From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
Human
Blood
Basophils
Activation
By Christoph
Stain,
Display
a Unique
Linked
Membrane
Hannes
Stockinger,
Klaus
To
evaluate
phils
a
the
membrane
panel
(MoAbs,
of
n
60)
=
was
(CD1
7),
7 (CD1
wt
(particularly
1 , CD1
(CD1
40
8).
MoAbs
3),
anti-gp
67
MoAb
CIKM5,
indicating
Under
express
least
detectable
on
defined
by
by
OKT-1
the
2 (IL
(anti-TAC,
lL2Rl,
CD9
2)
MoAb
(mol
the
myeloid
the
and
the
three
not
stained
MoAb
63D3
(VIM-i
results
p24
structure
determinants
for
MoAbs
In contrast
to neutrophils
membrane
antigens
detail.8”
peripheral
restricted
and
and
has
eosinophils,
the
not
been
and
eosinophils
(MNC)
preparations,
cells in MNC
analyses
remain
cannot
unless
in
of
expression
of
investigated
This is due to the small amount
of basophils
blood and to the fact that basophils,
which
neutrophils
in
in the
unlike
mononuclear
cell
be distinguished
from
additional
cytochemical
other
stain-
ing procedures
are performed.
Using a combined
cytochemical (toluidine)
and immunologic
(monocbonal
antibodies,
MoAbs)
staining
procedure,
we were
able to analyze
the
antigenic
membrane
From
the
University
profile
I. Medical
of
of this
Department
Vienna,
January
Supported
by the
8. 1987:
Kamillo
accepted
Eisner
the “Max-Kellner-Stipendium
Fakult#{228}t der
Address
na,
of Immunology.
of
6, 1987.
(Switzerland),
and
der
by
Medizin-
Wien.
requests
University
August
Stiftung
des Krebsausschusses
“
Universitat
reprint
Department,
Institute
Austria.
Submitted
ischen
cell type.
and
to
Peter
Vienna,
Bettelheim,
MD.
Lazarettgasse
I. Medical
14. A-1090
Vien-
Austria.
The
charge
publication
payment.
“advertisement”
indicate
© I 987
costs
ofthis
article
This
article
must
in
accordance
by Grune
if Stratton.
0006-4971/87/7006-0026$3.00/O
1872
with
this fact.
lnc.
were
defrayed
therefore
/8
U.S.C.
be
kd)
the
and
the
possibly
CD14
obtained
patients
a unique
the
by the
antibod-
monocyte-specific
In summary,
generate
against
monocyte/granulo-
by the
freshly
(CGL)
analyses.
directed
of neutrophils,
strucfrom
yielded
these
combination
represent
an
chronic
identical
data
of
indicate
surface
activated
cell
population.
a
to the identification
biochemical
activities.27
hitherto
defining
basophils
and
6 MoAbs
on
Basophils
1987
by Grune
& Stratton,
Inc.
short-term
UMAN
BASOPI-IILS
represent
a distinct
minority
of
peripheral
blood
cells with a prevalence
of 0.5% of
total
leukocytes.’
Mature
basophibic
cells have
to be distinctly
differentiated
from
neutrophils
and eosinophils
in
terms
of their physiologic
robe. So far, evidence
of basophil
was mostly
characteristics
2)
expressed
treatment.
70
antigen,
leukemia
basophils
to
the
neutrophilic/eosinophilic
recognizing
Enriched
H
differentiation
morphological
Mo
in FACS
that
50
p 200
3,
p 55.
wt
cell
display
is
at all by CD1
(CD12)
granulocytic
receptor
The
mononuclear
fractions
neuraminidase
(mol
cyte-associated
in
purified
antigens.
after
Fc y-receptor
structure
under
T4
both
as
only
p45
different
Moreover.
and
basophils
and
3-fucosyl-N-acetyllactosamine
ture
not
G#{246}ssinger,
basophils
ies
basophils,
surprisingly
the
VIP-2b.
by
MY
J#{227}ger,Heinz
structure
were
2 and
structures
BA-2,
2).
family
mature
ie,
recognized
anti-IL
LFA-1
basophils
0 and
HLA-DR
with
other
neutrophils,
toluidine/
E 1 1 , and
reactive
to
conditions
suspension
Fcy-receptor
activation-linked
mature
interleukin
were
Ulrich
Including
Bettelheim
(MNC)
MCS
1 MoAb
conditions,
three
MoAbs
identified
9, anti
relationship
normal
at
MY
Peter
culture
lactosylceramide
MoAbs
anti-CR
VIM-2)
a close
cells.
MoAb
baso-
Myeloid-assothe
against
1 50
and
antibodies
combined
against
(gp)
kd)
of human
procedure.
directed
MoAb
a
MoAbs
anti-glycoprotein
antiglycolipid
for
staining
MoAbs
profile
monoclonal
used
immunofluorescence
ciated
marker
well-established
Scharf,
Michael
Lechner,
Phenotype
Structures
in part
hereby
§1734
by page
marked
solely
to
MATERIALS
Cell
AND
METHODS
Preparation
MNC were isolated by gradient
centrifugation
on Ficoll-Hypaque
(Pharmacia,
Uppsala,
Sweden)
and were then subjected
to staining
with MoAbs.
Neutrophils
obtained
from healthy
controls
(n - 3)
were prepared
by standard
techniques
as previously
described.’2
Eosinophils
were isolated from two patients
with hypereosinophilia
and from two patients suffering
from transient
drug allergy. Purity
of these cell fractions
was >90%.
MoAbs
The MoAbs used in this study and referred
to as belonging
to a
cluster of differentiation
(CD) or for being reactive
with a welldefined structure
were: Leu I (CD5), Leu 2a (CD8), Leu 3a (CD4),
Leu 4 (CD3),
Leu 7 [human
natural
killer (NK) cells], Leu 1 la
(CD16),
and anti-HLA-DR
(Becton
Dickinson,
Sunnyvale,
CA);
MY 7 (CD513),
MY 9 (anti-p67),
Mo 2 (CD514),
14 (CD4), 18
(CD8), 11 1 (CD2), B1 (CD2O),
B2 (CD21),
B4 (CD19),
and IL 2
RI (CD25)
(Coulter
Immunology,
Hialeah,
FL); BA-l (CD24),
and BA-2 (CD9) (Hybritech,
San Diego); OKT-l
(CD5), OKT-9
(antitransferrin
receptor),
OKI-lO
(p45), 0KM-I
(CDI I), and
OKB-2 (CD24)
(Ortho Pharmaceuticals,
Raritan,
NJ); and 63D3
(CD5I2)
(BRL; Gaithersburg,
MD); anti-Il 2 (Eurogenetics,
Agoralaan,
Belgium);
BMA-022
(HLA-DR)
and BMA-0l
1 1 (PanTERFC receptor)
(Behringwerke
AG, Marburg,
FRG).
The MoAbs VIP-I (antitransferrin
receptor),’3
VIP-2b
(p45),’3
VID- 1 (anti-HLA-DR),’4
VIL-Al
(CDIO),’5
VIM- I 2 (CD1 1 ),“
VIM-l3
(CD514),”
VIM-D5
(CD15),’2
VIM-2
(not clustered),’7
VIM-C6
(CD15),’8
VIB-C5
(CD24),’9
VIT-3b
(CD3),#{176}VII-4
(CD4),’9 VII-6 (CDI),2’
VII-8 (CD8),’9 VII-l2
(CD6),’9 ViFcR2
(CD16),
and VIE-G4
(anti-glycophorin
A)22 were produced
at the
Institute
of Immunology,
University
of Vienna. The MoAb Na 1/34
(CDI)
was kindly provided
by Dr A. J. McMichael.
WT-l (CD7)
antibody
was sent by Dr W. I. M. Tax, and MCS-2
(CD513)
antibody
was donated
by Dr J. Minowada.
VEP-13
(CD16)
was
supplied
by Dr Rumpold
(Vienna).
Anti-IAC
(CD25)
was kindly
Blood,
Vol 70,
No 6 (December),
1987:
pp 1872-1879
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
THE BASOPHIL
PHENOTYPE
1873
provided
by Dr T. A. Waldmann.
CLBery3
was sent by P. 1.
Tetteroo.
MoAbs L4F3, IGIO (CDI5),
KiM5 (CDII),
T5A7 and
(G)035 (CDI7),TSI/18.I
I and MHM 23 (CD518, LFA-I-/3-chain;
McMichael,
personal communication,
1984, 1986), CIKM5
(40 kd
Fc’y-receptor)
were selected
from the myeloid panel of the Second
International
Workshop
on Human Leukocyte
Differentiation
Antigens. MoAb E I I (anti-CR
I receptor)
was taken from the myeloid
panel of the Third International
Workshop
on Human
Leukocyte
Differentiation
Antigens.
Supernatant
from the IgE-producing
human
myeboma
cell line
U-266 and a mouse anti-human
IgE MoAb (E124 2-8, Immunotech,
Marseille,
France)
was used for detection
of membrane-bound
IgE
(positive
control).
Monoclonal
antibodies
of either IgG 1, IgG 2a,
lgG 2b, and 1gM subclass
with irrelevant
specificity
were used as
negative controls.
Immunologic
Characterization
With
MoAbs
As previously
described,’2
the binding of the various antibodies
to
isolated
MNCs was assessed
by indirect
immunofluorescence
with
fluoresceinated
goat F(ab’)2 anti-mouse
IgG and 1gM antibodies.
Fluorescence
of MNCs was evaluated
by means of a Leitz Ortholux
microscope
(Leitz,
Wetzlar,
FRG).
Purified
basophils
of CGL
patients
and enriched
neutrophils
of one healthy
donor were analyzed with a FACS 440 (Becton Dickinson).
Combined
Immunologic/Toluidine
Staining
Procedure
Blood samples
from 15 volunteers
were drawn
for testing
the
entire panel three times. After the indirect
immunofluorescence
staining
procedure,
cells (6 x l0 for each MoAb)
were fixed in
glutaraldehyde
at room temperature
(RT) for I minute
(0.025%
glutaraldehyde
in fixation buffer: 0.1 mol/L
Iris buffer in I vol%
glucose,
pH 7.8). After three washings
with phosphate-buffered
saline (PBS, pH 7.2) cells were incubated
with toluidine
blue
(Sigma, St Louis) (0.0125%
wt/vol in PBS) at RI for 15 minutes.
Subsequently,
cells were washed three times in PBS and subjected
to
analysis
as follows: Toluidine-stained
cells were first identified
in
bright field and then examined
for antibody
binding under fluorescence light.
The antibodies
we used either stained practically
all cells exammed or did not stain basophils
at all. For FACS analyses,
a reactivity
of >20% was considered
positive.
Neuraminidase
Treatment
of
Cells
MNCs
(4 x l06/mL)
were incubated
with
Vibrio
cholerae
neuraminidase
0.2 U/mL
(Behringwerke
AG) in a shaking
water
bath at 37#{176}C
for 30 minutes.
The reaction
was terminated
by
washing the mixture
three times with RPMI 1640 medium supplemented with 10% fetal calfserum
(FCS).
Enrichment
of Basophils
To compare
the phenotype
of normal basophils
with that of CGL
patients
(two patients
in stable
phase,
one patient
in accelerated
phase), the combined
immunofluorescence
technique
and an analysis of enriched
basophils
was used. Enrichment
of basophils
was
achieved
by incubating
MNC with a mixture
of antibodies
and
subsequent
rabbit complement
lysis. After informed
consent
was
obtained
from each patient,
heparinized
peripheral
blood of three
CGL patients (5%, 1 1%, and I 5% basophils,
respectively)
underwent
MNC isolation as described
above; 5 x 10 cells were incubated
with
1 mL RPMI
at 4#{176}C
for 45 minutes,
the milliliter
of RPMI
containing
100 tg of MoAB VIM-D5.
After being washed,
cells
were exposed to 5 mL rabbit complement
(Behringwerke
AG) at
Fig 1 .
Purified
ment lysis.
CGL
basophils
obtained
by MoAb
comple-
+
37#{176}C
for 90 minutes.
Monocyte
depletion
of washed
cells was
achieved
with scrubbed
nylon wool (37#{176}C
for 45’). Cells were then
incubated
with a mixture of antibodies
consisting
of 25 zg VIT-3, 25
Mg VIB-C5,
anti-HLA-DR,
25
zg Leu
CLBery3
1, 50 ig Leu 7, 25 tg VIE-G4,
25 g
(ascites,
1:500 diluted),
25 og VIM-D5
at
4#{176}C
for 45 minutes,
and subsequently
incubated
with 4 mL rabbit
complement
at 37#{176}C
for 90 minutes. Cells were again centrifuged
on
Ficoll-Hypaque
and washed twice. Cytospin
preparation
of this cell
fraction revealed >95% basophils
(Fig I).
Culture
Studies
Activation
of
neutrophils
and
basophils
by formyl-methionyl-
As reported
previously,23
PMNs
(I x 107/mL) or MNCs (1 x 107/mL)
were incubated
at 37#{176}C
for
10 minutes,
the medium
(RPMI
1640, 5 g/L human albumin,
pH
7.2) containing
I zmol/L
fMLP and cytochalasin
B 10 .og/mL as
well as dimethylsulfoxide
(DMSO)
(final concentration
0.01%) as a
solvent. The reactivity
of stimulated
MNCs was evaluated
by means
of the combined
immunofluorescence/toluidine
staining procedure.
leucyl-phenylalanine
Activation
suspension)
(JMLP).
of
with
basophils
the
incubated
with the
37#{176}C
for 30 minutes.
was evident.
from
two
healthy
donors
(in
MNC
Cells (I x l0) were
Ca-ionophore
A23187
(I i.og/mL, Sigma)
at
After this procedure
degranulation
of basophils
Ca-ionophore
A23187.
Short-term
cultures
with biologic
factors.
Basophils
were cultured either in MNC suspension
(five healthy controls)
or as purified
fractions
(CGL
basophils
from two patients)
after lysis with a
mixture
of antibodies
(>95%
purity
as determined
by Wright
staining
of cytospin
preparations)
for 5 days in RPMI
1640 (Flow
Laboratories,
McLean,
VA) plus 10% FCS, supplemented
with
either 20 U/mL human recombinant
IL 2 (Boehringer
Mannheim),
100 U/mL human recombinant
-y-interferon
(hr--y-IFN,
Interferon
Sciences,
New Brunswick,
NJ), supernatant
of the HTB-9 cell line24
(9:1
vol/vol),
or
supernatant
of
the
I
cell
hybridoma
producing
basophil-like
promoting
activity
factor (BaPA,
4:1 vol/vol)
kindly
provided
by Dr B. Stadler.2526
Phenotyping
(normal
basophils
in
MNC fractions: combined
toluidine
immunofluorescence
technique;
purified
CGL basophils:
FACS
analyses)
of cultured
cells was
performed
on days 0, 2, and 5.
3H-incorporation.
Incorporation
of 3H-thymidine
was carried
out as described
previously.27
In brief, purified basophils
from two
CGL patients
(l0 cells/well)
were incubated
with factor-conditioned media (‘y-IFN, BaPA, HTB-9-supernatant,
and IL 2) at 37#{176}C
for up to 5 days in a humidified
atmosphere
with 5% CO2. One
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
1874
STAIN
microcurie
per well 3H-thymidine
(New England
Nuclear)
was
added 12 hours before harvest.
The incorporated
radioactivity
was
collected
on glass-fiber
filters and counted
in a liquid scintillation
counter.
Values
are given as cpm x l0
± SD of triplicate
cultures.
Enrichment
ofneutrophils
by MoAb
+ complement
lysis.
Heparinized
blood drawn from a normal donor was first centrifuged
on
Ficoll-Hypaque.
The sedimented
cell pellet containing
erythrocytes,
neutrophils,
and residual
MNCs,
subsequently
underwent
dextran
sedimentation.
Neutrophils
(I x 10) obtained
by this method were
incubated
with a mixture
of MoAbs comprising
25 zg anti-HLADR. 25 ig BMAOII1,
25 ig B!, 25 g V1M-I3,
and CLBery3
(ascites,
1:500 diluted)
at 4#{176}C
for 45 minutes.
Cells were then
exposed to 1 mL rabbit complement
at 37#{176}C
for 90 minutes.
After
two washings,
cytospin examination
revealed >95% neutrophils.
basophils
granules.
of a toluidine
staining
procedure
are easily
identified
by
This procedure,
combined
phils
application
of
determination
the
immunofluorescence
of the
basophil
marker
profile
(Fig
p 67
Of all MoAbs
tested
in this
MoAbs
(CD17)
showed
the
basophils
(Fig 2A and B). MoAbs
membrane
determinant
and,
with
neutrophils
as well.
to eosinophils
and/or
In contrast
in
our
bound
hands,
gave
neutrophils,
a
to basovery
weak
the structure
3-fucosyl-N-acetyllactosamine
tered
as CD1 5) and the
nized by CDI6
MoAbs)
(identified
by MoAbs
clus50- to 70-kd
Fcy-receptor
(recogwere not detectable
on the surface
membrane
of circulating
anti-monocyte-associated
basophils.
MoAbs
with basophibs.
We furthermore
tested
CD512
and CD514
also failed
to react
nonmyeboid-associated
clusters
CD1-lO,
19 through
against
the
antigen
TlO
The
tested
21,
and
24,
an
MoAbs
25,
MoAbs
antitransferrin
of
directed
receptor
MoAb.
A constant
and reproducible
finding
was the reactivity of various
activation-linked
markers
with basophils.
All
cytoplasmic
simultaneous
technique
the
structure.
moderately
reactivity
in suspension,
their
purple
with the
a glycolipid
antilactosylceramide
reactivity
with
detecting
RESULTS
By means
recognizes
study,
strongest
ET AL
allowed
three
T1O
2A
positive
and
anti-IL
MoAbs,
(CD25)
MoAb
tested,
both
BA-2
(CD9)
and
A panel of 60 MoAbs
was used to delineate
the phenotype
of basophils
from that of neutrophils
and eosinophibs.
Thirty
MoAbs
reacted
with at least one type of mature
granulocytes
structures,
MoAbs
were
directed
cyte-associated
structures
21, 24, anti-human
NK
(CD I through
8, 10, 19 through
cell MoAb
Leu7)
failed
to stain
and showed
a homogeneous
staining
samples
tested.
Table
1 shows
basophils.
MoAbs
giving
positive
basophils
at all. They included
anti-common
acute
lymphocytic leukemia
(cALLA)
MoAb
VIL-Al
(CDIO)
and CD24
MoAbs
known
to bind to neutrophils.
common
bar,
MoAbs,
and
anti-gp
granubocytic
anti-CRI
membrane
MoAbs
(220
anti-C3bi-receptor
Ki M5/CD
I 50
structures
kd),
antibodies
(CD,.
Fig 2.
I 3),
chain
and
(40
(0KMMoAb
(A and B) Reactivity
kd)
1 , VIM-
MoAbs
Neuraminidase
12,
(CD518),
VIM-2,
of the
recep-
not detectable
on
against
lympho-
in particu-
anti-Fcy-receptor
1 1), anti-LFA-l-fl
MoAbs
were,
the transferrin
antigave
antigens
for positive
subsets
in all
that
20 MoAbs
stained
results
and
identifying
HLA-DR
MoAbs
anti-p24
tor, also activation-linked
freshly
obtained
basophils.
B).
results.
2 receptor
and the
MoAb
Seven
VIP-I,
which
T5A7
with
Treatment
of MNCs
MoAbs
(VIM-D5,
BA-2,
T5A7,
VEP-13,
VID-I,
and
anti-TAC)
were
tested
after
neuraminidase
toluidine-stained
peripheral
blood
basophils.
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
THE
BASOPH)L
PHENOTYPE
1875
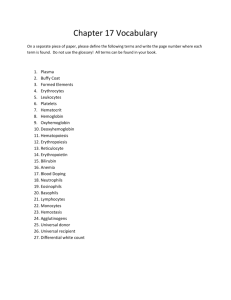
Table
1 . Reactivity
Pattern
MoAbs Reactive With
Peripheral
Blood Granulocytes
0KM-i
VIM-i2
of MoAbs
Bindi ng to Mature
WHO-Cluster!
Reactive Structure
KIM5
Granulocytes
Basophils
Neutrophils
Eosinophils
CD11/CR3
+
CD513/plSO
+
+
+
CD5i8/LFAi9-chain
+
+
+
Eli
p220/CR1
+
+
+
CIKM5
40-kd
+
+
VIM-2
NK
MCS2
MY7
TSI/i8.
11
MHM
T5A7t
23
(G)035t
Fc
y-receptor
++
+
+
+++
+++
+ +
+
p67
+
±
CD15/3-FAL
-
CD24
-
+
+
VIL-Ai
CD lO/cALLA
-
+
-
63D3
CD12
-
+
MY9
CD17/lactosylcer
+
L4F3
VIM-D5
VIM-C6
VIB-C5
1G1O
BA-i
VEP- 13
Leu
OKB-2
1 1a
ViFcR2
CD 1 6/50-
to 70-kd-Fc’y-
+
-
+ +
+
-
-
+
+
-
+
-
receptor
OKT-lO
VIP-2b
a-TAC
p45/T10
IL 2R 1
a-IL
2
CD25/IL
BA-2
2 receptor
CD9/p24
+
-
+
-
+
+
-
+
-
+
NK, not known.
Each
antigranulocytic
tReactive
with
treatment
MoAb
eosinophils
of
cells.
showed
When
normally
with this
tested
same
both
before
the
and
Purification
after
and
for
with
pattern
neuraminidase
positive
neuraminidase
VIM-D5
(anti-3-FAL)
very MoAb.
All other
reactivity
Phenotypic
staining
subsets
in all samples
bound
neutrophils
to a lower
extent
after
this
With regard
to basophils,
no change
of fluorescence
negaMoAbs
with
was
basophils
treatment.
Analysis
oJCGL
evident
with
Effect
of
After
MoAb
(Fig
>95%
plus complement
I ). Purified
cells
nofluorescence
staining
with
MoAbs
and were
evaluated
by FACS
Identical
results
were obtained
on day
0. These
obtained
toluidine
Analysis
phenotype
defined.
may
cause
a
therefore
of
an alteration
were
FACS.
use
of
has
the
preparations,
ionophore
A23
the
MoAb
already
a panel
of MoAbs
with
phenotype
results
combined
of
been
+ complement
structures,
The
the
the
purified
and
neutrophils
well
lysis
neu-
measured
appeared
to
remain
unchanged
by this procedure
and was identical
to the
neutrophil
reactivity
pattern
obtained
by indirect
immunofluorescence
microscopy
(data not given).
unchanged
JMLP
Studies
effect
and
neutrophils.
The
binding
of MoAbs
(VIM-D5/CD15,
T5A7/CD517,
VID- 1/H LA-DR.
VIP-l/transferrin
receptor,
BA-2/CD9,
and
anti-
TAC/IL
2 receptor)
was tested
before
and
activation
of basophils
and neutrophils
(two
trols).
Neutrophils
displayed
a distinct
increase
after
fMLP
healthy
conof the fluo-
rescence
intensity
with
MoAb
VIM-D5,
whereas
T5A7
on
reactivity
(same
basophils.
were
of
MoAbs
When
exposed
the
were
to the
MoAbs
tested
in factor-conditioned
basophils
still was
by morphological
Trypan
a viability
blue
staining
revealed
cells. FACS
analyses
patients
were performed
anti-TAC,
already
increased
on days
addition
of biologic
is given
detectable
2 and
on
5 and
factors.
in Fig
and 5. All three
identified
on cells
comparison
3C.
samples,
surface
in the
of the
media
of at least
not
98%
cells,
dependent
example
The
of
of this
LILA-DR
and
obtained
0, became
T4,
T4 antigens,
from healthy
donors
detectable
on days 2
anti-HLA-DR,
were
also
2 shows
a
and
T4
is shown
reac-
in the control
medium
(as
on days 0, 2, and 5). The
stronger
on BaPA
and
y-
reactivity
Leu
the
reactivity
basophils
than on those in the other
and the control
medium,
respectively
a moderate
was
on
structures
in question
control
medium.
Table
anti-TAC,
(VIT-4,
which
me>95%
in
criteria).
unstimulated
was
An
basophils
cultured
by FACS
analyses
of HLA-DR
was
Moreover,
antibodies
listed
of basophils
obtained
from two CGL
on days 0, 2, and 5. The reactivity
of
expressed
neither
on basophils
nor on CGL basophils
on day
tivities
of
determined
expression
Ca-
studied
as are
CGL
basophils
cultured
dia.
Purity
of 5-day-cultured
all samples
tested
(as determined
3D).
on basophils
23/87
experiment).
IFN-stimulated
conditioned
Culture
I 87,
procedure.
intensity
tested.
A
in MNC
pattern
of surface
stained
and B).
patients
Neutrophils
neutrophils
whether
significance
confirmed
by
ofPurified
To examine
trophils
on
data
of major
analyses
(Fig
3A
with all three CGL
with
normal
basophils
staining
procedure.
Phenotypic
The
FACS
lysis, purity
of basophils
underwent
indirect
immu-
MoAb
basophils,
remained
Basophils
any
Ca-ionophore
in the fMLP
was
tested.
syndrome.
pretreated
basophils,
which
are
tive, reacted
strongly
displayed
a homogeneous
in hypereosinophilic
3a)
was
in Fig 3E. The
factor(Fig
of the
three
anti-T4
noted
in
culture
reactivity
all
ofall
other
MoAbs
tested
remained
unchanged
(data
not shown).
Normal
basophils
cultured
in factor-conditioned
media.
Phenotypic
analyses
(combined
toluidine/immunologic staining
procedure)
of normal
basophibs
from all but
one
donor
(in
MNC
preparations)
cultured
for
5 days
in
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
1876
STAIN
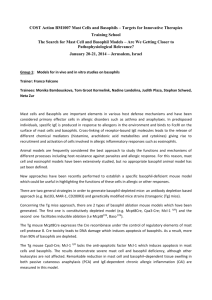
A
B
TSA7/C017
(938)
8,9-u/CD,,
MY?/CDl3
_______________________
(741)
ViIcRZ/C016
h___.___-_-
(851)
(741)
A-2/C09
(931)
Leu4/CD3
(21)
Ylil-OS/COIS
nlP-2b/p4S
_anti-T*C/CO2S
(618)
6Y9/p67
_
_______________________________
(96%)
ET AL
(41)
(SI)
troi
T4/C04
anti-lILA-DR
T1l/C02
C
(81)
(SI)(31)
D
d4y
dWy
day
day
day
day
5,
(93%)
5. antt-TAC
intl
control
(92%)
2. anti-TAt
(601)
(71)
siitI-HLA-DI/NTI-
2, control
0. anti-TAc
.HLADft/s-1f
antl-NLA-D*/IoP*
svperuiatsat
#{149}atl-NLA-Dt/IL-Z
(74%)
(311)
(461)
#{149}nti-HLA-DI/caatrol
media.
(471)
0. control
castro)
E
VlT-4/C04
(35%)
Leu3a/CD4
(401)
T4/CD4
control
(451)
day
V1T-4/CD4
factor-conditioned
media
) as compared
31-I-Incorporation
with
(41)
higher
on day
2 than
revealed
of 5 days.
0
results
(HLA-DR,
on day
was
the
prolifera-
uptake
on days
incorporation
5. A distinct
increase
of the
elevated
all
3H-uptake
In this study,
toluidine-stained
a panel
of MoAbs
to evaluate
of
peripheral
indicate
basophils
blood
cells
the
were phenotyped
with
antigenic
membrane
basophils.
The
results
2.
Culture
Expression
d in Control
of Surface
Medium
Determinants
as Measured
1
Antibody
Designation
Anti-TAC
Anti-HLA-DR
with
0
Reactive
74
8
(%)
2
Reactive
of basophils
of mem-
representing
responding
an
immedi-
of MoAbs
directed
against
the
with activated
T and B lymphocytes
as monocytes
of the recently
established
a subset
of myeboid
blast
stimulated
by ‘y-IFN.28#{176} With
IL
the
2
as
excep-
eosinophilic
cell line
cells,32’33 no granubocytic
3.
3H-Thymidine
Incorporation
EoL3’
cells
of CGL
5
Reactive
92
93
21
47
3
18
45
Control
0
0
0
59
67
77
Anti-HLA-DR
4
29
41
T4
Control
2
0
23
0
43
0
Basophils
on Days
2. and 5
Days
Analyses
T4
Anti-TAC
idea
tion
and
Medium
(%)
pattern
a population
well
Patient No.
Control
(%)
medium
HTB-9
‘y-lF
IL-2
2
the common
activated
cell type and/or
ately to certain
stimuli.
on CGL Basophils
by FACS
a unique
clearly
Days
Patient
No.
express
The most conspicuous
finding
was the detection
of three
activation-linked
structures
on the surface
membrane
of
basophils.
The presence
of the structures
in question,
ie, the
IL 2 receptor,
the T1O antigen,
and the structure
p 24, is
Table
Table
that
determinants.
So far, reactivity
receptor
was observed
DISCUSSION
profile
analyses
of anti-TAC
consistent
noted in the HTB-9-condiwith the control
medium,
no significantly
0,
FACS
0; (C) reactivity
brane
CGL-basophils.
Table
3 shows
by 3H-thymidine
that the 3H-thymidine
3H-thymidine
incorporation
tioned
medium.
As compared
other
samples
over a period
day
identical
studies.
tion kinetics
as measured
2, and 5. It is evident
was
gave
purified
of purified
CGL basophils.
(A and B) day
with cells in the control
medium
(days
0, 2, and 5); (D) HLA-DR
expression
on cultured
basophils
(day 5);
and (E) T4 expression
on cultured
basophils
(control
medium.
days
0 and 5).
(31)
14/C04
control
3.
Fig
(51)
Lea3a/C04
T4
5
BaPA
NT, not t ested.
0
2
5
1
0.6
±
0.05
5.2
±
0.3
2.4
±
0.2
2
0.5
±
0.2
4.8
±
0.9
0.7
±
0.06
1
0.9
±
0.05
13.6
±
0.8
4.8
±
0.3
2
0.7
±
0.07
8.2
±
0.5
3.3
±
0.2
NT
1
NT
NT
2
0.6
±
0.05
4.3
±
0.8
0.8
±
0.02
1
0.4
±
0.02
4.7
±
0.2
1.9
±
0.3
2
0.5
±
0.06
5.4
±
0.2
0.7
±
0.02
1
0.6
±
0.03
8.2
±
0.8
2.4
±
0.1
2
0.6
±
0.1
3.7
±
0.3
0.8
±
0.1
Values
are given
in cp m
x
i0
±
SD.
0,
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
THE
BASOPHIL
1877
PHENOTYPE
have yet been reported
to be reactive
antibodies.
Basophibs
also reacted
with MoAb
with
BA-2
(CD9),
ing the p 24 structure.
which
in our hands
to react
with
This
neutrophils,
was
lymphohematopoietic
structure
and
cell
p 24 has
from
evident
antibody,
also
surface
been
the
p 24 molecule
(CD18
recognizfails
the
T cells,”
preparations
it
is responsible
VIM-2,
a
Recently,
on activated
for
MoAbs),
lactosylceramide
(CD17
CR1 receptor
(MoAb
El I ), the 40-kd
CIKM5),
and the glycolipid
structure
to identify
structure.34
antigen
2 receptor
reported
detected
affinity-purified
that
initially
anti-IL
is now
present
cells
Moreover,
basophils
(MoAbs
MY9,
L4F3),
known
generated
to
be
monocytic
a protein
on all granulocytic
promyelocytes.
structure
p67
only
by
beyond
clearly
which
The p67
with ongoing
determinant
granulocyte
was reported
differentiation.43
eosinophil
this
structure
ered unreactive
with anti-TlO
Based
on the assumption
an activated
state
or that
stimuli,
we also
studied
culture.
To this
end,
and CGL
basophils
fMLP/cytochalasin
colony
the
short-term
basophil
phenotype
basophibs
or BaPA
differed
with
in three
day
of HLA-DR
days
with
the expression
2 and 5. Third,
three
different
At this point,
of HLA-DR
to culture
the T4 antigen
MoAbs
directed
we cannot
definitely
and T4 on basophils
conditions
or whether
A differentiation
in
to
in vitro
not
to a “late”
after
2
was detectable
on
became
against
demonstrable
this structure.
say whether
the expression
HLA-DR-positive
state
may
be
conceivable
with regard
to the other activation-linked
structures. Whether
the expression
ofdifferentiation
structures
or
the susceptibility
of receptors
corresponds
with
mediator
release
requires
further
investigation.
The
the
T4
expression
of various
antigen
on basophibs
possible
relationship
cabby stained
cells.39
question
suggests
differentiation
modulating
activation-linked
again
raises
of T lymphocytes
The detection
ofthe
that
the
the
question
properties
are influenced
the occurrence
nor
the
does
common
myeboid
in particular
the
presence
precursor
HL-60
cells
well.41’42
The
antigen
finding
structure
of this
since
were
on cultured
concerning
and/or
reported
determinants
the CR3
p150
receptor
(CDl3
antigen
monocytes
provide
and
to display
the
recognized
MoAbs),
the
evidence
not
cells,
T4
antigen
on basophils
by CDI
3 chain
as
were
1 MoAbs,
of LFA-1
gradually
staining
of
and
obtained
from
reactivity
with
cells
which
basophilic
structures
3-fucosyl-N-acetyllactosamine
(VIM-D5,
IG1O,
neuraminidase
VIM-C6)
treatment,
was
however,
on basophils,
which
represents
a pheobserved
with myeboid
and lymphatic
observation
basophils
by MoAbs
is of major
cytes.45
Because
human
IgG,”
of apparent
lack the
VEP-I3,
importance
functional
impor-
50- to 70-kd
Fc-y-receptor
Leubba,
ViFcR2).
This
for the phagocytotic
structure
basophils
minor
on the
are
basophils.
excluded
An
either
by MoAb
CIKM5)
to
of the
types
bind
receptor’s
of granulocytes
nonreactivity
alternative
is that
CR I and the
tors contributing
known
differences
different
for the
of the
CD16
possibility
which
the 40-kd
Fc-y-receptor
is the
sole
IgG
binding
LFA-1
structures,
to the functional
capacity
CR
1 receptor
on basophils,
particles,47
and
in the immune
have
obtained
are consistent
differentiation
influence
this
surface
molecular
could
be an
MoAbs
with
cannot
yet
(recognized
be
site of basophils.
particles,
were
types of mature
findings
of the
by use of complementwith
the role assigned
to
response.
been
ical,2’3’”’49 histochemicab,4’7’”
These
studies
were laborious
could
not be performed
the basophil
phenotype
offers a new possibility
aggregated
which are further
recepprocess
of phagocytosis
mainly
by providing
attachment
to target
identified
by corresponding
MoAbs
on all
granulocytes.
These
data
confirm
previous
explored
mostly
by morphobog-
and functional5’6’#{176}’5’ analyses.
and, with a few exceptions,
simultaneously.
and the technique
for the simultaneous
The knowledge
of
used in this study
determination
of
and function
and provides
the
cell type
specifically
through
opportunity
to
its different
structures.
for a
-y-I FN-stimulated
the
we detected
does
An
that
So far, basophils
by T cells or T cell
of the T4 antigen
basophils
myebomonocytic
MoAbs
After
is expressed
we already
receptor
basophils
in
and
of neutrophils.
Antibodies
against
this structure
completely
block the binding
and ingestion
of IgG-coated
sheep erythro-
of a
cultured
basophils,
the existence
of a common
precursor
cell, as proposed
by Burnet,#{176} seems
unlikely
with regard
to
the numerous
myeboid-associated
determinants.
The detecthe T4
a novel
by CDI5
cells.’8
coated
on
tion of
represent
3-FAL
nomenon
we
neutrophil-associated
structure
detectable.
and
and metachromatisurface
structures
functional
of basophils
factors.
Despite
structures
of
the
been
the decrease
to neutrophil
a different
in vitro-cultured
fetal
to be MY9 negative.”
The
explanation
is a phenomenon
restricted
this may also occur in vivo.
showed
webb-defined
tance
was
(recognized
was significantly
unchanged
until
Basophils
therefore
missing:
blast
normal
cells
in
First,
Certain
were
identified
by a T cell
respects:
of anti-TAC
and remained
adults
MY9,
as did
were reported
were
exposed
to
and cultured
for 5
synthesized
differentiation.
healthy
suspension
freshly
obtained
the phenotype
of
days of culture,
the reactivity
increased
in all samples
tested
5. Second,
be
either
hrIL 2, hr--y-IFN,
superline (which
is reported
to enhance
As compared
CGL
basophils,
cultures
to
after
in MNC
as purified
fractions
B and Ca-ionophore
formation),24
hybridoma.2526
basophils
and
reported
antibodies.37’38
that basophils
represent
cells
these
cells
rapidly
respond
normal
days in medium
containing
natant
of the HTB-9
cell
blast
was
cells as well as on activated
cells have so far been consid-
stage
progenitors
to be lost
Because
observation.
precursor
myeboid
the
displayed
had so far
myeboid
of basophils
was evident
in our study,
antibody
binding
seems
to be restricted
Whereas
the
(MoAb
by MoAb
cells.43
kinase
and for growth-promoting
properties.36
Moreover,
basophils
were stained
by MoAbs
detecting
the
Tl0 antigen,
which
represents
a new and quite
unexpected
expressed
on immature
lymphocytes,
maturing
MoAbs),
Fc’y-receptor
identified
ACKNOWLEDGMENT
We are indebted
this manuscript.
technical
advice,
skillful technical
ber for her help
manuscript.
to Professor
Dr W. Knapp for his suggestions
for
We also wish to thank Dr 0. Majdic for his helpful
Susanne
Frank and Roswitha
Gabriel
for their
assistance,
Mag. Alexandra
M. Jantscher-Karlhuin translating,
and Johanna
Moser for typing this
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
1878
STAIN
ET AL
REFERENCES
I . Juhlin
L: Basophil
leukocyte
differential
in blood and bone
marrow. Acta Haematol
29:89, 1963
2. 1-lastie R: A study of the ultrastructure
of human
basophil
leukocytes.
Lab Invest 31:223, 1974
3. Zucker-Franklin
D: Ultrastructural
evidence
for the common
origin of human mast cells and basophils.
Blood 56:534, 1980
4. Gilbert HS, Ornstein
L: Basophil counting
with a new staining
method using alcian blue. Blood 46:279, 1975
5. Denburg
JA, Befus AD, Goodacre
R, Bienenstock
J: Basophil
production
III: Relation of histamine
to guinea pig basophil growth
in vitro. Exp Hematol 9:214, 1981
6. Akiyama
K, Pruzansky
ii, Patterson
R: Hapten-modified
basophils:
A model of human immediate
hypersensitivity
that can be
elicited by IgG antibody.
J lmmunol
133:3286,
1984
7. Tadokoro
K, Stadler
BM, Dc Weck AL: Factor-dependent
in
vitro growth of human normal
bone marrow-derived
basophil-bike
cells. J Exp Med 158:857, 1983
8. Horton MA: On the bone marrow
mast cell: In vitro growth
and characterization
of human malignant
mast cells, in Bernard
A,
Boumsell L, Dausset J, Milstein L, Schlossman
SF (eds): Leukocyte
Typing. Berlin, Springer
Verlag, I 984
9. Rimmer
EF, Horton
MA: In-vitro culture of basophils
from
human
bone marrow.
Leuk
Res 10:1241,
1986
10. Foon KA, Todd RF III: Immunologic
classification
of leukemia and lymphoma.
Blood 68:1, 1986
1 1 . Roitt JM, Brostoff J, Male DK: Cells involved in the immune
response,
in Immunology.
London, Gower Medical,
1985
I 2. Majdic 0, Liszka K, Lutz D, Knapp W: Myeloid differentiation antigen
defined
by a monoclonal
antibody.
Blood 58:1127,
I981
13. Holter W, Majdic 0, Liszka K, Stockinger
H, Knapp W:
Kinetics
of activation
antigen
expression
by in vitro stimulated
human I lymphocytes.
Cell Immunol
90:322, 1985
14. K#{246}ller
U, Majdic
0, Liszka
K, Stockinger
H, PabingerFasching
I, Lechner
K, Knapp W: Lymphocytes
of haemophilia
patients treated with clotting factor concentrates
display activationlinked cell surface antigens.
Clin Exp Immunol
59:613, 1985
15. Knapp W, Majdic 0, Bettebheim
P. Liszka K: VIL-Al,
a
monoclonal
antibody
reactive with acute lymphatic
leukemia
cells.
Leuk Res 6:137, 1982
16. Knapp W, Majdic 0, Stockinger
H, Bettelheim
P, Liszka K,
K#{246}ller
U, Peschel Ch: Monocbonal
antibodies
to human myebomonocyte differentiation
antigens
in the diagnosis
of acute myeloid
leukemia.
Med Oncol Tumor Pharmacother
4:257, 1984
17. Majdic 0, Bettelheim
P. Stockinger
H, Aberer W, Liszka K,
Lutz D, Knapp W: M2, a novel myelomonocytic
cell surface antigen
and its distribution
on leukemic cells. Int J Cancer 33:617, 1984
18. Stockinger
H, Majdic 0, Liszka K, Aberer W, Bettelheim
P.
Lutz D, Knapp W: Exposure
by desialylation
of myeloid antigens on
acute lymphoblastic
leukemia
cells. J NatI Cancer
Inst 73:7, 1984
19. Stockinger
H, Majdic
0, Liszka
K, K#{246}ller
U, Holter
W,
Peschel Ch, Bettelheim
P, Gisslinger
H, Knapp W: T14, a nonmodulating
150 kd I cell surface antigen,
in Reinherz
EL, Haynes
BF, Nadler
LM, Bernstein
ID (eds): Leukocyte
Typing
II. New
York, Springer
Verlag, 1986
20. Holter W, Majdic 0, Stockinger
H, Knapp W: Analysis of I
cell activation
with a non-mitogenic
anti CD3 antibody
and the
phorbol ester IPA. Clin Exp Immunol
62:600, 1985
21. Amiot M, Bernard
A, Raynal
B, Knapp W, Deschildre
C,
Boumsell
L: Heterogeneity
of the first cluster
of differentiation:
Characterization
and epitopic
mapping
of three CDI molecules
on
normal human thymus cells. J Immunol
136:1752,
1986
22. Liszka K, Majdic 0, Bettelheim
P, Knapp W: Glycophorin
A
expression
in malignant
hematopoiesis.
Am J Hematol
15:219,
I983
23. Marone
G, Poto 5, Celestino
D, Bonini S: Human
basophil
releasability
III. Genetic control of human basophil releasability.
J
Immunol
137:3588,
1986
24. Hoang 1, Wong G, Clark 5, Minden
MD, McCulloch
EA:
Effects of recombinant
GM-CSF
on the blast cells of acute myeloblastic leukemia.
Blood 68:313, 1986
25. Stadler
BM, Hirai K, Brantschen
5, Nakajima
K, de Weck
AL: Biochemical
characterization
of the human basophil promoting
activity.
Int Arch Allergy AppI Immunol,
in press
26. Stadler BM, Hirai K, Brantschen
5, de Weck AL: Biological
and biochemical
characteristics
of the basophil
like cell promoting
activity
and a human
IL-3 like activity.
lmmunobiology
172:225,
I 986
27. Holter W, Fischer GF, Majdic 0, Stockinger
H, Knapp W: I
cell stimulation
via the erythrocyte
receptor.
J Exp Med 163:654,
1986
28. Uchiyama
1, Broder 5, Waldmann
IA: A monoclonal
antibody (anti-Tac)
reactive
with activated
and functionally
mature
human I cells. i Immunol
126:1393,
1981
29. Robb Ri, Greene
WC, Rusk CM: Low and high affinity
cellular receptors
for interleukin
2. J Exp Med I 60: 1 126, 1984
30. Holter W, Grunow R, Stockinger
H, Knapp W: Recombinant
interferon-gamma
induces interleukin
2 receptors
on human peripheral blood monocytes.
J Immunol
136:2171,
1986
31 . Saito H, Bourinbaiar
A, Ginsburg
M, Minato
K, Ceresi E,
Yamada
K, Machover
D, Br#{233}ard
J, Math#{233}
G: Establishment
and
characterization
of a new human
eosinophilic
leukemia
cell line.
Bbood66:l233,
1985
32. Armitage
Ri, Lai AP, Roberts
PJ, Cawley
JC: Certain
myeloid
cells possess receptors
for interleukin
2. Br J Haematol
64:799, 1986
33. Visani G, Delwel R, Iouw I, Bot F, Lowenberg
B: Membrane
receptors
for interleukin
2 on hematopoietic
precursors
in chronic
myeloid leukemia.
Blood 69:1 182, 1987
34. Kersey iH, LeBien 1W, Abramson
CS, Newman
R, Sutherband R, Greaves M: p24: A human leukemia-associated
and lymphohemopoietic
progenitor
cell surface structure
identified
with monoclonal antibody.
J Exp Med 153:726, 1981
35. Holter W, Majdic 0, Liszka K, Stockinger
H, Knapp W:
Kinetics
of activation
antigen
expression
by in vitro-stimulated
human T lymphocytes.
Cell Immunol
90:322, 1985
36. Zeleznik
NJ, Hollingsworth
MA, Metzgar
RS: Functional
studies of the CD9 antigen defined by monoclonal
antibody
DUALL- 1 . Third International
Workshop
and Conference
on Human
Leukocyte
Differentiation
Antigens,
Oxford,
1986 (abstr)
37. Janossy G, Tidman N, Papageorgiou
ES, Kung PC, Goldstein
G: Distribution
of I lymphocyte
subsets in the human bone marrow
and thymus:
An analysis
with monoclonal
antibodies.
J Immunol
126:1608,
1981
38. Cotner I, Williams
JM, Christenson
L, Shapiro
HM, Strom
TB, Strominger
J: Simultaneous
flow cytometric
analysis of human
I cell activation
antigen expression
and DNA content.
J Exp Med
157:461,
1983
39. Day RP,
antigen on rabbit
Singal
DP, Bienenstock
J: Presence
basophils.
J Immunol
114:1333,
1975
of thymic
40. Burnet FM: The probable
relationship
of some
cells to the 1-cell system. Cell Immunol
30:358, 1977
or all mast
41. Moscicki A, Amento
EP, Krane iT, Colvin RB: Modulation
of surface antigens
of a human cell line, U937, during incubation
with lymphocyte-conditioned
medium:
Detection
of 14 antigen and
its presence on normal blood monocytes.
J Immunol
1 3 1 :743, 1983
42. Dubreuil
P, Mannoni
P, Olive D, Winkler-Lowen
B, Mawas
C: Expression
of I cell-related
antigens
on cells from the myelomonocytic
lineage,
in Reinherz
EL, Haynes
BF, Nadler
LM,
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
THE
BASOPHIL
Bernstein
ID (eds): Leukocyte
Typing
II. New York, SpringerVerlag, 1986
43. Griffin JD, Linch D, Sabbath
K, Larcom P. Schbossman
SF:
A monoclonal
antibody
reactive
with normal and leukemic
human
myeloid progenitor
cells. Leuk Res 8:521, 1984
44. Seldin DC, Caulfield
JP, Hem A, Osathanondh
R, Nabel G,
Schlossman
SF, Stevens
RL, Austen KF: Biochemical
and phenotypic characterization
of human basophilic
cells derived
from dispersed fetal liver with murine I cell factors. i Immunol
136:2222,
I986
45. Fleit HB, Wright
SD, Unkeless
JC: Human
neutrophil
Fc-gamma
receptor
distribution
and structure.
Proc Natl Acad Sci
USA 79:3275,
1982
46. Ishizaka
I, Sterk AR, Ishizaka
K: Demonstration
of Fcgamma
receptors
on human
basophil
granulocytes.
i Immunol
123:578,
1979
1879
PHENOTYPE
47. Thomas
LL, Lichtenstein
LM: Augmentation
stimulated
histamine
release
from human
basophils
treated zymosan particles.
J Immunol
123:1462,
1979
48. Denburg
JA, Telizyn 5, Messner H, Jamal BLN,
Si, Gleich GJ, Bienenstock
J: Heterogeneity
of human
blood eosinophil-type
colonies:
Evidence
for a common
eosinophil
progenitor.
Blood 66:312, 1985
49. Leary A, Ogawa M: Identification
phil colonies in culture of human peripheral
Blood 64:78, 1984
50. Lett-Brown
MA,
with chronic myelogenous
51.
human
MacGlashan
basophils.
Juneja
HS:
Ieukaemia.
DW, Lichtenstein
i Immunol
124:2519,
of antigenby serum-
Ackerman
peripheral
basophil-
of pure and mixed
blood and marrow
basocells.
Basophil
function
in patients
Br J Haematol
61:621, 1985
LM:
1980
The
purification
of
From www.bloodjournal.org by guest on March 5, 2016. For personal use only.
1987 70: 1872-1879
Human blood basophils display a unique phenotype including activation
linked membrane structures
C Stain, H Stockinger, M Scharf, U Jager, H Gossinger, K Lechner and P Bettelheim
Updated information and services can be found at:
http://www.bloodjournal.org/content/70/6/1872.full.html
Articles on similar topics can be found in the following Blood collections
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of
Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.