Lecture 53
advertisement
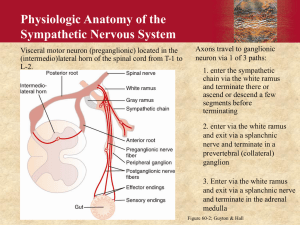
Cardiovascular Session 53 November 4, 2003 Dr. Jeffries Jordan Michelena (jmichel@cu) Anti-Hypertensive Drugs Part II 4.3 Other Properties relevant to Antihypertensive Effect: (of β-Blockers) 1. Intrinsic sympathomimetic activity- a drug is a partial agonist of β2 receptors while being a competitive antagonist at β1 receptors. a. Partial β2 agonist would cause vasodilatation in the peripheral vessels of the extremities and surface. Therefore, stimulation will increase vasodilatation but this property does not make a better hypertensive but does eliminate one side effect. b. Examples: Pindolol, Acebutolol, penbutolol 2. Mixed antagonism- block both β2 and α1 receptors (no additional anti HTN benefit) a. Labetalol and Carvedilol- for Heart failure as well 5:1 Therapeutic use in Hypertension 1. Can be used as a Monotherapy 2. β Blockers are drugs of choice in ischemic heart disease and Hypertensives that have concomitant Angina Pectoris. 3. Most effective in High rennin HTN not volume expanded HTN because of inhibition of rennin production and release. 4. Compliance is huge because of the low cost of drug, once a day, or pleasant effects. a. Propanolol can relief anxiety or nervousness. b. Ex. Mother got HTN giving birth to Dr. Jeffries. On diuretic, β blocker and Angiotensin receptor blocker. Diuretic is cheap, β blocker is very cheap- takes it because she likes it not because the needs it, AT II antagonists are $2 a pill and she will not take the medication until right before her visit so BP seems normal for visit. This happens. 5:2-5:3 Adverse Effects of β Blockers 1. Bradycardia 2. Branchospasm- causes wheezing due to β2 blockade. Reason why non selective drugs are contraindicated in asthma 3. Coldness of extremities- vasoconstriction in peripheral circulation due to a β2 blockade (nonselective drug only) 4. Withdrawal Effects- Long period block results in increased production of β receptors but dose blocks them. If suddenly stop the drug this multitude of β receptors is exposed to circulating catecholamines and sympathetic nervous system. Just a little stimulation, patient can get pronounced palpitations, tachycardia and other sympathetic effects mediated by β1 and β2 receptors. 5. Heart Failure- β blockers used to treat heart failure but if used too aggressively then they can cause heart failure or the patient has had an occult MI resulting in compensated heart failure therefore there is no cardiac reserve. 6. Glucose metabolism a. Prevent catecholamine-induced rise in glucose metabolism b. Most importantly- they prevent onset of tachycardia as a response to hypoglycemia 1 i. Insulin dependent diabetics can feel the onset of hypoglycemia through increased palpitations, heart rate, and other symptoms natural to a hypoglycemic state but blocked by β blockers 7. CNS effects- minor incidence of depression 8. Propanolol is both safe and effective in pregnancy 9. Rise in triglyceride conc. And decrease in HDL conc. a. Associated in older studies with high propanolol doses but effect fade over time 10. Drug Interaction: a. NSAIDs- blunt β blocker effect due to activation of cytochrome P450 responsible for β blocker metabolism b. Epinephrine- Normally a dual effect on BP- rise due to α1 receptor and fall due to vasodilatory β receptor activation. By blocking β2 only get the α response to epinephrine leading to severe hypertension c. The conduction effects of β blockers and Calcium channel blockers are additive. Do not want to use these two classes of drugs together. 6:1 α-Adrenoceptor Blockers 1. Mechanism of action- blockade of vascular α receptors 2. Nonselective- block both α1 and α2 but not used for treatment of many things a. Phentolamine and phenoxybenzamine are sometimes used for pheochromocytomaa benign chromaffinoma of the adrenal gland characterized by secretion of catecholamines resulting in HTN. Phenoxybenzamine- an alkylating agent acting as an irreversible antagonist. Phentolamine has effects similar to viagra, the catch- only if injected into the corpus cavernosum. Some reason it was not popular. 3. Selective- block α1 receptors such as prazosin. Any -azosin is an α1 blocker. Others terazosin, doxazosin, and trimazosin. 6:2 Therapeutic use in Hypertension 1. Nonselective used for hypertensive crises in pheochromocytoma 2. Selective was used as monotherapy for hypertension but the ALLHAT study poked a hole in this. a. Adjunctive therapy for the inhibition of compensatory increases in sympathetic tone i. Example- a β blocker increases peripheral resistance but a prazosin can block this. 6:3 Side effects of α1-adrenoceptor blockers 1. First dose phenomenon- Sympathetic nervous system allows you to stand up. Shy Drager syndrome patients- those with loss of a functional sympathetic system, complain of the inability to stand up. Sym. NS causes tone, forcing blood to return to the heart. Vasoconstriction allows for a constant return of blood to the heart. By standing w/o a SNS, blood pools in the legs and does not perfuse the brain leading to syncope. a. First dose phenomenon- with the first dose adverse effects are worst but fade with time but patient will not take the medication because of their first bad experience. Therefore have patients take medication before going to sleep. 2. Tachycardia is cause by the following mechanism: BP falls, baroreceptor stimulation, leading to sympathetic stimulation again. No vasoconstriction because α1 blockade but there is tachycardia from β receptor effects. 3. GI effects default answer. 2 4. ALLHAT has shown that doxazosin leads to a higher than expected incidence of Congestive Heart Failure when compared to other drugs, especially diuretics. No α blocker monotherapy. 7:1 Adverse Effects of Non Specific α-Adrenoceptor Blockers 1. Postural Hypertension- see First dose phenomenon 2. Reflex Tachycardia- see Tachycardia in slide 6:3 3. Fluid retention- long standing vasodilatation leads to kidney under perfusion. It then retains fluid to maintain renal perfusion. Does not always happen. 7:2 Other Sympatholytics (He thought he got rid of these but talked about them any way.) 1. Guanethidine-Acts somewhat like a peripheral neurotoxin. a. Inhibits sympathetic Nervous system by entering the storage vesicles replacing norepinephrine so that when sympathetic stimulation happens guanethidine- a poor vasoconstrictor- comes out leads to an impairment of peripheral sympathetic transmission. b. Adverse effects- severe postural hypotension. Also get fluid retention, diarrhea, and impaired ejaculation. 2. Ganglionic blockers- in here for completeness sake. Not used for hypertension any more. a. Trimethaphan is the prototypical Ganglionic Blocker- traditionally used for hypertensive crises and dissecting aortic aneurysm. 3