Additional Coding Guidelines - Health Network Laboratories
advertisement

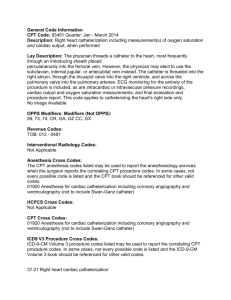
Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report This is CMS Logo. Additional Coding Guidelines 190.12 – Urine Culture, Bacterial 1. 2. 3. Specific coding guidelines: a. Use CPT 87086 Culture, bacterial, urine; quantitative, colony count where a urine culture colony count is performed to determine the approximate number of bacteria present per milliliter of urine. The number of units of service is determined by the number of specimens. b. Use CPT 87088 where a commercial kit uses manufacturer defined media for isolation, presumptive identification, and quantitation of morphotypes present. The number of units of service is determined by the number of specimens. c. Use CPT 87088 where identification of morphotypes recovered by quantitative culture or commercial kits and deemed to represent significant bacteriuria requires the use of additional testing, for example, biochemical test procedures on colonies. Identification based solely on visual observation of the primary media is usually not adequate to justify use of this code. The number of units of service is determined by the number of isolates. d. Use CPT 87184 or 87186 where susceptibility testing of isolates deemed to be significant is performed concurrently with identification. The number of units of service is determined by the number of isolates. These codes are not exclusively used for urine cultures but are appropriate for isolates from other sources as well. e. Appropriate combinations are as follows: CPT 87086, 1 per specimen with 87088, 1 per isolate and 87184 or 87186 where appropriate. f. Culture for other specific organism groups not ordinarily recovered by media used for aerobic urine culture may require use of additional CPT codes (for example, anaerobes from suprapubic samples). g. Identification of isolates by non-routine, nonbiochemical methods may be coded appropriately (for example, immunologic identification of streptococci, nucleic acid techniques for identification of N. gonorrhoeae). h. While infrequently used, sensitivity studies by methods other than CPT 87184 or 87186 are appropriate. CPT 87181, agar dilution method, each antibiotic or CPT 87188, macrotube dilution method, each antibiotic may be used. The number of units of service is the number of antibiotics multiplied by the number of unique isolates. ICD-9-CM code 780.02, 780.9 or 799.3 should be used only in the situation of an elderly patient, immunocompromised patient or patient with neurologic disorder who presents without typical manifestations of a urinary tract infection but who presents with one of the following signs or symptoms, not otherwise explained by another co-existing condition: increasing debility; declining functional status; acute mental changes; changes in awareness; or hypothermia. In cases of post renal-transplant urine culture used to detect clinically significant occult infection in patients on long term immunosuppressive therapy, use code V58.69. *October 14 Changes – Red Fu Associates, Ltd. 9 October 2014 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report This is CMS Logo. 190.13 – Human Immunodeficiency Virus (HIV) Testing (Prognosis Including Monitoring) 1. 2. Specific coding guidelines: a. Temporary code G0100 has been superseded by code 87536 effective January 1, 1998. b. CPT codes for quantification should not be used simultaneously with other nucleic acid detection codes for HIV-1 (that is, 87534, 87535) or HIV-2 (that is, 87537, 87538). Codes 647.60-647.64 should only be used for HIV infections complicating pregnancy. 190.14 - Human Immunodeficiency Virus (HIV) Testing (Diagnosis) 1. Specific coding guidelines: a. CPT 86701 or 86703 is performed initially. CPT 86702 is performed when 86701 is negative and clinical suspicion of HIV-2 exists. b. CPT 86689 is performed only on samples repeatedly positive by 86701, 86702, or 86703. c. CPT 87534 or 87535 is used to detect HIV-1 RNA where indicated. CPT 87537 or 87538 is used to detect HIV-2 RNA where indicated. 190.16 – Partial Thromboplastin Time (PTT) 1. 2. 3. 4. When patients are being converted from heparin therapy to warfarin therapy, use code V58.61 to document the medical necessity of the PTT. When coding for Disseminated Intravascular Coagulation (DIC), use 286.6 or code for the signs and symptoms clinically indicating DIC. If a specific condition is known and is the reason for a pre-operative test, submit the clinical text description or ICD-9-CM code describing the condition with the order/referral. If a specific condition or disease is not known, and the pre-operative test is for pre-operative clearance only, assign code V72.84. Assign codes 289.8 – other specified disease of blood and blood-forming organs only when a specific disease exists and is indexed to 289.8, (for example, myelofibrosis). Do not assign code 289.8 to report a patient on long term use of anticoagulant therapy (for example, to report a PTT value or re-check need for medication adjustment.) Assign code V58.61 to referrals for PTT checks or re-checks. (Reference AHA’s Coding Clinic, March-April, pg 12 – 1987, 2nd quarter pg 8 – 1989) 190.17 – Prothrombin Time (PT) 1. 2. If a specific condition is known and is the reason for a pre-operative test, submit the text description or ICD-9-CM code describing the condition with the order/referral. If a specific condition or disease is not known, and the pre-operative test is for preoperative clearance only, assign code V72.84. Assign codes 289.8 – other specified disease of blood and blood-forming organs only when a specific disease exists and is indexed to 289.8 (for example, myelofibrosis). Do not assign code 289.8 to report a patient on long term use of anticoagulant therapy (e.g. to report a PT value or re-check need for medication adjustment.) Assign code *October 14 Changes – Red Fu Associates, Ltd. 10 October 2014 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report This is CMS Logo. V58.61 to referrals for PT checks or re-checks. (Reference AHA’s Coding Clinic, March-April, pg 12 – 1987, 2nd quarter pg 8 – 1989) 190.19 – Collagen Crosslinks, Any Method 1. When the indication for the test is long-term administration of glucocorticosteroids, use ICD-9-CM code V58.69. 190.20 – Blood Glucose Testing 1. 2. 3. 4. 5. A diagnostic statement of impaired glucose tolerance must be evaluated in the context of the documentation in the medical record in order to assign the most accurate ICD-9CM code. An abnormally elevated fasting blood glucose level in the absence of the diagnosis of diabetes is classified to Code 790.6 - other abnormal blood chemistry. If the provider bases the diagnostic statement of impaired glucose tolerance” on an abnormal glucose tolerance test, the condition is classified to 790.2 -- normal glucose tolerance test. Both conditions are considered indications for ordering glycated hemoglobin or glycated protein testing in the absence of the diagnosis of diabetes mellitus. When a patient is under treatment for a condition for which the tests in this policy are applicable, the ICD-9-CM code that best describes the condition is most frequently listed as the reason for the test. When laboratory testing is done solely to monitor response to medication, the most accurate ICD-9-CM code to describe the reason for the test would be V58.69 -- long term use of medication. Periodic follow-up for encounters for laboratory testing for a patient with a prior history of a disease, who is no longer under treatment for the condition, would be coded with an appropriate code from the V67 category -- follow-up examination. According to ICD-9-CM coding conventions, codes that appear in italics in the Alphabetic and/or Tabular columns of ICD-9-CM are considered manifestation codes that require the underlying condition to be coded and sequenced ahead of the manifestation. For example, the diagnostic statement, “thyrotoxic exophthalmos (376.21),” which appears in italics in the tabular listing, requires that the thyroid disorder (242.0-242.9) is coded and sequenced ahead of thyrotoxic exophthalmos. Therefore, a diagnostic statement that is listed as a manifestation in ICD-9-CM must be expanded to include the underlying disease in order to accurately code the condition. 190.21 – Glycated Hemoglobin/Glycated Protein 1. A diagnostic statement of impaired glucose tolerance must be evaluated in the context of the documentation in the medical record in order to assign the most accurate ICD-9CM code. An abnormally elevated fasting blood glucose level in the absence of the diagnosis of diabetes is classified to Code 790.6 - other abnormal blood chemistry. If the provider bases the diagnostic statement of impaired glucose tolerance” on an abnormal glucose tolerance test, the condition is classified to 790.2 -- normal glucose tolerance test. Both conditions are considered indications for ordering glycated hemoglobin or glycated protein testing in the absence of the diagnosis of diabetes mellitus. *October 14 Changes – Red Fu Associates, Ltd. 11 October 2014 Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report This is CMS Logo. 190.22 – Thyroid Testing 1. 2. 3. 4. 5. 6. When a patient is under treatment for a condition for which the tests in this policy are applicable, the ICD-9-CM code that best describes the condition is most frequently listed as the reason for the test. When laboratory testing is done solely to monitor response to medication, the most accurate ICD-9-CM code to describe the reason for the test would be V58.69 - long term use of medication. Periodic follow-up for encounters for laboratory testing for a patient with a prior history of a disease, who is no longer under treatment for the condition, would be coded with an appropriate code from the V67 category -- follow-up examination. According to ICD-9-CM coding conventions, codes that appear in italics in the Alphabetic and/or Tabular columns of ICD-9-CM are considered manifestation codes that require the underlying condition to be coded and sequenced ahead of the manifestation. For example, the diagnostic statement “thyrotoxic exophthalmos (376.21),” which appears in italics in the tabular listing, requires that the thyroid disorder (242.0-242.9) is coded and sequenced ahead of thyrotoxic exophthalmos. Therefore, a diagnostic statement that is listed as a manifestation in ICD-9-CM must be expanded to include the underlying disease in order to accurately code the condition. Use code 728.9 to report muscle weakness as the indication for the test. Other diagnoses included in 728.9 do not support medical necessity. Use code 194.8 (Malignant neoplasm of other endocrine glands and related structures, other) to report multiple endocrine neoplasia syndromes (MEN-1 and MEN-2). Other diagnoses included in 194.8 do not support medical necessity. 190.26 – Carcinoembryonic Antigen 1. To show elevated CEA, use ICD-9-CM 790.99 (Other nonspecific findings on examination of blood) only if a more specific diagnosis has not been made. If a more specific diagnosis has been made, use the code for that diagnosis. 190.31 – Prostate Specific Antigen 1. To show elevated PSA, use ICD-9-CM code 790.93 (Elevated prostate specific antigen). If a more specific diagnosis code has been made, use the code for that diagnosis. *October 14 Changes – Red Fu Associates, Ltd. 12 October 2014