Artificial Blood The blood of the future
advertisement

Artificial Blood
The blood of the future
By
Anjali Thakkar
COSMOS 2007
Cluster 1
Mentor: Professor Paul Feldstein
The History of Artificial Blood
{
{
Milk was one of the first substances used as a blood
substitute in order to treat patients with Asiatic cholera.
(Squires 1).
After several patients died by receiving milk transfusions,
other substances were discovered as potentials (Squires 1):
z
z
z
Salt or saline solutions: used primarily as a plasma volume
expander, rather than as artificial blood
Hemoglobin isolated from red blood cells
Animal plasma could be used as a substitute for human blood
{
{
However, since many of the materials in animal plasma are toxic to
humans, this posed a problem to using it as a substitute
The problem of not having a workable substitute led to
Ringer’s Solution…
Ringer’s Solution
{
{
{
{
{
Created by the physiologist Sydney Ringer in 1882
Ringer’s solution is a saline solution which is able to
prolong the life of cells in the body
Solution contains sodium chloride, potassium chloride,
calcium chloride, and sodium bicarbonate: designed in the
concentrations found in the human body to keep the heart
pumping even outside of the body
This solution resembles blood serum
Often used to culture animal cells (Encyclopedia
Britannica)
Blood Grouping: Karl Landsteiner
• Karl Landsteiner was a worldrenowned immunologist and
pathologist in the 1900s.
•contributed to the world of
medicine in the fields of anatomy,
histology, and immunology
• 1909: Landsteiner classified
human blood into four different
groups: A, B, AB, and O
•Recognized the agglutinins in
the blood
•This has become the basis for
modern blood typing today
• received the Nobel Prize for
Physiology or Medicine in 1930
(Nobel Foundation)
http://nobelprize.org/nobel_prizes/medicine/laureates/1930/lan
dsteiner.jpg
Artificial Blood vs. Blood Substitutes
Artificial Blood
the main purpose of artificial blood is
to act as normal blood in the body,
providing a long-term solution to blood
loss or distortion (Squires 3).
{ no working artificial blood has been
created in the status quo
{
Blood Substitutes
the main purpose of a blood substitute
is to provide temporary support to the
circulatory system when necessary
(Squires 3).
{ blood substitutes generally are
focused on the role of transporting
oxygen for short-term cases such as
blood transfusions or surgeries
{ blood substitutes are generally simpler
since they are only focused on one of
the several functions of real blood
{ several types of blood substitutes have
been found including:
zHemoglobin-based oxygen carriers
zPerfluorocarbon emulsions
{
Ideal Characteristics of Artificial
Blood
{
Safe to use
{
Compatible in the human body
{
Able to transport and release oxygen where needed
{
Storable and durable for longer time periods
{
Is free of pathogens and toxins which would produce an
immune system response in the human body (Squires 3).
Problems Currently Associated with Artificial
Blood and Blood Substitutes
{
{
Bodily immune systems may sometimes react
negatively to the foreign blood that is inserted into
the body (Goorha et al 46).
Trauma/Shock Patients
z
{
Since these patients are often frequent recipients of
blood substitutes or plasma during surgery, it becomes
challenging to understand which types of blood
substitutes have affected which problem in the
patient’s body (Winslow 2).
Currently no real working source of artificial blood
exists that can perform the multifarious tasks of real
human blood cells (Goorha et al 46).
Types of Blood Substitutes
Perfluorocarbons (PFC) emulsions
Perfluorocarbons are derived from a group of
hydrocarbons in which the hydrogen atoms are
replaced by fluorine atoms.
z PFCs are chemically inert due to the strength of the
carbon-fluorine bonds
{ Used to create artificial blood during surgeries
Process of production:
z Water, salts, and phospholipids surfactant are
added and emulsified through high-pressure
homogenization
z Purified through high temperatures of steam
(Goorha et al 47-48).
{ Common PFCs:
z Perfluorodecalin
z Perflubron
{
Types of Blood Substitutes
Perfluorocarbons (PFC) emulsions
•
Oxygenation:
•
Saturation occurs with PFCs passively as oxygen
molecules “dissolve into molecular cavities within
droplets of the liquid” ("Types of Blood Substitutes”)
•
Thus, the oxygenation of PFCs is directly related to
the partial pressure of oxygen which is in contact
with the PFC (See figure below)
"Types of Blood Substitutes." eurobloodsubstitutes.com. 2007. Euro Blood Substitutes. 31 Jul 2007
<http://www.eurobloodsubstitutes.com/pfcInfo.htm>.
Types of Blood Substitutes
Perfluorocarbons (PFC) emulsions
{
Structure:
z
z
Perfluorocarbon core
Surrounded by a
phospholipid
surfactant (Werlin et
al)
{
A surfactant is “a
substance that
reduces the
surface tension of
the liquid in which
it is dissolved”
(Brown, useful
definitions)
http://biomed.brown.edu/Courses/BI108/BI108_2005_Groups/10/webpages/PFCli
nk.htm
Types of Blood Substitutes
Perfluorocarbons (PFC) emulsions
Advantages
Disadvantages
PFCs do not react with oxygen
(Goorha et al 46).
{PFCs allow easy transportation of
the oxygen to the body (Goorha et al
45).
{ they allow increased solubility of
oxygen in plasma (Goorha et al 45).
{PFCs minimize the effects of factors
like pH and temperature in blood
circulation (Goorha et al 45).
often causes flu-like symptoms (Goorha
et al 47).
z this is often caused by
phagocytosis of the perfluorocarbon
emulsion by the recipient organism’s
immune system
{ unable to remain mixed as aqueous
solutions – thus, they must be prepared
as emulsions for use in patients (Werlin et
al)
{ a decrease in blood platelet count
(Werlin et al)
{ PFC products cannot be used by the
human body, and must be discarded Æ
this takes approximately 18-24 months
(Werlin et al)
{ because PFCs absorb oxygen passively,
patients must breathe at a linear rate to
ensure oxygenation of tissues (Euro blood
substitutes).
{
{
Types of Blood Substitutes
Hemoglobin-based Oxygen Carriers (HBOCs)
{
{
Hemoglobin-based Oxygen Carriers were created as a
mechanism to mimic the oxygen-carrying role of hemoglobin
in the body, while still reducing the need for real human
hemoglobin.
Hemoglobin is a tetramer with two alpha and two beta
polypeptide chains; each is bound to an iron heme group
which successively binds to an oxygen molecule
•
Hemoglobin’s heme bond allows it to have a higher affinity for
oxygen, thus making it an excellent source of blood substitutes.
(Goorha et al 46).
Advantages
Disadvantages
{Available
{ reduced circulation half-life
in much larger quantities
{Can be stored for long durations
{Can be administered rapidly without
typing or cross-matching blood types
{Can be sterilized via pasteurization
disrupts certain physiological structures,
especially the gastrointestinal tract and
normal red blood cell hemoglobin.
{ the release of free radicals into the body
{
Types of Blood Substitutes
Hemoglobin-based Oxygen Carriers (HBOCs)
{
{
Currently, experimentation is occurring to develop vesicles which
carry the Hemoglobin before inserting it into the body as an HBOC
There are several advantages to HBOC carrier vesicles
•
•
{
Prevents the denaturation of the Hemoglobin
The vesicles themselves are made of purified Hb and lipids, making
them compatible with the human immune system
Current Setbacks with Hb Vesicle Technology
•
•
•
Materials such as nylon, gelatin, and gum arabic have been tried but
the human immune system, specifically the reticuloendothelial system,
removed the vesicle promptly as a natural bodily response.
Later, the theory of phospholipid vessels was used to create a vesicle
using phospholipids
Researchers are trying to develop a way to create liposome sacks to
carry the HBOCs (Goorha et al)
Types of Blood Substitutes
Goorha, Brig, and Maj Deb. "Artificial Blood." MJAFI 59(2003): 45-49.
Types of Blood Substitutes
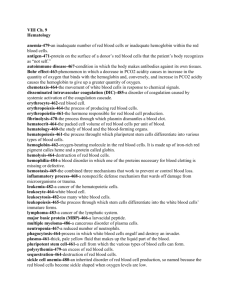
This figure displays the different forms of blood substitutes
that can be used to simulate the actions of a red blood cell
Goorha, Brig, and Maj Deb. "Artificial Blood." MJAFI 59(2003): 45-49.
Researchable Question
Can we make a blood substitute using
Biotechnological techniques?
{
{
In order to create a blood substitute that would effectively
transport oxygen throughout the body, the hemoglobin gene
would have to be inserted in a plasmid vector and multiplied
in a specific medium.
The hemoglobin gene would be inserted into the plasmid to
carry the cloned gene into E. Coli cells
z
This would allow for expression of large amounts of the
hemoglobin protein
Escherichia Coli P678-54
{
The particular strain of the bacteria E. Coli P678-54 has
the unique property of dividing abnormally – it forms a
mother cell and a daughter cell (Marszalone et al 1219)
z
z
The mother cell is similar to a regular cell in that it contains
chromosomal DNA. However, it contains ALL of the cell’s DNA
The daughter cell is achromosomal. It is smaller, and contains
no chromosomal DNA.
{
{
{
The daughter cell is often referred to as a “mini cell”
Because E. Coli P678-54 has the property of dividing
abnormally, it would be ideal if used as a Gene Delivery
Vehicle, or GDV (Cohen et al 64).
Since E. Coli P678-54 has a tendency to divide into
mother cells as well as mini cells, these mini cells could be
ideal for the creation of hemoglobin-based oxygen carriers
(Giacalone et al 1).
Method of HBOC production using E.
Coli P678-54 Mini cells
{
{
In order to produce a hemoglobin-based oxygen carrier using
E. Coli P678-54 mini cells, the hemoglobin gene must be
inserted into the E. Coli bacterium.
The general process to insert hemoglobin into E. Coli cells
uses several techniques of biotechnology:
z
z
z
z
z
z
z
PCR – to assemble the human hemoglobin gene
Western Blotting – to ensure that the substance being
produced really is the Hemoglobin protein
Inoculation – to grow the E. Coli cells after
transformation
Electroporation – to open the E. Coli cell pores and
allow the plasmid vectors containing the Hb gene to enter
Blue/White Screening – to test whether or not the E.
Coli cells have been successfully transformed with the Hb
gene
Gene Transformation – to incorporate the Hb gene into
E. Coli DNA through plasmid vectors
Enzyme digestion – to properly insert the Hb gene into
the plasmid vector containing the lacZ indicator gene
Experimental Design - Materials
{
{
{
{
{
{
Agar gel plate with Ampicillin antibiotic
Plasmids with the lacZ indicator gene
Micropipettes
E. Coli P678-54 cells
Human DNA
Primers (to make complete PCR products of
the human hemoglobin gene)
Experimental Design – Methods
Hemoglobin Gene Preparation
{
Preparation of Hemoglobin
z
z
z
z
z
{
PCR (Polymerase Chain Reaction)
z
{
Obtain and purify hemoglobin DNA
Use primers to cut hemoglobin DNA and remove introns
Use modification methods to ensure that the cell free
hemoglobin does not break down and lose its properties
This newly assembled hemoglobin DNA can be used as a PCR
product
PCR Product:
{ PCR buffer
{ dNTP
{ Hemoglobin primer mix
{ Sterile water
Run the PCR product through a PCR machine
Inserting hemoglobin into plasmid vectors
z
z
Using a plasmid vector with the lacZ indicator gene, we can
insert the hemoglobin DNA along with primers for both ends
so that the hemoglobin can enter the plasmid
This plasmid now contains the recombinant hemoglobin DNA
Experimental Design – Methods
Transformation of E. Coli Cells
{
The plasmid vectors are inserted into E. Coli
P678-54
z
z
{
Insert the plasmid vectors into a solution containing E. Coli
P678-54
Place the solution through “electroporation”: This allows the
plasmid vectors to enter the E. Coli cells by opening up pores
in the E. Coli
Blue/White Screening
z
Once the plasmid vectors have been inserted into the E. Coli
cells, spread the transformed cells onto an agar plate with the
Ampicillin antibiotic
{ White colonies: represent colonies which have
hemoglobin properly inserted into the plasmids Æ the
hemoglobin plasmid has successfully broken the lacZ
gene region
{ Blue colonies: represent colonies which haven’t been
properly transformed: the lacZ gene displays the blue
color; thus, colonies that show the blue color have the
lacZ region still intact, meaning that the hemoglobin gene
has not been incorporated into the region
Experimental Design – Methods
Mini Cell Separation
{
Separation of Mini Cells from normal cells
z
Suspend the solution by microcentrifuging it
{ Mini cells will be suspended higher than the normal cells
as they are less dense
{ Pipette out the supernatant above the mini cells
{ Pipette the mini cells without disturbing the normal E. Coli
cells
Experimental Design – Methods
Testing for Oxygen
{
Testing transformed E. Coli minicells for oxygen
content
z
a simple way to test the transformed mini cells for oxygen
binding to hemoglobin would be to check whether the
cells are red or blue
{
{
z
Oxygenated blood = red
Deoxygenated blood = blue
Check the Hemoglobin Saturation percentage (Wikipedia)
{
{
{
{
This is a sigmoidal (non-linear) function which measures
the partial pressure of oxygen
In a healthy human being, 98.5% of the oxygen is bound
to Hemoglobin, thus making it oxygenated
1.5% of the oxygen is bound to other liquids, making it
inaccessible
How to check
z
Infrared absorption between oxygenated and deoxygenated blood
varies highly, thus allowing hospitals and other clinics to
differentiate between oxygenated blood and deoxygenated blood
Experimental Design – Methods
Hemoglobin Modification Methods
{
Ensuring the stability of hemoglobin
z
z
When hemoglobin is left outside a cell, it has the tendency
to break into its individual parts, instead of remaining as
an entire hemoglobin protein (“Types of Blood
Substitutes”)
Methods have been discovered to retain the stability of
hemoglobin including:
"Types of Blood Substitutes." eurobloodsubstitutes.com. 2007. Euro Blood Substitutes. 31 Jul 2007
Further Research
{
Since hemoglobin has been inserted into E. Coli
cells, the body’s immune system will most likely
develop antibodies to combat the foreign E. Coli
cells that are inserted
z
z
Option 1: the mini cells could be packaged in a liposome to
trick the immune system (Li 3761).
Option 2: we could find the gene in E. Coli that stimulates the
production of antibodies and use gene silencing techniques to
turn the gene off
Works Cited
{
{
{
{
Cohen, Amikam and W. D. Fisher. "DNA Isolated from Escherichia
Coli Minicells Mated with F+ Cells." Proceedings of the National
Academy of Sciences of the United States of America 61 (1968)
61-68. 17/07/2007.
Giacalone , Matthew, and Gentile, Angela, and Lovitt, Brian, and
Xu, Tong, and Sabbadini, Roger, and Surbur, Mark. "The Use of
Bacterial Minicells to transfer Plasmid DNA to eukaryotic cells."
Cellular Microbiology 8 (2006) 1624-1633. 16/07/2007
<www.blackwell-synergy.com/doi/pdf/10.1111/j.14625822.2006.00737.x>.
Goorha, Brig, and Maj Deb. "Artificial Blood." MJAFI 59(2003):
45-49.
Li, Shuliang. "Liposome-encapsulated actin–hemoglobin (LEAcHb)
artificial blood substitutes." Biomaterials 26June 2005 3759-3769.
<http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B
6TWB-4DN13MC1&_user=4421&_coverDate=06%2F01%2F2005&_rdoc=1&_fmt=
&_orig=search&_sort=d&view=c&_acct=C000059598&_version=
1&_urlVersion=0&_userid=4421&md5=795149aeb4f49af0ef50ad
656ed4c02a>.
Works Cited
{
{
{
{
{
{
{
Marszalek, Piotr and Tian Tsong. "Cell Fission and Formation of
Mini Cell Bodies by High Frequency Alternating Electric Field."
Biophysical Journal 68 April 1995 1218-1221. 17/07/2007.
Nobel Foundation, "Karl Landsteiner." Nobelprize.org. 2007.
Nobel Foundation. 31 Jul 2007
<http://nobelprize.org/nobel_prizes/medicine/laureates/1930/lan
dsteiner-bio.html>.
“Ringer's solution." Encyclopedia Britannica. 2007. Encyclopedia
Britannica Online.
23 July 2007 <http://www.britannica.com/eb/article-9063724>.
Squires, Jerry E. "Artificial Blood." Science 295February 2002
1002-1005. 17/07/2007
<http://www.sciencemag.org/cgi/content/full/295/5557/1002>.
"Types of Blood Substitutes." eurobloodsubstitutes.com. 2007.
Euro Blood Substitutes. 31 Jul 2007
<http://www.eurobloodsubstitutes.com/pfcInfo.htm>.
Werlin, Evan. "Current Synthetic Blood Products."
biomed.brown.edu. April 2005. Brown University. 31 Jul 2007
http://biomed.brown.edu/Courses/BI108/BI108_2005_Groups/10
/webpages/PFClink.htm
Wikipedia, "Blood." Wikipedia.com. July 2007. Wikipedia. 31 Jul
2007 <http://en.wikipedia.org/wiki/Blood>.