Examination Content Specifications and
Clinical Experience Requirements
for ARRT Certification in
Vascular Interventional Radiography
Vascular Interventional Radiography
Practice Analysis
July 2012
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
TABLE OF CONTENTS
CHAPTER 1: PROJECT BACKGROUND AND METHODOLOGY .........................3
Introduction .............................................................................................................3
Practice Analysis Methods .......................................................................................3
Advisory Committee ................................................................................................5
Project Schedule ......................................................................................................5
CHAPTER 2: SURVEY METHODS ..........................................................................7
CHAPTER 3: DATA ANALYSIS AND RESULTS ....................................................8
Overview .................................................................................................................8
Data Analysis Techniques ........................................................................................8
Staff Questionnaire Results ......................................................................................8
CHAPTER 4: REVISION OF TASK INVENTORY, CONTENT SPECIFICATIONS,
AND CLINICAL EXPERIENCE REQUIREMENTS ......................... 11
Overview ............................................................................................................... 11
Finalization of Task Inventory ................................................................................ 11
Updating the Content Specifications ....................................................................... 13
Revision of the Clinical Experience Requirements .................................................. 15
APPENDICES
APPENDIX A:
APPENDIX B:
APPENDIX C:
APPENDIX D:
APPENDIX E:
APPENDIX F:
Prototype of the Staff Questionnaire
Results of the Staff Questionnaire
Final Task Inventory
Final Content Specifications
Final Clinical Experience Requirements
References
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 3
C HAPTER 1
PROJECT B ACKGROUND AND M ETHODOLOGY
Introduction
In the past, the content of most certification exams was closely linked to the curriculum of
educational programs or to the table of contents of a prominent textbook. In the late 1970s and early
1980s, certification boards and testing professionals began to realize that certification requirements
should be closely linked to the requirements of practice. It is now recognized that the content of
certification exams should be determined only after systematically studying and identifying the activities
performed in work settings. Enrichment topics, such as the history of a profession, should not be tested on
a certification exam unless these topics are clearly job-related (NCHCA, 1979).
The job-relatedness of an examination is generally established through a job or practice analysis
(AERA, APA, NCME, 1999). Practice analysis is useful for determining the topics to be covered by an
examination and the degree of emphasis that each topic receives. The Standards for Educational and
Psychological Testing (AERA, APA, NCME, 1999) and the National Commission for Certifying
Agencies (NCCA, 2004) outline the rationale for job or practice analyses. Legislative activity and legal
precedence also stress the importance of practice analysis in the development and validation of
certification exams. The Uniform Guidelines on Employee Selection adopted by the U.S. Equal
Employment Opportunity Commission, Department of Labor, and Department of Justice also indicate
that practice analysis is critical in the development of examinations related to employment (EEOC, 1978).
Practice analysis is equally critical for establishing other types of certification requirements such as
educational standards, experience requirements, and other eligibility criteria.
In 1980, the ARRT initiated its first large-scale effort to systematically document the job
requirements of entry-level personnel in the areas of Radiography, Nuclear Medicine Technology, and
Radiation Therapy (Reid, 1983). Since the original project was completed, the ARRT has conducted
practice analyses for those and other disciplines periodically for the purpose of updating the task
inventory and content specifications. Such updates are important for professions that continually evolve
due to advances in technology, because they help ensure that the content specifications and other
certification requirements (e.g., clinical competency requirements) reflect current practice 1.
Practice Analysis Methods
Practice analysis studies can be conducted in a variety of ways (Raymond, 2001). These methods
include direct observation, the use of work diaries, the use of task inventory questionnaires, and by logical
analysis—i.e., convening panels of experts and eliciting their opinions about practice responsibilities. The
choice of a practice analysis method can be influenced by a number of factors including, but not limited
1
Since 2005, the ARRT completes an interim update to content specifications and clinical competency requirements
every three years; a thorough and comprehensive practice analysis is conducted every nine years for post -primary
programs.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 4
to, previous studies, the size of the profession, and the amount of resources available to conduct the study.
These factors affect various decisions on how to conduct the study. Perhaps the two most important
decisions pertain to: (a) the type of practice-related information that is obtained; (b) the source(s) of that
information.
Type of Information. Practice analysis involves reducing to words the things people do in work.
One can describe work in terms of the behaviors necessary to complete a job, solve some problem, or
create an output, product, or service. For example, the statement “verify that informed consent has been
obtained” is a task-oriented descriptor. On the other hand, person-oriented approaches to job analysis
focus on the knowledge, skills, and abilities (KSAs) that a person should possess to successfully complete
the tasks required of a job. “Knowledge of radiation physics” is an example. Task-oriented descriptors
indicate the activities performed on the job, while person-oriented descriptors reflect the KSAs and other
personal characteristics presumed to be required for successful job performance. Practice analyses can
collect information about tasks/activities, about personal qualities, or both.
Sources of Information. Practice-related information can come from various sources. Physician
requisitions, patient charts, and billing statements all document what occurs in the practice setting. Most
practice analyses, however, obtain data directly from people who are knowledgeable about the work. This
could include practitioners, supervisors, managers, educators, or committees of subject-matter experts
(SMEs). The source of information will influence both the method of data collection and the sample size.
Method for Present Study. The results of this study helped develop a task inventory, establish
clinical experience requirements, and develop exam content specifications. These multiple needs required
data from multiple sources. Although the study could be completed by a committee of SMEs, we relied
on three independent sources of information. We first collected data regarding work activities from staff
vascular interventional (VI) radiographers with a task inventory questionnaire. Questionnaire recipients
indicated the frequency that the task was performed. The task inventory questionnaire is an efficient way
to obtain extensive information about the nature of a profession. It is also conducive to statistical analyses
that can help determine which tasks to include and which to exclude. The task inventory is consistent with
the methodology employed for previous ARRT studies. Once data about specific work activities was
collected, a committee of SMEs met to provide judgments regarding the KSAs required to perform those
activities. Finally, we conducted an analysis of data from the Centers for Medicare and Medicaid Services
in order to validate the survey results. In short, the present study relied on staff vascular interventional
radiographers to find out what is done on the job, confirmed the data gathered with an outside data source,
and SMEs revised the clinical experience requirements and exam content specifications.
The report is organized as follows. The remainder of this chapter discusses the establishment of the
Advisory Committee (i.e. SMEs) and summarizes the project schedule. Chapter 2 discusses details related
to questionnaire development and administration, while Chapter 3 presents the results. Finally, Chapter 4
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 5
describes procedures for translating the results of the questionnaires into the VI task inventory, content
specifications, and clinical experience requirements.
Advisory Committee
For comprehensive practice analyses, the ARRT Board of Trustees establishes an Advisory
Committee for the purposes of providing guidance to project staff by reviewing the plans for the conduct
of the study, revising documents as required, and by evaluating the results of all data collected during the
project. Based on the results of its deliberations, the Advisory Committee makes recommendations to the
Board of Trustees concerning the final composition of the task inventory, content specifications, and
clinical experience requirements. The individuals serving on the Advisory Committee included:
Advisory Committee
Kenneth A. Brasfield, R.T.(R)(CT)(VI)
Jeffrey D. Kins, R.T.(R)(VI)
Jennifer B. Levesque, B.S., R.T.(R)(CV)(VI)
Paula Pate-Schloder, R.T.(R)(CV)(CT)(VI)
Jason L. Scott, R.T.(R)(VI)
Jeff Crowley, R.R.A., R.T.(R)(VI)
ARRT Staff
Julie Hammons, B.S., R.T.(R)(CT)(ARRT)
Ben Babcock, Ph.D.
Teresa L. Vatterott, B.A., R.T.(R)(CV)(CI)(ARRT)
Project Schedule
Projects such as this require a closely monitored time schedule to ensure that all activities are
completed in a timely fashion and within budget. The following table presents the time and task schedule
used to guide this project.
Schedule of Activities
July 2010 - July 2012
Approx.
Date
Activity
July/Aug
2010 BOT
meeting
Board appoints members to the VI PA Advisory Committee. Staff mails appointment
letter, contract, and proposed dates for meeting.
Upon return
of contract
Welcome letter with date of first meeting, Designation of Beneficiary Page, Executive
Travel Profile Form, Serving the Profession Through ARRT Committees Brochure and a
Time and Task Schedule.
Sept 2010
Staff compiles existing task inventory and other materials for Advisory Committee
review.
Sept 2010
Advisory Committee reviews materials and makes notes regarding additions to task
inventory; discusses appropriate terminology.
* Oct/Nov
2010
Advisory Committee meets to review and update task inventory and also discuss
questionnaire content and format.
Oct/Nov
2010
Staff prepares first draft of questionnaire and mails to Advisory Committee for review.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 6
Approx.
Date
Activity
Oct/Nov
2010
Advisory Committee members contact staff to discuss questionnaire changes.
Nov 2010
Staff prepares final draft of questionnaire; submits for internal editorial review.
December
2010
Staff prepares questionnaire copy and sends to a questionnaire vendor for printing.
December
2010
Questionnaire vendor returns questionnaire for final proof.
January 2011
Questionnaire vendor mails questionnaires to large sample of technologists.
x
initial mailing
x
thank you/reminder post card with information to request a questionnaire
February
2011
Questionnaire vendor returns final comprehensive data file.
March 2011
Psychometrics Team analyzes data, prepares preliminary report, and the report is mailed
to the Advisory Committee.
* April 2011
Advisory Committee meets to 1) review questionnaire results, 2) finalize new task
inventory, 3) perform Task-Content Area mapping procedure, 4) develop initial clinical
experience requirements, and 5) develop initial content specifications.
July 2011
Board of Trustees approves the task inventory.
July/Aug
2011
Draft clinical experience requirements and content specifications mailed to professional
community and posted on ARRT.org for review and comment.
Sept 2011
Staff collates comments from professional community.
*October
2011
Advisory Committee meets to review public comments and finalize content specifications
and clinical experience requirements. Committee also reclassifies items in item bank.
January 2012
Board reviews and approves clinical experience requirements and content specifications.
April 2012
Exam Committee meets to assemble test forms according to new content specifications.
July 2012
Revised content specifications and clinical experience requirements placed into 2012
Candidate Handbooks and on ARRT.org.
* Indicates committee meeting
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 7
C HAPTER 2
SURVEY METHODS
The staff and Advisory Committee developed a questionnaire during November 2010. The
questionnaire consisted of tasks and equipment thought to relate to VI radiography. It was loosely based
on the activities comprising the ARRT task inventory in use since 2008.
Staff VI Radiographer Questionnaire Development. The staff questionnaires consisted of 105
clinical activities thought to be performed by VI radiographers. The questionnaire did not include all
possible activities, but was limited to those for which the Advisory Committee felt there was some benefit
to obtaining information. Some tasks involving general patient care and radiation protection were not
included because they are covered in ARRT’s Radiography exam, which one must first pass before
applying for the Vascular-Interventional certification. Activities known to be performed by virtually all
VI radiographers were excluded as a means to control questionnaire length, and this fact was explained in
the questionnaire instructions. The rating scale for the clinical activities related to the frequency with
which each activity was performed. The rating scale included six response categories: not responsible for
performing, yearly, quarterly, monthly, weekly, and daily. Instructions asked respondents to indicate
“approximately how often you perform” each activity.
The second part of the questionnaire consisted of 16 questions on education, experience, and
workplace demographics. Appendix A contains a prototype version of the questionnaire.
Staff VI Sample. ARRT staff compiled names and addresses for study participants from ARRT’s
database of registered technologists of people indicating that VI radiography was their primary modality
of work and also indicated that they had been working in VI radiography for 5 years or less. The
population of interest included 3,499 radiographers, not necessarily VI certified, working in the United
States. A random sample of 1,000 of these radiographers was sampled, stratified on self-reported years of
experience.
ARRT staff mailed the questionnaire in January 2011 to the sample of 1,000 VI radiographers. The
ARRT employed a two-stage mailing strategy, which consisted of an initial mailing followed by a thank
you / reminder post card after two weeks. A total of 327 useable questionnaires were returned within a six
week period. The next chapter presents results from the questionnaire.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 8
C HAPTER 3
D ATA A NALYSIS AND R ESULTS
Overview
This chapter summarizes the results of the questionnaire completed by VI radiographers. The
demographic characteristics are first, followed by discussions of the results for the clinical activities and
equipment. All tables corresponding to the staff questionnaire results appear in Appendix B.
Data Analysis Techniques
This report contains three different ways of analyzing the frequency with which each activity was
conducted. The first was to look at the percentage of respondents who indicated that were responsible for
the activity. The second data analysis technique was the Bradley-Terry-Luce (BTL, Bradley & Terry,
1952; Luce, 1959) paired comparisons model. Finally, ARRT staff compared the frequency rankings from
the BTL model to the procedure frequency rankings extracted from data from the Centers for Medicare
and Medicaid Services (CMS).
The percentage of respondents who indicated that they were responsible for an activity is a good
indicator of whether or not to include an item on the final task list. If enough people do not conduct an
activity in clinical practice, then the activity in question may not be included in the final task list or
content specifications. These numbers are also informative as to which tasks should and should not be
required for clinical experience requirements.
The BTL (Bradley & Terry, 1952; Luce, 1959) paired comparisons model analysis used all of the
response categories in order to come up with an overall task frequency rating for the 105 clinical
activities. In order to use the model, the staff broke down every possible pairing of activities for every
respondent into a single decision of which activity the respondent rated as doing more often. A coin flip
method decided which activity was greater if the two ratings tied. The BTL analysis then calculated the
ordered frequency locations of the activities. The final ratings were the mean of 10 replications in order to
protect against chance variation in the coin flip decision method.
The CMS data comparison is a good way to validate the results of a practice analysis
questionnaire (Babcock & Yoes, in press). If the CMS data and the data gathered using the VI
questionnaire match closely, then there is evidence that the questionnaire data are good. Areas of
disagreement would require further investigation.
Questionnaire Results
ARRT certification exams assess the knowledge and cognitive skills required to carry out the major
tasks typically required at entry into a discipline. Entry-level is generally interpreted by ARRT as 1 to 5
years of experience working in the post-primary discipline of interest. Because a few more experienced
VI radiographers were also included in the sample due, it seemed worthwhile to also evaluate their
responses. The differences between the entry-level respondents and the more experienced radiographers
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 9
concerning task responsibility were generally quite small. Therefore, the results are presented for the full
group.
The following text summarizes the demographic characteristics of the sample based on responses to
Section 2 of the questionnaire (Tables B.1.). This is followed by analyses of the practice activities section
of the questionnaire (Table B.2.).
Demographics. Tables B.1. summarize the demographic responses of those taking the questionnaire.
Note that the questions and responses that appear in the tables may have been abbreviated; the
questionnaire in Appendix A presents the full text of each question. Notable findings are discussed below.
x
Nearly all respondents were employed in a hospital or medical center (92.3%). Those working in
hospitals indicated most often that they worked in hospitals with 251 to 500 beds. The number of
VI radiographers in the department varied greatly, with relatively high percentages of respondents
in all categories. Most respondents (88.2%) had the job title of staff technologist.
x
Virtually all respondents reported having at least one VI nurse. A large percentage of people
(42.5%) indicated having 7 or more VI nurses. When matching these results to the number of VI
radiographers in a department, it appears that there are slightly more VI nurses than VI
radiographers on average in the workplace.
x
Respondents reported spending the largest amount of time in VI. Respondents spent relatively
little time in any other modality. This was particularly the case for CI, as 80% of respondents
reported spending no time in cardiac-interventional radiography. Respondents reported working
most often with interventional radiologists, vascular surgeons, and general radiologists.
Practice Activities Results. Table B.2 presents the details for each of the 105 clinical activities
appearing in section 1 of the questionnaire. For each of the practice activity questionnaire items, we report
the percentage of respondents who responded in the highest category (Daily), the percentage of
respondents who responded as not responsible, and the percentage of people who responded as having
some sort of responsibility (Yearly, Quarterly, Monthly, Weekly, and Daily combined). We also report
the percentage of missing responses. Finally, we report the BTL score, with higher numbers indicating
higher frequency. The staff scaled the BTL scores to have a mean (average) of 0. Note that the questions
and responses that appear in the tables have been abbreviated; the questionnaire in Appendix A presents
the full text of each question.
Some procedures were deleted from the task list based upon the 2003 comprehensive questionnaire
and 2008 interim questionnaire. They were included in this 2011 questionnaire to tack trends or changes
in practice. The committee recommended keeping a watch on tasks related to pulmonary procedures,
ionic contrast, venous sampling, and preparation of equipment for sterilization.
Primarily, any tasks for which the percent responsible was below 40% were excluded from the task
list. However, the committee decided to make exceptions to include the following five tasks that were
slightly below 40%: Stone extraction, Vasoconstrictors, Measure and record vital signs, Analgesics, and
IV conscious sedatives. The Advisory Committee predicted that either the performance will increase over
time or stated that that they are critical tasks.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 10
Sixteen tasks were removed because approximately fewer than 40% of the target sample performed
these tasks. These tasks can be grouped into the following categories and rationale: film screen related
tasks that are no longer performed, pharmaceutical-centered procedures in which the drug is no longer
available or is no longer standard of practice for use, and medications that are the responsibility of the
nursing staff to administer.
CMS Data Comparison. This study extracted the number of times that providers billed procedures
to Medicare and Medicaid using the CMS Physician / Supplier Procedure Summary (PSPS) data file for
the year 2009, which was the most recent year available at the time of the study. Not all tasks had
corresponding CPT codes because they corresponded to non-billable clinical activities that are “rolled
into” larger billed procedures. This narrowed the analysis down to 70 potential procedures. 8 procedures
had to be eliminated from this analysis because the corresponding CPT code was not specific to the
equipment or drug involved. 2 additional procedures (Pulmonary Pressure Measurement and Venous
Access for Peripheral I.V.) had to be eliminated because too many types of medical personnel conduct
these procedures. ARRT staff successfully matched 60 procedures on the task questionnaire to Current
Procedural Terminology (CPT) codes.
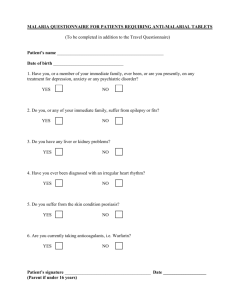
Figure 1 contains the results of the CMS / PA data comparison. The reader can see that the CMS
data and the PA questionnaire data showed a very high level of correspondence. The high Spearman’s ρ
correlation of 0.87 between the two sets of ranks demonstrates that, while CMS and the PA questionnaire
gathered data in very different ways (Babcock & Yoes, in press), the two data sources were in agreement
concerning how frequently the VI tasks were conducted.
Figure 1
CMS Rank on VI PA Paired Comparisons Frequency Rank, Spearman’s ρ = 0.87
60
2009 CMS Rank
50
40
30
20
10
0
0
10
20
30
40
50
PA Frequency Rank
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
60
70
Page 11
C HAPTER 4
R EVISION OF T ASK I NVENTORY, C ONTENT S PECIFICATIONS AND
C LINICAL E XPERIENCE R EQUIREMENTS
Overview
The previous chapter described the results the practice analysis questionnaire. This chapter describes
the process for using those data to revise the task inventory, update the content specifications, and revise the
clinical experience requirements. As noted in Chapter 1, the purpose of conducting the practice analysis
questionnaire is to ensure that the content specifications and clinical experience requirements are jobrelated. The first step in drafting the content specifications and clinical experience requirements is to
establish the task inventory based on the results of the practice analysis.
Finalization of the Task Inventory
The Advisory Committee met to review the questionnaire results and finalize the task inventory.
About two weeks prior to the meeting, the ARRT staff mailed tables summarizing questionnaire results to
the Committee. The Committee revised the task inventory so that it included: (a) tasks or activities on the
original inventory that were intentionally excluded from the questionnaire because they were known to be
job requirements (see Chapter 2); (b) tasks or activities on the questionnaire that at least 40% of VI
radiographers were responsible for performing; and (c) tasks or activities not exceeding 40% the
responsibility level but which the Committee felt were extremely critical to VI radiographers on the job.
The statement of purpose of ARRT’s examinations is that the exams should test knowledge concerning
typical practice. The ARRT currently uses an operational guideline of 40% responsibility level as being
typical practice, unless the Advisory Committee and the Board of Trustees feel that a certain infrequent
task is extremely critical. The following is a rationale for retaining tasks or activities that fell below 40%
and for adding newly written tasks.
Activities below 40% but kept
Rationale
x
Measure vital signs
In emergency situations, it is critical
for technologists to obtain and
interpret vital sign measurements
x
IV Medications:
o analgesics
o IV conscious sedatives
o vasoconstrictors
It is critical to VI practice to know the
effects of and how to administer these
drugs effectively
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 12
Rationale
New Activities
x
Neurologic:
o kyphoplasty
o discography
x
Dialysis Management
o fistulogram
o angioplasty
o stent placement
o thrombolysis/thrombectomy
x
Miscellaneous Procedures
o
All of these new tasks had a high
percentage of VI radiographers
reporting responsibility
radiofrequency ablation
Deleted Tasks
Rationale
x
Ready emergency cart to assure sufficient
emergency supplies
Infrequency; preparing the cart is
outside the scope of practice
x
Evaluate the operation of the automatic
film programmer
Infrequency
x
Inspect, prepare and troubleshoot
automatic film processors
Infrequency
x
Contrast: gadolinium
Not for VI based on new contrast
guidelines
x
Contrast: ethiodol
Infrequency
x
Assist in administering oral medications
according to physician’s orders
Infrequency, outside of scope of
practice
x
IV Medications:
o antiarrhythmics
o antiemetics
o antiplatelet inhibitors
o emergency medications (e.g.,
naloxone, protamine)
Infrequency
x
IV Medications: anti anxiety/anxiolytics
Task already covered under the task
“IV conscious sedatives”
x
Initiate the radiographic exposure: cut film
Infrequency
x
Process images as required: film
processing
Infrequency
x
GI: pharmacoangiography (e.g., pitressin
injection)
Infrequency; drug decreasing in usage
x
Thrombolytic Therapy:
o streptokinase
o urokinase
Infrequency
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 13
The ARRT Board of Trustees approved the final task inventory in the summer of 2011. Appendix C
contains the final task inventory.
Updating the Content Specifications
Topic Outline. The revision of the content specifications was based, in part, on the changes made to
the task inventory. For every activity in the task inventory, the Advisory Committee considered the
knowledge and skills required to successfully perform that task and to verify that the topic was addressed
in the content specifications. In other words, if one’s knowledge of a topic would have an impact on the
proficiency with which a task is performed, then that topic should be included in the content
specifications. The Committee similarly scrutinized the content specifications for practice relevance. The
Committee did not include topics not linked to practice on the content outline. To ensure that the content
specifications were job related, each task was linked to the appropriate topic in the content specifications.
The task inventory lists these links to the content specifications. The Committee devoted significant effort
updating the content specifications. The most notable revisions were:
Section A. “Equipment and Instrumentation” increased from 23 to 24 items.
Subcategory 3. “Catheters, Guidewires, Needles” was renamed “Procedural Supplies” and the
number of items increased from 8 to 10. The rationale for the increase included moving
“Closure Devices” into subcategory 3 from subcategory 4, and that this area of content
has greater bearing on the successful performance specific procedures.
Section B. “Patient Care” changed from 37 to 28 items.
Subcategory 1. “Patient Communication” increased from 1 to 2 items.
Subcategory 2. “Patient Assessment & Monitoring” decreased from 11 to 7. Two sections, “Vital
Signs” and “Physiologic Monitoring” were combined into one section and the “Lab
Values” section collapsed the subsections to lessen the focus on individual lab tests.
Subcategory 3. “Contrast Administration”: gadolinium was deleted as a result of the PA
questionnaire and removal from the approved task inventory.
Subcategory 4. “Medications” decreased from 8 to 6 due to the collapsed subsection, again to
minimize the focus on individual drugs and drug types that fell below the threshold on
the PA questionnaire and were deleted from the task inventory.
Subcategory 5. was moved to the procedure section.
Subcategory 6. now becomes 5 and the number of items increases from 2 to 3.
Subcategory 7. becomes 6 and the number of items drops from 8 to 5.
Number 3. “Bleeding” was added by the committee at the November meeting.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 14
Subcategory 8. is unchanged.
The overall number of items in this section decreased due to moving Subcategory 5 out of B and
into C and to have less of an emphasis on specific lab tests and drugs.
Section C. “Vascular-Interventional Procedures” increased from 100 to 108 items. The first five
categories were reorganized to begin anatomically superior, Neurologic, to inferior, Peripheral.
The former “GU and GI” subcategory was reclassified to “Abdominal” as the new subcategory 3,
then “GU and GI non-vascular”, as subcategory 4. Two new subcategories, “Dialysis
Management” and “Venous Access” were added as subcategories 6 and 7. These changes
required increasing the number of items by eight.
A draft of the content specifications and clinical experience requirements was available on the
ARRT website for about three weeks in October 2011. Interested parties filled out a short online
questionnaire and gave comments about the proposed changes. The Committee reviewed the
questionnaire results and comments at their final meeting in November 2011.
Assignment of Weights. As a final step in revising the content specifications, the Advisory
Committee established weights to indicate the number of test questions that should be allocated to each
section. The Committee participated in two different weighting activities. One activity had Committee
members allot a percentage of questions to each section. The second activity had Committee members
allot a raw number of questions to each section. ARRT staff analyzed these results, as well as highlighted
where there was agreement and disagreement between the activities. The Committee used these results to
guide their decisions in assigning numbers of questions to each section of the exam. The Committee made
a variety of changes to the section weights, but we only highlight the major changes here. First, the
Committee decreased the number of items in the Patient Care section, because the Committee moved
“Venous Access” out of the Patient Care section and into the Procedures section. The committee also
increased the number of questions about venous access, as it is a critical portion of practice. The
Committee also added the new “Dialysis Management” section with 11 questions. These questions came
mainly from reducing the number of questions in the “Peripheral” section in procedures.
Final Approval. The ARRT Board of Trustees reviewed comments from the online questionnaire
during a meeting held in the summer of 2011. They approved the content specifications, with the new
version becoming effective July 2012. Appendix D contains the 2012 Content Specifications for the
Vascular-Interventional Radiography Examination, which includes the numbers of items for each topic.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Page 15
Revision of the Clinical Experience Requirements
The purpose of the clinical experience requirements is to ensure that individuals certified by ARRT
have performed a core set of procedures that comprise a modality. More formally,
The purpose of the clinical experience requirements is to verify that candidates have completed a
subset of the clinical procedures within a modality. Successful performance of these fundamental
procedures, in combination with mastery of the cognitive knowledge and skills covered by the
certification exam, provides the basis for the acquisition of the full range of clinical skills required
in a variety of settings. Demonstration of clinical experience means that the candidate has
performed the procedure independently, consistently, and effectively.
When establishing the clinical experience requirements, the Advisory Committee focused on those
procedures in the task inventory typically performed by most entry-level vascular interventional
radiographers. The Committee made revisions during its April 2011 meeting. The notable changes are
outlined below.
x
The total number of procedures from which to choose decreased from 53 to 52; however, the
minimum number of required procedures remained the same, at minimum of 10 procedures and
200 repetitions.
x
A point under the rules for documentation was added for clarification of how to document more
than one procedure on one patient.
x
Titles for two of the six categories were edited. The new title for section C is “Abdominal” which
includes all vacular procedures. “Genitourinary” was moved to section D, to be included with
“Gastrointestinal non-vascular.” These changes match the changes made to the content
specifications; the categories are listed anatomically, superior to inferior.
x
Under section F, “Miscellaneous,” “abscess drainage” was changed to “percutaneous drainage”,
and “radiofrequency ablation” was added as a fourth procedure.
The revised draft was on the ARRT website in October of 2011, and interested parties could
participate in an online questionnaire and provide comments on the proposed changes. The Advisory
Committee reviewed the questionnaire results and comments at their final meeting in November 2011.
The Board of Trustees approved the clinical experience requirements in the January 2012, with the new
version becoming effective July 2012. Appendix E contains the 2012 Vascular-Interventional
Radiography Clinical Experience Requirements.
Copyright ¤ 2012 by the American Registry of Radiologic Technologists
Appendix A
Prototype of the Staff Questionnaire
A-1
VASCULAR-INTERVENTIONAL RADIOGRAPHY
PRACTICE ANALYSIS QUESTIONNAIRE
Dear Registered Technologist:
The American Registry of Radiologic Technologists is revising the content specifications and clinical
experience requirements for the examination in Vascular-Interventional Radiography. It is our philosophy
that a certification exam should be based on the job responsibilities of practicing technologists. The most
effective way to assure that the exam reflects current practice is by asking professionals such as yourself
about the procedures they perform.
The ARRT has assembled a preliminary list of activities that may be performed by technologists who work in
Vascular-Interventional Radiography. These activities appear on the enclosed practice analysis questionnaire.
In an effort to shorten the survey some tasks that are clearly being performed by a large majority of VascularInterventional Radiography technologists have been excluded from the survey. This questionnaire has been
sent to a carefully selected sample of Vascular-Interventional Radiography technologists across the country
in order to determine which procedures are performed in various practice settings. Since the questionnaire
was sent to only a sample, rather than to all technologists, it is very important that everyone return the
questionnaire. Your input is essential.
Please complete the questionnaire and return it to the ARRT within one week. A postage-paid envelope has
been included for your convenience. Simply enclose the questionnaire, seal the envelope, and drop it in the
mail.
Instructions for completing the questionnaire are provided on the inside cover. It should take less than 30
minutes to answer the questions. You may be assured of the complete confidentiality of your responses.
Individual responses will not be released to anyone under any circumstances.
Thank you very much for assisting us with this project. Your participation will help assure the integrity of
the certification process.
Respectfully,
Jerry B. Reid, Ph.D.
Executive Director
February 2011
FOR OFFICE USE ONLY
1
Correct marks
Incorrect marks
• Please use #2 pencil or blue or black pen to complete this survey.
• Do not use red pencil or ink.
• Do not use X's or check marks to indicate your responses.
• Fill response ovals completely with heavy, dark marks.
SECTION 1: PRACTICE ACTIVITIES
Directions: This section contains a list of numbered tasks and procedures (activities). Although you probably perform
many of these activities, there are likely some for which you are not directly responsible. If you are not personally
responsible for a particular activity, darken the oval labeled “Not Responsible for Performing” (NR) and proceed to
the next activity.
FREQUENCY. If you are responsible for performing an activity, please indicate approximately how often you perform
that task by filling in the appropriate oval (see sample below).
Daily
Weekly
Monthly
Quarterly
Yearly
Not responsible
On average, once per day or more often
On average, 3 times per month or more but less than “Daily”
On average, 10 times per year or more but less than “Weekly”
On average, 3 times per year or more but less than “Monthly”
On average, less often than quarterly but still conducted
Not responsible for performing
The sample below demonstrates how to mark your responses. Some tasks may be more difficult to rate than others –
just provide your best judgment. We value your input.
SAMPLE
D – Daily: on average, once per day or more often
W – Weekly: on average, 3 times per month or more but less than “Daily”
M – Monthly: on average, 10 times per year or more but less than “Weekly”
Q – Quarterly: on average, 3 times per year or more but less than “Monthly”
Y – Yearly: on average, less often than quarterly but still conducted
NR – Not responsible: not responsible for performing
NR
1. This is a sample task that is not part of my job responsibilities.
2. This is a sample task that I perform about twice weekly.
3. I perform this sample task 3 times a year.
4. This is a sample task that I performed 11 times this year.
5. I perform this sample task once every other year.
6. I perform this sample task every day on average.
2
Y
Q
M
W
D
Y
Q
M
W
D
NR
Y
Q
M
NR
Y
NR
Y
NR
NR
Y
M
D
W
D
W
D
Q
M
W
D
Q
M
W
Q
SECTION 1: PRACTICE ACTIVITIES (continued)
Directions: This section contains a list of numbered tasks and procedures (activities). Although you probably perform
many of these activities, there are likely some for which you are not directly responsible. If you are not personally
responsible for a particular activity, darken the oval labled “Not Responsible for Performing” (NR) and proceed to
the next activity.
Please fill in
only one
oval per item.
D – Daily: on average, once per day or more often
W – Weekly: on average, 3 times per month or more but less than “Daily”
M – Monthly: on average, 10 times per year or more but less than “Weekly”
Q – Quarterly: on average, 3 times per year or more but less than “Monthly”
Y – Yearly: on average, less often than quarterly but still conducted
NR – Not responsible: not responsible for performing
1. Check emergency (code) cart
2. Prepare treatment or examination equipment for sterilization
3. Evaluate the operation of the automatic film programmer
4. Inspect, prepare, and troubleshoot all equipment components of the procedure room
5. Inspect, prepare, and troubleshoot automatic film processors
6. Measure and record vital signs of patient prior to the procedure to establish a baseline
7. Physically prepare the patient for the examination to include ECG electrodes and
physiological monitoring equipment
In conjunction with physician, select the appropriate contrast agent
8.
ionic
nonionic
9.
low osmolality
10.
isosmolar
11.
CO2
12.
gadolinium
13.
Ethiodol
14. Assist in administering or obtaining oral medications according to physician’s orders
Prepare or assist in administering (e.g., obtain medication, fill syringe, etc.) the
following types of injectable medications according to physician’s orders
15.
analgesics
16.
antiarrhythmics
17.
anticoagulants
18.
antiemetics
19.
antiplatelet inhibitors
20.
anti-anxiety (anxiolytics)
21.
emergency medications (e.g., naloxone, protamine)
22.
IV conscious sedatives
23.
thrombolytics
24.
vasoconstrictors
25.
vasodilators
26. Monitor patient’s vital signs and ECG readings
27. Adjust exposure factors (e.g., mA, kVp, sec.) as required to obtain quality image
while minimizing dose
Initiate the radiographic exposure
28.
29.
cut film
digital acquisition
3
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
SECTION 1: PRACTICE ACTIVITIES (continued)
Please fill in
only one
oval per item.
D – Daily: on average, once per day or more often
W – Weekly: on average, 3 times per month or more but less than “Daily”
M – Monthly: on average, 10 times per year or more but less than “Weekly”
Q – Quarterly: on average, 3 times per year or more but less than “Monthly”
Y – Yearly: on average, less often than quarterly but still conducted
NR – Not responsible: not responsible for performing
NR
Y
Q
M
W
30.
film processing
31.
digital processing
32.
3D reconstruction
33. Assist with ultrasound guidance for vascular access or organ access/biopsy
34. Adjust and calibrate the pressure transducers used for intravascular pressures and/or
intraventricular pressures
35. Scrub-in with the physician
36. Record and maintain all procedural data (i.e., radiographic exposure factors, injection
data, elapsed fluoroscopic time, physiologic data, administered medications and
complications)
Assist with or perform the following procedures:
Neurologic
NR
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
intracranial angiography
extracranial angiography
neurologic embolization
neurologic thrombolysis/thrombectomy
neurologic angioplasty
neurologic stent placement
distal protection device placement
vertebroplasty
kyphoplasty
discography
Pulmonary
47.
48.
49.
pulmonary arteriograms
pulmonary embolization
pulmonary pressure measurement
Process images as required
D
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
GU
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
renal angiography
adrenal angiography
angiography of reproductive organs - female
angiography of reproductive organs - male
venous sampling
nephrostomy
ureteral stent placement
percutaneous stone extraction
embolization
renal artery angioplasty
renal artery stent placement
4
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
SECTION 1: PRACTICE ACTIVITIES (continued)
Please fill in
only one
oval per item.
D – Daily: on average, once per day or more often
W – Weekly: on average, 3 times per month or more but less than “Daily”
M – Monthly: on average, 10 times per year or more but less than “Weekly”
Q – Quarterly: on average, 3 times per year or more but less than “Monthly”
Y – Yearly: on average, less often than quarterly but still conducted
NR – Not responsible: not responsible for performing
NR
Y
61.
selective visceral angiography
62.
pharmacoangiography (e.g., pitressin injection)
63.
embolization
64.
angioplasty
65.
stent placement
66.
stone extraction
67.
percutaneous transhepatic cholangiogram
68.
biliary drainage/stenting
69.
cholecystostomy
70.
gastrostomy/gastrojejunostomy
71.
TIPS
72.
chemoembolization
Peripheral
NR
Y
Q
NR
Y
Q
NR
Y
Q
NR
Y
Q
NR
Y
NR
NR
NR
NR
NR
Y
73.
74.
75.
76.
77.
78.
79.
80.
81.
GI
thoracic aortography
abdominal aortography
upper extremity angiography
lower extremity angiography
inferior vena cava venography (cavagram)
superior vena cava venography (cavagram)
angioplasty
stent placement
stent graft placement
Thrombolytic Therapy
82.
streptokinase
83.
urokinase
84.
r-TPA
85.
mechanical thrombectomy
86.
atherectomy
87.
caval filter placement
88.
caval filter removal
89.
foreign body retrieval
90.
peripheral vascular embolization
Dialysis Management
91.
92.
93.
94.
fistulogram
angioplasty
stent placement
thrombolysis/thrombectomy
5
Q
M
W
D
M
W
D
M
W
D
M
W
D
M
W
D
Q
M
W
D
Y
Q
M
W
D
Y
Q
M
W
D
Y
Q
M
W
D
Y
Q
M
W
D
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
SECTION 1: PRACTICE ACTIVITIES (continued)
Please fill in
only one
oval per item.
D – Daily: on average, once per day or more often
W – Weekly: on average, 3 times per month or more but less than “Daily”
M – Monthly: on average, 10 times per year or more but less than “Weekly”
Q – Quarterly: on average, 3 times per year or more but less than “Monthly”
Y – Yearly: on average, less often than quarterly but still conducted
NR – Not responsible: not responsible for performing
NR
Y
Q
M
W
95.
PICC lines
96.
temporary dialysis catheter
97.
tunneled dialysis catheter
98.
port placement
99.
central lines
100.
peripheral IV
Miscellaneous Procedures
NR
101.
102.
103.
104.
105.
Venous Access
biopsy
abscess drainage
pressure measurements
vascular closure devices
radiofrequency ablation
D
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
NR
Y
Q
M
W
D
106. Is there a procedure that you perform that is not listed on this survey? Please write in if applicable.
SECTION 2: DEMOGRAPHIC AND WORK EXPERIENCE
These questions refer to your primary workplace in vascular-interventional radiography only.
4. How many registered nurses are employed in the
vascular-interventional department where you work?
1. Which of the following best describes
your place of employment?
0
1 to 3
Hospital/medical center
Physician group practice/clinic
Free-standing imaging center
Other
5. Which of the following best describes your job title?
Staff technologist
Lead or chief technologist
Administrator (manager)
Educator (program director, clinical instructor,
staff educator)
2. If you work in a hospital/medical center, what is its
approximate size (number of beds)?
If not, skip to question 3.
Less than 100
100 to 250
251 to 500
More than 500
Other
6. In what time frame does your department/facility require
advanced certification for vascular-interventional
radiologic technologists?
3. How many radiographers are employed in the
vascular-interventional department where you
work? (include yourself)
1 to 3
4 to 6
4 to 6
7 or more
7 to 9
10 or more
6
Prior to employment
Within 12 months of employment
Within 24 months of employment
Certification not required
SECTION 2: DEMOGRAPHIC AND WORK EXPERIENCE (continued)
7. Approximately what percentage of time do you personally spend in each modality?
0%
1 - 20%
21 - 40%
41 - 60%
61%+
Vascular-Interventional
Cardiac-Interventional
General Radiography
Other modality (e.g., CT, MRI)
Miscellaneous (e.g., management, teaching, PACS)
8. How many years have you worked in radiology?
10. What certifications do you currently hold?
(Mark all that apply)
11 to 15 years
More than 15 years
0 to 5 years
6 to 10 years
R.T. (R)
R.T. (VI or CV)
R.T. (CI)
R.T. (other)
RCIS
CCI (other)
9. How many years have you been regularly performing
VI radiography?
11 to 15 years
More than 15 years
0 to 5 years
6 to 10 years
11. Using the frequency scale from section 1, how often do you perform procedures with the following specialty physicians?
Never
Yearly
Quarterly
Monthly
Weekly
Daily
Interventional Radiologists
General Radiologists
Cardiologists
Vascular Surgeons
Neurosurgeons
Nephrologists
Other
12. In the past year, have you been asked to perform a
procedure that you had not conducted in the last
two years or had never performed?
Yes
15. If you used an electronic resource or search, please
write in the resource(s) that you used. Please write the
resource itself, NOT a search engine used to find the
resource.
No
13. If you answered “yes” to the previous question, what
was your course of action?
Performed the procedure
Performed the procedure with an experienced
technologist
16. What type of training or education initially prepared
you to work in vascular-interventional radiography?
(Mark all that apply)
Asked someone else to perform procedure
OJT
Workshop/seminar, 1 day
Workshop/seminar, multiple days
Formal VI educational program
14. If you performed the procedure, please mark any
informational resources that you consulted before
conducting the procedure. (Mark all that apply)
Another technologist
Physician
Commercial product specialist
Book/journal article
Institution-specific database/manual
Peer-reviewed medical Internet database
Other website
Portable device app. (smartphone, etc.)
Thank you for taking time from your busy schedule
to complete this very important survey.
The American Registry of Radiologic Technologists®
1255 Northland Drive, Saint Paul, Minnesota 55120
7
Appendix B
Results of the Staff Questionnaire
B-1
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
Tables B.1.: Demographic Statistics
1. Place of Employment
Hospital / Medical Center
Physician Group Practice / Clinic
Free-Standing Imaging Center
Other
%
92.3
5.8
0.9
0.9
2. Hospital / Medical Center Size
< 100
100 to 250
251 to 500
> 500
%
2.7
22.0
45.9
29.4
3. Number of Radiographers in VI
1-3
4-6
7-9
10 or more
%
30.8
33.5
15.7
20.0
4. Number of Nurses in VI
0
1-3
4-6
7 or more
%
0.9
24.2
32.1
42.8
5. Job Title
Staff Technologist
Lead or Chief Technologist
Administrator
Educator
Other
%
88.2
11.2
0.3
0.3
0.0
6. Certification Requirement
Prior to employment
Within 12 months of employment
Within 24 months of employment
Certification not required
%
0.6
8.4
13.9
77.1
7. % Time in Modalities
VI
CI
Gen. Radiography
Other Mod.
Misc.
0%
0
80
63
75
65
1-20%
0
10
24
20
25
8. Years Radiology Experience
0–5
6 – 10
10 – 15
more than 15
%
45.0
34.1
9.4
11.6
10. Certifications
R.T. (R)
R.T. (VI or CV)
R.T. (CI)
R.T. (Other)
RCIS
CCI (other)
%
91.7
26.9
1.5
10.7
0.3
0.0
21-40%
2
3
6
5
6
41-60%
9
5
6
0
3
9. Years VI Experience
0–5
6 – 10
10 – 15
more than 15
B-2
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
61%+
88
1
1
0
2
%
84.0
13.8
0.3
1.9
Tables B.1.: Demographic Statistics (continued)
11. How often do you work with these physicians?
Interventional Radiologists
General Radiologists
Cardiologists
Vascular Surgeons
Neurosurgeons
Nephrologists
Other
Never
5
49
69
30
65
73
77
Y
3
8
6
7
4
4
5
Q
1
6
5
8
7
6
4
M
3
11
5
11
8
6
4
12. Unfamiliar procedure
Yes
No
%
63.1
36.9
13. Course of action
Performed
Performed w/ exp. technologist
Asked someone perform
%
46.1
52.4
1.5
14. Informational resources used
Another technologist
Physician
Commercial product specialist
Book / journal article
Institution-specific database / manual
Peer-reviewed medical Internet database
Other website
Portable device app. (smartphone, etc.)
%
80.8
95.1
37.9
15.3
10.8
4.9
13.3
2.5
16. Initial training
OJT
Workshop / seminar, 1 day
Workshop / seminar, multiple days
Formal VI educational program
93.5
1.6
4.9
7.1
B-3
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
W
5
15
8
21
10
7
6
D
84
11
8
24
7
5
4
Code cart
Prepare equip. sterilization
Evaluate film programmer
Inspect procedure room
Inspect film processors
Measure vital signs
Physically prepare the patient
Contrast: ionic
Contrast: low osmolality
Contrast: isosmolar
Contrast: CO2
Contrast: gadolinium
Contrast: Ethiodol
Oral meds
Meds: analgesics
Meds: antiarrhythmics
Meds: anticoagulants
Meds: antiemetics
Meds: antiplatelet inhibitors
Meds: anti anxiety/anxiolytics
Meds: emergency medications
Meds: IV conscious sedatives
Meds: thrombolytics
Meds: vasoconstrictors
Meds: vasodilators
Monitor patient vitals
Adjust exposure factors
Initiate cut film
Initiate digital
Process film
Process digital
Process 3D
Task
% NR
75.5
48.6
68.2
19.0
77.7
70.6
30.9
41.9
11.6
41.0
28.4
53.2
59.0
77.4
71.3
87.5
52.9
88.7
82.9
89.0
84.1
82.3
45.3
68.2
56.9
56.9
8.9
90.8
3.7
73.7
2.1
32.4
%
Missing
1.2
4.3
2.8
0.6
4.0
1.2
1.5
4.3
4.0
8.9
2.1
3.1
3.4
6.7
2.4
1.5
1.5
2.4
2.1
0.9
2.1
1.8
1.8
2.1
2.1
1.8
0.9
1.8
0.6
11.0
11.0
8.0
% Resp.
(Y+Q+M
+W+D)
23.2
47.1
29.1
80.4
18.3
28.1
67.6
53.8
84.4
50.2
69.4
43.7
37.6
15.9
26.3
11.0
45.6
8.9
15.0
10.1
13.8
15.9
52.9
29.7
41.0
41.3
90.2
7.3
95.7
15.3
86.9
59.6
BTL
Coef.
−0.89
−0.14
−0.72
0.98
−1.08
−0.71
0.63
0.18
1.44
0.08
−0.10
−0.72
−0.86
−1.23
−0.78
−1.40
−0.15
−1.46
−1.25
−1.47
−1.41
−1.28
−0.20
−0.87
−0.57
−0.28
1.55
−1.47
2.09
−1.12
2.14
−0.07
Out: Infrequency
Out: Infrequency
In: Infrequent but critical
Out: Infrequency
Out: Infrequency, not part of VI process
Out: Covered under another task
Out: Infrequency
In: Infrequent but critical
Out: Not for VI, now just for MRI prep
Out: Infrequency
Out: Infrequency, outside of scope
In: Infrequent but critical
Out: Infrequency
Out: Infrequency
In: Infrequent but critical
Out: Infrequency
Comments
Out: Infrequency, outside of scope
B-4
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
Task #
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
%
Daily
15.3
29.4
20.5
60.9
11.6
20.8
54.1
45.0
74.6
36.4
13.8
7.6
6.4
6.4
19.0
4.9
28.1
3.7
6.7
4.0
3.7
6.1
14.7
8.6
9.8
30.3
79.8
4.9
93.0
11.0
83.2
18.3
Table B.2: Statistics for the Practice Activities
Task
Ultrasound guidance
Pressure transducers
Scrub in
Record procedural data
Neurologic: intracranial ang
Neurologic: extracranial ang
Neurologic: neurologic embo
Neurologic: neurologic thromb
Neurologic: neurologic ang
Neurologic: neurologic stent
Neurologic: distal protection
Neurologic: vertebroplasty
Neurologic: kyphoplasty
Neurologic: discography
pulmonary arteriograms
pulmonary embolization
pulmonary pressure
GU: renal angiography
GU: adrenal angiography
GU: angiography repro female
GU: angiography repro male
GU: venous sampling
GU: nephrostomy
GU: ureteral stent placement
GU: percutaneous stone
GU: embolization
GU: renal artery angioplasty
GU: renal artery stent placement
GI: selective visceral angiography
GI: pharmacoangiography
GI: embolization
GI: angioplasty
% NR
4.0
39.4
2.1
12.5
22.0
27.8
47.1
44.0
45.3
45.6
36.4
28.1
36.1
47.7
26.3
32.7
42.2
7.3
35.2
29.1
38.8
32.1
12.8
12.5
46.5
11.0
8.6
9.8
11.9
68.5
14.7
16.8
%
Missing
6.7
6.4
5.2
6.4
7.0
9.5
9.8
11.0
7.6
9.5
10.4
8.0
6.7
10.4
8.0
9.2
9.8
6.1
7.3
9.2
10.7
7.6
6.4
9.5
11.0
9.5
9.2
9.5
1.5
3.7
1.2
2.1
% Resp.
(Y+Q+M
+W+D)
89.3
54.1
92.7
81.0
70.9
62.7
43.1
45.0
47.1
45.0
53.2
63.9
57.2
41.9
65.7
58.1
48.0
86.5
57.5
61.8
50.5
60.2
80.7
78.0
42.5
79.5
82.3
80.7
86.5
27.8
84.1
81.0
BTL
Coef.
1.82
−0.13
1.93
1.54
0.35
0.10
−0.51
−0.61
−0.56
−0.61
−0.41
−0.07
−0.28
−0.83
−0.53
−0.70
−0.85
0.49
−0.64
−0.38
−0.88
−0.58
0.82
0.45
−0.89
0.31
0.10
0.02
0.49
−1.20
0.29
0.14
Comments
Out: Infrequency
B-5
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
Task #
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
%
Daily
72.8
17.1
80.7
78.0
22.0
17.7
8.9
6.4
8.6
6.1
7.3
8.3
7.0
3.4
4.0
3.7
3.4
12.2
4.3
4.6
2.4
5.8
22.0
11.6
2.1
13.1
6.4
5.8
15.3
2.4
14.1
15.0
Task
GI: stent placement
GI: stone extraction
GI: percu cholangiogram
GI: biliary drainage stenting
GI: cholecystostomy
GI: gastrostomy
GI: TIPS
GI: chemoembolization
Peripheral: thoracic aorto
Peripheral: abdominal aorto
Peripheral: upper ext ang
Peripheral: lower ext ang
Peripheral: inferior vc venography
Peripheral: superior vc venography
Peripheral: angioplasty
Peripheral: stent placement
Peripheral: stent graft placement
Peripheral: Thrombolytic: streptokinase
Peripheral: Thrombolytic: urokinase
Peripheral: Thrombolytic: r TPA
Peripheral: mechanical thrombectomy
Peripheral: atherectomy
Peripheral: caval filter placement
Peripheral: caval filter removal
Peripheral: foreign body retrieval
Peripheral: peripheral vascular embo
Dialysis: fistulogram
Dialysis: angioplasty
Dialysis: stent placement
Dialysis: thrombolysis thrombectomy
Venous Access: PICC lines
Venous Access: temp. dialysis catheter
% NR
21.7
59.0
16.8
15.0
31.2
22.3
30.3
33.3
14.4
8.6
3.1
4.0
4.3
5.5
3.1
3.1
23.2
82.0
77.7
21.1
13.5
38.2
7.0
11.9
15.3
14.1
3.4
4.9
6.4
7.3
11.0
6.7
%
Missing
1.8
4.0
1.5
2.1
1.8
2.4
1.2
1.5
2.4
2.8
1.8
1.2
3.1
2.8
1.5
2.1
2.1
3.1
4.3
4.3
4.0
4.0
2.1
1.5
1.8
1.2
1.2
1.8
1.2
1.5
2.8
3.1
% Resp.
(Y+Q+M
+W+D)
76.5
37.0
81.7
82.9
67.0
75.2
68.5
65.1
83.2
88.7
95.1
94.8
92.7
91.7
95.4
94.8
74.6
15.0
18.0
74.6
82.6
57.8
90.8
86.5
82.9
84.7
95.4
93.3
92.4
91.1
86.2
90.2
BTL
Coef.
−0.09
−1.11
0.23
0.28
−0.14
0.31
−0.48
−0.34
0.06
0.93
0.83
1.16
1.10
0.68
1.25
0.97
0.02
−1.51
−1.44
0.12
0.31
−0.43
0.94
−0.01
−0.37
−0.16
1.22
1.17
0.59
0.71
1.20
1.17
Comments
Out: Infrequency
Out: Infrequency
B-6
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
Task #
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
%
Daily
10.7
1.8
10.1
10.4
7.6
18.0
2.8
5.8
10.4
32.4
27.8
37.6
29.4
23.9
40.7
28.7
11.9
0.6
0.6
7.0
10.1
5.8
22.6
6.7
2.8
5.2
42.8
41.9
22.6
24.5
54.7
46.2
Task #
97
98
99
100
101
102
103
104
105
% NR
5.2
14.7
17.1
43.1
20.2
21.4
26.3
11.6
51.1
%
Missing
3.4
3.4
3.4
4.9
4.6
6.7
5.8
4.0
3.7
% Resp.
BTL
(Y+Q+M
Coef.
+W+D)
91.4
1.38
82.0
0.84
79.5
0.68
52.0
−0.12
75.2
0.57
71.9
0.47
67.9
−0.14
84.4
0.94
45.3
−0.79
B-7
Copyright ¤ 2012 by the American Registry of Radiologic Technologists.
Task
Venous Access: tunneled dialysis catheter
Venous Access: port placement
Venous Access: central lines
Venous Access: peripheral IV
Misc: biopsy
Misc: abscess drainage
Misc: pressure measurements
Misc: vascular closure devices
Misc: radiofrequency ablation
%
Daily
50.8
37.0
34.9
26.3
32.4
27.2
11.3
38.5
5.2
Comments
Appendix C
Final Task Inventory
C-1
TASK INVENTORY FOR
VASCULAR-INTERVENTIONAL
RADIOGRAPHY
ARRT® Board Approved: July 2011
Implementation Date: July 2012
Certification requirements for Vascular-Interventional Radiography (VI) are based on the results of a
comprehensive practice analysis conducted by ARRT staff and the Practice Analysis Advisory
Committee. In 2011, the ARRT surveyed a large national sample of radiographers who perform
vascular-interventional radiography to identify their job responsibilities. This document reflects the
results of that survey. The attached task inventory is the foundation for both the clinical experience
requirements and the content specifications.
Basis of Task Inventory
The practice analysis survey was used to identify the responsibilities typically required of staff
technologists who perform VI. When evaluating survey results, the advisory committee applied a
40% guideline. That is, to be included on the task inventory, an activity must have been the
responsibility of at least 40% of staff technologists who perform VI. The advisory committee could
include an activity that did not meet the 40% criterion if there was a compelling rationale to do so
(e.g., a task that falls below the 40% guideline but is expected to rise above the 40% guideline in the
near future.
Application to Clinical Experience Requirements
The purpose of the clinical experience requirements is to verify that candidates have completed
fundamental clinical procedures in VI. Successful performance of these fundamental procedures, in
combination with mastery of the cognitive knowledge and skills covered by the VI examination,
provides the basis for acquisition of the full range of clinical skills required i n a variety of settings. An
activity must appear on the task inventory to be considered for inclusion in the clinical experience
requirements. For an activity to be designated as a mandatory requirement, survey results had to
indicate that the vast majority of technologists who perform VI performed that activity. The advisory
committee designated clinical activities performed by fewer technologists, or which are carried out
only in selected settings, as elective. The clinical experience requirements are ava ilable from
ARRT’s website (www.arrt.org) and appear in the Vascular-Interventional Radiography Certification
Handbook.
Application to Content Specifications
The purpose of the ARRT Examination in VI is to assess the knowledge and cognitive skills
underlying the intelligent performance of the tasks typically required of staff technologists who
perform VI. The content specifications identify the knowledge areas underlying performance of the
tasks on the task inventory. Every content category can be linked to one or more activities on the
task inventory. Note that each activity on the task inventory is followed by a content category that
identifies the section of the content specifications corresponding to that activity. The content
specifications are available from ARRT’s website (www.arrt.org) and appear in the VascularInterventional Radiography Certification Handbook.
Copyright © 2011 by The American Registry of Radiologic Technologists . All rights reserved.
Reproduction in whole or part is not permitted without the written consent of the ARRT
Survey
Number
Task Statement
1.
Maintain inventory of sterile supplies and medications
2.
Prepare materials or trays with medications and materials for special treatments or
procedures according to standard order
3.
Prepare treatment or examination equipment for sterilization
4.
Provide regular daily maintenance and cleaning of the automatic pressure injector
5.
Monitor performance and dependability of the automatic pressure injector on a continual
basis as related to programmed injection parameters
6.
Inspect, prepare and troubleshoot all equipment components of the procedure room
7.
Verify presence of appropriate signed informed procedural consent
8.
Verify patient’s identification
9.
Obtain information about the patient which might indicate a risk of drug or contrast reaction
prior to any procedure, using patient records or by questioning patient
10.
Measure and record vital signs of patient prior to the procedure to establish a baseline
11.
Prepare the area of needle puncture and catheter insertion to include the required sterile
drapes and covers
12.
Provide for patient comfort and cooperation by familiarizing patient with the equipment and
procedural aspects of the examination and by responding to questions, and by providing
general psychological support
13.
Physically prepare the patient for the examination to include ECG electrodes and
physiological monitoring equipment
In conjunction with radiologist, select the appropriate contrast agent
14.
ionic
15.
nonionic
16.
a.
low osmolality
17.
b.
isosmolar
18.
19.
CO2
Set-up or operate the automatic pressure injector for administering contrast media
Prepare or assist in administering (e.g., obtain medication, fill syringe, etc.) the
following types of injectable medications according to physician’s orders
20.
analgesics
21.
anticoagulants
22.
IV conscious sedatives
23.
thrombolytics
C-3
Survey
Number
Task Statement
24.
vasoconstrictors
25.
vasodilators
26.
Monitor patient’s vital signs and ECG readings
27.
Recognize and respond to patient emergencies (seizure, cardiac distress, etc.)
28.
Monitor and maintain medical equipment (e.g., IVs, oxygen) used during the procedure
29.
Use sterile or aseptic technique as required to help prevent infection
30.
Handle blood and body fluids in a manner appropriate to biohazardous materials
31.
Position the patient and/or imaging equipment to achieve desired projections
32.
Adjust exposure factors (e.g., mA, kVp, sec.) as required to obtain quality image while
minimizing dose
Initiate the radiographic exposure
33.
digital acquisition
Process images as required
34.
digital processing
35.
3D reconstruction
36.
Employ special image-enhancement techniques (magnification, filtration, etc.) during
procedure to improve image quality
37.
Assist with ultrasound guidance for vascular access or organ access/biopsy
38.
Adjust and calibrate the pressure transducers used for intravascular pressures and/or
intraventricular pressures
39.
Scrub-in with the physician
40.
Record and maintain all procedural data. (i.e., radiographic exposure factors, injection
data, elapsed fluoroscopic time, physiologic data, administered medications and
complications)
Assist with or perform the following procedures:
Neurologic
41.
intracranial angiography
42.
extracranial angiography
43.
neurologic embolization
44.
neurologic thrombolysis/thrombectomy
C-4
Survey
Number
Task Statement
45.
neurologic angioplasty
46.
neurological stent placement
47.
distal protection device placement
48.
vertebroplasty
49.
kyphoplasty
50.
discography
Pulmonary
51.
pulmonary arteriograms
52.
pulmonary embolization
53.
pulmonary pressure measurement
GU
54.
renal angiography
55.
adrenal angiography
56.
angiography of reproductive organs – female
57.
angiography of reproductive organs – male
58.
venous sampling
59.
nephrostomy
60.
ureteral stents
61.
percutaneous stone extraction
62.
embolizations
63.
renal artery angioplasty
64.
renal artery stent placement
GI
65.
selective visceral angiography
66.
embolization
67.
angioplasty
68.
stent placement
C-5
Survey
Number
Task Statement
69.
stone extraction
70.
percutaneous transhepatic cholangiogram
71.
biliary drainage/stenting
72.
cholecystostomy
73.
gastrostomy/gastrojejunostomy
74.
TIPS
75.
chemoembolization
Peripheral
76.
abdominal aortography
77.
thoracic aortography
78.
upper extremity angiography
79.
lower extremity angiography
80.
inferior vena cava venography (cavagram)
81.
superior vena cava venography (cavagram)
82.
angioplasty
83.
stent placement
84.
stent graft placement
Thrombolytic Therapy
85.
r-TPA
86.
mechanical thrombectomy
87.
atherectomy
88.
caval filter placement
89.
removable IVC filter placement
90.
foreign body retrieval
91.
peripheral vascular embolization
C-6
Survey
Number
Task Statement
Dialysis Management
92.
fistulogram
93.
angioplasty
94.
stent placement
95.
thrombolysis/thrombectomy
Venous Access
96.
PICC lines
97.
temporary dialysis catheter
98.
tunneled dialysis catheter
99.
port placement
100.
central lines
101.
peripheral I.V.
Miscellaneous Procedures
102.
biopsies
103.
abscess drainage
104.
pressure measurements
105.
vascular closure devices
106.
radiofrequency ablation
Follow-Up Patient Care
107.
apply pressure to arterial or venous puncture site
108.
apply dressing to puncture
109.
explain post-procedure care instructions to patient
C-7
Appendix D
Final Content Specifications
D-1
CONTENT S PECIFICATIONS F OR
THE V ASCULAR-I NTERVENTIONAL
RADIOGRAPHY E XAMINATION
ARRT® Board Approved: January 2012
Implementation Date: July 2012
The purpose of The American Registry of Radiologic Technologists ® Examination in VascularInterventional Radiography is to assess the knowledge and cognitive skills underlying the
intelligent performance of the tasks typically required of the staff technologist at entry into the
profession. To identify the knowledge and skills covered by the examination, the ARRT
periodically conducts practice analysis studies involving a nationwide sample of staff
technologists. 1 The results of the most recent practice analysis are reflected in this document.
Every content category can be linked to one or more activities on the task inventory. The
complete task inventory is available from our website www.arrt.org.
The table below presents the three major content categories and seven procedural
subcategories covered on the examination, and indicates the number of test questions in each
category. The content specifications identify the knowledge areas underlying performance of
the tasks on the task inventory. The remaining pages provide a detailed listing of topics
addressed within each major content category.
This document is not intended to serve as a curriculum guide. Although certification programs
and educational programs may have related purposes, their functions are clearly different.
Educational programs are generally broader in scope and address the subject matter that is
included in these content specifications, but do not limit themselves only to this content.
NUMBER OF
SCORED
QUESTIONS 2
CONTENT CATEGORY
A.
B.
C.
Equipment and Instrumentation
Patient Care
Vascular-Interventional Procedures
1. Neurologic
2. Thoracic
3. Abdominal
4. GU and GI, non vascular
5. Peripheral
6. Dialysis Management
7. Venous Access
Total
24
28
16
12
25
15
20
11
9
160
1. A special debt of gratitude is due to the hundreds of professionals participating in this
project as committee members, survey respondents, and reviewers.
2. Each exam includes an additional 25 unscored (pilot) questions. On the pages that
follow, the approximate number of test questions allocated to each content category
appears in parentheses.
Copyright © 2012 by The American Registry of Radiologic Technologists ®. All rights reserved. Reproduction in whole
or part is not permitted without the written consent of the ARRT.
D-2
A. EQUIPMENT AND INSTRUMENTATION (24)
1.
Digital Imaging (6)
a.
Image Characteristics
1. pixel
2. image matrix
3. dynamic range
b.
Image Production
1. data acquisition
2. post processing
3. subtraction technique
4. archiving
5. quality control
6. display
7. 3-D reconstruction
3.
4.
2.
Procedural Supplies (10)
a.
Types
1. diagnostic (e.g., catheters, guidewires,
needles, sheaths)
2. interventional (e.g., balloon, cutting
balloon, atherectomy device,
mechanical thrombectomy devices)
3. closure devices
b.
Construction
c.
Indications for Use
Implantable Devices (5)
Automatic Pressure Injectors (3)
a.
Caval Filters (permanent and removable)
a.
Parts
b.
Central Venous Catheters (with or without
subcutaneous port)
b.
Function
c.
Embolic Materials
c.
Operation
d.
Stents
1. vascular
2. nonvascular
e.
Stent Grafts
D-3
B. PATIENT CARE (28)
1.
2.
3.
Patient Communication (2)
a.
Patient Education
b.
Informed Consent
Contrast Administration (3)
a.
Types and Properties of Contrast Agents
1. ionic
2. nonionic
a. low-osmolar
b. iso-osmolar
3. CO2
b.
Indications and Contraindications
Patient Assessment and Monitoring (7)
(normal and abnormal values; implications)
a.
Physiologic Monitoring
1. vital signs
2. ECG
a. equipment and patient preparation
b. interpretation (sinus rhythm,
common arrhythmias)
3. pulse oximetry
b.
Access Assessment
1. peripheral pulses
2. anatomical location
c.
Lab Values
1. renal function (e.g., BUN, creatinine,
eGFR)
2. blood coagulation (e.g., PT, PTT,
INR, ACT)
3. hematology (e.g., Hgb, WBC, platelet)
4. other (e.g., LFT, potassium)
d.
4.
Medications (6)
a.
Types and Administration Routes
1. analgesics (e.g., fentanyl)
2. IV sedatives (e.g., diazepam,
midazolam)
3. anticoagulants
4. thrombolytics
5. vasoconstrictors
6. vasodilators
b.
Indications and Contraindications
c.
Preparation and Dosage
d.
Complications
Maintaining Accessory Medical Devices
1. oxygen delivery systems
2. chest tubes
3. in-dwelling catheters
4. drainage bags
(Section B continues on the following page)
D-4
B. PATIENT CARE (cont.)
5.
Asepsis and Sterile Technique (3)
a.
Sterile Technique
1. sterile fields
a. patient preparation
b. procedural tray
c. maintenance of sterile fields
2. surgical scrub technique
b.
Infection Control
1. standard precautions
2. transmission-based precaution
a. contact
b. airborne
c. droplet
6.
7.
D-5
Emergency Care (5)
a.
Contrast Reactions and Complications
1. allergic-type
a. minor
b. intermediate
c. severe
2. adverse
a. hemodynamic responses
b. nephrotoxicity
c. CNS reactions
b.
Treatment and Medications
1. types (e.g., steroids, antihistamines)
2. indications and contraindications
c.
Symptoms and Treatment of Medical
Emergencies
1. air embolism
2. anaphylaxis
3. bleeding
4. cardiac arrhythmias
5. congestive heart failure
6. hemothorax
7. hypertensive episodes
8. hypotensive episodes
9. myocardial infarction
10. pneumothorax
11. respiratory arrest
12. sepsis
13. thrombosis
14. thrombotic embolism
15. TIA
16. vasovagal response
Cardiac Life Support (2)
a.
BLS
b.
Defibrillation
C. VASCULAR
INTERVENTIONAL PROCEDURES (108)
CATEGORY
1.
Neurologic
a.
b.
2.
b.
3.
FOCUS OF QUESTIONS
Questions for each section of the exam
may address any of the following factors,
as appropriate:
1. Anatomy and Physiology
2. Pathology
3. Indications for Procedure
4. Contraindications for Procedure
5. Patient Positioning
6. Access Method
12
7. Ultrasound Guidance
Angiography (7)
1. aortography
2. pulmonary
3. bronchial
4. superior vena cava
Interventional Procedures (5)
1. embolization
2. thrombolysis
3. thrombectomy
4. angioplasty
5. stent placement
6. biopsy
7. drainage procedures
8. foreign body retrieval
9. radiofrequency
Abdominal
a.
16
Angiography (9)
1. intracranial
2. extracranial
3. spinal
Interventional Procedures (7)
1. embolization
2. thrombolysis
3. thrombectomy
4. angioplasty
5. stent placement
6. distal protection device
placement
7. foreign body retrieval
8. vertebroplasty
9. kyphoplasty
10. discography
Thoracic
a.
# QUESTIONS
8. Patient Management
9. Intravascular Pressure
Measurements
10. Contrast Administration (i.e., ionic,
nonionic, CO2 )
11. Equipment (e.g., imaging media,
automatic injectors)
12. Exposure Technique
13. Image Enhancement
25
14. Closure Devices
Arteriography (11)
1. abdominal aortography
2. pelvic angiography
3. renal
4. adrenal
5. reproductive
6. celiac
7. SMA
8. IMA
15. Complications
(Section C continues on the following page)
D-6
C. VASCULAR
INTERVENTIONAL PROCEDURES (cont.)
CATEGORY
3.
Abdominal (cont.)
b.
c.
4.
# QUESTIONS
a.
b.
Questions for each section of the exam
may address any of the following factors,
as appropriate:
Venography (6)
1. pelvic
2. inferior vena cava
3. renal
4. adrenal
5. gonadal
6. venous sampling
7. splenic
8. hepatic
9. portal
Interventional Procedures (8)
1. caval filter placement
2. caval filter removal
3. stent grafts
4. embolizations
5. thrombolysis
6. thrombectomy
7. angioplasty
8. stent placement
9. foreign body retrieval
10. TIPS
11. chemoembolization
GU and GI, non-vascular
FOCUS OF QUESTIONS
1. Anatomy and Physiology
2. Pathology
3. Indications for Procedure
4. Contraindications for Procedure
5. Patient Positioning
6. Access Method
7. Ultrasound Guidance
8. Patient Management
9. Intravascular Pressure
Measurements
15
GU Interventional Procedures (7)
1. nephrostomy
2. ureteral dilation/stents
3. percutaneous renal stone
extraction
4. drainage procedures
5. radiofrequency ablation
GI Interventional Procedures (8)
1. biliary stone extraction
2. percutaneous transhepatic
cholangiogram
3. biliary drainage/stenting
4. cholecystostomy
5. gastrostomy/
gastrojejunostomy
6. drainage procedures
7. biopsy (percutaneous or
transvascular)
8. radiofrequency ablation
10. Contrast Administration (i.e., ionic,
nonionic, CO2 )
11. Equipment (e.g., imaging media,
automatic injectors)
12. Exposure Technique
13. Image Enhancement
14. Closure Devices
15. Complications
(Section C continues on the following page)
D-7
C. VASCULAR
INTERVENTIONAL PROCEDURES (cont.)
CATEGORY
5.
Peripheral
a.
b.
c.
6.
7.
FOCUS OF QUESTIONS
Questions for each section of the exam
may address any of the following factors,
as appropriate:
1. Anatomy and Physiology
2. Pathology
3. Indications for Procedure
4. Contraindications for Procedure
5. Patient Positioning
11
6. Access Method
diagnostic angiography
thrombolysis
thrombectomy
angioplasty
stent placement
Venous Access (9)
a.
b.
c.
d.
e.
f.
20
Arteriography (9)
1. upper extremity
2. lower extremity
Venography (2)
1. upper extremity
2. lower extremity
Interventional Procedures (9)
1. embolization
2. thrombolysis
3. thrombectomy
4. angioplasty
5. stent placement
6. atherectomy
7. foreign body retrieval
Dialysis Management (11)
a.
b.
c.
d.
e.
# QUESTIONS
7. Ultrasound Guidance
8. Patient Management
9. Intravascular Pressure
Measurements
9
PICC lines
temporary dialysis catheter
tunneled dialysis catheter
port placement
central lines
peripheral IV
10. Contrast Administration (i.e., ionic,
nonionic, CO2 )
11. Equipment (e.g., imaging media,
automatic injectors)
12. Exposure Technique
13. Image Enhancement
14. Closure Devices
15. Complications
D-8
Appendix E
Final Clinical Experience Requirements
E-1
V ASCULAR -I NTERVENTIONAL RADIOGRAPHY
C LINICAL E XPERIENCE R EQUIREMENTS
Eligibility Requirements Effective
for Examinations Beginning July 1, 2012*
The purpose of the clinical experience requirements is to verify that candidates have completed
a subset of the clinical procedures within a discipline. Successful performance of these
fundamental procedures, in combination with mastery of the cognitive knowledge and skills
covered by the certification examination, provides the basis for the acquisition of the full range
of clinical skills required in a variety of settings.
This document identifies the clinical experience required for certification. The American
Registry of Radiologic Technologists® (ARRT®) encourages individuals to obtain education and
experience beyond these minimum requirements.
Instructions for Eligibility
1. Perform the Procedures: Candidates are required to perform clinical procedures according
to the Specific Procedural Requirements and selected from the list of procedures found within
this document. All procedures must be performed within the 24 month period immediately
preceding the date of the candidate’s signature on the application for certification. Repetitions
may be completed in less than 24 months.
2. Document Performance: Candidates must use the following Vascular-Interventional
Radiography Clinical Experience Documentation Form or a reasonable facsimile to record the
performance of each of the procedures. Documentation includes: name of procedure, date
performed, time of day completed, facility where performed, and the initials of the person
verifying performance. The “Verifier’s Initials” column on the form must be initialed by a
Registered Technologist or a licensed physician and must match the Verification Identification
Page at the end of this document. The name and address of the person corresponding to each
set of initials must also be provided on the Verification Identification Page. Failure to meet the
minimum clinical experience requirements prior to the date of the application signature will result
in the application becoming “ineligible.” All documented procedures prior to that date will not be
accepted for future clinical experience requirements.
3. Apply for Certification: After the clinical experience requirements have been completed,
candidates are eligible to complete the verification section of the application for certification.
ARRT will accept the completed application up to six months after the date of signature. Mail
only the application for certification to the ARRT; do not send the Clinical Experience
Documentation Form to ARRT with the application. Submitting false documentation to ARRT as
part of the application process is a violation of ARRT Standards of Ethics and may result in
sanctions up to and including revocation of ARRT certification in all disciplines and ineligibility
for any additional ARRT certifications.
4. Maintain Your Records: Candidates must keep the Clinical Experience Documentation
Form for at least 24 months after the date that the application is signed. The ARRT conducts
audits of some applications for certification. Candidates who are audited will be required to
send the Clinical Experience Documentation Form to ARRT. Additional documentation may be
required from individuals who are audited.
*Candidates who submit their applications up through June 2014 may use either the previous requirements (effective
2009 or the current requirements (effective 2012). Candidates who apply after June 2014 may no longer use the
previous clinical experience requirements.
Copyright © 2012 by The American Registry of Radiologic Technologists . All rights reserved.
Specific Procedural Requirements
The Clinical Experience Requirements for Vascular-Interventional Radiography consist
of 52 procedures in 6 different categories. The 6 categories include:
A. Neurological
B. Thoracic
C. Abdominal
D. Genitourinary and Gastrointestinal, non-vascular
E. Peripheral
F. Miscellaneous
Candidates must document the performance of these procedures according to the
following rules:
x
Choose a minimum of 10 of the 52 procedures; more than 10 procedures may be
selected for completion.
x
For any given patient per day, you may count only one diagnostic but may count
multiple interventional procedures.
x
Each selected procedure must be performed a minimum of 5 times (repetitions)
in order for the candidate to receive credit for that procedure.
x
Each procedure may be counted a maximum of 20 times.
x
Each candidate must complete a total of 200 repetitions across all procedures
selected for performance.
Examples:
The following hypothetical candidates illustrate three ways of satisfying the clinical
experience requirements. Numerous other combinations are possible.
Candidate A: This person identified 10 different procedures from the list on the
following page and performed each of those procedures 20 times (10 x 20 = 200).
Candidate B: This person identified 25 different procedures from the list on the
following page. This applicant performed 15 of those procedures 10 times (15 x 10
= 150), and the other 10 procedures 5 times (10 x 5 = 50).
Candidate C: This person identified 40 different procedures from the list on the
following page and performed each of those procedures 5 times (40 x 5 = 200).
E-3
General Requirements
To qualify as a complete imaging procedure, the candidate must demonstrate active
participation in a primary role with appropriate:
x
preparation of supplies and maintenance of equipment
x
evaluation of requisition and patient, patient preparation, administration of
medications as required
x
patient monitoring during procedure
x
follow-up patient care
x
image processing, including evaluation of images to ensure they demonstrate
correct anatomy, radiographic techniques, and identification/labeling
E-4
Vascular-Interventional Radiography Procedures
A. Neurological
1.
2.
3.
4.
5.
6.
7.
8.
9.
Neurologic angiography
Spinal arteriography
Embolization
Thrombolysis
Thrombectomy
Angioplasty
Stent placement
Vertebroplasty and/or Kyphoplasty
Discography
D. Genitourinary and Gastrointestinal,
non-vascular
1.
2.
3.
4.
5.
Nephrostomy
Ureteral dilatation and/or stents
Percutaneous renal stone extraction
Biliary stone extraction
Percutaneous transhepatic
cholangiogram
6. Biliary drainage and/or stenting
7. Cholecystostomy
8. Gastrostomy or gastrojejunostomy
B. Thoracic
1. Thoracic aortography
2. Pulmonary arteriography
3. Superior vena cava (central
venography)
4. Embolization
E. Peripheral
1. Upper extremity arteriography
2. Lower extremity arteriography
3. Extremity venography
4. Dialysis angiography
5. Embolization
6. Thrombolysis
7. Thrombectomy
8. Angioplasty
9. Stent placement
10. Atherectomy
11. Central venous access
(non-tunneled/PICC line)
12. Central venous access
(tunneled/port)
C. Abdominal
1. Abdominal aortography
2. Selective visceral angiography
3. Renal angiography
4. Adrenal angiography
5. Reproductive angiography
6. Inferior vena cava
7. Embolization
8. Angioplasty
9. Stent placement
10. Stent graft placement
11. Caval filter placement
12. Caval filter removal
13. Venous sampling
14. TIPS
15. Chemoembolization
F. Miscellaneous
1.
2.
3.
4.
E-5
Biopsy
Percutaneous drainage
Removal of foreign body
Radiofrequency ablation
Clinical Experience Documentation Form
Vascular-Interventional Radiography
C ANDIDATE N AME
ARRT #
All procedures must be performed on patients (not phantoms or simulated patients). Procedures must be
verified and initialed by a Registered Technologist or a licensed physician and must match the Verification
Identification Page at the end of this document. The name and address of the person corresponding to
each set of initials must also be provided on the Verification Identification Page. List procedures in the
order they are listed on the preceding page, with like procedures grouped together. See the example
below. If all of your clinicals are completed at the same facility, documenting the facility name once is
sufficient. Only those procedures completed within the 24 months preceding the application signature will
be accepted.
Verifier’s Initials
Date
mm/dd/yy
Time of
Day
Facility Name
Example – renal angiography
01/05/11
10:00 a.m.
General Hospital
renal angiography
01/10/11
2:00 p.m.
renal angiography
01/20/11
10:00 a.m.
renal angiography
02/01/11
1:00 p.m.
renal angiography
02/25/11
10:00 a.m.
renal stent
01/05/11
10:05 a.m.
renal stent – RT
01/10/11
2:15 p.m.
General Hospital
renal stent – LF
01/10/11
2.25 p.m.
General Hospital
Procedures Performed
University Hospital
This form may be duplicated.
E-6
(handwritten)
C ANDIDATE N AME
Procedures Performed
ARRT #
Date
mm/dd/yy
Time of
Day
This form may be duplicated.
E-7
Verifier’s Initials
Facility Name
(handwritten)
C ANDIDATE N AME
ARRT ID #
VERIFICATION IDENTIFICATION PAGE
The previous pages of the Vascular-Interventional Radiography Clinical Experience Documentation Form
require only that the initials of the person verifying performance of a procedure be listed. On this page, the
verifiers must provide their full name and mailing address to match their initials on the previous pages.
These individuals may be contacted as part of the audit process. Registered Technologists should list their
home mailing address that is on file with ARRT. Other verifiers may list the facility address.
Verifier’s Initials
(handwritten)
Verifier’s Initials
(handwritten)
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Printed Name
Printed Name
Mailing Address
Mailing Address
City/State/Zip
City/State/Zip
Verifier’s Initials
(handwritten)
Verifier’s Initials
(handwritten)
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Printed Name
Printed Name
Mailing Address
Mailing Address
City/State/Zip
City/State/Zip
Verifier’s Initials
(handwritten)
Verifier’s Initials
(handwritten)
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Printed Name
Printed Name
Mailing Address
Mailing Address
City/State/Zip
City/State/Zip
Verifier’s Initials
(handwritten)
Verifier’s Initials
(handwritten))
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Verifying technologist ARRT ID # and credentials (if applicable)
Others, please note credentials this space
Printed Name
Printed Name
Mailing Address
Mailing Address
City/State/Zip
City/State/Zip
This form may be duplicated
Appendix F
References
F-1
American Educational Research Association, American Psychological Association, & National
Council on Measurement in Education (1999). Standards for Educational and
Psychological Testing. Washington DC: American Educational Research Association.
Babcock, B., & Yoes, M. E. (in press). Enhancing job analysis surveys in the medical specialties with
CMS data. Evaluation & the Health Sciences.
Bradley, R. A., & Terry, M. E. (1952). Rank analysis of incomplete block designs I: The method of
paired comparisons. Biometrika, 39, 324-345.
Equal Employment Opportunity Commission, Civil Service Commission, Department of
Labor, & Department of Justice. (1978). Adoption by four agencies of uniform guidelines
of employee selection procedures. Federal Register, 43(166), 38290-38315.
Luce, R. D. (1959). Individual choice behavior. New York: Wiley.
National Commission for Certifying Agencies (2004). Standards for the accreditation of
certification programs. Washington, DC: Author.
Raymond, M.R. (2001). Job analysis and the specification of content for licensure and
certification examinations. Applied Measurement in Education, 14, 369-415.
Reid, J.B. (1983). ARRT Job analysis project. Applied Radiology, 12, 27-32.
F-2