Treatment injury case study
advertisement

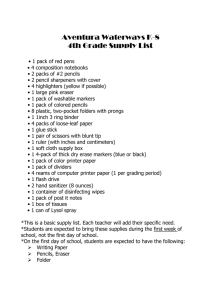
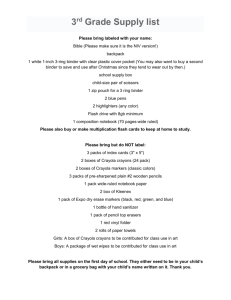
Treatment injury case study October 2010 – Issue 27 Sharing information to enhance patient safety Heat treatment EVENT: INJURY: Burns Case study Marcia, a 35-year-old expecting her second child, underwent a caesarean section after failing to progress in the second stage of a term labour. Her previous child had also been born by caesarean section at term, because of failure to progress. Marcia had experienced a first-trimester miscarriage previously, but had no other medical or obstetric history of note, and was taking no regular medication. The caesarean was performed under epidural anaesthesia through a Pfannenstiel (lower abdominal) incision, and was uncomplicated. A healthy baby boy was born with Apgars of 9 and 10 at one and five minutes respectively. The wound was closed in layers and a clear dressing applied. To reduce Marcia’s pain post-operatively, it was decided to leave the epidural in situ for 24 hours following the caesarean, then transition to oral analgesia. Overnight, Marcia began complaining of breakthrough pain. A nurse placed a heat pack on the abdominal wound to assist with pain relief. Key points • Do not use heat therapy if: - a patient has an impaired ability to feel pain - you can’t be sure that the temperature of the heat pack is safe (it’s best to use a disposable chemical heat pack, which has a specified maximum temperature) • When using heat therapy, keep a thick layer (such as a towel) between the heat pack and the patient’s skin • Do not apply the heat pack for more than 15-30 minutes • Closely monitor the patient’s skin integrity throughout, and don’t let the patient fall asleep while the heat pack is applied. 330383-PressFile.indd 1 When the heat pack was checked 90 minutes later, there was a 10 x 8 centimetre red, scalded area where the pack had been placed on Marcia’s abdomen. A cold compress was immediately applied to the burn and the obstetric registrar was called. Because of the burn’s size, the registrar immediately requested plastics review. Following review by the plastic surgery registrar, the burn was dressed appropriately by the nurse. Fortunately skin grafting wasn’t necessary, but Marcia did require a number of outpatient plastics appointments on discharge, as well as district nursing care. A treatment injury claim was made on Marcia’s behalf, which was accepted. ACC was able to assist with the costs of the prolonged treatment Marcia received for the burn. Expert Commentary Karen McBride Henry RN, PhD The application of heat as a therapeutic intervention (also known as heat therapy) is commonly used by both midwives and nurses (1). Evidence indicates that heat therapy may be beneficial for conditions such as back pain (2,3). However, despite its frequent use in practice, there’s little research or information available to inform professional decision-making (1,4). What we do know is that those most at risk from thermal injuries related to heat therapy are infants, children and the elderly (5). There are also a number of contraindications for heat therapy, including: • potential for haemorrhage • impaired mental acuity • slow or altered reaction times 30/09/10 12:28 PM Case study • bedridden patients • placement of heat packs where ointments have been applied • poor skin integrity • impaired ability to feel pain (1,4,5,6). The last point above is relevant to Marcia’s case – as her caesarean had been performed under epidural anaesthetic, she should not have been given heat therapy. The seminal work on the relationship between cutaneous burns, surface temperature and exposure time was conducted by Moritz and Henriques in 1947 (7). They found that the temperature of 44°C marks a critical point. Above this temperature, the rate at which human skin burns nearly doubles for each degree rise in temperature. Below 44°C, progressively longer contact time is required for each degree fall in temperature for burning to occur. Heat therapy requires a temperature of at least 40°C to be beneficial, but should not exceed 44°C (1). For neonatal, paediatric and elderly patients, heat therapy should only be used at the lower end of this range because of the increased risk of burns. The sensitivity of various tissues to burning varies (8), which means that monitoring the efficacy and impact of heat treatment can be problematic. Experts offer the following recommendations for practice (1,4,6,9): • heat therapy should only be used if you can be sure of the heat pack’s temperature (disposable chemical heat packs are the gold standard, because they achieve preset maximum temperatures) • it is not advisable to warm heat packs (including towels and washcloths) in microwaves, which heat their contents unevenly – also, differing wattages between microwaves add a further source of risk • hot water should not be used to heat packs either, because of the inability to measure the temperature accurately How ACC can help your patients following treatment injury • always explain the purpose and procedure of heat therapy to the patient and/or their family • keep a thick layer (such as a towel) between the heat pack and the patient • make sure the heat therapy can be easily removed by the patient or family • don’t apply the heat therapy for more than 15-30 minutes • closely monitor the patient’s skin integrity throughout the procedure • don’t let the patient fall asleep while the heat pack is on the skin • remove the heat pack immediately if any signs of adverse reaction are noted, including changes in skin colour or blistering • document the type, method and duration of therapy, as well as the patient’s response to it (including their skin condition before and after therapy). References 1. Ebbinghaus S, Kobayashi H. Safe heat application for pediatric patients: a hot item. J Nurs Care Qual 2010; 25(2):168-175. 2. Chou R, Hoyt Huffman L. Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007; 147:492504. 3. French S, Cameron M, Walker B, et al. Superficial heat or cold for low back pain. Cochrane Database of Systematic Reviews 2006; 1: Art. No.: CD004750. 4.Chandler A, Preece J, Lister S. Using heat therapy for pain management. Nurs Stand 2002; 17(9):40-42. 5. Bjerke D. Considerations for thermal injury: The elderly as a sensitive population. Chapter 16. In Farage M, Miller H, Maibach (eds.), Textbook of ageing skin. Berlin: Springer-Verlag, 2010; 159-172. 6. Barillo D, Coffe E, Shirani K, et al. Burns caused by medical therapy. J Bur Car & Rehab 2000; 21(3):269-273. 7. Moritz A, Henriques F. Studies of Thermal Injury: The relative importance of time and surface temperature in the causation of cutaneous burns. Am J Pathol 1947; 23:695-720. 8.Field S, Morris C. The relationship between heating time and temperature: its relevance to clinical hyperthermia. Radiotherapy and Oncology 1983; 1(2):179-186. 9. Metules TJ. Hands-on help: hot and cold packs. RN. 2007; 70(1):45-48, 50. Claims information Between 1 July 2005 and 30 June 2010, ACC received 332 treatment injury claims for burns, of which 230 (69%) were accepted. Some claims involved significant burns, requiring prolonged and extensive treatment. Of the accepted claims, the most common types of treatment responsible for injury were heat therapy, liquid nitrogen, dental treatment and laser treatment. The most common reason for declining claims for burns was that the injury was determined to be an ordinary consequence of the treatment. These sorts of claim were in relation to minor, superficial burns from cryotherapy, and localised burns caused by radiotherapy. Many patients may not require assistance following their treatment injury. However, for those who need help and have an accepted ACC claim, a range of assistance is available, depending on the specific nature of the injury and the person’s circumstances. Help may include things like: • • • contributions towards treatment costs weekly compensation for lost income (if there’s an inability to work because of the injury) help at home, with things like housekeeping and childcare. No help can be given until a claim is accepted, so it’s important to lodge a claim for a treatment injury as soon as possible after the incident. This will ensure ACC is able to investigate, make a decision and, if covered, help your patient with their recovery. About this case study This case study is based on information amalgamated from a number of claims. The name given to the patient is therefore not a real one. The case studies are produced by ACC’s Treatment Injury Centre, to provide health professionals with: • • an overview of the factors leading to treatment injury expert commentary on how similar injuries might be avoided in the future. The case studies are not intended as a guide to treatment injury cover. Send your feedback to: TI.info@acc.co.nz ACC5536 Printed October 2010 ©ACC 2010 330383-PressFile.indd 2 30/09/10 12:28 PM