Cytotoxic and Biotherapies Credentialing Programme
advertisement

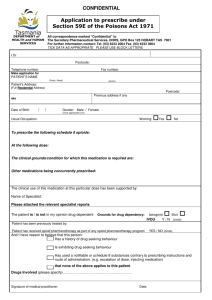
Cytotoxic and Biotherapies Credentialing Programme ‐ Module 5 1. 2. 3. 4. Drug Dose Determination Drug Calculations Role of the Second Checker The Checking Process At the completion of this module the RN will • Discuss the importance of the role of the second checker • Demonstrate how drug doses are determined • Demonstrate checking prescriptions using calculations • Pass the drug calculations test REFERENCES Christchurch Hospital Department of Nursing. (2008, June). Volume 12, Fluid & Medication Manual. Retrieved from CDHB Intranet. Ref 1372 American Pharmacists Association. (2005). Drug Information Handbook for Oncology. Pittsburgh, PA: Lexi Comp Inc. Polovich, M., White, J., Kelleher, L. (Eds.). (2005). Chemotherapy and Biotherapy Guidelines and Recommendations for Practice. Pittsburgh: Oncology Nursing Society. Drug Dose Determination ________________________________________________________________ The combination and dosing of the drugs is determined by clinical trials undertaken on different disease types, using single drug or combination drug regimens with varying doses to ascertain a sensitivity of the disease to the trial combination being undertaken. The majority of patients receive standard dose therapy worked out from these large and extensive clinical trials which are undertaken. High dose treatment is given for diseases such as acute leukaemias, lymphomas and bone marrow transplants. The aim is to eradicate the disease but this type of treatment can have severe and even lethal associated side effects and toxicities. Supportive or chemoprotectant agents are utilised in these regimens. In determining the dose for any regimen the person’s current height, weight, blood test results and age are considered. Other considerations will include • Co‐morbidities • Performance status • Obesity/cachexia • Liver/renal/cardiac function • Drug interactions • Children/elderly Variances in the calculated doses may occur due to consideration of some of these factors. However any variance should always be double checked with the prescriber before proceeding with administration. Variances of +/‐ 5% are usually allowable. It is not uncommon for dose adjustments to be made at the initiation or throughout treatment with due consideration given to the above factors or how the patient is currently tolerating treatment in terms of toxicity levels. It is much more common for dose reduction to occur than a dose increase. Most BSA calculations are done using actual body weight but some clinicians choose to use ideal body weight or lean body weight for those who may be obese to potentially decrease toxicity levels. Drug Calculations ________________________________________________________ Prior to administration it is necessary that you confirm the drug, dose schedule and rate of administration. Chemotherapy drugs are usually dosed according to the patient’s body surface area (BSA). The BSA can be calculated in two ways; using a formula as below or a nomogram. Nursing staff should always use the formula Height x Weight 3600 = BSA (m2) Other methods of calculating drugs Some drugs require a different method of calculating the correct dose. Review these carefully as you will be expected to be familiar with them. Area under the curve (AUC) AUC is a method that is used to calculate the dose of Carboplatin. It is calculated by: Carboplatin (mg) = desired AUC x (25 + GFR) where GFR is the creatinine clearance (measured or estimated) Creatinine Clearance using the Cockcroft & Gault method Estimated creatinine clearance (Cl cr) (ml/min): (140‐age) x BW (kg) Males = 72 x Scr Females = male x 0.85 MG / KG dosing Some drugs are prescribed using a mg per kg schedule. This is more common in paediatric oncology and biotherapy administration. Now complete the workbook section ‐ drug calculations test A 100% pass in the drug calculations test is required. Once this has been achieved you are able to be a second checker. Role of the Second Checker ___________________________________________________ To ensure an incident‐free procedure, the role of the second checker is as important as the role of the person actually preparing and administering the fluids and medications. The second checker acts as the final checking point for checking the • right fluid/medication • right dose • right patient • right route • right time • right rate The second checker must be involved in all stages of preparation and administration including • separate calculations of each drug • the drawing up of the medication • the check at the bedside • device review • the administration • checking the rate of infusion with the administrator The second checker must document on the appropriate chart that they have undertaken the second check. Remember, the notes are a legal document so the second checker’s signature is evidence that the check was done. If the second checker has any concerns during the checking procedure, these must be raised with the administrator and assistance sought by consulting with senior nursing staff and/or medical staff and by using resource material. The nurse is the last check before the patient receives the medication. The correct checking process must be undertaken at all times. Pre‐administration Process ________________________________________________________________ This guide should be followed prior to administration of the drugs. 1. Ensure the patient has had appropriate education on administration and possible side effects. 2. Ensure patient has given written consent. 3. Check blood counts and other results and ensure they fall within acceptable range for the treatment being given. 4. Establish patent venous access with blood return 5. 6. 7. 8. Review previous cycle of chemotherapy with the patient. Administer antiemetics as prescribed. Ensure a spill kit is available and the nurse knows how to clean up a spill. Each nurse should ensure they are familiar with the characteristics and side effects of each drug including whether they are an irritant or a vesicant. 9. Take any refrigerated chemotherapy out of the fridge an hour prior to administration. 10. Prime any IV lines with normal saline and label with a cytotoxic label. 11. Don personal protective equipment (PPE). Goggles are optional but should be considered if risk of splashing to the eyes. 12. Remove cytotoxic drugs from the container and put in a foil dish and placed on a plastic backed sheet on the trolley. All syringes and infusion bags should be checked for any leakage or contamination. 13. Two nurses, both of whom are entered on the cytotoxic database carry out the cytotoxic checking procedure 14. Prescription chart needs to be checked for appropriate medical practitioner’s signature, date and that blood parameters and other investigations are recorded and within an acceptable range. 15. Check labels on syringe/ infusion against the prescription. These are to include drug dose, route of administration and expiry, diluents and storage details. 16. Prescribed dosages should be checked against body surface area (BSA) or other method. 17. Check labels on outer bag of the syringe/infusion bag against the patient’s full name, hospital number & date of birth. 18. Check the medication details on the syringe/infusion bag against the prescription. 19. The patient’s name on the prescription and medication must then be checked with the patient. 20. Both nurses have the responsibility to complete the documentation required for the checking and administration of the cytotoxic drugs 21. Document administration in the clinical notes