large intestine - College of Veterinary Medicine
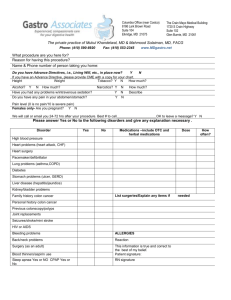
advertisement

LARGE INTESTINE MICHAEL W. ROSS The equine large intestine consists of the following segments (in aboral direction): the cecum, the large colon, and the small colon (Fig. 36-1). Although these segments form a continuum for the passage of digesta from the ileum to the anus, the three portions are considered to be separate structures, anatomically, functionally, and surgically. The large intestine of the horse is well developed and can be distinguished from that of other domestic mammals by the large capacity and shape of the cecum, and length of the small (descending) colon.' The large intestine is sacculated for most of its length and is approximately 7.5 to 8.0 m long.2 R. REID HANSON, JR. mesenteric attachment along the medial and lateral cecal bands, respectively. Because both cecal arteries are derived from a single parent vessel without collateral input, the cecum is particularly prone to thromboembolic disease. The caudal portion of the cecal base and body can be felt on rectal examination. The ventral band is prominent and is palpable per rectum. The cecal body can be exteriorized through a ventral midline incision; however, because of the presence of the dorsal attachment, the base and ileocecal junction can be seen but not exteriorized. Large Colon Cecum The cecum is approximately 1m long, has a capacity of 16 to 68 L , and occupies the right caudal abdominal quadrant.' The cecum is comma shaped and is divided into a base and body. The cecal base has a strong mesenteric attachment to the dorsal body wall and extends craniad to the level of the fourteenth or fifteenth rib.2 The cecal base curves ventrally into the cecal body, which ends in a cul-de-sac, the apex. The cecal body has four longitudinal bands (teniae), the dorsal, lateral, ventral, and medial bands, causing deep sacculations in the body. The ventral band joins the medial near the apex. The ileocecal fold runs from the antimesenteric border of the ileum to the dorsal cecal band. The ileum enters the medial, ventral aspect of the cecal base and terminates in the ileocecal orifice. The cecal base is divided into cranial and caudal portions by a transverse fold, arising from the floor of the cecal base, just craniad to the ileocecal junction. The cranial cecal base, or cupula, is voluminous, forms a sigmoid structure, and ends in the cecocolic orifice, which is located caudal in the cupula. A well-developed cecocolic ligament (fold) runs from the lateral cecal band to the lateral free band of the right ventral colon. Because of its dense dorsal mesenteric attachment, the cecocolic ligament and ileocecal fold, the cecum is immobile without concomitant mobility of adjacent organs. The cecal blood supply is derived from the cecal artery, a branch of the ileocolic artery. The medial and lateral cecal arteries (and veins) course in a loose R. Reid Hanson, Jr. wrote the subsection on the Transverse and Small Colon under the section on Anatomy and the section on Surgical Disorders. The large colon, measuring between 3 and 4.5 m, is composed of the right ventral colon (RVC), the left ventral colon (LVC), the left dorsal colon (LDC), and the right dorsal colon (RDC) and begins at the cecocolic orifice and ends at the transverse colon. The large colon forms a long U-shaped loop, which is attached to the dorsal body wall at the R D C and RVC. This welldeveloped, voluminous loop is mobile, predisposing the bowel to anatomic displacements and physical obstructions. The diameter of the large colon varies, with narrowing occurring at the pelvic flexure, formed between the LVC and the LDC. The R D C narrows before entering the transverse colon. The narrow areas are prone to obstruction by digesta or foreign material. The RVC begins at the cecocolic orifice and courses cranioventrally to the sternal flexure, which lies dorsal to the xyphoid cartilage. The RVC is sacculated and has four bands-medial and lateral mesocolic bands and medial and lateral free bands (Fig. 36-2). The RVC is continuous with the LVC at the sternal flexure. The LVC is similar to the RVC in sacculations and bands, and runs caudally to the pelvic inlet. The LVC joins the LDC at the pelvic flexure. At the pelvic flexure, the bands of the LVC fade, leaving the pelvic flexure unsacculated and with a narrow lumen. A single mesocolic band is found in the LDC. The LDC runs cranially to the diaphragmatic flexure and joins the RDC. Three bands are found in the moderately sacculated R D C as it courses caudodorsally, to end in the transverse colon. The RDC has an enormous diameter described as a stomach-like dilatation.' The ventral and dorsal segments of the colon are attached by the intercolonic mesentery. The major blood 380 ALIMENTARY SYSTEM Left dorsal colon Small colon Transverse colon \ The equine large intestine. Note the mesenteric attachments of the cecum are located at the cecal base and right dorsal colon (Redrawn from McIlwraith CW: Equine digestive system. In Jennings PB (Ed): The Practice of Large Animal Surgery. Philadelphia, W. B. Saunders Company, 1984, p 628.) FIGURE 36-1. ~ p e of x cecum supply to the colonic loop running in the mesentery is derived from the right colic artery, supplying the dorsal colon, and the colic branch from the ileocolic artery, supplying the ventral colon (Fig. 36-2).3 These vessels join at the pelvic flexure. The large colon is much less susceptible to thromboembolic disease because of this anastomosis and an extensive plexus of communications, the rete mirabile (within the intercolonic mesenterv). which is peculiar t; the equine specie^.^ Rectal examination is useful in identifying portions of the large colon in health and disease. The pelvic flexure can be palpated in most normal horses, and the ventral colon is easily recognized by the distinguishing bands. The R D C can only be felt with extensive impaction. With the exception of the initial 15 cm of the RVC and the last 25 cm of the RDC, the entire large colon can be exteriorized through a ventral midline surgical incision. J , , ~ ~~ Transversce and Small Colon The transverse colon is a constricted portion of large intestine passing from right to left, cranial to the root of the mesentery. The transverse colon joins the voluminous R D C and small colon (SC) and can be felt at surgery but cannot be exteriorized through a ventral midline incision. The SC, a caudal continuation of the transverse colon on the left of the mesenteric root, occupies the caudal left quadrant of the abdomen along with the jejunum. The SC is approximately 4 m long and has a diameter of approximately 6 to 8 cm. The mesocolon, which suspends the SC from the dorsal body wall, increases to a midsection width of 80 to 100 cm. The SC is connected to the duodenum by the short duodenocolic fold. The SC continues at the pelvic inlet as the peritoneal rectum that enlarges to form the ampulla recti. The SC has wide, muscular mesenteric and antimesenteric bands and coarse sacculations. FIGURE 36-2. Cross-sectional diagram of the equine large intestine, showing longitudinal smooth muscle bands (teniae, dark sections), intercolonic mesentery, and associated vessels. SC, small colon, and associated mesocolon; RDC, right dorsal colon; RVC, right ventral colon; LCA, lateral cecal artery; MCA, medial cecal artery; LVC, left ventral colon; LDC, left dorsal colon; RCA, right colic artery, a branch from the cranial mesenteric artery; CB, colic branch, from the ileocolic artery. The ileum is shown with its dorsal mesenteric attachment and the ileocecal fold, coursing from its antimesenteric band, to the dorsal band of the cecum. The cecocolic ligament courses from the lateral cecal band to the lateral free band of the RVC. (Redrawn from Habel RE: Applied Veterinary Anatomy. Philadelphia, W. B. Saunders Company, 1986, p 247.) LARGE INTESTINE 381 FIGURE 36-3. Lateral view of the small (descending) colon. 1, arcuate artery; 2, marginal artery; 3, long artery; 4, small branch supplying the mesenteric tenia; 5, secondary arcade; 6, small branch to mesocolon. (Redrawn from Beard WL, Lohse CL, Robertson JT: Vascular anatomy of the descending colon in the horse. Vet Surg 18:130, 1989.) The major arterial supply to the SC is from the caudal mesenteric artery, which divides into two major branches-the left colic artery and the cranial rectal artery. The left colic artery supplies the oral 75% of the small colon and branches into four to eight arcuate arteries that divide again into marginal arteries (Fig. 36-3).5.6 The cranial rectal artery courses caudally in the small colon mesentery to supply the aboral 25% of the small colon with similar arcuate and marginal arteries. The joining marginal arteries form one functional artery 1 to 2 cm dorsal to the entire bowel surface, which is obscured from view by mesocolic fat (Fig. 364). Marginal arterial overlapping obviates the need for preservation of the marginal artery when performing resection and anastomosis. The SC can be easily recognized on rectal examination by the presence of fecal balls and the thick antimesenteric band. The oral 30 cm and aboral 30 cm of the small colon cannot be exteriorized through a ventral midline surgical incision. The extrinsic innervation of the large intestine is derived from the celiacomesenteric plexus, celiac and cranial mesenteric ganglion, and pelvic plexus. The more important intrinsic neurons form the enteric nervous system and the myenteric plexus. Extrinsic denervation does not interrupt the intrinsic myoelectric activity of the equine mates of the resorptive capacity of the large intestine of a 160 kg pony approximate 30 Llday, a volume equal to the extracellular fluid volume (ECF) of the animal.8 Fecal water averages less than 10% of ileal outflow (Fig. 36-5), and net fluid absorption may approximate 95% of delivered fluid. Diseases interrupting fluid dynamics could potentially cause life-threatening changes in ECF and electrolyte balance. The greatest quantitative net water absorption occurs in the cecum. Solute transport in the large intestine appears complex but contributes greatly to the transmucosal movement of water. Although digesta osmolality is maintained at roughly isotonic levels from the cecum to the SC, concentrations of cations and anions change considerably. The Na' concentration decreases markedly, but there is a concomitant increase in K+ and NH,- concentrations from the cecum to the SC.' Organic acids increase in the cecum and ventral colon but then decrease in the dorsal and SC. There is a steady increase in the phosphate concentration. Although osmotic changes in organic acid (VFA) production may contrib- The two important physiologic functions of the large intestine include (1) storage and absorption of fluid and (2) retention of digesta for microbial digestion. These functions have extreme importance in fluid and electrolyte balance and nutritional considerations. Complex mechanisms are required to regulate digesta transit, to provide optimal conditions for transport of electrolytes and fluid, and to allow microbial fermentation of digesta.' 5 Fluid Absorption The most important function of the large intestine is likely the absorption of large volumes of fluid. Esti- FIGURE 36-4. Cross sectlon of the small colon with vascular anatomy shown. 1, marginal artery; 2, secondary arcade; 3, long artery; 4, branch supplying tenia; 5, anastomosis across antimesenteric surface. (Redrawn from Beard WL, Lohse CL, Robertson JT: Vascular anatomy of the descending colon in the horse. Vet Surg 18:130, 1989.) 382 ALIMENTARY SYSTEM MAN PONY * 1.5 FIGURE 36-5. Net water movement through the large intestine of a 70-kg man and 160-kg pony. Both species absorb approximately 90% of ileal outflow, but in the pony, this represents approximately 30 Llday. The volume is roughly equivalent to the animal's extracellular fluid volume. Note the cecum of the pony has greatest net water absorption. (Redrawn from Argenzio RA, Lowe JE, Pickard DW, et al: Digesta passage and water exchange in equine large intestine. Am J Physiol 22631035, 1974.) ute to net water movement, it appears likely that Na+ transport is the single most important f a ~ t o r . ~ A net decrease in cecal HCO,- is likely caused by buffering of organic acids. This buffering reaction (NaHCO, HAC + NaAC + H,O + CO, [AC:acetate] may aid in absorption of VFA, Na+ and C0,+.7 An important function of the colon involves acid-base balance. Horses with simple colonic obstructions may develop metabolic alkalosis, because of dis. ~ reduction in ruption of colonic buffering ~ a p a c i t y A VFA production in horses with colonic diseases may decrease the normal Cl-:HCO,- exchange mechanism, and lead to a relative decrease in HCO,- se~retion.~. lo + Microbial Digesti A major physiologic function of the large intestine is retention of fluid and digesta to facilitate important microbial digestion. Like colonic fluid dynamics, microbial digestion is regulated by the rate of passage of digesta through the large intestine. Experimentally, fluid (polyethylene glycol) and particulate markers leave the cecum quickly and are passed to the ventral and dorsal colon (Fig. 36-6).8 Marked retention of particulate markers occurs in the ventral and dorsal colons, which are considered the major sites of digesta retention. Marker concentrations are similar in the RVC and LVC, and therefore, the ventral colon is considered a single compartment. Similar marker concentrations in the LDC and R D C are found, and thus, a single dorsal colonic compartment exists. The ventral-dorsal colonic junction, the pelvic flexure, represents a major barrier to the outflow of markers. The dorsal colon preferentially retains larger markers. Transit of fluid and particulate markers occurs rapidly through the SC. Experimentally, no retrograde transit of carbon occurs from the ventral colon to the cecum or from the dorsal colon to the ventral colon." Neither polyethylene glycol nor particulate markers are passed in retrograde fashion from cecum to ileum, or from dorsal to ventral colon.10 From these results, it appears likely that the ileocecal junction, cecocolic junction, pelvic flexure, and transverse colon are responsible for the retention of digesta and compartmentalization of the large intestine. Mean transit time in the cecum is approximately 5 hours, whereas mean transit time for the large colon is 50 hours. Fifty percent transit of liquid markers to feces occurs 24 hours after oral administration, but 50% transit of particulate markers, 2 cm in length, takes greater than 10 days, demonstrating considerable retention of particulate digesta for microbial digestion (Fig. 3 6 6 ) . This prolonged retention appears to be greater than that in the ruminant fore stomach^.^^ Motility The motor events of the large intestine are complex and are incompletely understood. Both propulsion (the aboral movement of digesta) and retropulsion (the oral movement of digesta) exist in the cecum and the large colon. Digesta enters the cecum from the ileocecal junction, propelled by the migrating action potential complex-a prominent, rapidly progressive electrical event of the ileum.I3 Researchers have identified several motility patterns of the normal cecum through endoscopy and or visually through cannulas,I4.Is cinefluoro~copy,'~ indwelling intraluminal monometry, and by monitoring myoelectric activity.I7.l8 Coordinated series of spike bursts occur in the cecal base, which propel digesta to the cecal apex (Fig. 36-7). Several series of spike bursts within the cecal body appear to contribute to nonprogressive, haustra-to-haustra mixing events. A progressive motility pattern has been identified, which is initiated at the cecal apex, propagated to the cecal body, through the caudal and cranial portions of the cecal base, and into the RVC. This pattern occurs once every 3 minutes in the fed pony, is associated with a loud distinctive "rush" of digesta heard on auscultation, and is likely responsible for the transit of digesta from the cecum to the RVC. An electric pacemaker area located within the ventral 10 to 15 cm of the cecal apex appears to initiate this progressive motility pattern.I3. l8 Several retropulsive patterns, generated from the cranial or caudal cecal base, appear to be coupled with this progressive pattern. In the RVC, the aboral, progressive pattern gen- I LARGE INTESTINE 383 FIGURE 36-6. Retention of liquid and particulate markers by the cecum, ventral colon segments, and dorsal colon segments (including small colon), and fecal excretion of markers. Liquid markers are passed rapidly from the cecum, and 50% excretion occurred within 3 days after administration. Retention of particulate markers increased as marker size increased. Less than 50% excretion of 2-cm markers occurred in 10 days. Note relatively greater retention of larger markers in the dorsal colon. (From Argenzio RA, Lowe JE, Pickard DW: Digesta passage and water exchange in equine large intestine. Am J Physiol 226:1035, 1974.) erated at the cecal apex is rapidly propagated and SSB and LSB may not be useful to describe cecal motor events. Because of the large size and obvious reservoir appears to be the dominant motility pattern. Both nature of the RDC, strong retropulsion likely exists in propulsion and retropulsion exist in the RVC, independent of the progressive pattern. Progressive motor this area, but the motility of the RDC, transverse colon, and SC has not been characterized. events of the RVC likely continue around the sternal Motility of the cecum and large colon is markedly flexure to the LVC and end near the pelvic flexure. The motor events of the pelvic flexure, LVC, and affected by various pharmacologic agents and physiologic changes. Administration of xylazine, an a-2 adre14. l9 Coordinated LDC have been studied e~tensively.~. nergic agonist, reduces cecal progressive motilityU and oral, aboral, and bidirectional pressure peaks exist, mechanical activity24 for 30 minutes. Butorphanol, a originating from the pelvic flexure area, which demonsynthetic narcotic agonistlantagonist, reduces cecal prostrates that a colonic pacemaker region may exist here gressive motility. The combination of xylazine and bu(Fig. 36-8).19 Further study by in vitro electromyography torphanol further delays return of progressive motility. demonstrated the existence of an electric pacemaker and direct electric coupling of longitudinal and circular The anticholinesterase neostigmine increases cecal prosmooth muscle.4-I9 The electric pacemaker initiates progressive motility for approximately 30 minutes. In the large colon, narcotic agonists increase the pulsion and retropulsion, impeding the transit of digesta. Retropulsive spike bursts are likely propagated through resting tone of intestinal muscle, whereas in limited the LVC to the RVC, and propulsive spike bursts may studies of narcotic antagonists, an increase in propulsive continue around the dorsal colons to the transverse motility is seen.25Xylazine and atropine sulfate reduce motility of the pelvic flexure, whereas neostigmine incolon. In vivo electromyography of the cecum and large creases progressive motility.21 The acaricide Amitraz causes dissociation of the coordinated pressure peaks of colon has demonstrated the existence of long spike the LVC and LDC. Paralysis of visceral afferent nerves bursts (LSB) which are longer than 5 seconds and short ~ ~the pelvic flexure by the use of local anesthetics spike bursts (SSB) which are shorter than 5 s e c ~ n d s . ' ~ , of decreases coordinated pressure peaks.19 Feeding and In the colon, LSB are associated with progressive and electrical stimulation of extrinsic nerve supply increase simultaneous mechanical activity, whereas SSB result in intraluminal pressure peaks. Colonic cooling decreases local mixing events. In the cecum, SSB commonly occur conduction velocity and amplitude of pressure peaks.4 during the progressive motility pattern and the terms 384 ALIMENTARY SYSTEM obstruction of the large intestine represent between 37% to 46% of horses admitted for evaluation of colic or for surgical treatment.27-29The type and severity of obstruction dictate whether medical or surgical management is instituted. Large intestinal obstruction differs from small intestinal obstruction because of the aboral position of the large intestine, the large size of the colonic segments, and different physiologic functions and by-products. Simple Obstruction FIGURE 36-7. Myoelectric activity of the cecum and right ventral colon (RVC) in a pony. Time progresses from left to right. The approximate location of the electrodes correspond to the numbers in the anatomic insert. Two progressive motility patterns (b, b') initiate at the cecal apex, the pacemaker region, and progress to sequentially involve the cecal body, base, and continue into the RVC. Retrograde motility patterns (a, a') progress from the cecal base to the apex, before the progressive pattern, forming a repetitive pattern known as the cecal myoelectric complex. A local haustra-to-haustra pattern (c), likely involving mixing events in the cecal body, is present. (From Ross MW, Rutkowski JA, Cullen KK: Myoelectric activity of the cecum and right ventral colon in female ponies. Am J Vet Res 50:374, 1989.) Experimental Strongylus vulgaris infestation results in severe evidence of thromboembolism but fails to consistently alter colonic m ~ t i l i t y . ~Substance ,'~ P-like immunoreactivity of enteric neurons is found in submucosal ganglia, although its relationship to motility is unknown.26 Simple obstruction (nonstrangulating), characterized by complete or near-complete occlusion of the intestinal lumen, and strangulation obstruction, characterized by vascular compromise of the involved intestine, occur frequently in the large intestine. Horses with Simple obstruction of the large intestine is common and is caused by impaction with feedstuffs, fibrous foreign material, enteroliths, and fecaliths. Simple obstruction also occurs with nonstrangulating displacement of the large colon, although displacement may progress to strangulation obstruction. Functional obstruction, known as spasmodic colic, is a form of simple obstruction. Pathophysiologic changes with simple obstruction vary with severity and duration of the lesion. Partial obstruction, such as cecal impaction, or intermittent enterolith obstruction of the RDC, causes mild pathophysiologic changes. Complete simple obstruction can progress rapidly, however, causing severe clinical signs and irreversible pathophysiologic changes. Abnormal motility, causing ileus or, for example, impaction of the ventral colon, leads to the gradual accumulation of gas from microbial digestion. The large size of the ventral colon allows great quantities of gas to accumulate, causing abdominal distention and colic. Accumulation of digesta and fluid contribute to distention. Intestinal distention can decrease intestinal blood flow, but in cats, intraluminal pressure increases from 34 to 54 cm H 2 0 are needed for this to occur.30 In equine natural small intestine obstructions, intraluminal pressure changes of only 4.5 to 21 cm of H,O are found.31 Pressure changes in large intestinal diseases may be higher and may contribute to vascular derangements. Increases in intraluminal pressure could increase mural pressure, causing collapse of venules, increased capillary hydrostatic pressure, and interstitial edema. In the small intestine, mural edema does not develop after 4 hours of luminal distention." In ponies with experimentally produced pelvic flexure impaction, there is an increase in blood flow to intestinal segments with obs t r ~ c t i o n In . ~ ~horses operated on with simple obstructions, mural edema occurs, although it is not known whether edema is related to distention or other hemodynamic changes. Initial increases in intestinal blood flow may contribute to mural congestion and cause edema. Simple obstruction alters normal fluid and solute absorption. The colon may become secretory, contributing to luminal distention and clinical dehydration. Abnormal fluid dynamics with net fluid and electrolyte loss into the lumen may contribute to disturbances of motility and further propagate the obstructive process. In simple obstruction, septic or endotoxic shock is unusual and does not occur until late when necrosis of the intestinal segment occurs. Depletion of plasma vol- LARGE INTESTINE 385 FIGURE 36-8. Motor events of the left ventral and left dorsal colon segments and pelvic flexure. Number of motility tracing channels corresponds to the portion of the intraluminal catheters located in anatomic insert. Note the coordinated bidirectional pressure peaks, starting between loci 3-4, corresponding to both propulsion (4 + 6 ) and retropulsion (3 + 1). A wandering pacemaker area exists that initiates the bidirectional and unidirectional peaks and is responsible for controlling coordinated motility events in the area of the equine large intestine. (From Sellers AF, Lowe JE, Brondum J: Motor events in equine large colon. Am J Physiol 237:E457. 1979.) causing ume and reduction of cardiac output clinical signs of dehydration, elevation of the heart rate, and poor peripheral perfusion. These changes generally occur late in most horses with simple obstruction, and many of the systemic changes may be related to pain rather than to the hemodynamics of fluid loss. Acid-base disturbances occur but are generally not severe. The classic metabolic disturbance of horses with colic, namely metabolic acidosis, is uncommon in horses with simple obstruction, unless ischemia and necrosis of the obstructed segment occurs. Necrosis of the small or large colon can occur with severe impactions. Horses with cecal perforation secondary to simple obstructions develop cardiovascular collapse and metabolic acidosis. In horses with spasmodic colic (gaseous distention of the large colon) or impaction of the large colon, mild metabolic alkalosis may occur, secondary to alterations of VFA production and normal Cl-:HCO,- exchange mechanism (see the section on Physiology). Severe gaseous distention of the large colon may compress the duodenum, causing partial or complete obstruction. This results in retention of gastric and upper gastrointestinal secretions, and may lead to further metabolic alkalosis because of sequestration of gastric hydrochloric acid. Generally, acid-base disturbances are mild. The hallmark pathophysiologic changes of horses with simple obstruction, namely, gas distention and secondary distention of intestinal segments orad to the obstruction, abdominal distention, pain, progressive dehydration, slow cardiovascular collapse, and mild acidbase disturbances, progress with the severity of the lesion. Because of the aboral location of the large intestine relative to the small intestine, cardiovascular changes are generally slower to develop. Within the large intestine, horses with small colon obstruction develop signs more slowly than horses with large colon obstructions. Therefore, clinical signs may take 24 to 48 hours to develop. Abdominal auscultation of horses with simple obstruction often reveals an increase in borborygmi early in the disease process, followed by a progressive decrease. In ponies, experimental simple obstruction of the small intestine produces similar initial increases in electric activity in the oral segment, followed by a progressive decrease later in the obstructive process.35 Strangulation Obstruction Strangulation obstruction occurs most commonly due to volvulus (torsion) of the large colon (VLC) but can affect the cecum and SC as well. Two forms of strangulation obstruction exist. Hemorrhagic strangulation obstruction occurs when luminal obstruction is ~ ~this common accompanied by venous o c c l ~ s i o n .In form, there is a rapid onset of mural edema; thick, dark purple serosa; and purple-black mucosa. The second form, ischemic strangulation obstruction, involves luminal compromise plus venous and arterial occlusion.36 In ischemic strangulation obstruction, more mild edema develops, and the bowel serosa becomes gray or bluegray. In horses with VLC, hemorrhagic strangulation obstruction is most common but can rapidly progress to .~~ a combinacomplete ischemic o b s t r ~ c t i o nTherefore, tion of pathophysiologic mechanisms is generally present. The prognosis in horses with this severe form of disease is poor. Initial venous occlusion causes severe edema of the bowel wall and stagnation of blood flow. Vascular occlusion and low-flow states cause mucosal damage. Although mucosal changes have not been studied exten- 386 ALIMENTARY SYSTEM sively, changes may be similar to those seen in small intestinal o c c l ~ s i o n .In ~ ~ the small intestinal villi, a countercurrent exchange mechanism exists owing to the ~~ low-flow hairpin-like vascular a r r a n g e ~ n e n t .During vascular states, oxygen and other nutrients may "shortcircuit7' the villus tip, leaving the tip relatively anoxic compared with the villus base.36 During venous occlusion, this mechanism would explain the initial and most severe changes seen at the villus tip.36 In the colon, the mucosal architecture is different, but because of the close proximity of arterioles and draining venules, a countercurrent exchange mechanism may exist to explain mucosal damage."38 If both venous and arterial occlusion exist, or initial venous occlusion progresses to arterial occlusion, more severe histologic changes result. In horses with ischemic occlusion or hemorrhagic occlusion, the histologic changes may be similar. The equine colonic mucosa may be approximately 25% more resistant to ischemia than ~.~~ the equine small intestinal m u ~ o s a . ~Histologic changes of hemorrhage and edema in the mucosa and submucosa, the degree of superficial and crypt cell damage, and a measurement that reflects mucosal pres~,~' sure are used to grade large colon d a ~ n a g e . ~With increasing mucosal edema, there is an increase in interstitial-to-crypt ratio, a measurement of the width occupied by the interstitium relative to crypt Increasing interstitial-to-crypt ratio, an increase in the percent of superficial colonic mucosal cell sloughing, and an increase in crypt cell damage correspond to more severe colonic damage.36 Fluid and electrolyte loss accompany progressive mucosal damage. In hemorrhagic occlusion, initial fluid loss and cardiovascular collapse accompany bowel edema and mucosa damage, causing clinical signs of hypovolemic shock. In horses with advanced hemorrhagic occlusion or with ischemic occlusion, extensive mucosal damage is accompanied by disruption of the mucosal barrier. Transmural necrosis occurs, allowing absorption of endotoxin and, later, enteric bacteria access to the peritoneal cavity and then to the systemic c i r ~ u l a t i o n .The ~ ~ hepatic reticuloendothelial system, which is normally able to absorb endotoxin efficiently, becomes ischemic with cardiovascular deterioration, and further endotoxin distribution occurs.40 Endotoxin causes further deterioration in the hemodynamic, hematologic, and blood chemical systems, including hypotension, increased packed cell volume, leukopenia, metabolic acidosis, disseminated intravascular coagulation (DIC), and disruption of glucose metab~lism.~' From both a pathophysiologic and clinical standpoint, the most important consideration in treatment and prognosis is early medical and surgical intervention to limit loss of bowel integrity. Progressive bowel deterioration causes clinical signs of cardiovascular collapse, tachycardia, poor peripheral perfusion, increased capillary refill time, and poor peripheral pulse. Dehydration is accompanied by an increase in packed cell volume (PCV), but with further loss of bowel integrity, loss of plasma protein total (TTP) occurs. Elevation of PCV may not be accompanied by an increase in plasma protein, and the increase in PCV/TTP ratio is generally a poor prognostic sign. The pathophysiologic mechanism leading to mucosal damage during hemorrhagic or ischemic insults is clear, but recently, additional damage caused by return of blood flow, or reperfusion injury, has come to light. After surgical correction of strangulation obstruction, further damage may occur. Lipid peroxidation and protein denaturation leading to enzyme activation and alteration of membrane integrity occur, secondary to an increase in superoxide (0,) radicals, hydroxyl radical (,OH), single oxygen, and hydrogen p e r o ~ i d e . ~ ~ . ~ ~ Normal scavenging systems, including ascorbate, glutathione peroxidase, catalase, and superoxide dismutase may be depleted, allowing the build-up of damaging free radicals.36 During the ischemic period, neutrophils build up and may increase the severity of the reperfusion i n j ~ r y . ~In ~ ,clinical "~ situations, serosal color and gross vascular supply may improve after a strangulated segment is untwisted. However, mucosal and submucosal damage continues, leading to ileus, peritonitis, cardiovascular collapse, and death within 1 to 3 days. For an in-depth discussion on this subject, please review Chapter 33. Cecum Cecal Impaction ETIOLOGY The most important disease of the cecum is cecal impaction (CI), which represents approximately 5% of all intestinal impaction^.^. 45- Cecal impaction generally involves fibrous feedstuffs, but impaction with sand can occur. Although classic cases of CI include older horses with poor dentition and fed poor quality feedstuffs, recent reports indicate that younger horses, particularly horses hospitalized for other nonrelated disorders, are , ~ ' pathogenesis of CI likely involves a at r i ~ k . " ~ The primary cecal motility dysfunction. Observations at surgery or necropsy reveal a large, digesta-filled cecum and a relatively empty RVC (Fig. 36-9). Because only a single motor event is common to the cecum and RVC, interruption of this progressive motility pattern leads to cecal filling (see the section on Physiology). Propulsion in the RVC continues, and this segment empties. Altered cecal blood flow secondary to parasite damage, dietary changes, or other clinical conditions may interrupt or slow the cecal pacemaker. Transit of small volumes of digesta and gas continue, because oil appears in the feces and gas accumulation of the cecal base is unusual. Initially, digesta is normal in character but may become dry, resembling the expected "impacted digesta." HISTORY AND CLINICAL SIGNS Typically, horses with CI are intermittently anorexic, depressed, and show signs of mild abdominal pain, such as looking at the flanks, rolling, and pawing. Frequently, the horses have experienced a management LARGE INTESTINE 387 FIGURE 36-9. The cecum and large colon. ( A ) , Cecum and large colon from a normal horse, showing, the normal relative size of the organs. (B), Cecum and large colon from a horse with cecal impaction and subsequent perforation. Note the large, digesta filled cecum and relatively empty large colon. A motility dysfunction exists that causes cecal filling but allows colonic emptying. This lesion is found in horses with cecal impaction or cecal perforation secondary to cecal outflow dysfunction. change or are being treated for unrelated gastrointestinal or musculoskeletal disorders. Vital parameters and laboratory values are usually within normal limits. Rectal examination is diagnostic, but in rare instances, the enlarged cecum cannot be felt. The clinician must differentiate the cecum from other organs such as the RDC or a displacement of the ventral colon. A firm, near-hard viscus is often felt, with a single, distinct band (ventral cecal tenia). The cecum is attached to the dorsal body wall, and the examiner cannot pass a hand dorsal to the impacted mass. Because the colon is usually empty, it is difficult to feel the pelvic flexure. Fecal production is reduced, and feces range from dry to "cow-flop" in nature. Intermittent diarrhea can occur. Cecal progressive borborygmi are reduced. TREATMENT SELECTION.Disagreement exists over the most appropriate treatment of horses with CI. Medical manMost authors acknowlagement has been ad~ocated.~~-'O edge the limitations of medical management, although one author reports good success.50 Because the chance of cecal perforation exists with continued cecal filling, other authors have recommended surgical management, particularly in horses unresponsive to medical therapy. Earlier surgical techniques included manual massage, sometimes accom~aniedbv water infusion of the impacted digesta, evacuation of cecal contents by enterotomy (typhlotomy), and partial to complete typhlect ~ m y .47,~ 49,~ 51-53 . Results with enterotomy and evacuation of cecal contents, or infusion and massage, were variable, which sparked development of newer surgical techniques.'16 These techniques were developed to address the pathogenesis of CI, namely the development of a primary cecal motility dysfunction, which is slow to return after surgery. Currently, management of horses with CI depends largely on the result of rectal examination and physical examination of the patient. If the cecum is small or moderate in size and the patient's vital parameters are normal, initial medical management is recommended. 388 ALIMENTARY SYSTEM Surgery is recommended if the cecum is extremely large, or the digesta is near hard in consistency, in horses with CI refractory to medical management, or in horses with recurrent CI.54 NONSURGICAL MANAGEMENT. Successful medical management requires both oral and intravenous fluid therapy, and withholding feed until the cecum returns to normal size, based on rectal examination. Neostigmine (0.0125 to 0.025 mglkg) may increase cecal progressive motility, and has been used with limited success; however, one should be extremely careful because cecal perforation is a potential sequela. Until it is clinically justified, use of the drug should be restricted to horses with recurrent impaction or when economic constraints restrict surgical intervention. Stimulation of cecal motility by walking and grazing may represent a beneficial adjunctive treatment, although the volume of grass ingested must be closely regulated. Because fasting causes cessation of cecal progressive motility, it may be important to stimulate motility in this manner.13 SURGICALMANAGEMENT.Recently, several surgical techniques have been developed to prevent recurrence of clinical signs and are used in conjunction with surgical techniques such as infusion, massage, or simple evacuati~n.~~-~' Typhlotomy. Typhlotomy may be used alone or in combination with cecocolic, jejunocolic, or ileocolic anastomoses. Typhlotomy is performed midway between the ventral and lateral cecal bands, after appropriate draping has been performed to prevent peritoneal contamination. Peritoneal contamination is generally more common with typhlotomy incisions than with colotomy incisions, because only the apex and body of the cecum can be exteriorized. The surgeon must remember that the cecal base is divided and the cupula (cranial base) is generally large and digesta filled and needs to be emptied. Cecocolic Anastomosis. Cecocolic anastomosis, a technique developed to avert the possible postoperative complications of recurrent CI and perforation, provides an alternative route of digesta transit from the cecum to the RVC (Fig. 36-10).55 Generally, the technique is combined with typhlotomy and evacuation of cecal contents. The anastomosis, a combination of hand-sewn seromuscular layer closures and use of the GIA-stapling instrument (U.S. Surgical, Norwalk, CT), is performed between the lateral and dorsal cecal bands, and the lateral free and lateral mesocolic bands of the RVC. In the original report, 12 of 14 horses (86%) survived 2 months or longer and 10 horses (71%) survived longer than 1 year. Four horses had intermittent colic related to gas distention of the cecum or large colon, but none developed recurrent cecal impaction. Jejunocolic and Ileocolic Anastomoses. Jejunocolic'6 or ileocolic anastomosess7represent more recently developed surgical techniques designed to completely or incompletely bypass the cecum, thus rerouting digesta from the aboral small intestine to the colon. Typhlotomy with cecal evacuation can be performed. Jejunocolic or ileocolic anastomoses can be performed in a side-to-side fashion, using combined hand-sewn seromuscular layer closures and use of the GIA-stapling instrument. The incomplete side-to-side ileocolic anastomosis did not FIGURE 36-10. The cecum and origin of the right ventral colon. The dotted areas show the location of the cecocolic anastomosis, a surgical procedure useful for horses with cecal impaction. The anastomosis is performed between the lateral (A) and dorsal (B) cecal bands, and the lateral (C) and medial (D) free bands of the RVC. The cecocolic ligament (E) runs between the lateral cecal band and lateral free band of the RVC. (Redrawn from Ross MW, Tate LP, Donawick WJ, et al: Cecocolic anastomosis for the surgical management of cecal impaction in horses. Vet Surg 15:85, 1986.) prevent cecal filling, and the complete ileocolic anastomosis with ileal transection was s ~ p e r i o r . ~However, ' the incomplete jejunocolic anastomosis was successful in preventing recurrence of CI in one horse.s6 In summary, if surgery is required in horses with CI, typhlotomy and manual evacuation should be followed by some form of bypass procedure. Complete ileocolic anastomosis offers advantages over other procedures and has been effective clinically. Incomplete ileocolic or jejunocolic anastomoses, or cecocolic anastomoses remain viable surgical alternative. Cecal Perforation - PATHOGENESIS Cecal perforation (CP), although not considered a surgical disease, is a relatively recently characterized, important cecal disease. Because of the close association of CP to CI, equine surgeons should be familiar with the pathogenesis of the disease. The pathogenesis of CP, a uniformly fatal disease, appears to involve two different pathways: (1) CP may be primarily idiopathic in origin in broodmares near parturition, in which no obvious cecal motility dysfunction exists; and (2) more commonly, CP is secondary to a primary cecal motility dysfunction, which although undetected, leads to cecal filling and, later, to perforation. IDIOPATHIC DISEASE. Cecal perforation and LARGE INTESTINE death occurred in 11 horses within 24 hours after parturiti~n58-62 and during gestation in one mare.63 In this form of CP, gas accumulation may lead to perforation. The cecum and colon are normal in size, and no accumulation of digesta is found. In women undergoing obstetric procedures, signs of intestinal obstruction and late CP may occur. Cecal perforation in horses may be similar to this form of intestinal pseudo-obstruction (Ogilvie's syndrome) in humans. M o n ~ mDYSFUNCTION. The most common form of CP appears to be related to a dysfunction of cecal motility, leading to filling (impaction) and subsequent perforation. At necropsy examination, the cecum appears large and digesta filled, and the colon is relatively empty (see Fig. 36-9), similar to that seen in horses with CI. In a recent study, 22 horses (6 weeks to 13 years of age) had signs of CP.61 All horses had a single site of perforation (Fig. 36-11). The majority of these horses were hospitalized, receiving treatment with nonsteroidal anti-inflammatory drugs (NSAIDs). Early signs of the disease may be masked by the analgesic properties of NSAIDs, allowing horses actually affected with CI to progress to CP. Horses hospitalized with other disorders and treated with NSAIDs also appear to be at risk to develop CP. Subtle signs of gastrointestinal disease, such as partial anorexia, a reduction in fecal output, a change in fecal quality, or decreased borborygmi, should be carefully investigated. A rectal examination is indicated, but the clinician must remember that because of colonic emptying, the enlarged cecum can assume a more cranial location and may not be palpable. Clinical signs after CP include those seen with severe endotoxin shock or gram-negative sepsis. Although complete typhlectomy and peritoneal lavage remain theoretical treatment alternatives, euthanasia is most appropriate. 389 Cecocecal and Cecocolic lntunusception HISTORY AND CLINICAL SIGNS Intussusception of the cecal body into the base or a continuation of the invagination into the RVC is .~~~ uncommon but requires surgical i n t e r ~ e n t i o n The disease is not breed, age, or sex specific. The etiology is unclear, but various authors have suggested the involvement of the tapeworm Anoplocephala perfoliata. Tapeworms may cause abnormal motility of the cecum if they are present in high number^.^' Tapeworms were present in only 3 of 10 horses with intussu~ception.~~ A recent report questions the importance of tapeworms, because intussusception occurred in horses not infested with tapeworms with a frequency of two times that of infested horses.68 Abnormal motility caused by an organophosphate was proposed as a cause of intussusception.(j9 Three distinct forms of the disease exist, based on clinical examination and duration of the clinical signs. In the acute form, horses have severe abdominal pain and require immediate attention. Changes in vital parameters and laboratory values are generally more severe in this form, and the acute onset may reflect a greater degree of vascular and neural compromise of the intussusceptum. In the subacute form, horses are generally depressed and have intermittent abdominal pain and reduced fecal output. In the chronic form, horses exhibit weight loss, pyrexia, and mild, intermittent abdominal pain. When the invaginated portion becomes devitalized, there is an exacerbation of clinical signs, cardiovascular deterioration, acidosis, and changes in peritoneal fluid values. The clinical signs vary, depending on the time of examination relative to the onset of the disease. Rectal examination is most helpful in establishing the diagnosis. Four of eight horses with intussusception had an enlarged viscus felt on rectal examination, and in some horses, the cecum was not palpable at TREATMENT MEDIAL LATERAL FIGURE 36-1 I . Diagram of the medial and lateral aspects of the I 1 cecum, showing the reported sites of cecal perforation in 17 horses. A single site was identified in each horse. a, dorsal base, 3 horses; b, dorsomedial base, 2 horses; c, ventromedial base, 1 horse; d, ventral body, 6 horses; e , lateral body, 3 horses; f, distal lateral body, 2 horses. The interrupted line indicates the anatomic division between the cecal base and body. The cecum may perforate more frequently along bands, but no location appears particularly at risk. (From Ross MW, Martin BB, Donawick WJ: Cecal perforation in the horse. J Am Vet Med Assoc 187:249, 1985.) Surgical management is mandatory for a successful outcome, and in some horses, exploratory surgery is necessary to confirm the diagnosis. At surgery, the cecal apex is not found or a mass may be identified in the cecal base or the origin of the RVC. Manual reduction is often possible. The involved cecum is generally edematous, devitalized, and requires resection. Following double ligation of the medial and lateral cecal vessels, the devitalized portion is resected, followed by a double inverting closure of the cecal body. As much as 50% to 60% of the cecum can be removed through a ventral midline approach. In horses with cecocolic intussusception in which extramural manual reduction is not possible, an enterotomy of the RVC is necessary. The 15- to 20-cm long colotomy incision, made between the medial and lateral free bands of the RVC, is followed by intraluminal resection and closure of the edematous cecal apex. Double ligation of the cecal vessels is required. After resection and closure, eversion of the cecum through 390 ALIMENTARY SYSTEM the cecocolic orifice is usually possible. Once the colotomy incision is closed, an additional closure of the cecal body is performed. Manual reduction of the intussusceptum from within the lumen of the RVC can precede resection in some horses. The prognosis is considered favorable, if all of the necrotic cecum can be removed. The pacemaker area, necessary for generation of normal cecal motility, wanders over a 40 cm area near the apex in ponies.'' Therefore, nearly the entire cecal body can be removed. Cecal Infarction Thromboembolic disease of the cecal arteries is rare but can occur following damage from S. vulgaris migration. The arterial supply of the entire cecum arises from the single cecal artery, a precarious vascular arrangement. The medial and lateral cecal arteries are located 180 degrees apart and lack extensive communications, further predisposing the cecum to vascular insult. The disease can occur in a horse of any age but is more common in horses younger than 1 year of age. Clinical signs can vary from those associated with acute, severe abdominal pain and cardiovascular collapse, requiring immediate surgical intervention to low-grade abdominal pain, diarrhea, and peritonitis. Peritoneal fluid changes reflect ischemic necrosis. Surgical therapy consisting of partial typhlectomy may be successful, if the entire necrotic portion can be removed. Complete typhlectomy after 18th rib resection in left lateral recumbency is also a consideration. Progressive infarction after surgical removal can occur. The prognosis in these horses is grave. Cecal Torsion As a primary disease entity, cecal torsion is rare but can occur under unusual situations, such as with adhesion or entrapment of the cecum. Normally, the cecum is relatively immobile and can move only with concomitant movement of the RVC and ileum. Recently, cecal torsion was described as a consequence of hypoplasia of the cecocolic ligament.'O The cecum may be displaced or twisted in horses with volvulus of the large colon. When this occurs, the axis of rotation involves the dorsal mesenteric attachment of the cecum. The lesions in these horses are often severe, and the prognosis depends on the degree of vascular compromise. If a true cecal torsion is present, partial or complete typhlectomy may be necessary. Miscellaneous Conditions of the Cecum Adhesion of the cecum to the ventral body wall is unusual, except after ventral midline exploratory incisions. Clinicians have suspected cecal adhesion in horses with mild, intermittent colic. Rectal examination may reveal chronic cecal malposition. Cecal-cutaneous fistula is rare but was reported after application of an umbilical hernia clamp.'l Congenital abnormalities are rare, but the author has observed a single horse with colic due to absence of the dorsal mesenteric attachment of the cecum and subsequent large colon displacement. Large Colon The large colon is particularly prone to simple and strangulation obstruction because of certain physiologic functions. Retention of digesta and water absorption, complex motility patterns, the relative lack of mesenteric attachment, and changes in lumen diameter predispose the large colon to disease. Many forms of simple obstruction respond favorably to medical management but may progress to or be confused with lesions requiring surgical intervention. Impaction of the Ventral Large Colon ETIOLOGY Impaction of the ventral colon is one of the most common and important diseases of the equine colon. Commonly referred to as pelvic flexure impaction, this form of simple, intraluminal obstruction involves the accumulation of digesta in the LVC initially, with subsequent filling of the sternal flexure and RVC. The pathogenesis likely involves interruption or dysfunction of the pelvic flexure pacemaker region. Impactions are unlikely to develop through simple ingestion of dry or coarse feedstuffs. A decrease in propulsive motility or an increase in retropulsive motility could cause the accumulation of digesta. In horses with colonic impaction, the digesta appears to be retained just orad t o the pelvic flexure, involving a long segment of the ventral colon, and does not simply involve the pelvic flexure alone. The digesta is generally firm and contains fibrous feed material, although sand accumulation can cause a similar lesion. In horses with sand im~actionof this area, a shorter segment of colon is involved and the actual pelvic flexure can be obstructed. Factors such as poor feed quality, poor dentition, reduced water intake, and parasite damage could cause impaction. Change in management conditions such as a stable change, a move from pasture to barn housing, shipping, and systemic diseases may also predispose the large colon to impactions. HISTORY AND CLINICAL FINDINGS Typically, horses with impaction of the ventral colon exhibit a gradual onset of clinical signs. Often, horses are partially or completely anorexic, and there is a gradual decrease in fecal production. Signs of lowgrade abdominal pain, such as rolling, pawing, stretching, and looking at the flanks, are present initially but may progress to signs of severe abdominal pain with increasing large colon distention. Initial vital parameters are normal, but during painful episodes, heart and respiratory rates can be moderately elevated. Initially, auscultation may reveal an increase in borborygmi, but with disease progression, intestinal sounds are often reduced or absent. It could be shown experimentally LARGE INTESTINE that loud longer borborygmi are associated with colic and simultaneous increases in intraluminal pressure of 40 mm Hg.33 Horses treated early with oral fluid and electrolytes, restriction in oral feed intake, and analgesics to control abdominal pain generally respond favorably. However, many horses are refractory to early or inadequate treatment, and clinical signs progress. Signs may progress for 5 to 7 days. Gradual filling of the LVC and RVC with digesta and subsequent gas distention of the ventral colon and cecum occurs with complete obstruction. A gradual increase in abdominal distention is accompanied by increased signs of abdominal pain and an elevation in heart and respiratory rates. Auscultation reveals tympanitic sounds, and simultaneous auscultation and percussion reveal a high-pitched "ping" over the cecum. Clinicopathologic changes are generally minimal, but there may be a mild increase in PCV and total protein levels, indicating mild dehydration. Peritoneal fluid changes occur only with advanced impaction and subsequent devitalization of the colon. Late in the disease, progressive distention of the RVC and cecum may cause duodenal compression and passive build-up of gastric fluid, but this is unusual. During rectal examination, the firm, enlarged terminal LVC can be readily palpated. Often, the left colon segments are rotated 90 to 180 degrees in horses with impaction of the ventral colon. The LVC can be identified by the distinct free and mesocolic bands. Rectal examination is useful in monitoring progress of the impaction. The initial soft, doughy mass may progress to a firm, near-hard, digesta-filled ventral colon. Cecal gas distention can be readily palpated. Occasionally, the LVC and pelvic flexure are pushed caudally into the pelvic canal. Rectal examination reveals the firm, impacted viscus close to the anus. Obstruction in these horses is complicated by additional extraluminal restriction of the pelvic canal, resembling a pelvic hernia.72 TREATMENT NONSURGICALMANAGEMENT. Horses with impaction of the ventral colon should respond favorably to medical management. Withholding feed and admin- istering oral and intravenous fluids and analgesic therapy are usually successful. Feed should be withheld until the colic subsides, manure production has returned, and the impaction has resolved, based on rectal examination findings. During resolution of the impaction, semiformed and sometimes fluid feces can be passed. Occasionally, clinicians report mild colic associated with the return of normal motility and resolution of the impaction. The pathogenesis o f impactions may, in part, involve dehydration of the impacted digesta. Transit of dry digesta may be further impeded. Aggressive oral fluid therapy (8 L water and electrolytes given via nasogastric tube, three to four times each day), combined with intravenous fluid therapy (1 to 2 Llhr), hydrates the digesta, returns the patient to a more normal systemic hydration status, and may improve local conditions of the bowel wall that are necessary for normal motility. Abdominal pain is controlled by judicious use of flunixin meglumine in most horses. In some horses, however, xylazine administration is needed and effective for more potent analgesia, but xylazine inhibits progressive motility of the colon for a minimum of 30 minutes The clinician must avoid giving after admini~tration.~~ multiple doses of xylazine or narcotic analgesics, because motility dysfunctions may be prolonged. SURGICALMANAGEMENT. Surgical management is necessary in horses with impaction causing severe abdominal distention, in horses with severe abdominal pain, or in horses with progressive cardiovascular deterioration or changes in peritoneal fluid values. Ventral midline exploratory celiotomy reveals various degrees of digesta filling of the ventral colon and a small LDC (Fig. 36-12). Edema of the intercolonic mesentery and mild thickening of the bowel wall are commonly encountered. Extreme care must be taken not t o rupture the distended ventral colon during manipulation. To prevent this fatal sequela, the surgeon should use the arms for bowel handling (see Fig. 33-19), and use large abdominal incisions (up to 45 to 50 cm in some horses). Occasionally, infusion of sterile saline solution and massage of the digesta result in a successful outcome. Enterotomy combined with evacuation of the accumulated digesta is most successful but must be performed Origin of small colon FIGURE 36-12. Drawing of the equine cecum and large colon of a horse with impaction of the ventral large colon during colotomy and evacuation. The ventral colon segments are enlarged with firm digesta, whereas the dorsal colon segments are small and relatively empty. The enterotomy is performed between free bands in the terminal left ventral colon and a soft rubber tube is used to provide warm water lavage of the impacted colon. The same technique can be used for impaction of the colon at other sites. (Redrawn from Foerner JJ: Diseases of the large intestine, differential diagnosis, and surgical management. Vet Clin North Am Equine Pract 4:130, 1987.) 391 392 ALIMENTARY SYSTEM with adequate preparation to avoid excessive contamination. The enterotomy should be performed in the terminal LVC between bands. The pelvic flexure and origin of the LDC should be avoided. Evacuation is aided by using a hose and large volumes of water. An assistant, prepared and gowned for aseptic surgery, is necessary to aid during manipulation of digesta in the RVC. The prognosis after surgery is good to excellent. Occasionally, a motility dysfunction persists and impaction recurs. Medical management is instituted. Impaction of the Right Dorsal Colon ETIOLOGY The RDC preferentially retains larger digesta particles and has a large reservoir function for microbial digestion. Strong retropulsion must exist. Marked narrowing of the lumen diameter occurs as the RDC enters the transverse colon. Because of these factors, the RDC is prone to impaction. Impactions of the right dorsal colon are not as common as those of the ventral colon but generally consist of very firm digesta or sand. Horses with this disease may respond slowly to medical therapy and are at risk for recurrence of the problem. Impaction of the RDC may be more common in mares before parturition, which suggests that a motility problem may be a factor. An enlarged firm RDC is often found in horses with nonstrangulating displacements or volvulus of the large colon. The pathogenesis may involve a primary motility dysfunction of the RDC, digesta and gas accumulation, rotation with eventual displacement, or volvulus. HISTORY AND CLINICAL FINDINGS Horses with impaction of the RDC show signs similar to that seen in horses with impactions of the cecum or ventral colon. Because of the aboral position of the impaction, signs are slow to progress. Intermittent fecal passage indicates that a partial obstruction may exist. In horses with advanced disease, secondary duodenal obstruction due to enlargement of the RDC may cause gastric distention. Rectal examination is most helpful. In the normal horse, the RDC is not palpable. In horses with impaction, the RDC shifts caudally and may be palpated as a firm viscus without obvious bands. Occasionally, a mesocolic band with an associated vessel is felt. The examiner can usually pass the hand dorsal to the firm viscus, a useful technique to help differentiate impaction of the RDC from that of the cecum. In these horses, the clinician is most likely palpating the oral portion of the RDC. TREATMENT NONSURGICAL MANAGEMENT. Aggressive medical management as described for horses with impaction of the ventral colon can be successful, but horses may be refractory to treatment. Prolonged impaction of the RDC may lead to perforation. SURGICALMANAGEMENT. Surgical management generally involves softening the impacted material with infusion of saline or water. This process can be performed through a needle and tubing apparatus or with the aid of a nonsterile assistant passing a hose from the anus. This procedure has been termed a "high-enema." However, if a large volume of digesta or sand is present, enterotomy may be necessary. Enterotomy in the LVC, combined with the use of the intraluminal tube, is the safest method to avoid possible peritoneal soiling. A sterilely prepared assistant to help with manipulation and evacuation of the material is necessary. Removal of impacted sand by this method is difficult because the sand tends to settle in this area. Recurrent impaction or obstruction of the RDC may be caused by functional obstruction. In a recent case of recurrent colic, a contracted, corrugated RDC was detected during emergency celiotomy." A functional obstruction of the RDC, postulated to be related to irritable bowel syndrome in humans, was suspected. A side-to-side colocolostomy between the RDC and SC was successful in alleviating clinical signs. Fibrous Foreign Body Obstruction Obstruction of the RDC, transverse colon, and oral SC can occur with nondigestible material. Bailing twine, rubber fencing, nylon material, socks, or other nondigestible material cause obstruction. Typically, a hard concretion of fecal material forms around these substances. Rubber fencing material causes a classic form of the disease after horses ingest strands of the polyester and nylon fiber. In one notable outbreak, 28 horses had colic after ingesting the material.74 In one study, 10 of 207 horses with colic had fibrous foreign body impaction. Affected horses were 3 years of age or younger and had mild colic signs.75In the original description, 2 to 5 years were needed for obstruction to occur after ingestion of the material.74 Signs are similar to those seen with impactions, including the ability to pass mineral oil around the offending material, but surgical management is mandatory. The site of obstruction is nearly always the terminal RDC or the transverse or oral SC, sites that are not directly accessible. One or more enterotomies located orally or aborally to the lesion may be needed. Enterotomy in the dorsal colon, followed by manual retrieval, is most useful. Retrograde flushing or other forms of hydropulsion are ineffective because the concretions are tenacious. In horses with long-standing obstruction, the bowel wall may be devitalized, rendering a grave prognosis. If the bowel wall is healthy and the offending material can be removed, the prognosis is good. In one report, 5 of 10 horses Enterolith Obstruction ETIOLOGY Enteroliths, which are large concretions formed primarily of ammonium magnesium phosphate, can obstruct the terminal RDC, transverse colon, or SC. The ; I I 1 1 I LARGE INTESTINE mineral is deposited in concentric layers around a nidus of foreign material, such as small pieces of wood or chert or a small ~ t o n e . Ammonia ~ ~ . ~ ~ is continually produced in the large colon, and phosphates are found in abundance in horse feeds. The limiting factor in enterolith formation may be the level of magnesium in ingested feed or water.76 Enteroliths are formed in two basic shapes, spheres or tetrahedra. Clusters can occur, and multiple enteroliths are common. Enteroliths generally are not found in horses younger than 5 years of age and are most common in horses 5 to 10 years of age.78 CLINICAL SIGNS Clinical signs are typical of horses with impaction colic with one exception. Horses with enteroliths fail to pass any feces when complete obstruction occurs. Failure to pass manure for up to 24 hours may alert the clinician to this form of colic. Typically, signs are intermittent for several days, and then when complete obstruction occurs, they progress to become acute. Gas and fecal distention of the colon oral to the lesion cause abdominal distention. Vital parameters and laboratory data are within normal limits unless the bowel wall becomes devitalized. With complete obstruction, severe abdominal distention, pain, and cardiovascular collapse occur. Rectal examination is most helpful, but the enterolith is seldom palpated. I TREATMENT Surgical management is necessary; unfortunately, the enterolith lodges in areas that are inaccessible. Therefore, the surgeon must make judicious use of hydropulsion or manual extraction. A technique of retrograde flushing of obstructions in the transverse colon by introducing a tube into the SC has been described.79 However, the surgeon must be careful because high pressures can cause a rupture of compromised or normal bowel. Intraluminal retrieval, with the surgeon's hand introduced through an enterotomy site in the RDC near the diaphragmatic flexure, is useful when enteroliths lodge in the transverse colon or RDC. Transmural manipulation and massage to "milk" the enterolith into the R D C or aborally into a more accessible portion of the SC is useful. Rupture of the bowel can occur with manipulation, especially in the SC. The prognosis is reported to be fair. A 47% success rate was reported in one with the best results achieved when the enterolith was removed before the bowel became devitalized. After removal of the enterolith, especially one in the shape of a tetrahedron, the entire large bowel should be palpated for the presence of additional enteroliths. Sand Impaction of the Large Colon ETIOLOGY I I Sand impaction of the large colon occurs most commonly at the pelvic flexure and terminal RDC. 393 Horses stabled in a sandy environment and fed from the ground appear at risk. Clinicians often associate this form of colic with specific geographic areas. Ingested sand may cause foreign body enteritis or sediment over time to. cause impaction. Offending sand is generally fine beach sand or clay, but gravel can occasionally be found. CLINICAL SIGNS - In a recent study, sand colic was diagnosed in 48 horses, none of which were younger than 1 year of age." Clinical signs range from mild to severe pain and normal to deteriorating cardiovascular status. Rectal examination reveals cecal and large colon gas distention. An impaction could be felt in only seven of 48 horses." Sand can be present in feces without causing colic. In many horses, surgical exploration is undertaken because of abdominal pain, large colon distention, and deteriorating cardiovascular signs, without an accurate preoperative diagnosis. Abdominoparacentesis should be performed carefully, because the heavily laden sandimpacted colon can be lacerated inadvertently. In three of six horses with inadvertent enterocentesis, sand was found in the fluid, which was diagnostic for the disease.* Abdominoparacentesis should not be performed in horses that obviously require surgical intervention or in horses in which the procedure may be of low diagnostic value. Auscultation of horses with sand impaction may reveal sounds compatible with sand b o r b ~ r y g m i . ~ ' . ~ ~ Horses with true sand impaction of the large colon rarely respond to medical management. TREATMENT Sand impaction is often a surgical diagnosis and may be difficult to treat. Coordinated efforts are needed between the surgeon and the assistant surgeon, and both intraluminal and transmural manipulation are needed. Judicious, copious intraluminal lavage combined with egress tubing in some horses is needed.80 Because sand can settle in more than one viscus, multiple enterotomies may be needed. Twenty-six of 48 horses had multiple . ~ ~ impactions were seen sites of sand i m p a ~ t i o n Single most commonly at the pelvic flexure (14 horses), but when multiple impactions were present, the RDC was more frequently involved (15 horses). Sand impaction of the pelvic flexure may act as a pendulum, predisposing the horse to volvulus of the colon. Cranial dis~lacement of the pelvic flexure and nonstrangulating and strangulating colonic displacements were seen in 16 of 48 horses with sand i m p a ~ t i o n . ~ ~another .In study, 10 of 40 horses had volvulus or displacement of the colon.* COMPLICATIONS Complications after surgery include recurrence of the disease, peritonitis, diarrhea, and incisional problems. The prognosis is guarded to poor for horses with true sand impaction requiring s~rgery,'~ and in one study, the mortality rate was 30%.83 The long-term survival rate was 60% in a recent clinical study, which indicated a relatively high mortality rate compared with 394 ALIMENTARY SYSTEM other impactions of the large i n t e ~ t i n e Forty-four .~~ of 48 horses with sand impaction were discharged from the hospital, and follow up on 38 horses revealed a relatively low mortality rate (8.3%).80 Clinicians may differ with respect to how they arrive at the diagnosis of sand impaction or to the importance they place on the surgical finding of small amounts of sand when other lesions are present. Minimizing exposure to sand may be important in preventing recurrence. The weekly dosing of the natural fiber laxative psyllium hydrophobic mucilloid is useful in removing small amounts of sand from the large colon. Tympanites of the Large Colon and Cecum CLINICAL SIGNS Primary gas distention of the cecum and large colon occur but are generally short lived and respond to medical management. Occasionally, however, a more severe form of tympanites occurs. Clinical signs vary, depending on the degree of abdominal distention. Rectal examination reveals gas distention of the cecum characterized by taut bands. The bowel may shift and assume a transverse position in the caudal abdomen. The left ventral and dorsal colon segments may rotate 90 degrees. This anatomic abnormality is confusing, leading one to suspect a surgical lesion. Generally, no edema of the bowel wall is felt. Atropine can cause a particularly severe form of tympanites and should be used with ~ a u t i o n . ~Glycopyrrolate, " an antimuscarinic drug used for treatment of horses with increased respiratory secretions or bronchoconstriction, can also cause large intestinal stasis, tympanites, and colic. TREATMENT Medical management should be undertaken. The horse's response to treatment may be diagnostic. If auscultation and rectal palpation confirm cecal distention, cecal trocarization is both therapeutic and diagnostic. If the horse responds to treatment, primary tympanites is the diagnosis; whereas if distention recurs, tympanites may be secondary to another lesion. Cecal trocarization in the right paralumbar fossa is not without risk, and the peritoneal fluid nucleated cell count may rise dramatically (up to 100,00O/pL) after the proced ~ r e . 'Bowel ~ laceration and subsequent peritonitis can occur; therefore, the procedure should be used judiciously and sparingly. Surgical management may be necessary to alleviate colonic distention or may be undertaken because of the confusing nature of the clinical signs. At surgery, the cecum and colon are usually in the normal anatomic position and needle decompression is performed. Surgeons often suspect colonic displacement has occurred but has corrected itself once the horse is rolled into dorsal recumbency. The prognosis is good, but recurrence is possible if an underlying problem exists. Nonstrangulating Colonic Obstruction ETIOLOGY Because of the length of the bowel and the lack of extensive mesenteric attachments, the gas-distended large colon can twist or become malpositioned, displaced, or incarcerated (entrapped). In a clinical study, 32 of 232 horses (14%) undergoing surgery for colic had nonstrangulating displacements of the large colon.85Several forms of large colon displacement are recognized that cause similar clinical signs. In conditions such as impaction and tympanites of the large colon, there can be a 90-degree rotation of the colon without anatomic obstruction. However, 180- to 270-degree rotations of the colon cause anatomic obstruction of the flow of digesta and varying degrees of venous stasis. Some forms of nonstrangulating displacements may progress to strangulating lesions and may simply represent early forms of strangulation obstruction. CLINICAL SIGNS Each form of displacement has specific characteristics, but the history and clinical signs are similar. Horses exhibit signs of displacement for 12 to 24 hours before becoming more acutely painful. Generally, lowgrade signs of abdominal pain occur that are similar to those seen in horses with impactions. Horses generally respond to symptomatic treatment only to become painful-once again within several hours. Heart and respiratory rates are elevated during painful episodes but are usually normal, until late in the course of the condition. The preoperative heart rate was reported in one study to be elevated to a mean of 64 beats per minute in horses with displacement^.^^ Progressive abdominal distention usually causes increased abdominal pain. Occasionally, up to 2 to 3 gallons of gastric fluid are obtained by nasogastric intubation, presumably owing to duodenal compression by the distended large colon. Tension of the duodenocolic ligament has also been incriminated. Gastric reflux may be more of a problem in horses with left dorsal displacement of the lkft colon segments. In most horses, gastric distention is not present. Rectal examination is most helpful in establishing a diagnosis and distinguishing this form of colic from tympanites or impaction. Gaseous~distentionof the large colon and cecum with the associated tight bands is characteristic. Preoperative diagnosis of left dorsal displacement and right displacement of the left colon portions is possible, but there are no pathognomonic findings on rectal palpation. Most important, the clinician should note large colon distention, displacement, and mild edema of the bowel wall and make the correct decision for surgical intervention. The diagnosis is confirmed at surgery. TREATMENT Surgical correction of the anatomic displacement is mandatory. The pelvic flexure should be located first, and the remainder of the colon can then be identified. If the pelvic flexure cannot be found, the cecocolic L A R G E INTESTINE ligament is found and the surgeon follows the ventral colon to the pelvic flexure. The LVC and LDC are exteriorized, rotated, and placed back into the abdomen in the correct anatomic position. Generally, needle decompression of gas-distended cecum and large colon is adequate, but occasionally, an enterotomy is needed to relieve the accumulation of digesta. The enterotomy should be performed in the terminal LVC. Enterotomy is generally not necessary, because once the displacement is corrected, horses quickly regain normal intestinal motility. The prognosis of horses with nonstrangulating displacements is good, and the condition is considered one of the most favorable forms of all surgical problems. The long-term survival rate was 71% in horses with displacement^.^ The survival rate compares most favorably with that of horses requiring small . ~ a study of 140 intestinal resection and a n a s t o m o ~ i s In horses, the overall survival rate of small intestinal resection and anastomosis was 22%, although only 11% of horses survived more than 3 years after resection and ana~tomosis.~ Nonsurgical correction of left dorsal displacement has been described (see the section on Left Dorsal D i s p l a ~ e m e n t ) .Right ~ ~ , ~ ~dorsal and left dorsal displacement can recur, requiring additional surgery and possible colopexy. NONSTRANGULATING VOLVULUSOF THE LARGE COLON. Rotation of the colon between 90 to 270 degrees causes physical obstruction of the colon, interrupts digesta transit, and causes gas distention and colic. Nonstrangulating volvulus is one recognized form of displacement of the large colon and is classified as a simple obstruction (Fig. 36-13). Edema and hyperemia of the bowel wall is common, and therefore, partial venous obstruction occurs. Rotation of the colonic axis usually occurs in a clockwise direction when viewed from a caudal position, as if the examiner were performing a rectal examination. This rotation is also seen in horses with strangulating volvulus of the large colon. Obstruction occurs at the sternal and diaphragmatic flexures, although a report describes involvement of the .~ decompression is neccecum in some h ~ r s e s Needle essary in the ventral and dorsal colon segments and the cecum. The surgeon must identify the lesion, exteriorize the colon, and reposition it correctly. RIGHT DISPLACEMENT OF THE L E F ~COLON. Frequently called right dorsal displacement, this form of nonstrangulating obstruction may be related to a motility dysfunction of the RDC. Commonly, the RDC is digesta filled, predisposing the horse to gas distention and rotation. Rectal examination reveals a tight band associated with the LVC, traversing across the caudal abdomen and coursing lateral to the cecum. In some horses, the cecum is pushed forward and is not palpable. Usually, the ventral cecal band is tight due to cecal gas distention. Right displacement of the left colon portions can be a chronic condition and can initially be present without colic signs. Without concurrent volvulus or severe gas and digesta accumulation, a malposition of the left colon segments in a U-shaped fashion to the right impedes but does not stop the transit of digesta (Fig. 36-13A). With further rotation or with filling of the RDC, a simple obstruction occurs. Signs of colic 395 FIGURE 36-13. Nonstrangulating displacement of the large colon as viewed from the ventral aspect at exploratory surgery. (A), 180-degree volvulus of the large colon, located at the sternal and diaphragmatic flexures. (B), Right displacement of the left colon segments. Without further rotation or volvulus, this form of displacement may cause chronic, intermittent wlic before complete luminal occlusion occurs. (Redrawn from Hackett RP: Non-strangulating colonic displacement in horses. J Am Vet Med Assoc 182:235, 1983.) and progressive abdominal distention become obvious. Medical management including withholding feed, analgesic administration, and occasional trocarization of the gas-distended colon can help resolve the clinical signs. However, when the horse is returned to full feed, colic recurs. This form of displacement can cause chronic intermittent colic. The more typical form involves progressive large colon distention, secondary abdominal distention, and an increase in abdominal pain, which requires surgical intervention. Various forms of the displacement 396 ALIMENTARY SYSTEM are described to include flexion and torsion of the colon portions.89 In the most common form, the pelvic flexure rotates cranially to the right and finally sits tranversely in the abdomen, thus completing a counterclockwise rotation (when viewed from the ventral aspect at the time of surgery). Clockwise rotation can occur but is less common. LEFTDORSAL DISPLACEMENT OF THE LARGECOLON. Left dorsal displacement of the large colon, frequently called renosplenic (nephrosplenic) ligament entrapment, is a well-recognized form of nonstrangulating d i s p l a ~ e m e n t .87'~ ~ , 90- 91 The etiology is unknown, but one possibility includes concomitant splenic contraction and gas distention of the LVC and LDC. With dorsal displacement of the colon and subsequent refilling .of ~ of etiology, the spleen, the colon is t r a ~ p e d . 'Regardless the lesion involves an entrapment of the LDC and LVC over the dense, fibrous suspensory ligament between the kidney and spleen. Occasionally, concurrent impaction or volvulus of the colon is present (Fig. 36-14). This form of displacement can be seen in younger horses, whereas other forms of displacement are unusual in this age category. FIGURE 36-14. Left dorsal displacement of the colon, over the renosplenic ligament. (A), Surgeon's view of left dorsal displacement. Occasionally, the digesta in the entrapped portion of the colon is firm, requiring enterotomy, or a volvulus of the colon occurs in the entrapped portion. (Redrawn from Hackett RP: Non-strangulating colonic displacement in horses. J Am Vet Med Assoc 182:235, 1983.) (B), With concomitant gas distention of the left colon segments and a medial shift of the spleen, the colon segments become incarcerated dorsal to the renosplenic ligament. LDC, left dorsal colon; LVC, left ventral colon. (Redrawn from McIlwraith CW: Equine digestive system. In Jennings PB (Ed): The Practice of Large Animal Surgery. Philadelphia, W. B. Saunders Company, 1984, p 638.) In left dorsal displacement of the large colon, clinical signs may vary from mild to severe, presumably relating to the amount of tension on the renosplenic ligament or the amount of involved intestine. The level of colic is usually compatible with other forms of nonstrangulating displacement, but occasionally, horses are violent. The classic signs found on rectal examination that are associated with this form of displacement include (1) gas-filled LVC and LDC coursing craniodorsally over the renosplenic ligament; (2) a ventral and medial shift in splenic position; and (3) a tight, gasdistended cecum. However, there are no pathognomonic signs. With simple tympanites of the large colon, the left ventral and dorsal colon segments can assume dorsal position in the abdomen, mimicking left dor displacement of the large colon. Other large col displacements can mimic left dorsal displacement of 1 large colon as well. The lesion may be suspected more frequently than it actually occurs. Other more subtle clinical findings may lead one to suspect left dorsal displacement. In this form of displacement, horses can have a rather surprising amount of gastric distention, requiring nasogastric intubation. Relative to the amount of pain and distention, the heart rate is lower than expected. The PCV may be normal or slightly low, despite mild or moderate clinical dehydration. Splanchnic or splenic sequestration of red blood cell volume may explain this clinical finding. Abdominocentesis may yield bloody fluid from splenic puncture because of the ventral positioning of the spleen. Occasionally, horses with left dorsal displacement of the large colon suffer from intermittent pain, and a more chronic form of colic results. Two forms of correction have been advocated. Surgical exploration, decompression, and repositioning of the colon provide the most direct means of diagnosis and anatomic repositioning, without risking other complications reported with nonsurgical management.% At surgery, the LVC and LDC are found dorsal to and entrapped by the renosplenic ligament. The lesion is unequivocal when found and is easily corrected. To free the colon, the surgeon needs to carefully push the spleen medially, while with both hands and arms, gently rocking the colon free, bringing the structure first dorsally around the spleen, and then laterally and ventrally. This maneuver is more easily accomplished if the surgeon is standing on the horse's right side during ventral midline exploratory. Both hands are cupped around the colon, after the arms are used to push the spleen to the right (toward the surgeon). A method of nonsurgical correction of left dorsal displacement of the large colon has been d e ~ c r i b e d . ~ . ' ~ After inducing general anesthesia, the horse is positioned in right lateral recumbency. While providing a gentle "rocking" motion (shaking) of the abdomen, the horse's limbs are gradually hoisted to a vertical position and then the horse is rolled into left lateral recumbency. After completion of the rolling procedure, the spleen is once again against the lateral body wall, now lateral to the LVC and LDC. Occasionally, manipulation by rectal palpation is needed to free the entrapped colon. In a recent clinical study, 5 of 27 horses required rectal manipulation combined with rolling.% Maintenance of ~ I 1 R L A R G E INTESTINE the dorsal recumbent position for a few minutes may facilitate the correction of the problem. Published complications of the procedure include recurrence, inability to free the colon by the technique, cecal torsion, or large colon torsion. Recurrence of left dorsal displacement of the large colon and other displacements or volvulus of-the large colon have prompted surgeons to consider stabilizing the colon by c o l ~ p e x y . ~92' ,In two of nine horses, recurrence of left dorsal displacement of the large colon was found, requiring a second celiotomy. Other reported complications are adhesion formation after surgery in one horse and subsequent large colon necrosis in another. A technique to obliterate the renosplenic space was reported to be successful in preventing left dorsal displacement of the large colon in eight horse^.^',^^ Currently, surgical correction and colopexy should be undertaken if the condition recurs. Colopexy, however, results in a permanent adhesion of the large colon and may have long-term complications (see the section on Colopexy). CRANIALDISPLACEMENT OF THE PELVICFLEXURE. At exploratory surgery, the pelvic flexure may be located in the cranial abdomen. A cranial position of the pelvic flexure may not be a true lesion and may occur secondary to rolling or placing the horse in dorsal recumbency. If accompanied by a lesion of another intestinal segment, without large colon gas distention or impaction, the cranial displacement of the pelvic flexure may be incidental. However, in some horses, cranial displacement of the pelvic flexure with concomitant impaction or gas distention of the large colon, colic, and no other lesions found at exploratory surgery appears to be a true lesion. In one study, eight horses had the c o n d i t i ~ n Gas . ~ ~ distention and associated impaction of various colonic segments was common. The prognosis is considered good. OTHERTYPESOF DISPLACEMENT. The colon can rotate or displace into various positions, some of which are described, while others seem atypical. Tympanites can be associated with rotation of the colon. However, if large colon distention and an odd form of displacement are found at surgery, a thorough exploration should be performed to rule out other forms of obstruction. Intraluminal obstruction of the terminal RDC or transverse FIGURE 36-15. The cecum and large colon of a horse with volvulus of the large colon at the level of the cecocolic ligament. Volvulus at this level is the most common form of the disease. Note that clockwise rotation of the bowel (as viewed from the caudal aspect of the horse) is most common. Once the horse is in dorsal recumbency, the surgeon untwists the colon in a clockwise direction as well. RDC, right dorsal colon; RVC, right ventral colon. 397 colon can cause gas distention and rotation of the colon. Unless these areas are carefully palpated, lesions can be easily missed. Adhesions, Abscc and Neoplasia Nonstrangulating, simple obstruction of the large colon can occur with adhesions, abscessation, or neoplastic diseases. Mural abscessation and neoplasia are extremely rare. Omental adhesions to various portions of the large colon can occur after surgical incision, traumatic perforation, or ulceration. Adhesions of the large colon to the body wall can cause partial obstruction and displacement. At surgery, adhesions should be carefully disrupted to avoid penetration of the bowel lumen. If chronic scarring is present, intestinal resection or bypass may be needed. For more information on this subject please review Chapter 33. Strangulation Obstruction of the Large Colon VOLVULUS OF THE LARGE COLON (VLC) PATHOGENESIS. Volvulus of the large colon (sometimes including the cecum) causes one of the most acute, devastating forms of colic. By far, the most common form of the disease causes acute cardiovascular deterioration, severe abdominal pain, gross abdominal distention, and death within 4 to 24 hours unless the horse is operated on in a timely fashion. Initially, the pathogenesis involves venous occlusion and hemorrhagic strangulation obstruction, but later, progressive arterial occlusion causes ischemic changes. The colon rotates in clockwise fashion as viewed from behind, looking forward along the axis formed by the RVC and RDC (Fig. 36-15). The volvulus is generally 360 degrees, but surgeons have reported rotations of up to 720 degrees. The classic form of the disease involves a twist at the level of the cecocolic ligament, but the axis of rotation can be at the cecal base. Occasionally, VLC occurs at the sternal and diaphragmatic flexures, but this condition is unusual. Broodmares, late in gestation or after parturition, appear at risk of developing VLC. Other forms of nonstrangulating displacements may also occur in brood- 398 ALIMENTARY SYSTEM mares. In a recent study of 122 horses with VLC, 73 horses were females and 42% had foaled or were pregnant.94The disease is not restricted to broodmares, but changes in digestion or visceral positioning during pregnancy may predispose mares to the disease. The enlarging uterus may induce a shift in the position of the large colon or cause partial obstruction of the RDC. Digesta, gas distention, and secondary rotation of the colon lead to strangulation. A change in intestinal motility may occur during pregnancy. Large colon motility dysfunction occurs in women during pregnancy, but the condition is not known to exist in horses. The history may indicate a previous management change such as change in housing or in the type o r quality of feedstuffs provided. CLINICAL FINDINGS.The clinical signs generally reflect the duration of the volvulus. Severe, unrelenting pain is the most common clinical sign, and based on this factor alone, a decision for surgical intervention is often made. Horses sweat profusely and often display skin wounds. Abdominal distention is common and often severe, causing respiratory compromise. The heart rate is elevated between 60 and 80 beats per minute but is lower than expected for the degree of abdominal pain present. Horses with VLC and high heart rates (greater than 65 to 70 beats per minute) accompanied by severe dehydration (PCV >60%) have a very poor prognosis, because these parameters reflect severe changes in cardiovascular status. In a recent study, there were significant differences between survivors and nonsurvivors (values were lower in survivors) in heart rate, respiratory rate, capillary refill time, and PCV.94 In this study, the mean duration of clinical signs was 19 hours (range, 2 to 156 hours). Occasionally, horses may have a more chronic clinical course. Early nonstrangulating lesions may progress to strangulation obstruction. Rectal examination usually reveals large colon distention and tight bands coursing transversely in the caudal abdomen. An important finding is edema of the colonic wall, which reflects severe venous congestion. Occasionally, rectal examination reveals an empty caudal abdominal quadrant. The empty abdomen leads to a springy or bouncy feeling of the rectum, resembling the finding of pneumoperitoneum. In these horses, pain is severe and the colon has shifted forward, causing severe compression of the cranial abdominal viscera. In rare instances, rectal examination reveals edema of the colon without colonic gas distention. Severe unrelenting pain is the most consistent sign leading to surgical intervention, regardless of the findings on rectal examination. Examination before surgery may be pre-empted by unrelenting abdominal pain. Laboratory data generally reflect dehydration, with protein loss into the bowel wall and lumen. Mild metabolic acidosis may become severe in advanced disease. Peritoneal fluid can range from normal to serosanguinous in color. Serosanguinous fluid is common and generally is considered a poor prognostic sign. Mean protein levels and nucleated cell counts are usually slightly elevated, but generally, the clinical course is too short to have consistent elevations in these parameters. TREATMENT. Early surgical intervention is man- datory for a successful outcome. Even if surgery is undertaken as early as 3 to 4 hours after the onset of signs, there is no guarantee of a successful result. Aggressive intravenous fluid therapy is needed before surgery, if possible, to restore blood volume. Reperfusion injury may cause significant bowel damage after surgical correction, and some consideration should be given to the administration of free radical scavengers. A practical choice would be dimethyl sulfoxide (DMSO) (1 gmlkg IV), but recent evidence suggests it is not effective in preventing injury from either hemorrhagic .~~ or ischemic strangulation o b s t r ~ c t i o n Broad-spectrum intravenous antibiotics, flunixin meglumine, and corticosteroids are beneficial and should be given before surgery. In horses with VLC, induction and early maintenance of general anesthesia are critical and are complicated by the extreme large colon distention and poor metabolic state of the patient. Abdominal distention prevents adequate ventilation and predisposes the horse to ventilation-perfusion mismatches. Blood gas values typically show hypercapnia and inadequate oxygenation. Rapid release of endotoxin and stagnated venous blood after untwisting the colon may cause a hypotensive crisis, leading to fatal cardiac arrhythmias. Hypotension is common, and maintenance of anesthesia can be difficult. Early decompression of the bowel generally helps in improving ventilation, but oxygenation and peripheral perfusion still may be inadequate. Judicious use of preoperative cecal trocarization may help early in the anesthetic management. Efficient and timely surgical intervention, minimizing surgery time, and aggressive management of hypotension maximize survival after surgery. Large ventral midline incisions (up to 40 to 50 cm) are beneficial and allow easier manipulation of the distended colon. Early gaseous decompression and untwisting of the colon should be performed before manipulation. The surgeon needs to be gentle in handling the colon, because rupture, particularly of the RDC, occurs frequently. As much of the colon as possible should be exteriorized and held by an assistant. The surgeon then untwists the colon 360 degrees in a clockwise direction as viewed from the ventral midline approach with the horse in dorsal recumbency. A thick, edematous colonic wall; hemorrhagic, congested intercolonic mesentery; and various shades of serosal discoloration (from dark purple to greenish gray) are seen. After untwisting the colon, there is generally some improvement in serosal color, unless complete ischemia or end-stage hemorrhagic strangulation obstruction exists. Generally, a period of 10 to 15 minutes should be given to assess bowel viability. Absence of a pulse in colonic vessels, failure of the colon to return to its normal serosal color, necrotic odor, and black mucosal color are grave signs, and horses with these signs should be euthanized. Surface oximetry, if available, may help in predicting possibility of survival in horses with colonic strangulation obstruction.% Although clinical evaluation of horses with experimental colonic strangulation obstruction would have led to a prediction of poor survival, a return of serosal surface oxygen tension of greater than 50% of baseline correctly predicted survival in a LARGE INTESTINE I j ~I ~ 1 high percentage of horses. Recently, microscopic eval"ation of frozen sections of colonic wall have been useful in determining colonic viability with the aid of clinical assessment of p e r f ~ s i o n . ~ ~ Horses with loss of glandular epithelium are unlikely to survive. Resection of the involved colon remains a possibility, particularly if the volvulus occurs at the diaphragmatic flexure. However, successful resection in horses with true VLC at the cecocolic ligament or at the base of the cecum is difficult because the surgeon usually cannot remove all of the necrotic colon. A resection of 95% of the colon, as reported, may not be possible,98 because in clinical cases, a minimum of 25 to 30 cm of R D C and RVC are left intact. Although close to 95% of the length of the large colon may be removed in normal horses, removal at this level may leave 15 to 25% of the absorptive surface area severely affected by mucosal damage. Substantial damage to the RDC and associated endotoxemia reduce the survival rate in such horses even with the use of resection. Because of the severity of the lesion, up to 50% of the horses operated on for VLC may be euthanized at the time of surgery. Decompression, untwisting, and repositioning of the colon are required. If the colon is filled with digesta, making manipulation difficult, enterotomy and evacuation may be needed. Evacuation of the potentially dangerous toxins that may be absorbed after surgery may be desired, but the procedure is not mandatory. The R D C is usually large, and evacuation of this segment is difficult. A colopexy should be considered if VLC recurs. Aggressive management with intravenous fluids, antimicrobial agents, and anti-inflammatory agents is needed after surgery. Because of the high numbers of anaerobic organisms, metronidazole (15 mglkg, PO, QID) may help in horses with peritonitis or contamination from enterotomy sites. Endotoxin absorption from damaged mucosa can complicate recovery. Immunotherapy with J-5 antisera, producing passive immunity with antibodies directed against a core polysaccharide of gram-negative bacteria, has shown promising early results.99.loo Plasma administration to supplement protein loss from compromised bowel may help. Early after surgery, hemorrhagic diarrhea, fever, and leukopenia are common in horses with moderate to severe colonic compromise. Continued fecal passage is a good prognostic sign, but horses that develop ileus, large colon distention, and abdominal pain after surgery have a very poor prognosis. Reoperation, decompression, and large colon resection or euthanasia may be necessary. PROGNOSIS. The reported survival rate of horses with VLC ranges from 12% to 34.7%.36,94However, because differences exist with lesion definition and severity grading, survival rates may differ. Actual survival rates for horses with VLC of 360 degrees are likely in the 10% to 20% range. INTUSSUSCEPTION OF THE LARGE COLON Intussusception of the colon is rare but has been r e p ~ r t e d . l ~ ' -The ' ~ ~ short, strong intercolonic mesentery 399 should inhibit the development of intussusception, but abnormal motility, impaction, and parasite lesions may predispose the horse to the disease. Intussusception has been reported at the pelvic flexure, the LVC, and the LDC. These segments may be predisposed to the disease. Intussusception is less likely in the right colon segments, because the RDC and the RVC have dorsal mesenteric attachments and the cecocolic ligament attaches to the RVC.' Intussusception may cause initial simple obstruction, but venous obstruction, mural swelling, and arterial occlusion lead to strangulation obstruction. Clinical signs and laboratory parameters reflect the duration of the obstruction. Surgical intervention is mandatory. Manual reduction was successful in one horse,lo2 but usually resection and anastomosis are necessary. Both side-to-side o r endto-end anastomoses are successful, but end-to-end procedures are difficult because of the disparity in size of the colonic segments. The prognosis is guarded to good, depending on the timing of surgery, the degree of ischemia, and the surgical technique performed. LARGE COLON INFARCTION Thromboembolism of the colonic vessels is rare, but can occur secondary to migration of S. vulgaris larvae. The arterial supply of the colon arises from two separate branches, forms a loop at the pelvic flexure, and has extensive communications between the vessels. The vascular supply of the colon is relatively protected compared with the cecum. With extensive thromboembolic disease, infarction can occur, causing clinical signs associated with strangulation obstruction. Horses usually suffer from acute pain but can show depression with chronic pain. Resection and anastomosis are successful if the ischemic segment is short. Generally, the LDC and the LVC are involved, and end-to-end o r side-to-side anastomoses can be performed after resection. In one horse, end-toend colocolostomy was successful after infarction of the LDC.'" Continued thromboembolic disease after surgery limits the prognosis. Large Colon Resection Partial resection of the large colon can be performed successfully using both hand-sewn and autosuture techniq~es.'~.'" Much debate remains, however, regarding what is called 95%, or near-complete, resection of the large c o l ~ n . ' ~ ~Lesions -'~ aboral to the cecocolic ligament can be exteriorized from a ventral midline incision, and resection is possible. In a recent study, 36 of 122 horses had lesions amenable to resection from an anatomic ~ t a n d p o i n t Although .~~ the most common site for VLC is the level of the cecocolic ligament, the damage extends into the terminal R D C and the oral portion of the RVC. Resection, even at the cecocolic ligament, leaves necrotic bowel in situ, and endotoxin absorption and death are likely. Because the wall is thicker and compromised in horses with VLC, surgical techniques used in horses with experimental resection may fail. 400 ALIMENTARY SYSTEM Little doubt exists that extensive large colon resection can be performed successfully in normal horses. Resection at the level of the cecocolic ligament may remove all but 5% to 10% of the length of the large colon but may leave 15% to 20% of the absorptive surface area. Five of 10 normal horses survived 18 months after resection at the cecocolic ligament.lo6 After attaching stay sutures, a side-to-side anastomosis is performed between the RDC and the RVC at the level of the cecocolic ligament, using the GIA autosuture instrument. After completing the anastomosis and ligating the dorsal and ventral colic arteries, the large colon is transected using the TA-90 stapling instrument (U.S. Surgical, Norwalk, CT) across both the RDC and the RLC. This creates a side-to-side anastomosis and two blind colonic ends. In three horses, death was due to leakage from the staple lines. Modification in application of the TA-90 autosuture device may avert this and other complications such as adhesions to staple lines. Hand-sewn inverting suture lines offer a distinct advantage over the use of stapling equipment. Because failure occurs with use of stapling equipment in normal horses, it is likely to occur in horses with thick, edematous large colon after volvulus. Additional information on surgical techniques is found in Chapter 33. In horses with a large colon resection at the cecocolic ligament, digestion of dietary crude protein, cellulose, and phosphorus is decreased.lo8Fecal water output is increased 55%, and total fecal output is increased 45%. Horses lose weight after surgery but generally are able to regain weight within 6 months. In these horses, there is a shorter transit time of particulate digesta, and a decreased overall retention time because of the overall decrease in intestinal length and capacity.lo7 In horses with less extensive resection (60%), there is a decrease in digestion of crude protein, fiber, nitrogen-free extract, and phosphorus as we11.lW However, horses maintain body weight and develop adaptive digestion ability by 6 months after surgery. Further studies to evaluate digestion in horses with extensive large colon resection indicate that grass hay or alfalfa pellets did not provide adequate digestible energy.llO.lllAlfalfa hay, with a shorter fermentation lag time, is recommended, because transit and fermentation time are reduced in these horses. In summary, horses with a 60% reduction of the length of the colon experience adaptive changes; however, in those with extensive resection (up to 95%), although adaptive changes occur, feeding alfalfa hay is recommended. Because of the increased fecal water output, water consumption after surgery is increased. Prognosis after large colon resection depends largely on the length of resected segment. In horses with less than 50% removed, the survival rate was 81%, but in horses with more than 50% of the colon resected, the survival rate was only 53%.l1° Survival may correlate more closely to the severity of the lesion than to the length of the resected colon. More clinical experience with extensive large colon resection is needed to assess survival after resection in horses in which discolored or damaged tissue is left in situ. In a recent report, hand-sewn techniques resulted in survival of 12 of 18 horses undergoing extensive resectionfi2 Resection was performed at the level of the cecocolic ligament in most horses.l12 Survival decreased as the amount of devitalized tissue left in situ increased.lI2 Large colon resection remains a viable alternative to untwisting, enterotomy, and repositioning, but case selection is important. Hand-sewn techniques should be considered because edematous, thickened colon may not be suitable tissue for the application of currently available stapling equipment. Colopexy Recurrence of nonstrangulating displacement, or VLC, has led to the development of techniques for disease prevention. Techniques involving suturing the dorsal and ventral colon segments together fail to prevent experimentally induced volvulus and induced weight loss, and should not be used.". 113 A technique of suturing the lateral free band of the LVC to the left body wall, approximately 6 cm to the left of midline, is A nonabthe currently recommended te~hnique.l'~-"~ sorbable suture, such as #2 polypropylene or nylon is preferred, because adhesions caused by absorbable material tend to mature and lyse over time. Colopexy of the LVC may cause weight loss initially, but the horse regains the weight without complication^."^ Trials to assess digesta passage after colopexv revealed digesta was retained on day 4, and variatil in the rate of digesta passage within horses decrea after surgery.Il5 Therefore, after colopexy, stabilizat of the large colon may increase transit time initially, out no long-term complications such as impaction of the large colon were encountered. Colopexy appears to be safe but has received only limited clinical evaluation. The effect of colopexy on racing animals is unknown currently, but the technique has been used successfully in brood mare^."^ Special care must be taken not to penetrate the bowel lumen because leakage and peritonitis may develop. The technique should not be used if colon viability is q~estionab1e.l'~ Anecdotal reports of colon rupture near or at the site of the fixation are worrisome. The technique should be reserved for horses with recurrent disease and used only after adequate client education has been made available. Transverse and Small Colon Diseases of the small colon (SC), combined with those of the rectum, cause colic in 2.9% to 17.7% of Obstruction of the SC is caused most frequently by impactions or fecaliths. The diagnosis of small colon disease may be difficult when it is based only on clinical examination. Horses with SC obstruction usually exhibit mild colic and progressive abdominal distention. Failure to pass feces can be an important part of the history, leading the clinician to suspect a lesion of the small or transverse colon. Dehydration is not marked and vital signs are within normal range. Volvulus or vascular accidents involving the small colon have an abrupt onset and more rapid deterioration in vital parameters. I I I I LARGE INTESTINE Atresia Coli TREATMENT Atresia coli, a rare condition in foals, is seen more commonly in Thoroughbreds and develops as a result of an autosomal recessive inheritance. lZ4Vascular accidents during fetal development resulting in disruption of blood supply to the intestine can also produce atresia.lE-ln The lethal white foal syndrome of Paint horses is a different disease. The allele responsible for the all-white color is associated with a deficiency of ganglion cells in the colon myenteric plexus, resulting in thin muscular walls and s t e n o s i ~ . ' ~ ~ Foals with atresia coli often have elevated vital parameters. A digital rectal examination reveals an absence of feces. Contrast radiography is of limited diagnostic value unless the atresia is in the transverse colon or located aborally.lE Exploratory celiotomy reveals atresia of the colonic segment. Surgical correction is possible if it is performed early. Concurrent findings include atresia ani, renal ~~ in the size of hypoplasia, or renal a p 1 a ~ i a . lDisparity aboral and oral bowel diameter requires careful approximation, using end-to-end or end-to-oblique anastomotic techniques. The side-to-side technique is of value but may predispose the horse to blind loop syndrome. Resection of the severely dilated oral portion is recommended to obtain a normal vascularized and functional intestine.lZ5 Complications arising from surgical correction include ileus of the dilated oral portion, peritonitis resulting from leakage of the anastomosis, chronic incontinence, and diverticulitis. NONSURGICAL MANAGEMENT. Medical management is successful in horses with mild impactions. Aggressive oral fluid therapy, sometimes accompanied by intravenous fluid administration, and analgesic treatment are generally successful. Judicious use of enemas in the standing horse have been advocated but are not recommended unless the impaction is near the rectum and adequate patient restraint is provided. Rectal or small colon tearing is a potentially devastating complication. SURGICALMANAGEMENT. If surgical management is required, a combination of massage and a procedure known as a high enema are generally successful. A soft rubber hose attached to a garden hose is gently inserted per rectum by a nonsterile assistant. The surgeon aids in tube passage by transmural manipulation. Warm water is infused to soften the digesta. Distention and irrigation are continued until the material is flushed from the rectum. This procedure is traumatic to the bowel and occasionally predisposes the horse to colonic rupture. In horses with more advanced disease, necrosis of the colon can occur secondary to impaction, which requires resection and anastomosis. The prognosis after surgery is guarded. Recurrence of the impaction, ileus, and adhesion formation are possible sequelae. Fecaliths. Fecaliths, sometimes 15 to 20 cm in diameter and length, are composed of inspissated fibrous fecal material that is believed to form as a result of improper fecal ball formation.l18 Fecaliths may develop because of the diet composition and the resistance to flow of digesta through the intestinal tract. Fecalith obstruction of the small colon causes slow, progressive, intermittent colic. Phytoconglobates and Bezoars. Phytoconglobates are concretions of undigested food fragments and foreign particulate matter formed into balls.'" Bezoars are a combination of magnesium ammonium phosphate with a plant fiber (phytobezoars) or animal hair (trichobezoars). Trichobezoars and phytoconglobates are rare."6. 120 Bezoars have a smooth glistening surface but are light colored, unlike the darkly colored enteroliths. Small colon obstruction with phytoconglobates and bezoars can cause colic similar to impactions or foreign body obstruction. Foreign Body Obstruction. Yearling and weanling horses are prone to ingest foreign materials such as twine, rope, clothing, rubberized fencing materials, and tire threads. Twenty-eight horses with SC obstruction were reported from one farm alone due to the ingestion of nylon tires.74 In 10 horses, ingestion of strips of conveyer belt caused foreign body o b s t r ~ c t i o n .The ~~ pitted, uneven surface of the obstructing mass, which is surrounded by firm concretions of digesta, lodges against the mucosa. The mass can reach 1 m in length and weigh up to 7 kg.7SRupture of the SC can occur easily during surgical manipulation. Horses with foreign body obstruction show no clinical signs when the material passes through the small intestine owing to the higher fluid-to-solid ratio. Horses with foreign body obstruction exhibit acute colic if obstruction is complete. The obstruction can be preceded by signs of intermittent colic I I I I I I i , 401 Impaction of the Small Colon ETIOLOGY Simple obstructions of the SC are usually caused by feed impactions or fecaliths but can also be due to enteroliths, foreign bodies, phytobezoars, trichobezoars, and p h y t o c o n g l ~ b a t e s . ~118,~ -129-133 ~ ~ ~ Small colon impaction is the most common form of simple obstruction. Ponies appear to be predisposed to SC impaction.27Cold weather, limited roughage diets, and lack of water may predispose horses to the development of impactions. A primary motility problem or vascular insult may lead to the accumulation of digesta. CLINICAL SIGNS Horses with impactions of the SC have vague signs of anorexia, dullness, and mild abdominal pain. Horses may exhibit tenesmus if the impaction is near the rectum. In more chronic impactions, a rapid deterioration in condition may indicate necrosis of the affected bowel or the development of gaseous distention of the large colon. The diagnosis may be difficult to arrive at before surgery. Single or multiple loops of SC with firm, nearhard digesta can be felt on rectal examination. Although the clinical signs and history may suggest a small colon obstruction, confirmation on rectal examination often is not possible. 402 ALIMENTARY SYSTEM if the obstruction is incomplete, or if the material periodically returns to the RDC.'18 Surgical removal is mandatory. Colotomy in the RDC is necessary to retrieve the foreign body from the inaccessible area of the large colon. Intraluminal lubricants can be useful in relieving the obstruction but may contaminate peritoneal surfaces. Enteroliths. Enteroliths are mineral concretions composed primarily of magnesium ammonium phosphate salts, which are usually deposited concentrically around a foreign material such as a stone or metal. In a retrospective study, 24 of 30 horses had enteroliths lodged within the small colon, 17 of which were lodged in the oral portion of the organ.n The problem is seen more commonly in horses from 5 to 10 years of age.77. '35 The rate of enterolith formation is unknown, but the age of one large concretion (12 x 9 cm) with a nidus of a deciduous tooth was estimated to be 4 years.'36 Enteroliths are not found in horses younger than 3 years of age. In these horses, colonic obstruction occurs more frequently by foreign materials. Small enteroliths can be passed in the feces, whereas others may cause obstruction for short periods of time and then fall back into the RDC.79 When obstruction becomes complete, abdominal pain is persistent, tympany increases, and the patient's condition deteriorates. The intestinal wall surrounding the enterolith may undergo pressure necrosis, and if the condition is prolonged, the wall may perforate, leading to fatal peritonitis. A surgical approach similar to that described for foreign body removal is required for enterolith removal from the transverse or oral portions of the SC. Retrograde infusion of water through the rectum may loosen enteroliths that cannot be readily manipulated by hand.79 Retained Meconium. Retained meconium in foals is considered a surgical disorder only when medical therapy fails. Foals often exhibit tenesmus, intermittent colic, and large colon tympany shortly after birth. A fecal mass can be palpated craniad to the pelvic rim on digital rectal examination. The initial goals of therapy are to provide analgesia, to protect the foal from self-mutilation, and to relieve obstruction. Administration of warm, soapy water, by gravity flow enema through a well-lubricated soft flexible rubber tube is required. The addition of mineral oil or glycerin but not dioctyl sodium sulfosuccinate may assist passage of large firm meconium impaction^."^ Enemas may have to be repeated. Maintenance oral fluid therapy and exercise may stimulate bowel activity. If surgery is undertaken, aborally directed massage of the meconium in conjunction with an enema should be carried out before a colotomy is performed.123 Vascular Lesions The SC is rarely the site of primary vascular lesions that cause colic. The caudal mesenteric artery, which provides most of the blood supply to the SC, is rarely the site of occlusive verminous arteritis. Vascular lesions seen in the SC are intramural hematomas, mesocolic rupture with segmental infarction, and submucosal edema.120. 121.130.138-140 INTRAMURAL HEMATOMAS Hematomas of the SC are rare.138.139 The etiology is unknown, but rectal or other trauma is p0ssib1e.l~~ Intraluminal hematomas not attached to the mucosa can easily be manipulated in the rectum and withdrawn without entering the bowel. Submucosal hematomas require resection and anastomosis. MESOCOLIC RUPTURE Rupture of the mesocolon with subsequent ischemic necrosis of the SC is a rare complication of parturition in the mare.116."'. 120. 140, 142 The parturient mare is predisposed to type I11 or IV rectal prolapse, resulting from pelvic ligament laxity, increased abdominal pressure, forceful expulsive efforts, and uterine size.129Excessive tension can cause loss of vascular integrity of the mesocolon. Eventration of the small intestine or small colon can occur if the bladder, uterus, vagina, or rectum prolapses or ruptures.'43 Mesenteric tears result in segmental ischemic necrosis of the colon and later rupture. Severe injuries of the mesocolon and the SC may result in primary rupture and fatal peritonitis as well.140 The time from parturition to onset of abdominal pain (0 to 24 hours) is variable, and colic may be confused with the mild pain associated with uterine contraction.'" Mares fail to pass feces and develop impaction in the SC. Rectal palpation may not be diagnostic. Abdominocentesis usually reveals a marked increase in nucleated cell count and rote in levels. but abdominal hemorrhage may be the' primary finding. Exploratory celiotomy is recommended. Resection of de~italized~colon and end-to-end anastomosis should be attempted but is often not possible owing t o the location of the lesion. Colostomy may be needed if the lesion is located aborally. Strangulation Obstruction Strangulation obstruction of the SC is rare and can be caused by enlarged ovaries or-testicular teratomas in foals and in mature animals."'. '45. 146. 14' Volvulus, herniation, intussusception, prolapse, and neoplastic disease can cause strangulation obstruction. The initial clinical signs are mild, but the horse's condition deteriorates rapidly unless surgical intervention is undertaken. VOLVULUS, HERNIATION, AND INTUSSUSCEPTION Small colon volvulus is rare and is usually associated with abnormalities and malpositioning of other organs or is due to complications secondary to intra-abdominal Secondary '~ impaction can ocadhesions or a b s c e ~ s e s . ~ cur oral to the affected segment. Resection of the diseased segment may be necessary. Internal or external herniation of the S C can cause strangulation obstruction. The SC can become strangulated in umbilical or inguinal hernias and tears in the 1 L A R G E INTESTINE FIGURE 36-16. Small colon intussusception in a Standardbred broodmare. Notice the dark discolored small colon orad to the intussusception (entering layer). (From Ross MW, Stephens PR, Reimer JM: in a broodmare: J Am Vet Med Assoc Small colon intus~usce~tion 192:372, 1988.) broad ligament, omentum, uterus, and vagina.l19. 124 Incarcerations of the SC can be diagnosed by rectal examination but may be difficult to distinguish from small intestinal lesions. Intussusception of the SC, a lesion similar to type IV rectal prolapse, can cause strangulation obstruction. Rectal examination may reveal the intussusceptum. Exploratory celiotomy, resection, and anastomosis of the small colon was successful in one horse (Fig. 36-16).148 403 motic breakdown and leakage as compared with other intestinal segments. 15Z-155 The passage of solid fecal balls through a relatively narrow lumen; increased bacterial concentrations, particularly anaerobic organisms; strong muscular activity; and increased tissue collagenase activity may inhibit healing.153.'56. Is7 Portions of the SC are difficult to exteriorize, and the risk of peritoneal contamination is high. The preferred technique involves a two-layer handsewn anastomosis. A simple interrupted suture pattern that excludes mucosa is oversewn with a continuous Lembert suture using 0-polydioxanone or other absorbable suture material (Fig. 36-17). This method produces significantly larger lumen diameters, better anastomotic healing, and minimal intra-abdominal adhesion formation compared with end-to-end triangulated rows of stainless steel staples.Is8 Extensive mesocolic adhesions occur with stapled anastomoses. Complications that occur with single- and double-layer inverting methods of SC anastomosis included anastomotic leakage and stenosis, respecti~ely.'~~, la Removal of digesta from the large colon may help minimize stress on the anastomosis immediately after surgery. '"7 Each surgical condition of the large intestine requires specific monitoring and aftercare. Care after large NEOPIASIA Polyps, leiomyomas, and lipomas can occur in the SC. Polyps can be surgically removed without recurrence if they are pedunculated. Lipomas can cause strangulation obstruction of the SC in aged horses. Because of a large amount of fat, the mesocolon may be predisposed to lipoma f0rmati0n.l~~ Surgical Procedures COLOTOMY Enterotomy of the SC should be performed through the antimesenteric band, resulting in a quicker completion of the colotomy; easier, more accurate apposition; and less hemorrhage and inflammation than in those performed adjacent to the band.lS0,151 Bursting wall tensions of antimesenteric band colotomies are significantly greater than colotomies of the sacculated portion.lS1 The colotomy location is more important than the surgical technique used. Closure of the mucosa as a separate layer facilitates seromuscular layer closure but does not affect the postoperative healing response or lumen diameter in normal horses.'50 RESECTION AND ANASTOMOSIS Strangulation obstruction of the SC requires resettion and anastomosis. The SC may be prone to anasto- FIGURE 36-17. Small colon anastomosis using a 2-layer technique with 0-suture material. (A), The first layer is a nonmucosa penetrating simple interrupted pattern. (B), The second layer consists of a continuous Cushing suture pattern interrupted at 180 degrees to prevent a pursestring effect. 404 ALIMENTARY SYSTEM colon resection and anastomosis is different than care after enterolith removal, for example. General considerations include antibiotic administration, oral fluid therapy, and dietary and management changes. Antimicrobials Many of the surgical procedures performed in the large intestine require opening the bowel and performing clean-contaminated surgery. Peritoneal soiling, especially with particulate digesta, should be limited. Copious, continuous lavage and use of appropriate serosal covering with laparotomy sponges can limit contamination, even when the bowel cannot be completely exteriorized. The concentration of bacteria, particularly anaerobic species, increases in aboral direction, and contamination of the surgical field with pathogenic bacteria may occur. Therefore, broad-spectrum intravenous antibiotics such as gentamicin (2.2 mglkg, IV, QID) and potassium penicillin (22,000-44,000 IUIkg, IV, QID) are usually sufficient and should be given before and continued 3 to 5 days after surgery. Metronidazole (15 mglkg, PO, QID) may be useful if anaerobic infection is suspected but is not given routinely. Contamination during enterotomy or resection and anastomosis may theoretically contribute to an increased wound infection rate, but this problem has not been observed clinically. Any clean-contaminated procedure, of course, may contribute to wound infection or other complications such as hernia formation. Management Changes Management changes may help prevent recurrence of diseases after surgery. If sand impaction occurs, a change in housing arrangements and feeding programs may help prevent recurrence. Avoiding abrupt feeding changes may decrease the potential for motility changes, tympany, and subsequent displacements or volvulus of the colon. Impactions or other simple obstructions of the large intestine occur in horses after shipping, a change in training program, or are associated with other unrelated gastrointestinal or musculoskeletal problems. Horses resting for orthopedic problems may be prone to development of large intestinal diseases. Careful attention should be paid to vague or subtle signs of gastrointestinal disease in these horses. Avoiding abrupt dietary changes in broodmares and providing fresh clean water to all horses, particularly during the winter months, are important considerations. Feeding horses after large intestinal surgery should be carefully considered. Motility dysfunction may cause diseases of the cecum, the ventral colon, or the RDC. Normal motility may not return for several days after surgery. Therefore, the surgeon cannot expect normal motility to return immediately, particularly if an enterotomy and evacuation of accumulated digesta were performed. Although this particular surgery removes accumulated feedstuffs, it certainly does nothing to correct the primary problem. Feeding, therefore, should be staged, and the horse should be slowly reintroduced to its normal diet. Feed is withheld for a minimum of 24 hours. If gastric distention does not occur, oral fluid intake can begin approximately 12 hours after surgery. Laxative diets may be considered, but a slow reintroduction of the horse's regular diet is preferred. Pelleted feeds may increase fecal water content and decrease intestinal transit time, but some horses do not readily consume the diet. Pharmacologic Stimulation Occasionally, motility dysfunctions persist and reimpaction may occur, particularly after enterotomy for impaction of the ventral or small colon. Medical management is therefore required for these conditions. The use of neostigmine (0.0125 to 0.025 mglkg, SC, IV or IM) to stimulate motility of the large intestine may improve motility after surgery, but if an enterotomy or resection and anastomosis have been performed, the surgeon should proceed with caution. Neostigmine increases progressive motility of several segments of the large intestine, but strong contractions might be detrimental to healing of the intestine. Immediate general complications after surgery include dehydration, endotoxemia, peritonitis, ileus, motility dysfunctions, and death. Complications specifically associated with the large intestine include recurrence of the initial problem or inherent complications associated with resection, anastomosis, or colotomy incisions. Because problems of the large intestine can be mild at first, a prolonged clinical course before surgery predisposes the horse to the development of enterocolitis, caused by Salmonella sp. ~ndotoxemia,thrombophlebitis, and laminitis may then become apparent. Noninfectious enterocolitis, associated with mucosal damage of the large intestine, is common after nonstrangulating displacement or early strangulation obstruction of the large colon and can persist for 48 to 72 hours. Leukopenia is common, but horses are generally bright and afebrile, unlike horses with infectious enterocolitis. Fever on day 1 or 2 after surgery in horses with left dorsal displacement of the large colon occurs, but no firm evidence has been given to explain this response. Recurrence of nonstrangulating displacement and strangulating VLC has led to development of colopexy and resection techniques. Adhesions, although certainly possible, are generally not as severe in large intestinal surgery as they are in small intestinal surgery. Omental adhesions occur on exposed staple or suture lines at anastomotic sites or colotomy incisions. Obstructive disease due to adhesions occurs but to a lesser extent than after small intestinal surgery. LARGE INTESTINE In general, the prognosis for horses with surgical lesions of the large intestine is better than that associated with lesions of the small intestine. Long-term survival rates (21% to 42%) for horses with VLC compare f a v o r a b l y with those after small intestinal surgery (11%). Survival in horses with nonstrangulating lesions of the large intestine may approach 80% to 90%, depending on the initial condition. The long-term survival rate in horses with large intestinal disorders (56.7%) is significantly higher than for horses with small intestinal disorders (33.8%).29In horses with large bowel diseases requiring surgery, if inoperable cases are excluded, a survival rate of 73.3% is seen.28Horses with nonstrangulating displacements of the colon are found to have an overall survival rate of 71%.85 Survival rates are sufficiently high to attempt surgical intervention and correction of the lesion. 1. Schummer A, Nickel R, Sack WO: The Viscera of the Domestic Animals. New York, Springer-Verlag, 1979, p 188. 2. Getty R: Sisson and Grossman's The Anatomy of the Domestic Animals. Philadelphia, W. B. Saunders Company, 1975, p 483. 3. Sack WO, Habel RE: Rooney's Guide to the Dissection of the Horse. Ithaca, Veterinary Textbooks, 1977, p 54. 4. Sellers AF, Lowe JE, Drost CJ,et al: Retropulsion-propulsion in equine large colon. Am J Vet Res 43:390, 1982. 5. Beard WL, Lohse CL, Robertson JT:Vascular anatomy of the descending colon of the horse. Vet Surg 18:130, 1989. 6. Archer RM, Lindsay WA, Smith DF, et al: The vascular anatomy of the equine small colon. Am J Vet Res 50:893, 1989. 7. Argenzio RA: Functions of the equine large intestine and their interrelationship in disease. Cornell Vet 65:303, 1975. 8. Argenzio RA, Lowe JE, Pickard DW, et al: Digesta passage and water exchange in equine large intestine. Am J Physiol 226:1035, 1974. 9. Guard C: Gastrointestinal disturbances in the horse with associated metabolic alkalosis. Cornell University Library, 1980. 10. Argenzio RA, Southworth M, Lowe JE, et al: Interrelationship of Na, HCO,, and volatile fatty acid transport by equine large intestine. Am J Physiol233:E469, 1977. 11. Alexander F: Some functions of the large intestine of the horse. Q J Exp Physiol 37:205, 1952. 12. Balch CC: Factors affecting utilization of food by dairy cows: I. The rate of passage of food through the digestive tract. Br J Nutr 4:361, 1950. 13. Ross MW, Cullen KK, Rutkowski JA: Myoelectric activity of the ileum, cecum, and right ventral colon in ponies during interdigestive, nonfeeding, and digestive periods. Am J Vet Res 51:561, 1990. 14. Sellers AF, Lowe JE, Rendano VT, et al: The reservoir function of the equine cecum and ventral large colon: Its relation to chronic nonsurgical obstructive disease with colic. Cornell Vet 72:233, 1982. 15. Dyce KM, Hartman W: An endoscopic study of the caecal base of the horse. Tijdschr Diergenecskd 93:957, 1973. 16. Dyce KM, Hartman W, Aalfo RHG: A cinefluoroscopic study of the caecal base of the horse. Res Vet Sci 20:40, 1976. 17. Ross MW, Donawick WJ, Sellers AF, et al: Normal motility of the cecum and right ventral colon in ponies. Am J Vet Res 47:1756, 1986. 18. Ross MW, Rutkowski JA, CuUen KK: Myoelectric activity of the cecum and right ventral colon in female ponies. Am J Vet Res 50:374, 1989. 19. Sellers AF, Lowe JE, Brondum J: Motor events in equine large colon. Am J Physiol 237:E457, 1979. 20. Ruckebusch Y, Fioramanti J. Colonic myoelectric spiking activity: Major patterns and significance in six different species. Zentralbl Veterinarmed [A] 27:1, 1980. 21. Adams SB, Lamar CH, Masty J: Motility of the distal portion of the jejunum and pelvic flexure in ponies: Effects of six drugs. Am J Vet Res 45:795, 1984. 22. Clark ES, Becht JL, Thompson SA: Simultaneous measurement of motility and arterial blood flow in the equine cecum. Proc Equine Colic Symp 2:81, 1986. 23. Rutkowski JA, Ross MW, Cullen KK: Effects of xylazine andlor butorphanol or neostigmine on myoelectric activity of the cecum and right ventral colon in female ponies. Am J Vet Res 50:1096, 1989. 405 Clark ES, Thompson SA, Becht JL, et al: Effects of xylazine on cecal mechanical activity and cecal blood flow in healthy hones. Am J Vet Res 49:720, 1988. Roger TW,Bardon TH,Ruckebusch Y: Colonic motor responses in the pony: Relevance of colonic stimulation by opiate antagonists. Am J Vet Res 46:31, 1985. Cummings JF, Sellers AF, Lowe JE: Distribution of substance P-like immunoreactivity in the enteric neurons of the large colon of normal and Amitraz-treated ponies: An immunocytochemical study. Equine Vet J 17:23, 1984. Tennant B, Wheat JD, Meagher DM: Observations on the causes and incidence of acute intestinal obstructions in the hone. Proc Am Assoc Equine Pract 18:251, 1972. Pascoe PJ, McDonell WN, Trim CM, et al: Mortality rates and associated factors in equine colic operations-a retrospective study of 341 operations. Can Vet J 24:76, 1983. Ducharme NG, Hackett RP, Ducharme GR, et al: Surgical treatment of colic: Results in 181 horses. Vet Surg 12:206, 1983. Granger DN, Kvietys PR, Mortillaro NA, et al: Effects of luminal distention on intestinal transcapillary fluid exchange. Am J Physiol 239:G516, 1980. Allen D, White NA, Tyler DE: Factors for prognostic use in equine obstructive intestinal disease. J Am Vet Med Assoc 189:777, 1986. Allen D, White NA, Tyler DE: Morphologic effects of experimental distention of equine small intestine. Vet Surg 17:10, 1988. Lowe JE, Sellers AF, Brondum J: Equine pelvic flexure impaction-a model used to evaluate motor events and compare drug response. Cornell Vet 70:401, 1980. Billig D, Jordan P: Hemodynamic abnormalities secondary to extracellular fluid depletion in intestinal obstruction. Surg Gynecol Obstet 128:1274, 1969. MacHarg MA, Adams SB, Lamar CH, et al: Electromyographic, myomechanical, and intraluminal pressure changes associated with acute intraluminal obstruction of the jejunum in conscious ponies. Am J Vet Res 47:7, 1986. Snyder JR: The pathophysiology of intestinal damage: Effects of luminal distention and ischemia. Vet Clin North Am Equine Pract 5:247, 1989. Snyder JR, Olander NJ, Pascoe JR, et al: Morphologic alterations observed during experimental ischemia of the equine large colon. Am J Vet Res 492301, 1988. Snyder JR, Tyler WS, Pascoe JR, et al: Microvascular circulation of the ascending colon in horses. Am J Vet Res 50:2075, 1990. Moore JN, Gamer HE, Shapland JE, et al: Equine endotoxemia: An insight into cause and treatment. J Am Vet Med Assoc 179:473, 1981. Fine J: The intestinal circulation in shock. Gastroenterology 52:454, 1967. Ewert KM, Fessler JF, Templeton CB, et al: Endotoxin-induced hematologic and blood chemical changes in ponies: Effects of flunixin meglumine, dexamethasone, and prednisolone. Am J Vet Res 46:24, 1985. McCord JM: Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med 312:159, 1985. Parks DA, Granger DN: Contributions of ischemia and reperfusion to mucosal lesion formation. Am J Physiol 250:G749, 1986. Hernandez LA, Grisham MB, Twohig B, et al: Roles of neutrophils in ischemia reperfusion-induced microvascular injury. Am J Physiol 253:H699, 1987. Boles C: Surgical techniques in equine colic. J S Afr Vet Assoc 46:115, 1975. Ross MW, Donawick WJ, Martin BB: Cecal impaction and idiopathic cecal perforation in the horse. Vet Surg 57:13, 1984. Campbell ML, Colahan PL, Brown MP, et al: Cecal impaction in the horse. J Am Vet Med Assoc 184:950, 1984. Meagher DM: Obstructive disease in the large intestine of the horse: Diagnosis and treatment. Proc Am Assoc Equine Pract 18:269, 1972. Robertson ST: Impaction of the large intestine. In Mansmann RA, MCAllister ES, Pratt PW (Eds): Equine Medicine and Surgery. Santa Barbara, CA, American Veterinary Publishers, 1982, p 561. Foemer JJ: Diseases of the large intestine, differential diagnosis and surgical management. Vet Clin North Am Equine Pract 4:130, 1982. Hekmati P, Shahrasbi H: Treatment of caecal impaction by caecotomy in the horse. Br Vet J 130:420, 1974. Steyn DG: Typhlectomy in a horse. J S Afr Vet Med Assoc 37:440, 1966. ~ u s k a m pB:- ise eases of the digestive system and peritoneum. In Dietz 0 , Wiesner E (Eds): Diseases of the Horse: A Handbook for Science and Practice. Part 2 1 (English translation). Basel, Switzerland, Karger, 1984, p 124. Ross MW: Surgical diseases of the equine cecum. Vet Clin North Am Equine Pract 5:363, 1989. Ross MW, Tate LP, Donawick WJ, et al: Cecocolic anastomosis for the surgical management of cecal impaction in horses. Vet Surg 15235, 1986. Ross MW, Orsini JA, Ehnen SJ: Jejunocolic anastomosis for the surgical management of recurrent cecal impaction in a horse. Vet Surg 16~265, 1987. Craig DR, Pankowski RL, Hackett RP, et al: Ileocolostomy: A technique for surgical management of equine cecal impaction. Vet Surg 16:451, 1987. Donelan E, Sloss V: Two cases of rupture of the large intestine in the mare associated with unassisted parturition. Aust Vet J 48:413, 1972. 406 ALIMENTARY SYSTEM 59. Littlejohn A, Richie J: Rupture of the cecum at parturition. J S Afr Vet Assoc 46:98, 1975. 60. Platt H: Cecal rupture in parturient mares. J Comp Pathol 93:343, 1983. 61. Ross MW, Martin BB, Donawick WJ: Cecal perforation in the horse. J Am Vet Med Assoc 187:249, 1985. 62..Voss JL: Rupture of the cecum and ventral colon of mares during parturition. J Am Vet Med Assoc 155:715, 1969. 63. Platt H: Sudden and unexpected deaths in horses: A review of 69 cases. Br Vet J 138:425, 1982. 64. Allison CJ: Invagination of the cecum into the colon in a Welsh pony. Equine Vet J 9:84, 1977. 65. Robertson JT,Johnson FM:Surgical correction of cecocolicintussusception in a horse. J Am Vet Med Assoc 1763223, 1980. 66. Martin BB, Richardson DW, Ross MW, et al: Cecocecai and cecocolic intussusception in 10 horses. J Am Vet Med Assoc (in press). 67. Beroza GA, Barclay WP, Phillips TN, et al: Cecal perforation and peritonitis associated with Anoplocephala perfoliata. J Am Vet Med Assoc 183:804, 1983. 68. Owen Rh, ap Rh, Jogger DW, Quan-Taylor R: Caecal intussusception in horses and the significance of Anoplocephala petfoliata. Vet Rec 124:34, 1989. 69. Cowles RR, Bunch SE, Flynn OV, et al: Cecal inversion in a horse. Vet Med Small Anim Clin 72:1346, 1977. 70. Harrison IW: Cecal torsion in a hone as a consequence of cecocolic fold hypoplasia. Cornell Vet 79:315, 1989. 71. Brown MP, Meagher DM: Repair of an equine cecal fistula caused by application of a hernia clamp. Vet Med Small Anim Clin 73:1403, 1978. 72. Yovich JV, Stashak TS, Colbern GT: Colic resulting from internal pelvic hernia in a horse. Comp Cont Educ Pract Vet 6:S343, 1984. 73. Andrews FM, Robertson JT: Diagnosis and surgical treatment of functional obstruction of the right dorsal colon in a horse. J Am Vet Med Assoc 193:956, 1988. 74. DeGroot A: The significance of low packed cell volume in relation to the early diagnosis of intestinal obstruction in the horse, based on field observations. Proc Am Assoc Equine Pract 17:309, 1971. 75. Boles CL, Kohn CW: Fibrous foreign body impaction colic in young hones. J Am Vet Med Assoc 171:193, 1977. 76. Blue MG, Wittkopp RW: Clinical and structural features of equine enteroliths. J Am Vet Med Assoc 179:79, 1981. 77. Blue MG: Enteroliths in horses-a retrospective study of 30 cases. Equine Vet J 11:76, 1979. 78. McIlwraith CW: Equine digestive system. In Jennings PB (Ed): The Practice of Large Animal Surgery. Philadelphia, W. B. Saunders Company, 1984, p 628. 79. Taylor TS, Valdez H, Nomood GW, et al: Retrograde flushing for relief of obstructions of the transverse colon in the horse. Equine Pract 1:22, 1979. 80. Specht TE, Colahan PT: Surgical treatment of sand colic in equids: 48 cases (1978-1985). J Am Vet Med Assoc 193:1560, 1988. 81. Ragle CA, Meagher DM: Abdominal auscultation as an aid to the diagnosis of sand colic. Proc Am Assoc Equine Pract 33521, 1987. 82. Ragle CA, Meagher DM, Lacroix CA, et al: Surgical treatment of sand colic: Results in 40 horses. Vet Surg 18:48, 1989. 83. White NA, Cougil LM, Brown J: Epizootiology and risk factors in equine colic at university hospitals. Am Assoc Equine Pract Newsletter 1:67, 1986. 84. Duchame NG, Fubini SL: Gastrointestinal complications associated with the use of atropine in horses. J Am Vet Med Assoc 182:229, 1983. 85. Hackett RP: Nonstrangulating colonic displacement in horses. J Am Vet Med Assoc 182:235, 1983. 86. MacDonald MH, Pascoe JR, Stover SM, et al: Survival after small intestine resection and anastomosis in hones. Vet Surg 18:415, 1989. 87. Boening KJ, von Saldern FCH: Nonsurgical treatment of left dorsal displacement of the large colon of horses under general anesthesia. Proc Equine Colic Symp 2:325, 1986. 88. Kalsbeek HC: Further experiences with nonsurgical correction of nephrosplenic entrapment of the left colon in the horse. Equine Vet J 21442, 1989. 89. Huskamp B, Kopf N: Right dorsal displacement of the large colon in the horse. Equine Pract 5:20, 1983. 90. Milne DW, Tarr MJ, Lochner FK, et al: Left dorsal displacement of the wlon in the horse. J Equine Med Surg 1:47, 1977. 91. Markel MD, Orsini JA, Gentile DG, et al: Complications associated with left dorsal displacement of the l a r ~ ewlon in the horse. J Am Vet Med Assoc 18731379, 1985. 92. Spiers VC, Hilbert BJ, Blood DC: Displacement of the left ventral and dorsal colon in two horses. Aust Vet J 55542, 1979. 93. Huskamp B, Kopf N: Die Verlagerung des Colon ascendens in den Milznierenraum beim Pferd (2). Tierarztl Prax 8:495, 1980. 94. Harrison IW: Equine large intestinal volvulus: A review of 124 cases. Vet Surg 17:77, 1988. 95. Reeves MJ, Vansteenhouse J, Stashak TS, et al: Evaluation of the significance of reperfusion injury following ischemia of the equine large colon. Proc Equine Colic Symp 3:39, 1988. 96. Snyder JR, Pascoe JR, Holland M, et al: Surface oximetry of healthy and ischemic equine intestine. Am J Vet Res 47:2530, 1986. 97. Snyder JR, Pascoe JR, Olander HJ, et al: Intraoperative assessment of equine colonic tissue for determining viability. (Abstract). Vet Surg 19:76, 1990. 98. Bertone AL, Stashak TS, Sullins KE, et al: Experimental large wlon resection at the cecocolic ligament in the horse. Vet Surg 165, 1987. 99. Spier SJ, Meagher DM: Perioperative medical care for equine abdominal surgery. In Snyder JR, Markel MD (Eds): Advances in Equine Abdominal Surgery. Vet Clin North Am Equine Pract 5:429, 1989. 100. Spier SJ, Lavoie JP, Cullor JS, et al: Therapy for gram-negative sepsis and endotoxemia using hyperimmune plasma to E. coli (J5). Circ Shock 24:284, 1988. 101. Robertson JT: Resection of intussuscepted large colon in a horse. J Am Vet Med Assoc 181:927, 1982. 102. Dyson S, Orsini J: Intussusception of the large wlon in a horse. J Am Vet Med Assoc 182720, 1983. 103. Wilson DG, Wilson WD, Reinertson EL: Intussusceptionof the left dorsal colon in a horse. J Am Vet Med Assoc 183:464, 1983. 104. Embertson RM, Schneider RK, Granstedt M: Partial resection and anastomosis of the large colon in a horse. J Am Vet Med Assoc 180:1230, 1982. 105. Bertone AL, Stashak TS, Sullins KE: Experimental large colon resection and anastomosis in horses. J Am Vet Med Assoc. 188:612, 1986. 106. Bertone AL, Stashak TS, Sullins KE, et al: Experimental large colon resection at the cecocolic ligament in the hone. Vet Surg 165, 1987. 107. Bertone AL, van Soest PJ, Johnson D, et al: Large intestinal capacity, retention times, and turnover rates of particulate ingesta associated with extensive large colon resection in horses. Am J Vet Res 50:1621, 1989. 108. Bertone AL, van Soest PJ, Stashak TS: Digestion, fecal, and blood variables associated with extensive large colon resection in the horse. Am J Vet Res 50:253, 1989. 109. Ralston SL, Sullins KE, Stashak TS: Digestion in horses after resection or ischemic insult of the large colon. Am J Vet Res 47:2290, 1986. 110. Bertone AL: Large wlon resection. In Snyder JR, Markel MD (Eds): Advances in Equine Abdominal Surgery. Vet Clin North Am Equine Pract 5:377, 1989. 111. Markel MD, Ford TS,Meagher DM: Colopexy of the left large colon to the right large colon in the horse. Vet Surg 15:407, 1986. 112. Rose J, Rosen EM, Peterson PR: Clinical experience with subtotal large colon resection in the horse (1986-1988). Proc Am Assoc Equine Pract 34:29, 1989. 113. Markel MD, Dreyfuss DJ, Meagher DM: Colopexy of the equine large colon: Comparison of two techniques. J Am Vet Med Assoc 192354, 1988. 114. Markel MD, Meagher DM, Richardson DW: Colopexy of the large colon in four horses. J Am Vet Med Assoc 192:358, 1988. 115. Markel MD: Prevention of large colon displacements and volvulus. In Snyder JR, Markel MD (Eds): Advances in Equine Abdominal Surgery. Vet Clin North Am Equine Pract 5:395, 1989. 116. Kersjes AW, Bras GE: The surgical treatment of ileus in the horse. Tijdschr Diergeneeskd 98:968, 1973. 117. Pearson H, Pinsent PJ, Denny HR, et al: The indications for equine laparotomy-an analysis of 140 cases. Equine Vet J 7:131, 1975. 118. Tennant B: Intestinal obstruction in the horse-some aspects of differential diagnosis in equine colic. Proc Am Assoc Equine Pract 21:426, 1975. 119. Meagher DM: Intestinal strangulation in the horse. Arch Am CON Vet Surg 459, 1975. 120. Huskamp B: The diagnosis and treatment of acute abdominal conditions in the h o r s e t h e various types and Erequency as seen at the animal hospital in Hochmoor. Proc Equine Colic Symp 1:261, 1982. 121. Parry BW: Survey of 79 referral colic cases. Equine Vet J 15:345, 1983. 122. Adams SB, Mcllwraith CW: Abdominal crisis in the horse-a comparison of presurgical evaluation with surgical findings and results. Vet Surg 7:63, 1978. 123. White NA, Moore IN, Cowgil LM: Epizootiology and risk factors in equine colic at university hospitals. Proc Equine Colic Symp 2:26, 1985. 124. Crowhurst RL, Simpson DJ, McEvery RJ, et al: Intestinal surgery in the foal. J S Afr Vet Assoc 4659, 1975. 125. Schneider JG, Leipold HW, White SL: Repair of congenital atresia of the colon in a foal. J Equine Vet Science 1:121, 1981. 126. Barnard CN: The genesis of intestinal atresia. Surg Forum 7:393, 1956. 127. Earlam RJ: A study of aetiology of congenital stenosis of the gut. Ann Roy Surg Engl51:126, 1972. 128. Hultgren BD: IIeocolonic aganglionosis in white progeny of overo spotted horses. J Am Vet Med Assoc 180:289, 1982. 129. Keller SD, Horney FD: Diseases of the equine small colon. Comp Cont Educ Pract Vet 7:S113, 1985. 130. Merrit FD,Pickering LA, Bergevin JD: Small colon impaction and rupture into the colonic mesentery in a horse. Vet Med Small Anim Clin 70:1097, 1975. 131. Tate LP, Donawick WJ: Recurrent abdominal distresscaused by enteroliths in a horse. J Am Vet Med Assoc 172:830, 1978. 132. Gay CC, Speirs VC, Christie BA, et al: Foreign body obstruction of the small colon in six horses. Equine Vet J 11:60, 1979. 133. Van Wuijeckhuise, Sjouke LA: Three cases of obstruction of the Small colon by a foreign body. Vet Quart 6:31, 1984. 134. Nieberle K, Cohrs P: Textbook of the Special Pathobiological Anatomy of Domestic Animals. Oxford, Pergamon Press, 1967, p 389. RECTUM AND ANUS 135. Ferraro GL, Evans DR, Trunk DA, et al: Medical and surgical management of enteroliths in equine. J Am Vet Med Assoc 162:208, 1973. 136. Marden DT: Enterolithiasis: A practitioner's view of selected cases. Vet Med Small Anim Clin 63:611, 1968. 137. Bergman RV: Retained Meconium. In Robinson NE (Eds): Current Therapy in Equine Medicine. Philadelphia, W. B. Saunders Company, 1983. p 260. 138. Spiers VC, van Veenendaal BA, Christie RB, et al: Obstruction of the small colon by an intramural hematoma in three horses. Aust Vet J 57:88, 1981. 139. Pearson H, Waterman AE: Submuwsal hematoma as a cause of obstmction of the small colon in the horse: A review of four cases. Equine Vet J 18:340, 1986. 140. Livesey MA, Keller SD: Segmental ischemic necrosis following mesocolic rupture in postparturient mares. Comp Cont Educ Pract Vet 8:763, 1986. 141. Turner TA, Fessler JF: Rectal prolapse in the hone. J Am Vet Med Assoc 177:1028, 1980. 142. Jacobs KA, Barber SM, Leach DH: Disruption of the blood supply to the small wlon following rectal and small colon intussusception in a mare. Can Vet J 23:132, 1982. 143. Walker DF, Vaughan JT: Bovine and equine urogenital surgery. Philadelphia, Lea & Febiger, 1980, p 196. 144. Roberts SI: Veterinary Obstetrics and Genital Diseases. Ithaca, NY, Edwards Brothers, 1971, pp 198 and 326. 145. Evard JH, Fischer AT, Greenwood LD: Ovarian strangulation as a cause of small wlon obstruction in a foal. Equine Vet J 20:217, 1988. 146. Parks AH, Wyn-Jones G, Cox JE: Partial obstruction of the small colon associated with an abdominal testicular teratoma in a foal. Equine Vet J 18:342, 1986. 147. Wilson DA, Foreman JH, Boero MJ: Small wlon rupture attributable to granulosa cell tumor in a mare. J Am Vet Med Assoc 194:681, 1989. 407 148. Ross MW, Stephens PR, Reimer JM: Small colon intussusception in a broodmare. J Am Vet Med Assoc 192372, 1988. 149. Meagher DM: Surgery of the large intestine in the horse. Arch Am Coll Vet Surg 3:9, 1974. 150. Beard WL, Robertson JT, Getzy DM: Enterotomy technique in the descending wlon of the horse: Effect of location and suture pattern. Vet Surg 18:135, 1989. 151. Archer RM, Parsons JC, Lindsay WA: A comparison of enterotomies through the antimesenteric band and the sacculation of the small (descending) colon of ponies. Equine Vet J 20:406, 1988. 152. Hawley PR: Causes and prevention of colonic anastomotic breakdown. Dis Colon Rectum 16:272,1973. 153. Hawley PR, Faulk WP, Hunt TK, et al: Collagenase activity in the gastrointestinal tract. Br J Surg 57:896, 1970. 154. Wise L, McAlister W, Stein T, et al: Studies on the healing of anastomoses of small and large intestines. Surg Gynecol Obstet 141:190, 1975. 155. Trimpi HD, Khubchandani JT, Sheets JA, et al: Advances in intestinal anastomosis: Experimental study and an analysis of 984 patients. Dis Colon Rectum 20:107, 1977. 156. Jiborn H, Ahonen J, Zederfeldt B: Healing of experimental colonic anastomoses: Collagen metabolism in the colon after left wlon resection. Am J Surg 139:398, 1980. 157. Dunphy JE: Preoperative preparation in the colon and other factors affecting anastomotic healing. Cancer 28:181, 1971. 158. Hanson RR, Nixon AJ, Caldenvood-Mays M, et al: Comparison of staple and suture techniques for end-to-end anastomosis of the small colon in hones. Am J Vet Res 49:1621, 1988. 159. Hanson RR, Nixon AJ, Calderwood-Mays M, et al: Evaluation of three techniques for end-to-end anastomosis of the small wlon in horses. Am J Vet Res 49:1613, 1988. 160. Mansmann RA, Gourley IM: Antiperistaltic small colon segments in the horse. J Am Vet Med Assoc 157:1313, 1970.