Volume 3, Number 3 - JRW Behavioral Health Services
advertisement

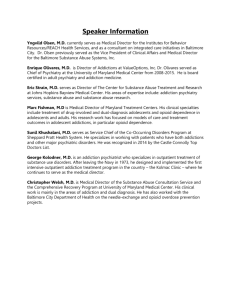
The Addiction and Behavioral Health Newsletter A publication of JRW Behavioral Health Services JRW Behavioral Health Services is a founding member of the Chicago Lakeside Group VOLUME 3, NUMBER 3 NOVEMBER 2013 Welcome to Volume 3, Number 3 of the Addiction and Behavioral Health Newsletter. This month, Mark Sanders’ featured article is “10 Important Things to Know When Working with Chemically Dependent Clients”. Also in the newsletter you will also find information regarding new training opportunities, available on-site workshop and inservice topics, regional and national conferences, news from the world of addiction science, and featured links to other resources for the substance dependency treatment and prevention community. Please Note: In addition to IAODAPCA-approved training events, we now offer LCSW and LCPC Continuing Education Units (Illinois License # 159.001214) Table of Contents Page 1 Welcome 2-3 Topic of the month: The “krokodil” Myth 4-6 Mark Sanders: 10 Important Chemically Dependent Clients 7 Home Study Course and Upcoming Webinars 8 News from the World of Addiction Science 9 Upcoming National and Regional Conferences 10 Things to Know When Working Internet Links (English and Spanish/Inglés y Espaňol) COMING SOON! In our next issue, look for the schedule of winter 2014 workshops presented by The Chicago Lakeside Group Mark Sanders, LCSW, CADC Mark Sanders & Associates Randall Webber, MPH, CADC JRW Behavioral Health Services © 2013 1 with Topic of the Month: The Myth of “Krokodil” Randall Webber, MPH, CADC Desomorphine is a synthetic opioid substance, synthesized in the 1930s. Although used medically in other countries, it is, in the United States, a Schedule I drug, in the same category as PCP, LSD and heroin. Because heroin is so scare in Russia, desperate, impoverished addicts use codeine tablets (sold over the counter in that country) as the starting point in the creation of homemade desomorphine. The codeine is crushed and then mixed with gasoline or paint thinner and the sulfur from match heads, resulting in a toxic brew called “krokodil”. When injected, krokodil produces a short-lived high, but also begins to destroy body tissue from the inside out, so that by the time the signs of toxicity are apparent, a great deal of physical damage has already occurred. One of the signs of krokodil toxicity is the green, often scaly skin from which the drug gets its name. “Krokodil” patient in Russia In 2004, the U.S. Drug Enforcement Administration (DEA) identified two samples of pure desomorphine in the United States, but has not seen any sign of that drug since then. However, in November of 2012, krokodil was implicated in the death of a 33 year-old man in Duncan, Oklahoma. Autopsy results, however, showed only morphine in his system, and his death was attributed to heroin overdose *. Later, The Oklahoma Bureau of Narcotics released a statement saying that accounts of “Krokodil” being circulated through the media “should be taken with a grain of salt.” In September of 2013, another report of krokodil-related hospitalizations was issued in Arizona, but later refuted when toxicological tests once again implicated heroin. The most extensive media coverage of krokodil occurred in the second week of October, when a physician at the Presence St. Joseph Medical Center in Joliet reported that he had seen numerous patients whose medical conditions were tied to krokodil use. Allegedly, these individuals mistakenly purchased krokodil when attempting to obtain heroin. Dr. Abhin Singla reports to Fox News that patients seen in Joilet had used krokodil * Heroin is metabolized into morphine before being excreted from the body, and heroin overdoses are substantiated by the presence of the latter in the victim’s tissue. 2 Later, krokodil reports surfaced in McHenry County, Illinois and several other sites. Once again, no analytical data confirmed the presence of desomorphine in any of the Chicago-area afflicted patients. The reports of krokodil were greeted with skepticism by the author’s Internet Linkedin.com “Emerging Drugs of Abuse” discussion group, composed of more than 2600 alcohol and other drug counselors, toxicologists, pharmacologists, physicians, harm reduction specialists, government officials, community volunteers, recovering individuals and law enforcement professionals in the United States and 45 other countries. Heroin is cheap and unusually pure in Chicago (often referred to as the “heroin capital of the United States”) and addicts would unlikely to purchase krokodil, which is commonly a liquid that does not resemble heroin. Further, codeine (required to make desomorphine) is a prescription drug in the United States, seldom used in tablet form and more difficult to obtain than heroin. In addition, the presence of krokodil has never been documented anywhere except for Russia. Regardless, breathless, sensationalistic reports of krokodil sightings in the Chicago area spread like wildfire through the Chicago (and eventually national) media . On October 27, 2013, the Chicago Tribune reported, in an article headlined, “Suspected krokodil a false alarm” that the United States Drug Enforcement Administration had interviewed both “krokodil” patients and the doctors who treated them, as well made hunting down the drug the top priority of 200 agents in five states. Yet, this search had yielded no krokodil samples. "We have run quite a few buys in the city and suburbs," said Jack Riley, Agent in Charge of the DEA’s Chicago office, "(but) the lab tells us is it's just heroin." In the same article, Dr. Jane Maxwell, a Professor of Social Work at the University of Texas at Austin, an advisor to National Institute on Drug Abuse and a member of the linkedin.com “Emerging Drugs of Abuse” group pointed out that the kind of medical conditions observed in alleged “krokodil” patients can be caused by reusing or sharing hypodermic needles and exposing themselves to a wide variety of bacterial infections. Is this simply a case of the media creating a virtually nationwide panic (as of November 5 th, this story was still being broadcast in Ohio) by reporting sensationalistic, unsubstantiated rumors? No; it’s much more. The krokodil myth is an example of how misinformation can divert attention from more important topics, such as the fact that sterile syringes are sold legally in Illinois pharmacies as well as available free at needle exchange programs in Chicago and other areas of the state. False information such as the krokodil reports can also lead to a serious loss of credibility when high-risk groups targeted for prevention activities discover the truth. Of course drug information is a very small part of an overall community-based prevention effort, but regardless, accurate facts about drug of abuse are important to the maintenance of public health. Finally, the media’s time can be better spent on highlighting the very real possibility of recovery from chemical dependency, and the reality of this recovery in the lives of millions across not only the United States, but the whole world. To separate fact from fiction about new, emerging drugs of abuse, join us on Friday, November 21, 2013 for our webinar “The New World of Street Drug Pharmacology”. Click here for more information or to register 3 10 IMPORTANT THINGS TO KNOW ABOUT WORKING WITH CHEMICALLY DEPENDENT CLIENTS Mark Sanders, LCSW, CADC Ideally, individuals with substance use disorders would primarily be treated by licensed and certified addictions counselors. Research reveals that this is not possible. In any given year approximately 10 percent of chemically dependent individuals seek help for their addiction, 25 percent will seek help directly for their addiction in their entire lifetime, and 75 percent will never receive treatment for their addiction. (White, Kurtz, and Sanders, 2006). They will, however, wind up in hospital emergency rooms, hospital beds (being treated for gout, high blood pressure, heart disease, strokes, cancer, and other medical conditions caused by their addiction), prison, mental health facilities, homeless shelters, domestic violence shelters, and child welfare agencies. Professionals in these allied fields will need working knowledge on how to address individuals with substance use disorders who show up at their facilities. As a specialist in addictions, you are often asked by non-addiction counselors how to work with individuals with substance use disorders. Below is a list of ten things that are important for other behavioral health specialists to know about working with chemically dependent clients. 1. Recovery is possible and happening every day! There is a great deal of pessimism caused by client relapse. It is important for behavioral health specialists to know that approximately 50 percent of clients who leave treatment never relapse. Therefore, it is important for those of us who specialize in working with addictions to stop saying, “Relapse is a part of recovery,” because, if it is not true for half of the clients we serve, it is not true. We should let them know that September is National Recovery and National Native American Welbriety Month, and millions of people all over the world march, rally, and celebrate recovery. Let them know that once a person gets sober, eventually he or she is filled with gratitude and becomes a force for goodness forever. 2. Clients whom you think will never recover often do. With all our current technology, we are unable to predict with 100 percent accuracy which clients will recover and which will not. History has taught us that often the ones whom we think will recover often don’t, and the ones we sometimes believe don’t have a chance to recover often do. They are frequently the ones who are the most resistant and stir up strong negative countertransference reactions in counselors. You can let specialists in allied fields know that their resistance is often caused by internalized discomfort because lessons they are learning in treatment are creating a challenge for them, making it difficult for them to continue with their current behavior. 3. Confrontation is overrated. For years addictions counselors were taught to be “good prosecuting attorneys”. Their job was to make clients squirm in their seats while they “broke their denial”. Research by Rollnick and Miller (2012) indicates that the more heavily we confront clients the more they drink. Other studies indicate that heavy confrontation can re-traumatize the traumatized and further decompensate the decompensated. 4 4. A little treatment is better than no treatment at all. Assessment might indicate that a client needs a more restricted level of care, while he or she is motivated for a less restricted level of care. You can let behavioral health specialists know that a little treatment is better than no treatment at all. In some instances, a less intensive level of care can be all that is needed to prime the pump of recovery, even though an assessment indicated that a more intensive level of care was needed. In other instance, clients can be motivated to pursue a higher level of care later. 5. Peer support is of utmost importance. Hundreds of thousands of people fill stadiums each year at annual AA, NA, and CA conventions, celebrating anywhere from one day to 70 years of recovery. 12-step programs have answered the question of what a client should do at 3:00 a.m. on Saturday night after waking up in a cold sweat craving heroin or cocaine and his therapist is asleep or on vacation. He can pick up the phone and call a member of one of the anonymous groups who will be there to help him. Perhaps he reaches a recovering truck driver who travels between cities on the midnight shift. My mentor once said, “If all paid addictions professionals lost their jobs, members of the recovery community would still support individuals in early recovery.” You can let allied professionals know that not all individuals want to attend traditional 12-step groups, that there are scores of other mutual aid groups, ranging from Women for Sobriety, Anesthesiologists Anonymous, Celebrate Recovery (a Christian-based recovery group), JACS (Jews Who are Alcoholic, Chemically Dependent and Significant Others), and White Bison (a Native American recovery movement). To learn more, they can visit www.facesandvoicesofrecovery.org and click on “Mutual Aid Groups.” 6. The word “aftercare” should be changed to “continuous care” – it is the most important part of recovery support. Of the 50 percent of clients who relapse, 80 percent of those relapses occur within the first 90 days of them leaving treatment (White, Kurtz, and Sanders, 2006). This means that we should stop treating aftercare as an afterthought. As NIDA’s research reveals, clients need 90 days of continuous recovery support in order to be launched on the path to recovery. 7. Relapse can be therapeutic if the client learns from the experience. It is important to let allied workers know that they should never take relapse personally. They should also know that most clients they serve will never get sober in front of their face, that other counselors will take credit for the work they initiate. Most important is to let them know that relapse can be therapeutic, so long as clients learn from the experience. They should ask every client who relapses, “What did you learn from this experience?” As Carter G. Woodson said, “If we do not learn from history, we are likely to repeat it.” If the client cannot figure out lessons learned, it is our job to help him or her discover those lessons. 8. As recovery capital increases the risk of relapse decreases. Recovery capital is defined as internal and external assets that a client can bring to bear on his or her recovery. This includes optimism and hope, employability, success prior to addiction, a good education, 5 vocational skills, family support, love, mutual aid group attendance, cultural pride, etc. When professionals in allied fields ask me, “What should I do when a client is in strong denial?” I encourage them to help clients build their assets instead of trying to “break the denial,” because when clients build their assets, their optimism that they can recover also increases. Someone once asked me, “Can a better life lead to recovery, or does recovery lead to a better life?” You can let workers in allied fields know that the answer to both questions is yes. 9. Resource development is an important part of recovery. The basic needs identified by Abraham Maslow for food clothing, and shelter are important parts of supporting recovery, along with helping individuals have a sense of community. Therefore, let allied workers know that good old fashioned case management can be instrumental in promoting recovery. Several recovery coaches in Chicago have told me that 75 percent of their work involves linking individuals in early recovery with needed resources, including everything from where to get a Social Security card, state ID, tattoo removal, free-to-inexpensive dental care, glasses, a winter coat, etc. 10. Competence helps increase recovery rates. Finally, you can encourage our colleagues in allied fields to pursue certification or licensure as addiction counselors. In most states, community colleges, through doctoral programs, offer certificates in addictions counseling leading toward certification. The knowledge gained while pursuing this credential will increase their competence and confidence in addressing substance abuse and dependence. REFERENCES Miller, William & Rollnick, Stephen (2012) Motivational Interviewing, Third Edition New York: Guilford Press White, W., Kurtz, E., and Sanders, M. (2006) Recovery Management. Great Lakes ATTC Monograph ABOUT THE AUTHOR Mark Sanders, LCSW, CADC, is an international speaker in the addictions and mental health fields whose presentations have reached thousands throughout the United States, Europe, Canada, and the Caribbean Islands. He is co-author of Recovery Management and author of Relationship Detox: How to Have Healthy Relationships in Recovery. His most recent book is entitled, slipping through the Cracks: Intervention Strategies for Clients with Multiple Addictions and Disorders. He is a lecturer at the University of Chicago. Click here to visit his website. Join Mark Sanders on December 19, 2013 for his cutting edge webinar “The Future of Substance Abuse Treatment in America” Click here for more information or to register 6 Home Study Courses and Upcoming Webinars* FREE COURSE We are still offering a free course entitled “DUI: The Effects of Prescription and Illicit Drugs”. To register for this course, click here or go to www.randallwebber.com/free_course * For additional information or to register for any of our courses or webinars, visit our website Contact us for information on group, series and multi-workshop discounts Webinars Preparing for the Future: Substance Abuse Treatment for Older Adults Presented by Randall Webber, MPH, CADC November 21, 2013 10:00 A.M.-12:10 P.M (CST) 2 Continuing Education Units (IAODAPCA/LCSW/LCPC) $25 The New World of Street Drug Pharmacology: Emerging Drugs of Abuse Presented by Randall Webber, MPH, CADC November 15, 2013 9:00-11:00 A.M. (CST) or 1:00-3:00 P.M. (CST) 2 Continuing Education Units (IAODAPCA/LCSW/LCPC) $25 The Future of Substance Abuse Treatment in America Presented by Mark Sanders, LCSW, CADC December 19, 2013 10:00 A.M.-12:10 P.M. (CST) 2 Continuing Education Units (IAODAPCA/LCSW/LCPC) $25 Home Study Courses Street Drug Pharmacology Advanced Street Drug Pharmacology Pharmacology and Physiology of Alcohol and Alcoholism * 7 All webinars and courses are approved for IAODAPCA, LCSW and LCPC continuing educations units (Illinois License # 159.001214) Upcoming Local, Regional and National Conferences Town Hall Meeting on Prescription Drug Abuse November 20, 2013 Fort Collins, CO 2014 NASPA Alcohol, Other Drug Abuse, and Violence Prevention Conference January 16-18, 2014 San Diego, CA 2014 Prescription Drug Abuse Conference: The Different Faces of Substance Abuse 5th Annual Conference Jan 28 - 29, 2014 National Harbor, MD 35th Annual Training Institute on Behavioral Health & Addictive Disorders Feb 10 - 13, 2014 Clearwater Beach, FL South Carolina 2014 Working Together Works Conference March 10 - 12, 2014 North Charleston, SC Alabama School of Alcohol and other Drug Studies 39th Annual Conference March 18 - 21, 2014 Tuscaloosa, AL 2014 American Society of Addiction Medicine 45th Annual Medical-Scientific Conference April 4-10, 2014 Orlando, Florida The 2014 National Rx Drug Abuse Summit Apr 22 - 24, 2014 Atlanta, GA Society for Prevention Research 22nd Annual Meeting May 27 - 30, 2014 Washington, DC 27th Annual Northwest Conference on Behavioral Health and Addictive Disorders May 28 - 30, 2014 Seattle (Bellevue), WA National Rural Institute on Drug Abuse June 8-12, 2014 Menomonie, Wisconsin 8 News from the World of Addiction Science Gabapentine (Neurontin) May be Effective in Reducing Cannabis Use and Facilitating Withdrawal Gabapentine (Neurontin) is an analog of the neurotransmitter gamma butyric acid (GABA), and is approved to treating seizures and peripheral neuropathy. Now, research in the journal Neuropsychopharmacology suggests that this medication may reduce cannabis use and craving as well as attenuate withdrawal. A study lead by Dr. Barbara Mason of the Committee on the Neurobiology of Addictive Disorders at The Scripps Research Institute in La Jolla, California found that compared to placebo, gabapentine reduced marijuana craving, days of use and the intensity of withdrawal symptoms (e.g., disturbances in mood and sleep, craving) in individuals who had been diagnosed with cannabis use disorder (DSM-V criteria). Further, the gabapentine group showed improvement in executive functioning (e.g., inhibition of impulses, cognitive flexibility, and complex information processing. Each subject was also provided with manual-guided, abstinence-oriented individual counseling on a weekly basis. Source: Mason, BJ; Crean, R; Goodell, V; Light, JM; Quello, S, et.al. (2012). A proof-of-Concept Randomized Controlled Study of Gabapentine: Effects on Cannabis Use, Withdrawal and Executive Function Deficits in Cannabis-Dependent Adults. Neuropsychopharmacology, 37(7): 1689–1698. Extreme binge drinking among high school seniors Binge drinking among high school seniors (defined as consuming five or more drinks in a row over the past two weeks) has risen and fallen in prevalence over the last decade. Between 2002 and 2012, the number of seniors who have engaged in binge drinking has been as high as 29.2 (2003) and as low as 21.6 (2011). Overall, this percentage has dropped somewhat steadily during that ten year period. At the same time, medical emergencies involving teen drinking have increased. A recent study published in Pediatrics has shed light on this apparent paradox. Using data from the University of Michigan’s Monitoring the Future study, Drs. Ralph Hingson and Aaron White of the National Institute on Alcohol and Alcoholism reported that in 2012, one in ten high school seniors had 10 or more drinks in a row and over one in had 15 or more drinks in a row at least once in the last two weeks. This finding is of great significance, since binge drinking, even at 5 or more drinks in a row, increases the risk of blackouts, homicides, car crashes, sexual assaults, altered brain development, and other serious outcomes. Dr. Megan Patrick, lead author of the binge drinking survey at the University of Michigan stated, "Alcohol use among adolescents is an enduring public health problem, and our findings regarding the rates of extreme binge drinking are particularly alarming," Patrick said. "We hope that this study is helpful in drawing attention to the extent of extreme binge drinking among our nation's high school seniors." Source: Hingson, RH & Aaron W (2013). Trends in Extreme Binge Drinking Among US High School Seniors. JAMA Pediatrics, 167(11):996-998. Click here to read the journal abstract. 9 Internet Links To Find More Links to Substance Use Disorder Resources, click here. LOS SITIOS INTERNET DE LA LENGUA ESPAŇOLA (Spanish Language Sites) Instituto en la Drogadicción/Sección de la Español NATIONAL SUBSTANCE ABUSE TREATMENT LOCATOR Substance Abuse and Mental Health Services Administration Treatment Locator PROFESSIONAL ASSOCIATIONS AND CERTIFICATION BODIES Employee Assistance Society of North America Illinois Alcoholism and Other Drug Abuse Professionals Certification Association Llinois Alcoholism and Drug Dependence Association NAADAC-The Association for Addiction Professionals National Council on Alcohol and Drug Dependence RECOVERY MANAGEMENT RESOURCES Behavioral Health Recovery Management Recovery Managment (William White, Ernie Kurtz & Mark Sanders) SCIENTIFIC JOURNALS Addiction Alcohol and Alcoholism Alcohol Research and Health Journal of Psychoactive Drugs Journal of Studies on Alcohol and Drugs Journal of Substance Abuse Treatment STATE AND FEDERAL AGENCIES Center on Substance Abuse Treatment Center on Drug Abuse Prevention Drug Enforcement Administration National Institute on Alcohol Abuse and Alcoholism National Institute on Drug Abuse SUBSTANCE ABUSE AND DEPENDENCE PREVENTION PROGRAMS Prevention First Mothers Against Drunk Driving 10