Medication Administration Record (MAR) Guidance for Care Homes
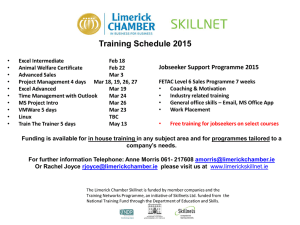
advertisement

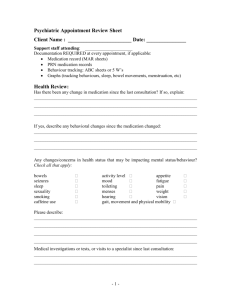
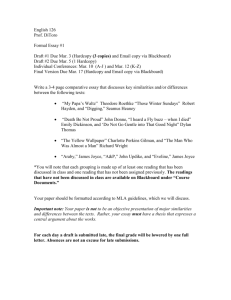
Using the Medication Administration Record (MAR) effectively Guidance Sheet 22 A MAR chart is the record that shows drugs have been administered to a patient. The carer signs each time a drug or device is administered to a patient. Carers administrating medication in the care home setting should be suitably trained and competent to do so. This should be documented and recorded by a senior carer or manager. General guidance on MAR charts 1. Care workers who give medication must have a MAR chart which details: a. Which medication(s) are prescribed for the patient b. When they must be given c. What the dose is d. Any special information, i.e. should the medication be given with food. 2. The MAR chart should be signed when the patient is administered an individual dose or a full pack if the patient self-administers. 3. The codes shown on the bottom of the MAR chart should be used when a medication is not given and possibly explained on the reverse of the chart. 4. The information on the MAR chart should be supplemented by the person’s care plan. The care plan should include personal preferences. For example the care worker giving the medication should be the same sex as the patient. 5. The MAR chart should be used to record medication which is carried over from a previous month. The printed MAR chart from the pharmacy may indicate that none of this medication has been supplied this month but the care worker is able to use the boxes below the medication box to indicate any medication carried over. Liaise with pharmacy to ensure all current medications are listed including those not ordered this cycle 6. The MAR chart should be used to record when any non-prescribed medication is given to a patient. For example a homely remedy. 7. Administrations of controlled drugs (CDs) should be recorded on the MAR chart as well as in the CD register with the same 2 witness signatures . How to keep a MAR chart up to date 1. Responsibility for providing and using MAR charts is with the care provider, not the dispensing GP or pharmacy. 2. Under the general medical services contract (GMS) the GP does not have to sign any documents produced by the care provider in relation to medicines administration. 3. There may be some incidences when it is appropriate to ask the GP to sign the MAR chart for example when they visit and change a dose of prescribed medication. 4. Poor records are a potential cause of preventable drug errors. Printed MAR charts are not essential but are better than handwritten MAR charts. This is due to less risk of error to: a. Incorrectly transcribing the details from another document b. Handwriting may be difficult to read or may be misunderstood. Where handwriting (this is necessary when new items are prescribed at times and on discharge from hospital) is the only option ensure that there is a robust system in place to check that the MAR is correct before it is used. Signing and countersigning are appropriate 5. Printed MAR charts are usually supplied by the pharmacy or dispensing GP when the medication is packaged though this is a complimentary service which the supplier is paying for and therefore care providers cannot insist on having a printed chart. Potential problem with MAR chart MAR charts are only correct at the time of printing New prescriptions can be issued at any time during a monthly cycle. This can result in a resident having a number of MAR charts, and some may have different start dates If the GP issues a new written prescription there should be a new MAR chart, but a new prescription is not always necessary Medicines prescribed ‘when required’ may not be required every month. The MAR chart may only be a list of medication prescribed and dispensed that month and therefore ‘when required’ medication may not be listed The MAR chart should be supplemented by information that clearly describes the circumstances when ‘when required’ medication can be safely given The MAR chart may include medication which has not be supplied. Solution Anyone can change a MAR chart. But the care provider should have a system in place to check the source and accuracy of the changes. A cross reference to the patients notes is recommended. When a residents medication is changed carers have responsibility to amend the MAR chart: a. Cancel the original directions b. Write the new directions legibly and in ink on a new line of the MAR chart c. Write the name of the doctor or other prescriber who gave the new directions d. Date and sign the entry (including a witness when possible) Ensure that ‘when required’ medication is added onto the MAR chart or medication carried over Ensure that any supplementary information is on the MAR chart or in the patients care plan The care provider must check whether the prescriber has stopped the medication and if so cross it off, clearly document the reason i.e. stopped and date and sign it. If treatment is to continue, the care provider should check why there is no supply. What does good look like? 1. MAR charts form an essential element in determining whether people who use social care have been given medication as the prescriber instructed. Consider: a. Is the person’s name clearly identified? b. Is the print or handwriting legible and in ink? c. Are hand written entries cross linked to daily notes? d. Does the chart show the date including the year? e. Does the chart look ‘used’ an indication that it was completed at each medication administration? f. Are there gaps in the records? If so, do these need to be investigated further? g. Can the reader clearly identify exactly what has been given on specified dates, for example if the dose is one or two tablets? h. Is there sufficient information to enable care workers to give ‘when required’ medication safely? i. Is there a guide to the codes used to explain why a medicine has not been given? j. Can you confirm that the records are valid, for example by checking whether the number of signatures recorded for the administration of an antibiotic are consistent with the quantity supplied. k. In care homes can you cross reference records for controlled drugs on both the MAR chart and in the CD register? l. The route of administration should be recorded on the MAR sheet. 2. MAR charts may include details of medication received and disposed of, if this is not the case ensure these records are kept in another format. 3. Any allergies the patient has should be clearly identified on the MAR chart for the resident. If you receive printed MAR charts for your residents ensure the pharmacy or dispensing GP has a record of these so that they can be printed onto the MAR chart. Example MAR chart. Record Keeping Once the current monthly cycle has been finished it is a legal requirement for these records to be kept in the home even when the service user has left. It is recommended they be retained for a minimum of 3 years and should be retrievable, if needed. In the case of children’s homes medication records should be kept for at least 15 years. To contact us please email: D-CCG.CaringForCareHomes@nhs.net Version 1_2014 _Review Date: December 2016