Physician Update July 2015 - University Hospitals
advertisement

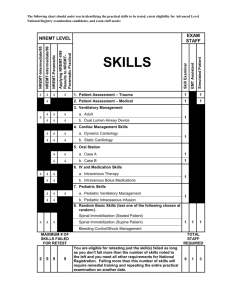
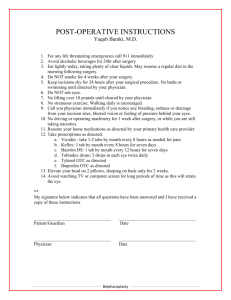
PHYSICIAN UPDATE News for University Hospitals physicians JULY 2015 INTRODUCING A New App for UH Physicians UH Physician Editorial Board Now there’s a new way for you and your UH colleagues to make referrals to one another. It is the physician-to-physician mobile app – called the UH Physician Directory App – which you can access now from Apple or Android phones. Richard Chang, MD Hematology and Oncology It’s easy to download the app to your phone; then you log in with your UH network user name and password. We emailed instructions to all physicians on June 24. operations easier. Your feedback is very important. To provide it, simply click on “Feedback” in the app itself, which you will find in the physician profile section. Phase I of this new app includes all UHPS physicians. In the future, we intend to add other physicians and practice managers. We’ll continuously be working to improve the process. PLEASE NOTE: YOU MUST USE AIRWATCH FOR ANY AND ALL EMAIL COMMUNICATIONS USING THIS APPLICATION. YOU MUST USE YOUR UH EMAIL ADDRESS TO SEND INFORMATION FROM THIS APPLICATION. USE OF ANY OTHER EMAIL ADDRESS IS PROHIBITED. PLEASE REFER TO UH POLICY GM-78 REGARDING EMAILING OF PROTECTED HEALTH INFORMATION FOR MORE DETAILS. Our new app enables you to look up physicians by name and specialty. You can create a “favorites” list of physicians you contact most often. There are tabs for UH Urgent Care locations, phone contact numbers for direct admission to UH hospitals (by site), regional emergency departments and hospital transfers. The physician-to-physician app is one of several initiatives to support clinical integration and make your practice If you have questions about using the app, contact Andrew.Laytin@UHhospitals.org. We also welcome any suggestions for future enhancements. Contact Cindy.Zelis@UHhospitals.org with your ideas. Associate Editors Rami Abbass, MD Gastroenterology Members May Al-Abousi, MD Internal Medicine Corinne Bazella, MD Obstetrics and Gynecology Philip D. Junglas, MD Internal Medicine Patricia Kellner, MD Family Medicine Sean McNeeley, MD Family Medicine Cliff Megerian, MD Otolaryngology – Head & Neck Surgery Erica E. Remer, MD Emergency Medicine Patrick Runnels, MD Psychiatry Martha Schinagle, MD Psychiatry Jay Shah, MD Otolaryngology – Head & Neck Surgery Jennifer Wurst, MD Family Medicine Physician Engagement Update During the past six months, considerable progress has been made in addressing key areas of improvement identified on the Physician Engagement Survey. Here are highlights from the past two months: COMMUNICATIONS Tools and Equipment • A new UH Physician Directory app was introduced on June 24. It provides direct contact information for physicians to reach UH doctors. This project is led by Cindy Zelis, MD, MBA. • L arge capital purchases include: • T he physician resource center (UHDoctor.org) is in final stages of development, with a launch date set for September 2015. The site has been mapped with both internally secure sections and external sections. The physician advisory group on the project includes Jeff Peters, MD, Cliff Megerian, MD, Evan Howe, MD, Mike Anderson, MD, and Conor Delaney, MD. • A Physician Editorial Board has been formed to help guide and contribute to physician communications. Rami Abbass, MD, and Richard Chang, MD, contributed articles to the June issue of Physician Update, and May Al-Abousi, MD, and Patrick Runnels, MD, have articles in this issue. – T elemetry system upgrade and expansion – U H bard microbiology system – ICU expansion (Neuroscience unit with enhanced EEG monitoring) – d aVinci® robotic upgrade – OR expansion – Ambulatory EMR servers and database upgrades • Minor capital purchases include: – O phthalmology OR equipment (finalizing quotes with practice administrator) – ENT OR suspension gallows – New orthopaedic operations OR power equipment – Endoscopic ultrasound – Westlake EMR – T rauma ED ultrasound machine, clinical response management system and Level 1 trauma rapid infuser/ fluid warmers • Ambulatory Enhancement Initiative “First 100 Days” effort: • Human Resources achievements: – U H IT and Allscripts have stabilized the system, with a significant reduction in unplanned downtime. – 1 71 new physicians have been recruited to UH this year. An additional 68 physicians have signed MOU/LOIs. – M ore than 1,300 employees and physicians have been engaged in EMR usage assessment to prioritize workflow and training needs. – T he Office of Physician Services has been implemented to support physician recruitment, onboarding and compensation. – More than 300 staff have been retrained on systems. – A n additional dedicated recruiter has been added to support the UHMP practices for office staff recruitment. – 6 5 practices have been scheduled for on-site “Elbow to Elbow” training. More than 200 physicians have already received training through this program. • S ecure messaging systems for physician-to-physician communications are being evaluated. – H uman Resources is implementing a systemwide process to redesign the onboarding experience, including the experience for physicians. Continued on next page UH Physician Update | UHhospitals.org | 2 The Next Time You Think About Hospice… By May Al-Abousi, MD – Medical Director, UH Hospice Medical Director, Palliative Care, UH Parma Medical Center Physician Engagement Update Continued from previous page Recognition and Voice The UH Primary Care Institute has established six regions with regional medical directors. These physician leaders provide voice, communication, leadership and guidance within their region. Since we started our own UH Hospice a year ago, we’ve faced the same challenges that other hospices face nationwide. I wanted to shed light on some key statistics to help us navigate the future of end-of-life care within the UH system. According to 2011 figures from the National Hospice and Palliative Care Organization (NHPCO), in 2010, almost 42 percent of all U.S. deaths – 1.5 million – involved hospice care. Here is the site breakdown: • C entral Region: Don Ebersbacher, MD, Jim Coviello, MD, and Denise Finkelstein, MD • Private residences 41 percent • N ortheast Region: Erika Mulligan, DO, and Yasser Mikhail, MD • Nursing homes 18 percent • N orthwest Region: Sona Kirpekar, MD, and Gary Dinger, DO • S outh Region: Joe Iemma, MD, and Karen Hummel, MD • S outheast Region: Brad Hillard, DO, and Larry Witmer, DO • S outhwest Region: George Topalsky, MD, and Marie Kychynski, MD • T he Center for Physician Leadership has been established for emerging physician leaders nominated by existing physician leaders. The center’s philosophy and objectives include: – E quipping physician leaders to drive and embrace change – Building skill and rigor in creating cost discipline – Enhancing ability to hardwire service excellence – Developing skills to lead with emotional intelligence – D efining a process for physician leaders to initiate breakthrough negotiations • T he UH Leadership Academy 2.0 includes 15 physicians, accounting for half of the class. • E xecutive leadership is continuing to leverage existing physician groups for personalized interactions and feedback. These groups include: • Inpatient hospice 22 percent • Acute-care facilities 11 percent • Residential facilities 7 percent Hospice often includes significant geriatric care, with 54 percent of hospice patients being 75 years or older. In 2010, the gender split was 56 percent female and 43 percent male. There were also more AfricanAmerican and Hispanic patients cared for in hospice than in previous years, at about 9 percent and 6 percent, respectively. The most common diagnoses in hospice differ from the most common causes of death in the United States. Both cancer and heart disease account for approximately one-quarter of U.S. deaths, in part because patients with heart disease and other chronic severe illnesses often fluctuate in the course of the disease in which the prognosis is relatively unpredictable. Therefore, meeting the prognostic criteria for hospice is more challenging. According to NHPCO data, the median length of stay in hospice was 19 days, although this varies dramatically by different regions in the United States. In fact, 35 percent of hospice patients received care for one week or less. – CMO Cabinet In 2015, we probably will find similar data, which sums up what we need to do as clinicians. The first and foremost principle is early diagnosis of the terminal illness and early referral to hospice care. – Voice of the Physician – UH Ahuja Medical Center Continued on next page – CEO Advisory Group – UHMG Department Town Halls UH Physician Update | UHhospitals.org | 3 The Next Time You Think About Hospice… Continued from previous page At UH, we’ve seen a decline in cancer patients in hospice for various reasons. Some of it could be related to patients enrolling in clinical trials for experimental chemotherapy and improving treatment of cancer in general. We are left with the most common diagnosis – heart disease, which can cause various effects, such as failure to thrive and debility. It still remains, however, a very unpredictable course. Patients with heart disease have recurrent remissions and exacerbations, with gradual and slow decline over a period of months. When patients transfer from one facility to another or change their primary care physician along the way, things can become even more complex. The bottom line? When we think about our patients, let’s think about hospice sooner rather than later. This will help our patients have a better end-of-life experience, along with their families. For more information on UH Hospice, email me at May.Al-Abousi@UHhospitals.org. Pediatric Heart Center at UH Rainbow at UH Rainbow Babies & Children’s Affiliates with Nationwide Children’s “UH Rainbow Babies & Children’s and Nationwide Children’s are joining forces to become one of Ohio’s largest pediatric heart programs by developing a long-term affiliation agreement based on meaningful clinical integration,” says Patricia DePompei, RN, MSN, President of UH Rainbow Babies & Children’s Hospital. University Hospitals Rainbow Babies & Children’s Hospital “UH Rainbow Babies & Children’s and Nationwide Children’s has entered into an affiliation agreement with Nationwide are joining forces to become one of Ohio’s largest pediatric Children’s Hospital in Columbus centered on pediatric heart programs by developing a long-term affiliation cardiology and cardiothoracic surgery services. The new agreement based on meaningful clinical integration,” program, titled The Congenital Heart Collaborative, is says Patricia DePompei, RN, MSN, President of UH Rainbow focused on providing the highest-quality heart care, granting Babies & Children’s Hospital. “By joining forces, we will access to advanced technology and procedures, improving ensure that families around the state have access to a outcomes and conducting research. system of superior-quality, coordinated care for acquired and congenital heart disease in babies, children and adults. Mark Galantowicz, MD, FACS, Chief of Cardiothoracic Given Nationwide Children’s culture and accomplishments, Surgery, Timothy Feltes, MD, Chief of Cardiology, and it was natural to pair it with UH Rainbow’s strengths, John Cheatham, MD, MSCAI, Director of Interventional including our culture of innovation, quality and most Cardiology, as well as members of their pediatric cardiology importantly our rich legacy of medical firsts in heart care.” and cardiothoracic surgery teams, have become credentialed members of the UH Rainbow Babies & Children’s medical Due to a declining birth rate, the number of pediatric staff. Collaborating with Christopher Snyder, MD, Chief cardiothoracic surgeries performed in Northeast Ohio has of Cardiology at UH Rainbow Babies & Children’s, declined in recent years. This new affiliation agreement Drs. Galantowicz, Feltes, Cheatham and their team will addresses this demographic reality, assuring that travel to Cleveland at regular intervals to provide surgical UH Rainbow Babies & Children’s patients have access to care and interventional cardiology services to Northeast pediatric cardiothoracic surgeons who are proficient in all Ohio patients. At the same time, a UH Rainbow Babies cardiothoracic surgical procedures from the most common & Children’s team, including Dr. Snyder and seven pediatric to the most complex. cardiologists, have been credentialed to provide cardiology Continued on next page services at Nationwide Children’s. UH Physician Update | UHhospitals.org | 4 Pediatric Heart Center Continued from previous page According to the most current data available from the Society of Thoracic Surgeons (STS), Nationwide Children’s Heart Center is designated a high-volume center, with outcomes ranking among the best in the nation. In 2013, in the STAT category 5 (most complex surgery level), the Nationwide Heart Center’s mortality rate was 2.9 percent, compared with the STS all-participant average of 15.2 percent. The Nationwide Children’s Heart Center is currently ranked 11th in the nation for pediatric heart and heart surgery by U.S. News & World Report. For Northeast Ohio patients, this new affiliation means access to more options – and access to the combined and extensive expertise of UH Rainbow Babies & Children’s and Nationwide Children’s. For more information about the new affiliation, contact Justin Williams, Director of The Congenital Heart Collaborative at UH Rainbow Babies & Children’s Hospital, at Justin.Williams@UHhospitals.org or 216-286-0132. When Time is Brain… PRIMARY STROKE CENTERS OFFER THE MOST SPECIALIZED CARE Each minute during a stroke, 1.9 million brain cells die. For your patients, getting to a Primary Stroke Center, with staff specially trained in expedited stroke care, is vital. As noted at the International Stroke Conference last February, an organized, standardized approach by medical centers and EMS leads to better outcomes. The UH system offers the highest quality of stroke care in the region through its network of community hospitals. UH Ahuja, Bedford, Geauga, Parma and Richmond medical centers, as well as St. John Medical Center and Southwest General Health Center, are all designated by The Joint Commission as Primary Stroke Centers. For the most complex cases, your patients also have access to UH Case Medical Center – the first Joint Commission-certified Comprehensive Stroke Center in Northeast Ohio. Stroke center designation has been associated with a number of quality improvements, including but not limited to access to timely thrombolytic therapy and utilization of stroke unit care, according to an article published in the Journal of Stroke in 2013. Care in a specialized stroke unit also has been associated with reduced length of care, reduced case fatality and improved cost-effectiveness, when followed by early supportive discharge. Just over a decade ago, two-thirds of U.S. hospitals did not have stroke protocols, and 82 percent did not have rapid identification of acute stroke patients, according to presenters at the International Stroke Conference. Now we know that patients have the best chance for a favorable outcome and a fuller recovery with prompt treatment at a Primary Stroke Center, where our medical experts use the latest technologies. Continued on page 8 UH Physician Update | UHhospitals.org | 5 S AV E T H E D AT E F O R T H E S E Continuing Medical Education Programs Intensive Course in Medical Ethics, Boundaries and Professionalism Thursday and Friday, Sept. 10 and 11 Sept. 10: 8 a.m. – 5:15 p.m. Sept. 11: 8 a.m. – 3:30 p.m. DoubleTree by Hilton, 3663 Park East Drive, Beachwood Sponsored by the Department of Bioethics and Continuing Medical Education Program, Case Western Reserve University School of Medicine and UH Case Medical Center. 4th Annual Dan and Linda Rocker Silverberg Heal the Healer Health Symposium Medical Documentation: Clinical, Legal and Economic Implications for Health Care Providers Friday, Oct. 16, 8:30 a.m. – 4:30 p.m. Hilton Garden Inn Cleveland East, 700 Beta Drive, Mayfield Village Thursday and Friday, Nov. 5 and 6 Nov. 5: 7:45 a.m. – 5 p.m. Nov. 6: 7:45 a.m. – 3 p.m. Presented by UH Connor Integrative Health Network. DoubleTree by Hilton, 3663 Park East Drive, Beachwood Sponsored by the Continuing Medical Education Program, Case Western Reserve University School of Medicine and UH Case Medical Center. For more information on these courses, call 216-983-1239 or visit casemed.case.edu/cme. Embracing New Models of Care By Patrick Runnels, MD – Program Director, Community Psychiatry, UH Case Medical Center While I’m employed by University Hospitals, much of my time is spent outside the UH system as medical director for a large community mental health center, so my vantage point is as an administrator both from within and outside the UH system. Here are some observations from “abroad” and how I see the future of UH and the practice of medicine. Ohio expanded Medicaid in January 2014, since which time tens of thousands of Ohioans have been enrolled, many of whom will seek care at UH. Paired with the closure of Huron Hospital, this has caused our main campus – even with newly expanded emergency services – to become overwhelmed with patients seeking care for chronic and progressive health issues. By definition, all of these individuals are economically stressed, and many are impoverished. They struggle to engage in preventive care because being poor, it turns out, negatively affects decision-making ability (referred to by researchers as “bandwidth poverty”). Engaging in care for diabetes or high blood pressure is hard to prioritize for a single parent who can’t arrange for child care or an individual who is worried about being evicted next week. In this context, it’s easy to despair about our ability to make an impact. And yet, the state plans to cut around $300 million from the biennial Medicaid budget, principally by inducing hospitals to reduce admissions. In short, they’re following Medicare’s lead by penalizing 30-day readmissions. How does a large tertiary care center evolve to meet increased demand under such onerous constraints? The state is also planning to invest in Medicaid Health Homes, a model of care that leverages primary care far more robustly than our current system does. It includes robust care coordination and a healthy dose of interprofessional, interdisciplinary and interagency integration. Imagine, for instance, psychiatry being provided on sight in GI specialty follow-up clinics. Imagine care managers and nurses collaborating with individuals in their homes to navigate around barriers to healthy living, with primary care being the home base for outpatient care, seamlessly coordinating the work of specialists so that treatment plans are manageable. Here’s the good news: These models exist and can be incredibly successful at reducing admissions and improving outcomes. However, they require paradigm shifts and investment in building workforce and redefining our roles toward team-based care. The fundamental challenge for our system now is how to move forward in this new world, when funding paradigms don’t yet pay for these models, while still operating a worldclass teaching and research center. UH Physician Update | UHhospitals.org | 6 GET PUMPED. UH Harrington Heart & Vascular Institute has launched an aggressive communications campaign to engage UH physicians and employees and help them understand that we have the best heart and vascular care available anywhere. From routine preventive care to the most sophisticated technology, UH has it all – and our doctors and staff achieve superior results. We want our physicians and employees to Get Pumped: • About our doctors. The infographic on this page illustrates how patients benefit from our institute’s expertise. Help us spread the word. Our physicians and employees are our best ambassadors. • About our expertise. • About our outcomes. Visit GetPumped.org to learn more. • About taking action. 1st adult stem cell procedure in Ohio for heart disease 55 minutes Median door-to-balloon time, among the fastest heart attack angioplasty in the U.S., featured in The Wall Street Journal 1st Nation’s Over 85 clinical trials Robust cardiovascular clinical trials program – following 2,500 patients – offering access to the newest devices and techniques in U.S. 1st teaching site to offer HeartFlow/FFR-CT, a revolutionary noninvasive tool to diagnose coronary artery disease – and one of just three routinely performing transcatheter aortic valve replacement (TAVR) in the awake, talking patient International center for treatment of atrial fibrillation Nearly 100% increase in heart surgery volume over past year, High volume of complex aortic dissections, with low mortality, with an expert surgical team at six medical centers in the region, bringing care close to home less than 1/3 national rate 1st Top 1% of hospitals in the nation for Cardiology and Heart Surgery by U.S. News & World Report in Ohio and only site in Cleveland for innovative therapies such as Parachute device for advanced heart failure and adult stem cells for heart failure and severe peripheral arterial disease (PAD) UH Physician Update | UHhospitals.org | 7 UH Physicians Recognized for Excellence at June UHPS Meeting Cindy Zelis, MD, MBA, Vice President of Clinical Integration, and Todd Zeiger, MD, Vice President of the University Hospitals Primary Care Institute, recognized a large number of UH physicians for excellence in patient satisfaction and patient access at the recent UHPS meeting. The following physicians were recognized for meeting metrics for patient satisfaction: When Time is Brain… Continued from page 5 DID YOU KNOW? More than 700 patients attended stroke risk assessments hosted at 11 UH locations throughout the region in May. Most notably, four patients were immediately admitted for treatment following these Stroke Awareness Month screenings. Ewa Bak, MD, Internal Medicine, UH University Suburban Health Center Alan Markowitz, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Marcus Baratian, MD, Pediatric Medicine, Healthy Kids Pediatrics Karen Monheim, MD, Internal Medicine, Internal Medicine Associates Amy Carruthers, MD, Pediatric Medicine, Partners in Pediatrics Janet Morgan, MD, Internal Medicine, Green Road – CPI IMMEDIATE ACCESS AVAILABLE Robert Cirino, MD, Internal Medicine, UH University Suburban Health Center Hoon Park, MD, Internal Medicine, Sass-Friedman Steven Cochran, MD, Family Medicine, Ghent Family Practice Stephen Rudolph, MD, Internal Medicine, UH University Suburban Health Center The UH Neurological Institute offers triage services and same-day/next-day availability for patients with urgent needs. When you call 216-844-2724 to refer a patient, please identify the level of urgency so that we can best accommodate you and your patient. Naser Danan, MD, Pediatric Medicine, Northeast Pediatrics Debra Anne DeJoseph, MD, Internal Medicine, Green Road – CPI Neha Sheth, MD, Pediatric Medicine, Northeast Pediatrics Gregory Stefano, MD, Cardiology, Lyn Hollis Dickert-Leonard, MD, Cardiology Pediatric Medicine, Suburban Pediatrics Richard E. Stein, MD, Internal Medicine, John Eyre, MD, Internal Medicine, Internal Medicine Group of Cleveland Westlake Internal Medicine William Steiner II, MD, Internal Scott Feudo, MD, Internal Medicine, Medicine, UH University Suburban Internal Medicine Group of Cleveland Health Center Angela Hardman, MD, Pediatric Lois Teston, MD, Hematology and Medicine, Pediatricenter Oncology, UHMG Med Hematology Emil Hayek, MD, Cardiology, and Oncology Western Reserve Heart Care Joseph Trunzo, MD, Colorectal Surgery, Alan Hirsh, MD, Internal Medicine, University Southwest Surgeons UH Ahuja Medical Center Kathleen Utech, MD, Pediatric Corporate Health & Executive Wellness Medicine, Pediatricenter Kari Jacono, MD, Pediatric Medicine, Susan Vargo, MD, Pediatric Medicine, University Pediatrics of Lorain Children’s Medical Group Jeffry Katz, MD, Gastroenterology, Virginia Vatev, MD, Internal Medicine, UHMG Med Gastroenterology Westlake Internal Medicine Thomas King, MD, Internal Medicine, UH University Suburban Health Center Margie Wenz, MD, Gynecology, Geauga Women’s Specialties Smitha Krishnamurthi, MD, Erika Whitney, DO, Internal Medicine, Hematology and Oncology, UHMG Geauga Internal Medicine Med Hematology and Oncology Debra Leizman, MD, Internal Medicine, Terry Wiseman, MD, Pediatric Medicine, Sandusky Pediatrics UHMG Medicine Internal Janice Lyons, MD, Radiation Oncology, UHMG Radiation Med William Wolf, MD, Cardiology, UHMG Med Cardiology Scott Mabee, MD, Internal Medicine, Fairlawn Internal Medicine Brian Zack, MD, Pediatric Medicine, Pediatricenter Matthew Mark, MD, Family Medicine, Bedford Family Medicine Continued on next page New Developments in UH Neurosurgery Several talented University Hospitals neurosurgeons are available for referrals and will provide a seamless transition for patients of David Hart, MD, who departed UH on July 1. The UH Neurological Institute’s complement of experienced neurosurgeons includes: Nicholas Bambakidis, MD, Director, Cerebrovascular & Skull Base Surgery; Alan Hoffer, MD, Director, Traumatic Brain Injury Center; Jonathan Miller, MD, Director, Functional & Restorative Neurosurgery Center; and Jennifer Sweet, MD. Soon we will welcome two new neurosurgeons. Yin Hu, MD, a microsurgical and endovascular neurosurgeon who completed his neurosurgery training at Case Western Reserve University School of Medicine, will join our team from Westchester Medical Center in New York. Alia Hdeib, MD, is completing a fellowship in surgical spinal oncology and complex deformity correction at The Johns Hopkins University and will join our team in September. To refer a patient, please call 216-844-7600. UH Physician Update | UHhospitals.org | 8 UH Physicians Recognized for Excellence Continued from previous page These UH physicians were recognized for meeting patient access metrics: Ravi Ashwath, MD, Pediatric Medicine, UHMG Peds Cardiology Jai Lee, MD, Thoracic Surgery, University Southwest Surgeons Basar Sareyyupoglu, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Marcelo Auslender, MD, Pediatric Medicine, UHMG Peds Cardiology Philip Linden, MD, Thoracic Surgery, UHMG Surg Thoracic Adult Jill Shivapour, MD, Pediatric Medicine, UHMG Peds Cardiology Susannah Briskin, MD, Pediatric Medicine, UHMG Peds Sports Med Alan Markowitz, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Christopher Snyder, MD, Pediatric Medicine, UHMG Peds Cardiology Salil Deo, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Patrick McConnell, MD, Thoracic Surgery, UHMG Surg Thoracic Peds Mary Solomon, DO, Pediatric Medicine, UHMG Peds Sports Med Yakov Elgudin, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Benjamin Medalion, MD, Thoracic Surgery, UHMG Surg Cardiac Adult James Strainic, MD, Pediatric Medicine, UHMG Peds Cardiology Anthony Furlan, MD, Neurology, UHMG Neuro Stroke Soon Park, MD, Thoracic Surgery, UHMG Surg Cardiac Adult Christopher Towe, MD, Thoracic Surgery, UHMG Surg Thoracic Adult Mark Galantowicz, MD, Thoracic Surgery, UHMG Surg Thoracic Peds Yaron Perry, MD, Thoracic Surgery, UHMG Surg Thoracic Adult Amanda Weiss-Kelly, MD, Pediatric Medicine, UHMG Peds Sports Med James Hill, MD, Pediatric Medicine, UHMG Peds Cardiology Jason Robke, MD, Thoracic Surgery, UHMG Surg Thoracic Adult Peter Kouretas, MD, Thoracic Surgery, UHMG Surg Thoracic Peds Michael Saalouke, MD, Pediatric Cardiology, Pediatric Cardiology UH cardiac surgeon Alan Markowitz, MD, had the distinction of meeting metrics for both patient satisfaction and access. Congratulations to all the honorees. New UH Physicians NOT PICTURED: Ehsan Malek, MD Hematology and Oncology 216-844-3951 UH Case Medical Center Jack King, MD Pediatrics 330-664-8120 Children’s Medical Group, Fairlawn and Hudson John Sanitato, MD Psychiatry 216-844-2400 UH Parma Medical Center Roger Ove, MD Radiation Oncology 440-324-0440 UH Case Medical Center, UH Elyria Medical Center Among the nation’s leading academic medical centers, University Hospitals Case Medical Center is the primary affiliate of Case Western Reserve University School of Medicine, a nationally recognized leader in medical research and education. UH Physician Update © 2015 University Hospitals COR 00882 | UHhospitals.org | 9