product information
advertisement

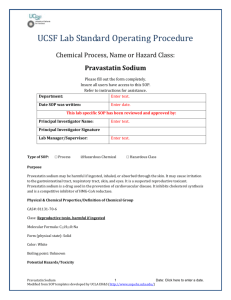
PRODUCT INFORMATION Pravastatin-RLTM TABLETS Name of the Drug Pravastatin sodium Description Chemical name: sodium (3R,5R)-7- [(1S,2S,6S,8S,8aR)- 1,2,6,7,8,8a- hexahydro-6hydroxy- 2-methyl-8-[(S)-2- methylbutyryloxy- 1-naphthyl]]-3,5- dihydroxyheptanoic acid. Pravastatin sodium is an odourless, white to off-white, fine or crystalline powder. It is a relatively polar hydrophilic compound with a partition coefficient (octanol/water) of 0.59 at a pH of 7.0. It is soluble in methanol and water (> 300 mg/mL), slightly soluble in isopropanol, and practically insoluble in acetone, acetonitrile, chloroform and ether. NaOOC OH HO O O CH3 H CH3 HO CAS: 81131-70-6. C23H35NaO7 MW: 446.52. Pravastatin-RLTM tablets also contain as inactive ingredients: Calcium hydrogen phosphate anhydrous, sodium starch glycollate, microcrystalline cellulose, trometamol, dibasic sodium phosphate dihydrate, povidone, magnesium stearate, ferric oxide. Pharmacology Pharmacodynamics Actions Pravastatin is one of a new class of lipid lowering compounds, the HMG-CoA reductase inhibitors, that reduce cholesterol biosynthesis. These agents are competitive inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the enzyme catalysing the early rate limiting step in cholesterol biosynthesis, conversion of HMGCoA to mevalonate. Pharmacology Pravastatin produces its lipid lowering effect in two ways. Firstly, as a consequence of its reversible inhibition of HMG-CoA reductase activity, it affects modest reductions in intracellular pools of cholesterol. This results in an increase in the number of low density lipoprotein (LDL) receptors on cell surfaces and enhanced receptor mediated catabolism and clearance of circulating LDL. Secondly, pravastatin inhibits LDL production by inhibiting hepatic synthesis of very low density lipoprotein (VLDL), the LDL precursor. Clinical and pathological studies have shown that elevated levels of total cholesterol (total-C), low density lipoprotein cholesterol (LDL-C) and apolipoprotein B (a membrane transport complex for LDL) promote human atherosclerosis. Similarly, decreased levels of high density lipoprotein (HDL) cholesterol (HDL-C) and its transport complex, apolipoprotein A, are associated with the development of atherosclerosis. Epidemiological investigations have established that cardiovascular morbidity and mortality vary directly with the level of total-C and LDL-C and inversely with the level of HDL-C. In multicentre clinical trials those pharmacological and/or non-pharmacological interventions that lowered total-C and LDL-C and increased HDL-C reduced the rate of cardiovascular events (both fatal and nonfatal myocardial infarctions) and improved survival. In both normal volunteers and patients with hyper-cholesterolaemia, treatment with pravastatin reduced total-C, LDL-C, apolipoprotein B, VLDL-C and triglycerides (TG) while increasing HDL-C and apolipoprotein A. The effects of HMG-CoA reductase inhibitors on lipoprotein A, fibrinogen and certain other independent biochemical risk markers for coronary heart disease are unknown. Pravastatin is a hydrophilic HMG-CoA reductase inhibitor. Clinical trials Hypercholesterolaemia: In controlled trials in patients with moderate hyper-cholesterolaemia, with or without atherosclerotic cardiovascular disease, pravastatin monotherapy reduced the progression of atherosclerosis and cardiovascular events (e.g. fatal and nonfatal myocardial infarction) or death. Pravastatin is highly effective in reducing total-C and LDL-C in patients with heterozygous familial, familial combined and nonfamilial (nonFH) forms of hypercholesterolaemia. A therapeutic response is seen within one week, and the maximum response usually is achieved within four weeks. This response is maintained during extended periods of therapy. A single daily dose administered in the evening is as effective as the same total daily dose given twice a day. Once daily administration in the evening appears to be marginally more effective than once daily administration in the morning, perhaps because hepatic cholesterol is synthesised mainly at night. In multicentre, double blind, placebo controlled studies of patients with primary hypercholesterolaemia, treatment with pravastatin significantly decreased total-C, LDLC, and total-C/HDL-C and LDL-C/HDL-C ratios, decreased VLDL-C and plasma TG levels, and increased HDL-C. Whether administered once or twice daily, a clear dose response relationship (i.e. lipid lowering) was seen by one to two weeks following the initiation of treatment (see Table 1). Table 1 Primary hypercholesterolaemia study: dose response of pravastatin* given once daily at bedtime. Dose 10mg 20mg 40mg Total cholesterol -16% -24% -25% LDL cholesterol -22% -32% -34% HDL cholesterol +7% +2% +12% Triglycerides -15% -11% -24% *Percent change from baseline after 8 weeks Pravastatin, in combination with diet, has been shown to reduce the incidence of cardiovascular events (e.g. fatal and nonfatal myocardial infarction). The mechanism responsible for the beneficial effects of pravastatin in hypercholesterolaemic patients is not known. Atherosclerosis: In the Pravastatin Limitation of Atherosclerosis in the Coronary Arteries (PLAC I) study, the effect of pravastatin therapy on coronary atherosclerosis was assessed by coronary angiography in patients with coronary disease and moderate hyper-cholesterolaemia (baseline LDL-C range 3.4 to 4.9 mmol/L). In this double blind, multicentre, controlled clinical trial in which 408 patients were randomised, angiograms were evaluated at baseline and at three years in 264 patients. No statistically significant difference between pravastatin and placebo was seen for the primary endpoint (per patient change in mean coronary artery diameter), or for one of two secondary endpoints (change in percent lumen diameter stenosis). For the other secondary endpoint (change in minimum lumen diameter), statistically significant slowing of disease was seen in the pravastatin treatment group (p = 0.02). Although the trial was not designed to assess clinical coronary events, for myocardial infarction (fatal and nonfatal) the event rate was reduced in the pravastatin group by a statistically significant margin (10.5% for placebo versus 4.2% for pravastatin, p = 0.0498). In another three year, double blind, placebo controlled, randomised trial in patients with mild to moderate hyperlipidaemia, the Pravastatin, Lipids and Atherosclerosis in the Carotids (PLAC II) study, the effect of pravastatin therapy on carotid atherosclerosis was assessed by B-mode ultrasound. No statistically significant differences were seen in the carotid bifurcation, internal carotid artery, or all segments combined (the primary endpoint); pravastatin did reduce the increase in wall thickness in the common carotid artery (p = 0.02). Although the study was not designed to assess cardiovascular events or mortality, the event rates were reduced in the pravastatin treatment group by statistically significant margins for two combined endpoints: nonfatal or fatal myocardial infarction (13.3% for placebo versus 2.7% for pravastatin, p = 0.018) and nonfatal myocardial infarction or all deaths (17.1% for placebo versus 6.7% for pravastatin, p = 0.049). Analysis of pooled events from PLAC I and PLAC II showed that treatment with pravastatin was associated with a 67% reduction in the event rate of fatal and nonfatal myocardial infarction (11.4% for placebo versus 3.8% for pravastatin, p = 0.003) and 55% for the combined endpoint of nonfatal myocardial infarction or death from any cause (13.8% for placebo versus 6.2% for pravastatin, p = 0.009). Divergence in the cumulative event rate curves began at one year and was statistically significant at two years. In consideration of the results of PLAC I and PLAC II, it is important to be aware of the limitations of angiography in defining the extent and site of atherosclerosis plaque. Acute coronary events tend to occur not at the site of severe stenosis, but at lesser stenoses which are lipid rich and more prone to rupture. In addition, angiographic changes are not properly validated endpoints to measure morbidity and/or mortality in patients with atherosclerotic coronary artery disease associated with hypercholesterolaemia. Prevention of coronary heart disease: Pravastatin is effective in reducing the risk of coronary heart disease death (fatal myocardial infarction and sudden death) and nonfatal myocardial infarction and improving survival in hypercholesterolaemic male patients without previous myocardial infarction. The West of Scotland (WOS) study was a randomised, double blind, placebo controlled trial among 6,595 male patients (45 to 64 years) with moderate to severe hypercholesterolaemia (LDL-C = 4 to 6.6 mmol/L), a total fasting cholesterol > 6.5 mmol/L, and without previous myocardial infarction. Patients were treated with standard care, including dietary advice, and either pravastatin 40 mg (n = 3,302) or placebo (n = 3,293) each evening for a median duration of 4.8 years. The study was designed to assess the effect of pravastatin on fatal and nonfatal coronary heart disease. Significant results (p < 0.05) are given in Table 2. Table 2 West of Scotland study results Endpoint Events prevented per 1,000 patients treated with pravastatin for 5 years* 19 Relative risk reduction Cardiovascular death 7 28% Death (any cause) 9 22% Coronary heart disease death or nonfatal myocardial infarction Coronary angiography 24 31% 14 31% 8 37% Non-fatal myocardial infarction Coronary angioplasty or coronary artery bypass graft 31% *Based on the Kaplan-Meier estimates of 5 years event rate The effect on the combined endpoint of coronary heart disease death or nonfatal myocardial infarction was evident as early as six months after beginning pravastatin therapy. There was no statistically significant difference between treatment groups in noncardiovascular mortality, including cancer death (see Table 3 and Figure 1). Table 3 West of Scotland study: effect of pravastatin on plasma lipids (mmol/L) (intention to treat analysis) Year 5 mean n = 1335 3.8 % Change mean* LDL-cholesterol Baseline mean n=3302 5.0 HDL-cholesterol 1.1 1.3 10.1 Total cholesterol 7.0 5.8 -18.6 Triglycerides 1.9 1.8 -4.4 -24.9 *All changes statistically significant (p<0.001) Figure 1 Myocardial infarction and unstable angina pectoris: Pravastatin is effective in reducing the risk of a fatal coronary event and nonfatal myocardial infarction in patients with a previous myocardial infarction and average (normal) serum cholesterol, who are > 65 years of age and whose serum LDL cholesterol is > 3.36 mmol/L. Pravastatin is effective in reducing the frequency of stroke in patients with a previous myocardial infarction and average (normal) serum cholesterol. Pravastatin is also effective in reducing the risk of total mortality, coronary heart disease death, and recurrent coronary events (including myocardial infarction) in patients with unstable angina pectoris. In the Cholesterol and Recurrent Events (CARE) study the effect of pravastatin on coronary heart disease death and nonfatal myocardial infarction was assessed in 4,159 men and women with average (normal) serum cholesterol levels (baseline mean total C=209 mg/dL) (5.4 mmol/L), and who had experienced a myocardial infarction in the preceding 3 to 20 months. Patients in this double blind, placebo controlled study participated for an average of 4.9 years. Treatment with pravastatin significantly reduced the rate of a recurrent coronary event (either CHD death or nonfatal myocardial infarction) by 24 % (p = 0.003). This risk reduction was statistically significant in those patients aged 65 years of age or older, and in those who demonstrated a serum LDL cholesterol of > 3.36 mmol/L. The reduction in risk for this combined endpoint was significant for both men and women. The risk of undergoing revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) was significantly reduced by 27% (p < 0.001) in the pravastatin treated patients. Pravastatin also significantly reduced the risk for stroke by 32% (p = 0.032), and stroke or transient ischemic attack (TIA) combined by 26% (p = 0.025). At baseline, 84% of patients were receiving aspirin and 82% were taking antihypertensive medications. The comparison of the primary, secondary and tertiary endpoints for the study are summarised in Table 4. Table 4 Cholesterol and Recurrent Event (CARE) study: effect of pravastatin on CHD and nonfatal MI Event Fatal CHD or definite* nonfatal Fatal CHD Total mortality Number (%a) of subjects Pravastatin (n= 2,081) 212 (10.4) Placebo (n = 2,078) 274 (13.3) 96 (4.9) 180 (8.6) Avoided eventsd Risk reductionb Logrank 95% Cl p-valuec 29 24 (9, 36) 0.003 119 (5.6) 7 20 (-5, 39) 0.104 196 (9.4) 8 9 (-12, 26) 0.366 a Kaplan-Meier estimate of 5 year event rate. Due to treatment with pravastatin by Cox proportional hazards model. c Mantel-Haenszel logrank p-value for between group difference of cumulative event curves d Per 1000 subjects on pravastatin over 5 years. * The term ‘definite’ refers to a report of a clinical MI by a clinical centre that meets that criteria of MI described in the Manual of Operations as determined by review by the MI Confirmation Centre. b In the Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) study, the effect of pravastatin 40 mg daily was assessed in 9,014 men and women with normal to elevated serum cholesterol levels (baseline total C = 4.0 to 7.0 mmol/L; mean total C=5.66 mmol/L; mean total C/HDL C ratio = 5.9), and who had experienced either a myocardial infarction or had been hospitalised for unstable angina pectoris in the preceding 3 to 36 months. Patients with a wide range of baseline levels of triglycerides were included (less than or equal to 5.0 mmol/L) and enrolment was not restricted by baseline levels of HDL cholesterol. At baseline, 82% of patients were receiving aspirin, 76% were receiving antihypertensive medication, and 41% had undergone myocardial revascularisation. Patients in this multicentre, double blind, placebo controlled study participated for a mean of 5.6 years (median = 5.9 years). Treatment with pravastatin significantly reduced the risk for CHD death by 24% (p = 0.0004). The risk for coronary events (either CHD death or nonfatal myocardial infarction) was significantly reduced by 24% (p < 0.0001) in the pravastatin treated patients. The risk for fatal or nonfatal myocardial infarction was reduced by 29% (p < 0.0001). Pravastatin reduced both the risk for total mortality by 23% (p < 0.0001) and cardiovascular mortality by 25% (p < 0.0001). The risk for undergoing myocardial revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) was significantly reduced by 20% (p < 0.0001) in the pravastatin treated patients. Pravastatin also significantly reduced the risk for stroke by 19% (p = 0.0477). Treatment with pravastatin significantly reduced the number of days of hospitalisation per 100 person years of follow-up by 15% (p < 0.001). The prespecified subgroup (age, sex, hypertensives, diabetics, smokers, lipid subgroups) analyses were conducted using the combined endpoint of CHD and nonfatal myocardial infarction. The study was not powered to examine results within each subgroup but formal testing for heterogeneity of treatment effect was undertaken across each of the subgroups and no significant heterogeneity was found (p greater than or equal to 0.08), i.e. a consistent treatment effect was seen with pravastatin therapy across all patient subgroups and event parameters. Among patients who qualified with a history of myocardial infarction, pravastatin significantly reduced the risk for total mortality by 25% (p = 0.0016); for CHD mortality by 23% (p = 0.004); for CHD events by 22% (p = 0.002) and for fatal or nonfatal myocardial infarction by 25% (p = 0.0008). Among patients who qualified with a history of hospitalisation for unstable angina pectoris, pravastatin significantly reduced the risk for total mortality by 26% (p = 0.0035); for CHD mortality by 26% (p = 0.0358); for CHD events by 29% (p = 0.0001) and for fatal or nonfatal myocardial infarction by 37% (p = 0.0003). The results of the LIPID study are shown in Table 5. Table 5 Comparison of event rates by treatment group (primary, secondary and tertiary efficacy measures) in the LIPID study. Event Number (%a) of subjects CHD mortality Pravastatin (n= 4,512) 287 (5.3) Placebo (n = 4,502) 373 (6.4) Total mortality 498 (8.9) CHD mortality or non-fatal MI Stroke All cause Nonhaemorrhagic Cardiovascular mortality Myocardial revascularization procedures (CABG or PTCA) Atherosclerotic events Fatal or non-fatal MI Avoided eventsd Risk reductionb Logrank (95% Cl) p-valuec 11 24% (12.35) 0.0004 633 (10.5) 16 23% (13.31) <0.0001 557 (10.5) 715 (13.5) 27 24% (15.32) <0.0001 169 (3.0) 154 (2.7) 204 (3.9) 196 (3.8) 9 11 19% (0.34) 23% (5.38) 0.0477 0.0154 331 (6.0) 433 (7.5) 15 25% (13.35) <0.0001 584 (11.4) 706 (14.1) 27 20% (10.28) <0.0001 1.116 (21.2) 1.352 (25.6) 44 21% (14.27) <0.0001 336 (6.5) 463 (9.0) 25 29% (18.38) <0.0001 a Kaplan-Meier estimate of 5 year event rate. Due to treatment with pravastatin by an unadjusted Cox proportional hazards model. c Stratified Mantel-Haenszel logrank P-value for between group difference of cumulative curves, stratified by qualifying event (MI or UAP at randomization). d Per 1000 subjects on pravastatin over 5 years. b Solid organ transplantation: The safety and efficacy of pravastatin treatment in patients receiving immunosuppresive therapy following kidney and cardiac transplantation were assessed in two prospective randomised controlled trials. Patients were treated concurrently with either 20 or 40 mg pravastatin and a standard immunosuppresive regimen of cyclosporin and prednisone. Cardiac transplant patients also received azathioprine as part of their immunosuppresive regimen. Plasma lipid levels were reduced in patients who received pravastatin. In the patients who received pravastatin in these trials (n = 71) no significant increases in creatinine phosphokinase or hepatic transaminases were observed and there were no cases of myositis and rhabdomyolysis. However, there are limited data available on the incidence of these adverse events in transplant patients and doctors should consider the risk of myositis and rhabdomyolysis when prescribing pravastatin therapy for hyperlipidaemia in transplant patients. Pharmacokinetics Pravastatin is administered orally in the active form. It is rapidly absorbed, with peak plasma levels attained 1 to 1.5 hours following ingestion. Based on urinary recovery of radiolabelled drug, the average oral absorption of pravastatin is 34% and absolute bioavailability is 17%. Pravastatin undergoes extensive first-pass extraction in the liver (extraction ratio 0.66), which is its primary site of action, and the primary site of cholesterol synthesis and of LDL-C clearance. Since it is excreted in the bile, plasma levels are of limited value in predicting therapeutic effectiveness. Pravastatin plasma concentrations (including area under the concentration time curve (AUC), peak (Cmax) and steady-state minimum (Cssmin)) are directly proportional to the administered dose. Steady-state AUCs, Cmax and Cssmin plasma concentrations showed no evidence of pravastatin accumulation following once or twice daily administration of pravastatin tablets. Approximately 50% of the circulating drug is bound to plasma proteins. The plasma elimination half-life (t1/2) of pravastatin (oral) is between 1.5 and 2 hours. Approximately 20% of a radiolabelled oral dose is excreted in urine and 70% in the faeces. After intravenous administration of radiolabelled pravastatin to normal volunteers, approximately 47% of total body clearance was via renal excretion and 53% by nonrenal routes (i.e. biliary excretion and biotransformation). Accumulation of drug and/or metabolites may occur in patients with renal or hepatic insufficiency, although, as there are dual routes of elimination, the potential exists for compensatory excretion by the alternate route. The major metabolite of pravastatin is the 3alpha-hydroxy isomer. This metabolite has one-tenth to one-fortieth the HMG-CoA reductase inhibitory activity of the parent compound. Indication As an adjunct to diet for the treatment of hypercholesterolaemia. Prior to initiating therapy with pravastatin, secondary causes of hypercholesterolaemia (e.g. poorly controlled diabetes mellitus, hypothyroidism, nephrotic syndrome, dysproteinaemias, obstructive liver disease, other drug therapy, alcoholism) should be identified and treated. Patients with previous myocardial infarction including those who have normal (4.0 to 5.5mmol/L) serum cholesterol levels. Patients with unstable angina pectoris (see Actions, Clinical Trials). Contraindications Hypersensitivity to any component of this medication. Active liver disease or unexplained persistent elevations in liver function tests. Use in pregnancy Atherosclerosis is a chronic process and discontinuation of lipid lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hypercholesterolaemia. Cholesterol and other products of cholesterol biosynthesis are essential components for fetal development (including synthesis of steroids and cell membranes). Since HMG-CoA reductase inhibitors decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, they may cause fetal harm when administered to a pregnant woman. Therefore, HMGCoA reductase inhibitors are contraindicated during pregnancy. Safety in pregnant women has not been established. Although pravastatin was not teratogenic in rats at doses as high as 1,000 mg/kg daily nor in rabbits at doses of up to 50 mg/kg daily, pravastatin should be administered to women of childbearing potential only when such patients are highly unlikely to conceive and have been informed of the potential hazards. If a woman becomes pregnant while taking pravastatin, it should be discontinued and the patient advised again as to the potential hazards to the fetus. Women of childbearing potential Pravastatin should not be administered to women of childbearing age unless using effective contraception and are highly unlikely to conceive, and have been informed of the potential hazards. If the patient becomes pregnant while taking this class of drug, therapy should be discontinued and the patient again advised of the potential hazard to the fetus. Precaution Use with caution in the following circumstances General Pravastatin may elevate creatine phosphokinase and transaminase levels (see Adverse Reactions). This should be considered in the differential diagnosis of chest pain in a patient on therapy with pravastatin. Homozygous familial hypercholesterolaemia Pravastatin has not been evaluated in patients with rare homozygous familial hypercholesterolaemia. In this group of patients, it has been reported that HMG-CoA reductase inhibitors are less effective because the patients lack functional LDL receptors. Hypertriglyceridaemia Pravastatin has only a moderate triglyceride lowering effect and it is not indicated where hypertriglyceridaemia is the abnormality of most concern (i.e. hypertriglyceridaemia types I, IV and V). Thyroid function Serum thyroxine was studied in 661 patients who were administered pravastatin in five controlled clinical trials. From observations of up to two years in duration, no clear association was found between pravastatin use and changes in thyroxine levels. Impaired renal function: A single oral dose of pravastatin 20 mg was administered to 24 patients with varying degrees of renal impairment (as determined by creatinine clearance). No effect was observed on the pharmacokinetics of pravastatin or its 3alphahydroxy isomeric metabolite (SQ 31,908). A small increase was seen in mean AUC values and half-life (1.5) for the inactive enzymatic ring hydroxylation metabolite (SQ 31,945). Given this small sample size, the dosage administered, and the degree of individual variability, patients with renal impairment who are receiving pravastatin should be closely monitored. Impaired hepatic function HMG-CoA reductase inhibitors have been associated with biochemical abnormalities of liver function. As with other lipid lowering agents, marked persistent increases (greater than three times the upper limit of normal) in serum transaminases were seen in 1.3% of patients treated with pravastatin in the US for an average period of 18 months. These elevations were not associated with clinical signs and symptoms of liver disease and usually declined to pretreatment levels upon discontinuation of therapy. Only two patients had marked persistent abnormalities possibly attributable to therapy. The significance of these changes, which usually appear during the first few months of treatment initiation, is not known. In the majority of patients treated with pravastatin in clinical trials, these increased values declined to pretreatment levels despite continuation of therapy at the same dose. These biochemical findings are usually asymptomatic although worldwide experience indicates that anorexia, weakness and/or abdominal pain may also be present in rare patients. As with other lipid lowering agents, liver function tests should be performed periodically. Special attention should be given to patients who develop increased transaminase levels. Liver function tests should be repeated to confirm an elevation and subsequently monitored at more frequent intervals. If increases in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) equal or exceed three times the upper limit of normal and persist, therapy should be discontinued. Caution should be exercised when pravastatin is administered to patients with a history of liver disease or heavy alcohol ingestion. Such patients should be closely monitored, started at the lower end of the recommended dosing range, and titrated to the desired therapeutic effect. Skeletal muscle Myalgia, myopathy and rhabdomyolysis have been reported with the use of HMG-CoA reductase inhibitors. Uncomplicated myalgia has been reported in pravastatin treated patients. Myopathy, defined as muscle aching or muscle weakness in conjunction with increases in creatine phosphokinase (CPK) values to greater than ten times the upper limit of normal, was reported to be possibly due to pravastatin in < 0.1% of patients in clinical trials. Rhabdomyolysis with renal dysfunction secondary to myoglobinuria has also very rarely been reported with pravastatin. However, myopathy should be considered in any patients with diffuse myalgia, muscle tenderness or weakness, and/or marked elevation of CPK. Patients should be advised to report promptly unexplained muscle pain, tenderness or weakness. Pravastatin therapy should be discontinued if markedly elevated CPK levels occur or myopathy is suspected or diagnosed. (Pravastatin therapy should also be temporarily withheld in any patient experiencing an acute or serious condition predisposing to the development of renal failure secondary to rhabdomyolysis, e.g. sepsis, hypotension, major surgery, trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy.) The risk of myopathy during treatment with another HMG-CoA reductase inhibitor is increased with concurrent therapy with either fibrates, cyclosporin, erythromycin or nicotinic acid. The use of fibrates alone is occasionally associated with myopathy. In a limited size clinical trial of combined therapy with pravastatin (40 mg/day) and gemfibrozil (1,200 mg/day) myopathy was not reported, although a trend towards CPK elevations and musculoskeletal symptoms was seen. The combined use of pravastatin and fibrates should generally be avoided. Myopathy has not been observed in three post-transplant clinical trials which had involved a total of 100 patients (76 cardiac and 24 renal). Some patients have been treated for up to two years with pravastatin (10 to 40 mg) and cyclosporin, with or without other immunosuppressants. In a separate lipid lowering trial involving 158 patients, no myopathy has been reported with pravastatin in combination with niacin. Endocrine function HMG-CoA reductase inhibitors interfere with cholesterol synthesis and lower circulating cholesterol levels, and, as such, might theoretically blunt adrenal or gonadal steroid hormone production. Results of clinical trials with pravastatin in males and postmenopausal females were inconsistent with regard to possible effects of the drug on basal steroid hormone levels. In a study of 21 males, the mean testosterone response to human chorionic gonadotrophin was significantly reduced (p < 0.004) after 16 weeks of treatment with pravastatin 40 mg. However, the percentage of patients showing a greater than 50% rise in plasma testosterone after human chorionic gonadotrophin stimulation did not change significantly after therapy in these patients. The effects of HMG-CoA reductase inhibitors on spermatogenesis and fertility have not been studied in adequate numbers of patients. The effects, if any, of pravastatin on the pituitary-gonadal axis in premenopausal females are unknown. Patients treated with pravastatin who display clinical evidence of endocrine dysfunction should be evaluated appropriately. Caution should also be exercised if an HMG-CoA reductase inhibitor or other agent used to lower cholesterol levels is administered to patients also receiving other drugs (e.g. ketoconazole, spironolactone, cimetidine) that may diminish the levels of activity of steroid hormones. Central nervous system toxicity CNS vascular lesions, characterised by perivascular haemorrhage and oedema and mononuclear cell infiltration of perivascular spaces, were seen in dogs treated with pravastatin at a dose of 25 mg/kg/day, a dose that produced a plasma drug level about 50 times higher than the mean drug level in humans taking 40 mg/day. Similar CNS vascular lesions have been observed with several other drugs in this class. A chemically similar drug in this class produced optic nerve degeneration (Wallerian degeneration of retinogeniculate fibres) in clinically normal dogs in a dose dependent fashion starting at 60 mg/kg/day, a dose that produced mean plasma drug levels about 30 times higher than the mean drug level in humans taking the highest recommended dose (as measured by total enzyme inhibitory activity). This same drug also produced vestibulocochlear Wallerian-like degeneration and retinal ganglion cell chromatolysis in dogs treated for 14 weeks at 180 mg/kg/day, a dose which resulted in a mean plasma drug level similar to that seen with the 60 mg/kg dose. Hypersensitivity With lovastatin an apparent hypersensitivity syndrome has been reported rarely which has included one or more of the following features: anaphylaxis, angioedema, lupus-like syndrome, polymyalgia rheumatica, thrombocytopenia, leucopenia, haemolytic anaemia, positive antinuclear antibody (ANA), erythrocyte sedimentation rate (ESR) increase, arthritis, arthralgia, urticaria, asthenia, photosensitivity, fever and malaise. Although to date hypersensitivity syndrome has not been described as such, in a few instances eosinophilia and skin eruptions appear to be associated with pravastatin treatment. If hypersensitivity is suspected pravastatin should be discontinued. Patients should be advised to report promptly any signs of hypersensitivity such as angioedema, urticaria, photosensitivity, polyarthralgia, fever or malaise. Use in the elderly Pharmacokinetic evaluation of pravastatin in patients over the age of 65 years indicates an increased AUC. There were no reported increases in the incidence of adverse effects in these or other studies involving patients in that age group. As a precautionary measure, the lowest dose should be administered initially. Use in children Safety and effectiveness in individuals less than 18 years old have not been established. Hence treatment in patients less than 18 years old is not recommended at this time. Carcinogenesis, mutagenesis, impairment of fertility. In a two year oral study of rats, a statistically significant increase in the incidence of hepatocellular carcinomas was observed in male rats given pravastatin 100 mg/kg/day. This change was not seen in male rats given 40 mg/kg or less, or in female rats at doses up to 100 mg/kg/day. Increased incidences of hepatocellular carcinomas were also observed in male and female mice dosed with pravastatin at 250 and 500 mg/kg/day, but not at 100 mg/kg/day or less. An increased incidence of pulmonary adenomas was seen in female mice dosed at 250 mg/kg/day. The AUC value for the serum concentration of pravastatin at the no effect dose level of 100 mg/kg/day in mice was 5.5 times higher than that in humans receiving pravastatin 40 mg/day. The hepatocarcinogenic effect of pravastatin in rats is associated with proliferation of hepatic peroxisomes. Other HMG-CoA reductase inhibitors (simvastatin and lovastatin) also induce hepatic peroxisome proliferation and hepatocellular carcinomas in rats and mice. The clinical significance of these findings is unclear. In six genetic toxicology studies performed with pravastatin, there was no evidence of mutagenic potential at the chromosomal or gene level. In a study in rats with a daily dose up to 500 mg/kg, pravastatin did not produce any adverse effects on fertility or general reproductive performance. The clinical significance of these findings is not clear. Use in pregnancy Category D - Drugs which have caused, are suspected to have caused or may be expected to cause an increased incidence of human foetal malformations or irreversible damage. HMG-CoA reductase inhibitors are contraindicated in pregnancy. The risk of foetal injury outweighs the benefits of HMG-CoA reductase inhibitor therapy during pregnancy. In two series of 178 and 143 cases where pregnant women took a HMG-CoA reductase inhibitor (statin) during the first trimester of pregnancy, serious foetal abnormalities occurred in several cases. These included limb and neurological defects, spontaneous abortions and foetal deaths. The exact risk of injury to the foetus occurring after a pregnant women is exposed to a HMG-CoA reductase inhibitor has not been determined. The current data do not indicate that the risk of foetal injury in women exposed to HMG-CoA reductase inhibitors is high. If a pregnant woman is exposed to a HMG-CoA reductase inhibitor, she should be informed of the possibility of foetal injury and discuss the implications with her pregnancy specialist. Also see Contraindications. Use in lactation A negligible amount of pravastatin is excreted in human breast milk. Because of the potential for adverse reactions in breastfeeding infants, if the mother is being treated with pravastatin, breastfeeding should be discontinued. Drug Interactions Gemfibrozil: In a crossover study in 20 healthy male volunteers given concomitant single doses of pravastatin and gemfibrozil, there was a significant decrease in urinary excretion and protein binding of pravastatin. In addition, there was a significant increase in AUC, Cmax and Tmax for the pravastatin metabolite SQ 31,906. Combination therapy with pravastatin and gemfibrozil is generally not recommended. Cholestyramine/colestipol: When pravastatin was administered one hour before or four hours after cholestyramine or one hour before colestipol and a standard meal, there was no clinically significant decrease in bioavailability or therapeutic effect. Concomitant administration resulted in an approximately 40 to 50% decrease in the mean AUC of pravastatin (see Dosage and Administration). Cyclosporin: In a single dose study, pravastatin levels were found to be increased in cardiac patients receiving cyclosporin. In a second multidose study in renal transplant patients receiving cyclosporin, pravastatin levels were higher than those seen in healthy volunteer studies. This does not appear to be a metabolic interaction involving P450 3A4. Warfarin: With concomitant administration, pravastatin did not alter the plasma protein binding of warfarin. Chronic dosing of the two drugs did not produce any changes in the anticoagulant status. Antipyrine: Clearance by the cytochrome P450 system was unaltered by concomitant administration of pravastatin. Since pravastatin does not appear to induce hepatic drug metabolising enzymes, it is not expected that any significant interaction of pravastatin with other drugs metabolised by the cytochrome P450 system (e.g. phenytoin, quinidine) will occur. Other drugs: Unlike simvastatin and atorvastatin, pravastatin is not significantly metabolised in vivo by cytochrome P450 3A4. Therefore, plasma concentrations of pravastatin are not significantly elevated when cytochrome P450 3A4 is inhibited by agents such as diltiazem and itraconazole. In interaction studies with aspirin, gemfibrozil, nicotinic acid or probucol, no statistically significant differences in bioavailability were seen when pravastatin was administered. In other interaction studies, antacids (one hour prior to pravastatin) reduced and cimetidine increased the bioavailability of pravastatin; these changes were not statistically significant. During clinical trials, no noticeable drug interactions were reported when pravastatin was added to diuretics, antihypertensives, digitalis, angiotensin converting enzyme inhibitors, calcium channel blockers, beta-blockers or nitroglycerins. Adverse Reactions Pravastatin is generally well tolerated. Adverse events, both clinical and laboratory, are usually mild and transient. In all clinical studies (controlled and uncontrolled), approximately 2% of patients were discontinued from treatment due to adverse experiences attributable to pravastatin. In seven randomised double blind, placebo controlled trials involving over 21,500 patients treated with pravastatin (N = 10,784) or placebo (N = 10,719), the safety and tolerability in the pravastatin group was comparable to that of the placebo group. Over 19,000 patients were followed for a median of 4.8 to 5.9 years, while the remaining patients were followed for two years or more. Clinical adverse events probably or possibly related, or of uncertain relationship to therapy, occurring in at least 0.5% of patients treated with pravastatin or placebo in these long-term morbidity/ mortality trials are shown in Table 6. Table 6 Percentage of patients with clinical adverse experiences in placebo controlled trials Cardiovascular Angina pectoris Disturbance rhythm (subjective) Hypertension Oedema Mycocardial Infraction Dermatological Rash Pruritus Endocrine/metabolic Sexual dysfunction Gastrointestinal Dyspepsia/heartburn Nausea/vomiting Flatulence Constipation Diarrhoea Abdominal pain Abdominal distension Pravastatin (n = 10, 784) (%) Placebo (n = 10, 719) (%) 3.1 0.8 0.7 0.6 0.5 3.4 0.7 0.9 0.6 0.7 2.1 0.9 2.2 1.0 0.7 0.7 3.5 1.4 1.2 1.2 0.9 0.9 0.5 3.7 1.6 1.1 1.3 1.1 1.0 0.5 General Fatigue Chest pain Weight gain Influenza Weight loss Weakness Musculoskeletal Musculoskeletal pain (including arthralgia) Muscle cramp Myalgia Musculoskeletal trauma Nervous Dizziness Headache Sleep disturbance Depression Anxiety/nervousness Paraesthesia Numbness Renal/genitourinary Abnormal urination (includes dysuria and nocturia) Respiratory Dyspnoea Upper respiratory infection Cough Sinus abnormality (includes sinusitis) Pharyngitis Special senses Vision disturbance (include blurred vision) Eye disturbance (includes eye inflammation) Hearing abnormality (includes tinnitus and hearing loss) Lens opacity 3.4 2.6 0.6 0.6 0.6 0.5 3.3 2.6 0.7 0.5 0.5 0.6 5.9 2.0 1.4 0.5 5.7 1.8 1.4 0.3 2.2 1.9 1.0 1.0 1.0 0.9 0.5 2.1 1.8 0.9 1.0 1.2 0.9 0.4 1.0 0.8 1.6 1.3 1.0 0.8 0.5 1.6 1.3 1.0 0.8 0.6 1.5 0.8 0.6 1.3 0.9 0.5 0.5 0.4 Lens: In 820 patients treated with Pravastatin for periods up to a year or more, there was no evidence that pravastatin was associated with cataract formation. In placebo controlled studies, 294 patients (92 on placebo/control, 202 on pravastatin) were evaluated using the Lens Opacity Classification System (a sophisticated method of lens assessment) at six months and one year following the initiation of treatment. When compared with the baseline evaluation, the final examination revealed the results in Table 7. Table 7 Lens evaluation results after one year of treatment Lens opacity changes Pravastatin Number of patients (%) (n = 202) 29 (14%) Placebo/control Number of patients (%) (n = 92) 13 (14%) No change 142 (70%) 63 (68%) Worsened 31 (15%) 16 (17%) Improved There was no statistically significant difference in the change in lens opacity between the control and pravastatin treatment groups during this time interval. Comparative data indicate that pravastatin is 100-fold less potent than both lovastatin and simvastatin (other HMG-CoA reductase inhibitors) in inhibiting cholesterol biosynthesis in rat lens and 40-fold less potent than lovastatin in inhibiting cholesterol biosynthesis in rabbit lens. Furthermore, unlike lovastatin and simvastatin, cataracts have not been observed in animal studies (beagle dogs) when chronic oral doses of pravastatin were administered for two years. In three large placebo controlled trials, West of Scotland Study (WOS), Cholesterol and Recurrent Events Study (CARE) and the Long-Term Intervention with pravastatin in Ischaemic Disease Study (LIPID) (see Actions, Clinical trials), involving a total of 19,786 patients treated with pravastatin (N = 9,895) or placebo (N = 9,873), the safety and tolerability profile in the pravastatin group was comparable to that of the placebo group over the median 4.8 to 5.9 years of follow up. The following effects have been reported with drugs in this class (not all the effects listed have necessarily been associated with pravastatin therapy). Skeletal: Myopathy, rhabdomyolysis, arthralgia. Neurological: Dysfunction of certain cranial nerves (including alteration of taste, impairment of extraocular movement, facial paresis), tremor, vertigo, memory loss, paraesthesia, peripheral neuropathy, peripheral nerve palsy, anxiety, insomnia, depression. Hypersensitivity reactions: An apparent hypersensitivity syndrome has been reported rarely which has included one or more of the following features: anaphylaxis, angioedema, lupus erythematosus-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, purpura, thrombocytopenia, leucopenia, haemolytic anaemia, positive ANA, ESR increase, eosinophilia, arthritis, arthralgia, urticaria, asthenia, photosensitivity, fever, chills, flushing, malaise, dyspnoea, toxic epidermal necrolysis, erythema multiforme, including Stevens-Johnson syndrome. Gastrointestinal: Pancreatitis, hepatitis, including chronic active hepatitis, cholestatic jaundice, fatty change in liver, and, rarely, cirrhosis, fulminant hepatic necrosis, and hepatoma; anorexia, vomiting. Skin Alopecia, pruritus. A variety of skin changes (e.g. nodules, discolouration, dryness of skin/ mucous membranes, changes to hair/ nails) have been reported. Reproductive: Gynecomastia, loss of libido, erectile dysfunction. Eye: Progression of cataracts (lens opacities), ophthalmoplegia. Laboratory abnormalities: Elevated transaminases, alkaline phosphatase and bilirubin; thyroid function abnormalities. Laboratory test abnormalities: Increases in serum transaminase (ALT, AST) values and CPK have been observed (see Precautions). Transient asymptomatic eosinophilia has been reported. Eosinophil counts usually returned to normal despite continued therapy. Anaemia, thrombocytopenia and leucopenia have been reported with HMG-CoA reductase inhibitors. Dosage and Administration Prior to initiating pravastatin, the patient should be placed on a standard cholesterol lowering diet (American Heart Association (AHA) Phase 1 or NCEP Step 1) for a maximum of three to six months, depending upon the severity of the lipid elevation. Dietary therapy should be continued during treatment. The recommended starting dose is 10 to 20 mg once daily at bedtime. In primary hypercholesterolaemic patients with significant renal or hepatic dysfunction, and in the elderly, a starting dose of 10 mg daily at bedtime is recommended. For maximum effect pravastatin should be taken at bedtime on an empty stomach. Since the maximal effect of a given dose is seen within four weeks, periodic lipid determinations should be performed at this time and dosage adjusted according to the patient's response to therapy and established treatment guidelines. The recommended dosage range is 10 to 40 mg administered once a day at bedtime. Pravastatin may be given in divided doses. For the prevention of coronary heart disease in patients with hypercholesterolaemia the dose is 40 mg per day as a single dose. The same dose is recommended for secondary prevention of myocardial infarction in patients with average (normal) serum cholesterol. In patients taking cyclosporin, with or without other immunosuppressive drugs, concomitantly with pravastatin, therapy should be initiated with 10 mg/day and titration to higher doses should be performed with caution. Concomitant therapy. Pravastatin has been administered concurrently with cholestyramine, colestipol, nicotinic acid, probucol and gemfibrozil. Preliminary data suggest that the addition of either probucol or gemfibrozil to therapy with lovastatin or pravastatin is not associated with greater reduction in LDL cholesterol than that achieved with lovastatin or pravastatin alone. No adverse reactions unique to the combination or in addition to those previously reported for each drug alone have been reported. Myopathy and rhabdomyolysis (with or without acute renal failure) have been reported when another HMG-CoA reductase inhibitor was used in combination with immunosuppressive drugs, gemfibrozil, erythromycin, or lipid lowering doses of nicotinic acid. Concomitant therapy with HMGCoA reductase inhibitors and these agents is generally not recommended. (See Precautions and Interactions.) Overdosage There has been limited experience with overdosage of pravastatin. To date there are two reported cases, both of which were asymptomatic and not associated with clinical laboratory test abnormalities. Of these two cases, one occurred in a clinical trial patient who ingested pravastatin 3 g; the other ingested pravastatin 280 mg as marketed tablets. Both cases also involved overdose of concomitant medications. Treatment: Should overdose occur, treat symptomatically and institute supportive measures as required. Presentation 10mg: A yellow, oval, convex, sidewall scored tablet encoded “P 10” 20mg: A yellow, oval, convex, sidewall scored tablet encoded “P 20” 40mg: A yellow, oval, convex, sidewall scored tablet encoded “P 40” Storage Conditions Store below 25°C. Protect from light and moisture. POISON SCHEDULE S4 NAME AND ADDRESS OF SPONSOR Real-RL A Division of GlaxoSmithKline Australia Pty Ltd 1061 Mountain Highway Boronia Victoria 3155 ™Pravastatin-RL is a trade mark of the GlaxoSmithKline group of companies. Date of TGA approval: 17 November 2005 Date of most recent amendment: 2 May 2006 Issue 1