here - Mental Health Foundation

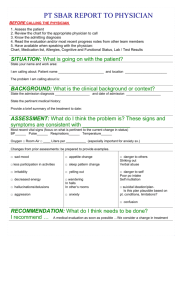
Objectives: This self study module provides a practical overview of the Mental Health
Act for staff, clients and families.
Before 1960, people with mental illnesses who had been institutionalized were considered incapable of making decisions. Patients received whatever course of treatment the physician recommended. In the 1970s, the mental health legislation was changed to include specific criteria for admission based on danger of behavior following the advice of the Law Reform Commission of Canada. Increased public awareness of mental health and patient rights in the 1980s resulted in the proclamation of Alberta
Mental Health Act in 1990 to regulate the admission and detention of individuals with mental illness, their treatment and control, and a process for review. In late 2007, Bill 31 received Royal Assent to amend this act by introducing community treatment orders and to replace the ‘dangerousness’ certification criteria with a ‘need for treatment’ type of criteria. It was another two years before Bill 31 was proclaimed.
Part One: Admission and Treatment in a Designated Facility
Families of people with a mental illness need to be well informed about their options during a psychotic episode or crisis. It is often a terrifying ordeal for both the family and the person with the illness. Crisis lines can be an invaluable source of support, information and even intervention. Families will find it helpful to know the three criteria for certification since that is what they will be questioned about repeatedly by police and health care providers. In some cases, obtaining a warrant of apprehension (Form 8) from
Family Court Services may be another route to obtain treatment. It is important to remember that the Mental Health Act is not a criminal law but sometimes the involvement of police may create this disturbing impression to clients and their families.
1. One Admission Certificate (also a conveyance certificate) (Form 1)
Any Physician can examine and issue an admission certificate within 24 hours of examination. All three criteria must be present:
(a) suffering from a mental disorder
(b) in a condition likely to cause harm to the person or others or to suffer substantial mental or physical deterioration or serious physical impairment,
(c) unsuitable for admission to a facility other than as a formal patient
A mental disorder is defined in the Act as a substantial disorder of thought, mood, perception, orientation, or memory that grossly impairs the person’s judgment, behavior, capacity to recognize reality and/or their ability to meet the ordinary demands of life .
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
One admission certificate is sufficient authority to:
(a) apprehend the person named in the certificate and convey the person to a facility within 72 hours of issue, and
(b) to care for, observe, examine, assess, treat, detain and control the person named in the certificate for a period of 24 hours from the time the person arrives at the facility. The physician must examine the person during this period and may let the first certificate expire, treat the patient as voluntary, discharge the patient, or issue a second certificate.
2. Two Admission Certificates (Form 1)
When two admission certificates are issued, the person becomes a formal or involuntary patient.
Two Admission Certificates are sufficient authority to care for, observe, examine, assess, treat, detain and control the person named in them for a period of one month from the date and time that the second Admission Certificate is issued. Admission certificates can be issued by any two physicians- a psychiatrist is not required - however, one of the physicians must be staff of the facility where the patient is to be detained.
3. Renewal Certificates (Form 2)
After a period of one month, if the patient still has all of the criteria for a formal patient, the period of detention of a formal patient can be extended with renewal certificates. The two certificates must be written by two physicians after separate examination of the patient. At least one of the physicians must be a psychiatrist and one must be staff of the facility. Two renewal certificates are sufficient authority to care for, observe, examine, assess, treat, detain and control the person for a period of not more than one month from the date of the second Renewal Certificate is issued.
•
Two renewal certificates the first and second time: 1 additional month
•
Two renewal certificates the third and subsequent times: 6 additional months (the patient must be given a mandatory review by the Review Panel)
4. Judge’s Warrant for Apprehension (Form 8)
Anyone who has reasonable and probable grounds to believe that a person is suffering from a mental disorder, and is in a condition presenting or likely to cause harm to the person or others or to suffer substantial mental or physical deterioration or serious physical impairment may bring information under oath before a provincial judge ( Form
7).
Anyone who has reasonable and probable grounds to believe that a person who is subject to a community treatment order is not complying with the community treatment order, may bring information under oath before a provincial judge.
The warrant issued by the Judge (Form 8) becomes sufficient authority for the police to apprehend, detain and convey that individual to any designated facility for examination. The warrant is good for seven days after it has been issued. If the patient
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
has not been apprehended during this time, the warrant ceases to be effective unless, before the expiry of the 7 day period, a judge extends the duration of the warrant, on the application of a peace officer. This can be extended only once for a period of up to another 7 days (Form 9) .
The warrant for apprehension (Form 8) is sufficient authority to care for, observe, assess, detain, and control that individual at a facility for a period of 24 hours.
5. Peace Officer’s Power (Form 10)
A peace officer may apprehend and convey an individual to a facility if the officer has reasonable and probable grounds to believe that
•
the individual is suffering from a mental disorder and is in a condition presenting a danger to himself or others, or the person is subject to a community treatment order and is not complying with the community treatment order and
•
that the person should be examined in the interests of the person’s own safety or for the safety of others.
A form 10 has the same authority as one Admission Certificate during apprehension and conveyance. It is valid for up to 24 hours from arrival at the facility (unless 2 admission certificates are issued).
Formal Patient Treatment and Control
1. Treatment
A patient can make treatment decisions if deemed mentally competent. If a formal patient objects to treatment, and is deemed to be mentally competent, then the physician can apply to the Review Panel for a treatment order (Form 12) . The treatment order may be issued if the Review Panel feels it is in the best interest of the patient to receive the treatment:
•
whether likely to be improved by the treatment
•
whether condition will deteriorate without treatment
•
whether anticipated benefit will outweigh the risk of harm; and
•
whether it is the least restrictive and least intrusive treatment
If an application is made to a review panel to review the physician’s opinion of
incompetence, no one may act on the opinion pending the outcome of the application
2. Incompetence
If the patient objects to treatment and is in the opinion that the patient is not mentally competent, the physician can complete and file with the board a certificate indicating written reasons for the opinion that the formal patient is not mentally competent to give informed treatment consent (Form 11 ).
Both the patient and the next of kin/guardian/agent are given copies of this form and either one can object in writing to the Review Panel. The purpose of this procedure is to obtain consent for treatment decisions as a substitute decision maker on behalf of the incompetent formal patient or the formal patient who is a minor.
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
If the next of kin/guardian/agent of the incompetent formal patient is unwilling to make treatment decisions or if there is no one available, the physician can apply to the Office of the Public Guardian to get a Substitute Decision Maker of Last Resort.
If the patient objects to treatment (but has not appealed), a second physician must also examine the formal patient and agree that the patient is not mentally competent before acting on the substitute consent. The patient may appeal the Physician’s
Certificate of incompetence or the substitute decision maker may object to treatment. In either case, the physician may then apply to the Review Panel for a Treatment Order.
However, no treatment may be given by anyone pending the outcome of the application.
3. Control
The physician has the authority to control any patient without the patient’s consent.
Control is defined as the minimal use of force, mechanical means or medication as is reasonable, with regard to the physical and mental condition of the person to prevent serious bodily harm to the person or another person. This applies to all patients, not only psychiatric or formal patients.
The use of medication for the purposes of control versus treatment is not much different. It is important, however, to document the use of medication and to describe the behavior in such circumstances as the use for control and not as for treatment.
Duties toward Formal Patients
1. Notification
In accordance with the Mental Health Act, when two admission or renewal certificates are issued, the board shall inform the formal patient and the person’s guardian or designate (if any). They must also make a reasonable effort to inform the next of kin (unless the patient objects). A copy of the certificates is given to the patient and a copy is given to the guardian/next of kin /agent (if applicable).
The patient and others must be informed, in simple language, of:
• The reason for issuance of certificates
• The authority for detention and the period of it
• Name and address of chair of review panel
• Notice of the right:
– to apply to a Review Panel for cancellation of certificates
– to appeal treatment orders
– to appeal finding of incompetence
– to retain and instruct counsel without obstruction
• Notice when certificates have expired or been cancelled
Both written information and verbal explanations must be given. Provide pamphlets about rights and copies of all certificates/documents. An interpreter must be provided by the facility, if necessary to facilitate understanding.
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
2. Documentation
The following documentation in the patient’s record is necessary:
1) Patient’s and Other’s receipt of:
•
Certificates
•
Verbal and written information about formal status, reasons, duration and legal rights
2) Date the actions were completed
3) Patient’s awareness and understanding of formal status and legal rights
4) Patient’s response to information, behavior and mental status
5) If an appeal is being made
6) Patient’s consent to treatment
7) Patient’s refusal of treatment
3. Discharge/ Cancellation of Certificates
Certificates can be cancelled and the patient be treated as a voluntary patient or be discharged by any of the following methods: b) Review Panel cancels (criteria not met) c) Physician cancels (criteria not met)
When a patient is discharged from a facility notice shall be given to the patient’s:
(b) nearest relative, unless the patient being discharged objects, and
(c) family doctor, if known, along with the discharge summary, including any recommendations for treatment
4. Leave of Absence
Formal patients may be granted a leave of absence by their physician.
When a leave of absence has not been granted, an order granting authority to a peace officer to apprehend and return the formal patient may be obtained (Form 3) . If the Formal Patient expires for any reason, in or out of the hospital, the Medical Examiner must be notified.
5. Formal Patient Rights
In addition to the right to be informed as described in Duties toward Patients ,
Formal patients have the right to:
•
Contact and receive visits from a lawyer at any time.
•
Receive visitors during regular hospital visiting hours unless their physician thinks that a visitor would be harmful to their health.
•
Confidentiality of any communications written by or to the patient. Staff cannot open, read, withhold or interfere with the delivery of a formal patient’s letters or notes.
•
Contact the Alberta Mental Health Patient Advocate Office regarding any questions or concerns they may have with respect to their rights, treatment or care. They should call 780 422-1812 in Edmonton or toll free at 310.0000
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
Part Two: Community Treatment Orders (CT0)
A community treatment order provides a legal mechanism whereby a person can receive mandatory treatment for a mental disorder in a community setting. It is a tool meant to assist people in maintaining treatment compliance. The CTO can be written for someone living in the community with no history of hospitalization if other criteria are met.
1. Criteria for CTO
A community treatment order may be issued after separate examinations of a person by 2 physicians (one must be a psychiatrist) within the immediately preceding 72 hours if:
(a) the person is suffering from a mental disorder and
(b) one or more of the following apply:
(i) within the immediately preceding 3-year period the person has on 2 or more occasions, or for a total of at least 30 days,
(A) been a formal patient in a facility,
(B) been in an approved hospital or been lawfully detained in a custodial institution where the person would have met the admission criteria set out in 2(a) and (b), or and/or
(C) a combination of (A) and (B);
(ii) the person has within the immediately preceding 3-year period been subject to a community treatment order; and/or
(iii) the person has, while living in the community, exhibited a pattern of recurrent or repetitive behaviour that indicates that the person is likely to cause harm to the person or others or to suffer substantial mental or physical deterioration or serious physical impairment if the person does not receive continuing treatment or care while living in the community, and
(c) both physicians are of the opinion that the person is likely to cause harm to the person or others or to suffer substantial mental or physical deterioration or serious physical impairment if the person does not receive continuing treatment or care while living in the community, and
(d) the treatment or care the person requires exists in the community, is available to the person and will be provided to the person, and
(e) in the opinion of each physician, the person is able to comply with the treatment or care requirements set out in the community treatment order, and
(f) either (i) or (ii)
(i) consent has been obtained,
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
(A) if the person is competent, from the person, or
(B) if the person is not competent, following the formal treatment process or
(ii) consent has not been obtained but in the opinion of the issuing physicians
(A) the person has, while living in the community, exhibited a history of not obtaining or continuing with treatment or care that is necessary to prevent the likelihood of harm to others, and
(B) a community treatment order is reasonable in the circumstances and would be less restrictive than holding the person as a formal patient.
2. Issuance of the CTO (Form 19)
The community treatment order must include dates and location of the examinations, the facts by which the physicians formed their opinions, specify the treatment or care to be followed, and identify the person responsible for supervising the CTO and related reporting obligations. Form 19 is completed by:
Part 1 & 2: Physician, Psychiatrist or Designated Physician (Act requires 2 physicians, one of whom must be a psychiatrist or designated physician);
Part 3: Treatment or Care Provider.
If treatment/care is provided by Alberta Health Services (AHS) this part must be signed by person designated by AHS. June Clark, Director, Adults and Seniors- North has been designated as the representative for the Edmonton Zone. This authority can be delegated to facilitate appropriate and timely collaboration necessary for the development of a treatment plan. Eric Pearce, Supervisor (North Central) has been delegated with these responsibilities. No other AHS staff in the Edmonton Zone should sign Part 3. If a physician is the care provider, the physician provider must sign Part 3 since physicians are not employees of Alberta Health Services.
Part 4: Psychiatrist or Physician responsible for supervising CTO;
Part 5: Person consenting to CTO or Issuing Psychiatrist
Note: If psychiatrist not available a physician may be designated under MHA 9.7(1).
Designated physician must consult with a psychiatrist prior to issuing, renewing, amending or canceling a CTO. Designation is for maximum 2 years. (Form 25)
3. Duration and Renewal of CTO (Form 20)
Community treatment orders expire 6 months after the date of issuance unless they are renewed or cancelled before expiry. As long as the person continues to meet the criteria, there is no limit on how many times a CTO may be renewed. There is a mandatory review panel on the first renewal and at the time of every 2 nd
renewal.
(Form 20) is filled out by:
Part 1 & 2: is completed by the Physician, Psychiatrist or Designated Physician.
(Act requires 2 physicians, one of whom must be a psychiatrist or designated physician)
Part 3 is completed by Treatment or Care Provider. If the treatment/care is provided by AHS, it must be signed by person designated by AHS and not individual provider. (see Form 19 above)
Part 4: completed by Psychiatrist or Physician responsible for supervising the
CTO;
Part 5: Person consenting to CTO or Issuing Psychiatrist
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
4. Consequences of Non-compliance
Providers of treatment or care to the person who is subject to the CTO are required to report any failure to comply by completing ( Form 27) and submitting it to Alberta
Health Services in their zone within 24 hours. If a psychiatrist is satisfied that reasonable assistance has been provided to the person to help them comply with the Community
Treatment Order and the person fails to comply, the psychiatrist may issue an order for apprehension and assessment (Form 23) . Prior to apprehension, the person must be informed:
•
that they have failed to comply with the Community Treatment Order
•
that an order for apprehension and assessment may be issued and
•
of the possible consequences of that assessment.
If the person does not comply and is conveyed to a facility, an examination of the person must be conducted by 2 physicians (one must be a psychiatrist) within 72 hours
(Form 24) . The physicians may:
•
cancel the CTO and release the person ( Form 22) or
•
amend and continue the CTO (Form 21) or
•
cancel the CTO (Form 22) and issue admission certificates (Form 1) .
5. Notification
(a) Issuance, amendment or renewal of CTO (Form 26)
When a community treatment order is issued, amended or renewed, a written statement must be prepared which includes:
•
the reason, in simple language, for the issuance, amendment or renewal
•
the authority for the issuance, amendment or renewal
•
information regarding the function of review panels,
•
the name and address of the chair of the appropriate review panel, and
•
the right of the person to apply to the review panel for cancellation of the community treatment order,
This written statement and other related notices and information must be given to:
•
the person who is subject to the community treatment order,
•
any person who exercises authority under section 28(1) to make treatment decisions on behalf of the person
•
any persons providing treatment or care to the person related to the CTO
•
any other person prescribed in the regulations.
In the case of language difficulty, an interpreter must be provided to facilitate understanding.
(b) Cancellation or expiry
When a community treatment order expires or is cancelled, notice of the expiry or
cancellation, along with any recommendations for treatment, must be given to
•
the person who was subject to the community treatment order
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
•
to the persons who were given a written statement under 14(1.1)
•
to the person’s family doctor, if known.
Review Panel
Upon proper application, formal patients or individuals subject to community treatment orders may have their cases reviewed (with or without counsel present) by the
Review Panel. The MHA also designates certain mandatory review panels for formal patients (at the time of issuance of a 3rd set of renewal certificates) and persons subject to a CTO (on the first renewal of the CTO and on every 2 nd
renewal thereafter).
On receipt of an application, the review panel shall give at least 7 days of notice for the date, time, place, and purpose of hearing, and make a decision ASAP within 21 days of receipt of application. A review panel must take place and make a decision within 7 days of receipt of application .
The Review Panel consists of 4 members:
•
Chairman or Vice Chairman (lawyer) - 1or 2 votes
•
Psychiatrist (not from same facility and not involved with patient) - 1 vote
•
General Physician – 1 vote
•
Member of the general public - 1 vote
At the hearing, the attending psychiatrist, along with any other professional staff involved with the patient, may be asked to be present. The Review Panel, after hearing and reviewing the case can either uphold or cancel the certificates. If upheld, the patient or next of kin/guardian/agent can appeal the decision to the Court of Queen’s Bench within 14 days (lawyer can apply to the court to hold all treatment pending outcome).
Legal counsel may visit the formal patient at any time and not be restricted by visiting hour policy at the facility. If Legal counsel chooses not to have the staff present, the request is honored and the staff remains outside the room. If Legal counsel chooses to have the staff remain, the staff does not participate in the interview.
If the formal patient’s legal counsel asks to see the medical record, there are requirements in the Health Information Act about what information must be removed
(“severed”) before providing access to a copy. For example, any health information about an individual other than the patient that was from a source other than the patient must not be in the copy given to the lawyer. The patient must also give consent.
According to HIA, Section 34, consent must include authorization for specific health information, identification of the recipient, explanation of why the information is needed and the risks/benefits of consenting/refusing, date effective (expiry date is not required), and revocation statement.
Mental Health Patient Advocate
The Mental Health Patient Advocate reports directly to the Minister and investigates complaints/concerns of formal patients. The advocate also provides information about patient rights, the process to obtain legal counsel, the process to appeal to the review board, and the process to appeal to Court of Queen’s Bench. Call 780 422-1812 or visit www.mhpa.ab.ca
for more information.
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca
CTO Coordination
CTO Coordinators assist the Zones in process development, problem solving, education, tracking, and evaluation. They are not responsible for the distribution of
Forms nor will they be the Designate from the Zone. The Designate also "coordinates" with the Coordinator to allow for "overarching" coordination. The Coordinator has specific knowledge regarding the status of CTO orders and works with the Zone-based designate.
Conclusion
Loss of judgment and insight commonly occurs with all types of mental illness with varying severity and duration. The Mental Health Act is an attempt to ensure that when people are no longer able to maintain their own safety that there are legal safeguards in place to ensure their protection. Patients may experience this protection as a loss of freedom to choose. Regardless of the circumstances, this experience is real and can be distressing. On the other hand, families often feel helpless and angry when their loved ones go untreated because they may not meet the full legal criteria for involuntary admission. The application of the Mental Health Act must be done in a way that builds trust and rapport with all those involved. Although safety may sometimes become an immediate priority, the overall goal of interventions is always recovery.
Guidelines in a Crisis
1) Try to appear calm.
2) Decrease distractions, such as a TV or other people in the room.
3) Only one person talks at a time.
4) Speak slowly and clearly.
5) Make statements about the behavior you are observing now.
6) Avoid authoritative or challenging statements.
7) Repeat questions or statements as necessary. Always use exactly the same words each time.
8) Allow lots of personal space and avoid continuous eye contact.
9) Avoid trying to reason with the person.
10) Do not argue with others about what to do in the person’s presence.
11) Do not block the doorway.
Adapted from Schizophrenia: A Handbook for Families by Health Canada
Information & Evaluation Services January 2010 daniel.scott@albertahealthservices.ca