Nursing care for non-ambulatory patients.pptx
advertisement
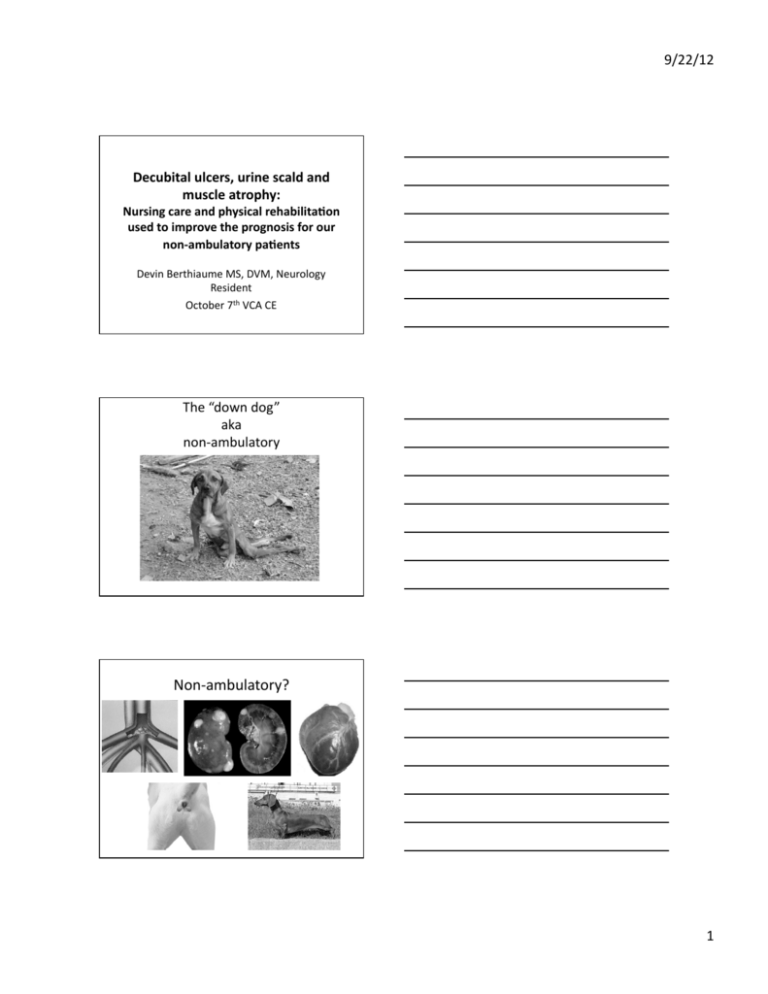
9/22/12 Decubital ulcers, urine scald and muscle atrophy: Nursing care and physical rehabilita8on used to improve the prognosis for our non-­‐ambulatory pa8ents Devin Berthiaume MS, DVM, Neurology Resident October 7th VCA CE The “down dog” aka non-­‐ambulatory Non-­‐ambulatory? 1 9/22/12 Neurologic Causes of Non-­‐ambulatory Status Disk Disease • IVDD Trauma Stress Weakness CNS Disease • Fracture • FCE • High Velocity Disc • Neuromuscular • Metabolic • Neoplasia • Vascular • EncephaliSs Paresis vs Plegia Paresis: weakness Movement Pain percepSon Plegia: absence of any voluntary movement Pain percepSon? Reflexes? 2 9/22/12 Types of Paresis/Plegia • • • • Mono: One limb Para: Back limbs Hemi: One side Tetra: All 4 ComplicaSons • • • • • • • • Pulmonary atelectasis or pneumonia Bedsores and decubital ulcers Urinary bladder damage Urine scald Inadequate nutriSon Muscle atrophy and joint sSffness Pain PaSent (and client) depression Development of an ulcer 3 9/22/12 4 9/22/12 Urine Scald Muscle atrophy Weight loss and muscle atrophy 5 9/22/12 PrevenSng complicaSons associated with non-­‐ambulatory paSents Bedding • Thickness • Substrate • Cleanliness 6 9/22/12 Posi8oning • Sternal (if possible) • Reduce atelectasis • Head elevaSon • Frequent turning • Every 4-­‐6 hours Bladder DysfuncSon 7 9/22/12 Upper Motor Neuron Bladder DysfuncSon • Typical of T3-­‐L3 lesions • Tense, spasSc bladder/sphincter • May be unable to start urinaSon or empty bladder • Overflow inconSnence Lower Motor Neuron Bladder DysfuncSon • Typical of L4-­‐S2 or peripheral neuropathies • Decreased bladder and urethral tone • Flaccid, easily expressed bladder • Urinary inconSnence UrinaSon ComplicaSons PyelonephriSs Atonic bladder Urine scald 8 9/22/12 How Do We Conquer Bladder DysfuncSon??? • Manual expression • CatheterizaSon – Intermieent – Indwelling • Medical therapy ComplicaSons of Bladder Expression Bladder rupture Bladder wall damage PaSent discomfort/anxiety Bladder Expression Technique – Lateral recumbency or standing – Hands on either side, caudal to last rib – Palpate abdomen, moving hands medial, dorsal, and caudal unSl bladder felt – Steady even pressure (medial/caudal) 9 9/22/12 CatheterizaSon Reduces abdominal or bladder trauma Useful in recumbent or criScal paSents Ability to measure and characterize urine output Indwelling or intermieent CatheterizaSon ComplicaSons UTI • 50% of dogs have UTI aher 4+ days of catheterizaSon • AsepSc placement and care Urethral and bladder damage • Aggressive placement • Self trauma or accidents with closed systems Bladder atony 10 9/22/12 DefecaSon Overview When did Spike poop last? ConsSpaSon not usually a problem L4-­‐S2 lesions -­‐ fecal inconSnence Fecal Expression RehabilitaSon t en Cli cSon sfa S sa M ob Muscle streng th Hasten recovery ilit y tud aj ent PaS Decrease pain e Range of MoSon (ROM) AcSve Passive Increased joint mobility Decreased muscle atrophy Decreased Sssue adhesions Increased circulaSon Increased lymph drainage Muscle lengthening 11 9/22/12 ROM Exercises Begin 24 hrs aher surgery or injury unless severe trauma or other contraindicaSons. 5 to 15 minutes each limb q 4-­‐8 hrs Series of repeSSve movements Flexion and Extension Use care extending traumaSzed, geriatric or sensory deprived limbs Massage Increase circulaSon RelaxaSon Decrease pain Loosen sSff muscles Supported Walking Slings Wheelchairs – pelvic, thoracic or all 4 Decreases limb edema, atelectasis Encourages voluntary movement, urinaSon 12 9/22/12 Supported Walking ComplicaSons – Pedal ulceraSon • BooSes – Worsening of unstable lesions – Discomfort or anxiety – Human injuries Hydrotherapy Most dogs (and some cats) love it Low impact Full range of moSon Resistance Builds muscle 13 9/22/12 14