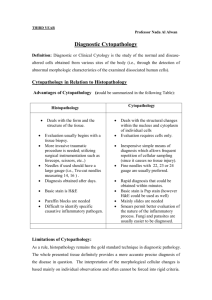
CHAPTER NINE CYTOPATHOLOGY
advertisement

CHAPTER NINE CYTOPATHOLOGY CLINICAL CYTOLOGY (DIAGNOSTIC CYTOLOGY) This is the study of normal & abnormal morphologic characteristics of human cells. Differences between histopathology and cytopathology Histopathology 1. Deals with the form & the structure of the tissue. 2. Evaluation usually begins with biopsy Clinical cytology 1. Deals with the structural changes in the nucleus & cytoplasm. 2. Evaluation requires cells only Collection of materials for cytology: 1. From normal (physiological) desquamation products, examples include - Bronchial secretion (sputum) - Urine - Vaginal, cervical and endometrial secretion - Nipple discharge 2. By superficial scraping of the lesion (artificial mechanical desquamation) including - Cervical scraping or smear - Buccal mucosal smear - Direct imprint of a tumor - Skin scraping (Note: Pap smear is used for early detection of cervical cancer in cervix). 3. Fine needle aspiration (FNA) including that of - Pathologic mass (tumor or tumor-like mass) for example nodules of the thyroid and breast masses; this is to help differentiating between benign and malignant lesions. - Accumulated fluid within anatomical cavity, for example the pleural, peritoneal and pericardial aspirates. - Enlarged lymph nodes (lymphadenopathy) 4. Brush cytology (during fiber-optic endoscopy); this is considered as mechanical exfoliation (desquamation). Cytological techniques - The materials obtained from the above techniques (e.g. exfoliation, fine needle aspiration, etc.) are smeared on microscopic slide. - In preparation for Papanicoloau staining, fixation is through 95% ethyl alcohol. - Smears for May-Grunwald Giemsa staining are air-dried (fixed by air drying). In the evaluation of a smear the cytologist is looking for the following changes 1. Modification of normal nuclear & cytoplasmic structures - for example, the stratified squamous epithelium consists of several layers and the cells in each layer has a definite shape , so we see if there is any change. (Fig. 9-1) - Changes occur in inflammation, hyperplasia, precancerous lesions (dysplasia) & cancer. 2. Maturation status i.e., see if the cells are mature or immature. 3. The quantity of the cells (i.e., if the smear is hypo- or hypercellular) (Fig. 9-2) & their mode of desquamation (scattered as clusters, sheets or individually). 4. The abnormal presence of leukocytes, histiocytes, RBCs for e.g. the urine is normally free of pus (leukocytes) and RBCs, so if there is a change (inflammation, calculi, parasite, or tumor) these cells (pus, RBCs) may appear in urine. Hematuria (RBCs in urine) for e.g. occurs in Bilhariziasis, calculi as well as in the presence of tumors (both benign and malignant). The advantages (values) of cytologic examination 1. Evaluation of the gonad’s hormonal activity for e.g. in vaginal smears the desquamated cells are under the influence of ovarian hormones. (Fig. 9-3) 2. Detection of inflammatory lesion & their causes for e.g. the cause of vaginal secretion is vaginitis due to Trichomonus vaginalis or moniliasis. Similarly the cause of cystitis may be Bilharzial and this is established through the detection of Bilharzial ova in smears of urine samples. 3. Detection of precancerous and cancerous cellular changes. No tumor occurs suddenly; there are precancerous steps that are manifested by the presence of dysplastic cells. Dysplasia may be graded as mild, moderate, & severe. All of these are precancerous modifications (for example in the cervix uteri) (Fig. 9-4) that may regress or progress to invasive malignancy, but can be eliminated (treated) by excision. Similarly carcinoma in situ (pre-invasive stage) can be treated by excision. However, if invasion occurs, radical and drastic surgery (hysterectomy with bilateral salpingo-oophorectomy) will be required. 4. Identification of neoplastic cells in primary, metastatic (secondary) or recurrent tumors: - Detection of primary cancers e.g. sputum containing blood (hemoptysis) could be due to for e.g. T.B. or cancer. Cytological examination can differentiate between these two. - Secondary (metastasis) for e.g. through the detection of cancerous cells in cavity fluids. The fluid in pleural cavity after breast cancer removal may contain metastatic cancerous cells in the pleural cavity; in this case we will see the malignant cells in the pleural fluid. - Recurrent tumor. It is important to follow-up the patient after the removal of his/her cancer through the checking the local area from which the tumor has been removed. Patients with carcinoma breast may develop nodules at the site of mastectomy scar. FNA of the nodule may reveal cancerous cells and in such a case this signifies recurrence. Alternatively the nodule may be due to a stitch granuloma or fat necrosis (as a result of surgery trauma). 5. Follow –up of cancer cases treated by radiation or by chemotherapy. 6. The identification of sex chromosome Sometimes a baby is born with ambiguous genitalia and one can not tell whether the sex is male or female; this is an important differential to achieve in a newborn child. - The presence of a dark dot attached to the nuclear membrane from inside (Barr body +ve) indicates that a sex chromosome is present i.e. the genotype of the baby is XX (♀). - Conversely the absence of the spot (Barr body) indicates that there is no X chromosome i.e. the newborn is genotypically a male so (XY; male; ♂). - If the appearance (phenotype) of the individual is that of a male; the presence of a Barr body (+ve) indicates XXY genotype (male; ♂); this is called Klinefelter’s Syndrome. (Fig. 9-5) In this case the male is infertile. THE DIAGNOSIS OF CELLULAR MALIGNANCY There are certain structural changes (modifications) of the cells that may be present in all types of human cancer; the presence of these allow cytological diagnosis of malignancy 1. Nuclear enlargement that leads to increased N/C (Fig. 9-6) and (Fig. 9-7) 2. Hyperchromatism; this is due to increased chromatin materials. Not only this but in malignant cells the chromatin is not evenly distributed within the nucleus; it is also distributed as coarse clumps (Fig. 9-8). This in contradistinction to normal cells, which have evenly distributed chromatin i.e., vesicular nuclei. 3. Abnormal mitosis; malignant nuclei may show multiple poles e.g. three poles (tripolar mitosis; triploidy) or four poles (tetrapolar mitosis; tetraploidy). This is abnormal since normal mitosis has two poles (bipolar). Thus normal cells show diploid pattern on flow cytometry whereas malignant cells show aneuploid pattern. 4. Irregular outline of the nucleus this is due to the increased amount of nuclear chromatin that pushes the nuclear membrane irregularly ahead of it i.e. forming bulges. (Fig. 9-9) 5. Prominent nucleolus (Fig. 9-10); giant nucleoli or multiple nucleoli may present that differ in their size. It should be remembered, however, that normal columnar and goblet cells may contain 2 nucleoli. 6. Multinucleation: malignant cells may contain more than one nucleus (Fig. 9-11) but some normal cells such as hepatocytes and histiocytes may contain more than one nucleus. However, multinucleated malignant cells differ from nonmalignant multinucleated cells by the fact that the nuclei of malignant cells are unequal in size (in contrast to that of normal cells) & display features of malignancy. 7. Enlargement of the cell as whole. 8. Variations in cells shape It should be noted that not all the above criteria can be demonstrated in a malignant cell. Conversely, the demonstration of one criterion is not enough to make the diagnosis of malignancy because many normal cells may contain one or more of the listed criteria above e.g. hyperchromatism may occur in cases of hyperplasia. FINE NEEDLE ASPIRATION CYTOLOGY (FNAC) In general, the definitive diagnosis of a breast lump can be established by open biopsy, tissue core biopsy (Trucut) & Fine needle Aspiration (FNA) Biopsy. Compared to FNA, Tru-cut biopsy is a more traumatic procedure which should be performed under local anesthesia. It requires more time & special equipments that are more expensive. Pain, discomfort & bleeding are common complications. FNAC, on the other hand, provides many advantages to the surgeons. It is an easy, non-invasive, reliable, & cost effective diagnostic technique that can give rapid results within even 15 minutes. The procedure could be performed in an office setting without anesthesia. It is usually not more painful than a venipuncture & can be repeated immediately if the acquired material is inadequate. The National Health Service Breast Screening Program (NHSBSP) displayed that many centers wished to include FNA as an additional test to provide preoperative diagnosis of breast cancer & to reduce the number of operations for benign breast diseases. History of the Technique Despite its early employment in the USA as first documented by Martin & Ellis in 1930, yet FNA has been primarily popularized after its use in Sweden. The Swedish success has been shaped by the clinical cytopathologists since the majority of FNAs were procured there, by the same person who analyzed the preparations. Karolinska Hospital became a leading center for FNAC. Dr. Sixten Franzen, a radiotherapist, was largely responsible for the upsurgence of the technique, together with Dr. J. Zajicek & Dr. T. Lawhagen (cytopathologists). Prof. Lawhagen was instrumental in setting up the aspiration clinic at the Karolinska Hospital & thereby establishing a worldwide model for this kind of clinics manned by cytopathologists. Procedure When reduced to its simplest terms, FNAC consists of: 1. Using a needle & a syringe to remove material from a mass 2. Smearing it on a glass slide 3. Applying a routine stain 4. Examining it under the microscope (Fig. 9-12). The skin over the palpable mass is sterilized with an antiseptic. Utilizing the index & the middle finger or the thumb & the index finger, the mass is localized with the non-dominant hand. With firm downward pressure on the skin over the mass, it should be compressed against a rib & stabilized. Aspirates should be obtained using preferably a 23 gauge, 1 ½ inch disposable needle mounted on a 10 ml plastic syringe, held by the dominant hand. Larger needles (22 gauges) are used in aspirating material from hard fibrous masses & in cases of suspected cysts. Without using anesthesia, the needle should be gently introduced through the skin passing to the level of the dominant mass. Having confirmed the position of the needle within the mass, negative pressure should be created within the syringe by pulling back the plunger. Next begins the process that is probably responsible for the generous sampling with the thin needle, which is the hallmark of FNA. The needle should move back & forth through the mass, in different rotational directions using sewing-like-motion. Suction should be maintained throughout the process by outward pressure of the right thumb on the underside of the syringe. By this method the needle can cut loose many small pieces of tissue that are then readily aspirated due to the suction applied by syringe. These to & fro strokes should be repeated at least 6-8 times. In general most of the aspirations are terminated when material begins to appear in the needle hub. The following step should be designed to protect the material that has been obtained. All suction should be released before removing the needle from the mass. This is accomplished by allowing the syringe plunger to return gently to its resting position. Then the needle should be withdrawn gently from the mass & the breast. To limit haematoma formation, from the site of the puncture, firm pressure should be applied with a piece of cotton for two minutes. Equipments 1. Syringes The key feature in a syringe is lightness in weight, adequate in volume, & one hand control. Modern sterile disposable plastic syringes are perfect for use in FNAC. Most practitioners use the 10 cc size, while some prefer the 20 cc size (specifically when a cyst is suspected). 2. Needles Several variables should be considered in choosing the proper length & gauge. In general the length should be at least 1.5 inch (3-8 cm). This is desirable in the breast because many lesions are found deeper than expected. It has also been demonstrated that small gauges (22-23) are preferred. , since they are rigid enough & at the same time cause less sensation & haematoma. Needles with a plastic hub rather than a metal hub are preferred as well. This permits the aspirator to monitor the recovery of tissue, blood or other fluids as they appear in the hub. 3. Glass Slides Common routine slides measure 75 mm X 25 mm X 1mm. An important procedure is slide labeling at the time of sampling. That is why slides which have one frosted end are preferred. Various substances are used to increase the adherence of specimens to the slide surface, the most commonly used being albumin. 4. Fixatives These are applied to the smears as a spray or by immersion of the slide into a liquid. The most commonly used is 95 % Ethanol. This inexpensive readily available liquid provides excellent cytological details. Its only disadvantage is the need to store & transport slides in a container of liquid & to have them immersed in for at least 20 minutes. 5. Routine Stain For cytological diagnosis, fixed material is usually stained by Papanicolaou Stain (which is preferred) or by Hematoxylin & Eosin (H&E) method. Both employ one of the Hematoxylins for staining of the nuclei. This dye colors the nucleic acids as a dark purple blue color. The counter staining with Eosin is designed to show cytoplasmic characteristics. With the Pap stain one hallmark is the use of Orange-G, which stains cytoplasmic keratin with a bright orange color. Air-dried smears on the other hand are usually stained by any Romanowsky stains, which are various combinations of methylene blue & its breakdown products (Azure A, B, &C) with Eosin. Most rely on Methanol fixation. Papanicolaou Stain All slides should be wet fixed with in 95% Ethanol: 95% ethanol 10 dips 80% ethanol 10 dips 70% ethanol 10 dips 50% ethanol 10 dips Distilled water 10 dips Hematoxylin Stain 1-2 min. Running Tap water 10 dips 50% ethanol 10 dips 70% ethanol 10 dips 80% ethanol 10 dips 95% ethanol 10 dips Eosin Stain 2 min. 95% ethanol 10 dips Orange-G Stain 2 min. 95% ethanol 10 dips 95% ethanol 10 dips Absolute ethanol 10 dips Absolute ethanol: Xylol (50:50 mixture) 5 min. Xylol 20 min. Mount with Canada Balsam Pitfalls to Reliable Results from FNAC No Mass Vague Mass Mass being too Small (less than 1 cm) Mass being too Deep Gross Blood into the Syringe (RBCs can mask the picture) Scanty Cellularity in the aspirated Mass Dense Fibrosis Gross Fluid into the Syringe - False Positive Reports should be 0 (or less than 0.1%) - False Negative Reports should be less than (5-7%) of cancers (Usually associated with attempted diagnosis on too few cells)