Thromboembolic Disease: Pulmonary Embolism and Deep Vein
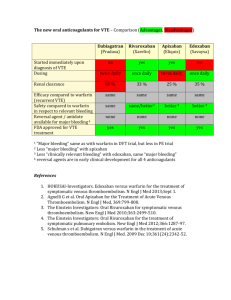
advertisement

ACTIVITY DISCLAIMER Thromboembolic Disease: Pulmonary Embolism and Deep Vein Thrombosis Daniel Tambunan, MD The material presented here is being made available by the American Academy of Family Physicians for educational purposes only. This material is not intended to represent the only, nor necessarily best, methods or procedures appropriate for the medical situations discussed. Rather, it is intended to present an approach, view, statement, or opinion of the faculty, which may be helpful to others who face similar situations. The AAFP disclaims any and all liability for injury or other damages resulting to any individual using this material and for all claims that might arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by a physician or any other person. Every effort has been made to ensure the accuracy of the data presented here. Physicians may care to check specific details such as drug doses and contraindications, etc., in standard sources prior to clinical application. This material might contain recommendations/guidelines developed by other organizations. Please note that although these guidelines might be included, this does not necessarily imply the endorsement by the AAFP. Daniel Tambunan, MD DISCLOSURE It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/invitation of participation. Disclosure documents are reviewed for potential conflict of interest (COI), and if identified, conflicts are resolved prior to confirmation of participation. Only those participants who had no conflict of interest or who agreed to an identified resolution process prior to their participation were involved in this CME activity. The Following individuals in a position to control content relevant to this activity has disclosed the following relevant financial relationships: Assistant Director, Florida Hospital Internal Medicine Residency; Clinical Assistant Professor, University of Central Florida, College of Medicine; Clinical Assistant Professor, Florida State University, College of Medicine; Assistant Professor of Medicine, Loma Linda University School of Medicine. Dr. Tambunan is a frequent and popular FMX presenter. He practices internal medicine and has been teaching for 17 years. He specializes in anticoagulation, venous thromboembolism, and viral hepatitis. Daniel Tambunan, MD, Boehringer (Atrial fib, VTE, Anticoagulation), Jannsen (VTE), Bristol Myers Squibb (VTE) - Consultant or Advisory Board All other individuals in a position to control the content for this activity have indicated they have no relevant financial relationships to disclose. The content of my material/presentation in this CME activity will not include discussion of unapproved or investigational uses of products or devices. Learning Objectives 1. Establish protocols to identify patients at risk for a thromboembolic event, and provide counseling to reduce risks and recognize signs and symptoms. 2. Use an evidence-based algorithm to diagnose DVT/PE, taking into account the stability of the patient. 3. Prescribe appropriate anticoagulant agents, according to the most recent clinical guidelines, to treat and help prevent recurrence of thrombotic events in patients. 4. Develop collaborative care plans with patients; emphasizing adherence to prescribed therapies, and monitoring with follow-up. Audience Engagement System Step 1 Step 2 Step 3 1 Prevalence of VTE ENDORSE Study • 51.8% hospitalized patients at risk for VTE – based on cross-sectional survey of 68,183 hospital inpatients ≥ 40 years old in 32 countries in 20062007 – 64.4% surgical and 41.5% medical patients considered at risk for VTE – proportion of at risk patients ranged from 35.6% in Turkey to 72.6% in United Arab Emirates Recognized Unrecognized Total > 500,000 cases/yr of DVT 5‐10% of all hospital deaths/year from PE Anderson, et al. Arch Intern Med 1991; 151:933. Cohen AT, Tapson VF, Bergmann JF, et al. Lancet 2008; 371(9610):387‐94. Arterial vs Venous VIRCHOW’s TRIAD • Arterial - thrombosis does not occur if endothelium is intact & functional. The usual cause is vascular damage through atherosclerotic plaque formation and eventual rupture • Venous - “Virchow’s” triad - endothelial injury, circulatory stasis and hypercoagulable state • Circulatory STASIS: immobility, CHF, advanced age, obesity and venous obstruction • Endothelial Injury (TRAUMA): surgery (e.g., orthopedic), postpartum, infections & valve damage • HYPERCOAGULABLE state: Factor V Leiden, oral contraceptives, cancer, deficiencies of protein C&S or ATIII , homocysteine, impaired fibrinolysis Hypercoagulable Studies Poll Question B.V. is a 35 y/o Caucasian gentleman who comes to the ER with complaint of left leg pain and swelling for 3 days. Denies any insect bite, fall or trauma. Denies any shortness of breath or chest pain. PE: Afebrile, B/P 110/70, P= 100. Normal exam except asymmetric thigh size and mild tenderness on palpation. No chords palpable and negative Homan’s sign. Would you include coagulopathy studies now? A. No B. Yes • • • • • • • • Factor V Leiden Antiphospholipid Antibodies Homocysteine Prothrombin gene 20210 A allele Elevated Factor VIII (> 90th percentile) Antithrombin III deficiency Protein C deficiency Protein S deficiency Federman DG, Kirsner RS. Arch Intern Med. 2001;161:1051‐1056 2 Poll Question • In a person with recurrent pulmonary embolism which one of the following is the most common abnormality? – – – – A. Antithrombin III deficiency B. Protein C deficiency C. Protein S deficiency D. The presence of Factor V Leiden mutation – E. The presence of antiphospholipid antibodies Factor V Leiden • Resistant activated Protein C • Most common hypercoagulable state 3.71% • More common in Caucasian (5.27%) Hispanics (2.21%) African-americans (1.23%) Asians (0.45%) • OCP’s or smoking increases risk 30 fold for VTE • No increased incidence of stroke or myocardial infarction Price D, et al. Annals of Int Med 1997;127:895‐903. Poll Question • VTE Prophylaxis • • • A 54-year-old Indonesian morbidly obese gentleman was admitted to the hospital for acute abdominal pain. Upon further work up by the ED physician pt was diagnosed of having suspected cholecystitis. PMH: DM type 2, HTN and hyperlipidemia. SH: occasional alcohol. Meds: metformin, glyburide, lisinopril, aspirin and pravastatin PE: T=100.6, P=104, R=16, B/P=138/86. General: awake, nonresp distress. Exam is normal except abdomen shows tenderness on deep palpation on the RUQ area, +/- Murphy sign, no rebound, bowel sound is hypoactive, no mass palpable. Labs: Normal CBC and CMP except WBC is at 14.4, AST/ALT = 88/74, Alk P = 258, Bili = 2.8 He is scheduled for possible open cholecystectomy by the surgeon tomorrow AM. Which of the following peri-operative orders would be the most acceptable? – – – – Thrombophylaxis in Surgical Patients: ACCP Risk Classification • Low Risk (<10%) – Minor surgery – Medical pt’s who are mobile • Moderate Risk (1040%) – Most surgery – Medical pt’s who are bedrest/sick • High Risk (40-80%) – Hip/knee arthroplasty – History of VTE – Hip or total joint procedures – Spinal cord injury; major trauma Kahn SR, Gould MK, Falck‐Ytter Y. Chest 2012; 141:195S‐325S. A. No peri-operative orders needed since he is a fairly healthy gentleman B. Continue with metformin C. Enoxaparin 40 mg subcut daily D. UFH 15,000 units subcut twice daily Thromboprophylaxis in Surgical Patients • Low risk: No prophylaxis • Moderate risk: LMWH or LDUH (5,000 U bid) • High risk: LMWH or Warfarin or Fondaparinux or NOAC + IPC Kahn SR, Gould MK, Falck‐Ytter Y. Chest 2012; 141:195S‐325S. 3 Thromboprophylaxis in Knee/Hip Orthopedic Surgical Patients • Low molecular weight heparin (LMWH) • Warfarin, rx 2 days prior to surgery or immediately post surgery (INR 2.0-3.0) • Fondaparinux 2.5 mg daily • Novel anticoagulant – Dabigatran 220 mg daily, Rivaroxaban 10 mg daily, Apixaban 2.5 mg BID (hip, 28–35 days & knee, 10-12 days) • Intermittent pneumatic compression is only an adjuvant therapy • Low dose unfractionated heparin is inadequate. Kahn SR, Gould MK, Falck‐Ytter Y. Chest 2012; 141:195S‐325S. Apixaban, Dabigatran and Rivaroxaban package insert Prevention during travel • • • • ASA Vitamin E LMWH Below knee compression stocking • Recommended: Moving frequently, loose clothing and hydration DVT - Deep Vein Thrombosis • PROXIMAL *Any vein from the popliteal v. and up *Larger clot *High propensity to embolize (40-60%) *REMEMBER: Superficial femoral v is a deep v. - do tx. Deep Vein Thrombosis (DVT) Pretest probability of DVT • Active cancer • Paralysis, paresis or immobilization • Recently bedridden for > 3 days or major surgery within 4 weeks • Localized tenderness along the distribution of the deep venous system • Entire leg swollen • Calf swollen by > 3 cm when compared to asymptomatic leg • Pitting edema • Collateral superficial veins • Alternative diagnosis greater than DVT • 1 • 1 • 1 • 1 • 1 • • • • 1 1 1 -2 • DISTAL *Below popliteal v. *Smaller clot *Less symptomatic and less likely to cz PE *Can propagate up to the proximal v. Poll Question • • • • B.V. is a 35 y/o Caucasian gentleman who comes to the ER with left leg pain and swelling for 3 days and recent chest pain. Denies any insect bite, fall or trauma. Denies any shortness of breath, long travel, or previous surgical procedure. PMH: None. Denies any history of DM or cancer. FH: Denies any history of DVT or PE. PE: Afebrile, B/P 110/70, P = 100, R= 30. Normal exam except asymmetric thigh/leg size, mild tenderness on palpation, & unilateral pitting edema. No palpable chords, negative Homan’s sign and nonerythematous. What is the pretest clinical probability score for DVT? A. 1 B. 2 C. 3 D. 4 E. 6 Wells PS, et al. Lancet 1997;350:1795‐1798. 4 Role of D-dimer in DVT • Prospective cohort study in Canada. 556 patients with suspected first DVT divided into two groups : negative D-dimer vs positive D-dimer • Endpoint: Negative D-dimer assay with low or moderate pretest probability eliminates further testing • Results – 1/283 (0.3%) vs 34/168 (16.8%) * on low/mod pretest prob – 0/20 (0.0%) vs 21/51 (41.2%) on high pretest probability • Conclusion: Negative D-dimer with a low or moderate pretest probability safely eliminates the need for ultrasound Bates SM, Kearon C, et al. Ann Intern Med. 2003:138:787‐794. Summary • High probability – • Intermediate probability – • Duplex U/S • Positive – TREAT • Negative - consider venography » Positive – TREAT » Negative – DVT r/o D-dimer • Positive - do U/S – Positive – Treat & consider venography or repeat U/S in 1 wk – Negative – DVT r/o • Negative – DVT r/o Low probability – D-dimer • Positive - do U/S – Positive – Treat & consider venography or repeat U/S in 1 wk – Negative – DVT r/o • Negative – DVT r/o Complications • • • • pulmonary embolus postthrombotic syndrome phlegmasia alba dolens phlegmasia cerulea dolens Pulmonary Embolus: Signs & Symptoms • • • • • • • Tachypnea (70% of patients) Chest pain (70%) Cough (40%) Tachycardia (33%) Shortness of breath (25%) Signs of DVT (10%) Syncope (5%) Chest 1995; 107(suppl):25S‐32S. Pulmonary Embolus Pretest Probability of PE • Clinical signs and symptoms of DVT • An alternative diagnosis is less likely than PE • Heart rate > 100 • Immobilization or surgery in previous 4 weeks • Previous DVT/PE • Hemoptysis • Malignancy • 3 points • 3 points • 1.5 points • 1.5 points • 1.5 points • 1 point • 1 point Wells PS, et al. Thromb Haemost 2000;83:416‐20. 5 Basic tests Poll Question • • CXR - normal in 50% RS, a 65 y/o WF comes in with acute shortness of breath for the last 2-3 days. Denies any cough, hemoptysis, fever, or vomiting. Has h/o of hypercholesterolemia & DM type 2 for 10 years, otherwise negative PMH. FH was noncontributory. Vitals, BP 125/85, P=120, R=24. Physical was normal except an asymmetric leg swelling R>L and tenderness. Meds: Glucophage, Zestril, Estrogen, & Lipitor – Hampton’s hump (wedge shape consolidation) – Others: elevated diaphragm, pleural effusion, infiltrate, atelectasis. • EKG – S1Q3T3 (pathognomonic) rarely seen. – Others: sinus tach, T wave inv on V1 to V4, acute RBBB, new onset a-fib, RV strain. What is the pretest clinical probability of PE? A. 1.5 B. 3.0 C. 4.5 D. 6.0 E. 7.5 • ABG – Usually decreased PaO2 and PaCO2, and increased pH – Increase A-a gradient (150 - PaCO2/0.8 - PaO2) The PIOPED Investigators. JAMA 1990;263:2753‐2759. VQ Scan Clinical Score: “Poor Man’s Test” 1090 patients between 1992-1997 Based on 8 variables: – – – – Pulse rate > 100 PaCO2 PaO2 CXR • • • Platelike atelectasis Elevation of hemidiaphragm Score system (max score of 16 points) – – – • VQ Scan probability - Age - Previous PE or DVT - Recent surgery < 4 = low probability 5 - 8 = intermediate probability > 9 = high probability Comparison between Empirical vs Score probability • low probability 9 % vs 10 % • intermediate probability 33 % vs 38% • high probability 66 % vs 81% Wicki J, et al. Arch Intern Med 2001; 161:92‐97 Spiral CT • “The Good” – – – – Highly sensitive for central vessels Can differentiate between acute vs chronic clot Quick test (done in 30 sec and single breath) May give clues to alternative diagnosis (67%) Index of suspicion • • High Intermediate Low Normal High 28/29 96% 27/41 66% 6/15 37% 0/5 0% Low 5/9 56% 11/68 16% 4/90 4% 1/61 2% The PIOPED Investigators. JAMA 1990;263:2753-2759. D-dimer: “An old timer” • Several types of assays – Latex agglutination (LA) – Enzyme-linked immunosorbent assays (ELISA) • “The Bad” • Advantages • “The Ugly” • Disadvantages – Cost – Uses contrast: contraindicated in RI &/or history of contrast allergy – Lower sensitivity for subsegmental vessels – Shunt, eg., patent foramen ovale Remy‐Jardin M, et al. Radiology 1992; 185:381‐387. Remy‐Jardin M, et al. J Thoracic Imaging 1997; 12:103‐117. – High negative predictive value - especially the ELISA test 91-100% – High false positive rate, ranges from 9 - 15% – Low specificity - especially in elderly over 80 y/o Brill‐Edwards P, et al. Thromb Haemost 1999; 82:688‐694. 6 Pulmonary Angiogram: “Mr. Right” • High sensitivity - 98% • High specificity - 97% • Advantages – May perform adjunctive procedures, eg., local catheter-directed thrombolysis, suction thrombectomy, IVC filter placement – Can differentiate acute vs chronic PE • Disadvantages – Invasive (risk: death - 0.5%, morbidity - 1%) – Contrast allergy patients and RI The PIOPED Investigators. JAMA 1990; 263:2753‐2759. Stein PD, et al. Circulation 1992; 85:462‐468. Mortality Risk - Simplified PESI – 995 outpatients with objectively confirmed acute symptomatic PE, validation cohort of 7,106 patients with acute symptomatic PE – 7 factors • • • • • • aged > 80 years old history of cancer history of chronic lung disease or heart failure pulse ≥ 110 beats per minute systolic blood pressure (SBP) < 100 mm Hg arterial oxyhemoglobin saturation level < 90% – 30-day mortality risk stratified by simplified PESI score • • score = 0 for low-risk score ≥ 1 for high-risk – 30-day mortality in validation cohort • • 1.1% of 2,569 patients classified as low risk (98.9% NPV) 8.9% of 4,537 patients classified as high risk Arch Intern Med 2010 Aug 9;170(15):1383 UF-Heparin Anticoagulation Pentasaccharides •Mode of mechanism: Inhibits factor Xa only •Indicated for VTE prophylaxis and treatment •VTE treatment (dose varies with weight) • < 50 kg ‐‐‐ 5.0 mg SC • > 50 to 100 kg ‐‐‐ 7.5 mg SC • >100 kg ‐‐‐ 10.0 mg SC •Monitor platelets frequently •Caution in pts with RI (CrCl < 30 mL /min) •Caution in underweight pts (< 45 kg) EPHESUS and PENTATHLON study, 2000 • MW = 35-50,000 Kd • Poor bioavailability due to binding to proteins • Targets Xa, ATIII, & thrombin • Needs regular lab monitoring - Q 6 hrs • Rapid plasma clearance • Needs platelet, H/H monitoring LMWH • MW = 5-10,000 Kd • Good bioavail., little binding to proteins • Targets Xa & ATIII only • No lab monitoring needed, except in obese (>110 kg) or renal dz • Slow plasma clearance • Needs platelet, H/H monitoring EINSTEIN • 3,449 patients with acute symptomatic DVT randomized to rivaroxaban (15 mg po BID for 3 wks then 20 mg daily) vs standard therapy (enoxaparin SubQ + warfarin) • Results: – Early treatment discontinuation 11.3% v 14.2% (p=0.01) – Symptomatic recurrent VTE 2.1% v 3% (HR 0.68, CI 0.44-1.04 – Major bleeding 0.8% v 1.2% (NS) . EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. N Engl J Med 2010 Dec 23;363(26):2499 7 EINSTEIN - PE • 4,883 patients with acute symptomatic PE +/- DVT randomized to rivaroxaban ( 15 mg po BID for 3 wks then 20 mg po daily thereafter) vs standard therapy (enoxaparin SubQ + warfarin) • Results: – – – – symptomatic VTE 2.1% v 1.8% (NS) major bleeding 1.1% v 2.2% (p = 0.003) major bleed or nonmajor bleed 10.3% v 11.4% (NS) mortality 2.4% v 2.1% (NS) EINSTEIN‐PE Investigators, Buller HR, Prins MH, et al. N Engl J Med 2012 Apr 5;366(14):1287 AMPLIFY – 5,395 adults (mean age 57 years) with acute symptomatic proximal deep vein thrombosis or pulmonary embolism were randomized conventional therapy vs apixaban 10 mg BID first 5 days then 5 mg BID for 6 months. Followed up for 7 months – primary outcome was composite of recurrent symptomatic venous thromboembolism (VTE) and VTE-related death – 30 patients who did not receive study drugs were excluded from safety analysis – comparing apixaban vs. conventional therapy • • • • • primary outcome in 2.3% vs. 2.7% (95% CI for difference -1.3% to +0.4%, noninferiority met) major bleeding in 0.6% vs. 1.8% (p < 0.001, NNT 84) clinically relevant non-major bleeding in 3.8% vs. 8% (p < 0.05, NNT 24) all-cause death in 1.5% vs. 1.9% (not significant) any serious adverse event in 15.6% vs. 15.2% (no p value reported) Agnelli G, Buller HR, Cohen A, et al. N Engl J Med 2013;369(9):799‐808 RECOVER – 2,564 patients (mean age 55 years) with acute symptomatic VTE and normal renal function randomized to dabigatran 150 mg orally twice daily plus warfarin-like placebo vs. warfarin plus dabigatran-like placebo for 6 months • all patients initially given parenteral anticoagulation therapy for median 9 days • primary outcome was time to first occurrence of composite of symptomatic VTE or VTE-related death • comparing dabigatran vs. warfarin – – – – symptomatic VTE or VTE-related death at 6 months in 2.3% vs. 2.2% (noninferiority met) any death in 1.6% vs. 1.7% (not significant) major bleeding episodes in 1.6% vs. 1.9% (not significant) any bleeding episodes in 16.1% vs. 21.9% (p < 0.05, NNT 18) • no significant differences in acute coronary syndromes or abnormal liver function tests Hokusai - VTE – 8,292 patients, intention to treat study with acute VTE randomized to edoxaban 60 mg once daily vs. warfarin with INR ratio 2-3. Non inferior study. – at baseline • 59% had deep vein thrombosis and 41% had pulmonary embolism • all patients had initial treatment with enoxaparin or unfractionated heparin for ≥ 5 days – 99.4% were included in modified intention-to-treat analyses – comparing edoxaban vs. warfarin • symptomatic recurrent VTE in 3.2% vs. 3.5% (hazard ratio 0.89, 95% CI 0.7-1.13), noninferiority established • major or clinically relevant nonmajor bleeding in 8.5% vs. 10.3% (p = 0.004, NNT 56) • clinically relevant nonmajor bleeding in 7.2% vs. 8.9% (p = 0.004, NNT 59) • major bleeding in 1.4% vs. 1.6% (not significant) • any bleeding in 21.7% vs. 25.6% (p < 0.001, NNT 26) • death in 3.2% vs. 3.1% (no p value reported) Schulman S, Kearon C, Kakkar AK, et al. N Engl J Med 2009;361(24):2342‐52 Buller HR, Decousus H, Grosso MA, et al. N Engl J Med 2013;369(15):1406‐15. 10 mg warfarin LOADING Novel anticoagulants Pearls • Dosing: • • • • Qday – Edoxaban & Rivaroxaban BID – Apixaban & Dabigatran Initial acute treatment: Dabigatran and Edoxaban uses parenteral AC for 5-9 days. Apixaban 10 mg BID for 5 days then 5 mg BID afterwards. Rivaroxaban 15 mg BID for three weeks then 20 mg Qday afterwards. Half life: 8-14 hours Renal clearance: Dabigatran 80%, the rest 25-50%. All are contraindicated if CrCl < 30 mL/min. Edoxaban contraindicated if CrCl > 95 mL/min Food: Rivaroxaban (mandatory) Drug interactions: P-gp inhibitor –azole increase the NOAC’s while P-gp inducer – eg. Anticonvulsants decrease the NOAC’s Apixaban, Dabigatran, Edoxaban and Rivaroxaban package insert % 100 90 80 70 60 50 40 30 20 10 0 INR < 2.0 INR 2.0 - 3.0 INR > 3.0 12 36 Hours 60 84 Harrison L, et al. Annals of Internal Medicine 1997;126:133‐136. 8 5 mg warfarin Optional Warfarin Initiation Day % INR 1 2 100 90 80 70 60 50 40 30 20 10 0 3 INR < 2.0 INR 2.0 - 3.0 INR > 3.0 4 12 36 60 Warfarin Dose < 1.5 < 1.8 1.8 - 2.0 2.1 - 3.0 > 3.0 < 1.6 1.6 - 2.0 2.1 - 3.0 3.1 - 3.5 > 3.5 < 1.6 1.6 - 2.0 2.1 - 2.5 2.6 - 3.0 3.1 - 3.5 >3.5 84 Hours Harrison L, et al. Annals of Internal Medicine;1997:126:133‐136. 10 10 5 2.5 0 15 10 5 2.5 0 15 10 7.5 5 2.5 0 Kovacs MJ, et al,. Ann Int Med 2003; 138:714‐719. Therapeutic Ranges INDICATION Thromboembolic Clinical effects Prophylaxis of DVT Treatment of DVT Prevention of cardioemb. stroke S/P acute MI A. fibrillation Cardiomyopathy (<25%) Valvular heart disease Mechanical heart valve Hypercoagulable states Tissue heart valve Acute MI Hemorrhagic INR DURATION 2-3 2-3 2-3 2-3 2-3 2-3 2-3 2.5-3.5 2-3 2-3 2-3 7 days to 1 month Varies, see table Indefinite Indefinite Indefinite Indefinite Indefinite Indefinite Indefinite 3 mths < 3 mths Kahn SR, Gould MK, Falck‐Ytter Y. Chest 2012; 141:195S‐325S. 2.0 3.0 INR Poll Question • • A 47 y/o African-American gentleman was admitted to the hospital for severe left hand pain and swelling for ten days. States that he noticed it while gardening last week. He was started on oral dicloxacillin by his primary MD last week. He has history of atrial fibrillation and hypertension. His meds includes quinapril, warfarin and simvastatin. He states that his INR has been well controlled for the last year. His physical exam shows his left hand is warm, tender to touch, erythematous, edematous, with a central lesion. Labs shows WBC = 15.9, Hgb = 11.3, Plt = 156 K, normal BMP. INR = 1.57 What is the reason of patient’s sub therapeutic INR? – A. Non-compliance – B. Drug interaction with lisinopril – C. Drug interaction with dicloxacillin – D. Pt has a CYP2C9 mutation Warfarin Drug Interactions POTENTIATE • Antibiotics/Antifungal – • Cardiovas. agents – • sulfamethoxazole, ciprofloxacin, tetracycline, metronidazole, all -azoles, isoniazid, macrolides amiodarone, disopyramide, propafenone Others – cimetidine, ASA, NSAID’s, allopurinol, omeprazole, herbals; vitamin E, garlic, gingko biloba, garlic, ginseng REDUCE • Antibiotics/Antifungal – rifampin, nafcillin, dicloxacillin • Anticonvulsants • Others – phenytoin, barbiturates – sucralfate, cholestyramine, colestipol, chlorodiazepoxide, trazodone 9 Warfarin reversal treatment: non-bleeding Case Study INR Vit K dose Route <5 none Hold dose 5-9 1.0-2.5 mg PO >9 2.5-5.0 mg PO * Check INR in 6-12 hrs and repeat if necessary. ! In severe/life threatening bleeding use Vit K 5-10 mg slow IV infusion and B.V. is a 35 y/o Caucasian gentleman who comes to the ER with complaint of left leg pain and swelling for 3 days. Denies any insect bite, fall or trauma. Denies any shortness of breath or chest pain. PE: Afebrile, B/P 110/70. P= 100 Normal exam except asymmetric thigh size and mild tenderness on palpation. No chords palpable and negative Homan’s sign. How long would you treat the LLE DVT with an antithrombotic agent? FFP Ansell M, Hirsh J, et al. Chest 2008;133:123S‐131S 2012 ACCP Recommendations Duration of therapy of VTE • 3 months - reversible risk factors* & 1st event - distal DVT • 3 mths or more - unprovoked VTE & 1st event depending on the risk-benefit ratio • 3-6 months -cancer, until resolved • Indefinite -second episode of unprovoked Risk - Benefit • • • • • • • >75 y/o Previous GI bleed Previous noncardioembolic stroke Chronic renal or hepatic disease Concomitant antiplatelet therapy Other serious illness Poor anticoagulant control *Transient immobilization, trauma, surgical operation, or pharmacologic estrogen use. Kearon C, Akl EA, Comerota AJ, et al. Chest 2012;141:e419S-494S Kearon C, Akl EA, Comerota AJ, et al. Chest 2012;141:e419S-494S Other management options D-dimer for anticoagulation duration? • • 608 patients, prospective, three armed study with first episode of symptomatic, idiopathic proximal DVT &/or PE who has been treated at least for 3 months with warfarin. One arm – normal D-dimer, the other – abnormal D-dimer - placebo vs warfarin • • Objective: Composite recurrent VTE and major bleeding during 1.4 years of follow-up Results: – – – – – • Normal: 24/385 (6.2%) Abnormal and placebo: 18/120 (15.0%) Abnormal and treated: 3/103 (2.9%) p value = 0.02 (2/3 comparison) Major bleeding: 1 on the treated group, 0 on the others. Conclusion: Consider longer therapy with warfarin if D-dimer is abnormal. The PROLONG Investigators. N Engl J Med 2006;355:1780-9. • Positive d-dimer • Proximal DVT • Antiphospholipid antibody • Previous episode of VTE • Hereditary thrombophilia • Male • Residual thrombosis in proximal veins • Non-Asian ethnicity • Inferior Venal Caval Filter – – – – contraindication or complication from anticoagulant therapy recurrent thromboembolism despite adequate anticoagulation chronic recurrent embolism with pulmonary hypertension concurrent performance of surgical pulmonary embolectomy • Thrombolytic Therapy • Surgical Pulmonary Embolectomy • Catheter Transvenous Extraction Kearon C, Akl EA, Comerota AJ, et al. Chest 2012;141:e419S-494S 10 Practice Recommendations 3. Factor V Leiden is the most common hypercoagulable disorder 2. Superficial femoral vein is a deep vein – DO TREAT My e:mail address; daniel.tambunan.md@flhosp.org QUESTIONS? 1. D‐ dimer has a very high negative predictive value BUT low PPV 11