Organ Donor Management: Survey of Guidelines and Eligibility
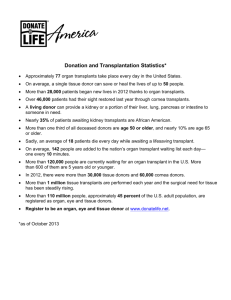
advertisement

Organ Donor Management: Survey of Guidelines and Eligibility Criteria Prepared for the Forum: Medical Management to Optimize Donor Organ Potential February 23-25, 2004 by Lead Investigator Sam D. Shemie, MD, Chair, on behalf of the MEMODOP Steering Committee Coordinator Karen Hornby Montreal Children’s Hospital Contents Acknowledgements ...................................................................................................................v Executive Summary ..................................................................................................................1 I. Survey of Canadian and Selected International Organ Donor Management Guidelines and Eligibility Criteria.......................................................................................8 Methodology for Data Gathering and Inclusion ...............................................................8 Survey Responses............................................................................................................8 II. Analysis of Canadian Management Guidelines Received ..........................................10 Oxygenation and Ventilation .........................................................................................10 Organ Perfusion ............................................................................................................11 Fluid Balance and Electrolytes ......................................................................................13 Hematology...................................................................................................................17 Temperature ..................................................................................................................17 Infection........................................................................................................................18 Additional Treatments ...................................................................................................18 III. Canadian Donor Organ Eligibility Criteria ....................................................................20 OPO Organ Donor Eligibility Criteria ...........................................................................20 IV. International Issues in Organ Donor Management.........................................................21 V. Conclusion ..........................................................................................................................24 Appendix I – Canadian Organ Procurement Organizations ................................................25 Appendix II – Spanish Guidelines..........................................................................................27 Appendix III — UNOS Critical Pathway ..............................................................................32 Appendix IV – New England Organ Bank.............................................................................39 Appendix V – Papworth approach.........................................................................................45 Appendix VI – Leuven University Hospital ...........................................................................48 References ...............................................................................................................................52 iii Acknowledgements The Steering Committee for the Forum on Medical Management to Optimize Donor Organ Potential (February 23-25, 2004) commissioned this paper, a working draft, as a background information piece for participants attending the Forum. During the Forum, consideration will be given to editing this working draft for wider circulation. The views of the paper do not necessarily reflect the official policy of the Forum host, the Canadian Council for Donation and Transplantation, and are not intended for publication in their current format. iv Executive Summary This report summarizes the results of a survey of Canadian intensive care units, organ procurement organizations (OPOs) and transplant associations. The survey requested copies of organ donor management guidelines and eligibility criteria. Selected international OPOs were also contacted, and a brief summary of their activities is included. This research was conducted in preparation for the Canadian Forum on Medical Management to Optimize Donor Organ Potential, sponsored by the Canadian Council for Donation and Transplantation (CCDT). Canadian Donor Management Guidelines Half of the pediatric centers and 43% of the adult centers surveyed stated that they used their OPO’s guidelines. All OPOs stated that they were involved (to varying degrees) in organ donor management at intensive care units within their respective provinces and provided these units with OPO guidelines. The intent of the survey was to identify existing guidelines; the survey was not intended to assess the utilization of these documents (i.e., if guidelines were actually in use and how many sites were using them). As a result, this analysis is based on 17 unique documented guidelines. (Refer to the tables on pages 3 and 4). Canadian Donor Organ Eligibility Criteria Donor organ eligibility is not an intensive-care-based responsibility according to the centers surveyed. All hospital centers (except one) referred decisions to determine eligibility to their respective OPOs. Ten OPOs provided information on donor organ eligibility criteria. One OPO currently addresses eligibility by encouraging all centers to refer potential organ donors to it, stipulating that the only contraindication is HIV/AIDS. Six OPOs stated that “eligibility was assessed on a case by case basis”; three of these provided absolute contraindications. One OPO provided a draft protocol (approval is outstanding, and the protocol is therefore not included in the analysis). Another OPO uses the Canadian Standards (tissue and organ donation), and its only absolute contraindication is West Nile virus. One OPO cited that it “looks at everything … and then consults with individual transplant programs”. International Issues in Organ Donor Management Worldwide, organ donation and the medical management of organ donors is at various stages of development. Among the countries with mature systems in this field, recent efforts have been on optimizing medical management to maximize organ yield. Refer to pages 6 and 7 for management details. Countries at the forefront of this movement are Spain, the United States, the United Kingdom, Australia and members of Eurotransplant. Spain The Spanish Model consists of a team of specially trained individuals (physicians and nurses) separate from the medical/transplant teams who are responsible for raising the donor rate in all hospitals. Among other things, these teams identify all potential donors and handle the evaluation and management of the donor. 1 United States The United Network for Organ Sharing has developed a Critical Pathway for the Organ Donor, endorsed by the Association of Organ Procurement Organizations, the American Society of Transplantation, the American Society of Transplant Surgeons and the North American Transplant Coordinators Organization. United Kingdom A standardized donor management technique was developed at the Papworth Hospital in Cambridge, England. Details on the Papworth approach to organ donor management will be provided in a separate presentation. Australia South Australia adopted the Spanish Model and experienced a significant increase in its donor rate compared to other states. As well, the Alfred Hospital in Melbourne has developed a successful system of transplant coordination and organ allocation. Its system is considered a good example of the Australian approach. Eurotransplant Eurotransplant is an international framework including all transplant hospitals, tissue-typing laboratories and hospitals where organ donation takes place in Austria, Belgium, Germany, Luxembourg, the Netherlands and Slovenia. The Leuven University Hospital in Belgium has developed a secure-access website containing organ donation information and protocols. This website is accessible to all members of their donor hospital network. Since its implementation, a substantial increase in donors has occurred. 2 Summary table 1. Canadian organ donor management guidelines Respiratory Targets O2 sat (%) FiO2 (%) PaO2 (mm Hg) PCO2 (mm Hg) pH Lower limit pH Upper limit PEEP (mm Hg) TV lower limit (ml/kg) Peak airway pressure (mm Hg) Hemodynamic MAP Electrolytes Serum sodium Lower (mmol/L) Upper Serum potassium Lower (mEq/L) Upper < 50 85 N/Ab 7.35 7.45 5 9 ≤ 30 GLa 10 6 3 10 9 8 8 6 9 4 ≥ 70 N/A > 100 N/A ≥ 60 ≤ 120 N/A 6 10 8 10 5 3 7 2 5 7 2 15 12 3 3 125–130 ≤ 150 – ≤ 155 130 ≤ 150 5 6 > 3.0 – > 4.0 < 4.5 – < 5.5 > 3.5 < 5.5 6 5 Range ≥ 90 – ≥ 96 “any value to maintain O2 sat” < 40 – < 60 65–100 35–45 7.30–7.35 7.45 4–7.5 5–12 ≤ 30 Adults (mm Hg) Peds Adults (mm Hg) Peds Adults (bpm) ≥ 70 age adjusted SBP > 90 – > 100 age adjusted HR ≥ 60–70 ≤ 110 – ≤ 160 Peds age adjusted CVP (mm Hg) ≥ 4–7 ≤ 8–12 PCWP Lower (mm Hg) 8 Upper 10–12 Median ≥ 95 Urine Output Adults Lower (ml/h) Upper Peds Lower (ml/kg/h) Upper ≥ 30 – ≥ 120 ≤ 180 – ≤ 300 1–2 2–3 ≥ 100 ≤ 250 1 2 9 6 5 5 Diabetes Insipidus (DI) Adults U/O (ml/h) Osmol (mOs/L) Na+ (mmol/L) SG Serum osmol Peds U/O (ml/kg/h) Osmolality Na+ (mmol/L) SG Serum osmol > 180–400 < 300 < 10 ≤ 1.000 > 300 mOs/kg & _ >4–>5 “low” > 145 < 1.000 – < 1.010 “high” > 240 < 300 < 10 ≤ 1.000 > 300 mOs/kg & _ > 4 ml “low” > 145 <1.005 “high” 9 2 2 1 2 4 1 2 3 1 Blood Sugar Lower limits (mmol/L) Upper limits 4–8 10–20 6 12 5 6 3 Summary table 1. Canadian organ donor management guidelines (cont’d) Insulin Adults (U/h) Peds (U/kg/h) 0.5 –1 0.025–0.1 0.75 0.025 2 3 Hematology Hematocrit (%) Hemoglobin (g/dL) 20–35 8–12 30 9 6 3 Temperature Lower limit (°C) Upper limit 35–36.5 37–38 35.3 37.5 14 11 Invasive Monitoring Arterial line Central venous line Pulmonary artery catheterization Cardiovascular Support Dopamine (max dose) (µg/kg/min) Norepinephrine Lower (µg/min) Upper Epinephrine Lower (µg/min) Upper Vasopressin Lower (U/h) Upper Percentage 93% 100% 53% Range 10–15 0.6–3 36–60 0.6–3 36–60 1.1–3 2.4–6 Median < 10 1.2 48 1.8 48 1.2 4.2 GLa 15 15 15 GLa 11 3 2 2 2 3 2 Desmopressin Suggested Dosages to Treat DI Adults Pediatrics 1 µg q6h prn intranasal (no dose indicated) 1 µg push _ 2 0.25–1 µg per dose 1–2 µg push 5–10 µg ETT or 0.25–4 µg IV 2 µg infuse over 30 minutes (2 guidelines) 1–4 µg IV, IM or SC q12–24h prn 2–4 µg q4–6h or 1 µg/h infusion 2 µg, then 4 µg repeat as needed 4 µg q2h _ 2 call MD if 3rd dose required (2 guidelines) Vasopressin Suggested Dosages to Treat DI Adults 1 U/h, titrate to target u/o 2 U bolus, 1 U/h titrate to target u/o (2 guidelines) 2.5–5 units IV q4h Antibiotics One hour prior to OR: Or if hospital > 72 hrs AND Pediatrics 0.5–3 mU/kg/h 5–15 mU/kg/h (2 guidelines) 6–15 mU/kg/h cefazolin IV Adults: 1 gm (n = 1) cefotaxime IV Adults: 1 gm (n = 1) metronidazole IV Adults: 500 mg (n = 1) Corticosteriods The following dosages were suggested: 10 mg/kg, max 1g (n = 1) 15 mg/kg, max 1g (n = 2) 1 g IV _ 1 (n = 3) 4 Peds: 30 mg/kg, max 1gm (n = 2) Peds: 40 mg/kg, max 1 gm (n = 2) Peds: 15 mg/kg, max 500 mg (n = 2) Summary table 1. Canadian organ donor management guidelines (cont’d) Hormonal Therapy One guideline suggested: methylprednisolone: 15 mg/kg IV (not to exceed 1 gm) insulin infusion: 0.5–1.0 U/h starting dose T4: 40 µg bolus IV _ 1 desmopressin infusion: 1µg/h Investigations Supportive Testing Chest x-ray 82% Electrocardiogram 71% Echocardiogram 65% Bronchoscopy 41% Cardiac angiogram 24% Cardiology consult 18% a Number of guidelines that provided target values for variable of interest. b N/A = not applicable 5 Summary table 2. International organ donor management guidelines The following details have been extracted from guidelines provided by the Organización Nacional de Trasplantes (Spain), the United Network for Organ Sharing (U.S.), the Papworth Hospital (U.K.) and the Leuven University Hospital (Belgium). Targets O2 sat (%) FiO2 (%) PaO2 (mm Hg) PCO2 (mm Hg) pH PEEP (cm H20) Spain 95–100 up to 100 90–100 35–45 7.35–7.45 5 U.S. ≥ 95 up to 100 ≥ 90 30–35 N/A 5 U.K. > 98% min for sat ~ 264 @ 50% 35–45 N/A 5 Belgium N/Aa min for PaO2 100 35–45 7.35–7.45 5 Respiratory TV (ml/kg) Peak airway pressure (mm Hg) 8–10 < 30 10–15 < 30 15 N/A 15 N/A Hemodynamic MAP SBP (mm Hg) HR (bpm) CVP (mm Hg) PCWP (mm Hg) SVR (dynes/sec/cm5) N/A ≥ 100 ≤ 100 10–12 8–14 ≥ 60 ≥ 90 ≥ 70 – ≤ 120 4–11 8–12 800–1200 > 60 N/A N/A < 12 < 12 800–1200 > 70 N/A N/A 8–10 N/A N/A Electrolytes Serum Na (mEq/dl) Serum K+ (mEq/dl) N/A N/A < 150 > 4.0 N/A N/A N/A N/A Urine Output Adults (ml/kg/h) Peds (ml/kg/h) >1 >2 ≥1–≤3 N/A N/A N/A ≥ 1– ≤ 3 N/A DI U/O (ml/kg/h) Osmolality Na+ SG Serum osmol N/A N/A N/A N/A N/A >3 N/A N/A N/A N/A N/A N/A N/A N/A N/A >3 N/A N/A N/A N/A Blood Sugar (mg/dl) 150 120–180 70–115 (4–6 mmol/L) N/A Insulin no doses given see HRT see HRT see HRT ≥ 30 ≥ 30 ≥ 35 multi-organ 10–12 ≥ 10 N/A ≥ 30 > 10 ≥ 11 Temperature (°C) > 35 36.5–37.5 N/A > 35 Invasive Monitoring Arterial line Central venous line Pulmonary artery catheterization yes yes yes yes yes yes yes yes yes yes yes yes Respiratory Hematology Hematocrit (%) Hemoglobin (g/dl) 6 Summary table 2. International organ donor management guidelines (cont’d) Cardiovascular Support Dopamine (max dose) (µg/kg/min) Norepinephrine Epinephrine Vasopressin ≤ 10 no dose given no dose given N/A < 10 N/A N/A see HRT ≤ 10 N/A N/A see HRT ≤ 10 N/A N/A N/A Desmopressin Suggested Dosages (to treat DI) no dose given N/A N/A 2–4 µg (max 6) Vasopressin Suggested Dosages (to treat DI) N/A see HRT see HRT N/A Antibiotics prophylactic use broadspectrum vancomycin 1 g on basis of meropenem 1 g cultures Corticosteriods N/A see HRT 500 mg see HRT methylprednisolone Hormonal Therapy T3 N/A 4 µg bolus, 3 µg/h same as US Vasopressin/Pitressin N/A 1 U bolus, 0.5–4.0 U/hb Steroids N/A methylprednisolone 15 mg/kg bolus q24h 1 U bolus, 0.5–2.0 U/h N/A Insulin N/A min 1 U/hc sliding scale Investigations/Supportive Testingd Chest x-ray N/A yes no Electrocardiogram N/A yes yes Echocardiogram N/A yes yes Bronchoscopy N/A yes yes Cardiac angiogram N/A yes yes Cardiology consult N/A yes yes a N/A = not applicable b Titrate to SVR. c Titrate to blood glucose. d These may be mentioned in sections on donor organ evaluations that were not provided. 7 2–4 µg in 1h, then 1.8 u/h N/A hydrocortisone 3 _ 200 mg/24h up to 600 mg 1–2 U/h no yes no no no no I. Survey of Canadian and Selected International Organ Donor Management Guidelines and Eligibility Criteria This report summarizes the results of a survey of Canadian intensive care units, organ procurement organizations (OPOs) and transplant associations. The survey consisted of a request for organ donor management guidelines and eligibility criteria. Documents were received from three categories of institutions: adult centers, pediatric centers and provincial OPOs. Selected international OPOs were also contacted, and a brief summary of their activities relating to organ donor management is included. This research was conducted in preparation for the Canadian Forum on Medical Management to Optimize Donor Organ Potential, sponsored by the Canadian Council for Donation and Transplantation (CCDT). Methodology for Data Gathering and Inclusion A total of 55 centers were contacted across Canada. Twelve OPOs responded, and two provided pediatric guidelines in addition to adult ones. (See Appendix I for further details on provincial differences in OPOs.) Adult intensive care units in all major Canadian cities as well as all Canadian pediatric intensive care units were contacted. Table 1 categorizes their responses. Table 1. Canadian centers contacted/responded Centers Contacted (n = 55) No. Responses OPOSs 14 Adult centers 21 Pediatric centers 16 Canadian Association of Transplantation N/Aa Canadian Society of Transplantation N/A Other (Yukon, P.E.I.) N/A a N/Aa = not applicable Survey Responses Table 2 breaks down the survey responses by type of center and guidelines used. Half of the pediatric centers and 43% of the adult centers surveyed stated that they used their OPO’s guidelines. All OPOs stated that they were involved (to varying degrees) in organ donor management at intensive care units within their respective provinces and provided these units with OPO guidelines. Some OPOs provided lists of intensive care units within their provinces. The intent of the survey was to identify existing guidelines; the survey was not intended to assess the utilization of these documents (i.e., if guidelines were actually in use and how many sites were using them). Therefore, only unique guideline documents were entered into the study database. 8 Table 2. Breakdown of survey responses Guidelines Uses No Guidelines Provided OPO’s Documented Adult center 24% (5/21) 43% (9/21) 33% (7/21) Pediatric center 25% (4/16) 50% (8/16) 25% (4/16) OPO 64% (9/14)a N/Ab 36% (5/14) a One pediatric guideline not included, as it was based on a hospital guideline already analysed. b na = not applicable For a variety of reasons, 16 centers did not provide guidelines: no guidelines available (n = 8); management is at MD discretion (n = 5); management is on a case-by-case basis (n = 1); guidelines are in draft format and not yet approved (n = 1); unable to locate (n = 1). As a result, this analysis is based on 17 unique documented guidelines. All guidelines were for multi-organ management in the following formats: documents (n = 9), standing orders (n = 5), algorithms (n = 2) and pamphlet (n = 1). Many guidelines did not address all the variables of interest to this study; therefore, percentages in the following sections are based on the number of guidelines that addressed those particular issues of interest. 9 II. Analysis of Canadian Management Guidelines Received Oxygenation and Ventilation Oxygenation and ventilation management includes respiratory targets, the use of the O2 challenge test and lung treatments. Respiratory targets There was agreement among the guidelines for a majority of the respiratory management targets (table 3). Discord occurred in the areas of PaO2 and tidal volume targets, with a variety of values cited. O2 challenge Ten guidelines mentioned the use of the O2 challenge test, with some variations. All cited using an FiO2 of 100% with a PEEP of 5 mm Hg and a predetermined delay before blood is drawn for arterial blood gases (ABGs). Recommended tidal volumes and delay prior to ABG measurement varied. Only two guidelines identified desirable PaO2 targets (≥ 300 mm Hg and ≥ 250 mm Hg) for the O2 challenge. Lung treatments Suctioning frequencies (n = 6) were either q2h (n = 4), q3–4h (n = 1) or prn only (n = 1). Other lung treatments suggested were repositioning (n = 4), chest physiotherapy (n = 2), postural drainage (n = 1) and manual lung inflation (n = 1). Table 3. Respiratory management targets Targets O2 sat FiO2 PaO2 PCO2 pH Lower limit Upper limit PEEP TV (lower limit) Peak airway pressure a Range Median ≥ 90% – ≥ 96% ≥ 95% “any value to maintain O2 sat” < 40% – < 60% < 50% 65–100 mm Hg 85 mm Hg 35–45 mm Hg 35–45 mm Hg 7.30–7.35 7.35 7.45 7.45 4–7.5 mm Hg 5 mm Hg 5–12 ml/kg 9 ml/kg ≤ 30 mm Hg ≤ 30 mm Hg Number of guidelines that provided target values for variable of interest. 10 GLa 10 6 3 10 9 8 8 6 9 4 Organ Perfusion Organ perfusion management includes target pressures, invasive monitoring and cardiovascular support. Target pressures Table 4 outlines the hemodynamic management targets. Not unexpectedly, most pediatric guidelines indicated age-adjusted values for these targets. Table 4. Hemodynamic management targets Targets MAP Adults Peds SBP Adults Peds HR Adults Peds CVP PCWP Lower limit Upper limit a Range ≥ 70 mm Hg age adjusted > 90 – > 100 mm Hg age adjusted ≥ 60–70 bpm ≤ 110 – ≤ 160 bpm age adjusted ≥ 4–7 mm Hg ≤ 8–12 mm Hg 8 mm Hg 10–12 mm Hg Median ≥ 70 mm Hg N/Ab > 100 mm Hg N/A ≥ 60 bpm ≤ 120 bpm N/A 6 mm Hg 10 mm Hg 8 mm Hg 10 mm Hg GLa 5 3 7 2 5 7 2 15 12 3 3 Number of guidelines that provided target values for variable of interest. N/A = not applicable b One pediatric guideline provided age-adjusted values for the central venous pressure target. Only one guideline (adult) mentioned targets for systemic vascular resistance (800–1200 dynes/sec _ cm5), cardiac index (2.4–3.0) and left ventricular stroke volume (1800–2400 dynes/sec _ cm5). Invasive monitoring Standard care for invasive monitoring consists of an arterial line and a central venous line. Five guidelines gave instructions for placement in specific anatomical locations. Table 5 breaks down the types of invasive monitoring identified. Table 5. Invasive monitoring Arterial line Central venous line Pulmonary artery catheterization a Percentage 93% 100% 53% Number of guidelines that referred to invasive monitoring. 11 GLa 15 15 15 The indications for pulmonary artery catheterization were heart/lung donors, or management difficulties or both (n = 5), desirable (n = 2) and absolutely necessary (n = 1). One pediatric guideline suggested the use of an intra-osseous line if access was difficult. Cardiovascular support Eighty-two percent of the guidelines provided suggestions for the use of inotropes or vasopressors. In a majority of cases (n = 9), adequate fluid resuscitation prior to starting any inotrope or vasopressor was indicated. Dopamine is the drug of choice in 59% of the guidelines. Indications for the use of other vasopressors varied greatly: “avoid if possible” (n = 3), “as an option” (n = 1) and “as required” (n = 1). Table 6 summarizes the dosing information provided. In most cases, these drugs were used in addition to dopamine. Table 6. Inotropes and vasopressors Drug Dopamine (maximum dose) Norepinephrine Lower Upper Epinephrine Lower Upper Vasopressin Lower Upper a Range 10–15 µg/kg/min 0.6–3 µg/min 36–60 µg/min 0.6–3 µg/min 36–60 µg/min 1.1–3 U/h 2.4–6 U/h Median 10 µg/kg/min 1.2 µg/min 48 µg/min 1.8 µg/min 48 µg/min 1.2 U/h 4.2 U/h GLa 11 3 2 2 2 3 2 Number of guidelines that provided target values for variable of interest. Only 35% of guidelines mentioned the use of short-acting antihypertensives. The following drugs were identified: nitroprusside (n = 4), labetalol (n = 3), propranolol (n = 2) and nitroglycerin (n = 1), with some guidelines identifying more than one drug. Only two guidelines provided dosing information. Both indicated 1–2 mg propranolol IV push, and one provided an alternative of 5–10 mg labetalol IV. 12 Fluid Balance and Electrolytes Fluid and electrolyte management requires attention to IV fluids, electrolytes and fluid balance, including monitoring for diabetes insipidus. IV fluids All guidelines provided indications for the use of intravenous fluids, with a variety of suggestions for the type of fluid used, the quantity and fluid management targets. Seven guidelines based the decision of which fluid to use on electrolyte laboratory values, four of which were specifically based on serum sodium values. Both crystalloids (n = 8) and colloids (n = 6) were indicated for volume expansion. Two guidelines targeted specific levels of urine output as their fluid management strategies, and three guidelines targeted pressures (MAP or CVP). One guideline recommended avoiding the use of Ringer’s lactate. The same guideline contraindicated the use of plasma, hetastarch and Pentaspan (pentastarch) for organ donors. One other guideline had a contraindication for the use of Pentaspan, and five guidelines recommended its use. Electrolytes Fifty-three percent of guidelines surveyed indicated the importance of strict monitoring and correction of electrolyte imbalances. Six centers provided target values for serum sodium and potassium (table 7). Table 7. Electrolyte targets Range Median GLa Serum sodium Lower limit Upper limit 125–130 mmol/L ≤ 150 – ≤ 155 mmol/L 130 mmol/L ≤ 150 mmol/L 5 6 Serum potassium Lower limit Upper limit > 3.0 – > 4.0 mEq/L < 4.5 – < 5.5 mEq/L > 3.5 mEq/L < 5.5 mEq/L 6 5 a Number of guidelines that provided target values for variable of interest. 13 Fluid balance All centers identified upper and lower urine output targets. Table 8 details these values. Table 8. Target urine outputa Adults Lower limit Upper limit Peds Lower limit Upper limit Range ≥ 30 – ≥ 120 ml/h ≤ 180 – ≤ 300 ml/h 1–2 ml/kg/h 2–3 ml/kg/h Median ≥ 100 ml/h ≤ 250 ml/L 1 ml/kg/h 2 ml/kg/h GLb 9 6 5 5 a When urine output for adults was provided in ml/kg/h, it was converted into ml/h based on an average adult weight of 60 kg. b Number of guidelines that provided target values for variable of interest. Diabetes insipidus Diagnosis. Ninety-four percent of guidelines provided instructions for the management of urine output, with 88% suggesting the use of antidiuretics. A definition of diabetes insipidus (DI) was provided by 76% of guidelines. Urine output limits for DI are presented in table 9. Table 9. Indicators of DIa Adults Urine Output Osmolality Na+ SG Serum osmolality Pediatrics Urine Output Osmolality Na+ SG Serum osmolality Range Median GLb > 180–400 ml/h < 300 mOs/L < 10 mmol/L ≤ 1.000 > 300 mOs/kg and rising > 240 ml/h < 300 mOs/L < 10 mmol/L ≤ 1.000 > 300 mOs/kg and rising 9 2 2 1 2 > 4 – > 5 ml/kg/h “low” > 145 mmol/L < 1.000 – < 1.010 “high” > 4 ml/kg/h “low” > 145 mmol/L <1.005 “high” 4 1 2 3 1 a When urine output for adults was provided in ml/kg/h, it was converted into ml/h based on an average adult weight of 60 kg. b Number of guidelines that provided target values for variable of interest. 14 Therapy. All of the guidelines that recommended using antidiuretics to treat DI suggested using desmopressin, with a variety of doses and methods. Two guidelines indicated that desmopressin was preferred over vasopressin to treat DI. Fifty-nine percent provided information on the use of vasopressin. One guideline indicated that its use should be avoided, and another suggested contacting the transplant team prior to use for extra-renal organ donors. One pediatric guideline recommended the use of vasopressin if the donor was not hemodynamically stable; otherwise, desmopressin was indicated. When vasopressin was recommended, three guidelines indicated that it had to be discontinued 1 h prior to OR (n = 1), 1–2 h prior to OR (n = 1) or 2 h prior to OR (n = 1). Tables 10 and 11 list the recommended dosages. Table 10. Desmopressin: Suggested dosages Adults Pediatrics 1 µg q6h prn intranasal (no dose indicated) 1 µg push _ 2 0.25–1 µg per dose 1–2 µg push 5–10 µg ETT or 0.25–4 µg IV 2 µg infuse over 30 minutes (2 guidelines) 1–4 µg IV, IM or SC q12–24h prn 2–4 µg q4–6h or 1 µg/h infusion 2 ug, then 4 µg repeat as needed 4 µg q2h _ 2 call MD if 3rd dose required (2 guidelines) Table 11. Vasopressin: Suggested dosages Adults 1 U/h, titrate to target u/o 2 U bolus, 1 U/h titrate to target u/o (2 guidelines) 2.5–5 units IV q4h Pediatrics 0.5–3 mU/kg/h 5–15 mU/kg/h (2 guidelines) 6–15 mU/kg/h Oliguria diagnosis and therapy Only 24% of guidelines provided indications on oliguria. Each of these suggested the use of diuretics to treat oliguria. Three specifically identified using furosemide to treat a urine output of < 50 ml/h, ensuring a corrected central venous pressure and blood pressure prior to its use. The remaining guideline defined oliguria as a urine output of < 50 ml/h with a CVP of > 12 mm Hg, with no indication of treatment. 15 Glucose Seventy-one percent of guidelines provided information on regulation of blood sugar (BS). The use of insulin to maintain target BS was identified in 65% of guidelines. Two of these suggested that insulin be used with caution for increased BS as potassium boluses may be required prior to insulin use. Two adult guidelines recommended a sliding scale for insulin infusions (no dosages given), and two others simply indicated “insulin drip”. All titrated dosages to meet target BS levels; however, many did not provide target parameters. Table 12 outlines the target values provided for BS and insulin dosages. Table 12. Regulation of blood sugar BS Targets Lower limits Upper limits Insulin Dosages Adults Pediatrics a Range Median GLa 4–8 mmol/L 10–20 mmol/L 6 mmol/L 12 mmol/L 5 6 0.5 –1 U/h 0.025–0.1 U/kg/h 0.75 U/h 0.025 U/kg/h 2 3 Number of guidelines that provided target values for variable of interest. 16 Hematology Sixty-five percent of guidelines referred to the use of blood products. Six of these identified the use of packed red blood cells; of these, four indicated this was to maintain a target hematocrit, one that it was to maintain a target hemoglobin and one indicated no target. Three guidelines provided a general comment concerning the use of blood products, such as “treat coagulopathies”. Three others identified the use of whole blood to maintain either a target hematocrit (n = 2) or a circulating blood volume (n = 1). Other blood products mentioned were fresh frozen plasma (n = 3), platelets (n = 2) and cryoprecipitate (n = 1). Only one guideline specified the use of CMV negative-only products. Table 13 lists hematocrit and hemoglobin targets. Two guidelines linked their hematocrit targets to specific organs: ≥ 20% for kidney donors or ≥ 30% for heart or liver donors. Table 13. Hematocrit and hemoglobin targets Hematocrit Hemoglobin a Range 20–35% 8–12 g/dL GLa 6 3 Median 30% 9 g/dL Number of guidelines that provided target values for variable of interest. Temperature Targets All but one guideline mentioned the importance of body temperature control. When the method for temperature measurement was identified (n = 8), 63% indicated that temperatures should be measured rectally. Table 14 summarizes body temperature targets. Table 14. Body temperature targets Lower limit Upper limit a Range 35–36.5° C 37–38° C GLa 14 11 Median 35.3° C 37.5° C Number of guidelines that provided target values for variable of interest. Methods to maintain temperature Various methods to maintain body temperature within target limits were suggested (n = 16): warming blankets (75%), warming IV fluids (43%), warming inspired gases (25%), heating lamps (13%) and cooling blankets (13%). Other guideline-specific suggestions to maintain target body temperatures were ambient room temperature, hats, socks, Bair huggers and uncovering the patient. 17 Infection Only 35% of guidelines mentioned antibiotic use. Of these, 2 had general comments: “antibiotherapy indicated” and “discuss with transplant coordinator”. One guideline suggested broad spectrum antibiotics, and three had very specific indications for antibiotic use: “1 hour prior to OR: cefazolin IV (1 gm adults, 30 mg/kg peds to max 1gm) or if in hospital > 72 hrs, cefotaxime IV (1 gm adults, 40 mg/kg peds to max 1 gm), and metronidazole IV (500 mg adults, 15 mg/kg max 500 mg peds).” Additional Treatments Corticosteroids Only 35% of guidelines suggested the use of methylprednisolone. Three guidelines indicated its use for lung donors, and another guideline stated, “it contributes to stability and improved oxygenation”. The following dosages were provided: • 10 mg/kg, max 1g (n = 1) • 15 mg/kg, max 1g (n = 2) • 1 g IV _ 1 (n = 3) Hormone therapy Only 1 guideline mentioned the use of hormonal replacement therapy. It consisted of the following: • methylprednisolone: 15 mg/kg IV (not to exceed 1 gm) • insulin infusion: 0.5–1.0 U/h starting dose • T4: 40 µg bolus IV _ 1 • desmopressin infusion: 1µg/h This therapy was indicated to “to replace the loss of hypothalamic function and to maintain cell metabolism”. 18 Investigations/Supportive Testing Supportive investigations required during the management of organ donors is detailed in table 15. Table 15. Supportive testing Chest x-ray % of GL 82% Electrocardiogram Echocardiogram 71% 65% Bronchoscopy 41% Cardiac angiogram Cardiology consult 24% 18% a Indicationsa Lung donors (n = 5) Heart donors (n = 1) Heart donors (n = 1) Heart donors (n = 5) Tx coordinator request (n = 1) Lung donors (n = 4) Tx coordinator request (n = 1) N/Ab N/A When mentioned. N/A = not applicable b 19 III. Canadian Donor Organ Eligibility Criteria Information on donor organ eligibility criteria was obtained using the same methodology as that used to obtain donor organ management guidelines (see “Methodology for Data Gathering and Inclusion”, page 3). According to the centers surveyed, donor organ eligibility is not an intensive-care-based responsibility. One adult center provided donor organ eligibility criteria. All other hospital centers refer decisions to determine eligibility to their respective OPOs. OPO Organ Donor Eligibility Criteria Ten OPOs provided information on donor organ eligibility criteria. One provided a detailed document outlining eligibility criteria for individual organs as well as donor-specific contraindications. This document was dated 1993, and the OPO explained that it currently assesses eligibility by encouraging all centers to refer potential organ donors to the OPO, stipulating that the only contraindication is HIV/AIDS. Six OPOs stated that “eligibility was assessed on a case by case basis”. Three of these also provided a list of absolute contraindications (table 16). One OPO provided a draft protocol for organ donor eligibility; however, approval is outstanding, and the protocol is therefore not included in this analysis. Another OPO indicated it uses the Canadian Standards for tissue and organ donations, and its only absolute contraindication is West Nile virus. One final OPO indicated that it “looks at everything and does a medical assessment, and then consults with individual transplant programs”. Table 16. Absolute contraindications to donor eligibility Positive tests for anti-HIV-1 or anti-HIV-2 hepatitis B or C human T-cell lymphotropic viruses types I and II History or evidence of HIV high-risk behaviours, even if HIV-antibody negative Death with neurological disease of an unestablished etiology (i.e., ALS, Alzheimer’s, multiple sclerosis, Parkinson’s) Prion-related disease (i.e., CJD, family hx CJD, recipient of human-derived pituitary growth hormone or dura mater) Active systemic bacterial, viral or fungal infections Rabies Leukemias, lymphomas and active malignancies Progressive multi-focal leukoencephalopathy Subacute sclerosing panencephalopathy 20 IV. International Issues in Organ Donor Management Worldwide, organ donation and the medical management of organs donors are at various stages of development. Among the countries with mature systems in this field, recent efforts have focused on optimizing the medical management of organ donors to maximize organ yield per potential donor. Countries such as Spain, the United States, the United Kingdom, Australia and members of Eurotransplant (comprising Austria, Belgium, Germany, Luxembourg, the Netherlands and Slovenia) are at the forefront of this movement. Nonetheless, standardized international donor management strategies remain elusive. According to Leo Roels, Scientific Program Director of the International Transplant Coordinators Society, “Organ exchange organizations and organ procurement organizations may have some guidelines, but at the bottom end it’s the ICU physician who will decide upon how to treat a potential donor.”1 He also highlighted recent efforts by the North American Transplant Coordinators Organization and Donor Action Foundation to encourage standardization; the former edited Donor Management Issues, published by D.J. Powner, and the latter is developing an international e-learning course on donor management. Spain The Organización Nacional de Trasplantes (ONT) was formed in 1989 to address declining organ donation rates in Spain. ONT focuses on identifying potential donors and obtaining consent. They have implemented a standardized donation process in every hospital in Spain. The Spanish Model2 consists of a team of specially trained individuals (physicians and nurses), separate from the medical/transplant teams, who are responsible for raising the donor rate in all hospitals. Among other things, these teams identify all potential donors and handle the evaluation and management of the donor. Donor management guidelines included in the Spanish model are outlined in Appendix II.3 The United States The United Network for Organ Sharing (UNOS), incorporated in 1984, is “a private, non-profit corporation that, with government oversight, develops, implements, and monitors policies in a national health system relative to transplantation. In 1986, UNOS was awarded the federal government contract to operate the national Organ Procurement and Transplantation Network (OPTN). Subsequent regulations required all transplant centers to join the OPTN and be governed by UNOS policies. The OPTN is mandated to assure the effectiveness, equity and quality of the nation’s organ procurement, allocation and distribution system.”4 UNOS has developed a Critical Pathway for the Organ Donor (see Appendix III). This document has been endorsed by the Association of Organ Procurement Organizations, the American Society of Transplantation, the American Society of Transplant Surgeons and the North American Transplant Coordinators Organization. Its use has resulted in an 11.3% increase in the number of organs transplanted per 100 donors.5 21 There are 59 organ procurement organizations governed by UNOS policies. All were contacted and requested to provide donor organ management guidelines and eligibility criteria (as it is not mandatory that they use the Critical Pathway). Details on organ donor management in the United States will be provided in a separate presentation at the Canadian Forum on Medical Management to Optimize Donor Organ Potential. Another example of U.S. organ donor management guidelines is provided in Appendix IV. It is the New England Organ Bank guideline (revised Jan 2001). The United Kingdom UK Transplant is a special health authority within the National Health Service. Its key role is to match and allocate donated organs. It also supports transplantation services across the United Kingdom and is responsible for “contributing to the development of performance indicators, standards and protocols which guide the work of organ donation and transplantation”.6 UK Transplant is directly accountable to health ministers in Scotland, Wales and Northern Ireland and to Parliament through the Department of Health in England. The United Kingdom Transplant Coordinators Association is the association that promotes organ donation, best practices in transplantation and supports transplant coordinators working in the United Kingom. (See also United Kingdom Hospital Policy for Organ and Tissue Donation.7) A standardized donor management technique was developed at the Papworth Hospital in Cambridge, England. Murali et al. (2003)8 have published the most recent description of this approach. Guidelines from the Papworth Hospital for the management of the multi-organ donor are provided in Appendix V. Further details on the Papworth approach to organ donor management will be provided in a separate presentation at the Canadian Forum on Medical Management to Optimize Donor Organ Potential. Australia The Federation of Australia is composed of six states and one territory. Five states have transplant programs. “The delivery and organization of health services is a state responsibility although only the central (Federal) government has taxing powers; it therefore controls the funds available for health care.”9 In 1977, South Australia adopted the Spanish Model, described above. “Since the introduction of the modified Spanish model, the organ procurement rate in South Australia is double the rate of the rest of Australia”10 (23 vs. 10.5 donors per million population). The Alfred Hospital in Melbourne has developed a successful system of transplant coordination and organ allocation.11 Its system is considered a good example of the Australian approach to organ donation and transplantation. A detailed description of the medical management of the potential organ donor at the Alfred Hospital has been published.12 22 Eurotransplant The Eurotransplant International Foundation is responsible for the organization and allocation of organ donation in Austria, Belgium, Germany, Luxembourg, the Netherlands and Slovenia. This international framework includes all transplant hospitals, tissue-typing laboratories and hospitals where organ donation takes place.13 The Leuven University Hospital in Belgium has developed a secure-access website containing organ donation information and protocols, including multi-organ donor management guidelines (see Appendix VI). The information contained on this website is accessible to all members of the hospital’s donor hospital network and is licensed and protected for the hospital and the network. According to Frank Van Gelder, Senior Transplant Coordinator, Department of Transplant Surgery, since the implementation of this simplified protocol the hospital has seen a 40% increase in donors.14 23 V. Conclusion This analysis of Canadian management guidelines was based on 17 unique documents. These guidelines are for multi-organ donation and are generally consistent in content, although many do not address all variables of interest. For oxygenation and ventilation, discord occurs in PaO2 and tidal volume targets, with a variety of values cited. Target pressures for organ perfusion often differ between adult and pediatric guidelines (the latter providing age-adjusted values). Few guidelines provide targets for pulmonary capillary wedge pressure, systemic vascular resistance, cardiac index and left ventricular stroke volume. Standard care for invasive monitoring consists of an arterial and a central venous line. Only eight guidelines provide information on pulmonary artery catheterization. A majority of guidelines cite dopamine as the drug of choice for cardiovascular support. The management of fluid balance, electrolytes, hematology and body temperature do not differ greatly from standard ICU care. Definitions of diabetes insipidus are mainly based on exceeding a specific urine output, with a few guidelines including targets for urine osmolality (and serum), sodium and specific gravity. Therapy consists of desmopressin (in all cases), at a wide variety of dosages, and (in some cases) vasopressin. Supportive testing and investigations identified, to varying degrees, are chest x-ray, electrocardiogram, echocardiogram, bronchoscopy, cardiac angiogram and cardiology consultations. Areas covered by a minority of guidelines include the use of antibiotics, corticosteroids and hormone replacement therapy. Decisions to determine donor organ eligibility are referred to the provincial organ procurement organizations. Generally, eligibility is assessed on an individual basis, taking into consideration recipient need at that point in time. Slight variations exist between OPOs for absolute contraindications; however most included HIV/AIDS, West Nile virus, active infections and malignancies. International issues in organ donor management are directly related to the level of maturity of a country’s particular program. Recent efforts to optimize the medical management of organ donors (and thus maximize organ yield per potential donor) are under way. Countries at the forefront of this movement are Spain, the United States, the United Kingdom, Australia and members of Eurotransplant. 24 Appendix I – Canadian Organ Procurement Organizations Note: The following descriptions are based on the authors’ understanding of surveys received. British Columbia OPO is a separate entity from hospitals. Stated that their guidelines covered the entire province but did not provide a list of hospitals. Received a reply from one PICU to confirm this. Received separate GL from one adult center. Alberta 2 OPOs (Northern and Southern Alberta). Stated they each cover specific territory of province and provided list of hospitals covered. Hospitals (in both regions) that responded confirmed they are covered by OPOs. Northern provided pediatric and adult guidelines, Southern has no documented guidelines at this time. PICU in Northern provided additional GL. Saskatchewan OPO located and functions within hospital. Only reply received from this province was that of OPO. Stated their guidelines covered all hospitals within the province, provided list of hospitals. Manitoba OPO located and functions within hospital. Stated their guidelines covered hospitals in province and provided list. Responses from hospitals confirmed this. No additional GL received. Ontario 3 OPOs functioning within the province (transitional period). Trillium has in-hospital coordinators, “draft” guidelines provided which were not recorded as not yet in use. Quebec OPO separate entity from hospitals, provided pediatric and adult guidelines. Resource Nurses (IRs) have dedicated organ donor roles within the hospitals (OPO “Red Binders” on units with IRs). OPO coordinators also help manage patients. New Brunswick OPO located and functions within hospital. Only received reply from OPO for this province, stated their guidelines covered all hospitals within the province, provided list of hospitals. Prince Edward Island No OPO covered by Nova Scotia and New Brunswick OPOs. 25 Nova Scotia OPO located and functions within one of hospitals contacted. Stated their guidelines covered hospitals in province and provided list. Responses from hospitals confirmed this. No additional GL received. Newfoundland OPO located and functions within hospital contacted. Only received reply from OPO, stated their guidelines covered all hospitals within the province and provided list. Yukon Not an OPO. Their donors are covered by BC Tx. Canadian Association of Transplantation and Canadian Society of Transplantation No guidelines or eligibility criteria. 26 Appendix II – Spanish Guidelines MANUAL OF DONATION OF ORGANS FOR HEALTH PROFESSIONALS MAINTENANCE OF THE DONOR OF ORGANS (These guidelines have been translated from the original Spanish.) Once established, encephalic death, independently of the cause that originates it, results in ischemic-necrosis of the neurological structures. A series of secondary pathophysiological alterations lead to the absence of function of this great "regulating organ" that is the brain. This fundamentally produces: 1. Absence of spontaneous breathing. 2. Hemodynamic instability. 3. Loss of control of corporal temperature. 4. Loss of control of fluid and electrolyte balance. 5. Alterations in hormonal secretion. The most frequently occurring complications are: hypotension, hypotherma and neurogenic diabetes insipidus (NDI), NDI contributes to the aggravation of hemodynamic instability by causing polyurias and secondary electrolytic alterations. All these aspects endanger the viability of the transplantable organs, turning the multi-organ donor into a critical patient requiring strict control and monitoring (tables I and II), as well as an energetic treatment and in many occasions the complexity of a patient with multi-system failure. Table I. Monitoring the organ donor ECG. Arterial tension. Central venous pressure. Hourly Diuresis. Arterial Gasometry. Saturation of O2 by means of pulsoxymetry. Temperature. The main targets in the maintenance of the donor of organs are: 1. 2. 3. Cardiocirculatory Stability Suitable Oxygenation Correction and treatment of other problems like neurogenic diabetes insipidus, electrolytic arrhythmias, alterations, prevention of infections, etc... In table II a summary of maintenance objectives can be seen. 27 Table II. Maintenance objectives Cardiac Frequency ≤ 100 bpm. SBP ≥ 100 mm Hg. CVP: 10–12 cm H2O. PCP: 8–14 mm Hg. Diuresis: > 1 cc/kg/h in adults, > 2 cc/kg/h in children Temperature > 35ºC. Arterial Gasometry: pH: 7,35–7,45. PaO2 values next to 90–100 mm Hg. PaCO2: 35–45 mm Hg. Hematocrit ≥ 30% (if multi-organ donor must be ≥ 35%) 1 HEMODYNAMIC Control : To maintain hemodynamic stability: • • • • • • Arterial hypotension is the most frequent alteration. It is recommended to maintain systolic ABP ≥ 90–100 mm Hg. The initial treatment consists of volume administration: o Dependant upon the volume of the losses, electrolyte values and levels of hemoglobin. o The contribution must be controlled hourly, because large volumes are useful to maintain good renal flow but can jeopardize cardiac, pulmonary and hepatic donation. Monitoring CVP or PCP using Swan-Ganz catheter. If normovolemia is obtained (CVP 10–12 cm H2O, PCP 8–14 mm Hg) and hypotension persists, add vasoactive drugs at minimum doses. Drugs of choice are DOPAMINE, DOBUTAMINE and NORADRENALINE. Hourly control of diuresis. Values of concern: < 50 or > 200 cc/h. If in spite of adequate fluid resuscitation (CVP of 10–12 cm of H20/PCP of 8–14 mm Hg), arterial hypotension continues, initiate treatment with inotropic drugs. The suggested order is the following one: 1. Dopamine. It is the drug of choice for its beneficial effect on renal flow and some authors have found a relation between the decreased appearance of tubular necrosis acute postransplant and the use of dopamine in doses < 5 µg/kg/min. Avoid exceeding doses of 10 µg/kg/min (which worsen cardiac and hepatic perfusion through its alpha-agonist effect). 28 2. Dobutamine. Its fundamental indication would be in polytrauma donors with myocardial contusion where it is suspected that ventricular dysfunction is the fundamental cause of the hypotension. Use with caution since it can increase vasodilation and worsen the hemodynamic situation, by diminishing systemic vascular resistance. 3. Other vasopressor drugs: Noradrenaline and adrenalin. Their use is restricted to donors with persistent hemodynamic instability in spite of adequate volume resuscitation and support with dopamine of 10 µg/kg/min. It is necessary to consider that both can produce hyperglycemia. Therefore a strict control of glycemia must be maintained with precise dosing of insulin. The vasoconstriction invalidates the CVP measurements, thus it is necessary to place a Swan-Ganz catheter to optimize the handling of fluids and vasoactive drugs. Noradrenaline produces arterial vasoconstriction, diminishing blood flow to the liver, pancreas and kidneys. Thus the simultaneous use of low doses of dopamine are advised to improve renal flow. If the donor needs large doses of noradrenaline for long periods of time, it is recommended to change to an infusion of adrenalin. This drug has the advantage of improving hepatic blood flow. The use of high doses of these alpha-stimulants can cause vasoconstriction producing tissue hypoperfusion. This results in frequent assessment of the function of the different organs and must be communicated to the surgical transplant teams (who will evaluate organ viability). 2. ARRHYTHMIAS. Cardiac arrhythmias of atrial and ventricular origin can occur, as well as diverse degrees of blockade. Causes are multi-factorial, the most frequent being: 1. Hypovolemia. 2. Hypotension. 3. Hypothermia. 4. Catecholamine use. 5. Myocardial contusion. 6. Gasometric alterations (hypoxia and changes in pH). 7. Secondary electrolytic alterations due to neurogenic diabetes insipidus. Therefore, in the prevention of arrythmias it is necessary to correct hypotherma and all factors leading to metabolic or hemodynamic disturbances. 3. SUITABLE OXYGENATION And RESPIRATORY CARE. • To maintain the permeability of the aerial route. • To prevent atelectasis by means of respiratory physiotherapy, postural drainage, bronchial suctioning of secretions, etc. • To maintain arterial oxygen saturation between 95 and 100% by means of FiO2 up to 100% and hemoglobin up to 10–12 g/L. • For lung donation, the target FiO2 is < 50% to avoid pulmonary toxicity and PEEP of 5 cm H2O to prevent pulmonary collapse. 29 The lung donor requires maintenance with respirators of volumetric type and the routine use of PEEP of 5 cm H2O to prevent atelectasis which would contraindicate the extraction of this organ. In these donors the FiO2 must be strictly controlled to avoid pulmonary toxicity by oxygen. Maintain CVP between 5–10 cm of H2O avoiding volume overloads that could produce pulmonary edema. Use a tidal volume of 8–10 ml/kg and obtain a maximum tip of pressure in aerial routes inferior to 30 cm of H2O to avoid pulmonary damage by hyperpressure. In some cases donors can present/display neurogenic pulmonary edema. This can produce a severe hypoxia that can jeopardize the viability of the organs to be transplanted. In donors with pulmonary edema who require elevated levels of PEEP, it could be necessary to insert a SwanGanz catheter to adapt treatment based on cardio-respiratory variables. In all cases, frequent control of arterial gasometry and arterial oxygen saturation is necessary to detect episodes of desaturation early. Finally and as in any other type of critical patient, the endobronchial suctioning will be carried out with maximum conditions of asepsis to avoid local respiratory infections or infections leading to sepsis. 4. METABOLIC ALTERATIONS. 1. Electrolytic Disturbances. The most frequent are hypernatremia, hypokalemia, hypomagnesemia, hypocalcemia and hypophosphatemia. Early correction of electrolytic alterations is important in order to avoid arrhythmias that could lead to cardiovascular instability. With the goal of obtaining a correct electrolyte administration, measurements should be made q3–4hrs. Besides checking for imbalances this allows for adequate replacements of Na and K. 2. Hyperglycemia. The etiology of hyperglycemia is multi-factorial and could also be due also to a peripheral resistance to insulin. Amoung its causes it it is necessary to emphasize: infusion of inotropes, resuscitation with liquids that contain glucose, previous treatment with corticosteroids, endogenous catecholamine secretion during the process of cerebral coning, hypotherma, etc... Hyperglycemia can result in a hyperosmolar situation with intracellular dehydration, metabolic acidosis and polyuria (which in turn contributes to hypovolemia). In all cases it is necessary to correct hyperglycemia with a rapid intravenous infusion of insulin. Use a continuous infusion of insulin titrated to maintain serum glucose at approximately 150 mg/dl. 5. HYPOTHERMIA. Hypothermia results from the destruction of the central hypothalamic thermoregulator. Bradycardia and other severe arrythmias are the principle consequences. Maintain a core body temperature ≥ 35ºC. Maintain donor temperature with warming blankets, heating lamps, an ambient room temperature of 20–22ºC and warm infusion fluids. 30 6. NEUROGENIC DIABETES INSIPIDUS Brain death can cause diabetes insipidus which presents as a polyuria. Treat with precise volume replacement and/or administration of desmopressin. 7. HORMONAL ALTERATIONS Following brain death there is a rapid depletion of thyroid hormones. Levels of T3 or T4 may be practically undetectable 14 hours after brain death. Normal levels of thyroid stimulating hormone (TSH) are maintained in these cases. Also seen is an important reduction in levels of antidiuretic hormone (ADH), cortisol and insulin. 8. PREVENTION OF INFECTIONS. • Manipulation of catheters, suctioning, etc., should be performed with strict aseptic technique. • Prophylactic use of antibiotics is recommended. • Ocular hygene is important: keep moist with physiological saline. The diagnosis of local infections (adequately treated) is not an absolute contraindication to organ donation. Assessment is based on the results of bacteriological cultures and consultations between the intensivist and surgical transplant teams. 31 Appendix III — UNOS Critical Pathway Collaborative Phase I Practice Referral The following professionals may be involved to enhance the donation process. Notify physician regarding OPO referral Check all that apply. Physician Critical care RN Contact OPO ref: Potential donor with severe brain insult OPC on site and begins evaluation: Time ___Date ___ Organ Procurement Organization (OPO) Ht____ Wt ____ as documented OPO Coordinator (OPC) ABO as documented _____ Medical Examiner (ME)/Coroner Notify house supervisor/charge nurse of presence on unit Respiratory Laboratory Radiology Anesthesiology OR/Surgery staff Clergy Social worker Phase II Phase III Phase IV Phase V Declaration of Brain Death and Consent Donor Evaluation Donor Management Recovery Phase Brain death documented Obtain pre/post transfusion blood for serology testing (HIV, Hepatitis, VDRL, CMV) Time _____ Date _____ Pt accepted as potential donor Obtain lymph nodes and/or blood for tissue typing MD notifies family of death Plan family approach with OPC Notify OR & anesthesiology of pending case Offer support services to family (clergy, etc) OPC/Hospital staff talks to family about donation Family accepts donation Chest & abdominal circumference Cardiology consult as requested by OPC Time _____ Date _____ ME/Coroner notified Organ recovery process discontinued – donor organs unsuitable for transplantation ME/Coroner releases body for donation Family/ME/Coroner denies donation – stop pathway – initiate postmortem protocol – support family. 32 Organ placement OPC sets tentative OR time Checklist for OR OR Supplies given to Prepare patient for transport to OR Insert arterial line/ CVP/2 large-bore IVs Notify house supervisor of pending donation Lung measurements per CXR by OPC OPC obtains signed consent & medical/social history OPC writes new orders IVs Pumps O2 Ambu Peep valve Transport to OR Date ________ Time ________ OR nurse reviews consent & brain death documentation & checks patient’s ID band Collaborative Phase I Practice Referral Labs/ Diagnostics Phase II Phase III Phase IV Phase V Declaration of Brain Death and Consent Donor Evaluation Donor Management Recovery Phase Review previous lab results Blood chemistry Review previous hemodynamics CBC + diff UA PT, PTT ABO Liver function tests C&S A Subtype Blood culture _ 2 / 15 minutes to 1 hour apart Sputum Gram Stain & C & S Type & Cross Match ____# units PRBCs CXR ABGs EKG Echo Consider cardiac cath Consider bronchoscopy Determine need for additional lab testing CXR after line placement (if done) Serum electrolytes Rx H & H after PRBC PT, PTT BUN, serum creatinine after correcting fluid deficit Notify OPC for ___ PT >14___ PTT < 28 ___ Urine output is < 1 mL/kg/hr ___ > 3 mL/kg/hr ___ Hct < 30 / Hgb < 10 ___ Na > 150 mEq/L 33 Labs drawn in OR as per surgeon or OPC request Communicate with pathology: Bx liver and/or kidneys as indicated Respiratory Pt on ventilator Suction q 2 hr Reposition q 2 hr Prep for apnea testing: set FiO2 @ 100% and anticipate need to decrease rate if PCO2.< 45 mm Hg Maximize ventilator settings to achieve SaO2 98–99% Notify OPC for ____ BP < 90 systolic PEEP = 5cm O2 challenge for lung placement FiO2 @ 100%, PEEP @ 5 _ 10 min Portable O2 @ 100% FiO2 for transport to OR ____ HR < 70 or > 120 Ambu bag and PEEP valve ____ CVP < 4 or > 11 ABGs as ordered ____ PaO2 < 90 or VS q 1° ____ SaO2 < 95% Check NG placement & output Move to OR Use warming/cooling blanket to maintain temperature at 36.5–37.5 °C Treatments/ Ongoing Care NG to low intermittent suction Obtain actual Ht _____ & Wt _____ if not previously obtained Set OR temp as directed by OPC Post mortem care at conclusion of case Medication as requested by OPC Fluid resuscitation – consider crystolloids, colloids, blood Medications DC meds except pressors & antibiotics Broad-spectrum antibiotic if not previously ordered DC antidiuretics Diuretics as needed 350 U heparin/kg or as directed by surgeon Vasopressor support to maintain BP > 90 mm Hg systolic Electrolyte imbalance: consider K, Ca, PO4, Mg replacement Hyperglycemia: consider Insulin drip Oliguria: consider diuretics Diabetes insipidus: consider antidiuretics Paralytic as indicated for spinal reflexes Optimal Outcomes The potential donor is identified & a referral is made to the OPO. The family is offered the option of donation & their decision is supported. The donor is evaluated & found to be a suitable candidate for donation. Shaded areas indicate Organ Procurement Coordinator (OPC) Activities 34 Optimal organ function is maintained. All potentially suitable, consented organs are recovered for transplant. Cardio-Thoracic Donor Management 1. • Early echocardiogram for all donors: Insert pulmonary artery catheter (PAC) to monitor patient management (placement of the PAC is particularly relevant in patients with an EF < 45% or on high dose inotropes.) use aggressive donor resuscitation as outlined below. 2. • • • Electrolytes Maintain Na < 150 meq/dl Maintain K+ > 4.0 Correct acidosis with Na Bicarbonate and mild to moderate hyperventilation (pCO2 30–35 mm Hg). 3. • • Ventilation Maintain tidal volume 10–15 ml/kg keep peak airway pressures < 30 mm Hg maintain a mild respiratory alkalosis (pCO2 30–35 mm Hg). 4. Recommend use of hormonal resuscitation as part of a comprehensive donor management protocol Key elements Tri-iodothyronine (T3): 4 mcg bolus; 3 mcg/hr continuous infusion Arginine Vasopressin: 1 unit bolus: 0.5–4.0 unit/hour drip (titrate SVR 800–1200 using a PA catheter) Methylprednisolone: 15 mg/kg bolus (Repeat q 24º PRN) Insulin: drip at a minimum rate of 1 unit/hour (titrate blood glucose to 120–180 mg/dl) Ventilator: (See above) Volume Resuscitation: Use of colloid and avoidance of anemia are important in preventing pulmonary edema albumin if PT and PTT are normal fresh frozen plasma if PT and PTT abnormal (value ≥ 1.5 _ control) packed red blood cells to maintain a PCWP of 8–12 mm Hg and Hct > 10.0 mg/dl • • • • • • • • • 5. • • • • • • • When patient is stabilized/optimized repeat echocardiogram. (An unstable donor has not met 2 or more of the following criteria.) Mean Arterial Pressure ≥ 60 CVP ≤ 12 mm Hg PCWP ≤ 12 mm Hg SVR 800–1200 dyne/sec/cm5 Cardiac Index ≥ 2.5 l/min/M2 Left Ventricular Stroke Work Index > 15 dopamine dosage < 10 mcg/kg/min. The Critical Pathway was developed under contract with the U.S. Department of Health and Human Services, Health Resources and Services Administration, Division of Transplantation. 36 Hormonal Resuscitation of the Organ Donor Brain-dead donors who fail conventional resuscitation measures as manifested by a poor cardiac output, inadequate organ perfusion pressures, and increasing lactic acidosis often respond to three-drug hormonal resuscitation (1). Administration of a methylprednisilone bolus and infusions of arginine vasopressin and triiodothyronine to 701 brain-dead donors resulted in a 22.5% increase in the number of organs transplanted per donor(1). Hormonal resuscitation was beneficial for donors both under, and over, age 40. Hearts recovered from hormonal resuscitation donors have a significantly reduced 30 day mortality and a significant reduction in prolonged graft dysfunction (2). Bibliography 1. Transplantation 75:482–7, 2003. Aggressive Pharmacologic Donor Management Results in More Transplanted Organs. 2. Abstract, International Congress of the Transplantation Society. Transplantation 74:205, 2002. Hormonal Resuscitation Yields More Transplanted Hearts with Improved Early Function. 3. Hormonal Resuscitation Yields More Transplanted Hearts with Improved Early Function. Transplantation 75: April 27, 2003. Donor-Related Malignancies Transmission of donor malignancies is rare with 18 cases from 34,933 cadaver donors and 3 cases from 32,052 living donors being reported to UNOS from 1994–2001 (1,2). Donors with past histories of certain types of cancers may be considered as donors (3) including certain types of primary CNS tumors (4). Tumors that pose a high transmission risk include choriocarcinoma, melanoma, lymphoma, and carcinoma of the lung, colon, breast, kidney and thyroid. High risk donors include glioblastoma multi-forme, high grade astrocytomas, medulloblastomas, and any brain tumor donor who has undergone ventriculo-peritoneal shunting. Bibliography 1 Transplantation 74:358–62, 2002. Transplant Tumor Registry: Donor Related Malignancies. 2. Transplantation Reviews 16:177–91, 2002. Donor-Related Malignancies. 3. Transplantation 70:1747–51, 2000. First Report of the United Network for Organ Sharing Transplant Tumor Registry: Donors with a History of Cancer. 4. Transplantation 73:579–82, 2002. Transplant Tumor Registry: Donors with Central Nervous System Tumors. 37 UNOS Critical Pathway Bibliography 1. Holmquist M., Chabalewski F., Blount T., Edwards, C. McBride V., Pietroski R. Critical Care Nurse, 19(2):84–98, 1999. A Critical Pathway: Guiding Care for Organ Donors. 2. American Journal of Transplantation, 2:761–8, 2002. Increased Transplanted Organs from the Use of a Standardized Donor Management Protocol. UNOS Critical Pathway for the Organ Donor resulted in a 10.3% increase in organs recovered and an 11.3% increase in organs transplanted. There was no reduction in the quality of the organs transplanted. 3. Circulation 106:836–41, 2002. Consensus Conference Report: Maximizing Use of Organs Recovered from the Cadaveric Donor: Cardiac Recommendations. Heart donor criteria and a donor management algorithm for heart recovery. 4. Abstract, International Congress of the Transplantation Society. Hormonal Resuscitation Yields More Transplanted Hearts with Improved Early Function. Hearts from hormonal resuscitation donors had significantly reduced early graft dysfunction and one-month patient mortality. 38 Appendix IV – New England Organ Bank The purpose of this document is to describe the principles of organ donor evaluation and management to be followed for New England Organ Bank (NEOB) organ donors. For each organ donor, the goals of donor evaluation and management include: • • • Determination of organ suitability for transplantation Optimization of the function of these organs Maximization of the number of organs recovered General Principles 1. Absolute Contraindications to Organ Donation: • Donor age > 80 years • AIDS or HIV seropositivity • Malignancy other than primary intracranial tumor or non-melanoma skin cancer 2. Donor Evaluation Initial assessment shall include a review of the admission history and physical, hospital course, temperature, electrolytes, CBC, fluid balance, hemodynamics, medications, infections, pulmonary function, cardiac function, renal function, and liver function. In extremely unstable cases (i.e., severe hypotension refractory to volume replacement and pressors), plans should be made in consultation with the AMD to proceed to the operating room (OR) as soon as possible for rapid hepatonephrectomy or nephrectomy. Aggressive management should continue through the recovery surgery. 3. Determination of Organs Suitable for Transplantation Organs may be deemed unsuitable based on donor age, organ injury, disease or gross abnormality. Questions regarding organ suitability in marginal cases should be directed to the medical director on call. 4. Initial Management Goals • Restore and maintain normothermia • Correct acid/base imbalances • Optimize lung function • Restore intravascular volume • Normalize blood pressure • Maintain hematocrit _ 30 % • Treat severe hyperglycemia, central DI, DIC 39 5. Organ-specific Considerations Lung / Heart-lung Prevent pulmonary interstitial fluid overload Prefer PRBC's for volume expansion if needed Maintain FIO2 _ 40% and PO2 > 100 mm Hg Prefer PEEP at 5 cm H20 Large ET tube for bronchoscopy Liver / Pancreas Prefer dopamine for tx of hypotension Prefer minimal or no pitressin therapy (to minimize splanchnic vasoconstriction) Avoid excessive crystalloid infusion (to minimize liver congestion) Maintain PO2 > 100 mm Hg Heart If hypotensive with low SVR, prefer pure vasoconstrictor Cardiac cath indicated for pts. at risk for CAD Maintain PO2 > 100 mm Hg May request PA catheter to assess cardiac function and determine appropriate therapy Kidney Prefer dopamine for tx of hypotension Prefer brisk diuresis (urine output > 200 cc/h) Maintain PO2 > 100 mm Hg 6. Specific Donor Management Problems Poikilothermia Loss of thermoregulatory function follows hypothalamic dysfunction in brain dead patients. Passive heat loss may lead to progressive hypothermia which in turn may result in clinically significant changes in organ function (EKG changes, depressed cardiac function, altered cellular metabolism, etc.) It is far easier to prevent hypothermia than to reverse it. Therefore, patient temperature should be carefully monitored and hypothermia should be treated early. Treatment: • • • • Maintain room temperature _ 75° F Keep body and head well covered; use warming blanket as needed Heat IV fluids with blood warmer, if temp < 35° C Heated (45° C) humidified oxygen via ventilator (may cause thermal injury to airway) Hypertension Severe hypertension (systolic BP > 200 torr) is infrequently encountered in brain dead patients. Most often, it is temporally related to brainstem herniation and is therefore self-limiting. Often, this hypertension is associated with transient rhythm disturbances. On occasion, severe hypertension persists following herniation. Treatment: • • • • Sodium nitroprusside (Nipride) infusion is the treatment of choice. The goal of treatment should be to maintain the diastolic BP below 100 mm Hg. Nipride should only be used in cases of severe, persistent hypertension, and should be discontinued as soon as possible. 100 mg Nipride in 250 ml D5W yields a concentration of 400 mcg/ml. Initial dosage should be 0.5 mcg/kg/min. Titrate upward in increments of 0.25 or 0.5 mcg/kg/min to achieve desired BP control. 40 Hypotension Hypotension (SBP < 90 mm Hg) will develop in most brain dead patients at some point in the donor management process. Many potential donors are hypotensive at the time of the initial referral. Even brief intervals of severe hypotension can have significant deleterious effects on end organs. Therefore, hypotension should be treated aggressively with therapy based on a sound understanding of the cause of the hypotension. A central venous pressure line and an arterial line are essential in order to manage hypotension appropriately. When requested by the cardiac team, especially in hemodynamically unstable donors, a pulmonary artery catheter may be introduced, and serial cardiac outputs and SVR measurements can be collected. Hypovolemia Excessive intravascular volume loss (hemorrhage, third spacing, DI, fluid restrictions, etc.) is common in potential organ donors, especially trauma victims. Neurogenic vasodilatation (loss of both venous and arterial vasomotor tone) is present in the majority of donors as well. One or both of these factors may contribute to a relative or absolute hypovolemia. Therefore, whenever possible, intravascular volume deficits should be corrected prior to the use of vasoactive drugs. (In practice, low to moderate dose dopamine infusion may be required to maintain adequate BP during the initial interval of volume repletion. Once volume is restored, however, vasoactive drugs should be used only as needed.) Care should be taken to avoid the development of pulmonary interstitial fluid overload, especially in potential lung donors. Therefore, in most cases, colloid (albumin, Plasmanate) and blood products (PRBCs) should be used in combination with crystalloid solutions for volume expansion. Treatment: • • • • • In general, IV fluid should be D5_NS at rate of 1 liter per 1/2 hour to raise CVP (in adult pts. only; consultation with a pediatric intensivist is advised for fluid management recommendations in pediatric donors) Use albumin or Plasmanate to supplement crystalloid volume expansion Monitor CVP closely; target is 8–10 cm H20; avoid excessive increase in CVP PRBC's are indicated for Hct. < 30 % in hypovolemic donor Monitor electrolytes carefully and supplement K+ as indicated 41 Decreased Vascular Resistance Neurogenic vasodilatation (loss of both venous and arterial vasomotor tone) is present in the majority of donors. Despite adequate volume restoration, some donors will require vasoactive drug therapy directed at the underlying cause of the hypotension. Effective management of these donors requires insertion of PA catheter for determination of cardiac filling pressures, CO, and SVR. Due to the possibility of decreased perfusion to certain organs, vasoconstrictors should be used with extreme caution. High dose vasoconstrictor therapy should be avoided in this setting. The systemic vascular resistance (SVR) should be calculated based on thermodilution cardiac output measurements. If the SVR [(MAP or CVP) _ 80/CO] is < 400, vasoconstrictor therapy is indicated. Treatment: • • • • Norepinephrine Bitartrate (Levophed) 4 mg/250 ml D5W yields 16 mcg/ml Initial dose is 0.02 mcg/kg/min; increase gradually to max. of 0.10 mcg/kg/min Monitor CO, SVR, and cardiac filling pressures closely Monitor urine output and serum creatinine closely Depressed Cardiac Function Following resuscitation from cardiopulmonary arrest, due to pre-existing cardiac disease, or secondary to brainstem herniation, some donors may exhibit depressed cardiac function. These patients will be hypotensive despite adequate volume restoration. The use of vasoconstrictors in these patients will exacerbate cardiac dysfunction. Donors with depressed cardiac function require inotropic and chronotropic support to maintain an adequate cardiac output. Effective management of these donors requires insertion of PA catheter for determination of cardiac filling pressures, CO, and SVR. If the cardiac index (CO/BSA in m2) is less than 2.0 L/min/m2, inotropic therapy is indicated. Treatment • • • • • Dopamine hydrochloride (Intropin) 400mg / 250 ml D5W yields 1600 mcg/ml Initial dose is 2–4 mcg/kg/min. Titrate to increase SBP > 90 mm Hg. Low dose dopamine (< 5 mcg/kg/min) has a salutary effect on renal blood flow Monitor CO, SVR, and cardiac filling pressures closely Monitor urine output Respiratory Insufficiency Brain dead patients require frequent pulmonary hygiene to prevent atelectasis and to maintain adequate oxygenation. Positive end-expiratory pressure of 5 cm H2O ("physiologic PEEP") is helpful, but higher levels of PEEP should be avoided to minimize potentially deleterious effects on venous return and cardiac output. High FIO2 levels must also be avoided in potential lung donors to prevent pulmonary oxygen toxicity. Ventilator settings should include a tidal volume of 10 to 15 cc's per kg and a respiratory rate sufficient to maintain arterial PCO2 in the 40–45 mm Hg range. 42 Hypoxemia Arterial oxygen saturations should be maintained at > 95%. PAO2 levels should be = 100 mm Hg. Hypoxemia should be treated aggressively to minimize injury to transplantable organs. Treatment: • • • • • Maintain hematocrit > 30 %; transfuse PRBC's as necessary Turn and suction patient frequently Increase FIO2 by increments of 10%, recheck ABGs Increase PEEP to > 5 cm H2O only as last resort Lasix therapy may be indicated if CXR is c/w pulmonary edema Note: If PAO2 persists at < 250 torr on 100% FIO2 , NEOB lung transplant programs will exclude donor lungs for transplantation. Hypercarbia Apnea testing to confirm the diagnosis of brain death can result in significant hypercarbia leading to respiratory acidosis. Careful attention should be paid to the patient's ventilatory status and ABGs, especially following clinical exams for determination of brain death. The ventilator rate should be increased as needed to normalize PACO2 levels in the 40 to 45 mm Hg range. Polyuria Polyuria (urine output > 500 ml per hour) is frequently seen in brain dead patients. It may be due to physiological diuresis, osmotic diuresis (mannitol, glucose), diuresis caused by hypothermia, partial or complete diabetes insipidus, other diuretics, or a combination of the above. Excessive polyuria due to osmotic diuresis or DI may lead to hypernatremia, hypokalemia, and hyperosmolality. Serum potassium should be monitored and treated as indicated. Urine and serum electrolyte levels and osmolality aid in the determination of the cause of polyuria. Physiological diuresis Aggressive volume restoration may result in a physiological diuresis. No treatment is warranted, but intake and output should be monitored carefully. Osmotic diuresis Prior mannitol administration or excessive glucose infusion may result in an osmotic diuresis. Treatment: • Mannitol administration should be avoided in this setting. Glycosuria and hyperglycemia should be treated with sliding scale IV insulin therapy to normalize blood glucose levels. 43 Diabetes insipidus Once the abovementioned causes for polyuria have been excluded, the diagnosis of DI can be made by evaluating the volume of urine output, urine specific gravity, urine and serum electrolyte levels, and urine and serum osmolality. At least three of the following findings should be present simultaneously to establish the diagnosis of DI: • • Urine output > 500 ml per hour Urine specific gravity < 1.005 Serum sodium > 155 mEq/L Serum osmolality > 305 mOsm/L Treatment: • • • • Aqueous pitressin IV infusion (10 U / 250 ml D5W) Initial dosage 1.2 U per hour (rate: 30 ml per hour) Titrate Q. 15 min. to maintain u/o of 150–300 ml/hr Discontinue for hourly u/o < 150 ml In addition to Pitressin therapy, the free water deficit should be calculated and 50% of the calculated deficit should be infused as rapidly as possible, preferably with a hypotonic solution such as D5W or 0.5 NS. The use of pitressin should be avoided when possible in liver and pancreas donors to minimize the possibility of decreased perfusion to these organs. 44 Appendix V – Papworth approach Philosophy The Papworth philosophy is to assess the donor organs at the referral hospital whenever possible. It is also to employ aggressive therapeutic intervention and invasive measurement in order to optimise the physiological environment for the heart and lungs. Once all the possible manoeuvres have been employed, the mechanical function of the heart and the gas exchanging function of the lungs are reassessed. Then, and only then, is it appropriate to reject organs where function falls below acceptable minimum targets. The practical implications of this philosophy include increased financial expense and an increased number of procurement journeys with no transplantable organs being obtained, but the possibility of wasting transplantable organs will be minimized. Management of the multi-organ donor 1. Infection Control Organ retrieval should be carried out in an operating theatre to the standard of any other surgical procedure. In particular, staff should follow the normal practice of limiting the number of individuals present to those involved in that part of the procedure and a maximum of two visitors (at the discretion of the Papworth surgeon). Movement of staff in and out of the theatre should be kept to a minimum. 2. Ventilation 2.1 Ventilate to normocarbia (4.5–5.5 kPa) using large tidal volumes (15 ml/kg) with either a low respiratory rate or deadspace and 5 cm H2O) PEEP. 2.2 Use minimal FiO2 consistent with adequate oxygen delivery (SaO2 > 98%). 2.3 Ensure clear airway using tracheal suction and check position of ET tube. Collect sputum sample for culture. 2.4 Manually inflate lungs under direct vision after sternotomy and opening pleura, and note any consolidation and trauma. 3. Vascular Access A separate fresh, venepuncture must be made from which to obtain blood culture samples. 3.1 Prepare the following access lines: a. Left arterial line (radial or brachial) b. Right triple lumen (internal jugular) c. Right Swan-Ganz (internal jugular) 45 3.2 Use these lines in the following manner: a. Swan introducer – blood & colloids. Venesection and samples. Use a warming coil for infusion. b. Triple smallest lumen – ADH/Adrenaline infusion. c. Triple lumen – T3 and insulin. d. Triple large lumen – inotropes/dilators. 4. Haemodynamics 4.1 Use Swan-Ganz and arterial pressure to enable calculation of cardiac index, pulmonary and systemic resistances and LV static power. 4.2 Target the following status: (Use Normogram) a. SVR 800–1200 dynes/sec/cm5 b. LVPo 0.6–1.0 Watts c. Minimal preload (< 8 mm Hg) 4.3 Use ADH infusion to increase the afterload (max 4 ml/hr) 4.4 Use Sodium Nitroprusside to decrease the afterload (max 4 µg/kg/min) 4.5 Use Dopamine if all else fails to produce an adequate output in the face of a normal SVR (max 10 µg/kg/min). 5. Fluid Management 5.1 Use colloids only to replace peri-operative loss and to adjust filling pressures. Infuse via a warming coil. 5.2 Give whole blood or packed cells to keep Hb > 10 g/dL. 5.3 Replace urinary losses with 4.3% Dextrose/0.25% saline and K+ 20 mmols/L. 6. Antibiotics 6.1 Give the following regime at induction after taking blood samples for culture: a. Vancomycin 1 g b. Meropenem 1 g 7. Steroids 7.1 Methyl Prednisolone 500 mg stat dose. 46 THE PAPWORTH DONOR MANAGEMENT HORMONE REPLACEMENT PROTOCOL The following infusions should be prescribed and commenced as soon as possible: 1. • • • T3 (Triiodothyronine) 20 microgram vials, made up with water for injection = 1 µg/ml. Given an initial bolus of 4 µg followed by an infusion of 3 µg/hr. • • • Pitressin (Argipressin) Ampoules 1 ml (20 units/ml). Make up to 40 mls with 5% glucose = 0.5 units/ml. Give initial bolus of 1 unit followed by an infusion at 0.5–2.0 units/hr (i.e. 1–4 ml/hr). 2. NB If mean arterial pressure > 90 mm Hg following administration of pitressin, discontinue infusion. 3. • • Insulin (Human actrapid) Commence sliding scale insulin to maintain blood sugar between 4–6 mmol/l Blood sugar > 15 mmols 8–15 mmols 4–8 mmols < 4 mmols Insulin Perfusiona 5.5 IU/hr 3.5 IU/hr 1.5 IU/hr GIK 1.5 ml/kg/hr a These dosages are suitable for patients weighing between 40–100 kg. If the patient is < 40 kg use half the above dose. Discuss with the on call transplant fellow at Papworth if in any doubt. 47 Appendix VI – Leuven University Hospital Procedure multi-organ donor General remarks In every multi-organ donor (MOD), attempts must be made to achieve optimum protection for all organs which can potentially be procured. This protocol therefore applies to all cases in which organs can be procured from donors with a "beating heart". This protocol becomes effective as soon as the "pronouncement of death" (brain death) has been completed and signed by three independent doctors, in accordance with Belgian legislation and the procedure applicable in that specific hospital. It goes without saying that before brain death occurs, optimum protection for all organs must be ensured. If cardiocirculatory stability cannot be achieved by the usual methods, the additional measures of donor management must be performed. Every potential donor must be reported to a transplant coordinator. Sterility Complete sterility of the donor must be guaranteed when using and positioning catheters, caring for ventilation appliances, bronchial toilet and all other invasive procedures. • • • • • • • ECG : modified V5 lead Capnography, pulsoxymetry, endotracheal tube and ventilation equipment Arterial pressure measurement (desirable) with transducer and continuous screen display CVD with transducer and continuous screen display, Swan-Ganz (if possible) only with haemodynamic instability 2 “thick” (14 or 16 gauge) intravenous catheters. Catheters inserted before admission to hospital or catheters suspected of being infected must be removed immediately – catheter tip culture!) + blood heater on a peripheral “volume” line Bladder and stomach catheters Heating mattress Infusion therapy The filling situation is extremely important Aim for a central venous pressure of 8 mm Hg to 10 mm Hg mean at positive pressure respiration PEEP +5 and the transducer at the level of the right atrium when the donor is horizontal. Overfilling can very quickly compromise the lungs and under filling causes haemodynamic instability. 48 CVD is LOWER than +8 mm Hg • Check Hct., Na., glycaemia, diuresis. If diabetes insipidus is present, start with glucose 2.5% and add further solutions as needed. Possibly give K+ • Give PC + SOPP if Hct < 30 • Give SOPP if Hct > 32 and TE < 11 mg/l or < 5g% • Use Ringer lactate if Hct > 32 and TE > 11 mg/l or > 5g% CVD is HIGHER than +8 mm Hg • Give minimum fluids and give diuretics if urine output is low • Once CVD has been achieved, continue with compensation of abnormal losses. In addition, give maintenance therapy with physiological 50 ml/hour for an adult donor. If hypernatremia is present, give glucose 2.5% in quantities per hour equal to the previous urine output per hour + 50 ml. Avoid hypernatremia at all costs • BUT: unrestrained administration of a solution containing sodium in order to prevent diabetes VERY QUICKLY causes dangerous hypernatremia Urine output The ideal urine output to aim for is 1,5 ml/kg/hour Urine output is LOWER than 1 ml/kg/hour • Optimise filling (see above) • If no cardiovascular instability is present, give diuretics • If cardiovascular instability is present, correct haemodynamic situation and then give diuretics if necessary Urine output is HIGHER than 3 ml/kg/hour • This is usually due to excessive use of diuretics or diabetes insipidus. Excessive use of diuretics usually leads to hyponatremia, diabetes insipidus leads to hypernatremia. Both cause volume problems and temperature losses • Stop diuretics • Correct volume deficiencies and ion anomalies • If diabetes insipidus is present: give Desmopressin (intravenously) 2–4 up to max, 6 µg (1 amp. = 1 ml = 4 µg). Repeat as soon as necessary, i.e. when diuresis again rises sharply (usually every 6 hours) Ventilation Place a filter on the Y section of the ventilator tubes. Use of an artificial nose is a valid alternative. However, if the patient is supercooled, use a humidifier and place a filter on the inspiratory leg of the ventilator tubes in front of the humidifier Ventilate with a flow volume of 15 ml/kg and PEEP +5. Ventilate up to normal PH, which implies normal PaCO2 in the absence of a metabolic component. If the tidal minute volume has to be adjusted, this is done based on frequency, not based on flow volume Aim for a PaO2 of 100 mm Hg by adjusting the FiO2. Every 2 hours, carry out a strictly aseptic bronchial toilet, followed by careful bag squeezing. 49 Acid–base equilibriums, electrolytes and glucose Anomalies are corrected • Blood gas values are not corrected for temperature. Ventilate up to normal PH including where pronounced metabolic acidosis is present. In the mean time, the metabolic acidosis is corrected based on the base deficit. If the bicarbonate content is normalised, ventilation can of course take place up to a normal PaCO2 Ion anomalies are corrected. It is often necessary to administer large quantities of K+ (check and regulations per hour). If hyperglycaemia is present, insulin therapy is started. Cardiovascular (hormone substitution) The most important aspect is optimum filling Aim for an average arterial pressure of > 70 mm Hg. Nonetheless, extreme tachycardia and hypertension must occasionally be treated with (careful!) use of beta-blockers or labetalol If average arterial pressure is lower than 70 mm Hg, first optimise filling and correct ions and acid–base disorders If average arterial pressure remains lower than 70 mm Hg, start dopamine up to max. 5 µg/kg/min If dopamine in doses of 5 µg/kg/min. does not solve the problem, start hormone substitution. Hormone substitution chart T3 (1 vial=20 µg) Loading dose of 2 or 4 µg IV over 1 hour, (Adults). Dose dependant upon patient’s reaction. 0.6 µg/kg/24 h. (= 1.8 µg/h dependant upon the patient’s condition and for wt of 70 kg) Attention: large doses may provoke tachycardia, arrhythmias, hypertension, CO2 production and increased body temperature. Hydrocortisone (Solu-Cortef® Upjohn) 3 _ 200 mg/24 h Up to: 600 mg continuous IV infusion. Human Insulin: Actrapid® 1 to 2 U/h. (Solution: 50 U/50 ml. NaCl 0.9%) Independent of the blood sugar value, this signifies that insulin should not be titrated to the blood sugar values! Verify ionized Ca ++ and P levels and correct any deficiencies with infusions of Ca2+ / P2+ Always maintain optimal volume replacement. Only in situations when it is certain that the lungs will NOT be transplanted can a fluid challenge be performed or the CVP be allowed to rise to 10–12 mm Hg. 50 If the previous measures are inadequate, insert a Swan-Ganz catheter. Only after the necessary interventions have been performed can the dopamine be increased up to a maximum of 10 µg/kg/min or eventually administration of vasoconstrictor infusions Cardiac arrests are treated « lege artis », and a re-evaluation of the donor is undertaken. Coagulation Disseminated intravascular coagulation (DIC) occurs relatively often in multi-organ donors. If coagulation tests indicate, a thromboelastogram may be required. Severe coagulopathies are treated « lege artis » when a volume replacement problems exist. (CMV negative preparations). Aminocaproic acid and tranexamic acid are completely contraindicated. Coagulopathies are only treated if donor stability is threatened. Temperature Control Efforts are made to maintain a temperature > 35°C with the help of a heated mattress, a warmer for blood infused for volume replacement, an artificial nose filter and eventually a respiratory humidifier, limitation of volume loss due to excessive diuresis, administration of T3. Antibiotics In principal, antibitics are only given on the basis of culture results. 51 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Roels L. Personal correspondence with author, 18 November 2003. Matesanz R, Miranda B. A decade of continuous improvement in cadaveric organ donation: The Spanish Model. Journal of Nephrology 2002;15:22–8. Manual de donación de órganos para profesionales sanitarios [online]. Hospital General Universitario de Alicante. No date [accessed 14 February 2004]. <http://donacion.organos.ua.es/info_sanitaria/proceso/manual/indice.htm>. Pierce GA, Graham WK, Kauffman Jr HM, Wolf JS and the United Network for Organ Sharing (UNOS). The United Network for Organ Sharing: 1984–1994. Transplantation Proceedings 1996;28(1):12. Rosendale JD, Chabalewski FL, McBride MA, Garrity ER, Rosengard BR, Delmonico FL, Kauffman HM. Increased transplanted organs from the use of a standardized door management protocol. American Journal of Transplantation 2002;2(8):761–8. About us [online]. 2003 [accessed 14 February 2004]. UK Transplant. <http://www.uktransplant.org.uk/about_us/about_us.htm>. UK Transplant and Transplant Co-ordinators Advisory Group. United Kingdom Hospital Policy for Organ and Tissue Donation [online]. UK Transplant. April 2003 [accessed 14 February 2004]. <http://www.uktransplant.org.uk/newsroom/policy_and_statements/policy_documents/ uk_hospital_policy_for_donation.pdf>. Murali B, Vuylsteke A, Latimer RD. Anaesthetic management of the multi-organ donor. Annals of Cardiac Anaesthesia 2003;6(1):31–4. Mathew TH. The organ shortage: What are Australian organ sharing organizations doing about it? Transplantation Proceedings, 1997;29(8):3209. Twenty-Fifth Report of the Standing Committee on Uniform Legislation and Intergovernmental Agreements. Legislative Assembly, Parliament of Western Australia, Perth, Australia. 2000. Snell GI, Griffiths A, Macfarlane L, Gabbay E, Shiraishi T, Esmore DS, Williams TJ. Maximizing thoracic organ transplant opportunities: The importance of efficient coordination. Journal of Heart and Lung Transplantation 2000;19(4):401–7. Scheinkestel CD, Tuxen DV, Cooper DJ, Butt W. Medical management of the (potential) organ donor. Anaesthesia Intensive Care 1995;23(1):51–9. About Eurotransplant [online]. Eurotransplant. No date [accessed 14 February 2004]. <http://www.transplant.org/index.php?id=about>. Van Gelder F. Personal correspondence with author, 20 January 2004. 52