Clinical Oncology (2004) 16: 523–527
doi:10.1016/j.clon.2004.06.024
Original Article
Small-cell Carcinoma of the Urinary
Bladder: 10-year Experience
S. A. Mangar*, J. P. Logue*, J. H. Shanksy, R. A. Cooperz, R. A. Cowan*, J. P. Wylie*
*Department of Clinical Oncology, Christie Hospital NHS Trust, Manchester; yDepartment of Histopathology, Christie
Hospital NHS Trust, Manchester; zDepartment of Clinical Oncology, Cookridge Hospital, Leeds, UK
ABSTRACT:
Aims: Small-cell carcinoma of the urinary bladder is rarely encountered in clinical practice. We report on our clinical experience with
affected patients presenting to our institution from 1986 to 1996.
Materials and methods: We retrospectively analysed 14 pathologically confirmed cases, specifically looking at stage, presenting features,
treatment and overall survival. The median age at presentation was 74 years (range 54–91 years).
Results: Ten patients presented with stage III disease, and four patients with stage IV disease (1 Z nodal, 3 Z distant metastases). Four
patients were treated with radical radiotherapy (one patient receiving neoadjuvant chemotherapy) and two underwent a radical
cystoprostatectomy. Five patients received palliative bladder radiotherapy and three were too frail for treatment at presentation. The overall
median survival was 5 months. Patients receiving radical treatment had a median overall survival of 21 months, with only one long-term
survivor.
Conclusion: This highly aggressive tumour tends to affect an elderly population who are generally frail and have significant comorbidity.
Many are unfit for radical treatment. In patients with disease confined to the pelvis who are able to tolerate radical intervention, the results
of local therapy alone are poor. It therefore remains incumbent on treating clinicians to explore means of improving these results. Initial
chemotherapy analogous to small-cell lung cancer may offer a durable response with a better chance for long-term survival. Mangar, S. A.
et al. (2004). Clinical Oncology 16, 523–527
Ó 2004 The Royal College of Radiologists. Published by Elsevier Ltd. All rights reserved.
Key words: Chemotherapy, radiotherapy, small-cell bladder cancer
Received: 21 January 2004
Revised: 20 May 2004 Accepted: 23 June 2004
Introduction
Materials and Methods
Extrapulmonary small-cell carcinoma is a rare but welldescribed tumour occurring at sites as diverse as the
gastrointestinal tract, thymus, larynx, salivary gland, skin,
breast, prostate and cervix [1–8]. Within the urinary
bladder, it accounts for less than 0.5% of malignancies
[9]. Since the first published case by Crameret al. [10] in
1981, about 150 cases have been reported to date [11].
With such paucity of clinical data, it is not possible to
offer a didactic approach to treatment. Many of the reported
cases present with either locally advanced or metastatic
disease, and most patients ultimately die of disseminated
disease. We report our clinical experiences with 14 patients
treated at this institute, and review the published literature
about the management of this disease.
All cases (n Z 14) of small-cell carcinoma of the urinary
bladder (SCBC) referred to the Christie Hospital, Manchester, UK from 1986 to 1996 were retrospectively
reviewed. Data on age, sex, presentation, stage, treatment
and outcome were obtained from the medical notes.
Certified causes of death were obtained from the National
Cancer Registry. All patients had an initial transurethral
resection (TUR). All pathology was reviewed centrally. For
those patients in whom radical treatment was intended,
computed tomography of the abdomen and pelvis, and
chest radiographs, were obtained. The time to relapse was
calculated from the date of diagnosis, and absolute survival
figures are quoted. Where possible, patients were staged
according to the UICC TNM 1987 classification.
Results
Author for correspondence: Dr S. Mangar, Academic Department of
Radiotherapy, Royal Marsden Hospital, Sutton, Surrey SM2 5PT, UK;
Tel.: 0208-661-3261; Fax: 0208-643-8809; E-mail: stephenmangar@
supaworld.com
0936-6555/04/080523C05 $35.00/0
The clinical details are summarised in Table 1. Twelve men
and two women with a median age of 74 years (range 54–
91 years) were treated within the 10-year study period. The
Ó 2004 The Royal College of Radiologists. Published by Elsevier Ltd. All rights reserved.
524
CLINICAL ONCOLOGY
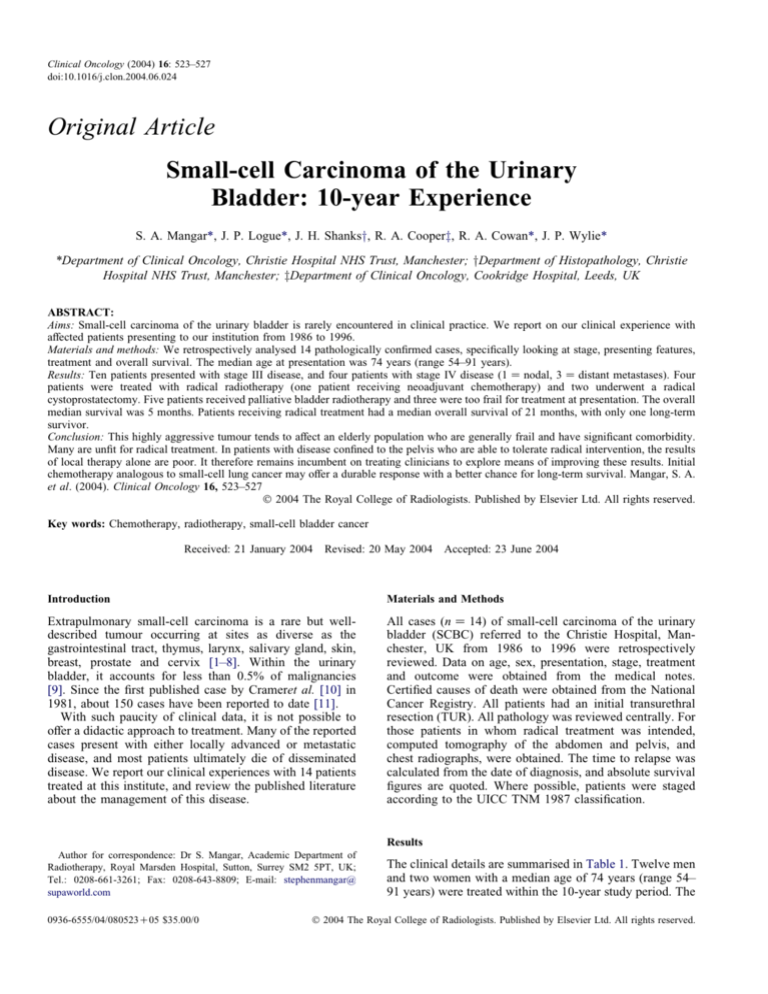
Table 1 – Summary of patient details
Age
(years)
Stage*
1; male
70
T3N0M0
Radical bladder radiotherapy
2; male
3; female
81
91
T3
T3
4; male
86
T3, M1
5; male
6; male
62
79
pT3N0M0
T4N0M0
7; male
58
T3N0M0
8; male
85
T3N0M0
9; male
10; male
11; female
81
64
84
T3N1M0
T3N0M0
M1
Palliative bladder radiotherapy
Too frail
for treatment
Too frail
for treatment
Cystoprostatectomy
Palliative bladder
radiotherapy
Induction chemotherapy
( platinum/etoposide)
Radical bladder radiotherapy
Palliative bladder
radiotherapy
Palliative bladder radiotherapy
Radical bladder radiotherapy
Palliative bladder radiotherapy
12; male
65
T4N0M0
Radical bladder radiotherapy
13; male
74
M1
14; male
54
pT3N0M0
Too frail
for treatment
Cystoprostatectomy
Patient; sex
Treatment
Site of relapse/further treatment
Neck nodes at 14 months/six
cycles of platinumchemotherapy
Brain metastases at 22 months/cranial
radiotherapy
Outcome
Cancer death at 24 months
Cancer death at 4 months
Cancer death at 1 month
Clinical evidence of brain metastases
at presentation
Cancer death at 2 weeks
Cancer death at 4 months
Cancer death at 18 months
Para-aortic lymph nodes at
15 months/abdominal
radiotherapy
Bone metastases at 5 months
Bone metastases
at presentation
Liver and bone
metastases at 4 months
Bone metastases
at presentation
Cancer death at 18 months
Cancer death at 9 months
Cancer death at 3 months
Intercurrent death at 39 months
Cancer death at 4 months
Cancer death at 6 months
Cancer death at 2 months
No clinical evidence of
disease at 7 years
*Staging according to UICC TNM 1987. In some cases, there is insufficient information to give complete TNM stage.
most common presenting symptom was haematuria in 13
patients. One patient presented with urinary frequency. Of
the nine completely staged patients, eight presented with
stage III disease (T3N0-6, T4N0-2), and one with a stage
IV tumour (T3N1M0). Five patients were too frail at
presentation to undergo full staging investigations. Three
patients presented with distant metastasis.
Two patients had a previous history of malignancy. Case
11 had an invasive transitional cell carcinoma of the
bladder treated with radiotherapy 21 years earlier, and case
eight had an early stage prostatic adenocarcinoma diagnosed but not treated 9 years previously.
The most frequent site of involvement within the bladder
was on the lateral and posterior walls. The lesions were
invariably unifocal and had a predominantly papillary
morphology. The pathology findings are summarised in
Table 2. One case was negative for both cytokeratins, and
five cases were negative for both chromogranin and
synaptophysin. In 12 cases, there were elements other than
small-cell carcinoma present (Table 3).
All treatment was at the discretion of the treating
clinician. Three patients were too frail for any further
treatment following TUR. Of these, one had bone
metastases at presentation and one had suspected cerebral
metastases. Five patients were treated with palliative
radiotherapy to the pelvis, and four received radical
radiotherapy to the bladder. The radical dose given was
50–52.5 Gy/20 fractions using megavoltage photons
planned as a four-field brick covering the whole bladder
with a 1.5 cm margin. One of these patients received
treatment with six cycles of neoadjuvant chemotherapy
(carboplatin AUC 5, and etoposide 120 mg/m2 d1–3)
before radical radiotherapy, and another patient received
the same chemotherapy regimen at relapse. Two patients
had a radical cystoprostatectomy.
Overall, 10 (70%) patients died of disease within 2 years
of diagnosis (median overall survival 5 months). Eight died
Table 2 – The panel of immunohistochemical markers
Detectable antigen
Chromogranin
Synaptophysin
Neuron-specific enolase
MIC-2
CAM 5.2 (cytokeratin)
MNF 116
MIC-2 (CD99 antigen);
CAM 5.2 (cytokeratin 7C8);
MNF 116 (cytokeratin 6, 16, 17).
Positive
Negative
8
6
14
0
12
10
6
8
0
14
2
4
525
SMALL-CELL CARCINOMA OF THE URINARY BLADDER
Table 3 – The presence of other histological elements
Histological elements other than small-cell
carcinoma present (n Z 12)
5
5
4
Flat surface dysplasia or carcinoma in situ
Transitional cell differentiation
Focal glandular differentiation
Note that the above categories were not mutually exclusive.
within 6 months of presentation. The 2-year cancer-specific
death rate was 86% overall, and 70% for those receiving
local treatment. The only intercurrent death was in a patient
who died of heart failure at 39 months after radical
radiotherapy, with no evidence of recurrence. The six
radically treated patients had a median overall survival of
21 months, with one patient remaining alive, with no
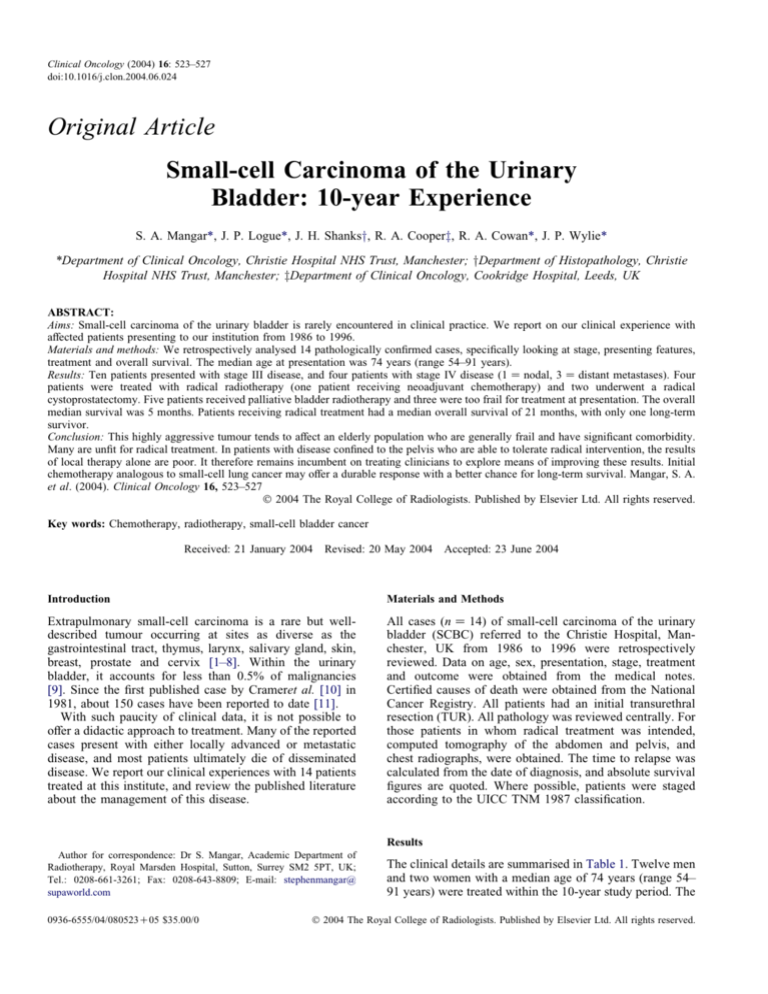
evidence of disease, 7 years after a radical cystoprostatectomy. The relationship between stage and overall survival
is shown in Fig. 1. The sites of relapse were varied and
included liver, brain, bone and lymph nodes.
Discussion
Primary small-cell carcinoma occurs at several sites along
the urinary tract [12], but the bladder is the most frequently
reported [13]. Bladder metastases from small-cell lung
cancer (SCLC) [14] are described, but are normally
associated with widely disseminated disease and should
be easily identified with staging investigations.
The pathology of SCBC is similar to that of SCLC.
There is normally positive staining for cytokeratin and
neuroendocrine markers (chromogranin, synaptophysin, or
both) [15]. However, as our study shows, these can
occasionally be negative. Neuron-specific enolase is almost
always positive, although this marker is not regarded as
specific. However, our study and others [15,16] have shown
that, unlike SCLC in SCBC, there is a higher proportion of
mixed small-cell and non-small-cell carcinoma. The nonsmall cell elements are typically urothelial or glandular,
with or without carcinoma in situ.
In keeping with other reports, this series confirms the high
propensity for metastatic spread and early death shown by
SCBC [15–17]. Three patients were so debilitated at
presentation that no treatment could be offered, and only
two patients were alive and disease-free 2 years after
treatment. Outcome is related to stage, and no patients with
stage IV disease survived beyond 6 months, with a median
survival of only 2 months in patients with extrapelvic
metastasis. Abbas et al. [7] compiled all the published cases
of SCBC in 1995, and estimated a 25% 2-year survival and
8% 5-year survival for patients with disease confined to the
pelvis. Although various treatment approaches were used,
most of the patients did not receive chemotherapy.
The correct treatment strategy for this rare tumour
remains unclear. However, there are analogies, in histology
and natural history, to SCLC where regimens containing
platinum are standard [18,19]. Review of the published
literature certainly suggests improved outcome when
chemotherapy is added to the local treatment of SCBC.
Dalpiaz et al. [20] analysed data on 139 reported cases.
Although the median survival was only 13 months, there
seemed to be an improved survival in people receiving
additional chemotherapy.
Blomjous et al. [15] reported five patients, predominantly
with advanced stage disease, who received chemotherapy
after local treatment. Various chemotherapy combinations
were used, but most were platinum-based. All ultimately
relapsed, but the median survival at the time of reporting
was 22 months. Grignon et al. [16] reported a series of 22
cases, of which eight received chemotherapy either as their
sole treatment or combined with cystectomy (63%) or
radiotherapy (13%). About 90% had advanced stage
(OT3b) disease. The precise details of scheduling of the
chemotherapy are not given, although combinations
containing platinum were used in most cases. Patients
Proportion alive (%)
100
80
T3
T4
60
Overall survival
Metastatic
40
20
0
0
10
20
Time (months)
30
40
50
Fig. 1 – Treatment outcomes: the relationship between stage and overall survival. Overall survival for all stages is compared with survival
according to specific stage at presentation.
526
CLINICAL ONCOLOGY
receiving chemotherapy had longer disease-free intervals
(range 10–77 months) compared with the remainder of the
group (range 1–28).
More recently, Lohrisch et al. [21] reported their experiences using chemotherapy, radiotherapy, or both, for 10 out
of 14 eligible patients presented to the British Columbia
Cancer Agency between 1985 and 1996. All patients had
disease confined to the pelvis. Four patients received three
to four cycles of chemotherapy, followed by local
radiotherapy; an equal number had concurrent chemoradiotherapy (the exact timing was not clearly documented)
after TUR. The remaining two patients were treated with
chemotherapy alone. The most commonly used regimen
was etoposide and cisplatin. The use of concurrent
chemoradiotherapy was not associated with an increase in
local morbidity. The 2- and 5-year actuarial survival for the
10 patients was 70% and 44%, respectively. These
impressive results, albeit for a selected group of patients,
provide optimism for a chance of long-term survival for
individuals with limited stage disease.
In deciding optimal local treatment, there are no direct
comparisons between cystectomy and radical radiotherapy.
Some investigators have suggested that cystectomy may be
preferred [16,22,23]. Dalpiaz et al. [20] reported that the
combination of surgery and chemotherapy resulted in 70%
of patients alive at median follow-up of 20 months
compared with 54% for patients receiving chemotherapy
and radiotherapy. Selection bias may explain these results.
By offering initial cystectomy, there is genuine concern that
chemotherapy will be delayed until the patient has sufficiently recovered. Using the analogy of SCLC, initial
chemotherapy followed by radical radiotherapy may be preferred. Within our series, isolated local recurrences occurring after radiotherapy seem rare, with only one case seen
in a patient who received palliative bladder radiotherapy.
Unfortunately, despite these presumed advantages to
using chemotherapy, this approach was not possible in most
patients reported in our series. Many of the patients were
elderly and frail as a result of their cancer, intercurrent
illness, or both, and were felt to be unlikely to tolerate
chemotherapy. Another concern is that patients may have
impaired renal function due to the site and bulk of their
disease, and this is likely to hamper administration of
nephrotoxic chemotherapy, such as cisplatin. Even simpler
chemotherapy schedules recommended for frail patients
with SCLC [24] may be too toxic in this particular group.
Conclusion
Small-cell carcinoma of the urinary bladder is a rare
tumour, and agreed treatment protocols are lacking. The
experiences of this and other series suggest that this is an
aggressive tumour that usually presents with an advanced
stage, with a pattern of spread similar to pulmonary smallcell carcinoma. Treatment schemes may be derived from
the analogy with SCLC. In suitably fit patients, we would
therefore recommend platinum-based chemotherapy followed by bladder radiotherapy if appropriate. However,
most patients present in such a frail state that this approach
will not be feasible, and palliative pelvic radiotherapy for
local symptom control would be more appropriate accepting that the patient is likely to soon develop disseminated
disease.
Acknowledgements. The authors would like to thank Mr N Clarke
and Mr V Ramani for help in providing the necessary database, and the
departments of Medical Illustration and Kostoris Library- Christie Hospital
for helping to research and prepare the manuscript. Acknowledgements
also to F Power, I Mangar, and R Mangar for their help in the final
preparation of this article.
References
1 Sarma DP. Oat cell carcinoma of the oesophagus. J Surg Oncol 1982;
19:145–150.
2 Wick MR, Schiethauer BW. Oat cell carcinoma of the thymus. Cancer
1982;49:1652–1657.
3 Porto DP, Wick MR, Ewing SL, Adams GL. Neuroendocrine
carcinoma of the larynx. Am J Otolaryngol 1987;8:97–104.
4 Gnepp DR, Wick MR. Small cell carcinoma of the major salivary
glands. An immunohistochemical study. Cancer 1990;66:185–192.
5 Taxy JB, Ettinger DS, Wharam MD. Primary small cell carcinoma of
the skin. Cancer 1980;46:2308–2311.
6 Yogore MGD, Saghal S. Small cell carcinoma of the male breast:
report of a case. Cancer 1977;39:1748–1751.
7 Abbas F, Civantos F, Benedetto P, Soloway MS. Small cell carcinoma
of the bladder and prostate. Urology 1995;46:617–630.
8 Sykes AJ, Shanks JH, Davidson SE. Small cell carcinoma of the uterine
cervix: a clinicopathological review. Int J Oncol 1999;14:381–386.
9 Blomjous CE, Thunnissen FB, Vos W, deVoogt HJ, Meijer CJ. Small
cell neuroendocrine carcinoma of the urinary bladder. An immunohistochemical and ultrastructural evaluation of three cases with a review
of the literature. Virchows Arch A Pathol Anat Histopathol 1988;413:
505–512.
10 Cramer SF, Aikawa M, Cebelin M. Neurosecretory granules in small
cell invasive cancer of the urinary bladder. Cancer 1981;47:724–730.
11 Alcala JA, Ripa Saldias L, Aldave Vllanueva J, et al. Neuroendocrine
small cell carcinoma of the bladder. Review of the literature and review
of a case. Arch Esp Urol 2002;55:452–456.
12 Morgan KG, Banergee SS, Eyden BP, Barnard RJ. Primary small cell
neuroendocrine carcinoma of the kidney. Ultrastruct Pathol 1996;20:
141–144.
13 Wu TT, Lee YH, Huang JK. Primary small cell carcinoma of the
urinary bladder: report of a case. J Formos Med Assoc 1995;94:
576–577.
14 Coltart RS, Stewart S, Brown CH. Small cell carcinoma of the
bronchus: a rare cause of haematuria from a metastasis in the urinary
bladder. J R Soc Med 1985;78:1053–1054.
15 Blomjous CE, Vos W, deVoogt HJ, Van der Valk P, Meijer CJ. Small
cell carcinoma of the urinary bladder. A clinicopathologic, morphometric, immunohistochemical, and ultrastructural study of eighteen
cases. Cancer 1989;64:1347–1357.
16 Grignon DJ, Ro JY, Ayala AG, et al. Small cell carcinoma of the
urinary bladder. A clinicopathological analysis of twenty two cases.
Cancer 1992;69:527–536.
17 Holmang S, Borghede G, Johansson SL. Primary small cell carcinoma
of the urinary bladder: a report of 25 cases. J Urol 1995;153:
1820–1822.
18 Spiro SG, Souhami RL, Geddes DM, et al. Duration of chemotherapy
in small cell lung cancer: a cancer research campaign trial. Br J Cancer
1989;59:578–583.
19 Bleehan NM, Girling DJ, Machin D, Stephens RJ. A randomised
trial of three or six courses of etoposide, cyclophosphamide
methotrexate and vincristine or six courses of etoposide and
ifosfamide in small cell lung cancer. Br J Cancer 1993;68:1150–
1156.
20 Dalpiaz O, Al Rabi A, Galfono A, et al. Small cell carcinoma of the
bladder: a case report and literature review. Arch Esp Urol 2003;56:
197–202.
SMALL-CELL CARCINOMA OF THE URINARY BLADDER
21 Lohrisch C, Murray N, Pickles T, Sullivan T. Small cell carcinoma of
the bladder. Long term outcome with integrated chemoradiation.
Cancer 1999;86:2346–2352.
22 Oesterling JE, Brendler CB, Burgers JK, et al. Advanced small cell
carcinoma of the bladder. Successful treatment with combined radical
cystoprostatectomy and adjuvant methotrexate, vinblastine, doxorubacin and cisplatin chemotherapy. Cancer 1990;65:1928–1936.
527
23 Podesta AH, True LD. Small cell carcinoma of the bladder. Report of
five cases with immunohistochemistry and review of the literature with
evaluation of prognosis according to stage. Cancer 1989;64:710–
714.
24 Girling DJ. Comparison of oral etoposide and standard intravenous
multidrug chemotherapy for small-cell lung cancer: a stopped multicentre randomised trial. Lancet 1996;348:559.