Hematocrit Determination
advertisement

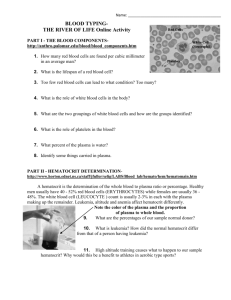
OBJECTIVES • To become familiar with the “normal” values obtained with selected blood tests. • To understand how common laboratory procedures for examining blood can indicate pathology, or a state of disease. • To learn how the following blood tests are performed: o hematocrit (packed cell volume) determination o blood typing • To understand what each of these procedures is measuring in a sample of blood. • To realize the importance of proper disposal of laboratory equipment that has come in contact with blood. • To understand the importance of matching blood types for blood transfusions. Blood transports soluble substances to and from all cells of the body. Blood cells are also important in defense against pathogens. Laboratory analysis of the blood gives important information about how well these functions are being carried out. This lab exercise consists of five common laboratory tests performed on blood: hematocrit determination; erythrocyte sedimentation rate; hemoglobin determination; blood typing; and total cholesterol determination. Today, you will use software to do simulations of Hematocrit Determination, and Blood Typing. Hematocrit Determination Pre-Lab Questions: Answer the following question be reading the passage on Hematocrit Determination below: 1. What does Hematocrit mean? 2. How is Hematocrit level determined? 3. What is the average hematocrit level for males? __________ for females? ____________ 4. What is Anemia? 5. What is Polycythemia? Hematocrit refers to the percentage of red blood cells (RBCs) in a sample of whole blood. A hematocrit of 48 means that 48% of the volume of blood is red blood cells. Since the function of red blood cells is the transport of oxygen to the cells of the body, the higher the hematocrit, the more red blood cells are available to carry oxygen. Hematocrit values are determined by spinning a microcapillary tube filled with a whole blood sample in a special microhematocrit centrifuge. This procedure separates the blood cells from the blood plasma and leaves a “buffy coat” layer of white blood cells between the heavier red blood cell layer and the lighter plasma. The hematocrit value can be determined after centrifuging by measuring the height of the layer of red cells in millimeters and dividing that number by the height of the initial column of blood to obtain the percentage of red blood cells. The percentage of white blood cells PAGE 1 OF 8 (WBCs) can also be determined after centrifuging by comparing the height of the buffy coat to the initial height of the blood column. The average hematocrit value for males is 47%, and the average for females is 42%. The normal upper limit is 55%. A lower-than-normal hematocrit indicates anemia. A higher-than-normal hematocrit indicates polycythemia. Anemia is a condition in which insufficient oxygen is transported to the body’s cells. There are many possible causes for anemia, including inadequate numbers of red blood cells, decreased amount of the oxygen-carrying pigment hemoglobin, and abnormal hemoglobin. The heme portion of hemoglobin molecules contains an atom of iron. If adequate iron is not available, the body cannot manufacture hemoglobin. This results in a condition called iron-deficiency anemia. Aplastic anemia is the result of the failure of the bone marrow to produce adequate blood cells. Pernicious anemia is due to a lack of vitamin B12, which is necessary for cell division. Intrinsic factor, produced by the stomach, allows absorption of vitamin B12. Individuals who do not produce adequate intrinsic factor, or individuals who do not have adequate vitamin B12 in their diet, will suffer from pernicious anemia. Sickle cell anemia is an inherited condition in which the protein portion of hemoglobin molecules is folded incorrectly. As a result, oxygen molecules cannot fit with the misshapen hemoglobin, and anemia results. Polycythemia refers to a significant increase in red blood cells. There are many possible causes of polycythemia, including living at high altitudes, strenuous athletic training, and tumors in the bone marrow. HEMATOCRIT DETERMINATION PROCEDURE In the following activity, we will simulate the blood test that is used to determine hematocrit. From the main menu, select Blood Analysis. You will see the opening screen for the Hematocrit Determination experiment (Figure 11.1). To familiarize yourself with the equipment, select Help from the menu bar and then select Balloons On. This feature allows you to scroll around the screen and view equipment labels. You can turn the feature off by returning to Help and then selecting Balloons Off. In the upper right portion of the screen is a dispenser containing six thin tubes, which are heparinized capillary PAGE 2 OF 8 tubes. Heparin is a substance that keeps blood from clotting. Below the capillary tubes are six test tubes containing samples of blood to be tested. When a capillary tube is dragged to a test tube of blood, it partially fills by fluid capillary action. To the left of the samples of blood is a container of capillary tube sealer (a clay material, shown on-screen as an orange-yellow substance). The capillary tubes must be sealed on one end with this tube sealer so that the blood sample can be centrifuged without spraying out the blood. When the tubes have been sealed, they are moved to slots in the microhematocrit centrifuge. When the Start button is clicked, the centrifuge will rotate at 14,500 revolutions per minute. After the centrifuge stops and opens, the capillary tubes are moved, one at a time, next to the metric ruler on the upper left of the screen. When you click on the Record Data button next to the data table at the bottom of the screen, the following information about the sample will be recorded: the height of the column of blood in millimeters, the height of the red blood cell layer, the height of the buffy coat (white blood cells), the hematocrit (percentage of red blood cells) and the percentage of white blood cells. In the lower left corner of the screen is a contaminated disposal container. Every piece of glassware that has come in contact with the blood must be disposed of by dragging it to this container for proper disposal. Hematocrit Determination Simulation The following individuals have contributed their blood for this test: Sample 1: healthy male, living in Boston Sample 2: healthy female, living in Boston Sample 3: healthy male, living in Denver Sample 4: healthy female, living in Denver Sample 5: male with aplastic anemia Sample 6: female with iron-deficiency anemia 1) Click and drag one heparinized capillary tube over to the test tube containing blood sample 1. Make sure the capillary tube is touching the blood. The capillary tube will fill itself by fluid capillary action. 2) Drag the capillary tube containing sample 1 to the container of capillary tube sealer to “seal” one end of the tube. 3) Drag the capillary tube to the microhematocrit centrifuge. 4) Repeat steps 1–3 for the remaining five samples of blood. 5) Set the timer for the centrifuge for 5 minutes by clicking the () button, and then click the Start button. 6) When the centrifuge stops and opens, click and drag capillary tube 1 to the metric ruler. 7) Click Record Data to record the information about sample 1. 8) Click and drag capillary tube 1 to the contaminated disposal container. 9) Repeat steps 6–8 for the remaining five capillary tubes in the centrifuge. 10) Fill in Chart 1 with the data you collected. If you wish to restart or repeat the lab, click the Reset button next to the data table. PAGE 3 OF 8 HEMATOCRIT DETERMINATION POST LAB QUESTIONS: 1. What is the hematocrit value of a healthy male living at sea level in Boston? 2. What is the hematocrit value of a healthy male living at one mile elevation in Denver? 3. Is there as much oxygen in the air in Denver as there is in Boston? 4. How do your kidneys respond to a decrease in blood oxygen? (Review this section in your textbook if necessary.) 5. If your bone marrow is producing an elevated number of red blood cells, what happens to your hematocrit? 6. What is the hematocrit value of the male with aplastic anemia? 7. Would the red blood cell count for an individual with aplastic anemia be higher, lower, or the same as the red blood cell count of a healthy individual? 8. What is the hematocrit value of a healthy female living in Boston? 9. Explain the difference in hematocrit values obtained from a healthy female living in Boston and a female with irondeficiency anemia. PAGE 4 OF 8 Blood Typing Pre-Lab Questions: Answer the following questions after reading the passage about Blood Typing. 1. What are the surface antigens on red blood cells called? 2. Which Red Blood Cell surface proteins cause the most vigorous and potentially fatal transfusion reactions? 3. What does agglutinate mean? 4. When testing for blood type, if the blood agglutinates in anti-sera containing Anti-A antibodies, but not in antisera containing Anti-B antibodies, what is the ABO blood type? All of the cells in the human body, including the red blood cells, are surrounded by a plasma (cell) membrane. The plasma membrane contains genetically determined glycoproteins, called antigens, that identify the cells. On red blood cell membranes, these antigens are called agglutinogens. It is important to determine blood types before performing blood transfusions in order to avoid mixing incompatible blood. Although many different antigens are present on red blood cell membranes, the ABO and Rh antigens cause the most vigorous and potentially fatal transfusion reactions. If a blood transfusion recipient has antibodies (called agglutinins) to the antigens present on the transfused cells, the red blood cells will be clumped together, or agglutinated, and then lysed. This results in a potentially life-threatening blood transfusion reaction. The ABO blood groups are determined by the presence or absence of two antigens: type A and type B (see Figure 11.4b). These antigens are genetically determined so a person has two copies (alleles) of the gene for these proteins, one copy from each parent. The presence of these antigens is due to a dominant gene, and their absence is due to a recessive gene. • A person with type A blood can have two gene alleles for the A antigen, or that person could have one gene allele for type A antigen and the other allele for the absence of either A or B antigen. • A person with type B blood can have two gene alleles for the B antigen, or that person could have one gene allele for type B antigen and the other allele for the absence of either A or B antigen. • A person with type AB blood has one gene allele for the A antigen and the other allele for the B antigen. • A person with type O blood will have inherited two recessive gene alleles and has neither type A nor type B antigen. Antibodies to the A and B antigens are found preformed in the blood plasma. A person has antibodies only for the antigens not on his or her red blood cells, so a person with type A blood will have anti-B antibodies. This is summarized in Chart 4. The Rh factor is another genetically determined protein that may be present on red blood cell membranes. Approximately 85% of the population is Rh positive and has this protein. Antibodies to the Rh factor are not found preformed in the plasma. These antibodies are produced only after exposure to the Rh factor by persons who are Rh negative. Separate drops of a blood sample are mixed with antisera containing antibodies to the types A and B antigens and antibodies to the Rh factor. An agglutination reaction (showing clumping) indicates the presence of the agglutinogen. PAGE 5 OF 8 PROCEDURE In this experiment, we will conduct blood typing tests on six blood samples. From the Experiment menu, select Blood Typing. You will see the opening screen for the Blood Typing lab (Figure 11.4a). Use the Balloons On/Off feature from the Help menu to familiarize yourself with the equipment on the screen. In the upper right portion of the screen is a shelf with six samples of blood. In the upper left portion of the screen is a shelf containing bottles of anti-A serum (blue color), anti-B serum (yellow color), and anti-Rh serum (white color). These bottles contain antibodies to the A antigen, B antigen, and Rh antigen, respectively. In the center of the screen is a lab table for performing the blood typing. To the left of the lab table is a blood typing slide dispenser. Above the blood typing slide dispenser is a container of stirring sticks. These sticks are color coded: the blue stick is to be used with the anti-A serum, the yellow stick is to be used with the anti-B serum, and the white stick is to be used with the anti-Rh serum. To the right of the lab table is a light box for viewing the blood type samples. When you click on the Light button, the screen above unrolls to display the blood types. To the left of the light box is a data table to record your results. In the bottom right portion of the screen is a contaminated disposal container. All glassware and sticks that have come in contact with blood must be placed in this container for proper disposal. PAGE 6 OF 8 Blood Typing Simulation Six individuals with different blood types have donated their blood for this exercise. 1) Click and drag a blood typing slide from the blood typing slide dispenser to the lab table. Note that the three wells on the slide are labeled “A,” “B,” and “Rh.” 2) Click on the dropper for blood sample 1, and drag it over the well labeled A on the blood typing slide. A drop of blood will be dispensed into the well. 3) The dropper will automatically slide over to each of the remaining wells. 4) Click on the dropper for anti-A serum, and drag it over the well labeled A on the blood typing slide. A drop of anti-A serum will be dispensed into the well. 5) Repeat step 4 with the anti-B serum. Be sure to dispense it into the well labeled B. 6) Repeat step 4 with the anti-Rh serum. Be sure to dispense it into the well labeled Rh. 7) Obtain a blue-tipped stirring stick, and drag it to well A. It will mix the blood and anti-A serum. 8) Dispose of the stirring stick in the contaminated disposal container. 9) Select a yellow-tipped stirring stick, and drag it to well B. 10) Dispose of the stirring stick in the contaminated disposal container. 11) Select a white-tipped stirring stick, and drag it to well Rh. 12) Dispose of the stirring stick in the contaminated disposal container. 13) Drag the blood typing slide to the light box, and click the Light button. The screen will unroll, displaying the results of the blood typing. 14) Examine the results labeled A on the screen. If coagulation (agglutination, or “clumpiness”) is present, click on Positive. If no coagulation is present (the sample will look smooth), click on Negative. 15) Repeat step 14 for the results labeled B and Rh. In each case, choose Positive if the sample is coagulated and Negative if the sample is not coagulated. 16) Click the Record Data button on the data table to record the results of blood sample 1. 17) Click and drag the blood typing slide to the contaminated disposal container. 18) Click the X at the top right of the scroll to close the scroll. 19) Repeat steps 1–18 for the remaining samples of blood. 20) Using the data you have collected in this activity, fill in Chart 5. (Indicate coagulation as either “positive” or “negative.”) Determine the blood type of each sample and fill in the last column. For Rh positive or negative, add + or - to the blood type; for example, AB -. PAGE 7 OF 8 . BLOOD TYPING POST LAB QUESTIONS 1. If the anti-A antibody causes the blood to coagulate, which antigen would be present on the blood cells? 2. If a person has type AB blood, which antigens are present on the red blood cells? 3. Which antibodies are present in the plasma of a person with type AB blood? 4. Does a person with type O blood have A or B antigens on the red blood cells? PAGE 8 OF 8