Barney Graham - Sabin Vaccine Institute
advertisement

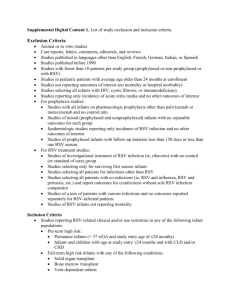
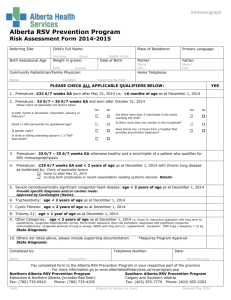
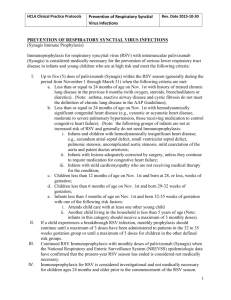
Novel RSV Vaccines Under Development Barney S. Graham, M.D., Ph.D. Achievements and Future Challenges in the Surveillance of Respiratory Viruses San Jose, Costa Rica January 30, 2013 Vaccine Research Center National Institute of Allergy and Infectious Diseases National Institutes of Health Department of Health and Human Services For more information: 1-866-833-LIFE vrc.nih.gov VRCforLIFE@mail.nih.gov RSV Genome Organization and Protein Functions le P NS1 NS2 N F M SH G M2-1 M2-2 L 3´ tr 15,222 nt total 0 2 4 8 6 10 plasma membrane 15 kb envelope spikes G (298) - attachment nonstructural NS1 (139) - inhibit Type I IFN induction NS2 (124) - inhibit Type I IFN signaling - activate PI3K and NF-B - inhibit apoptosis 150 nm nucleocapsid-associated regulatory M2-2 (90) - viral transcription - RNA replication N (391) - RNA-binding P (241) - phosphoprotein L (2165) - polymerase M2-1 (194) - transcription processivity factor - neutralization and protective antigen - antibody decoy (secreted G) - fractalkine mimic - TLR antagonist F (574) - fusion and entry - neutralization and protective antigen - TLR4 agonist SH (64) - putative viroporin - inhibits apoptosis inner envelope face M (256) - assembly 2 Disease Severity is Greatest in Children <2.5 Months of Age Boyce TG et al J Pediatr. 2000; 137:865 40 30 20 <=28 wk 29-<33 wk 10 33-<36 wk Low-risk Dec Nov Oct Sep Aug Jul Jun May Apr 0 Mar CHD (5%) BPD (3%) CHD Other disease Feb Low-risk (53%) BPD 50 Jan Prematurity (12%) RSV Hospitalizations per 100 Children 60 Other disease (23%) Month of Birth Biological challenges for vaccination • • • • • Relatively weak induction of cellular responses Reduced capacity for somatic mutation of antibody Presence of maternal antibody Frequent reinfection Legacy of vaccine-enhanced disease 3 Biological Factors Associated with Difficult Vaccine Targets • Infection is not easily controlled by natural immunity – – – • Alteration or evasion of host immune response – – • • • • • High frequency of severe disease (filoviruses) Persistent infection (HSV, HIV, HCV) Reinfection is common (RSV, HIV) Interference with innate and adaptive immunity Integration, sequestration, and immune sanctuaries Significant genetic variation or multiple serotypes Site of initial infection is major target organ for disease Animal models do no recapitulate pathogenesis of human disease Critical role for T cell-mediated immunity (HIV, HCV) Delay between infection and induction of cellular immunity (HCV) Graham & Walker in The Immune Response to Infection, 2011 4 Biological Factors Associated with Difficult Vaccine Targets • Infection is not easily controlled by natural immunity – – – • Alteration or evasion of host immune response – – • • • • • High frequency of severe disease (filoviruses) Persistent infection (HSV, HIV, HCV) Reinfection is common (RSV, HIV) Interference with innate and adaptive immunity Integration, sequestration, and immune sanctuaries Significant genetic variation or multiple serotypes Site of initial infection is major target organ for disease Animal models do no recapitulate pathogenesis of human disease Critical role for T cell-mediated immunity (HIV, HCV) Delay between infection and induction of cellular immunity (HCV) Graham & Walker in The Immune Response to Infection, 2011 5 Factors that Diminish Incentives for Industrial Vaccine Development • Concern about safety – RSV • Concern about achieving efficacy – HIV, RSV • Sporadic or biodefense threats without a dependable commercial market – Ebola/Marburg – New emerging viral diseases Graham et al. Clinical Pharmacology and Therapeutics 2009 6 Factors that Diminish Incentives for Industrial Vaccine Development • Concern about safety – RSV • Concern about achieving efficacy – HIV, RSV • Sporadic or biodefense threats without a dependable commercial market – Ebola/Marburg – New emerging viral diseases Graham et al. Clinical Pharmacology and Therapeutics 2009 7 Overview of RSV Vaccine Clinical Development No Efficacy – Serious Adverse Effects Formalin-inactivated alum-precipitated whole virus No Efficacy – Low/No Efficacy – Inappropriate No Immediate Immune Response Safety Concerns Subunit vaccine G protein – streptococcal conjugate Subunit vaccine F glycoprotein in alum in adults Various live attenuated RSV nasally in children Efficacy unknown – Currently in Clinical Testing Live attenuated RSV nasally in children rA2cp248/404/1030/ΔSH ΔM2-2 Efficacious None Post-fusion F Rosettes Live virus vaccine delivered IM in children BPIV-RSV live chimeric virus nasally 8 FI-RSV Vaccine-Enhanced Disease Vaccine n Infected (%) Hospitalized (%) Deaths FI- RSV 31 20 (65) 16 (80) 2 FI-PIV-1 40 21 (53) 1 (5) 0 Kim et al. Am J Epidemiol 1969;89:422 9 % Eosinophils in BAL Correlates of FI-RSV Vaccine-Enhanced Illness 45 40 35 30 25 20 15 10 5 0 FI-Vero Graham et al. JI 1993;151:2032 Tang et al. Vaccine 1997;15:597 FI-rRSV wt FI-rRSV FI-rRSV FI-r RSV GepDG DSH Johnson et al. J Virol 2004; 78:6024 Polack et al. J Exp Med 2002; 196:859 Properties to Avoid • Antibodies with poor NT activity → Immune complex deposition • CD4+ Th2-biased response → Allergic inflammation 10 Options for Vaccine Evaluation Platforms Live-attenuated • • RSV chimeric paramyxovirus vectors Gene-based vectors • • • Nucleic acid – DNA or RNA Replication defective Replication competent Subunit or particle-based • • • • • Purified protein Virus-like particle Virosome Nanoparticle Peptides Antigens Delivery Target Populations F Respiratory tract Neonate (<2 mo) G Parenteral Infants and children (>6 mo) SH Internal Multiple Other mucosal site • • Sero-negative Sero-positive Siblings and parents of neonates Young adult women • • Pregnant women Women of child-bearing age Elderly (>65 yr) Whole-inactivated RSV 11 11 Considerations for Immunizing RSV-Naïve Infants • Opportunity to prevent or delay first RSV infection – Reduced primary morbidity – Reduced childhood wheezing • Opportunity to establish future immune response patterns (antibody specificity and T cell phenotype) – Improved immunity against reinfection • Target age is critical – Peak age of hospitalization ~2.5 mo – ~50% of hospitalization occur >6 mo – If incidence is ~60% in first year, ~70% are RSV-naïve at 6 mo 12 12 Selecting Target Age for Initiating Vaccination <4 mo >6 mo Somatic mutation - ++ Dendritic cell and APC maturation - ++ Clearance of maternally-derived antibody - ++ No longer breast-feeding - + Idiosyncratic apnea and other rare adverse events + - Small airway size ++ - Relative Th2 bias ++ - Efficacy Safety 13 13 RSV Vaccine Pipeline Product Sanofi RSV vaccine BBG2na MEDI-559 MEDI-534 MEDI ΔM2-2 & others Novavax RSV Sendai-RSV chimera RSV vaccine NanoBio RSV MVA-BN RSV GenVec RSV Universal RSV RSV vac_Oka VEE-F RNA replicon Mymetics RSV TechnoVax SynGem RSV VLP Vac F protein RSV vaccine AMV601 / RespiVac PEV4 Epitope-scaffold SHe T4-214 TWi RSV vaccine Sponsor Sanofi Queen’s Univ Belfast MedImmune MedImmune NIAID +/- MedImmune Novavax St. Jude’s Merck/Nobilon Nanobio/Merck Bavarian Nordic GenVec Crucell/J&J Okairos Alphavax Novartis Mymetics Technovax Mucosis LigoCyte Novartis GSK AmVac Pevion U. Wash/ TSRI) Ghent/Immunovaccine TI Pharma TWi Biotech Type of Vaccine Subunit Subunit Live-attenuated Live chimeric Live-attenuated Nanoparticle Live chimeric Single-cycle Inactivated Vector Vector Vector Vector Vector Vector-RNA VLP-Virosome VLP VLP-lactococcus VLP Subunit Subunit Subunit Subunit Epitope-scaffold Subunit Target Antigen F, G, M protein G Whole virus F Protein Whole virus F Protein F Whole virus Whole virus Subunit F Subunit F-N-M2-1 F F Multiple Multiple F F F F F F epitope SH Sources: Company Website, Fierce Vaccines, RSV 2012 Symposium, Clinicaltrials.gov Target population Elderly patients n/a Infants and children Infants Adults, infants and children n/a n/a n/a n/a Adult high risk patients Children and infants Infants and elderly n/a n/a n/a Elderly patients n/a n/a n/a n/a Pediatric n/a n/a Pediatric and at-risk adults n/a n/a n/a Phase Phase II Phase II Phase I-IIa Phase I-IIa Phase I Phase I Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical Pre-clinical 14 Comparing Product Concepts Based on Immunological Concepts Native F or G MHC pathway CD8 T cell induction IL-4 Delivery route Replication competence - II - ++ IM - ++/- II - +/- IM - ++ II +/- I +/- -/+ IM - ++ I & II ++ - IM or nasal - or + ++ I & II + - IM - Recombinant, or chimeric viruses ++ I & II + - nasal + WT or attenuated virus ++ I & II + - nasal or IM + Whole-inactivated virus Protein subunits VLPs or virosomes Vectors Naked DNA or RNA 15 Passive Prophylaxis with Synagis •Humanized mouse monoclonal antibody •Monthly injections reduce hospitalizations by 50% •Licensed for select high-risk infants •Demonstrates neutralizing antibodies against the F glycoprotein are protective Shane Storey, Nat Rev Drug Discovery (2010) 9, 15-16 16 Vaccine Antigen Selection: Rationale for Choosing F Reasons for choosing F: • Target of Synagis • Higher sequence conservation than G • Unlike G, F is absolutely required for virus entry Target cell cytoplasm Receptor Prefusion Postfusion Prehairpin Delivery of nucleocapsid and genome 17 Organization of RSV F Glycoprotein F2 * 27 F1 70 116 126 500 FP HR1 1 21 * 37 69 * HR2 TM 212 Unique to RSV 313 322 333 343 358 367 382 393 416 422 439 • Signal peptide Fusion peptide Heptad repeat Transmembrane domain Cysteine Disulfide bond N-linked glycosylation • 574 Type I integral membrane protein essential for RSV entry and cell-to-cell fusion Primary target for neutralizing antibody. • • • pH-independent class I viral fusion protein Multiple furin cleavage sites Two heptad repeat regions that form an antiparallel six-helix bundle in post-fusion state. • F1 has a cysteine-rich domain. C-linked palmitylation Known or potential furin cleavage site 550 Neutralizing antibody epitope Infection inhibiting peptide 18 New Technologies Have Made an RSV Vaccine Possible Viral Vaccines Major Conceptual and Technological Advances Cell Molecular Potential areas for new culture biology technical advances Discovery of immunity 16 RSV ? HPV Rotavirus 14 Varicella Japanese 12 encephalitis Hepatitis A 10 Hepatitis B Rubella 8 Mumps Adenovirus 6 Measles Poliovirus 4 Influenza Yellow fever 2 Rabies Smallpox Animal Models B & T cell biology Delivery devices Genomics Glycobiology Informatics Manufacturing Nanobiology Proteomics Structural Biology Vector biology 0 1800 1820 1840 1860 1880 1900 1920 1940 1960 1980 2000 2020 2040 2060 2080 19 Summary • There is a robust pipeline of candidate RSV vaccines and antigen design is being facilitated by atomic structure • We need RSV-devoted NGO involvement for advocacy, advancing candidates, and coordination of public-private partnerships • Developing clinical trial infrastructure through North-South partnerships would facilitate clinical development • The regulatory process will be facilitated if we avoid generic terms for new vaccine platforms and describe them by immunological and biophysical properties • For RSV-naïve infants it may be best to achieve licensure first in children >6 mo of age – Expand safety database – Perform studies to evaluate herd (neonatal) immunity – Develop mathematical transmission models to refine timing and schedule for vaccination – Consider passive-active approaches 20 Viral Pathogenesis Laboratory Sung-Han Kim, Syed Moin, Barney Graham, Kaitlyn Morabito, Azad Kumar, Kevin Graepel, Kayvon Modjarrad, Man Chen, Tracy Ruckwardt, Allison Malloy, Jason McLellan, Jie Liu, Erez Bar-Haim 21 Questions 22