Fat (fat) and Tubby (tub): Two Autosomal Recessive Mutations
advertisement

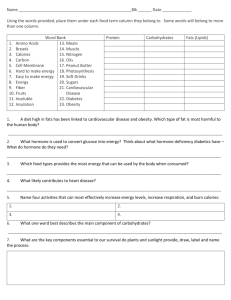
Fat (fat) and Tubby (tub): Two Autosomal Recessive Mutations Causing Obesity Syndromes in the Mouse D. L. Coleman and E. M. Eicher This report describes the development of obesity syndromes in mice caused by two autosomal recessive mutations, fat (fal), located on chromosome 8, and tubby (tub), located on chromosome 7. Both mutations cause slowly developing but ultimately severe obesity conditions. Although hyperinsulinemia, hyperactivity of the B cell of the islets of Langerhans, and -cell degranulation are consistent features, these obesity syndromes do not progress to severe diabetes. The many different singlegene mutations in the mouse that produce obesity-diabetes syndromes of varying degrees of severity make the mutant mouse a powerful tool for analyzing the number and nature of the primary defects than can cause obesity states. From The Jackson Laboratory, Bar Harbor, Maine 04609. This research was funded in part by NIH research grants DK14461 (DLC), GM20919 and RR01 183 (EME). We thank Christina Gott for originally noting the progenitor tubby male, Janice Southern for establishing the mutant colony of tubby mice, and Elizabeth S. Russell for providing us with the C57BL/6J-HbbP congenic strain. Dorothy B. Chapman and the late Richard H. Copp provided colony management and technical assistance. The Jackson Laboratory is fully accredited by the American Association of Laboratory Animal Care. Address reprint requests to Dr. Coleman, Senior Stall Scientist. The Jackson Laboratory, 600 Main St., Bar Harbor, Maine 04609-0800. Journal of Heredity 1990;81:424-427; 0022-1503/90/$2.00 Diabetes-obesity syndromes are present in all human societies and are widespread in the animal kingdom. Of special importance to research workers in this field is the availability of small rodent models that can be bred in the laboratory and maintained under controlled genetic and environmental conditions. Although the abnormalities associated with each obesity type may have similarities with regard to their overall development, the documentation that several different single genes are involved in the different conditions makes it unlikely that the various syndromes will be reduced to disturbances in a single metabolic pathway. Single-gene mutations maintained on standard inbred backgrounds are particularly useful for study since appropriate matings can be made that produce predictable numbers of unaffected and affected animals, all of which are of the same genetic background, differing only by the presence of a single mutant gene or a small region of the chromosome containing the mutant gene. Several such single-gene mutations are known in the mouse, and their characteristics and interaction with inbred backgrounds have been well described (Bray and York 1979; Coleman 1978, 1982; Herberg and Coleman 1977). This report deals with two previously unreported obesity mutations that occurred spontaneously in mouse colonies maintained at The Jackson Laboratory. With the rapid development of molecular techniques, these new murine mutations causing obesity may play a fundamental role in elucidating the number and nature of such defects and their relationships to each other. Materials and Methods All mice were housed three to five mice per cage and fed natural ingredient chow (Old Guilford 96, Emory Mouse Co., Guilford, Connecticut) ad libitum. We obtained body weights and blood sugar concentrations weekly and made plasma insulin determinations at monthly intervals on selected normal and mutant mice. Blood (50 1l)for blood sugar determination was obtained from the retroorbital sinus, while that for plasma insulin (0.5 ml) was obtained from the tail vein. Analytical and histological procedures were as previously described (Coleman and Hummel 1967). Results The Fat (fat) Mutation Origin and inheritanceof the fat mutation. Obese mice were found in an HRS/J inbred mouse colony in 1973 and progenitor mice were provided to us for genetic and metabolic analyses. Breeding tests established that this obesity condition was caused by an autosomal recessive mutation, which we named fat, gene symbol fat. Forty (20.7%) of 176 offspring born to fat/+ parents developed the obese phenotype establishing autosomal recessive inheritance. Allelism tests with the phenotypically similar diabetes (db, chromosome 4) and obese (ob, chromosome 6) mutations 70 A B 60 50 1- 40 a 30 U o 20 10 l 0 10 20 30 AGE 10 20 30 (weeks) and eight female -. O HRS/J-/at/fat mutants. The growth curve for normal HRS/J is similar to that of normal B6 Figure 1. (A) Growth curve of eight male H-and seven female mice (Figure B), except that the attained body weight at 24 wk is greater, 32 g for males and 26 g for females; (B) Growth curve of six male --and five female A-A normal littermates. --O 6-tub/tub mutants compared with five male A- produced no offspring having the obese phenotype, which established that fat was a new mutation, not a remutation at the db or ob locus. Recent evidence suggests that fat is located on chromosome 8 linked to esterase-I (Es-i) (Paigen B, The Jackson Laboratory, unpublished observations). Physiologicalcharacteristicsof the fat mutation. Fat mutants develop obesity between 6-8 weeks of age (Figure IA). The increase in body weight develops more slowly than that seen with the more severe obese (ob) and diabetes (db) mutations in which the obese phenotype can be recognized at 18 days of age. Even so, the obesity produced by the fat mutation can be characterized as massive since mutants attained body weights of 60-70 g by 24 wk of age (Figure IA). No sex differences were seen in the rate of weight gain in fat mutants in contrast to that seen with normal littermate controls (data not shown) where males after weaning are always heavier than females. Most of the excess weight in mutants represented increased weight of body fat that extended to fat stores throughout the body rather than being confined to the axial and inguinal regions as is typically observed by the pear-shaped body conformation of the phenotypically similar ob/ob and db/db mutants. Homozygous fat mutants are infertile, but not sterile, and litters can be obtained from homozygous male and female mutants if they are mated before obesity develops at 5-8 wk of age. Hyperglycemia was observed only transiently and just in males (Table 1) approaching 250 mg/ml at 7-8 wk and then declining to within the normal range (120150 mg/dl). Female mutants remained normoglycemic throughout the entire period of study. Hyperinsulinemia was a consistent feature in mutants of both sexes and was severe at weaning (4 wk). The hyperinsulinemia was associated with hypertrophy and hyperplasia of the islets of Langerhans, features that became more pronounced as the mutants aged. Varying degrees of cell degranulation were consistent findings in males but were only obvious in females at 12 wk and older (Table 1). No signs of islet or a-cell atrophy were observed in even the oldest mutants examined (11-13 mo). To determine whether the fat/fatobesity condition could be exacerbated to a fullblown diabetes condition, as seen in either ob/ob or db/db mice maintained on the C57BL/KsJ (BKs) inbred strain background, we transferred the fat mutation from the HRS/J background onto the BKs background via five cross-intercross cycles of breeding followed by inbreeding at N5. On the BKs background, the syndrome remained mild and similar in all parameters (rate of weight gain, blood sugar concentration, hyperinsulinemia, pancreatic ° Table 1. Characteristics of HRS/J-fat/ut mice with age Characteristic Age (wk) 4 Blood glucose (mg/dl) Male 143 ± 141 ± Female Plasma immunoreactive insulin (AU/ml) Male 612 ± Female 417 ± Islet hypertrophy and hyperplasia Male Trace Female None -cell degranulation Male Some Female None 8 12 175 ± 32 124 ± 10 16 199 ± 22 20 150 ± 22 147 ± 13 7.1 8.8 228 ± 40 121 ± 11 13 24 805 ± 190 988 ± 208 1,100 ± 96 1.752 ± 415 Some Trace Mild Some Moderate Mild Severe Moderate Some None Mild Some Moderate Some Moderate Mild 133 ± 8.1 2,920 ± 479 2,240 ± 427 ° Figures represent mean + SEM from six to eight mice of each group. Coleman and Echer *New Obesity Mutants in the Mouse 425 Table 2. Mapping of the tub gene on chromosome 7 Cross: (Gpi-.l Hbbd +/Gpi-lb Hbb' tub)F, female x Gpi-1* Hbb' tub/Gpi-lb Hbb tub male Loci inherited Gpi-l No. of bb tub offspring Gpi-l" Gpi-lb Hbt Gpb-bb Hbb + rub 14 I 10 Gpi-l Hbb tub 13 Hbbd + 8l Gpi--IHbbd Gpi-P Hbb rub + 1 Gpi-I Gpi-Pl Hbb Hbb + tub CGl~pi-lb Cpi 1 Total Region of recombination None Cpi- l-Hbb Hbb-tub 0 0 47 Gpi-I-Hbb; Hbb-tub Gene order with %recombination ± SE: Gpi-) - 44.7 + 7.2 - Hbb - 4.2 + 2.9 - tub mative as to the relative order of Hbb and Gpi-i, the actual proximal or distal location of tub relative to Hbb will need to be confirmed. Establishing the B6-HbbP +/Hbbs tub strain. After we determined that tub was located on chromosome 7 near the Hbb locus, we established a breeding stock of B6 mice segregating for both tub and Hbb in order to use the Hbb locus to "tag" the tubby mutant gene and thus select tub/+ and tub/tub offspring from informative matings before their obese phenotype was evident. This B6 stock was established as follows: A female of the B6-Hbbcongenic strain was mated to a B6-tub/tub male and the resulting HbbP +/Hbb' tub offspring morphology) to that seen in mutants maintained on the HRS/J inbred background. Most significantly, plasma immunoreactive insulin (IRI) was high 886 + 95 uU/ ml at I yr and remained high up to 2 yr. No signs of B-cell atrophy were seen in BKs-fat/lfat mutants in contrast to the severe atrophy and drop in plasma IRI that occurred at about 2-3 mo of age in either diabetes (db) or obese (ob) mutants maintained on the BKs background. The Tubby (tub) Mutation Origin and inheritanceof the tub mutation. The first tubby mouse noted was a C57BL/ 6J (F125) male breeder located in the Animal Resources Colonies of The Jackson Laboratory. This male, together with his normal sister and their eight young, were transferred to our research colony. Four single-pair matings were established from this litter. Both mice in one breeding pair became obese and produced a litter of young, all of which developed obesity after weaning. None of the mice in the other three pairs of mice developed obesity. Each of these breeding pairs of mice, however, did produce normal and obese young. We concluded from this result that the newly identified obesity condition was inherited, probably as an autosomal recessive gene. To determine the exact mode of inheritance of this new mutation, an obese male was mated to two normal unrelated C57BL/ 6J (B6) females. Because their nine offspring were normal, we concluded that the mutation was not inherited as an autosomal dominant or X-linked gene. Three single-pair matings and one trio mating were established from these nine young and their offspring were classified at weaning and at 8-10 wk of age for obesity. Approximately 25% of these offspring developed an obese condition by 10 wk of age, suggesting that the obese condition was caused by an autosomal mutation, hereafter named tubby, gene symbol tub. To determine the genetic linkage of the tubby mutation, a B6 homozygous tubby female was mated to a CAST/Ei male. This particular cross was chosen for mapping tubby because the CAST/Ei inbred strain is known to differ from the B6 strain at a number of genetic loci. F, females were then mated to B6-tub/tub males and 47 backcross offspring were typed for segregating loci, including the Hbb (hemoglobin beta-chain complex) and the Gpi-l (glucose phosphate isomerase-1) loci, both of which reside on chromosome 7, order centromere - Gpi-l - Hbb. These data, presented in Table 2, indicate that the tubby locus is located four map units from Hbb on chromosome 7, probably distal to Hbb. Because only two mice were infor- were intercrossed. Offspring from this cross were typed for their Hbb phenotype. From this mating, mice that were heterozygous Hbb/ Hbb ', presumed to be HbbP +/ Hbb' tub, were mated to mice that were homozygous Hbbs, presumed to be Hbb' tub/Hbb tub. The next generation of mice were again typed at weaning for their Hbb genotype. This system of breeding is now used to maintain the tubby mutation. Physiological characteristics of the tub mutant. Tubby mice are very similar to fat mice except that the progression to obesity is slower (Figure B). The phenotype cannot be recognized until 9-12 wk of age and the average body weight at 24 wk is less (46 g in tubby males vs 66 g in fat males). Another difference between tubby and fat mice is sexual dimorphisms with respect to rate of weight gain, plasma in- Table 3. Characteristics of C57BL/6J-tubtub mice with ageI Age (wk) Characteristic 4 8 12 16 20 147 ± 5.5 130 ±+3.3 139 ± 6.0 104 + 4.7 110 +±5.1 112 _+ 4.6 115 ± 3.9 120 ± 3.3 101 ± 3.0 120 + 4.6 83.4 ± 23 57.3 ± 16 96.7 ± 9.3 37.0 ± 7.6 258 ± 71 72 ±+ 14 418 ± 113 53.9 ± 7.3 None None None None Some Moderate Trace Severe Some None None None None None None Some Moderate None Blood glucose (mg/dl) Male Female Plasma immunoreactive insulin (U/ml) Male Female 69.9 ± 16 305 ± 64 Islet hypertrophy and hyperplasia Male Female None d-cell degranulation Male Female None I Figures represent mean SEM obtained from six to eight mice of each group. Normal values are 130-150 mg/ dl for glucose and 28-37 eU/ml for insulin. sulin concentration, and pancreatic morphology (Table 3). The attained average weight at 24 wk of tub/tub females is only 38.6 ± 1.1 g compared to 46.4 + 0.9 g in males. Mild hypoglycemia (110 mg/dl in mutants vs 140 mg/dl in controls) associated with hyperinsulinemia develops in mice of both sexes (Table 3). The hyperinsulinemia is mild at weaning and increases gradually with age. Histological examination of the pancreas showed relatively normal islet morphology in mutants of both sexes compared to normal littermates up to 12 wk of age, at which time some enlargement of the islets occurred in males, a condition not seen in females until much later (>24 wk). By 1 yr of age many large hypertrophied islets with enlarged sinusoids were seen in tub/ tub males whereas these changes were not nearly as evident in like-aged mutant females. Degranulation of the cells was observed only in the late stages, suggesting that insulin synthesis and secretion in tub/tub mice can be sustained at levels sufficient to maintain near normal 8-cell granulation in spite of hyperinsulinemia without degenerative changes in the islet or E-cell being produced. Tubby homozygotes, like fat homozygotes, are infertile, but not sterile, and can produce litters when the animals are mated before severe obesity develops (up to 12 wk). The increased adipose tissue, as in the fat mutation, is distributed over the entire body. The insulin II gene in the mouse is located on chromosome 7 (Lalley and Chirgwin 1984) suggesting that the tubby condition may result from some structural defect in insulin. HPLC analysis of the insulin from tubby mutants showed no abnormalities, compared to normal littermates, in the ratio of insulin I to insulin II or in structure (based on retention time) showing that a structural defect in insulin is not associated with this obesity syndrome (Coleman DL, unpublished observations). Discussion The two obesity mutations tubby and fat produce a more slowly developing obesity syndrome than that in the phenotypically similar obese and diabetes mutants. Additionally, problems in glucose homeostasis are mild and only transient. Hyperglycemia is only seen in homozygous fat males between the ages of 7-11 wk whereas fat females and tubby mutants of both sexes remain normoglycemic or slightly hypoglycemic. In this regard, the mutations fat and tubby produce an obesity syndrome similar to that produced by the viable yellow (Av) mutation. A mutants are characterized by a severe but slowly developing obesity with modest hyperinsulinemia associated with normal glycemia or even mild hypoglycemia (Coleman 1985). When the fat and viable yellow mutations were placed on the BKs inbred background, the conditions remained mild and diabetes was not seen. This differs from the change from mild to severe diabetes seen when either the obese (ob) or diabetes (db) mutation was placed on the BKs inbred background. Tubby has not been placed on the BKs background, but it appears that in these milder obesity syndromes (viable yellow, fat and tubby) insulin synthesis and secretion can adjust to meet the higher than normal demand without producing islet atrophy and severe diabetes. Longevity studies have not been done with either the fat or tubby mutants, but one would anticipate that the lack of diabetes symptoms would allow a lifespan similar to that seen with viable yellow obese or diabetes maintained on the diabetes protective B6 inbred background. Histological examination of the pancreas showed that the syndromes produced in tub/tuband fat/fatmice ranged from most severe (hyperplasia, hypertrophy, and marked degranulation of fS cells) in older fat males to the nearly normal pathology seen in middle-aged tubby females. One striking feature of fatmutants on either the HRS/J or BKs background is the pronounced hyperinsulinemia evident as early as 4 wk of age, at a time when obesity is not detectable. Hyperinsulinemia of this magnitude at this age without substantial obesity is not typical of any of the other known obesity mutants. The severe hy- perinsulinemia sustained for most of the lifespan of the fat mutants maintained on the BKs background without islet atrophy tends to dissociate chronic hyperinsulinemic stress from d-cell necrosis. The five mutations obese (ob), diabetes (db), viable yellow (A'), fat (fat), and tubby (tub) in the mouse offer the investigator obesity-diabetes syndromes with a wide range of severities, from mild obesity and no diabetes to severe obesity with transient diabetes or severe obesity with severe and life-shortening diabetes. This wide range of changes in the manifestation of obesity coupled with varying degrees of diabetes provide the investigator precision tools with which to advance our understanding of the causes and development of obesity-diabetes conditions. That five genes in mice have been found that cause obesities with varying degrees of severity suggests that similar genes will be found in man and that human obesity may have many possible genetic etiologies. Mutant mice maintained on defined genetic backgrounds and used in conditions of stringent environmental control should provide the standardized material required to ultimately understand the causes of obesity at the molecular level. References Bray GA and York DA, 1979. Hypothalamic and genetic obesity in experimental animals: an autonomic and endocrine hypothesis. Physiol Rev 59:719-809. Coleman DL 1978. Obese and diabetes: two mutant genes causing diabetes-obesity syndromes in mice. Diabetologia 14:141-148. Coleman DL, 1982. Diabetes-obesity syndromes-in mice. Task force recommendations. Diabetes 31(Suppl 1): 1-6. Coleman DL, 1985. Antiobesity effects of etiocholanotones in diabetes (db) viable yellow (A-) and normal mice. Endocrinology 117:2279-2283. Coleman DL and Hummel KP, 1967. Studies with the mutation, diabetes, in the mouse. Diabetologla 3:238248. Herberg L and Coleman DL, 1977. Laboratory animals exhibiting obesity and diabetes syndromes. Metabolism 26:59-98. Lalley PA and Chirgwin JM, 1984. Mapping of the mouse insulin gene. Cytogenet Cell Genet 37:515 (abstr). Coleman and Eicher - New Obesity Mutants in the Nfoue 427