Neurological examination
advertisement

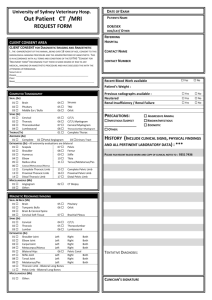
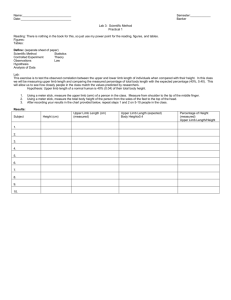
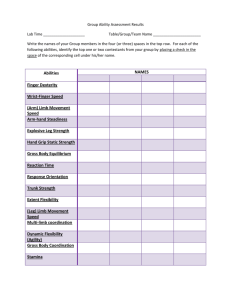
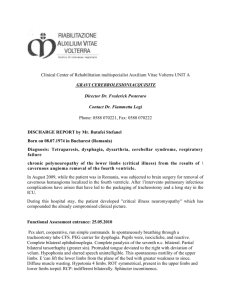
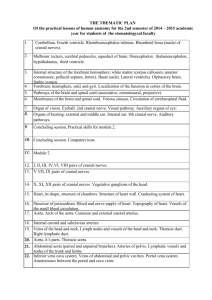
Dr. Csébi Péter, Dr. Ipolyi Tamás Sebészeti Tanszék Neurological examination is the most important part of the clinical evaluation of the neurological patient Auxilary examinations: Radiology, MRI, CT, Scintigraphy, ect. The neurological examination should be always performed slowly and playfully without causing unnecessary stress to the animal! Define if the animals problem is neurological or not Define which part of the nervous system is affected Make the list of possible diseases able to cause the condition Make the diagnostic work-up plan in order to confirm the diagnosis D egenerative V I T A ascular Discopathia Degenerative myelopathy Thrombosis diopathic raumatic, toxic Luxatio, fractura nomaly vertebtal malformatio M etabolic I nflammatory/infectiosus N eoplasma, nutritional FIP, Toxoplasma, Discospondylitis Lymphoma Osteosarcoma Menigioma (Pelvic) fractures Patellar luxation Cranial Cruciate rupture Coxofemoral osteoarthrosis Other diseases: myopathy, aorta embolisation Bilateral Observation Palpation/manipulation Cranial nerves Postural reactions Spinal reflexes Urinary function Sensory evaluation 1. 2. 3. 4. 5. 6. 7. Mental status Behaviour Posture, gait Postural reactions Head nerves Spinal reflexes and Pain perception Posture must be evaluated while the patient is at rest. The position of the head, neck, back, and legs are evaluated. Head: Tilt/Twist Trunk: Abnormal muscle tone Limbs: proprioceptive deficit, LMN or UMN lesion – Increased tone in extensor muscles - UMN – Decreased tone - LMN lesion Uneven distribution of weight - weakness or pain Lameness Must be differentiated from monoparesis/monoplegia Circling Involuntary movement Tremor – an involuntary, rhythmic, oscillating movement Patient must be able to move freely on a non-slip surface Ataxia : failure of muscle coordination Dysmetria : improper range and/or force of movement Paresis : deficit of voluntary movement, but patient is able to walk Plegia : complete loss of voluntary ability to move, patient cannot stand, support itself, or walk Paralysis : complete loss of motor function, term used when cranial nerve function is completely lost Postural Reactions: Proprioceptive Positioning Wheelbarrowing, Neutral and with Head Extended Extensor Postural Thrust Reaction Hopping Hemistanding/Hemiwalking Placing Reaction The awareness of where the limbs are in space Visual placing reaction Tactile placing reaction triceps Sciatic, tibial cr. Biceps, ext. carpi rad. C1-C5 Motor function Sensory function Patellar C6-T2 Tetrapatesis, tetraplegia UMN- all limbs UMN- pelvic limb, LMN- thoracic limb Ataxia- all limbs Hypalgesiaall limbs Hypalgesiathoracic limb T3-L3 L4-S1 Paraparesis, paraplegia UMN- pelvic limb LMN- pelvic limb Ataxia- pelvic limb Hypalgesia/analgesia Pelvic limb Clinical signs correlate with the diameter of fibers, but not with the localization! Forelimbs: norm/increased Hindlimbs: norm/increased UMN sign LMN of forelimbs UMN of hindlimbs Cerebral signs: Seizures, cranial nerve abnormalities Encephaloptahy Forelimbs: decreased Hindlimbs: decreased Forelimbs: decreased Hindlimbs: norm/increased LMN of all four legs No cerebral signs Spinal chord lesion C1-C5 Vertebral fracture/luxation Disc herniation, Fibrocartilaginous embolism Meningomyelitis X-ray, CT, MRI Spinal chord lesion C6-T2 Multifocal spinal chord disease Meningomyelitis CSF (liquor) tap, MRI, CT Neuromus cular disorder Polyradiculoneuritis Metabolic disorders Myasthenia polymyositis Blod tests Flaccid paresis/plegia Reduced to absent reflexes in the hindlimbs Possible urinary retention Possible urinary or faecai incontinence Spastic paresis/plegia Increased hindlimb reflexes Possible urinary retention LMN signs UMN signs T3-L3 L4-S2 Absence femoral pulse, cold limbs, pale or buish pads, reduction or absence of pain sensation : Cat Vertebral fracture, luxation, herniated disc, fibrocartilaginous embolism Xray, myelography, CT, MRI Ischemic neuropathy following an aortic thromboembolism Ultrasonography: HCMP Hit by a car 1 hour ago Lamness in the right thoracic limb No bears weight on the limb The paw is held in a knuckled-over position All other limbs ok, cranial nerves ok Ipsilateral Horner’s syndrome on the right eye Superfitial pain- absent (Deep pain- absent) Bicipital reflex- 0 Tricipital reflex- 0 Exstensor carpi radialis reflex- 0 Proprioceptive positioning- 0 Negative sensation on medial, lateral, cranial, and palmar aspects of the foot Ipsilateral Horner’s syndrome LMN injury Radial nerve paralysis And what about Horner’s? The firs 3 thoracic segments contain neurons that from the symphatic nerves that innervate the eye. Yesterday jumped down off the owner’s kitchen counter Paraparesis, pelvic limb Superficial pain- present (Deep pain- present) Patellar reflex- increased (bilateral) Sciatic reflex- increased (bilateral) Withdrawal reflex- increased (bilateral) Cranial tibial reflex- increased (bilateral) Proprioceptive reflex decreased (bilateral) Pain upon palpation of the spine overlying Th12-Th13 Paraparesis UMN injury to the pelvic limbs D egenerative V I T A ascular Discopathia Degenerative myelopathy Thrombosis diopathic raumatic, toxic Luxatio, fractura nomaly vertebtal malformatio M etabolic I nflammatory/infectiosus N eoplasma, nutritional FIP, Toxoplasma, Discospondylitis Lymphoma Osteosarcoma Menigioma Native x-ray Myelography CT, MRI Diagnosis: Vertebral malformation Intervertebral disc disease Other vet diagnosed bilateral hip dysplasia 3 moths ago. No diagnostic testing, got carprofen 2x/day Improved slightly but now is worse Signs: Difficult to get up, Bilateral hindlimb ataxia (worse on left side) Knucking over both pelvic limbs Cranial nerves ok Thoracic limb ok Pelvic limb bilateral ataxia, with shores on the dorsal surfaces of both feet Patellar reflex- increased (bilateral) Sciatic reflex- decreased (bilateral) Cranial tibial reflex- decreased (bilateral) Proprioceptive reflex- decreased (bilateral) Hip dysplasia- explain the signs? CEC (What is pseudohyperreflexia?) Discopathia intervertebralis Neoplasma Degenerative myelopathy Fibrocartilage embolism Discospondylitis L4 L5 N. femoralis L4,5,6. N. obturatorius (L4), 5,6. N. gluteus cranisalis L6,7, S1. L6 N. gluteus caudalis L7. S1 L7 CEC N. ischiadicus L6, 7, S1, (2) S1 N. peroneus communis S2 N. tibialis N. pudendus S3 Radiology Myelography CT, MRI