Base Excess <2 mo: -10 - -2 2 mo-2 yr: -4-2 >2 y: 2.5-2.5 O2 Saturation 95-98 Units Testing Site LIS Code Chem - RGH & PH BGM Chem - RGH & PH BGV Chem - RGH & PH BGVVA Transfusions *BLGR mmol/L mmol/L mmHg mmHg mmol/L mmol/L % mmHg mmHg mmol/L mmol/L mmHg mmol/L mmol/L Hematology - RGH BLPA Chemistry – RGH Print Date: June 12, 2015 BNPA 19 Test Name Specimen Container Volume NT-Pro BNP Blood 1 SST (For Cancer Patients/ Allan Blair Patients only) EDTA Body Fluids Pleural, (counts) Peritoneal Dialysate, Pericardial and Synovial Fluids Bone Donor (Initial Testing) Blood Bone Donor (6 Month Testing) Bone Specific ALP *Bordetella pertussis (Whooping Cough) Blood Blood Nasopharyngeal *Brucella Antibodies *BSE *Butazoldin (Phenylbutazone) C&S Blood CSF Blood 1 mL Frozen. 3-5 mL All fluids must be in lab Dialysate normal range: within 4 hr from the time of WBC 0.0-0.1 x 109/L collection Pleural, synovial fluids normal range: clear, pale, yellow WBC: Pleural: 0-1.0 x 109/L Synovial: 0.02 x 109/L RBC: 0 x 1012/L Diff: <25% neutrophils Peritoneal fluid normal range: clear, pale, yellow WBC: 0-300 per mm3 (<0.3 x 109/L) RBC: 0-1012/L Diff: - <75 neutrophils per mm3 (<25%) Tubes must be labelled with full name, DOB and MRN or PHN No longer performed 2 SST and 1 Red top 2 EDTA 2 SST and 1 Red top 1 SST 1 mL *Borrelia borgdorferi 1 SST 2 Red L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Frozen See Pertussis. *Nasopharyngeal Pertussis (Culture and PCR) See Lyme Disease Total IgM and IgG Serology. 3 mL serum Aliquot and freeze. See Creutzfeld Jakob Disease. 4 mL serum Units WBC x 109/L RBC x 1012/L Diff - % Testing Site LIS Code SDCL to Hospitals in Common, Toronto NTBNP Hematology- RGH & PH Specific to each fluid Mt Sinai, Toronto, Ontario BDINI SDCL /RGH Transfusions SDCL/Toronto BD6M OSTAS PERTU SDCL BRUCS SDCL PHEBZ See Micro Section Print Date: June 12, 2015 20 Test Name Specimen Container Volume *C1 Blood A *C1 Esterase Inhibitor level is done first to see if C1 function is sent away. *C1 Esterase Inhibitor Blood Fasting preferred Testing Site LIS Code SDCL - Denver C1 SDCL TAT = 2-3 days C1EST SDCL-Toronto C1QAB 1 mL serum Refrigerated. SDCL – MAYO C1QLV 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at –70º C within 2 hr of collection. 0.5 mL Freeze. Send on dry ice. serum 1 mL serum C3: 0.74-1.85 C4: 0.16-0.44 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 mL Aliquot and freeze at -70º plasma C within 2 hr of collection. SDCL –National Jewish Reference Centre C2 SDCL – MAYO C2LEV 1 Red 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 SST 2 mL serum Allow to clot for no more 0.21-0.39 than an hr. Aliquot and freeze at –70º C within 24 hours of collection. 1 mL serum Separate and freeze within 60 minutes of collection *C1Q Immune Complex Antibody Blood 1 Red *C1q Level Blood *C2 Functional test Blood 1 RED ( can use SST but not preferred) 1 Red *C2 Level Blood 1 RED C3, C4 (Complement) Blood 1 SST *C5 Level Request C5F if Functional test is required *C5 Function Blood 1 Red Blood 1 Red Blood 1 EDTA Blood 1 Red *C6 Level Request C6F if Functional test is required *C6 Function Specimen Requirements Reference Range L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. Units g/L g/L Immunology - RGH C3C4 SDCL - MAYO C5 SDCL – MAYO C5F SDCL – National Jewish Health, Denver C6 SDCL – MAYO C6F Print Date: June 12, 2015 21 Test Name Specimen Container Volume Specimen Requirements Reference Range *C7 Level Request C7F if Functional test is required *C7 Function Blood 1 EDTA 1 mL plasma Aliquot and freeze at -70º C within 2 hr of collection. Blood 1 Red Blood 1 EDTA Blood 1 Red *C8 Level Request C8F if Functional test is required *C8 Function Testing Site LIS Code SDCL - National Jewish Health, Denver C7 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 mL Aliquot and freeze at -70º plasma C within 2 hr of collection. SDCL – MAYO C7F SDCL - National Jewish Health, Denver C8 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 mL Aliquot and freeze at -70º plasma C within 2 hr of collection. SDCL – MAYO C8F SDCL – National Jewish Health, Denver C9 1 mL serum Allow to clot for no more than an hr. Aliquot and freeze at -70º C within 2 hr of collection. 1 mL serum Send frozen or 1 mL plasma (EDTA) 1 mL serum 0-35 See Carbohydrate Antigen 1 mL serum Aliquot & Freeze SDCL – MAYO C9F SDCL – Toronto TAT = 2 weeks CA15 Chemistry - RGH CA15 SDCL - Mayo Lab CA27 SDCL - Toronto CADMB *C9 Level Request C9F if Functional test is required *C9 Function Blood 1 EDTA Blood 1 Red *CA15-3 Blood 1 SST or 1 Mauve CA 125 *CA19-9 *CA27-29 Blood 1 SST Blood *Cadmium (Blood) Blood 1 SST preferred RED is acceptable 7 mL whole 1 – 7 mL Royal Blue blood EDTA) Units BD368381 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 22 Test Name Specimen Container Volume *Cadmium (Urine) Urine *CAE Blood 24 hr or random acidwashed container 1 Red *Calcitonin Collect after 14 hr fast Calcium Blood 1 SST Blood 1 SST Calcium Calcium State collection period Calcium – ionized *Calculi Fluid Urine Calculus either passedor surgically removed (renal, bladder, ureter, biliary or prostatic) Prefer 24 hr Send calculi in a dry, sealed, clearly marked container *C-ANCA *Cannabinoids (Cannabis) Urine Random urine L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range 10 mL aliquot of urine in polypropyle ne vial 2 mL serum Collect in acid-washed container. Record collection date, 24 hr volume if submitted or random urine. Remove serum from cells within 2 hr of collection freeze. Must arrive at SDCL frozen. 2 mL serum Aliquot & freeze. Record fasting serum on requisition. 1 mL serum ≥60 0-10days=1.90-2.60 >10days =2.14-2.66 None available Intake 200n mg/d: 0.3-4.5 Intake 200-600 mg/d: 1.3-5.0 Intake 1 g/d: <7.5 1 mL serum No Longer Available 10 mL urine Acidify before analyzing Indicate on Requisition if Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen See Ionized Calcium Send calculi in a dry, Descriptive report sealed, clearly marked container See Anti-Neutrophil Cytoplasmic Ab (PR3) 20 mL urine Keep cool Negative Units Testing Site LIS Code SDCL – Toronto TAT = 3 weeks CADMU SDCL - done weekly CAE SDCL - Toronto CALCI mmol/L Chem - RGH & PH CA mmol/L mmol/d Chem - RGH & PH Chem - RGH & PH CAE units CAUR (random) CA24 (24 hr) SDCL TAT = 7 days STONE SDCL TAT = 3 days CANNA Print Date: June 12, 2015 23 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Carbamazepine (Tegretol) See TDM section for ideal sampling times *Carbohydrate Antigen Ca 19-9 *Carbohydrate Deficient Transferrin Carbon Monoxide (Carboxy Hemoglobin) Blood 1 EDTA 1 mL plasma Collect 0-1 hr before dose. μmol/L Chemistry - RGH CARBA Blood 1 SST 1 mL Aliquot SDCL - Toronto TAT = 3 weeks CA19 Blood 1 SST 1 mL serum Aliquot and Freeze SDCL - California CDTRF Blood 1 small 5 mL whole Do not open tube Green (full) blood % Chem - RGH & PH COHBA Carcinoembryonic Antigen (CEA) Carcinoembryonic Antigen Cardiac Antibodies *Cardizem (Diltiazem) Collect immediately before next oral dose *Carnitine (Total & Free) Acylcarnitine – PKU card Blood 1 SST g/L Chemistry - RGH CEA Chemistry – RGH CEAFL SDCL TAT = 5 days CARDI Freeze. Avoid hemolysis. Separate plasma from cells. SDCL CARNS *Carnitine Freeze SDCL (ABC Lab Saskatoon) CARNU SDCL TAT = 7 days CAROT Fluid 1 mL 1 mL Therapeutic: 17-50 Toxic: ≥63 (Earliest time for first TDM is one week) Non-smoker: <2 Smokers: 2-5 Heavy Smokers: 5-9 Toxic: >20 Fatal: >50 0-5 See Anti-Myocardial Ab Blood 2 Red 3 mL serum Blood 1 Red or 1 Green Urine Random 24 hr if 1 mL plasma or serum (200 L for babies 5 mL urine quantitative *Carotene Blood results required results required 1 SST *Cat Scratch Disease Blood L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2 mL serum Keep in dark See Bartonella henselae (Cat Scratch Fever). Print Date: June 12, 2015 24 Test Name Specimen Container Volume Specimen Requirements Reference Range *Catecholamines (Free) Blood 2 Mauve (EDTA) Plasma – Adrenalin, Noradrenalin, Epinephrine, Norepinephrine Collect after pt. has been at rest in a supine position for 30 min. No smoking, tea or coffee during procedure. Immediately place specimen on ice after collection. *Catecholamines Urine Urine (includes epinephrine & nonepinephrine) 24 hr urine CBC Blood CBC for Hemodialysis Blood 1 Mauve 1 Mauve CBC for Neonates Micro sample EDTA 1 SST Blood CCU Panel (renal, Blood liver, glucose, Ca, Mg, PO4, uric acid, CK, AST, LD) NB: Pasqua Hospital does not include LD *CD4\CD8 Blood (CBC must be done with test) Weekdays only 1 Mauve CEA *Celiac Disease Profile Blood 1 SST *Cell Markers L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 350 uL minimum Testing Site LIS Code Not recommended because of pulsatile variation in levels of peripheral blood. Have urine done first. Separate and freeze immediately. Send on dry ice. SDCL – Hamilton TAT = 10 days CATEP Refrigerate during collection. Adjust pH to 2-4 with HCL or freeze. Pediatric - include weight. State 24 hr volume. SDCL TAT = 7 days CATEU Please order CBCK for post-dialysis or unknown dialysis and CBCP for PreHemodialysis patients For C-NC and C-2D Units Hem - RGH & PH CBC Hematology - RGH CBCK CBCP Hematology - RGH CBCNC Chem - RGH & PH Send before 1400 hr - Att'n Flow Cytometry specimen must be processed within 24 hr of collection. Keep at room temperature. See Carcinoembryonic Antigen Includes Gliadine Ab IgA/IgG and tissue transglutaminase Ab See Flow Cytometry CCURG CCUPH Hematology - RGH CD4 + 8 SDCL - Toronto TAT = 3 weeks Print Date: June 12, 2015 CDP 25 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code *Ceruloplasmin (CER) Blood Aliquot. Refrigerate. Transport on ice packs within 24 hr. mg/L SDCL TAT = 2-3 days CERUL 1 SST *CH 50 (will do CH 100) *CH 100 2 mL serum. 200-600 SDCL **Chickenpox Blood **Chlamydophila Blood pneumoniae IgM and IgG 1 SST Replaced with Complement Activation E (CAE) See Varicella Zoster. 3 mL serum IgM and IgG performed simultaneously on all specimens. SDCL CH100 SDCL CHLAS 1 mL (BAL) Freeze and ship ASAP to or SDCL. lung biopsy Documentation must include clinical background leading to suspicion of C.pneumoniae in the patient. See Psittacosis Serology. SDCL - Winnipeg CHLPP SDCL CHLOC SDCL CHLGC SDCL TAT = 3 days CHLHY (Anti-Chlamydia pneumoniae, C. pneumoniae, TWAR) *Chlamydophila pneumoniae PCR Bronchioalveolar lavage (BAL) or lung biopsy *Chlamydophilia psittaci *Chlamydia trachomatis Culture Blood *Chlamydia trachomatis Urine Chlamydia and GC (NAAT) *Chloralhydrate (Noctec) (Trichloroethanol) Sterile screwcapped container Cervical, Urethral, Rectal, Oral, Eye, Respiratory (neonatal) Urine Universal Transport Medium APTIMA Blood 1 Red L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 20 -30 mL first catch void uine in collection cup 2 mL serum Using provided disposable pipette, add 2 mL of urine specimen to APTIMA tube. Urine level must be between black fill lines. Do not use SST. Record Therapeutic: 9-90 time of collection on tube (expressed as Trichlorethanol) and req. mol/L Print Date: June 12, 2015 26 Test Name Specimen Container Volume *Chloramphenicol (Chloromycetin) Blood 1 SST 1 mL serum Collect trough level specimen before the next dose is administered. Collect peak level (postdose) specimen 60-90 minutes after drug infusion. Submit separate requisition for both trough and peak specimen. *Chlordiazepoxide (Librium) Blood 1 Red 2 mL serum Do not use SST Chloride Blood 1 SST or 1 Green or Syringe with electrolyte dry heparin Chloride Chloride Chloride Chloride CSF Fluid Sweat Urine *Chloropropamide (one of the Sulfonyl ureas) *Chlorpromazine (Largactil) *Chlorpromazine *Cholecalciferol Blood Blood Specimen Requirements Reference Range 1 mL serum or 1.5 mL whole blood for adults or 0.6 mL for neonates in a syringe 1 mL CSF No Longer Available 1 mL fluid No Longer Available See Sweat Chloride Random or 10 mL Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 2 Green 2 mL Aliquot and freeze plasma 2 Red Urine L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 4 mL serum Units Testing Site LIS Code SDCL – Toronto CHLAM CHLOZ Therapeutic: 2-17 Toxic: >33 mol/L Serum: 98-110 Whole blood: 98-106 mmol/L SDCL TAT: Emerg = 4 hr Routine = 3 days Chem - RGH & PH 120-130 None available mmol/L mmolL Chemistry - RGH Chem - RGH & PH <14 yr: 50-170 >14 yr: 150-250 mmolL Chemistry - RGH CLURA CL24 SDCL CHPRO SDCL TAT: Emerg = 4 hr Routine = 3 days CHLOP 0.1-2.0 mol/L See Phenothiazines See Vitamin D 25 Hydroxy Print Date: June 12, 2015 CL (Serum) ABLCL (whole blood) 27 Test Name Specimen Container Volume Cholesterol Blood Cholesterol Cholinesterase, Pseudo (if ordered with Dibucaine #) Fluid Blood *Cholinesterase, Pseudo (no Dibucaine #) Note: Baseline specimen (30-60 days before the pesticide spray season) is highly recommended. Chorionic Gonadotropins *Chromium Blood 1 SST 1 SST 1 SST Specimen Requirements Reference Range Units Testing Site LIS Code mmol/L Chemistry - RGH CHOL mmol/L Chem - RGH & PH Special Chem RGH CHOFL PSDIN SDCL TAT = 2 days PCHOL Separate ASAP into polypropylene tube. Indicate on requisition that specimen is lithium heparin plasma. SDCL - Toronto TAT = 3 weeks CHROM Record on req. collection date and 24 hr volume. SDCL - Toronto TAT = 3 weeks 1 mL serum <30 yr: 3.2-4.6 30-65 yr: 3.8-5.2 >65 yr: 4.2-6.2 1 mL fluid None available 1 mL serum Separate serum as soon Dibucaine No: 78-89 as possible Fluoride No: 62-71 Cholinesterase: Female: 150-330 Male: 200-350 1 mL serum Separate from cells ASAP. 7-19 Refrigerate. Transport ice packs within 24 hr of collection. U/L U/L U/mL See ß-hCG Blood 3 mL 1 – 7 mL Royal Blue plasma EDTA) BD368381) *Chromium Urine 24 hr urine 10 mL in acidaliquot washed container *Chromogranine-A Blood 1 EDTA (Mauve) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL EDTA Freeze plasma SDCL – Hospital in CHRGA Commons Print Date: June 12, 2015 28 Test Name Specimen Container Volume Specimen Requirements Reference Range Chromosome Studies Blood (Whole Blood) Collect specimen Monday to Thursday mornings only. Diagnosis must be stated on req. 1 Green (Sodium Heparin, not Lithium) 3-4 mL Keep at room temperature (adult) at all times. Must be at whole RGH by noon. blood heparinized 1-2 mL (newborn) Chromosome Studies Bone (Bone Marrow) Marrow Collect specimen Monday to Thursday mornings only. Diagnosis must be stated on req. Bone marrow put in RPMI Bone Marrow Transport Media. Two containers of media 2 - 15 mL Sterile falcon centrifuge tubes 2 mL bone marrows aspirate Chromosome Studies Amniotic (Amniocentesis) Fluid Collect specimen Monday to Thursday mornings only Chromosome Studies for Molecular Testing DNA Chylomicrons Citrate Patient's age is required. State collection period. Blood Urine *CJD CSF CK (CPK) Blood 15-20 mL amniotic fluid Units Testing Site LIS Code RGH will send to BLCHR Royal Columbian Hospital, New Westminster -New Leukemia children to Calgary Lab Services -JAKS2 and BCRAB to BC Cancer Agency RGH will sent to BC -Royal Columbia (Temporarily) BMCRS Vancouver, BC Keep at room temperature. Must be at RGH by noon. Keep at room temperature at all times. Transport the same day. Occasionally BC Cancer BMCHR RGH will send to Royal Columbian Hospital, New Westminster AMCHR See Molecular testing 1 SST 24 hr urine 10 mL aliquot of 24 hr urine mmol/d SDCL to U of A CITRU 1 SST U/L Chem - RGH & PH CKS L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen to Chemistry Refrigerate during Lower limit of normal at age 20 is collection. Send frozen. 0.78 and increases at rate of 0.037 Record 24 hr volume.(If for each year collected with oxalate send sep req and specimen.) See Creutzfeld Jakob Disease. 1 mL serum Male: 55-170 Female: 30-135 Print Date: June 12, 2015 29 Test Name Specimen Container Volume CK-MB Screen CK-MB Mass Blood (Total CK available only – not MB) *Clobazam (Frisium) Blood Includes N-desmethyl clobazam *Clomipramine Blood (Anafranil) Units Testing Site LIS Code Chemistry - RGH MASS nmol/L SDCL TAT = 3 days CLOBA nmol/L SDCL TAT: Emerg = 4 hr CLOMI nmol/L SDCL TAT = 3 days CLONZ nmol/L SDCL CLOZA No longer available MB and MBRI NO LONGER AVAILABLE 2 Red 4 mL serum 2 Red 4 mL serum Do not use SST. Record time of collection on tube and req. 4 mL serum Do not use SST. Record or 4 mL time of collection on tube plasma and req. 4 mL serum Do not use SST. Record Therapeutic: 300-2100 or 4 mL time of collection on tube Toxic: >4000 plasma and req. No longer available ORDER: CMV Viral Load Whole blood 1 mL Freeze and ship ASAP to SDCL 2 mL serum If acute is negative, submit convalescent in 5-10 days. *Clonazepam (Rivotril) Blood 2 Red or 2 Green *Clozaril (Clozapine) Blood 2 Red or 2 Green *CMV - Antigenemia *CMV - Buffy Coat Blood 2 Mauve *CMV – CSF PCR **CMV IgM Cytomegalovirus IgM Serology * *CMV IgG Cytomegalovirus IgG Serology *CMV Urine CMV Isolation or Detection *CMV – Viral Load CSF Blood Sterile container 1 SST Blood 1 SST Urine Sterile urine container 1 Mauve Blood Specimen Requirements Reference Range Clobazam: 150-1000 N-desmethylclobazam: 280014000 16-630 (up to 1500 for nonresponders) Toxic: >1700 Therapeutic: 60-220 Toxic: >230 CMV/A SDCL CMV/B SDCL to RUH, Saskatoon SDCL CMV/C CMVMS 2 mL serum Convalescent (Immune status) SDCL CMVIS 20 mL urine (random) SDCL CMV/U Whole blood SDCL- Saskatoon CMVVL SDCL - Toronto COBAL Ship on Ice. Collect in AM and must be at SDCL by (CMV PCR) noon Monday – Thursday. If unable to reach SDCL by noon aliquot plasma and refrigerate. Notify referral desk: 787-3131. *Cobalt Urine Random or 10 mL urine Wash container with 24 hr urine 500 mL of a 10% sol'n of Provide collection container nitric acid. Rinse the date and DOB L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 30 Test Name Specimen Container Volume *Cocaine Urine *Coccidioidomycosis Serology *Codeine *Codeine Cold Agglutinins Blood Blood Urine Blood acidwashed Random. Tightly sealed container 1 SST 1 Red Random 1 Mauve + 1 Red clotted at 37º C Specimen Requirements Reference Range container twice with deionized water. 20 mL urine Blood unsuitable. Refrigerate. Units Negative 3 mL serum 50 mL urine 3 mL whole Centrifuge and separate blood and 4 serum. Label tubes with mL serum first and last name, MRN or HSN and DOB. See CAE *Complement Activation E Complete Blood Count Coombs Blood 1 Mauve Congentin *Copper (Plasma) Blood Blood 2 Red 4 mL serum 2 mL EDTA Separate ASAP into 1 – 7 mL polypropylene tube. Royal Blue plasma Indicate on requisition that EDTA) BD368381 specimen is EDTA plasma. DO NOT FREEZE *Copper (Urine) Urine 24 hr or random urine in acidwashed container Testing Site LIS Code SDCL TAT = 2 days COCAI SDCL - Edmonton TAT = 3 weeks SDCL SDCL Transfusions - RGH COCCS CODS CODU *COLA See CBC Coproporphyrin *Cordarone L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Label tubes with first and last name, MRN or HSN and DOB 7 mL of 24 hr or random urine in acidwashed container Send in polypropylene container. Record 24 hr volume if submitted or random urine and collection date on req. Negative 0-3 m: 1.4-7.2 3-6 m: 3.9-17.3 6-12 m: 7.9-20.1 1-13 yr: 12.6-19.0 13-Adult (Female): 9-27 13-Adult (Male): 11-22 Transfusions - RGH *DANT mol/L SDCL SDCL TAT = 2 weeks CONGE COPS SDCL - Toronto TAT = 3 weeks COPU See Porphyrins See Amodarone Print Date: June 12, 2015 31 Test Name Specimen Container Volume *Core Antigen Correction Studies Blood *Corticosteroids Blood 1 SST or 1 Green *Cortisol (Saliva) Saliva *Cortisol (Serum) Blood *Cortisol Urine Free Urine Doctor’s office must contact SDCL 787-3197 for collection kit and instructions 1 SST 1 mL serum Critical - record time of collection. (250 L – neonates) Cannot be capillary specimen. 24 hr urine 10 mL of 24 Record volume hr urine 1 SST *C-Peptide (must be fasting) Testing Site LIS Code SDCL HEBCO SDCL COSTE SDCL CORSA (AM) 0800 h: 138-690 nmol/L (PM) 1600 h: approximately half of AM values SDCL TAT = 3 days CORTR Adult: 25-146 nmol/d SDCL TAT = 7 days CORTU 298-1324 pmol/L SDCL TAT = 7 days CPEP Chemistry - RGH CRPA Chemistry - RGH CRPHS See Bleeding Disorder Investigation (BLDWS) 2 mL serum or plasma See ACTH Stimulation Blood Blood See Rickettsial Serology. **C. pneumoniae Blood C-Reactive Protein (CRP) Blood 1 SST 1 mL serum Avoid hemolysis. Note fasting sample on req. Freeze within 2-3 hrs of collection. Submit as separate samples. See Chlamydophilia pneumoniae IgM and IgG. 1 mL CRP (high sensitivity) Blood 1 SST 1 mL serum Creamatocrit Units 1 mL serum CosyntropinStim. *Coxiella burnetii Specimen Requirements Reference Range 1 SST Milk L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL No Longer Available human milk CRP Reference Range mg/L 0 - 8 mg/L >10 mg/L -infection or inflammation hsCRP - Risk of cardiovascular mg/L disease: Low risk - < 1.0 mg/L Average risk - 1.0 - 3.0 mg/L High risk - >3.0 mg/L Special Chem RGH Print Date: June 12, 2015 32 Test Name Creatine Kinase Creatinine Creatinine Creatinine State collection period Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code mol/L Chem- RGH & PH CREAT mol/L mmol/d Chem - RGH & PH CREFL Chem – RGH & PH CRURA (random) CRE24 (24 hr) Chem - RGH & PH CC24C See CK Blood 1 SST Fluid Urine 1 mL fluid Random or 2 mL urine 24 hr urine Creatinine Clearance Urine and Blood (State patient's height (cm) & weight (kg) and collection period) 1 ml serum 24 hr urine 10 mL of and 1 SST 24 hr urine and 1 mL serum *Creutzfeld Jakob CSF Disease CSF Creutzfeld Jakob Disease (BSE, CJD) Cross Match Blood (Requires diagnosis and reason for transfusion) Sterile leak 2 - 3 mL proof tube Cryofibrinogen Blood 2 Blue Cryoglobulin Blood 1 Red 2 Mauve Adult: 60-130 Pediatric Ranges: 0 – 5 yrs 20-60 6 – 12 yrs 30-70 13 – 14 yrs 40-85 None available Record 24 hr urine volume 24 hr: 7.1-18.0 Record 24 hr urine volume. Needs a serum specimen, patient's height in cm and weight in kg. Rural sites: Send aliquot frozen. Freeze CSF ASAP. If specimen thaws, it is unsuitable for analysis. Needs a Typenex # on out-patient. Requires patient armband (full name, Typenex # or MRN and DOB). Label tubes with full name, DOB and MRN or PHN and Typenex#. 5 mL Collect and keep at 37º C plasma until spun 2 mL serum RGH and PAS - Collect and keep at 37º C, clot in 37º C waterbath. Children(<14yrs) 40-108 mL/min /1.73m2 mL/min (corrected) CC24A (actual) Male: 84-125 mL/min /1.73m2 Female: 76 -114 mL/min/1.73m2 SDCL - Winnipeg CJDC Transfusions - RGH *GSM Immunology - RGH CRYOF Immunology - RGH CRYGL GDML and Rural labs – Clot at 37º C, send serum to RGH ASAP Cryptococcal Antigen Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 0.5 mL MICRO - RGH Print Date: June 12, 2015 CRYPB 33 Test Name *Cryptococcal Antigen CSF Cell Count CSF Cell Count for Cancer Clinic Specimen Container Volume CSF CSF 1 sterile tube 1 sterile tube serum 0.5 mL CSF 1 mL CSF CSF 1 sterile tube 1 mL CSF *Cyanide Blood 1 Mauve *Cyclic AMP Provisional diagnosis for interpretation required. Fasting overnight. *Cyclobenzapine Cyclosporine Blood & Urine 1 Mauve (full) and Random urine Blood Blood 1 Red 1 Mauve 3 mL whole blood 2 mL plasma EDTA and 10 mL random fresh urine 2 mL serum 2mL whole blood Culture & Sensitivity *Cutaneous Immunofluorescence Antibodies L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Units Requires 0.5 mL Specimen must be in lab within a half hour from the time of collection. If sharing same tube, cell count should be done first. Specimen must be in lab within a half hour from the time of collection. If sharing same tube, cell count should. be done first. See Micro Section See Anti-Skin Ab LIS Code Microbiology - RGH CRYPC WBC: (Adults) 0-5 WBC: (Neonates) 0-30 RBC: 0 X 106/L Hem - RGH & PH FLCSF WBC: (Adults) 0-5 WBC: (Neonates) 0-30 RBC: 0 X 106/L Hem - RGH & PH ABCSF Normal: <0.2 Toxic: 2.0 g/mL SDCL - Mayo Labs CYAN Acidify urine with a few drops of 6N HCL. Freeze specimens and send on dry ice. Collect prior to AM dose Testing Site Ranges: Introduction phase up to 3 months post transplant: Kidney 150-225 g/L Liver 225-300 g/L Heart 250-350 g/L Maintenance after 3 months post transplant: Kidney 100-150 g/L Liver 100-150 g/L Heart 125-175 g/L g/L SDCL - Hamilton CAMPS (serum) CAMPU (urine) SDCL Chemistry - RGH CYCLB CYCLO Print Date: June 12, 2015 34 Test Name Specimen Container Volume Specimen Requirements Reference Range Cystic Fibrosis DNA Analysis Check out Blood 2 Mauve (adult) 1 Mauve (child) *Cysticercosis Serology Cystine Blood 1 SST Blood 1 Green 2 mL plasma Aliquot & freeze *Cystine Urine Random Urine Container 5 mL Freeze **Cytomegalovirus IgM Serology (CMV IgM) **Cytomegalovirus IgG Serology (CMV IgG) *Cytomegalovirus Blood 1 SST Blood 1 SST 10 mL (adult) whole blood 5 mL (child) whole blood 3 mL serum Testing Site LIS Code Keep at room temperature at all times. Must be at RGH by noon. Variety of places DNACF Aliquot. SDCL - Edmonton TAT = 4 weeks SDCL- Saskatoon TAT = 1 week CYSTI CYSTP SDCL- Saskatoon TAT = 1 week CYSTU 2 mL serum If acute is negative, submit convalescent in 5-10 days. SDCL CMVMS 2 mL serum Convalescent (Immune status) SDCL CMVIS SDCL CMV/U Transfusions RGH Saskatoon SDCL SESTD Blood See CMV. *Cytomegalovirus Urine Urine CMV Isolation or Detection *Cytotoxic Antibodies Blood Sterile 20 mL urine urine (random) container 1 Red (full) 10 mL blood *Dalmane (Flurazepam) *Darvon D-Dimer Blood 2 Red 4 mL serum Blood Blood 2 Red 1 Blue (full) 4 mL serum 1 mL Can use same tube as PT <500 plasma and APTT. Must be Double-spun and sent frozen if referred in. 1 mL serum Centrifuge immediately, or plasma protect from light. Freeze. *7-dehydrocholesterol Blood (Smith-Lemli-Opitz Screen) Units 1 Red or 1 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 g/mL FLURA SDCL DARVO Hematology - RGH DDIM SDCL - Toronto Print Date: June 12, 2015 7DHYC 35 Test Name Specimen Container Volume *Dehydroepiandrosterone Blood 1 SST 1 mL serum (DHEA-S) *Demoral *Dengue Fever Serology Blood Blood 1 Red 1 SST 3 mL serum 2 mL serum *11 Deoxycortisol Blood 1 SST or 1 EDTA *11 Deoxycorticosterone Blood 1SST or 1 RED 1 mL serum Specimen must be frozen or plasma Frozen 1 mL serum Specimen must be frozen Frozen *Depakane (Valproic Acid) Blood *Desipramine (Norpramin) Blood *Desmythylcolbazam *Desyrel (Trazodone) Blood *Dexamethasone Suppression Test (DST) *DHEA-SO4 (DHEAS) Specimen Requirements Reference Range Female: 0.9-12.0 Male: 2.2-15.0 Units Testing Site LIS Code g/mL SDCL TAT = 3 days DHEAS SDCL SDCL to National Micro Lab, Winnipeg SDCL - Hamilton DEMER DENFS 11DEO SDCL- Mayo Clinic 11DCS See Valproic Acid 2 Red 4 mL serum Do not use SST. Record time of collection on tube and req. Minimum: 150-470 Maximum: 600-1100 Toxic: >1700 nmol/L SDCL DESI TAT: Emerg = 4 hr Routine = 3 days See Clobazam 2 Red 4 mL serum SDCL TRAZO See Lab Service Manual for instructions *Diazepam (Valium) Blood 2 Red Dibucaine Number *Digitoxin Blood 1 Red See Dehydroepiandrosterone Sulfate 4 mL serum Do not use SST. Record time of collection on tube Therapeutic: 350-900 Toxic: >3500 nmol/L SDCL DIAZ TAT: Emerg = 4 hr Routine = 3 days See Cholinesterase L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum SDCL Print Date: June 12, 2015 DITOX 36 Test Name Specimen Container Volume Digoxin (Digitalis) Blood Collect 0-1 hr before next dose; no earlier than 6 hr after last dose. See TDM section for ideal sampling times *1,25 Dihydroxy Vitamin D Dilantin (Phenytoin) Blood 1 EDTA if sending to RGH Or 1 SST for ANHH *Dilantin - Free 1 Red *Diltiazem Dilute Russell Viper Venom Time (DRVVT) *Diphenhydramine (Gravol) *Diphenylhydantoin *Diphtheria Antitoxin Direct Antiglobulin Test (DAT/Coombs) Direct Immunofluorescence Blood Blood Blood Specimen Requirements Reference Range 1 mL plasma Therapeutic & potentially toxic: 2.6-3.2 Therapeutic: 1.0-2.6 Therapeutic & potentially suboptimal: 0.6-1.9 N.B. Potassium status may modify Digoxin Toxicity Or 1 mL serum Units Testing Site nmol/L Chem – RGH & PH DIG Chem - ANHH See Vitamin D1,25 Dihydroxy See Phenytoin 2 mL serum Do not collect in SST. Freeze. SDCL See Cardizem Test is part of LUPWS, see LUPWS 3 Blue (full) and 1 Red 2 Red 4 mL serum Do not use SST. Record time of collection on tube and req. Blood 1 Red Blood 1 Mauve Therapeutic: 40-430 Toxic: >2000 nmol/L See Dilantin 2 mL serum Aliquot serum. Capital Health Requisiton Label tube with first and last name, HSN or MRN FRPTN Special Coag Hem - RGH Negative Tissue biopsies *Disopyramide Blood (Rhythmadon) Collect immediately before nest oral dose for trough concentration. Peak occurs 2-3 hr after last dose LIS Code SDCL DIPH TAT: Emerg = 4 hr Routine = 3 days SDCL- Edmonton TAT = 3 weeks DIPAT Transfusions RGH *DANT Histology - PH 2 Red or 3 mL serum Do not use SST 2 Green or or 3 mL 2 Mauve plasma L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Venous: 9-15 Arterial: 8.2-9.4 mol/L SDCL TAT = 1 day Print Date: June 12, 2015 DISOP 37 Test Name Specimen Container Volume Specimen Requirements Reference Range D-Lactate Add DNA testing Blood 1 Grey 1 mL fluoride plasma Separate immediately. Freeze. DNA Analysis for CF *Note: Call Supervisor, Accession (4495) or Asst Mgr, Lab Support Services (4465) 2 Mauve (adult) 1 Mauve (child) 10 mL Keep at room temperature (adult) at all times. Must be at whole RGH by noon. blood 5 mL (child) whole blood Blood 1 SST 0.5 mL serum *DNASE-B (Anti) *DNASE Titre 24 hr urine 10 mL of 24 Adjust pH to <2 with HCL. hr urine State volume and collection date. 2 Red 3 mL serum 2,3 DPG Blood (Diphosphoglycerate) *Drug Screen Blood Drugs to screen for must be listed individually. *Drug Screen Urine NO LONGER AVAILABLE 4 mL serum Do not use SST. Record or 4 mL time of collection on tube plasma req. Testing Site LIS Code SDCL - Hamilton DLACS (serum) DLACU (urine) RGH will send to DNACF BC Children's Hospital, Vancouver No Longer Available 14 days refrigerated or can be frozen. *Dopamine Urine State collection period *Doriden Blood (Glutethimide) *Doxepine (Sinequan) Blood 2 Red or 2 Green Units Therapeutic: Lower level 300-500 Maximum 800-1000 Toxic: >1700 nmol/L SDCL to MAYO ABDNS SDCL - Toronto DOPA SDCL DORID SDCL DOX TAT: Emerg = 4 hr Routine = 3 days 2 Red 5 mL serum SDCL DRUGS Random 2-5 mL Street drugs screened. aliquots in See SDCL compendium plastic for list of drugs included. tubes(12x7. 5mL) at time of collection. If not SDCL DRUGU L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 38 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code SDCL - Montreal TAT = 4 weeks SDCL TAT = 3 days ECHIN aliquotted send source container. D'Xylose E2 *Eastern Equine Encephalitis **EBV Blood CSF Blood CSF Blood See Xylose See Estradiol See Encephalitis (Viral). See Epstein-Barr Virus. *Echinococcosis Serology *Effexor (Venlafaxine) Blood 1 SST 3 mL serum Aliquot. 2 Red 4 mL serum Do not use SST. Record time of collection on tube and req. *Ehrlichia Serology Blood 1 SST 2 ml serum *Elavil (Amitriptyline) Electrolytes (Na, K, Cl, CO2) Blood Blood 2 Red 1 SST or 1 Green if STAT Electrolytes (Na & K) Breast Milk Sterile Container 5 mL serum 1.5 mL serum or 1.5 mL plasma 5 mL breast milk Electrolytes (Na & K) Not performed on formed stools Feces Stool Container Electrolytes (Na & K) Electrolytes (Na & K) Fluid Urine nmol/L EFFEX SDCL – Winnipeg ERHLS TAT = 4 weeks SDCL Chem – RGH & PH HLYTE (hospital) PLYTE Use Green if STAT or patient does not clot (Hemodialysis or OHS) See individual tests NOT AVAILABLE None available Chem - RGH & PH LYBRM 1 g feces NOT AVAILABLE None available NOT AVAILABLE 1 mL fluid Random or 100 mL 24 hr urine NOT AVAILABLE None available See individual tests for reference ranges of 24 hr urine. None available or random urine. Chem - RGH & PH LYFLD Chem - RGH & PH LYTUR (random) LYT24 (24 hr) Electrophoresis *Encephalitis (Bacterial) – Blood PCR Therapeutic: 250-900 (community) LYFEC See specific test (I.e. protein, hemoglobin) Blood 1 Mauve 2 mL EDTA Refrigerate specimen. Do whole not freeze. Ship on ice blood pack. SDCL (Hemophilus influenzae, L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 BANTS 39 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code 2 mL EDTA Separate ASAP and freeze plasma plasma. Ship on ice. Plasma must be received frozen. Sterile leak 1 ml CSF Freeze CSF ASAP. proof tube. If specimen thaws, it is unsuitable for analysis. SDCL – Winnipeg ENCAS SDCL – Winnipeg ENCCF 1 SST SDCL - Toronto ABEND Neisseria meningitidis, Strept pneumoniae) *Encephalitis (Viral) – Blood Plasma PCR (Eastern Equine, Japanese Encephalitis) *Encephalitis (Viral) CSF Encephalitis (Viral) PCR CSF 1 Mauve (Eastern Equine, Japanese Encephalitis) *Endomysial Antibodies (Anti-Glutenial Ab) *Entamoeba **Enterovirus Serology Eosinophils (urine) *Epinephrine *Epival (Valproic Acid) **Epstein-Barr Virus IgM Serology Blood 1 mL serum Keep specimen cool. Send on ice packs. Blood See Amoebiasis (Entamoeba) Serology. No longer available. Blood Urine Random urine ENTAS 10 mL Hematology – RGH UREOS See Catecholamines See Valproic Acid) SDCL EPIN Blood 1 SST 2 mL serum If acute is negative, submit convalescent in 5-10 days. SDCL EBVMS Blood 1 SST 1 mL serum Convalescent (Immune status) SDCL-Saskatoon EBVGS CSF Sterile leak 1 mL CSF proof tube SDCL EBVC (EBV IgM, Viral Capsid Antigen) **Epstein-Barr Virus IgG Serology (EBV IgG) *Epstein-Barr CSF Epstein-Barr Virus PCR Erythrocyte Protoporphyrin *Erythropoietin (Eprex) (EPO) Recommend collection time 07301200 hr ESR Blood 1 SST or 1 Green Blood 1 Mauve L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Freeze CSF ASAP. If specimen thaws, it is unsuitable for analysis. NO LONGER AVAILABLE. See Zinc Protoprophyrin 2 mL serum Separate from cells and or plasma freeze ASAP. Avoid hemolysis. 3 mL whole SDCL SDCL - Toronto TAT = 3 weeks 0-20 mm/hr Hem - RGH & PH Print Date: June 12, 2015 ERYTH ESR 40 Test Name Specimen Container Volume blood 1 mL serum Refrigerate and keep cool. Female: assay must be done within Follicular phase: <977 48 hr. Mid-cycle: 433-1303 Luteal phase: 95-606 Post-menopausal: <110 Male: <205 1 mL serum Estradiol Blood 1 SST *Estriole - Free (Unconjugated) *Esterone Ethanol Blood 1 SST Blood Blood 1 SST 1 mL serum 1Gray or 1 Green or 1 SST Random 20 mL urine urine 1 Red 2 mL serum *Ethanol (Ethyl Alcohol) Ethchlorvynol (Placidyl) *Ethosuximide (Zarontin) Collect 0-1 hr before dose See TDM section for ideal sampling times Ethyl Alcohol Urine Blood Refrigerate. Send in tightly sealed container. 1 Red or 1 mL serum Do not use SST 1 Green or or 1 mL 1 Mauve plasma Blood 1 Gray 1 Green or 1 SST 1 Grey or 3 mL whole 1 Red blood 0.5 mL serum 1 Blue (full) Blood Euglobulin Lysis Blood Exposure: INHOUSE Source of Exposure Blood 1SST Exposed Person Blood 2 SST & 1EDTA 1 EDTA & 2 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Testing Site LIS Code pmol/L Chemistry - RGH ESTRA SDCL – Toronto FREST TAT = 2 weeks SDCL - Hamilton ESTRO Chemi - RGH & PH ALC Aliquot and freeze Do not open tube Blood *Ethylene Glycol Exposure:ASSAULT Specimen Requirements Reference Range Negative Therapeutic: 283-708 Toxic: >708 mol/L Do not open tube Keep tube stoppered Normal negative Record time and date of Panic value: >4 collection on tube and req. Extra information If this Exposure is due to an depending on if staff or assault please see the following public must be included on ASSAULT Exposure. the requisition (Ward to complete)eg. copies If Pediatric Assault order EXPOS with a VDRL SDCL TAT = 2 days SDCL TAT = 3 days SDCL TAT = 1 day URALC ETHVY ETHOL Chem - RGH & PH ALC mmol/L SDCL ETHGL TAT: Emerg = 2 hr Routine = 1 day Hematology - RGH EUGLO RGH RGH Print Date: June 12, 2015 SORCE (source) EXPOS (exposed person) ASSLT 41 Test Name Specimen Container Volume Exposure: RURAL Source of Exposure Exposed Person Blood Factor Assays Blood 3 Blue (full) Factor V Leiden Blood 1 Mauve (full) Factor VIII Related Antigen Blood 3 Blue (full) Specimen Requirements Reference Range Units Testing Site LIS Code RGH-Chemistry RUSOR (source) RUEXP exposed BLDWS 1 SST (for either) *Farmer’s Lung Blood Fat Content of Breast Milk Fat in Feces Feces 6 mL citrated plasma 4.5 mL whole blood EDTA 6 mL citrated plasma Test is part of BLDWS (see BLDWS) Special Coag Hematology - RGH See Hypercoag Special Coag HCOAG Hematology - RGH ? Saskatoon Special Coag Hematology - RGH Test is part of BLDWS (see BLDWS) See Aspergillus Serology. See Creamatocrit Containers available from SDCL only. No longer available at RGH. Sent out by SDCL with prior approval from Dr. Lehotay. FCFAT *Fatty Acids (Free Fatty Acids) Collect Fasting *Fatty Acids (Very Long Chain) Blood 1 SST 1 mL serum Freeze serum SDCL FFA Blood 2 Red or 2 Mauve SDCL- Saskatoon FALC *Fecal Elastase *Feldene *FEP (Free Erythrocyte Protoporphyrin) *Fenoprofen (Nalfon) Ferritin Stool Blood Blood 1 Red 1 Mauve (full) 2 mL serum Send frozen - 2 mL or plasma minimum (Neonate - 0.5 mL minimum) 5g Frozen 2 mL serum 5 mL whole Keep in dark. Do not spin. blood SDCL – Calgary SDCL SDCL FELAS FELDE TEP 1 Red 1 SST 2 mL serum 1 mL serum SDCL Chemistry - RGH FENOP FER Blood Blood L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 0m-12 m: 9 - 72 1 yr – 5 yr: 3 – 127 6 yr – 10 yr: 9 – 185 11 yr – 14 yr: 6 – 216 g/L Print Date: June 12, 2015 42 Test Name Specimen Container Volume Fetal Hemoglobin Blood Fetal Lung Maturity Amniotic Fluid Fibrinogen Anticoagulant status must be provided on req. Blood Fibrinogen Degradation Products *Fifth Disease *Filariasis Serology 1 Mauve Specimen Requirements Reference Range 15 yr – 20 yr: 5 – 207 > 20 yr Female: 10-200 > 20 yr Male: 30-300 <1 m: 55-85 1 m-6 m: 0-30 6 m-12 m: 0-20 12 m-18 m: 0-10 18 m-5 yr: 0-3 >5 yr: 0-1 3 mL whole blood Units Testing Site LIS Code % Special Chem RGH HBF g/L Hem - RGH & PH FIB SDCL – Montreal TAT = 4 weeks FILAR SDCL - May Lab FLECA See Lamellar Body Count 1 Blue (full) 1 mL citrated plasma Can be same tube if PT and APTT are ordered 2-4 3.5-4.5 (maternity patients) Rural labs: doublespin and freeze if specimen not at RGH within 4 hrs. Order D-Dimer instead Blood Blood FK506 Flecainide Blood (Tambocor) Collect 0-1 hr before dose for trough. Peak occurs 2-3 hr after last dose. 1 SST 2 Red or 2 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Parvovirus B19. 3 mL serum Aliquot. See Tacrolimus 3 mL serum Separate from cells within Toxic: >1 or plasma 2 hr of collection. Send on ice packs or frozen. g/mL Print Date: June 12, 2015 43 Test Name Specimen Container Volume Specimen Requirements Reference Range *Flow Cytometry (CBC must be done with test) Blood, Bone Marrow, Tissue, Body Fluid, FNA Test done Monday-Friday. Specimen must be received within 24 hr and processed within 48 hr. Keep blood and bone marrow specimens at room temperature. Tissue, FNA and body fluids must be refrigerated. Flow Cytometry for PNH Blood Blood and Bone Marrow (sodium heparin) Tissue, FNA and Body Fluids (RPMI media) 1 full ACD (yellow) tube 10 mL ACD Store and transport at whole room temp (18-22 ◦C) blood Collect Monday-Thursday mornings only. 1.8 mL Must be at RGH lab by Sodium noon. Citrate for Specimen must be sent Newborns out the same day as collection Flow Cytometry FNA, Blody Do not add RPMI media (RGH – flow fridge, PH – cyto fridge) (Saskatoon) Fluid, formalin. Deliver to (CBC must be done Tissue lab immedwith test) iately (RGH/PH) to be placed in RPMI media *FLU Test for Severe NasoUniversal Specimen must be Respiratory Illness pharyngeal Transport accompanied with RQHR , Medium Microbiology Requisition Aspirate, and/or Severe Respiratory Washings Illness and Pandemic Influenza Requisition. *Fluoxetine (Prozac) Blood 2 Red 4 mL serum Do not use SST. Record Therapeutic: 16-1600 time of collection on tube and req. *Fluconazole (AntiBlood 1 SST or 2 mL serum Frozen fungal drug) RED L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Testing Site LIS Code Hematology - RGH FLOWG nmol/L RGH to Calgary PNHRF Saskatoon (RUH) (CBC done in Hematology) FLOWC SDCL FLU-R SDCL TAT = 3 days FLUOX SDCL to Edmonton FLUCZ Print Date: June 12, 2015 44 Test Name *Fluphenazine (Moditen) *Flurazepam (Dalmane) Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code nmol/L SDCL TAT = 3 days FLURA See Phenothiazines Blood 2 Red 4 mL serum Do not use SST. Record time of collection on tube and req. *Fluoride Blood 2 mL serum Draw blood into vacutainer and then remove rubber stopper immediately. Aliquot with plastic pipette SDCL - California FLUOR *Fluoride Urine 1 Red Avoid contact with rubber stopper Random SDCL - California FLUOU *Flucytosine Blood 20 mL urine Do not collect in glass container 1 mL serum or plasma SDCL - Toronto FLUCY *Fluvoxamine Folic Acid, Red Cell Blood Folic Acid and Blood Vitamin B12 NOTE: RBC folate done. If either B12 or RBC folate is decreased, serum folate is done. Follicle Stimulating Hormone *Follitropin Fragile X Blood Chromosome 1 Red or 1 Green See Luvox 1 Mauve 1 mL whole Needs hematocrit run in blood Hematology first 1 SST and 1 mL serum Give EDTA tube to 1 Mauve & 1 mL Hematology first. Needs whole to have hematocrit run. blood Therapeutic: 250-640 408.6-1389.8 nmol/L Chemistry - RGH RCFOL RBC folate: 408.6-1389.8 Serum folate: 7.9-36.6 B12: Deficient: <116 Borderline: 116-138 Normal: 138-781 nmol/L Chemistry - RGH B12FO BC Children's Hospital, Vancouver FRAGX pmol/L See FSH **Francisella Acute Serology (Tularemia) Blood 2 Mauve and 2 Green (Na Heparin) 1 SST **Francisella Conval Serology (Tularemia) Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See FSH Keep at room temperature. Collect Monday through Thursday. Specimen must be at RGH by noon. Whole blood (do not spin) 3 mL serum Submit acute and convalscent sera for diagnosis. SDCL – Winnipeg TAT = 4 weeks FRAAS 3 mL serum Submit acute and convalscent sera for diagnosis. SDCL – Winnipeg TAT = 4 weeks FRACS Print Date: June 12, 2015 45 Test Name Specimen Container Volume *Free Androgen Index Blood (Calculated from sex hormone, binding globulin and total testosterone assays) 1 SST *Free Carnitine Blood 1 SST or 1 Green *Free Cortisol Urine *Free Iron (Nontransferrin bound) Blood Free Light Chains (Kappa, Lambda) Blood Free Light Chains (Kappa, Lambda) Urine Free PSA Done if PSA >4 and </=10 *Free-T3 *Free-T4 *Free Testosterone *Frisium (Clobazam) *Fructosamine Fructose in Semen Specimen Requirements Reference Range 1 mL serum 1 mL serum or 1 mL plasma 24 hr Urine 10 mL of 24 hr urine collection 1 Red 1 SST collected, remove serum from cells ASAP 1 SST 2 mL serum Avoid hemolysis. Separate from cells. Freeze. Send on dry ice. Record volume. Refrigerate. Replaces Free Testosterone Male: 14.8-94.8 Female: Normal cycling: 0-8.5 Oral contraceptives: 0-3.4 Postmenopausal (untreated): 06.6 Hirsute: 1.7-20.6 Adult: 18-63 <12 yr: 16-51 Adult: 25-146 Free Kappa:3.3-19.4 Free Lambda:5.7-26.3 Ratio: 0.26-1.65 Units Testing Site LIS Code SDCL TAT = 5 days FAI mol/L SDCL TAT = 10 days CARNS nmol/d SDCL TAT = 7 days CORTU SDCL FREFE Immunology-RGH FRLCI mg/L Immunology-RGH NO LONGER AVAILABLE DO NOT ORDER Blood Blood Blood Blood 1 SST 1 SST 2 mL serum 2 mL serum 2.6-5.7 9-19 pmol/L pmol/L Chemistry - RGH Chemistry - RGH See Testosterone 2 Red Semen L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 3 ml serum 1 mL semen SDCL See Glycosylated Proteinj UNAVAILABLE Special Chem RGH Print Date: June 12, 2015 FRT3 FRT4 FTEST CLOBA FRUCT 46 Test Name Specimen Container Volume FSH Blood 1 SST *FTI (Free Thyroxine Index) *Fungal Serology Blood *Gabapentin *Galactomannin Galactose Blood Blood Galactose Urine Random Galactose-1Phosphate Blood 1 Sodium Heparin Galactose-1Phosphate Uridyl Transferase (GAL-PUT) Gamma Glutamyl Transferase (GGT) Gamma Hydroxy Butyric Acid Gamma Hydroxy Butyric Acid *Gastric Antibody Blood 1 EDTA Blood 1 Red or 1 Green 1 mL serum Keep cool. Do not freeze. Calculation from free T4 and TBG Must indicate requested test on requisition. See: Aspergillus Blastomycosis Coccidioidomycosis Cryptococcal Antigen Histoplasmosis Sporotricosis See Neurontin See Aspergillus Serology. 1 mL serum Separate from cells and or 1 mL freeze plasma 10 mL urine Frozen FSH Male: 13-70 yr: 1.4-18.1 Females: Follicular: 2.5-10.2 Mid-cycle: 3.4-33.4 Luteal: 1.5-9.1 Pregnant: <0.3 Postmenopausal: 23-116.3 Units Testing Site LIS Code IU/L Chemistry - RGH FSHA SDCL <1.11 at 60 minutes after galactose mmol/L feed Special Chem RGH GALSE 0.0-0.8 3.3 for neonates Special Chem RGH SDCL to Diagnostics Services of Manitoba SDCL to Diagnostics Services of Manitoba Chem - RGH & PH GALUR GGT SDCL GHBAU SDCL GHBAS mmolL 4 mL whole Collect on ice. blood Freeze whole blood in plastic vial ASAP. Send frozen to SDCL 4 mL whole Refrigerate blood 1 SST 1 mL serum Urine Random 4 mL urine Blood 1 RED (NO SST) 2.0 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Female: 12-43 Male: 15-73 Frozen. Collect ASAP after suspected ingestion Frozen. Urine preferred. See Anti-Gastric Antibody U/L Print Date: June 12, 2015 GALPH GALPU 47 Test Name Specimen Container Volume *Gastrin Collect fasting (10 hr minimum) Blood *GC Urine Blood Testing Site LIS Code 1 mL serum Centrifuge in the cold ASAP. Freeze serum immediately. Submit a separate sample. Note fasting serum on req. Avoid hemolysis. Send on dry ice. See Neisseria gonorrhoeae. See HCV Genotyping See Hemochromatosis 0-100 ng/L SDCL TAT = 14 days GAST 1 EDTA 1.0 mL plasma Trough: 0.0-2.0 Peak: 5.0-10.0 Toxic: >=15.0 for post > 2.0 for pre mg/L Chemistry - RGH GENT GENPR (trough) GENPO (peak) 1 SST 1 mL serum Taken 1 hr after drink 3.6-7.8 mmol/L Chemistry - RGH GL50G 1 SST for each sample 1 mL serum Specimens (fasting, 1 hr and 2 hr after drink) See section on glucose tolerances for interpretation Chemistry - RGH GTTGE GGT *Gliadin Antibody *Glucagon Patient must be fasting. Units 1 RED Genotyping for HCV Genotyping for Hemochromatosis Gentamycin Trough Blood Peak NOTE: Record exact date and time of last dose and exact date and time of collection See TDM section for ideal sampling times. Gestational 50 g Blood Screen Gestational Glucose Blood Tolerance (75 g drink) Specimen Requirements Reference Range 2 Mauve (EDTA) prechilled L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2- 5 mL EDTA plasma 2 mL minimum. Trough – usually drawn ½ hr before drug is administered. Peak – usually drawn 1 hr after drug is administered, but physician may vary. Daily – 6 to 14 hrs after dose. See Gamma Glutamyl Transferase Anti-Gliadin Ab Place tubes on ice immediately after collection for at least 10 minutes. Spin in refrigerated centrifuge and Freeze plasma. Unsuitable for analysis if specimen thaws. SDCL – Minnesota GLUCA Print Date: June 12, 2015 48 Test Name Specimen Container Volume Glucose Blood ` Glucose CSF NB – Plasma glucose should be measured simultaneously with CSF glucose Glucose Fluid Glucose Tolerance Blood 1 SST or 1 Green or syringe with electrolyte balanced dry heparin Specimen Requirements Reference Range mmol/L 0.5 mL CSF 2.7-4.2 mmol/L None available See section on glucose tolerances for interpretation mmol/L Urine Random Glucose (Urine) State collection period 24hr Urine 24 hr 1 mL urine 1 Mauve 2 mL whole For Newborn - 1 EDTA <1 mo: 11.3 – 21.3 blood microtainer. >1 mo: 4.6 – 13.5 EDTA NO LONGER AVAILABLE 1 Red L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Chem - RGH & PH GLU GLUCR (random) GLUFA (fasting) GLUPC (2 hr PC) ABLGL (Whole Blood) Chem - RGH & PH GLUCF Fasting: 3.6-6.1 Random: <11.1 Whole blood: 3.9-5.8 Glucose(Urine) Glucose-6-Phosphate Blood Dehydrogenase (G6PD) *Glutathione Peroxidase Recommended to order simultaneously with Selenium *Glutethimide Blood (Doriden) Testing Site 1 mL serum or plasma or 1.5 mL whole blood for adults or 0.6 mL for neonates in a syringe 1 mL fluid 0.5 mL serum from each collection 10 mL urine 1 SST for each collection Units 3 mL serum 2 hr (F, 2h) 5 hr (F, 0.5h, 1h, 1.5h, 2h, 3h, 4h, 5h) Gestational (F, 1h, 2h) Will be performed as part of routine urinalysis. LIS Code Chem - RGH & PH GLUFL Chem - RGH & PH GTT2H GTT5H GTTGE Chem - RGH & PH NO LONGER AVAILABLE U/gm Hb Special Chem RGH G6PHD SDCL - Toronto GLUTA SDCL DORID Print Date: June 12, 2015 49 Test Name Specimen Container Volume *Gluten Sensitive 1 SST Glycerol Lysis Time *Glycol (Ethlene) See Acid Glycerol Lysis 1 Grey 3 mL whole Do not use alcohol swab blood 1 Mauve 1 mL whole Refrigerate blood EDTA. Or Capillary – 200 L whole blood EDTA 1 SST or 1 mL serum Avoid hemolysis 1 Green or or plasma 1 Mauve *Glycosylated Blood Hemoglobin (A1CHB) (For monitoring control of diabetics) *Glycosylated Protein Blood Fasting not required *GM1 Ganglioside Ab Blood 1 Red 2 - 1mL serum aliquots. *Gold Gonococcal Blood *GQ1b IgG Blood (Autoimmune Neurological Disease Profile) *Gravol Blood (Diphenylhydramine) Units See Endomysial Antibodies Freeze. *Glyburide (one of the Blood Sulfonyl Ureas) Blood 1 mL serum Specimen Requirements Reference Range Allow specimen to clot at room temp. for 3 hr. Spin, separate and freeze immediately. NO LONGER AVAILABLE Canadian Diabetes Association Guidelines: Ideal non-diabetic: < 6.0% normal Optimal diabetic: < 7.0% target goal Suboptimal diabetic: 7.0-8.4% action may be required Inadequate: >8.4 action required Up to 285 mol/L Testing Site LIS Code SDCL – Specialty labs GLYBU SDCL ETHGL Special Chem RGH A1CHB SDCL TAT = 2 days GLYPR SDCL – Toronto GM1AB (If ordered GM2 see NEURP) No longer available. GONOS 1 RED 1 mL serum Frozen within 60 minutes of collection SDCL –Calgary 2 SST 4 mL serum SDCL DIPH TAT: Emerg = 4 hr Routine = 3 days L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 GQ1b 50 Test Name Specimen Container Volume Specimen Requirements Reference Range Group & Screen Blood Needs a Typenex # on outpatient. Requires patient armband (full name, Typenex # or MRN and DOB). Label tubes with full name, DOB and MRN or PRN and Typenex#. Freeze and submit a separate sample 2 Mauve *Growth Hormone Blood 1 SST Collect fasting or as specified by physician *H1N1 Nasopharyngeal , Aspirate, Washings *Halcion (Triazolam) Blood 2 Red *Haldol (Haloperidol), Blood (Novoperidol), (Apo-Haloperidol), (Peridol) Collect trough before next dose is administered Ham's Test Blood *Hantavirus Serology Blood 1 Green 2 mL 0.06-5.0 Units g/L LIS Code Transfusions RGH *GSM SDCL TAT = 7 days GROWH SDCL TRIAZ SDCL - Toronto HALDO See FLU test for Severe Respiratory Illness. 4 mL 1 mL plasma Separate ASAP. Freeze. 2 Red and 4 mL serum Usually ordered with 1 Mauve & 2 mL Sucrose Lysis Test whole blood EDTA 1 SST 2 mL serum Hematology - RGH HAMSU SDCL – Winnipeg TAT = 3 weeks SDCL – Winnipeg TAT = 3 weeks (Sin Nombre Virus) *Hantavirus CSF Hantavirus Serology Testing Site CSF Sterile leak 2 mL CSF proof tube. Blood 1 SST Also send serum for Hantavirus Serology. HANTA HANTC (Sin Nombre Virus) Haptoglobin HAV L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum 0.53-2.37 g/L Immunology - RGH HAPTO See Hepatitis A Print Date: June 12, 2015 51 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site HBA1C Blood 1 Mauve Refrigerate (for monitoring 4-6 (Non-Diabetic) control of diabetics) % Special Chem RGH *HBV-DNA Blood 2 Mauve Blood 2 Mauve 4 mL plasma Blood 1 SST 2 mL serum 1 Mauve Anti-Myocardial Ab 2 mL whole Order as CBC blood EDTA HCG *HCV Genotype Patient should be HepC positive before ordering this test HDL-Cholesterol Collect fasting *Heart Muscle Ab Hematocrit Blood *Heavy Metals Do not order as such. Req must state specific test(s) (Lead, Copper, Mercury) **Helicobacter pylori Blood Ab Serology 1 mL whole blood EDTA. CapillaRY – 5 L whole blood placed in a tube containing processing reagent. 2 – 1.5 mL EDTA plasma Freeze aliquots –send as dangerous goods. See β-hCG Remove plasma ASAP. Freeze and ship on dry ice. Split plasma equally between 2 vials. 0.90-2.40 d0-3 mo: 0.44-0.64 3-12 mo: 0.32-0.44 1-3 yr: 0.36-0.44 4-12 yr: 0.37-0.45 Female: 0.37-0.47 Male: 0.4-0.5 mmol./L LIS Code HBA1C SDCL- Winnipeg HBDNA SDCL TAT = 3 weeks HCGEN Chemistry – RGH & PH LIPID Hem - RGH & PH HCT SDCL 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2-5 mL serum Requires only a single serum sample. Specimen must be frozen if not received at RGH within 48 hrs. Chemistry - RGH Print Date: June 12, 2015 HPYLS 52 Test Name Specimen Container Volume Specimen Requirements Reference Range Helicobacter pylori Titre Blood Titre - No longer available. Hemochromatosis Blood Must have clinical info and family history on req. Usually ordered by Dr. Devaraj.**MUST have approval before collection. Hemoglobin Blood Hemoglobinopathy Study (Hemoglobin Electrophoresis, Iron Studies, CBC) Hemoglobin F 3 Mauve 1 Mauve Collect Mon, Tues, Wed, Thurs mornings only. Specimen must be kept at room temp at all times. Specimen must be received at RGH lab by noon and ready for FED-EX pickup at 1400 h 2 mL whole Order as CBC blood EDTA 1 Mauve (full) 1 SST 5 mL whole blood EDTA and 1 mL serum Blood 1 Mauve Hemoglobin in Plasma Blood 1 Mauve Hemosiderin Urine Random Heparin Assays Anticoagulant status & type of heparin used must be provided on the requisition. Must be approved by Dr. Devaraj Heparin Induced Thrombocytopenia (HITT) Blood 1 Blue (full) 1 mL whole blood EDTA 2 mL EDTA Centrifuge immediately plasma and take plasma off into a new tube 10 mL urine 1 mL Must be drawn 4 – 6 hrs citrated post dose. plasma Must be double-spun and sent frozen Blood 1 Red 2- 1mL aliquots of serum If sending, specimen must arrive frozen Testing Site LIS Code HPYLT Whole blood EDTA Blood L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units d0-3 mo; 135-195 4-12 mo: 96-126 1 –3 yr: 110-130 4-6 yr: 120-140 7-12 yr: 115-145 Female: 120-160 Male: 140-180 HbF (adult): 0-1 HBA2: 1.8-3.5 Winnipeg Health Sciences Centre HEMOC g/L Hem - RGH & PH HGB % op total Hb Special Chem RGH HGBWS Special Chem RGH HBF Special Chem RGH PLHB See Fetal Hemoglobin 0-70 mg/L Hematology - RGH URHEM U/mL Hematology - RGH HEPAR Special Coag – RGH Print Date: June 12, 2015 HITT 53 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code *Hepatitis A-IgM, IgG Blood Antibody *Hepatitis A - Total Blood Antibody *Hepatitis B – Blood Genotyping 1 SST 2 mL serum SDCL HEAAB 1 SST 2 mL serum SDCL HEATO 1 SST 2 – 1.5 mL serum Not frozen SDCL-Winnipeg HBGEN *Hepatitis B – Viral Load Blood 2 EDTA Blood 1 SST SDCLImmunoserology Dept. SDCL HBVVL *Hepatitis B Surface Antibody (HBsAb) 2 – 1.5 mL Freeze, ship on dry ice aliquots and send as Dangerous plasma goods. 1 ml serum HEBAB *Hepatitis B Surface Antigen (HBsAg) Blood 1 SST 2 mL serum SDCL HEBAG *Hepatitis B Core *Hepatitis Be Antibody *Hepatitis Be Antigen *Hepatitis C Antibody *Hepatitis C Antigen Hepatitis C Genotyping Blood Blood 1 SST 1 SST 2 mL serum 2 mL serum SDCL SDCL HEBCO HEBEB Blood Blood Blood Blood 1 SST 1 SST 1 SST 1 Mauve 2 mL serum 2 mL serum 2 mL serum SDCL SDCL SDCL SDCL HEBEG HECAB HECAG HCGEN Hepatitis C PCR Blood 2 Mauve 4 mL plasma (EDTA) *Hepatitis C Viral Load Blood 2 Mauve 4 mL plasma EDTA *Hepatitis D Only done if HBV positive *Hepatitis E *Hepatitis F Blood 1 SST 2 mL serum SDCL HEDAB Blood Blood 1 SST 1 SST 2 mL serum 2 mL serum SDCL - Winnipeg SDCL HEEAB HEFAB L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Separate plasma within 6 hr of collection. Freeze and send on dry ice. Separate plasma within 6 hr of collection. Split plasma equally between 2 vials. Freeze and send on dry ice. Separate plasma within 6 hr of collection. Split plasma equally between 2 vials. Freeze and send on dry ice. Send as Dangerous goods. SDCL PCR Test performed 2-3 times per week SDCL HCVVL Test performed 1-2 times per month Print Date: June 12, 2015 54 Test Name Specimen Container Volume *Hepatitis G *Hepatitis Screen *Heroin *Herpes Simplex CSF Herpes Simplex Virus PCR *Herpes Simplex Herpes Simplex Virus IgM Serology *Herpes Simplex Virus IgG Serology Blood Blood Urine CSF 1 SST 1 SST Random Sterile leak proof tube. Lesion Blood Blood 1 SST Specimen Requirements Reference Range Units Testing Site LIS Code 2 mL serum 2 mL serum Includes HAV, HBV & HCV 20 mL urine 2 mL CSF Freeze CSF ASAP. If specimen thaws, it is unsuitable for analysis. See Viral, Lesion. No longer available. SDCL - Winnipeg SDCL SDCL SDCL HEGAB HESCR HEROI HSPCR SDCL HRPVC HSPCS 2 mL serum Immune status SDCL HSPIS (HSV Type 1 & 2) **Herpes Zoster Hexosaminidase Level A & B or Taysachs Test Blood Lesion Blood See Varicella Zoster. See Viral, Lesion. 2 – 5 mL Green (adult) 2 Ped. Green (children) 7 mL whole blood HFE Studies *HGH *HGPRT *HHV-6 Blood *Histamine Blood 1 Mauve prechilled *Histamine Urine *Histoplasmosis Serology Blood 24 hr Urine 5 mL aliquot of well-mixed urine 1 SST 3 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL plasma (EDTA) SDCL - Saskatoon HEXOS See Hemochromatosis See Growth Hormone See Hypoxanthene guanine phosphoribosil transferase. See Roseola IgM and IgG Serology. Collect in prechilled tube and place on ice immediately. Separate ASAP. Freeze. Avoid hemolysis. NO LONGER DONE SDCL - California HISTS SDCL - California HISTA SDCL – Edmonton HPLAS TAT = 3 weeks Print Date: June 12, 2015 55 Test Name Specimen Container Volume *HIV Blood 1 SST HIV Point of Care (performed in-lab) Blood HIV – DNA- PCR Blood Whole blood or whole blood capillary 2 Mauve *HIV Genotyping Blood 2 Mauve 3-5 mL plasma *HIV Viral Load (Ordered on known anti-HIV positive patients, seen by infectious disease physician) Blood 2 or 3 Mauve 3-5 mL plasma HLA Typing Blood Varies with testing site HLAB27 Collection must be booked with Saskatoon HLA 306 655-5205 Blood 1 EDTA tube L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Testing Site LIS Code 1 mL serum Fill in special req. Address of where report is to go must be on req. Plasma or Lab performed only serum specimens SDCL HIV 10 mLwhole bld SDCL-Ottawa HIDPC SDCL-Vancouver HIVGT SDCL HIVVL Saskatoon Lab HLAOD Saskatoon – St. Pauls HLAB2 4 mL Specimen Requirements Reference Range Room Temperature DO NOT Order Fridays or Weekends. Must be received in Ottawa within 48 hrs. Notify SDCL at 787-8635. Centrifuge and freeze 3-5 mL plasma in cryogenic tube. Ship on dry ice. Centrifuge and freeze at –70 degrees at least 1.5 mL plasma in separate cryogenic tubes. Ship on dry ice. (If not enough for 2 tubes use 1 aliquot and note on requisition. Requires pre-booking with testing site. Collect as per requisition. Monday – Thurs. Must be at RGH by noon. Can only be ordered by rheumatologist or ophthalmologist. Must be accompanied by physician completed Saskatoon HLA req. Shipped Monday – Thursday. Must be at RGH by noon for same day shipping. Units HIVPC Print Date: June 12, 2015 56 Test Name Specimen Container Volume *Homocysteine in plasma & urine (child) Blood or Urine 1 Green or 2 mL Same as amino acid. Random plasma Freeze. Urine 10 mL urine *Homocysteine (adults) Blood 1 SST Homogentisic Acid Urine *Homovanillic Acid (HVA) State collection period Include weight of patient if less than 15 years *HPV Cervical HPV PCR (Human Papillomavirus) *HSV Urine HTLV1, HTLV2 *Human Anti-Mouse Antibody *Human Growth Hormone **Human Herpes 6 Virus *Human Papillomavirus **H. zoster, VZV Cervical swab Specimen Requirements Reference Range 1 mL serum Collect on ice. Centrifuge and separate within 1 hr. Freeze serum. Random 30 mL fresh Freeze urine 24 hr Urine 25 mL Keep refrigerated during aliquot of collection. Acidify to pH 224 hr urine 4 with HCL or freeze. Record 24 hr volume and collection period. Universal Transport Medium Blood CSF Lesion Blood 1 SST 2 mL serum Blood 1 RED 1 mL serum Aliquot and Freeze frozen See Growth Hormone Units mol/L Testing Site LIS Code SDCL AACID (serum) AARUR (urine) HCYST SDCL SDCL – Saskatoon HOMAC Adults: up to 82 mol/d 1 mo-2 yr: up to 25 2-5 yr: up to 19 5-15 yr: up to 12 mol/d SDCL HVA SDCL HPVCV RGH, Chemistry Lab SDCL – Mayo HTLV mmol./L creatinine See Herpes Simplex Virus. See Viral, Lesion. Blood Cervical swab Blood Lesion *Human T-Cell Lymphotropic Virus Antibody L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Roseola IgM and IgG Serology. See HPV. Cervical HPV PCR See Varicella Zoster. See Viral, Lesion. See HTLV Print Date: June 12, 2015 HAMA 57 Test Name Specimen Container Volume *5 Hydroxyindoleacetic Acid Urine *17 Hydroxycorticosteroids (17 OHCS) State collection period *17 HydroxyProgesterone Collect between 8 and 10 Urine Blood *17 Blood Hydroxypregnenolone *21 Hydroxylase Blood Antibody Specimen Requirements Reference Range Keep refrigerated during collection. Acidify to pH 24 with HCL or freeze. Record 24 hr volume and collection period. 24 hr Urine 100 mL Adjust pH to <5 with glacial aliquot of acetic acid or freeze. 24 hr urine Record 24 hr volume and collection period. Provide age and sex. 1 SST or 1 mL serum Refrigerate and transport Female: 1 Green or or plasma on ice packs within 24 hr Oral contraceptives: 3-5.1 1 Mauve Neonate: or send frozen. Submit Follicular: 0.3-3.6 separate sample to SDCL. Luteal: 0.3-12.1 100 L Stable for 4 days at 2-8º Prepubertal: <1.8 Separate from cells ASAP Menopausal: 0.3-3.6 Male: 2.2-10.9 1 RED 1 mL serum Freeze Units 24 hr Urine 100 mL aliquot of 24 hr urine 1 SST *25-Hydroxy Vitamin D L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Freeze ASAP. frozen Requires approval from Jeff Eichhorst at SDCL 787-3131. See Vitamin D 25 Hydroxy nmol/L Testing Site LIS Code SDCL 5HIPL SDCL CORTU SDCL TAT = 15 days 17HYD SDCL to Mayo Cl. 17HYP SDCL to Mayo Cl. 21HYD Print Date: June 12, 2015 58 Test Name Specimen Container Volume Urine Hydroxyproline State collection period. About 24 hr before and also during the collection of the sample, give the patient a diet free of collagen. A collagen-free diet contains no meat, meat products, fish, poultry, meat extracts, soup, soup concentrates, gravy, pudding, ice cream, soft candy or other products containing gelatin. Hypercoag Blood - ATIII - Plasminogen - Protein C - Protein S - APC - PTMUT - FVLeiden *Hypoxanthene Blood guanine phosphoribosil transferase 24 hr 10 mL aliquot of well-mixed 24 hr urine 3 Blue(full) 1 Red (Plasma should be double spun) 1 EDTA whole bld 3 Sodium Heparin(3 mL) Ibuprofen IFE Blood 1 Red IgA Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Freeze sample. Record 24 hr volume and collection period. Provide age, weight and height <1 yr: 420-1680 1-22 yr: 190-610 22-65 yr: 40-170 >65 yr: 40-130 Units Testing Site 2 LIS Code Metabolic Diseases Lab in Saskatoon OHPRO 1 mL Arrival at hospital within 4 plasma in 4 hr. Must be sent frozen tubes. and on dry ice. 1 mL serum in 2 tubes. Special Coag Hematology RGH HCOAG Min. 3 mL plasma and saline washed RBCs SDCL to Alberta HGPRT Children’s Hospital Collection must be done at No Transfusions in the last 60 days RGH. Separate ASAP – Freeze plasma. Wash Red cells with saline x2 and after rmoving the last saline wash, freeze the red cells. 2 mL serum Aliquot See Immunofixation Electrophoresis 1 mL serum <3 mo: 0-0.30 3-6 mo: 0-0.50 6 mo-1 yr: 0.10-0.70 1-3 yr: 0.15-1.00 μmol/d/m SDCL g/L IBUPR Immunology - RGH IGA Print Date: June 12, 2015 59 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code SDCL - Toronto IGD SDCL IGE SDCL TAT = 21 days SOMC 3-5 yr: 0.25-1.55 5-8 yr: 0.30-2.35 8-11 yr: 0.20-2.50 11-16 yr: 0.30-2.40 >16 yr: 0.87-3.94 IgD Blood 1 SST *IgE Blood 1 SST *IGF (Somatomedin C) Insulin-like Growth Factor IgG Blood 1 SST 2 mL serum Separate serum ASAP. Freeze Blood 1 SST 1 mL serum IgG Index Blood & CSF *IgG Subclass Blood 1 SST IgM Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Freeze frozen State age of patient 1 mL serum 1 mL serum Both serum & CSF 1 mL CSF required CSF IgG/serum IgG CSF aIb/serum aIb 1 mL serum Freeze and send on ice packs. Provide patient age.Fasting specimen preferred. If not, mark requisition Non-fasting. 1 mL serum Neonates: <1.5 Infants in 1st year of life: <15 1-5 yr: <60 6-9 yr: <90 10-15 yr: <200 Adult: <100 <1 mo: 6.00-16.30 1-3 mo: 2.10-6.20 3-6 mo: 1.35-5.75 6 mo-1 yr: 2.15-8.75 1-2 yr: 3.60-10.40 2-3 yr: 4.20-10.75 3-5 yr: 4.15-12.60 5-8 yr: 5.10-14.35 8-11 yr: 6.10-14.80 11-16 yr: 5.50-14.85 >16 yr: 5.52-17.24 0.30-0.60 IU/mL g/L Immunology - RGH IGG Immunology - RGH IGIDX SDCL - Toronto <1 mo: 0.00-0.20 1-3 mo: 0.10-1.20 3-6 mo: 0.10-1.55 6-12 mo: 0.45-1.20 g/L IGGSC Immunology - RGH IGM Print Date: June 12, 2015 60 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code SDCL - Mayo INHBA SDCL - Mayo INHBB 1-2 yr: 0.40-1.95 2-3 yr: 0.45-2.05 3-5 yr: 0.50-2.25 5-8 yr: 0.40-2.30 8-11 yr: 0.40-2.50 11-16 yr: 0.45-3.00 >16 yr: 0.44-2.47 Inhibin A Blood 1 RED Inhibin B Blood 1 RED *Imipramine (Tofranil) Blood 2 Red or 2 Green 1 mL serum Frozen. Approval required from Jeff Eichhorst at SDCL (787-3131) unless ordered by Dr. C. Aspe-Lucero. 1 mL serum Frozen. Approval required from Jeff Eichhorst at SDCL (787-3131) unless ordered by Dr. C. Aspe-Lucero. 4 mL serum Aliquot. Do not use SST. Minimum: 300-500 or plasma Record time of collection Maximum: 800-1000 on tube and req. Toxic: 1700 See Immunofixation Electrophoresis Immunoelectrophoresis Immunoelectrophoresis Urine Immunofixation Blood Electrophoresis (IFE) 24 hr Urine 50 mL urine aliquot 1 SST 1 mL serum nmol/L SDCL IMIPR TAT: Emerg = 4 hr Routine = 3 days Immunology - RGH IFE Immunology - RGH IFEU Immunology - RGH IFE Immunoglobulins (Quantitative) IgA, IgG, IgM *Inderal *Indocid (Indomethacin) *Infliximab Blood 1 SST 1 mL serum State age Blood Blood 2 Red 1 Red 3 mL serum Aliquot 2 mL serum Aliquot SDCL SDCL INDER INDOM Blood 1 RED SDCL – Mayo Cl INFLX *Influenza A & B Nasopharyngeal 2 mL serum Approval from Jeff Frozen Eichhorst prior to collection (787-3131) Freeze and send ASAP to SDCL See Respiratory Virus Isolation or Detection. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See individual immunnoglobulins for reference ranges Immunology - RGH QIG Print Date: June 12, 2015 61 Test Name *Influenza Pandemic INH Specimen Container Volume Aspirate, Washes Throat Nasopharyngeal Aspirate, Washes Blood 2 Green (full) Specimen Requirements Reference Range 4 mL plasma Aliquot See Bleeding Disorder Investigation Blood 1 Blue *Insulin Blood 1 SST *Insulin Antibodies (Insulin Receptor Antibodies) *-Interferon (Nabferon Inf-B Ab.) Blood 1 SST Blood 1 Red *Interleukin-1 (IL-1) Blood 1 Red *Interleukin-6 (IL-6) Blood 1 Red *Intrinsic Factor Blood Antibodies Avoid administration of B12 for 48 hr before collection *Insulin-like Growth Blodd Testing Site LIS Code SDCL INH See Throat Virus Isolation or Detection. See FLU test for Severe Respiratory Illness. Inhibitor Correction Studies INR Anticoagulant status must be provided on req. Units 1 mL plasma Draw is critical. 2.7 mL in a 3 mL tube. Remove plasma within 2 hr. If not analyzed within 4 hr, freeze. 1 mL serum Freeze serum. Avoid 250 μL hemolysis. neonates Cannot be capillary specimen 1 mL serum 2 mL serum *Needs approval from SDCL 787-7900 Dr.Lehotay 1 mL serum Freeze @ -80 C. Send on dry ice. Special Coag RGH Therapeutic range: DVT: 2-3 Mechanical valve & recurrent P.E.: 2.5-3.5 Hem - RGH & PH PT Fasting 43-194 pmol/L (6-27 μIU/mL) SDCL TAT = 5 days INSUN SDCL - Toronto ABINS SDCL - Mayo SDCL – Toronto IL1 1 mL serum Freeze @ -80 C. Send on dry ice. SDCL - Toronto IL6 2 SST 3 mL serum SDCL – Hamilton TAT = 4 weeks ABINF 1 SST 1 mL serum Frozen SDCL – Toronto IGFBP L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 62 Test Name Factor Binding Protein 3 *Insulin-like Growth Factor Ionized Calcium Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code mmol/L Chemistry - RGH ABLCA (whole bld) IONCA (serum) μmol/L Chem - RGH & PH IBIND See IGF Whole blood: Hospital Sites: <1 mo: 1.05-1.37 1 full green top or blood >1 mo: 1.10-1.29 gas syringe – order Serum: 1.16-1.35 ABLCA-send to lab immediately on ice. OR 1 Tourniquet SST – order IONCA. should not Stable at room temp for be used. 24 hrs or at 4°C for 72 hrs. DO NOT OPEN TUBE. Community Sites: 1 SST-order IONCA. Centrifuge ASAP and send to RGH within 24 hrs. DO NOT OPEN TUBE 1 mL serum Iron: 7-32 TIBC: 45-80 2 mL serum Freeze serum Blood 1 Green (full) or syringe containing electrolyte balanced heparin or 1 SST Iron and Iron Binding (TIBC) *Islet-Cell Antibodies (Pancreatic) *Iso-Propanol (Iso-Propyl Alcohol) Blood 1 SST Blood 1 SST Blood 1 Grey 3 mL whole Keep tube stoppered. blood Refrigerate. JC Virus PCR CSF Sterile container 1 mL JC Virus PCR Blood 1 EDTA 2 mL plasma JC Virus PCR Urine Sterile Container 20 mL Random JAKS-2 Blood 1 EDTA Whole blood *Japanese Encephalitis *JO-1 Antibody Kaolin clotting Time Blood CSF Blood 1 SST 1 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Whole blood 1.6-2.5 mL in syringe. Freeze ASAP If specimen thaws it is unsuitable Freeze ASAP If specimen thaws it is unsuitable Freeze ASAP If specimen thaws it is unsuitable Ship as per Chromosomes Studies *Encephalitis (Viral). Netative Panic value: >8 SDCL mmol/L ABISC SDCL ISOPR TAT: 1 day Emerg = 2 hr SDCL – National Microbiology Lab in Winnipeg SDCL – National Microbiology Lab in Winnipeg SDCL – National Microbiology Lab in Winnipeg BC Cancer Agency JAKS2 SDCL - Hamilton ABJO See Bleeding Disorder Print Date: June 12, 2015 JCVIC JCVIR JCVIU 63 Test Name (KCT) Karyotyping *Keppra *17-Ketogenic Steroids (17KGS) Ketones *Ketoprofen (Orudis) *17-Ketosteroids Provide age, sex and collection period. Pediatric - include patient's weight. Specimen Container Volume Blood Blood Blood Urine Kidney Room PreBlood panel (Na, K, Cl, CO2, glucose, urea, creat, TP, alb, Ca, PO4, Bili, ALT, ALP) Kidney Room PostBlood panel (Na, K, Cl, CO2, glucose, urea, creat, TP, alb, Ca, PO4) Kleihauer Blood 1 Red Specimen Requirements Reference Range Investigation See Chromosome Studies 1 mL serum Syn: Levetiracetam 1 SST or 1 Green 0.5 mL serum or plasma 1 Red 2 mL serum 24 hr Urine 25 mL aliquot of 24 hr urine 1 SST 1 mL serum 1 SST 1 mL serum Test Discontinued Urinary-Free Cortisol done instead Do not open tube Negative Aliquot Refrigerate during collection. Adjust pH to <5 with glacial acetic acid or freeze. Record 24 hr volume, collection period, age and sex. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Male: 35-70 Female: 15-50 Children: 0-3 yr: 0-2 4-8 yr: 0-7 9-10 yr: 2-14 11-14 yr: 2-35 (male) 11-14 yr: 2-30 (female) See individual tests for reference ranges See individual tests for reference ranges 1 Mauve Whole (full) blood Same tube as CBC, if ordered KLM Units μmol/d Testing Site LIS Code SDCL to Mayo KEPRA Chem - RGH & PH KETON SDCL SDCL KETOP 17KS Chemistry - RGH KRPRE Chemistry - RGH KRPOS Hematology - RGH KLEIH See Anti Kidney & Anti Liver Antibodies Print Date: June 12, 2015 64 Test Name Specimen Container Volume Specimen Requirements Reference Range Lactic Acid Blood Lactic Acid CSF Grey: Separate plasma Plasma: 0.7-2.1 from cells within 15 min. Whole blood: 0.5-1.6 Stable at 2-8◦C for 14 days or may be frozen. If Shipping freeze plasma aliquot and send on dry ice. Syringe: deliver to lab ASAP 1.10-2.20 Lactic Acid Lactose Intolerance Fluid Lamellar Body Count Amniotic Fluid *Lamictal (Lamotrigne) Collect pre-dose *Lanoxin *LATS (long acting thyroid stimulator) Blood LD/LDH Blood LD/LDH CSF LD/LDH LD/LDH Isoenzymes Fluid Blood LDL - Cholesterol (calculation) Blood 1 Grey or syringe with electrolyte balanced dry heparin 1 mL plasma or 1.5 mL whole blood for adults or 0.6 mL for neonates in syringe 0.5 mL CSF 1 mL fluid None available Units Testing Site LIS Code mmol/L Chem - RGH & PH LA (plasma) ABLLA (whole bld) mmol/L Chem - RGH & PH LACSF mmol/L Chem - RGH & PH LAFL Hydrogen Breath test done in GI Unit at Pasqua 2 mL 1 SST /uL 2 mL serum Aliquot ASAP Special Chemistry- LBC RGH SDCL Toxicology LAMIC See Digoxin See Thyroid Binding Inhibitory Immunoglobulin 1 SST 1 mL serum 0.5 mL CSF 1 mL fluid <6 mo: 441-564 6 mo-5 yr: 319-441 Adult: 120-245 None available U/L Chem - RGH & PH LDH U/L Chem - RGH & PH LDCSF None available U/L Chem - RGH & PH LDFL Special Chem ISOLD RGH Chem - RGH & PH LIPID No Longer Available 1 SST LE L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2 mL serum Target LDL-C values by level of risk *Risk: LDL-C Very high: <2.5 mmol/L High: <3.0 mmol/L Moderate: <4.0 mmol/L Low: <5.0 mmol/L *To determine risk refer to CMAJ 2000; 162(10):1441-7 Not available. Do ANA Print Date: June 12, 2015 65 Test Name Specimen Container Volume *Lead If a concurrent assay for zinc protoporphyrin is required, it must be specified on the req. Blood 2 mL whole 1 – 7 mL Royal Blue blood Ensure EDTA) BD368381 specimen is well-mixed *Lead Urine 24 hr urine container acidwashed or random acid washed container Lecithin/Sphingomyeln Ratio (L/S Ratio) Amniotic Fld 7 mL of 24 hr or 7 mL random acidwashed container. Aliquot. Specimen Requirements Reference Range Testing Site LIS Code SDCL TAT = 7-10 days LEAD Send in polypropylene container. Provide 24 hr volume and collection date. State if 24 hr or random urine on req. SDCL - Toronto TAT = 2 weeks LEADU See Fetal Lung Maturity Special Chem RGH Also send urine for Legionella Antigen Detection. SDCL LEGC See report or SDCL Compendium Units *Legionella Bronchial *Bronchial Legionella Lavage/ Culture Aspirate Sterile sputum container *Legionella *Urine Legionella Antigen Detection Sterile urine container 20 mL urine Urine (first morning) or at least 2 hrs after last urination SDCL LGU **Legionella Serology Blood 1 SST 2 mL serum Acute (onset) and convalescent (1-3 weeks) SDCL - Etobicoke TAT = 3 weeks LEGAS **Leishmaniasis Blood Serology **Leptospira IgM Blood Serology Leukocyte Alkaline Phosphatase (LAP) CBC must be done at the same time 1 SST 3 mL serum Aliquot. 1 SST 1 mL serum Keep cold but not frozen. SDCL – Montreal LEISH TAT = 4 weeks SDCL – Winnipeg LEPTO TAT = 3 weeks Hematology - RGH LAPSC Urine *Levetiracetam *LH L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 NO LONGER AVAILABLE See Keppra See Luteinizing Hormone Print Date: June 12, 2015 66 Test Name Specimen Container Volume Specimen Requirements Reference Range *Librium Blood *Lidocaine (Xylocaine) See TDM section for ideal sampling times Lipase Blood Blood Lipase Fluid Lipid Profile (Chol, Trig, HDL, LDL) Blood 1 SST 2 mL serum Fasting specimen *Lipoprotein Fractionation (Phenotyping) 14 hr fast. Blood 3EDTA Collect only Monday and Tuesday 7 mL *Lipoprotein A Blood 1 SST *Lipoprotein Electrophoresis Lithium Blood 2 mL Aliquot plasma 3 mL serum Aliquot. Do not use SST. 2 Red or 2 Green or or plasma 2 Mauve Units 1 Green 1 SST or 1 Green 1 mL serum Aliquot or plasma 1 mL 6-21 Toxic: 25-34 Therapeutic: 114-286 Annotate type of fluid on requisition See individual test reference ranges μmol/L Testing Site LIS Code SDCL LIBRI SDCL TAT = 3 days LIDO SDCL TAT = 2 days LIP SDCL LIPFL Chem - RGH & PH LIPID Must be fasting for 14 hrs. Place tubes in ice water immediately after collection. Separate plasma within 1 hr of collection using 30 min. spin. Transfer to polypropylene vial and send cold, not frozen. 1 mL serum Separate within 4 hr of collection. Freeze. SDCL LIPFR SDCL - Toronto LIPOA 1 SST 1 mL serum Not Available SDCL LIPEL Blood 1 SST 1 mL serum Do not collect less than 8 hrs after last dose. See Anti Kidney & Anti Liver Antibodies Therapeutic: 0.5-1.3 Toxic: >2.0 Liver Panel (Hospital) Blood (Bili, ALP, ALT, ALB) 1 SST 1 mL serum See individual test reference ranges Chem - RGH & PH HLIVE Liver Panel (Clinics) (Bili, ALP, ALT) 1 SST 1 mL serum See individual test reference ranges Chemistry - RGH *Liver/Kidney Muscle Antibodies (LKM) Blood *Long Acting Thyroid Stiumlator L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 mmol/L Chemistry - RGH See thyrotropin Binding Inhibitor Immunoglobulin Print Date: June 12, 2015 LI PLIVE 67 Test Name Specimen Container Volume *Long-Chain Fatty Acids (Very) Blood 2 Red or 2 Mauve *Lorazepam (Ativan) Blood 2 Red *LSD L/S Ratio *Ludiomil (Maprotiline) Urine Random *Luminal Lupus Anticoagulant Luteinizing Hormone (LH, Lutropin) Blood 2 Red Blood 3 Blue (full) & 1 Red Blood 1 SST *Luteotrophic Hormone (LTH) Lutropin Luvox Specimen Requirements Reference Range 2 mL serum Aliquot and freeze or plasma Neonates: 0.5 mL serum or plasma 4 mL serum Aliquot. Record time of Therapeutic: 560-740 collection on tube and req. Do not use SST. See Fetal Lung Maturity 4 mL serum Aliquot. Do not use SST. See Phenobarb 4 mL Double spin plasma and plasma separate into 4 tubes. 2 mL serum Freeze all plasma and serum tubes. 1 mL serum Therapeutic: 180-720 Toxic: >1800 Units nmol/L nmol/L Testing Site LIS Code SDCL- Saskatoon FALC SDCL TAT = 5 days LOR SDCL - Toronto LOR SDCL MAPRO TAT: Emerg = 4 hr Routine = 3 days Hematology - RGH LUPWS Male: 20-70 yr: 1.5-9.3 >70 yr: 3.1-34.6 Female: Follicular: 1.9-12.5 Mid-cycle: 8.7-76.3 Luteal: 0.5-16.9 Pregnant: <0.1-1.5 Postmenopausal: 5.0-52.3 Contraceptives: 0.7-5.6 Children: <0.1-6.0 IU/L Chemistry - RGH LHA Therapeutic: 90-500 nmol/L SDCL TAT = 3 days LUV SDCL (Indeterminate – LYMES See Prolactin Blood **Lyme Disease Total Blood IgM and IgG Serology 2 Red or 2 Green 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Luteinizing Hormone 4 mL serum Aliquot. Do not use SST. or 4 mL Record time of collection plasma on tube and req. 2 mL serum Lyme indeterminate specimens are referred to Print Date: June 12, 2015 68 Test Name Specimen Container Volume (Borrelia burgdorferi) 1 mL Specimen Requirements Reference Range NML for supplemental testing. Freeze ASAP Ship ASAP to SDCL CSF Sterile Lymphocytotoxic Antibodies Macroglobulin Macroprolactin Blood 1 Red top Blood Blood 1 SST 1 SST Magnesium Blood 1 SST or 1 Green Magnesium Magnesium State collection period Fluid Urine Malaria Blood Malaria PCR Blood *Malarial (Plasmodium falciparum) Serology *Mandrax (Methaqualone) *Manganese Blood 1 mL fluid No Longer Available None available Random or 10 mL urine Indicate on Requisition if 24 hr: 3.00-5.00 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 1 Mauve Whole Can use same tube as blood CBC 1 Mauve 2 mL ETDA whole blood 1 SST 3 mL serum Aliquot. Blood 2 Red Blood 3 mL 1 – 7 mL Royal Blue plasma EDTA) Aliquot and freeze 4 mL serum Aliquot Aliquot ASAP into polypropylene vial Testing Site NML, Winnipeg TAT = 3 weeks) SDCL to National Microbiology Lab Winnipeg Transplant Centre *Lyme Disease CSF PCR 2 mL serum 2 mL serum Aliquot equally into 2 plastic tubes. Freeze ASAP 1 mL serum or plasma Units 0.66-1.07 (RGH, PH) 0.70-1.10 (SEICC, ANHH) LYMEC SESTO Immunology - RGH MACRG SDCL – Hospitals MACRP in Common, Toronto mmol/L Chem - RGH & PH MG mmol/L Chem - RGH & PH mmol/L Chem - RGH & PH MGUR (random) MG24 (24 hr) Hematology - RGH MALAR SDCL – Montreal TAT = 4 weeks MALRP SDCL - Montreal TAT = 4 weeks MALRS SDCL METHQ SDCL - Toronto TAT = 2 weeks MANG BD368381 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 LIS Code Print Date: June 12, 2015 69 Test Name Specimen Container Volume Specimen Requirements Reference Range Manganese Urine Aliquot. Record collection date, total 24 hr urine volume, if submitted, or random urine on req. *Maprotiline (Ludiomil) Blood 24 hr or random urine in acid washed container 2 Red *Maternal Serum Screen (Maternal serum screening req. must be fully completed. **Measles (Rubeola) IgM Serology **Measles (Rubeola) IgG Serology *Measles (Rubeola) Nasopharyngeal or Throat – Measles PCR Blood *Measles (Rubeola) Urine Measles PCR Urine Sterile Urine Container -> Universal Transport Medium Melanin Urine *Mellaril Blood 10 mL Therapeutic: 180-720 Toxic: >1800 1 SST 2 mL serum Random sample drawn between 15 & 20 weeks gestation. Optimum is 16-17 weeks. Includes: AFP, bHCG, Estriol, Inhibin-A. Also known as QUAD screen. Blood 1 SST Blood 1 SST Random 2 mL serum If acute is negative, submit convalescent in 5-10 days. 2 mL serum Convalescent (Immune status) Leave swab in Universal Transport Medium. Ship to SDCL on ice pack or freeze at -70C. (Can be kept cold up to 24 hrs before specimen must be processed.) 50 mL Centrifuge urine at 2500xg for 15 min. at 4C. Resuspend the sediment in 2 mL Universal Transport Medium. Freeze at -70C. (Can be kept cold up to 24 hrs before processing.) 10 mL Frozen 2 Red 4 mL serum Aliquot L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Testing Site LIS Code SDCL - Toronto TAT = 4 weeks 4 mL serum Aliquot. Do not use SST. Record time of collection on tube and req. Nasophary Swab in ngeal or Universal Throat Transport Medium Units nmol/L SDCL MAPRO TAT: Emerg = 4 hr Routine = 3 days SDCL MSS TAT = 1 day SDCL MEAMS SDCL MEAIS SDCL – Winnipeg TAT = 3 weeks MEA/R SDCL – Winnipeg TAT - 3 weeks MEA/U SDCL- Specialty Lab in California SDCL MELAU Print Date: June 12, 2015 MELLA 70 Test Name Specimen Container Volume *Mercury Blood Specimen Requirements Reference Range Units 7 mL whole Do not separate or freeze 1 – 7 mL Royal Blue blood EDTA) Testing Site LIS Code SDCL - Toronto TAT = 4 weeks MERC SDCL - Toronto TAT = 2 weeks MERCU SDCL TAT = 7 days METAN BD368381 *Mercury Assay of whole blood may be more reliable and is recommended Metabolic Studies *Metanephrine (Catecholamines) Urine Urine 24 hr or Random acidwashed plastic container 24 hr L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 10 mL 24 hr or random aliquot 25 mL aliquot Collect in plastic container. Record urine volume, collection period and date. State if 24 hr or random urine on req. See Amino Acids Refrigerate during collection. Adjust pH to 2-4 with 6N HCL or freeze. Record volume and collection period. 0-3 mo: Metanephrine: 0.03-0.19 Normetanephrin: 0.26-0.85 Total Metanephrine: 0.29-1.04 4-6 mo: Metanephrine: 0.03-0.21 Normetanephrin: 0.17-0.61 Total Metanephrine: 0.20-0.82 7-9 mo: Metanephrine: 0.06-0.21 Normetanephrin: 0.23-0.60 Total Metanephrine: 0.29-0.81 10-12 mo: Metanephrine: 0.04-0.51 Normetanephrin: 0.12-0.56 Total Metanephrine: 0.17-1.07 1-2 yr: Metanephrine: 0.03-0.26 Normetanephrin: 0.18-0.65 Total Metanephrine: 0.21-0.91 2-6 yr: Metanephrine: 0.06-0.50 Normetanephrin: 0.27-0.60 Total Metanephrine: 0.33-1.10 6-10 yr: Metanephrine: 0.28-0.70 Normetanephrin: 0.26-0.96 μmol/d Print Date: June 12, 2015 71 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code SDCL to MAYO METAP SDCL METHS Total Metanephrine: 0.54-1.66 10-16 yr: Metanephrine: 0.20-1.23 Normetanephrin: 0.29-1.59 Total Metanephrine: 0.49-2.82 Adult: Metanephrine: 0.37-1.50 Normetanephrin: 0.57-1.93 Total Metanephrine: 0.94-3.43 Metanephrine (Plasma) Blood 1 EDTA Methadone Blood 1 Red Methadone Urine Random 20 mL Negative *Methaqualone (Mandrax) Blood 2 Red Therapeutic: 2-20 μmol/L Methemalbumin Blood 2 SST 4 mL serum Aliquot. Do not use SST. Record time of collection on tube and req. 4 mL serum 0 mg/L Methemoglobin Blood 1 Green 1 mL whole blood 0-2 % Met Hemoglobin Blood Reductase Deficiency 1 mL plasma Freeze ASAP. Ship frozen, if specimen thaws it is unsuitable. Collect peak 3-4 hr after dose 1 Mauve or 0.2 mL 1 Green whole blood 1 Grey 3 mL whole blood *Methyl Alcohol (Methanol) Blood Methotrexate Blood 1 EDTA 1 mL plasma *Methylmalonic Acid (Patient must be fasting) Blood 2 RED 3 mL serum Aliquot into plastic tube ASAP and freeze. Send frozen.Serum must be separated from cells within 30 minutes. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 SDCL TAT = 2 days SDCL TAT = 3 days Special Chem RGH Special Chem RGH Special Chem RGH Negative Panic value: >15 After high dose chemotherapy: Toxic: 24 hr post dose: >10 48 hr post dose: >1 72 hr post dose: >0.1 After regular therapy: Toxic: >0.1 mmol/L SDCL TAT: Routine 1 day Emerg. 2 hr μmol/L Chemistry - PH SDCL –Alberta Children’s Hosp, Calgary. TAT = 3 weeks Print Date: June 12, 2015 METHQ METHA MTHGA METRD METH MTX MMA 72 Test Name Specimen Container Volume Specimen Requirements Reference Range *Methylphenidate (Ritalin) Urine Random Refrigerate *Mexilitine (Mexitil) Collect trough just before next dose. Peak occurs 2-3 hr after last dose. Microalbumin Blood 2 Red or 3 mL serum Aliquot. Do not use SST. 2 Green or or 2 Mauve 3 mL plasma Therapeutic: 4-11 Toxic: 11.2 Severe toxic: >34 Urine First 10 mL urine Morning or random or 24 hr Urine First 10 mL Morning or random Blood Blood 1 Red 2 Red Microalbumin/ Creatinine Ratio 20 mL Microbiology Tests *Microsomal Antibody *Mitotane *Moclobemide (Menerix) *Modetin (Fluphenazine) *Mogadon (Nitrazepam) To monitor therapy, draw trough specimen before next dose is given *Molecular Testing (DNA) 2 mL 4 mL Samples contaminated with blood are not recommended. Indicate random or 24 hr on sample. For 24 hr, record volume and collection period. Rural sites: Send aliquot frozen. Samples contaminated with blood are not recommended. Rural sites: Send aliquot frozen. See Micro Section See Anti-Thyroid Peroxidase Refrigerate Aliquot Units Testing Site LIS Code SDCL - Toronto TAT = 7 days RITAU μmol/L SDCL TAT = 1 day MEXIL Random: 0-20 24 hr: 0-30 mg/L mg/d Chemistry - RGH MIALB (random) MA24 (24 hr) Female: 0-2.8 Male: 0-2.0 mg/mmol Chemistry - RGH Negative MA/C SDCL- Mayo SDCL MITOT MOCLO SDCL - Toronto MOG Reference Lab MOLEC See Phenothiazines Blood 1 Red or 1 Green Blood Varies (check with supervisor) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Aliquot or plasma Requires pathologist preapproval Print Date: June 12, 2015 73 Test Name Specimen Container Volume Monotest Blood *Morphine Blood *MPO 6-MP/GTG Blood (Metabolite of Azathioprine Crohn's drug) (Thiopurine Metabolites) Mucopolysaccharides Urine **Mumps IgM Serology 1 SST or 1 EDTA Specimen Requirements Reference Range 0.5 mL serum or 2 mL whole blood Units Testing Site Hem - RGH & PH LIS Code MONO SDCL MORPH California 6TGMP Random or 10 mL urine Freeze. State 24 hr or 24 hr random on req. If 24 hr, record volume on req. SDCL- Saskatoon TAT = 2 weeks MUCO (random) MUC24 (24 hr) Blood 1 SST 2 mL serum If acute is negative, submit convalescent in 5-10 days. SDCL MUMMS Blood 1 SST 2 mL serum Convalescent (Immune status) SDCL MUMIS Urine Sterile Urine Container -> Universal Transport Medium 50 mL SDCL - Winnipeg MUM/U Blood 1 Mauve 2-3 mL plasma See P-ANCA 1 Mauve top EDTA whole blood (Parotitis IgM) **Mumps IgG Serology (Parotitis IgG) *Mumps Urine Mumps PCR *Mycology Serology *Mycophenlite L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Centrifuge urine at 2500xg for 15 min. at 4C. Resuspend the sediment in 2 mL Universal Transport Medium. Freeze at -70C. (Can be kept cold up to 24 hrs before processing.) Must indicate requested test on requisition. See: Aspergillus Blastomycosis Coccidioidomycosis Cryptococcal Antigen Histoplasmosis Sporotricosis Spin and Freeze SDCL-Hamilton MYCPH Sent Wednesdays Print Date: June 12, 2015 74 Test Name Specimen Container Volume Specimen Requirements Reference Range *Mycobacterium (TB) Blood Culture *Mycoplasma hominis Mycoplasma and Ureaplasma Culture (Ureaplasma urealyticum, Mycoplasma genitalium) Mycoplasma pneumoniae Culture **Mycoplasma pneumonia (IgM) Serology *Myelin Basic Protein Myoglobin *Mysoline (Primidone) Nabferon(INF-B) Antibody(Beta Interferon) Blood/Bone Marrow See Blood Culture TB (Mycobacterium). *Nalfon *NAPA (N-Acetyl Procainamide) See TDM section for ideal sampling times Units Cervical, Universal Urethral, Transport Respiratory Medium (neonatal) Respiratory Blood CSF Urine Blood Blood Blood Testing Site LIS Code SDCL UREMH No longer available. 2 mL serum If the acute is negative, submit convalescent in 510 days. 0.5 mL Frozen No Longer Available 1 Red 3 mL serum Aliquot 1 Red 2 mL serum Refrigerate.Sample needs to be collected before treatment with interferon or more than 24 hrs postdose See Fenoprofen 1 Red or 1 mL serum Do not use SST 1 Green or or plasma 1 Mauve MYCOP 1 SST MUST BE APPROVED Patient should not be on steroid therapy for at least 2 wks prior to testing. Sum of Procainamide and NAPA Therapeutic range: 43-129 μmol/L SDCL MYPMS SDCL-Calgary MBPCF SDCL SDCL to Athena Diagnostics MYSO SDCL TAT = 1 day PROC *Naproxen (Naprosyn) *Neonatal Screen (PKU, thyroid function) Blood 1 Red 2 mL serum Aliquot SDCL NAPRO Blood Card SDCL TAT = 3 days PKU *Neisseria gonorrhoeae Urine Chlamydia and GC (NAAT) Urine APTIMA Whole blood applied to lab supplied card 20 -30 mL first catch void uine in collection cup SDCL CHLGC L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Using provided disposable pipette, add 2 mL of urine specimen to APTIMA tube. Urine level must be between black fill lines. Print Date: June 12, 2015 75 Test Name Specimen Container Volume *Neurological Disease Profile (Anti-GM1, GM2, GM3, GD1a, GD1b, Bt1b, GQ1b Blood Specimen Requirements Reference Range 1 SST 1 mL serum Freeze ASAP *Neuromyelitis Optica Blood Antibody 1 SST or 1 RED 1 mL serum Freeze specimen. Frozen *Neuron-specific Enolase Blood 1Red DO NOT USE SST Serum *Neurontin (Gabapentin) Collect 2 hr post dose after patient reaches steady state *Niacin Blood 1 nonSST or 1 Green Blood 2 EDTA Nickel Blood 3 mL serum Aliquot into polypropylene 1 – 7 mL Royal Blue or plasma vial EDTA) Do not use SST Aliquot and keep cold but not frozen. Send on ice packs. 1 mL serum Aliquot ASAP and freeze or heparinized plasma 4 mL of plasma Protect from light. Spin and Send frozen Units Testing Site SDCL to Mitogen NEURP Diagnostics, Calgary (if GM1 ordered alone see GM1ABgoes to Toronto) SDCL-Calgary ABNMO SDCL-Mayo ENONS SDCL – Hospital in NEUR Commons, Toronto TAT = 2 weeks SDCL – Minnesota NIACN SDCL - Toronto TAT = 2 weeks BD368381 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 LIS Code Print Date: June 12, 2015 NICKS 76 Test Name Specimen Container Volume Specimen Requirements Reference Range Nickel Urine Record collection datae and 24 hr urine volume, if submitted, or random urine on the req. *Nitrazepam Blood (Mogadon) To monitor therapy, draw trough specimen before next dose is given Nitro Blue Blood Tetrazolium (NBT) *Nitroprusside Therapy *Noctec *Noradrenalin *Norclomipramine *Norepinephrine *Norovirus Stool Norovius PCR Stool Random or 15 mL of 24 24 hr acid- hr or washed random urine container 1 Red or 1 Green 1 mL serum Aliquot or plasma Syringe Sterile stool container Collected only by Hematology staff Must be approved by Hematologist See Thiocyanate Walnut size stool portion with no viral transport or preservative *Norpace *Norpramin *Nortryptyline (Aventyl) Blood Blood Blood 1 Red 2 Red 2 Red *Norverapamil Nuclear Antibodies 5-Nucleotidase L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units 1 mL serum 4 mL serum 4 mL serum See Chloralhydrate See Catecholamines See Clomipramine See Catecholamines Stool must be collected within 48 hrs from onset of symptoms. When an institution suspects an outbreak, inform the Virology Section at (306)787-3138 prior to submitting specimens. Aliquot Aliquot Aliquot. Do not use SST. 190-570 Record time of collection Toxic: >1800 on tube and req. nmol/L Testing Site LIS Code SDCL - Toronto TAT = 2 weeks NICKU SDCL - Toronto NITRA RGH NBT SDCL NORPA STLNW SDCL NORPA SDCL SDCL NORTR TAT: Emerg = 4 hr Routine = 3 days See Verapamil See ANA Not available. Recommend GGT. Print Date: June 12, 2015 77 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Occult Blood –Fecal Stool (FIT) Inpatient and Emerg patients Occult Blood – Fecal Stool (FIT) Outpatient and Community patients Oligoclonal Bands CSF Sterile container New Method kit - Not previous Hemoccult cards. Chemistry FITIN Kit KIT and instructions given to patient. SDCL FIT *Oligosaccharides *Opiates Urine Urine Random Random 2.5 mL CSF 10 mL urine Freeze 20 mL urine Refrigerate *Organic Acids Organic acids in serum are not available *Orudis (Ketoprofen) Osmolality Urine Random 10 mL urine Freeze Blood Blood 1 Red 1 SST or 1 Green Osmolality Osmolality Fluid Urine Osmolal Gap Osmotic Fragilities (Acid Glycerol Lysis Test is usually done instead) Ostase *Ovarian Antibodies Blood 2 mL serum Aliquot 1 mL serum or plasma 1 mL fluid Random or 10 mL urine Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 1 SST or 1 mL serum Serum glucose and urea 1 Green or plasma result required. Calculated Osmolality - Measured Osmolality No Longer Available See ACID GLYCEROL LYSIS L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Negative Special Chem RGH SDCL- Saskatoon SDCL TAT = 2 days SDCL- Saskatoon TAT = 2 days 280-305 None available 300-900 OLIGO OLISA OPIAT OGACU SDCL KETOP mmol/kg Chem - RGH & PH OSMO mmol/kg Chem - RGH & PH OSFL mmol/kg Chem - RGH & PH OSMRU (random) OSM24 (24 hr) 0-14 mmol/kg Chem - RGH & PH OSGAP Hematology - RGH OSMFR See Bone Specific ALP See Anti-Ovarian Ab Print Date: June 12, 2015 78 Test Name Specimen Container Volume *Oxalate Avoid large amounts of vitamin C for 48 hr prior to collection Urine *Oxazepam (Serax) Blood 24 hr Urine 25 mL urine Adjust pH to 2-4 with 6N aliquot HCL or freeze. Record 24 hr volume on req.(If ordered with Citrate, send sep specimen and req) 2 Red 4 mL serum Aliquot. Do not use SST. *Oxcarbazepine Blood 1 Red 2 mL serum Remove serum from cells as soon as possible. SDCL *P-ANCA (MPO) Blood 1 SST 2 mL serum SDCL - Saskatoon PANCA TAT = 2 weeks *Pancreatic Islet Cell Ab Pancretic polypeptides (fasting) *PAPP-A Maternal Serum Screen (Maternal serum screening req. must be fully completed. *Paragonimus Serology *Parainfluenza *Paraneoplastic Disease Profile (Includes: HU, YO, RI, Amphyphysin and PNMA-2) Specimen Requirements Reference Range Male: 80-490 Female: 40-320 7-14 yr: 140-420 <7: not determined Therapeutic: 0.6-5 Units μmol/d Testing Site LIS Code SDCL TAT = 7 days OXU SDCL TAT = 3 days OXAZE OXCRB See Anti-Islet Cells Ab Blood 2 mauve Blood 1 SST 3 mL EDTA Aliquot and freeze plasma 2 mL serum Random sample drawn between 11 & 14 weeks gestation. Blood 1 SST 3 mL serum Aliquot. Nasopharyngeal Aspirate, Washes Throat Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Includes: PAPP-A, Free bHCG, and nuchal translucency test. SDCL PAPEP SDCL TAT = 1 day PAPPA SDCL – Montreal TAT = 4 weeks PARAG SDCL – Mitogen Diagnostics, Calgary PNPDP See Respiratory Virus Isolation or Detection. See Throat Virus Isolation or Detection. 1 mL serum Freeze and ship frozen frozen Includes: HU, YO, RI, Amphyphysin and PNMA-2 Print Date: June 12, 2015 79 Test Name Specimen Container Volume Specimen Requirements Reference Range *Parasitology Serology Blood *Parathyroid Hormone (PTH) Blood 1 EDTA 1 mL EDTA plasma Must indicate requested test on requisition. See: Amoebiasis Babesiosis Cysticercosis Echinococcosis Filariasis Leishmaniasis Malaria PCR Malaria (P.falciparum) Paragonimus Schistosomiasis Strongyloidiasis Toxocariasis TORCH Toxoplasma Antibody Toxoplasma Total Trichinellosis Trypanosomiasis Can be refrigerated up to 2 1.6 – 7.2 days. Rural sites: Freeze plasma *Parathyroid Hormone (PTH) Related Peptide Blood 1 EDTA 2 mL plasma *Parietal Cell Antibody (Parietal Antibodies) Blood 1 SST **Parotitis Blood **Parvovirus B19 IgM Blood Spin and freeze within 2 hrs of collection. Unsuitable if specimen thaws. 2 mL serum Send last B12 result with specimen Units pmol/L Testing Site LIS Code RGH Chemistry PTHA SDCL - Quebec PTHRP SDCL- Saskatoon ABPCA TAT = 2 weeks See Mumps. 1 SST 2 mL serum If acute is negative, submit convalescent in 5-10 days. SDCL PAVMS 1 SST 2 mL serum Convalescent (Immune status) SDCL PAVIS Serology (Fifth Disease IgM) **Parvovirus B19 IgG Blood Serology (Fifth Disease IgG) *Paroxetine L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Paxil Print Date: June 12, 2015 80 Test Name Specimen Container Volume Partial Blood Thromboplastin Time Anticoagulant status must provided on req Paul Bunnell Blood Paxil Blood *PCP *Pemphigoid (Pemphigous) Antibodies *Penicillin Allergen Blood Test (Penicillin G/Penicillin V) *Pentazocine (Talwin) *Pentobarbital Blood Pentothal (Thiopental) 1 mL plasma Draw is critical. 4.5 mL in 24-36 a 5 mL tube. Remove 55-80 (therapeutic range) plasma within 2 hr. If not analyzed within 4 hr, freeze. 1 Red (full) 2 Red or 4 mL serum Do not use SST. Record 2 Green or plasma time of collection on tube and req. See Phencyclidine See Anti-Skin Ab Therapeutic: 94-188 Units sec. nmol/L 2 mL serum 1 Red or 2 Green (full) Blood 1 Red or 2 Green (full) NasoRegan pharyngeal Lowe Transport Medium *Pertussis *Nasopharyngeal Pertussis (Culture and PCR) (Bordetella pertussis) (Whooping cough) Pertussis Serology Blood PFA Blood PH PH 1 Blue Specimen Requirements Reference Range 1 Blue Blood Fluid L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Talwin 3 mL serum Do not use seraclear for or plasma separating plasma (false positives) 3 mL serum Do not use seraclear for or plasma separating plasma (false positives) Testing Site Hematology RGH SDCL SDCL TAT = 3 days LIS Code APTT PAXIL SDCL- Saskatoon Hpnotic: 4-22 Toxic: >44 Coma: 88-221 Hpnotic: 4-21 Toxic: >41 Coma: 124-413 μmol/L Special Chem RGH BARBQ μmol/L Special Chem RGH BARBQ SDCL No longer available. 5 mL whole Approval by Hematologist blood required Whole Blood “Unspun” See Blood Gases 1 mL fluid Specimen must be kept on None available ice PERTU PERTS Special coag RGH PFA Chem - RGH & PH Print Date: June 12, 2015 PHFL 81 Test Name Specimen Container Volume Specimen Requirements Reference Range *Phencyclidine (PCP) Urine Random Urine container 20 mL urine Refrigerate Negative Phenobarbital Blood See TDM section for ideal sampling times Urine *Phenothiazines Chlorpromazine (Largactil) Fluphenazine (Moditen) Mesoridazine Methotrimeprazine Perphenazine (Trilafon) Prochloroperazine (Stemetil) Promazine (Sparine) Thioridazine (Mellaril) Trifluoperazine (Stelazine) Trifluopromazine (Sequil) Trimeperazine *Phenylalanine (PKU) Blood 1 EDTA 1 mL plasma 64-172 Random Urine container 20 mL urine Negative *Phenytoin - Free Blood 1 mL serum or plasma or whole blood 2 Red 4 mL serum 1 EDTA if 1 mL sending to plasma RGH Or Or 1 SST for 1 mL serum ANHH 1 Red 2 mL serum *Philidelphia Blood 2 EDTA *Phenylbutazone Blood Phenytoin (Dilantin) Blood Collect 0-1 hr before dose. See TDM section for ideal sampling times 1 SST or 1 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Record date and time of 1st week of life up to 360 μmol/L, collection on tube and req. thereafter 210 Aliquot Collect 0-1 hr before dose. Therapeutic: 40-80 Toxic: ≥119 Units μmol/L μmol/L μmol/L Testing Site LIS Code SDCL TAT = 3 days PHENC Chemistry - RGH PHENO SDCL TAT = 3 days PHEOZ SDCL TAT = 2 days PHALA SDCL Chem - RGH & PH PHEBZ PHENY CHEM - ANHH Aliquot and freeze in plastic tube. Do not use SST. Keep cool SDCL FRPTN BC Cancer BLPHC Print Date: June 12, 2015 82 Test Name Specimen Container Volume Chromosome Blood Phosphorus Fluid Phosphorus State collection period Urine Phyantic Acid Blood *Placidyl (Ethchlorvynol) Plasma Hemoglobin Plasminogen Platelet 1 SST 1 mL serum 1 mL fluid <14 yr: 1.30-2.00 >14 yr: 0.75-1.55 No Longer available 24 hr: <14 yr: 16-26 >14 yr: 11-36 Blood Random or 10 mL urine Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 1 Green 2 mL Freeze plasma plasma 1 Red 2 mL serum Aliquot Blood 1 Mauve 2 ml plasma 0-70 Blood 1 Mauve Whole blood Platelet Aggregation Centrifuge and remove from cells within 30 minutes See Hypercoag Order CBC Special test - notify hematology Platelet Antibody 1 RED 3 EDTA Blood Pre 1 SST Post – 1 SST P-Neutrophil Cytoplasmic Antibodies *Polio Neutralization Units Testing Site LIS Code Must be sent to SDCL same day as collection by noon. Phosphorus **Pneumococcal Serology Specimen Requirements Reference Range Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Approval Required by Hematologist and must be pre-booked with Saskatoon at 306 655-5205 2 ml serum Requires both pre- and post-immunization samples before sending out. Give vaccination date and clinical history. See P-ANC 1 ml serum mmol/L Chem - RGH & PH Chem - RGH & PH mmol/d Chem - RGH & PH SDCL – Hospital in Commons SDCL mg/L PHOS PO4UR (random) PO424 (24 hr) PHYTA ETHVY Special Chem RGH PLHB Hem - RGH & PH PLT Special Coag Hematology RGH Saskatoon PLABS SDCL – Cadham Prov Lab, Manitoba TAT = 4 weeks PNEUS SDCL POLNT Print Date: June 12, 2015 83 Test Name Test *Polymerase Chain Reaction (PCR) for Hepatitis C (RNA) *Polyomavirus – BK Virus, Porphobilinogen (PBG) Specimen Container Volume Specimen Requirements Reference Range Blood Remove plasma ASAP. Freeze and ship on dry ice. Blood CSF Urine Urine 1 Mauve 1 mL plasma Units Testing Site SDCL LIS Code PCR See BK Virus. Random Frozen 5 mL urine Keep urine in the dark 10 mL plasma Protect from light by wrapping in tin foil. Send plasma frozen. Porphyrins Blood 2 Mauve (EDTA) Porphyrins Fractionation Urine Porphyrins Screen Urine 24 hr Urine 50 mL urine Preservative: 5 g aliquot Na2CO3. Freeze. Collect in brown bottle. Wrap aliquot in tin foil. Record collection time and volume. Keep refrigerated during collection. Random 5 - 10 mL Collect in brown bottle and wrap in foil. Freeze Porphyrins (Qualitative) Quantitation done if screen positive *Porphyrins (Quantitation) Feces Fecal Fat Container 50 g of well-mixed feces Feces Fecal Fat Container 50 g of well-mixed feces L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Protect from light (use dark container or wrap in tin foil). Must be sent in a sealed container. Send frozen. Protect from light – as above. 0-9 Uroporphyrin I: 0-44 Uroporphyrin III: 0-20 Heptacarboxyl Porphyrin: 0-16 Hexacarboxyl Porphyrin: 0-2 Pentacarboxyl Porphyrin: 0-2 Coproporphyrin I: 5-90 Coproporphyrin III: 15-242 μmol/L nmol/d Special Chem RGH PBG SDCL - Toronto TAT = 3 weeks PORPP SDCL TAT = 7 days PORPH Special Chemistry- RGH PORSC SDCL - Toronto SDCL - Toronto TAT = 3 weeks Print Date: June 12, 2015 PORPS PORPF 84 Test Name Specimen Container Volume Potassium (K) Blood 1 SST or 1 Green or Syringe with electrolyte balanced dry heparin Potassium (plasma) Blood 1 Green – Lithium Heparin Potassium Vitreous Fluid only Urine Potassium State collection period PRA (Plasma Renin Activity) PreAlbumin Pregnancy Test (hCG) Pregnancy Test (hCG) 1 mL serum or plasma or 1.5 mL whole blood for adults or 0.6 mL for neonates in syringe 1 mL Only order on request by plasma physician or instruction in LIS. 1 mL fluid Random or 10 mL urine Indicate on Requisition if 24 hr Urine Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen See Renin Blood Blood 1 SST 1 SST 1 mL serum Frozen 1 mL serum Urine Random Urine 5 mL urine *Pregnanediol *Pregnanetriol Prenatal Antibody Screen (Maternal or Paternal) Specimen Requirements Reference Range 3.5-5.0 Units Testing Site mmol/L Chem - RGH & PH 2 Mauve L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Whole blood Label samples with patient’s full name and one of the following: PHN, MRN or DOB. Sign and Date Req. K (serum) ABLK (whole bld) KHEP None available 24 hr: 25-125 Positive/negative Sensitivity 25 IU/L Positive/negative Sensitivity 25 IU/L mmol/L Chem - RGH & PH mmol/d Chem - RGH & PH KFL KURA (random) K24 (24 hr) SDCL - Saskatoon PREAL Chem - RGH & SPREG PH Chem - RGH & PREGU PH Replaced by Progesterone No Longer Available Blood LIS Code CBS Print Date: June 12, 2015 85 Test Name Specimen Container Volume *Primidone (Mysoline) Blood See TDM section for ideal sampling times 1 Red or 1 Green Prion Analysis (PRNP Analysis) Blood 3 ACD 25 mL (yellow Whole glass tube) blood *Procainamide (Pronestyl) See TDM section for ideal sampling times Performed simultaneously with NAPA. *Prochlorperazine (Stemetil) *Progesterone Blood Specimen Requirements Reference Range 1 mL serum Aliquot. Do not use SST. or plasma Store at room temp. Do Not Freeze. Ship at ambient temp. Requisiton for Prion Diseases Program required. Consent form required. 1 Red or 1 mL serum Aliquot. Do not use SST. 1 Green or or plasma 1 Mauve 23-55 Toxic: >55 Units μmol/L Testing Site LIS Code SDCL TAT = 1 day PRIMO SDCL - Winnipeg PRNPA Therapeutic: 17-43 Toxic: >43 Sum of Procainamide & NAPA: 43129 μmol/L SDCL TAT = 1 day PROC Normal Menstruating Female: Follicular phase (preovulation): <0.32-0.95 Luteal phase (postovulation): 3.82-50.6 Postmenopausal: <0.32-0.64 Pregnancy: 1st trimester: 8.9-468 2nd trimester: 72-303 3rd trimester: 89-771 Male: <0.32-0.64 nmol/L Chemistry - RGH PROGS See Phenothiazines Blood 1 SST *Prograf *Proinsulin Patient must be Fasting Blood 1 EDTA (prechilled) Prolactin Blood 1 SST *Promazine (Sparine) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Avoid hemolysis See Tacrolimus 1.5 mL Place tubes on ice plasma immediately after collection for at least 10 minutes. Spin in refrigerated centrifuge and Freeze plasma. 1 mL serum Avoid hemolysis Male: 2.6-18.1 Female: 1.2-29.9 SDCL -Minnesota PROIN μg/L Chemistry - RGH See Phenothiazines Print Date: June 12, 2015 PROLC 86 Test Name Specimen Container Volume Specimen Requirements Reference Range *Pronestyl *Propafenone (Rythmol) Blood Blood 1 Red 2 Red 1 mL serum 3 mL serum Aliquot *Propoxyphene (Darvon) Blood 2 Red 4 mL serum Aliquot. Record time of Therapeutic: 150-600 collection on tube and req. Do not use SST. 4 mL serum Aliquot. Do not use SST. Therapeutic: 190-770 *Propranolol (Inderal) Blood Peak occurs 2-3 hr after last dose. Collect trough level just before the next dose. *Propyl Alcohol Blood 2 Red or 2 Green or 2 Mauve 1 Grey 3 mL whole Do not use alcohol swab blood Prostatic Specific Antigen (PSA) Protein Blood 1 SST Blood 1 SST 1 mL serum Free PSA done if PSA >4 and =10 1 mL serum Protein CSF Protein Fluid Protein State collection period Urine Protein/Creatinine Ratio Urine Protein Electrophoresis Blood 0.5 mL CSF 1 mL fluid Random or 10 mL urine Indicate on Requisition if 24 hr Urine Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen Random 5 mL urine Samples contaminated with blood are not recommended 1 SST 1 mL serum L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Testing Site LIS Code SDCL SDCL TAT = 5-14 days PRONE PROPA nmol/L SDCL TAT = 3 days PROPO nmol/L SDCL TAT = 3 days PROPR SDCL TAT = 1 day PROPY 0-4 μg/L Chemistry - RGH PSA <3 mo: 46-70 3-12 mo: 45-65 1-2 yr: 54-75 2-3 yr: 53-80 >3 yr: 60-80 0.15-0.60 g/L Chem - RGH & PH TP g/L PROCF None available g/L 24 hr: 0.00-0.15 g/d Chem - RGH & PH Chem - RGH & PH Chemistry - RGH Hypertensive Disorders of Pregnancy: < 30mg/mmol mg/ mmol Chemistry – RGH TP/C Albumin: 30-50 Alpha1 globulin: 1-4 Alpha2 globulin: 4-8 Beta globulin: 6-11 Gamma globulin: 7-17 g/L Immunology RGH SPE Print Date: June 12, 2015 TPFL TPUR (random) TP24 (24 hr) 87 Test Name Specimen Container Volume Protein Electrophoresis CSF Protein Electrophoresis Urine Protein C Protein S Prothrombin Time Anticoagulant status must be provided on the req Protoporphyrin (Erythrocyte) Specimen Requirements Reference Range 1 mL CSF CSF Albumin: 111-483 CSF IgG: 6-86 IgG/Albumin Ratio: 0.07-0.25 See Hypercoag See Hypercoag See INR 1 Blue (full) 1 mL plasma Blood 1 Mauve Blood 2 Red 5 mL whole DO NOT SPIN. Keep in blood the dark. EDTA 4 mL serum Aliquot See Prostatic Specific Antigen PseudocholinBlood esterase (If ordered with Dibucaine #) PseudocholinesBlood terase *Psittacosis Serology Blood 1 SST Testing Site Immunology RGH IMCSF Immunology RGH TPEU sec. Hem - RGH & PH 0.30-1.80 μmol/L RBCs Special Chem RGH TEP SDCL FLUOX Special Chem RGH PT PSDIN 1 SST 1 mL serum SDCL 1 SST 1 mL serum SDCL – Winnipeg PSIAS TAT = 4 weeks *PTH *PTH Related Peptide See Parathyroid Hormone See Parathyroid Hormone Related Peptide Blood LIS Code 11.9-13.8 Dibucaine No: 78-89 Fluoride No: 62-71 (Chlamydophilia psittaci, Chlamydia psittaci) PTMUT mg/L 24 hr Urine 50 mL urine Record 24 hr urine volume aliquot and collection period Blood *Prozac (Fluoxetine) PSA Units 1 Mauve Whole blood See Hypercoag *Purkinje Cyto Ab See Anti-Yo *Pyridoxine *Pyruvate (Pyruvic Acid) NO LONGER AVAILABLE See Vitamin B6 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 PCHOL 88 Test Name Specimen Container Volume *Pyruvate Kinase (PK) Blood *Q Fever Blood *Quinidine See TDM section for ideal sampling times *Quinolinic Acid *Rabies Serum Serology 1 Mauve 5 mL whole Ward (NICU), will collect blood on newborn. Collect on Monday and Tuesday See Rickettsial Serology. Blood 1 Red or 1 Green 1 mL serum Do not use SST. Aliquot. or plasma Refrigerate. Blood Blood 2 Green 1 SST *Rabies CSF CSF Rabies Serology *Rapamycin Trough specimen must be drawn immediately pre-dose *Rapid Plasma Reagin *RASH viral panel Rast Test Special sheet must accompany specimen Red Cell Fragility (Osmotic Fragility) Acid Glycerol Lysis Test is usually done instead Specimen Requirements Reference Range Blood Plasma Freeze plasma 2 mL serum Aliquot ASAP and send frozen. Human Rabies Serology Requisition must be completed by ordering physician. Sterile leak 2 mL CSF Freeze CSF ASAP. proof tube If specimen thaws, it is unsuitable for analysis. Human Rabies Serology Requisition must be completed by ordering physician. 1 Mauve 3 mL whole Refrigerate immediately. blood Ship on ice packs. Therapeutic: 6-15 Toxic: >15 Units μmol/L Testing Site LIS Code SDCL - Toronto PK SDCL TAT = 1 day QUIN SDCL- Saskatoon QUINO SDCL - Winnipeg RABIS TAT = 4 weeks SDCL - Winnipeg TAT = 4 weeks RABIC Chemistry-RGH SIROS 1 mL serum To include patient symptoms and date of onset on requisition. Serum 100 µL serum required for each test ordered SDCL RASHP Whole blood Hematology RGH See RPR Blood 1 SST Blood 1 SST Blood 1 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Check with hematology before collection. Collect before 1200. SDCL- Saskatoon RAST Print Date: June 12, 2015 OSMFR 89 Test Name Specimen Container Volume Reducing Substances Urine Reducing Substances Feces *Renal Calculus Renal Panel (urea, Blood creatinine, electrolytes) Renin Direct (replaces renin activity) Blood Random Random 5 mL urine 2g 1 SST 1 mL serum 2 Mauve 3 mL room temp plasma Neonates: 750 uL *Respiratory Syncytial NasoVirus (RSV) pharyngeal Aspirate, Washes Throat Reticulin Ab Reticulocytes Blood 1 Mauve Specimen Requirements Reference Range NO LONGER AVAILABLE NO LONGER AVAILABLE See Calculi See individual tests for reference ranges Separate and Freeze plasma ASAP. Collect between 07001000 See Respiratory Virus Isolation or Detection. See Throat Virus Isolation or Detection. See Anti-Reticulin Ab Can use same tube as CBC Rheumatoid Factor (RA Latex, Latex Fixation) *Rhythmadon Blood 1 SST Whole blood 1 mL serum Blood 1 Red or 1 Green 3 mL serum Aliquot or plasma *Riboflavin *Rickettsial Serology Blood Blood 1 SST (Rickettsia rickettsii, Rickettsia typhi, Rocky Mountain Fever, Q Fever, Coxiella burnetii) Ristocetin Cofactor *Ritalin Urine or Blood *Rivotril (clonazepam) Blood Random Urine or 2 Red 2 Red L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Vitamin B2 2 mL serum Screen includes Q Fever (Phase I & II), Coxiella burnetii, Rickettsia rickettsii IgG and Rickettsia typhi IgG specific assays. Test is part of BLDWS 20 mL urine Urine is preferred. Units Testing Site LIS Code Chemistry - RGH Chemistry - RGH RDSUN RDSFN Chem - RGH & PH HRENA (hospital) PRENA (PML sites) RENIN SDCL Hem – RGH & PH RETIC Immunology RGH RF SDCL RHTHY SDCL - Winnipeg TAT = 6 weeks RICKT SDCL RITAU SDCL CLONZ 4 mL serum Aliquot 4 mL serum Aliquot Print Date: June 12, 2015 90 Test Name Specimen Container Volume Specimen Requirements Reference Range *Rocky Mountain Spotted Fever **Roseola IgM & IgG Serology Blood See Rickettsial Serololgy. Blood 1 SST Blood 1 SST (HHV-6, Human Herpes 6 Virus) *RPR (VDRL) Rapid Plasma Reagin *RSV (Respiratory Syncytial Virus) **Rubella IgM Serology **Rubella IgG Serology **Rubeolla Russell Viper Venom Nasopharyngeal Aspirate, Washes Throat Blood 1 SST Blood Blood *Rythmodan Blood (Disopyramide) *Rythmol *Sabril *Saccharomyces Blood cerevisiae antibodies (Anti-Saccharomyces cer) Salicylate Blood See TDM section for ideal sampling times SARS *SARS Nasopharyngeal or 1 SST 2 Red LIS Code SDCL VDRL SDCL RUBMS SDCL RUBIS See Respiratory Virus Isolation or Detection. See Throat Virus Isolation or Detection. 2 mL seum If acute is negative, submit convalescent in 5-10 days. 1 mL serum Convalescent (Immune status) See Measles (Rubeolla). See DRVVT 3 mL serum Aliquot 1SST 1 mL serum 1 SST or 1 Green 1 mL serum or plasma L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Testing Site SDCL – Winnipeg ROSEO TAT = 3 weeks 1 mL serum Screen includes Roseola IgG and IgM. Viral Exanthemata Requisition must be completed by ordering physician before specimen is forwarded. 1 mL serum RGH DISOP See Propafenone Not available Blood NasoUniversal pharyngeal Transport Units SABRI SDCL – Hospitals ASCA in Common, Toronto Therapeutic: 1.10-2.20 Toxic: >2.3 Usually lethal: >5.0 N.B. Children are more sensitive to the effects of salicylate No longer available. Phone SDCL at (306)787-3131 to pre- mmol/L Chem – RGH & PH SDCL Print Date: June 12, 2015 SALI SARSG SARSR 91 Test Name Specimen Container Volume Throat - SARS or Throat Medium Blood 1 SST Blood Blood 1 SST 1 Mauve (full) *SBG *Schistosomasis Serology (Bilharzia, Bilharziosis, Snail Fever) Scleroderma-70 Sedimentation Rate with CBC Specimen Requirements Reference Range approve testing prior to shipping. See Sex Hormone Binding Globulin 3 mL serum Aliquot. 2 mL serum Whole Can use same tube as blood CBC Test within 8 hrs of collection 3 mL Separate plasma ASAP 1 – 7 mL Send in metal-free Royal Blue plasma polypropylene tube EDTA) Selenium Blood *Selenium Urine 24 hr urine 10 mL container *Serotonin Patient to be on a low tryptophan diet for 2 days prior to collection. Patient to be off all drugs for 3 days prior to collection, if possible. Foods high in tryptophan Include avocadoes, bananas, tomatoes, plums, eggplant, hickory nuts, walnuts, pineapple and mollusks. Blood 1 SST Units Testing Site SDCL – Montreal TAT = 4 weeks LIS Code SCHS Immunology-RGH SCL70 Hematology ESR RGH SDCL- Toronto TAT = 20 days SELEN SDCL – Mayo TAT = 2 weeks SELUN SDCL - Toronto TAT = 4 weeks SEROS BD368381 L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2-1mL serum aliquots Freeze specimen within 4 hr of completing 24 hr collection Centrifuge and separate into 2 aliquots ASAP. Freeze. Print Date: June 12, 2015 92 Test Name Specimen Container Volume *Serotonin See above diet for restrictions Urine 24 hr Urine *Serpax *Severe Respiratory Illness (H1N1) Blood 2 Red Nasopharyngeal , aspirate, washings Sex Hormone Binding Blood 1 SST Globulin (SHBG, SBG) **Shingles Blood Lesion Sickle Dex Blood 1 Mauve (Sickle Cell) All specimens with a Sickle Dex request should also have Hb electrophoresis studies done as well as a CBC. *Silver Urine 24 hr Urine (acidwashed plastic container) *Sin Nombre Virus Blood CSF *Sinequon Blood 2 Red or (Doxepin) 2 Green Specimen Requirements Reference Range Add 20 mL 6N HCL to brown bottle before collection. Do not use Boric Acid. Record volume and collection period. Aliquot urine and freeze. 4 mL serum Aliquot See FLU test for Severe Respiratory Illness. 1 mL serum Male: 13-71 Female: 18-114 nmol/L Testing Site LIS Code SDCL - Toronto SEROU SDCL SERPA SDCL TAT = 5 days SHBG Hematology RGH SICKC SDCL TAT = 3 weeks SILVE SDCL DOX See Varicella Zoster. See Viral, Lesion. 2 mL whole blood 7 mL aliquot Add 20 mL of 6N Nitric Acid at start of collection See Hantavirus. 5 mL serum or plasma *Siquil (Triflupromazine) See Phenothiazines *Sirolimus See Rapamycin L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Print Date: June 12, 2015 93 Test Name Specimen Container Volume Smith-Lemli Opitz Screen Sodium Blood Sodium Fluid Sodium State collection period Urine *Somatomedin-C (IGF-1) Blood *Somatostatin Blood Units Testing Site LIS Code See 7-Dehydrocholesterol *Somatotropin *Sominex Specific Gravity Blood Fluid Specific Gravity Urine 1 SST or 1 Green or Syringe with electrolyte balanced dry heparin 1 mL serum or plasma or 1.5 mL whole blood for adults or 0.6 mL for neonates in syringe 1 mL fluid No Longer Available Random or 10 mL urine Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 1 SST 2 mL serum Separate ASAP. Divide specimen into two equal aliquots and freeze. 1 EDTA 2 mL Keep on Ice. Separate plasma and Freeze immediately. 2 Red 135-145 mmol/L Chem - RGH & PH None available mmol/L Chem - RGH & PH mmol/d Chem - RGH & PH 24 hr: 43-217 See Growth Hormone 4 mL serum Aliquot 1 mL fluid None available 5 mL urine 1.002-1.030 *Sperm Antibodies Spinal Fluid *Sporotricosis Specimen Requirements Reference Range NA (serum) ABLNA (whole bld) NAURA (random) NA24 (24 hr) SDCL - Toronto TAT = 2 weeks SOMC SDCL - California SOSTA SDCL Chem - RGH & PH Chem - RGH & PH SOMIN SGFL SDCL – SPORS U/A See Anti-Sperm See individual tests (glucose, protein, lactic acid, LD, protein electrophoresis) Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 3 mL serum Print Date: June 12, 2015 94 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Serology Edmonton TAT = 3 weeks SDCL 3 mL serum Aliquot See Phenothiazines See Calculi LIS Code *Stelazine *Stemetil Stones Blood *Streptozyme Blood *Strongyloidiasis Serology Blood 1 SST 3 mL serum Aliquot. SDCL – Montreal TAT – 4 weeks STRON *Strychnine *Strychnine Blood Urine 1 RED 2 mL serum 10 mL random urine SDCL SDCL STRYC STRYU Sucrose Lysis Blood 2 Red & 1 Mauve Hematology RGH Special Chem RGH HAMSU Sugar Chromatography Blood Sugar Chromatography Sugar Chromatography Feces Random 3 g feces Urine Random 5 mL urine *Sulfaethoxazole *Sulfatide AutoBlood Antibodies (Sulfamethoxazole) Blood (Septra) (Bactrim) Trough - just before dose. Peak - 3-4 hr after dose. *Sulfonyl Ureas 2 Red Testing Site TRIFL See Anti-Streptoysin (ASO). Usually ordered with Ham's Test NO LONGER available NO LONGER Available 1 SST Freeze if not tested within 24 hrs. Approval required by Dr. B.Mali 766-4493 or Dr.T.Burton 766-4476 See Sulfonamides 2 mL serum Freeze 1 Red 1 mL serum Aliquot L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 SUCRP Ward must state which one (I.e. glyburide, tolbutamide, chloropropamide). Freeze. Therapeutic: 400-730 μmol/L Special Chem RGH Special Chem RGH SUCRF SDCL - California ABSUL Special Chem RGH SULFA SUCRU SDCL - Etobicoke SULUR Print Date: June 12, 2015 95 Test Name Specimen Container Volume Specimen Requirements Reference Range Sulfhemoglobin with Methemoglobin Blood 1 Green 1 mL whole blood *Surmontil (Trimipramine) Blood 2 Red 5 mL serum Aliquot Sweat Chloride Sweat Sulfhemoglobin: 0 Methemoglobin: 0-2 Book with special chemistry at RGH (766-4497) *Syphilis MHA-TP Blood Syphilis IgG (Treponema pallidum) 1 SST 2 mL serum *T3 (Triiodothyronine) Blood (Total T3) 1 SST *T4 (Thyroxine) (Total T4) Blood 1 SST Tacrolimus State drug dosage and time of dose *Talwin For suspected Talwin/ Ritalin abuse only ritalin urine screen is done *Tambocor (Flecainide) Blood 1 Mauve 1 mL serum Order after consultation Neonate – with endocrinologist or 100 μL SDCL consultant biochemist 1 mL serum Order after consultation Neonate – with endocrinologist or 100 μL SDCL consultant biochemist 3 mL whole Collect before dose given. blood Done daily Mon-Fri Urine or Blood Random or 4 mL urine Aliquot. Do not use SST. 2 Red or 2 or serum or Green plasma Blood 2 Red L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 3 mL serum Aliquot Units % Testing Site Special Chem RGH SHB METHB SDCL TRIM (Sweat Chloride by Classic Method) mmol/L Special Chem RGH Interpretation/Results: up to and including 6 months of age: <=29 mmol/L CF unlikely 30 - 59 mmol/L Intermediate >=60 mmol/L Indicative of DF older than 6 months of age: <40 mmol/L CF unlikely 40 - 59 mmol/L Intermediate >60 mmol/L Indicative of CF The result must be interpreted with regard to the patient's age and clinical presentation. Non-reactive LIS Code SWCL3 SDCL TAT = 2-3 days SYPHS 0-89-2.44 nmol/L SDCL TAT = 3 days TT3PL 63-151 nmol/L SDCL TT4PL 3.0-15.0 μg/L Chemistry - RGH TACRS Serum/Plasma: Therapeutic: 170-700 Toxic: >1500 Urine: Negative nmol/L SDCL TAT = 3 days TALWU SDCL FLECA Print Date: June 12, 2015 96 Test Name Specimen Container Volume Tay Sachs Test *TBII Specimen Requirements Reference Range Units Testing Site LIS Code See Hexoaminidase See Thyrotropin Binding Inhibitory Immunoglobulin TAU protein *TB (Mycobacterim) Blood Culture *TBG Blood/Bone Marrow *Teichoic Acid Blood 1 Red All Beta 2 transferrin See Blood Culture TB (Mycobacterium). See Thyroxine Binding Globulin 1 mL serum Aliquot and freeze. Tegretol Tenolin (Tenormen) *Testosterone Blood 1 SST 1 mL serum Therapeutic: 17-50 μmol/L Blood 1 SST Test not available 1 mL serum Submit as a separate sample. Avoid hemolysis. Male: 5.8-28 Female: 0.45-3.74 nmol/L *Tetanus Antitoxin Blood 2 SST Thallium Blood 1-10mL GLASS Sodium heparin tube SDCL - California. TECHO TAT = 4 weeks Chemistry - RGH CARBA SDCL TAT = 14 days TESTO 5 mL serum Capital Health Requisition SDCL- Edmonton TAT = 3 weeks TETAT 7 mL whole blood Do not separate or freeze SDCL - Toronto TAT = 20 days THALS Use polypropylene vial. Record collection date and total 24 hr urine volume, if submitted, or random on the req. SDCL - Toronto TAT = 2 weeks THALU Chemistry - RGH THEO (BD366480) Thallium Urine (24 hr or random) 24 hr or random acidwashed container 10 mL Theophylline Provide Date and Time of Last Dose See TDM section for ideal sampling times *THC Blood 1 EDTA 1 mL plasma Therapeutic: <1 mo: 28-83 >1 mo: 28-85 Toxic: ≥111 μmol/L See Cammabompods (Tetrahydrocannabinol) *Thiamine L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Vitamin B1 THIAM Print Date: June 12, 2015 97 Test Name Specimen Container Volume *Thiocyanate Blood Thiopental Thiopurine Methyltransferase, RBC 1 SST Specimen Requirements Reference Range 1 mL serum Record time of collection on tube and req. Normal: Non-smoker: 0.02-0.21 Smoker: 0.05-0.21 Toxic: >1.75 Units nmol/L Testing Site SDCL TAT = 1 day THIO SDCL – Diagnostic Services of Manitoba THIOM Blood 2 Red 1 Blue (full) 1 SST See Pentothal 5 mL whole Keep refrigerated but not blood frozen. Collect Tues or Wed. morning and must be at SDCL by noon Wed. See Mellaril 3 mL serum Aliquot 1 mL Same tube for PT & APTT plasma 1 mL serum Hematology RGH SDCL Blood 1 SST 2 mL serum Freeze serum aliquot SDCL *Thyroglobulin Level Biospy wash 1 RED *Thyroid Antibodies Blood 1 SST 2 mL serum 1 SST See Anti-Thyroid Peroxidase See TSH 1 mL serum Aliquot and freeze serum. frozen. Indicate thyroid status of patient including presence of exophthalmos on req. *Thioridazine *Thorazine Thrombin Time *Thyroglobulin Includes antithyroid peroxidase (microsomal Ab and thyroglobulin autoantibodies) *Thyroglobulin Level *Thyroid Peroxidase Ab Thyrotropin *Thyrotropin Binding Inhibitory Immunoglobulin Blood Blood Blood Blood 1 EDTA Thyroid Receptor Ab (Thyrotropin) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Wash out FNA needle with normal saline into the Red top tube. Requisition clearly marked as “saline wash from biopsy, Attn Debbie Caswell” LIS Code THIOR THORA TT THYGL THYGB SDCL - In house THYWA for Cancer Agency <100 IU/mL SDCL TAT = 2-3 days ABTH SDCL - Toronto TAT = 3 weeks TBII See Thyrotropin Binding Inhibitory Immunoglobulin Print Date: June 12, 2015 98 Test Name Specimen Container Volume Thyroid Stimulating Hormone *Thyroid Stimulating Immunoglobulin Thyroxine - Total *Thyroxine - Free *Thyroxine Binding Globulin (TBG) Specimen Requirements Reference Range Units Testing Site LIS Code See TSH See Thyrotropin Binding Inhibitory Immunoglobulin TSI See T4 See Free T4 Blood Thyroxine Stimulating Hormone Receptor Ab TIBC *Tissue Blood Transglutaminase Antibody (IGA) Tobramycin Blood 1 SST 1 mL serum SDCL - Toronto TAT = 3 weeks TBG SDCL TAT = 2 weeks ABTTG Chemistry - RGH TOBRA TPBPR TOBPO SDCL IMIPR SDCL TOLBU See Thyrotropin Binding Inhibitory Immunoglobulin See Iron 1 SST 1 mL serum 1 EDTA 1 mL plasma Trough – usually drawn ½ hr before drug is administered. Peak – usually drawn 1 hr after drug is administered, but physician may vary. Daily – 6 to 14 hrs after dose. 5 mL serum Aliquot Therapeutic: Pre: 0.0-2.0 Post: 5.0-10.0 *Tofranil (Imipramine) *Tolbutamide (one of the Sulfonyl Ureas) *Topiramate (Topomax) Blood 2 Red Blood 1 Green Blood 1 non-SST 1 mL serum Aliquot and freeze *ToRC screen *TORCH (Toxoplasma, Rubella, CMV) (Herpes Simplex) *Total Carnitine Blood 1 SST 3 mL serum If unable to collect 0.5 mL 0.5 ml on neonates serum, neonates specify which tests are most important. Blood 1 SST or 1 Green 1 mL serum Separate from cells. Avoid Adult: 21-74 or plasma hemolysis. Freeze <12 yr: 22-60 Total Iron Binding L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 2 mL plasma mg/L Aliquot and freeze SDCL- Hosp. In TOPIR Commons,Toronto TAT = 2 weeks SDCL TORCH μmol/L SDCL TAT = 10 days See Iron Print Date: June 12, 2015 CARNS 99 Test Name Specimen Container Volume *Toxocariasis Blood Serology *Toxoplasma Blood Antibody Confirmation Serology **Toxoplasma Total Blood IgM and IgG Serology 1 SST 3 mL serum Aliquot. 1 SST 3 mL serum Aliquot. 1 SST *TPHA *TPO Blood 1 Red *Transcobalamine Blood 1 SST Transferrin Blood Transferrin Blood Isoelectric Focusing Transglutaminase Ab 1 SST 1 SST *Trazodone Treponema Pallidum *Triazolam (Halcion) Blood 2 Red Blood 2 Red *Trichinellosis Blood Serology *Trichloroethanol *Triiodothyronine (T3) 1 SST *TriiodothyronineFree *Tricyclic Drugs (TCA) *Triflupromazine Triglycerides Collect fasting Triglycerides Specimen Requirements Reference Range Units Testing Site LIS Code SDCL - Montreal TAT = 4 weeks SDCL - Montreal TAT = 4 weeks TOXOC 2 mL serum If the total antibody is present, a specific IgM test will be performed. SDCL TOXOP 2 mL serum NO LONGER AVAILABLE See Anti-Thyroid Peroxidase 2 mL serum Separate immediately. Keep cool. 1 mL serum 1 mL serum Freeze SDCL TPHA SDCL - Toronto TRANS 1.80 – 3.42 See Tissue Transglutaminase 4 mL serum Aliquot See Syphilis 4 mL serum Aliquot 3 mL serum Aliquot. aliquot See Chloralhydrate See T3 g/L TOXIS Chemistry - RGH TFERN SDCL - Saskatoon TRISO SDCL TRAZO SDCL TRIAZ SDCL - Montreal TAT = 4 weeks TRICS SDCL TRICY See Free T3 Blood Blood 2 Red 4 mL serum Aliquot 1 SST See Phenothiazines 1 mL serum Fasting speicmen 0.35-1.70 mmol/L Chem - RGH & PH 1 mL fluid None available mmol/L Chem - RGH & PH Fluid *Trilafon L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Phenothiazines Print Date: June 12, 2015 TRIPR TRIG TRFL 100 Test Name Specimen Container Volume *Trimipramine (Surmontil) Blood Specimen Requirements Reference Range 2 Red 4 mL serum Aliquot. Do not use SST. Triple Screen Troponin I Blood 1 SST See Maternal Serum Screen 1 mL serum Aliquot Troponin T (Cancer patients/ Allan Blair Patients only) Trypsin Blood 1 SST 1 mL serum Frozen Units Testing Site LIS Code Therapeutic: 170-680 Toxic: >1800 nmol/L SDCL TRIM TAT: Emerg = 4 hr Routine = 3 days <=0.02 ug/L ug/L Chem-RGH TROPA SDCL to MAYO TTROP Feces NO LONGER AVAILABLE Chemistry - RGH TRYPS Trypsin *Trypanosomiasis Serology Fluid Blood 1 SST NO LONGER AVAILABLE 3 mL serum Aliquot. Chemistry - RGH SDCL – Montreal TAT – 4 weeks TRYFL TRYPA Tryptase Collect 1 hr postallergic reaction Tryptophan TSH Blood 1 SST 1 mL serum Aliquot and freeze SDCL - Toronto TTASE Blood 1 SST 1 mL serum 100 μL neonate Chemistry - RGH (SDCL does neonate testing) TSHSC (screen) TSHFU (follow-up) TSH with T3 and T4 Blood 1 SST 1 mL serum 600 μL neonates Chemistry - RGH (SDCL does neonate testing) NETSH (to SDCL) SDCL-Toronto TNF See Amino Acid *TSH Receptor Ab 0.49-4.67 mIU/L See Thyrotropin Binding Inhibitory Immunoglobulin Tumor Necrosis Factor **TWAR Blood Blood Tylenol Tyrosine Blood 1 Red 1 Green L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 1 mL serum Freeze at –80 C. Send on dry ice. See Chlamydophilia pneumoniae IgM and IgG. See Acetominophen 1 mL plasma 25-200 μmol/L SDCL- Saskatoon AACID Print Date: June 12, 2015 101 Test Name Specimen Container Volume *Unconjugated Estriol (Perfomed only as part of Maternal Serum Screen) Urea Blood 1 SST or 1 Green Urea Fluid *Ureaplasma *Mycoplasma and Ureaplasma Culture Cervical, Universal Urethral, Transport Respiratory Medium (neonatal) Urea State collection period Urine Uric Acid Blood Uric Acid Fluid Uric Acid State collection period Urine Urinalysis Urine Specimen Requirements Reference Range 1 ml serum or plasma 1 mL fluid Random or 10 mL urine Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen 1 SST 1 mL serum 1 mL fluid Random or 10 mL urine Indicate on Requisition if 24 hr Random or 24 hr urine. Record Collection Time, Date and Volume (if 24 hr ). Rural sites: Send aliquot frozen Random 10 mL L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 0-12 months: 1.4-6.8 1-15 yrs: 2.2-7.0 >15 yr: 3.0-7.1 None available Units Testing Site LIS Code mmol/L Chem - RGH & PH UREA mmol/L Chem - RGH & PH SDCL UREFL 24 hr: 250-600 mmol/L Chem - RGH & PH URURA (random) URE24 (24 hr) Male: 200-500 Female: 145-430 None available μmol/L Chem - RGH & PH μmol/L Chem - RGH & PH mmol/L Chem - RGH & PH URIC μmol/L U/A 24 hr: 1.2-4.5 Glucose: negative Bilirubin: negative Ketones: negative SG: 1.002-1.030 Blood: negative PH: 5.0-8.0 Protein: negative UBG: 3-17 Nitrite: negative Chem - RGH & PH Print Date: June 12, 2015 UREMH URAFL URAUR (random) URA24 (24 hr) 102 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Leucocyte esterase: negative *Urine Free Cortisol (UFC) Urobilinogen See Free Cortisol Urine Random 5 mL urine *Uroporphyrin *Uroporphyrinogen Synthetase Blood 2 Green *Valium (Diazepam) Blood 2 Red Valproic Acid (Depakane, Epival) See TDM section for ideal sampling times Blood 1 EDTA *Vanadium Urine Vancomycin Trough and peak NOTE: Record exact date and time of last does and exact date and time of collection See TDM section for ideal sampling times *Vanillyl Mandelic Acid (VMA) State weight with pediatric specimens. State collection period. *Varicella Zoster Blood Random or 10 mL urine 24 hr urine container, acidwashed 1 EDTA 0.5 mL plasma Urine Keep in dark See Porphyrins Protect from light by wrapping in tin foil 10 mL whole blood 5 mL serum Aliquot 1 mL plasma Collect 0-1 hr before dose. 350-700 Significant liver enzyme elevation and thrombocytopenia may occur at levels >1000 μmol/L Wash container with 500 mL of 10% solution of nitric acid. Rinse container twice with deionized water. Trough - Usually drawn ½ hr before drug is administered. Peak - usually drawn 1 hr after drug is administered, but physician may vary. 24 hr Urine 25 mL urine Refrigerate during aliquot collection. Adjust pH 2-4 with 6N HCL or freeze. Record volume and collection period. Do not over acidfy. Lesion Done as part of urinalysis Chem - RGH & PH U/A SDCL TAT = 14 days UPS SDCL DIAZ Chemistry - RGH VALPR SDCL - Toronto VANAD Trough: 10.0 – 20.0 Peak: 20.0-40.0 Toxic Peak: >=60.0 Toxic Trough: >=20.0 mg/L Chemistry - RGH VANCO VANPR (trough) VANPO (peak) Adult: 9-34 Children: 7-30 d: up to 0.9 30 d-6 mo: up to 1.2 7 m-10 yr: up to 0.8 μmol/d SDCL TAT = 3 days VMA μmol/ kg/day See Viral, Lesion. (H. Zoster, VZV, Herpes Zoster, Chickenpox, L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Print Date: June 12, 2015 103 Test Name Specimen Container Volume Specimen Requirements Reference Range Units Testing Site LIS Code Shingles) **Varicella Zoster IgM Blood Serology 1 SST 2 mL serum If acute is negative, submit convalescent in 5-10 days. SDCL HZVMS 1 SST 2 mL serum Convalescent (Immune status) SDCL HZVIS 2 Mauve 3 mL plasma (EDTA) SDCL - Mayo TAT = 4 weeks VIP SDCL TAT = 1 week CSFVD (H. Zoster, VZV, Herpes Zoster, Chickenpox, Shingles) **Varicella Zoster IgG Blood Serology (H. Zoster, VZV, Herpes Zoster, Chickenpox, Shingles) *Vasoactive Intestinal Blood Polypeptide (VIP) (Collect after an overnight fast) *Vasopressin *VDRL Blood (STS & FTA Absorption) *VDRL CSF Venlafaxine Very Long Chain Fatty Acids Blood Verapamil Blood Draw 1-2 hr after last dose (peak value) *VIP Blood (Vasoactive Intestinal Polypeptide) Fasting specimen *Viral CSF Virus Isolation ( Enterovirus) CSF Separate from cells ASAP. Freeze. Record fasting plasma on req. See ADH SEE Syphilis Sterile Tube 2 Red or 2 Mauve 2 Red 2 Mauve (prechilled) 0.5-1 mL Refrigerate. Non-reactive Provide patient symptoms and onset, recent vaccinations on requisition See Effexor 2 mL serum Send frozen or plasma 500 μL neonates 5 mL serum Aliquot and freeze SDCL - Mayo VERAP 3 mL plasma Collect on ice. Separate ASAP and freeze. Send on dry ice. Record fasting plasma on req. SDCL - Mayo TAT = 4 weeks VIP Do not freeze CSF for viral isolation. SDCL CSFVC Sterile leak 2 mL CSF proof tube. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 SDCL- Saskatoon FALC Print Date: June 12, 2015 104 Test Name Specimen Container Volume *Viral Eye swab Eye Virus Isolation or Detection *Viral Genital Lesion Virus Isolation or Detection (Viral Lesion, Lesion, Herpes, Herpes Simplex, HSV) *Viral Blood Hemmorrhagic Fever (PCR) Universal Transport Medium *Viral Blood Hemmorrhagic Fever (Serology) 1 SST 1 EDTA *Viral Other Lesion Virus Isolation or Detection (Viral Lesion, Lesion, Herpes, Chickenpox, Shingles) *Viral – Lesion Lesion Universal Isolation or Detection swab, Transport aspirate or Medium scrappings L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Units Testing Site SDCL LIS Code EYEVC NOT AVAILABLE – see Lesion Viral Isolation or Detection SDCL Ship refrigerated on wet ice. Contact Microbiologist on call at RGH Requisition for Special Pathogens (NML,Winnipeg) Ship TDG RG4 Ship centrifuged specimen refrigerated on wet ice. Contact Microbiologist on call at RGH Requisition for Special Pathogens (NML,Winnipeg) Ship TDG RG4 NOT AVAILABLE - see Lesion Viral Isolation or Detection Winnipeg – National Microbiology Lab VHF_P Winnipeg – National Microbiology Lab VHF_S Include specimen source, patient symptoms and date of onset on the requisition. SDCL SDCL Print Date: June 12, 2015 LESVC 105 Test Name Specimen Container Volume Specimen Requirements Reference Range *Viral Respiratory Virus Isolation or Detection (Adenovirus, Influenza A & B, Parainfluenza, Respiratory Syncytial Virus-RSV, Enterovirus) *Viral Stool Viral Isolation or Detection (Enterovirus, Coxsackie) NasoUniversal pharyngeal Transport Aspirate, Medium Washings (See Viral, Throat Virus Isolation or Detection.) Stool (Eastern Equine, Japanese Encephalitis) Walnut size (See Norovirus PCR). stool portion Testing Site LIS Code SDCL RESVC SDCL STLVC with no viral transport or preservative *Viral Throat Throat Virus Isolation swab or Detection (Adenovirus, Influenza A & B, Parainfluenza, Respiratory Syncytial Virus-RSV) *Viral Tissue Tissue Virus Isolation *Viral Urine Viral Isolation or Detection **Viral Acute Serology **Viral Convalescent Serology *Viral Meningitis Sterile stool container Units Urine Universal Transport Medium Universal Transport Medium Sterile Urine Container Blood CSF L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 NO LONGER AVAILABLE -STAT(Urgent) protocolPhone SDCL at (306)787-3131 to prearrange testing prior to shipping. 20 mL urine (See CMV Urine). (random) NOT AVAILABLE – order specific viral serology NOT AVAILABLE – order specific viral serology See Encephalitis (Viral). SDCL SDCL TISVC SDCL URVC SDCL SDCL Print Date: June 12, 2015 106 Test Name Specimen Container Volume Specimen Requirements Reference Range Viral Surveillance Blood 3 Blue tops 2 Red tops Require completion of consent and questionnaire Viscosity Blood 1 Red *Vitamin A Blood 1 Red *Vitamin B1 Blood 1 Mauve *Vitamin B2 Blood (Riboflavin) Patient must fast for 12-14 hr and refrain from alcohol for 24 hr before collection *Vitamin B3 *Vitamin B6 Blood (Pyridoxine) 1 GRN Vitamin B12 Vitamin B12 & Folates Vitamin C *Vitamin D1,25 Dihydroxy *Vitamin D2 Blood 2 mL serum Send within 3 hr of collection. Separate from cells ASAP. Freeze. 1 mL serum Protect from light by wrapping in tin foil. Freeze. Transport on ice packs within 24 hr. 4 mL whole Wrap in tin foil blood 1 mL Hep plasma Protect from light. Freeze 2 Mauve 3 mL plasma Not available Freeze. Wrap in tin foil within 5 min. of collection. 1 SST 1 mL serum 1.1-1.3 Deficient: <116 Borderline: 116-138 Normal: 138-781 Units cps pmol/L Testing Site LIS Code Transfusions RGH STVIR Hematology RGH VISCO SDCL - Toronto TAT = 2 weeks VITA SDCL - Mayo Clinic VITB SDCL - MAYO VITB2 SDCL - Toronto VITB6 Chemistry - RGH B12AX SDCL - Calgary TAT = 4 weeks VD125 SDCL VITD2 See B12 & folates Blood 1 RED Blood 1 SST L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 See Ascorbic Acid 2 mL serum Aliquot and freeze serum If specimen thaws it is unacceptable. 2 mL serum Aliquot and send separately with its own requisition Print Date: June 12, 2015 107 Test Name Specimen Container Volume *Vitamin D 25 (25Hydroxy Vit D3) Blood 1 SST *Vitamin D 25 Hy Blood 1 SST droxy *Vitamin D (Vitamin D3) Blood 1 SST *Vitamin E Blood 1 SST Blood 1 Green Vitamin K *VMA *Voriconazole **VZV *Water Deprivation Test WBC and Diff. Blood Lesion Specimen Requirements Reference Range Units Testing Site LIS Code 2 mL serum Aliquot and send separately with its own requisition 2 mL serum Aliquot and send separately with its own requisition SDCL-Chemistry TAT= 10 days VID25 SDCL TAT = 10days VD25 2 mL serum Aliquot and send separately with its own requisition 2 mL serum Protect from light by wrapping in tin foil. Aliquot and freeze. Not available. Replacement test is protime. See Vanillyl Mandelic Acid 1 mL Frozen plasma SDCL - Toronto VITD3 SDCL - Toronto TAT = 4 weeks VITE SDCL to Hospitals VORIC in Common,Toronto See Varicella Zoster. See Viral, Lesion. See ADH Blood 1 Mauve *West Nile Virus IgM Serology Blood 1 SST *West Nile Virus IgG Serology *West Nile Virus – Plasma PCR Blood 1 SST Blood 1 Mauve (only for immunocompromised/ encephalitis / meningitis patients) L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Whole Order CBC blood 2 mL serum Acute Initial test for diagnosis of suspect West Nile Virus. 2 mL serum Convalescent Hematology RGH SDCL WNVAS SDCL WNVCS 1 mL EDTA Separate ASAP and freeze plasma plasma. Ship on ice. Plasma must be received frozen. SDCL WNPCR Print Date: June 12, 2015 108 Test Name Specimen Container Volume Specimen Requirements Reference Range *West Nile Virus CSF West Nile Virus PCR CSF *WNV Blood CSF Freeze CSF ASAP. If specimen thaws, it is unsuitable for analysis. (For symptomatic or immunocompromised patients.) See West Nile Virus. Xylose Specimens include fasting, and 1hr after D-Xylose drink Xylose Fasting. D-Xylose drink to be given *Xylocaine (Lidocaine) Yersina Serology *Zarontin (Ethosuximide) *Zinc Blood 2 SST 5 mL serum Freeze serum Children at peak: >20 (0-10 yr) Adults: at least 1.67 should be reached after 2 hr Urine 5 hr collection after drink Adults: 21-31% excretion/5 hr Blood 1 Red 10 mL urine Collect urine for 5 hrs post dose, no preservative. Record volume. Freeze and send 10 mL. 3 mL serum Aliquot Blood 1 Red No longer available. 1 mL serum Aliquot Blood 3 mL 1 – 7 mL Royal Blue plasma 500 μL for EDTA) BD368381 neonates *Zinc Urine 24 hr or random urine container acidwashed Sterile leak 2 mL CSF proof tube. L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Units Testing Site SDCL mmol/L SDCL to Edmonton SDCL to Edmonton LIS Code WVPCR XYLO XDU SDCL LIDO SDCL ETHOL Separate plasma ASAP. Pour into polypropylene tube. Indicate on req. that specimen is sodium heparin plasma. SDCL - Toronto ZNS 10 mL urine Send in polypropylene aliquot container. Record on the req. the collection date, total 24 hr urine volume, if submitted, or random urine. SDCL - Toronto TAT = 3 weeks ZNU Print Date: June 12, 2015 109 Test Name Specimen Container Volume *Zinc Protoporphyrin Blood Recommend that lead be ordered simultaneously to detect lead exposure (may not be a good indicator of lead exposure in women and children) 1 – 7 mL 10 mL Royal Blue whole blood EDTA) BD368381 500 μL for neonates L:\LabProcedures\DeptLIS\LABLisOP8007T1.26 Specimen Requirements Reference Range Specimen must be analyzed within 5 days of collection. Suggest ordering LEAD Units Testing Site SDCL - Toronto TAT = 2 weeks Print Date: June 12, 2015 LIS Code ZPORP