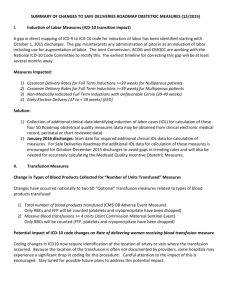
Nuts and Bolts of ICD-10
advertisement

The Nuts and Bolts of ICD-­‐‑10 Dr. Kelly Kerksick, OD About Your Presenter • OD Advisor for Revolution EHR • Group practice in Southern Illinois near St. Louis • Cards Fan! • Mom of two boys From My City to Yours Discussion Points • • • • • ICD Overview “Crosswalking” General Equivalence Mapping Choosing ICD-10 Codes in Clinical Care 5 step process to prepare for October 1 Overview of ICD International Classification of Diseases World Health Organization (WHO) Started in 1900 with ICD-1 ICD-9 is the disease/problem/condition code for US provider claims through September 30, 2015 • ICD-10 is the updated coding & documentation system that will be used for US provider claims on October 1, 2015 • • • • ICD-­‐‑9 • Almost 14,000 codes • Used in US since 1979 • No documentation • • • Laterality Pertinent negatives Context • 3-5 characters • Always three characters minimum, with two optional after decimal ICD-­‐‑10 • Over 68,000 diagnosis codes • ICD-10-CM (Clinical Modification) has 21 chapters, about 10 have codes that relate to eye care delivery • Up to 7 characters, 3-7 alpha-numeric • • First character alpha, 2nd numeric, not case sensitive Documentation of: • Laterality • Pertinent negatives • Context (e.g. MVA, on a residential street, texting while driving, fighting with in-laws) • State of care (initial, subsequent, sequela) ICD-­‐‑11, up next… • WHO undertaking development with plan for final endorsement in 2015 and release in 2017 • Will align with SNOMED coding • Expanded multilinguality • Enhanced “Content Model” will guide users • Each disease will have definitions that give key descriptions and guidance on the meaning of the code in human readable terms ICD-­‐‑10 Implementation • CMS will pay claims with ICD-10 for services rendered on and after October 1, 2015 • Testing is underway in 2015 • End-to-end testing is only necessary for those who do not use an electronic clearinghouse • Your practice’s clearinghouse must confirm successful CMS ICD-10 submissions Crosswalking • Called General Equivalence Mapping (GEM) • Identifies the 1-to-n mapping from ICD-9 to -10 • • • • • No match: 3% 1-to-1 match: 24% 1-to-1 approximate match with 1 choice: 49% 1-to-1 approximate match with Mult choices: 19% 1-to-many match with 1 or many scenarios: 5% General Equivalence Mappings • The purpose is to: create a useful, practical, code to code translation reference dictionary for both code sets o Offer acceptable translation alternatives wherever possible o • Mappings from specific concepts to more general concepts are possible • It is not possible to use mappings to add specificity when the original information is general ICD-­‐‑10 Peculiarity • 39,000 codes for injury and poisoning • Multiple codes due to laterality • NOTE: some codes do not have laterality • AMD, POAG, Diabetic Retinopathy, Presbyopia • O is only in the first position • All other round figures are zeroes • X is a placeholder or allows for future expansion • 7th position codes for trauma • A = Initial encounter • D = Subsequent encounter • S = Sequela (resulting from) Anatomy of the ICD-­‐‑10 code Anatomy of ICD-­‐‑10 • • • • • 3-7 alpha-numeric First character alpha (not case sensitive) Second character numeric Truly considered clinical documentation Example: Primary Open Angle Glaucoma H40.11X1 Glaucoma Open Angle Mild Stage Primary Placeholder Choosing ICD-­‐‑10 in Clinical Care • Identify the disease and consider the context • Laterality when appropriate: • • • 1 in the last position = Right Eye 2 in the last position = Left Eye 3 in the last position = Bilateral • Pertinent negative, with/without: o 1 in the sixth position means “with”: E11.321 – T2D, mild NPDR, with DME o 9 in the sixth position “without”: E11.329 – T2D, mild NPDR, without DME ICD-­‐‑10 for Eyes • H00-H59: Diseases of eye and adnexa • • • • • • • H00-H05 H10-H11 H15-H22 H25-H28 H30-H36 H40-H42 H43-H44 Eyelid, lacrimal system, orbit Conjunctiva Sclera, cornea, iris, ciliary body Crystalline lens Choroid, retina Glaucoma Vitreous body, globe ICD-­‐‑10 for Eyes • H00-H59: Diseases of eye and adnexa • • • • • H46-H47 Optic nerve, visual pathways H49-H52 Muscles, binocular movement, accommodation, refractive error H53-H54 Visual disturbances, blindness H55-H57 Nystagmus, Other disorders H59 Intraoperative and post-procedural complications/disorders of eye and adnexa, not elsewhere classified Example Patient 1: ICD-­‐‑9 MPL Patient 1: Conversion View Patient 1: Vitreous Lookup View Patient 1: ICD-­‐‑10 MPL Example Patient 2: ICD-­‐‑9 MPL Patient 2: Conversion View Patient 2: ICD-­‐‑10 MPL ICD-­‐‑9 to ICD-­‐‑10 Conversions Example Conversion Display Patient 1 – Before Conversion Patient 1 – Conversion Patient 1 – After Conversion Patient 2 – Before Conversion Patient 2 – GLC Conversion Patient 2 – DM Conversion Patient 2 – Bleph Conversion Patient 2 – After Conversion ICD-­‐‑10 Assessments ICD-­‐‑10 Plans ICD-­‐‑10 Plan Tracking to ICD-­‐‑9 Choosing ICD-­‐‑10: Eyelids • All eyelid conditions reference the location: • • • • • 1 in 2 in 4 in 5 in the last position: the last position: the last position: the last position: right upper eyelid right lower eyelid left upper eyelid left lower eyelid HCPCS modifiers for CPT coding are the same: • • • • E1 – left upper E2 – left lower E3 – right upper E4 – right lower Choosing ICD-­‐‑10: Refractive Error • H52.11 – Myopia, right eye • H52.12 – Myopia, left eye • H52.13 – Myopia, bilateral • H52.0 – Hypermetropia • H52.2 – Astigmatism (5th digit for unspecified, irregular, regular • H52.4 – Presbyopia (no laterality) ICD-­9: 367.1, 367.0, 367.2, 367.4 Choosing ICD-­‐‑10: Dry Eye • H04.121 – Dry eye syndrome, right lacrimal gland • H04.122 – Dry eye syndrome, left lacrimal gland • H04.123 – Dry eye syndrome, bilateral lacrimal glands • Coding H04.121 and H04.122 together is EQUAL to H04.123 ICD-­9: 375.15 Choosing ICD-­‐‑10: Nuclear Cataract • • • • • H25.11 – Age-related nuclear cataract, right eye H25.12 – Age-related nuclear cataract, left eye H25.13 – Age-related nuclear cataract, bilateral H26.03 – Infantile and juvenile nuclear cataract Q12.0 – Congenital cataract (nuclear embryonal) ICD-­9: 366.16 Choosing ICD-­‐‑10: Dry AMD • H35.31 – Non-exudative/atrophic AMD • • • • NO LATERALITY H35.32 – Exudative AMD With 6th digit for right/left/bilateral: NO LATERALITY H35.35 – Cystoid macular degeneration H35.36 – Drusen (degenerative) of macula ICD-­9: 362.51 Choosing ICD-­‐‑10: Glaucoma (POAG) • • • • • H40.11x0 – POAG, stage unspecified H40.11x1 – POAG, mild stage H40.11x2 – POAG, moderate stage H40.11x3 – POAG, severe stage H40.11x4 – POAG, indeterminate stage NO LATERALITY • H40.2- – Primary angle-closure glaucoma • H40.13 – Pigmentary glaucoma WITH LATERALITY ICD-­9: 365.11 + stage Choosing ICD-­‐‑10: Diabetes with DR • E11.321 – T2D, mild NPDR, with DME • E11.329 – T2D, mild NPDR, without DME NO LATERALITY 5th position = mild/moderate/severe NPDR or Proliferative retinopathy E11.339 – moderate NPDR, (-­)DME E11.349 – severe NPDR, (-­)DME E11.359 – proliferative DR, (-­)DME • E11.9 – T2D without complications • E10 codes represent T1D ICD-­9: 250.52 + 362.04 Choosing ICD-­‐‑10: Medical Mgmt. • Patient on long-term medication who have no findings – code the underlying medical condition • L93.0 – Lupus • M06.09 – Rheumatoid Arthritis • Example for plaquenil retinal assessment: • • • • H35.381 – Toxic maculopathy, right eye H35.382 – Toxic maculopathy, left eye H35.383 – Toxic maculopathy, bilateral Z79.899 – Other long term (current) drug therapy ICD-­9 (Lupus + Plaquenil): 695.4 + V58.69 Common Concerns • What happens if I use the wrong ICD-10 code? Will my claim be denied? o Correct level of specificity is the goal o Medicare review contractors will not deny physician or other practitioner claims billed based solely on errors relating to specificity of the ICD-10 code for 12 months • Can I use ICD-9 codes at all after October 1st? o No o Unless you don’t want to be paid. Preparing for October 1 • If you are not using an electronic clearinghouse, review CMS resources to participate in testing claim submission from EHR to CMS • If you use an electronic clearinghouse: • • They test submission from clearinghouse to CMS (back-end testing) Front-end testing is done by the practice or the EHR vendor, to affirm that claims sent to the clearinghouse “pass” Preparing for October 1, cont. • EHR will likely dictate coding that can be applied to claims based upon the Oct. 1 date o ICD-9 only paid through Sept. 30 o ICD-10 required for payment on/after Oct. 1 • Filters at the clearinghouse may help identify mistakes on claims o Consider use of Revenue Cycle Management resources for claims filing and processing Preparing for October 1, Internally • Billing team and doctor must manage: o Master Problem (Diagnosis) List o Same-day Encounter Coding • If you have filtered down to limited ICD-9 codes, you will have more effort to deal with the specificity of ICD10 o Unspecified codes in ICD-10 will be targets for rejections Action Plan • Confirm that your EHR has been updated to support the new code set, or will be by late summer • Train staff on ICD-10 code structure • Review documentation from CMS, major insurers, and AOA • Develop plan for ICD-10 selection • Practice ICD-10 selection on fictitious patients Let’s recap! Steps Needed to Be Prepared • Step 1: Make a Plan! • Obtain Access to ICD10 Codes • cms.gov/ICD10 to download code tables and index • Other references: Step 2: Training • Training for staff and doctors • Clinical application and Billing/Coding application • Focus on documentation of new clinical concepts captured in ICD-10 • Identify top codes and code current cases in ICD-10 to test your knowledge Step 3: Update Your Processes • Make sure that you have the correct CMS 1500 forms • Be sure you have the 2012 version for paper claims submissions • Know how the new ICD-10 codes will be linked to your CPT codes. This is important for claims submission Step 4 Talk To Your Vendors • Is YOUR electronic health records system going to be ready? • Is YOUR clearinghouse going to be ready? • Find out if they are doing the leg work for you • Confirm that these things have been tested Step 5: Test Your Systems and Processes • Verify that you can generate claims with ICD-10 • Testing is needed with health plans, clearinghouses, and vendors Conclusions • Plan for some denials, challenging office morale and possibly cash flow • EHR Diagnosis lists in ICD-9 will undergo some conversion to ICD-10, but you will have some effort • Find references to assist when you code medical conditions not commonly referenced, and when treating uncommon conditions (trauma) Contact Information & Resources CMS: http://www.cms.gov/Medicare/Coding/ICD10/ProviderResourc es.html MGMA: http://www.mgma.com/icd-10-5010-implementation