Heart-Rate Response of Elderly Women to Nonweight
advertisement

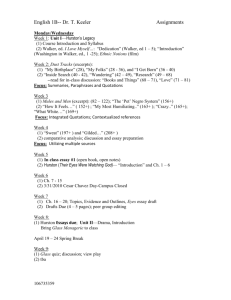
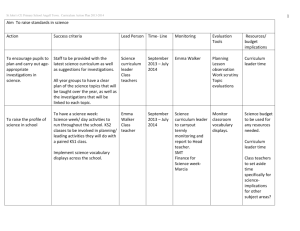
Heart-Rate Response of Elderly Women to Nonweightbearing Ambulation with a Walker INGRID M. BARUCH and KURT A. MOSSBERG The purpose of this study was to determine the heart-rate reponse to nonweightbearing ambulation with a walker in a group of active, healthy 60- to 80-year-old women. The subjects walked for three minutes over a smooth-surfaced tile track using a three-point nonweight-bearing gait at a self-paced rate. Heart rate was monitored by biotelemetry at rest, during the last minute of exercise, and for the first five minutes of recovery. The mean velocity of ambulation with a walker selected by this group was 12 ± 5 m/min. Mean heart rate increased 49 ± 14 bpm during the third minute of activity over the mean resting rate of 77 ± 8 bpm. Group heart rates rose to an average of 83 percent of their age-predicted maximum heart rate. All subjects achieved steady-state heart rate during the third minute of walking. This study suggests that an excessive amount of cardiac work may be demanded of the elderly individual during walker use. This stress on the heart is a major source of concern to the physical therapist whose goal is to provide a safe and effective therapeutic program for the geriatric patient. Key Words: Gait, Geriatrics, Heart rate, Physical therapy. Gait training with various assistive devices has been described as vigorous and brief, intense exercise1 and has long been studied in terms of its stress on the heart of an individual performing such a task. 2 ' 3 However, investigation of the stress of walker use is a topic that has received little attention in the literature. Many physical therapists may not be aware of just how much is demanded of the cardiovascular system when an elderly patient receives gait training with a walker. A variety of physiological and pathological changes associated with aging create a general condition of instability and weakness that warrants the use of an assistive device to aid in performing functional walking. Although the walker is the gait aid most frequently used for the unstable elderly patient who needs extra support and security during walking,4 only one published report has been found that studied the stress of using a walker on an elderly population. 2 Cordrey and colleagues in 1958 compared energy expenditure of 20 patients, 50 to 87 years of age, who were asked to walk with axillary crutches, in parallel Ms. Baruch was a student in the master's degree program in physical therapy, Texas Woman's University, Houston, TX, when this study was conducted. She is now a physical therapist in the state of New York and resides at 50-45 184 St, Fresh Meadows, NY 11365 (USA). Mr. Mossberg is an instructor at Texas Woman's University, School of Physical Therapy, Houston, TX 77030. This paper was submitted February 7, 1983; was with the authors for revision six weeks; and was accepted June 28,1983. 1782 bars, or with a walker using either a nonweightbearing (NWB) or partial weightbearing (PWB) gait. No significant differences between the oxygen consumption of the various modes of ambulation were found, although use of the walker in a NWB gait resulted in the greatest increases in heart rate. In the only other study found of walker use, Harsh in 1982 studied oxygen consumption in a group of 25 young females, 19 to 30 years of age, using a NWB gait with axillary crutches and with a walker (unpublished data, FL Harsh, 1982). When Harsh considered velocity of ambulation, she found that use of the walker required a significantly higher level of oxygen consumption than use of the crutches. This study demonstrated that at the same rate of energy expenditure, crutch users could ambulate a greater distance than the walker users. Most of the studies of energy expenditure during specific tasks have been carried out by measuring oxygen consumption. This technique requires the collection of expired air with the Douglas bag apparatus. Its use is impractical, however, in a clinical setting, especially with the aged, handicapped children, or anyone who might become anxious while using such a cumbersome contraption. 5 In an elderly group tested with the face mask and Douglas bag system, many were unable to tolerate the mouthpiece, and some panicked because of a feeling of lack of air.6 Because heart rate has been shown to be linearly related to oxygen uptake and energy cost at submaxPHYSICAL THERAPY RESEARCH imal work loads, researchers have proposed heart rate as a valid and reliable index of exercise intensity under controlled conditions.7 (pp344-355),8 In addition, heart rate is considered to be a valid indicator of the work performed by the heart in response to exercise.9(p51) Many researchers have adopted guidelines for the use of heart-rate responses as indicators of levels of safe and tolerable exercise intensities in relation to age and physical condition. Some guidelines call for monitoring actual heart rate attained during the exercise,10 and then reporting the percent of the age-predicted maximum heart rate attained. 9(pp2-4),11,12 (pp22-24) Other methods including using predetermined standard heart-rate values at which activity is considered too strenuous2,13,14 and tables listing functional work-load intensity by heartrate response.10,15,16 Determining the cardiovascular stress of walker use is needed to provide safe and effective gait training to elderly patients. The purpose of this study was to determine the heart-rate response to NWB ambulation with a walker in a group of active, apparently healthy, 60- to 80-year-old women. METHOD Subjects Twenty-five women between 60 and 80 years of age with no history of cardiovascular, respiratory, or major musculoskeletal abnormalities consented to be studied. No subject was under a physician's care or taking prescribed medication for any of the abovementioned conditions. The subjects solicited were from various hospital volunteer organizations in the Texas Medical Center and other community volunteer organizations from the surrounding area. Participants were asked not to consume food and beverages other than water for at least two hours before testing. Smoking was prohibited at least 30 minutes before the exercise. Equipment Heart rate was monitored using a Narco Biotelemetry unit* and recorded by a desk model Physiograph®.† Electrode sites were cleansed with alcoholsoaked gauze pads. Conductive gel and tape were used to ensure good contact between the monitoring electrodes and the subject's skin. An adjustable adult aluminum four-point walker was the ambulatory assistive device. As each subject walked at a self-selected comfortable pace for the three-minute exercise, we * Model FM-1100-E2 and FM-1100-6, Narco Bio-Systems, Inc, Houston, TX, 77061. † Model DMP-4B, Narco Bio-Systems, Inc, Houston, TX, 77061. Volume 63 / Number 11, November 1983 measured velocity with a stopwatch and a tape measure. Procedure The protocol for this research had been approved by a Human Subjects Review Committee and by a separate committee composed of faculty members from the Department of Physical Therapy of Texas Woman's University. After the subject had arrived at the testing area, we explained the procedure and the subject signed a consent form. Subjects were reminded before the experiment that if at any time during the walk, they felt short of breath, excessive fatigue, or too much discomfort, the experiment would be stopped immediately and the subject would be under no obligation to complete the task. The walker was fitted to the subject in the standing position. With the walker approximately 30 cm (1 ft) in front of the subject, the height was adjusted so that there was an approximate angle of 30 degrees of elbow flexion when the hands were placed on the walker and the shoulders were relaxed. Instructions and demonstration of the three-point NWB gait were given, but subjects did not receive training sessions before the experiment. The women were allowed to select whichever leg was most comfortable for weight bearing, but they could not switch legs at any time during the exercise. The subject was then prepared for electrode placement. We cleansed the areas over the manubrium and the fifth intercostal space with alcohol and gauze until slight erythema occurred. The silver disk electrodes, filled with electrode gel, and the telemetry transmitter were placed and secured by tape. After the subject rested for five minutes in a sitting position, we obtained resting heart-rate values. Following the rest, the subjects ambulated with the walker at a comfortable but steady pace using the NWB gait for three minutes over a smooth-surfaced tile track. Heart rate response during the last minute of exercise (actual number of ECG cycles during 60 seconds) and during each of the first five minutes of the recovery phase were recorded by the physiograph. Measurement of the velocity of the walk was determined as distance covered over the three-minute period in meters per minute. Analysis We used a descriptive design to gather data. Means of group age, resting heart rate, exercise heart rate during the third minute of ambulation, and velocity in meters per minute were calculated. We reported heart-rate response during the third minute of ambulation in several ways. First, we determined mean increases in the heart rate reported in beats per minute 1783 HR ex Subject Age (yr) HR rest (bpm) HRex (bpm) HR max minus (220-age) HR rest (bpm) Percent Increase Of HRex over HR rest Walker Ambulation for Three Minutes Percent of HR max Reached 1 60 80 110 160 30 38 69 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 64 80 72 72 70 73 63 60 64 70 75 69 73 62 73 66 72 71 65 61 61 70 65 68 80 69 76 68 65 74 76 92 89 84 67 62 70 84 70 81 90 82 82 88 78 70 78 78 132 150 108 135 111 129 118 128 128 124 136 96 107 148 124 135 151 124 129 116 137 114 112 144 156 140 148 148 150 147 157 160 156 150 145 151 147 158 147 154 148 149 155 159 159 150 155 152 52 81 32 67 46 55 42 36 39 40 69 34 37 64 54 54 61 42 47 28 59 44 34 66 65 117 42 99 71 74 55 39 44 48 103 55 53 76 77 67 68 51 57 32 76 63 44 85 85 107 73 91 74 88 75 80 82 83 94 64 73 94 84 88 102 83 83 73 86 76 72 95 HRrecov after 5 min (bpm) TABLE 1 Data for Twenty-Five Women (Ages, 60 to 80) Performing Nonweight-bearing not measured 92 82 81 80 66 91 77 85 91 85 79 69 73 86 86 95 91 87 92 96 90 75 79 85 Distance Traveled (m) Velocity (m/min) 39.0 13.0 30.5 24.1 14.3 57.6 33.8 28.4 24.1 31.4 20.1 32.3 30.8 24.7 30.8 63.7 41.2 32.9 44.2 36.6 36.6 27.1 94.5 28.1 30.5 48.8 10.2 8.0 4.8 19.2 11.3 9.5 8.0 10.5 6.7 10.8 10.3 8.2 10.3 21.2 13.7 10.9 14.7 12.2 12.2 9.0 31.5 9.4 10.2 16.3 above the resting level. Second, we calculated mean percent increases over resting values, and third, we derived percentage of the age-predicted maximum heart rate (220 minus the age in years).7 (pp189-191), 9 (pp2-4) Variability within the group was described for the above characteristics by calculating standard deviations and reporting the ranges. returned to within 5 bpm of their resting heart rates during the first five minutes of the recovery period. On the average, the group traveled 36 m (117 ft) during the three-minute walk resulting in a self-selected mean speed of 12 ± 5 m/min. RESULTS Nonweight-bearing use of a walker elicited heartrate responses that were considered excessively high in most of the elderly women studied. In studies that have investigated activities similar to NWB use of a walker, reports of excessive stress on the cardiovascular system have been emphasized. In Cordrey's study of 20 elderly patients with femoral fractures who ambulated with a walker, with axillary crutches, or in parallel bars, use of a walker with a NWB gait elicited pulse rates that were almost twice that observed in patients using the other assistive devices.2 In two separate studies of unilateral amputees using either their prostheses or axillary crutches, Erdman and colleagues17 and Ganguli and Datta5 found that the static component of weight support by the upper extremities involved in walking with crutches, especially with a NWB gait, resulted in a heavy load placed on the heart. Even in groups of healthy young Raw scores for each individual are listed in Table 1. The descriptive results of this study are summarized in Table 2. The mean age for the group was 68 ± 5 years (range, 60 to 80 years). Mean resting heart rate was 77 ± 8 bpm. Group mean for heart rate reached during the third minute of exercise was 125 ± 15 bpm. By comparing the number of heart beats during the second half of the third minute with the number of heart beats during the first 30 seconds of that minute, we determined that every subject had reached steady state by the end of the three-minute task. The work performed resulted in a mean increase of 64 ± 21 percent (49 ± 14 bpm) over the resting heart rate. This walking task elicited a heart-rate increase equal to 83 ± 11 percent of the age-predicted maximum heart rate. The heart rates of 12 of the 25 subjects 1784 DISCUSSION PHYSICAL THERAPY RESEARCH TABLE 2 Summary of Descriptive Data Related to Nonweight-bearing Use of a Walker in Twenty-five Elderly Women Age (yr) HR ex a (bpm) HRrest (bpm) HRex minus Percent InHRrest (bpm) crease of HRex over Percent of HRmaxb Velocity (m/min) Reached HRrest Mean Standard deviation Range a b 67.9 5.3 77.3 8.2 125.8 14.5 48.5 14.1 63.9 21.4 82.9 10.5 60-80 62-92 96-151 28-81 32-117 64-107 11.9 5.4 4.8-31.5 HRex = heart rate response during the third minute of exercise. HRmax = 220 minus the age in years. adults, use of the swing-through and NWB gait patterns with axillary crutches at various speeds resulted in excessively high heart rates.18,19 Unfortunately, we cannot compare our work with others' because relatively few studies of the elderly performing gait activities have been conducted. Acquiring a sufficiently large control group from the elderly population is difficult because in addition to their intolerance to many of the common testing procedures described earlier, many elderly people cannot be selected as subjects because they take medications or have varying degrees of physical and mental disabilities. Yet, study of older individuals is of vital importance because with advancing age, cardiopulmonary function declines and physical strength and the ability to sustain strenuous exercise are gradually reduced.20 The older person, when asked to perform rehabilitative exercise, is carrying much more of a burden than the young, healthy, physically active individual asked to perform the same task. The present study was designed, therefore, to investigate the heart-rate response to NWB ambulation with a walker in a group of normal, apparently healthy, elderly individuals. Four major factors (systolic arterial pressure, left ventricular size, heart rate, and contractility) determine myocardial oxygen demand and the work performed by the heart. Of these factors, heart rate is most easily monitored. With the use of radiotelemetry, which is easily attached to the patient and allows freedom of movement throughout the activity,21 heart rate is now considered to be a direct, simple, accurate, and highly reliable means of assessing the intensity of an exercise protocol in a clinical setting.5,22 Because many researchers have defined various ways of assessing exercise stress according to heartrate response, a comparison of the results of the present study with the results of others is of interest. Several authors have stated that when heart rate has exceeded 120 bpm in response to exercise, the activity should be stopped.2,14 The mean heart-rate response to the NWB walker exercise was 126 bpm; 16 out of the 25 subjects exceeded a heart rate of 120 bpm. The World Health Organization has recommended that in Volume 63 / Number 11, November 1983 persons over 60 years of age, cessation of exercise should occur when heart rate has reached 130 bpm.13 Of the 25 women studied, 9 exceeded these limits. According to Grandjean, most investigators in the field of exercise physiology agree that the optimum limit of work performance is reached when the average pulse rate during work is approximately 30 bpm over the resting level.10 Twenty-three of the 25 subjects produced heart rates that exceeded this limit in response to three minutes of work with the mean increase over the resting level at 49 bpm. Determining a target heart rate during graded work based on age-predicted maximum heart-rate values has been widely used in many exercise rehabilitation programs.11,12 (pp22-24) These training heart-rate ranges represent an estimate of the safest effective training intensity. Amundsen has stated that at intensities of exercise that increase heart rate to a maximum of 60 to 75 percent of the age-predicted maximum heart rate, the patient should be able to reach and maintain steady-state conditions for 20 minutes or more.9 (pp2-4) Based on calculations of these levels in the subjects under study, the mean percent of maximum heart rate (HRmax) reached during the third minute of exercise was 83 percent. Only two subjects were able to stay below the 70 percent mark during this activity. Most subjects reached between 70 and 95 percent of their HRmax levels. Two subjects even exceeded 100 percent of their age-predicted HRmax levels. These results strongly indicate that NWB walker ambulation is a stressful activity in regard to its work demands on the heart. Still another means of interpreting these results is based on tables of work-load classification according to heart rate. Buskirk has categorized "heavy" work as that which elicits a heart-rate response between 120 and 140 bpm and "very heavy" work as causing responses of 140 to 160 bpm.15 Thus, this task caused 12 subjects to perform heavy work and 4 subjects to perform very heavy work. If one looks at activities categorized as "heavy" work according to heart rate, oxygen consumption, and metabolic equivalent level (METS), the stress that may be placed on the person who must use a walker with a NWB gait pattern is 1785 emphasized. Twelve subjects performed work comparable to heavy shoveling and carrying objects weighing between 60 and 90 lbs.9(p26) The problem encountered with the use of these work-load classification tables is that no listing is made of the duration of exercise related to these heart-rate responses or the age group for which these levels apply. Robinson, however, in a study of healthy older men observed that during an exercise routine that he described as "exhaustive," heart-rate responses ranged from 130 to 150 bpm after three minutes of exercise.16 Thus, by Robinson's standards, nine of the subjects in our study performed exhaustive activity during NWB ambulation with a walker. The heart rates of only 12 out of the 25 subjects returned to within 5 bpm of their resting levels during the first five minutes of the recovery phase. This finding is also indicative of a high level of exercise intensity because the time required for the heart rate to return to normal after exercise depends on the fitness level of the individual and the severity of the work.9(p8) The subjects in this study were all instructed to walk at a comfortable but steady pace for the threeminute task. We chose self-selected velocity because a subject walking at a comfortable or natural speed will adopt a velocity comparable to the one at which minimal energy expenditure occurs.23 The use of a naturally selected speed provides baseline data for comparison of these results with those of physically disabled people who can walk only at self-selected rates. A study by Blessey and colleagues in 1976 determined that 20- to 60-year-old healthy women who performed unrestrained or "free" walking chose 74 m/min as their mean comfortable speed.24 Although the subjects in the present study were older, the intensity of the NWB walker activity may be emphasized by the slowness of the mean velocity of 12 m/min selected by the group; this is considerably slower than normal walking. The task length of three minutes is considered to be a functional duration that would be used by an elderly patient (time needed to walk to the bathroom from their bed or walk outside to a car). The mean distance walked during the three-minute exercise was 36 m (117 ft), which is quite close to the distance commonly attained in physical therapy departments during ambulation training. The task was of short but functional duration, and the women were allowed to move at their own pace. Their slow speed and high heart-rate responses indicate that the activity was a costly one in terms of energy expenditure. 1786 The picture is complicated even further when the whole condition of the patient is taken into consideration. In addition to the normal decline in the efficiency of the cardiovascular system with aging, the hospitalized patient experiences heightened anxiety and cardiac stress because of the unfamiliar surroundings, in addition to the physical and mental discomfort resulting from their disease or injury. Another factor that must be considered when applying these results to a patient population is the potential effect of medication on heart-rate response. Also, the detrimental effects of bedrest alone on the physical condition of an individual have been well documented.22'25 This investigation focused on one group of relatively active and healthy 60- to 80-year-old women. Future studies using a larger group of subjects whose physical condition more closely resembles that of the elderly hospitalized patient would be informative. A measurement of the rate-pressure product (heart rate multiplied by systolic blood pressure) during gait activities such as walker ambulation would be helpful in providing a more accurate picture of the myocardial work demanded during such exercises.12(p9) Another area for research would be a study to determine whether receiving a training program using the upper extremities before ambulation training would affect the subject's heart rate response during gait. Comparison of the energy required of the elderly individual using different ambulation aids (crutches, walker, or wheelchair) is also an area in need of investigation. CONCLUSION Because the subjects involved in this study were healthy women with no history of cardiovascular disease, the results suggest that an elderly patient who may have some degree of cardiac dysfunction is at risk of developing cardiac intolerance during a therapeutic activity such as NWB use of a walker. Physical therapists must be more aware of how stressful certain therapeutic exercises actually may be and how patients can easily be monitored during potentially hazardous rehabilitative activities. Teaching the patient to monitor pulse rate independently with a simple measure before and after exercise may be sufficient.22 Physical therapists have a responsibility to recognize and prevent intolerance to exercise, thereby minimizing the risks of physical exercise and guiding each patient in selecting a safe, yet beneficial, level of activity during treatment. PHYSICAL THERAPY RESEARCH REFERENCES 1. Amundsen LR: Assessing exercise tolerance: A review. Phys Ther 59:534-537, 1979 2. Cordrey LF, Ford AB, Ferrer MT: Energy expenditure in assisted ambulation. Journal of Chronic Diseases 7 : 2 2 8 233, 1958 3. Fisher SV, Gullickson G: Energy cost of ambulation in health and disability: A literature review. Arch Phys Med Rehabil 5 9 : 1 2 4 - 1 3 3 , 1978 4. Steinberg FU: Gait disorders in old age. Geriatrics 2 1 : 1 3 4 143,1966 5. Ganguli S, Datta SR: Prediction of energy cost from peak heart rate in lower extremity amputees. J Med Eng Technol 10:52-55, 1975 6. Kavanagh T, Shephard RJ: The application of exercise testing to the elderly amputee. Can Med Assoc J 108:314-317, 1973 7. Astrand PO, Rodahl K: Textbook of Work Physiology, ed 2. New York, NY, McGraw-Hill Inc. 1977 8. deVries HA: Prescription of exercise for older men from telemetered exercise heart rate data. Geriatrics 2 6 : 1 0 2 111,1971 9. Amundsen LR (ed): Cardiac Rehabilitation. New York, NY, Churchill Livingstone Inc, 1981 10. Grandjean E: Fitting the Task to the Man. London, England, Taylor & Francis Ltd, 1971, pp 5 3 - 5 6 11. American College of Sports Medicine: Guidelines for Graded Exercise Testing and Exercise Prescription, ed 2. Philadelphia, PA, Lea & Febiger, 1980, pp 3 9 - 4 8 12. The Committee on Exercise: Exercise Testing and Training of Apparently Healthy Individuals: A Handbook for Physicians. Dallas, TX, The American Heart Association, 1972, pp 9, 2 2 - 2 4 13. Anderson KB, Shephard RJ, Denolin H, et al: Fundamentals of Exercise Testing. Geneva, Switzerland, World Health Organization, 1971, pp 4 5 - 4 6 Volume 63 / Number 11, November 1983 14. Tobis JS, Zohman LR: A rehabilitation program for patients with recent myocardial infarction. Arch Phys Med Rehabil 49:443-448, 1968 15. Buskirk ER: An introduction to exercise and performance evaluation. JSC Med Assoc 65 (Suppl):4-7, 1969 16. Robinson S: Experimental studies of physical fitness in relation to age. Arbeitsphysiologie 10:251-323, 1938 17. Erdman WJ, Hettinger T, Saez F: Comparative work stress for above-knee amputees using artificial legs or crutches. Am J Phys Med 3 9 : 2 2 5 - 2 3 1 , 1960 18. Sankarankutty M, Stallard J, Rose GK: Relative efficiency of 'swing-thru' gait on axillary, elbow and Canadian crutches compared to normal walking. J Med Eng Technol 1:55-57, 1979 19. Patterson R, Fisher SV: Cardiovascular stress of crutchwalking. Arch Phys Med Rehabil 62:257-260, 1981 20. Harris R, Frankel LF, Harris S: Guide to Fitness after Fifty. New York, NY, Plenum Publishing Corp, 1977, pp 5 - 1 0 2 1 . Clarke CP, Itoh M, Solomon M, et al: Radioelectrocardiogram monitoring during ambulation training of patients with amputations. Phys Ther 51:906-913, 1971 22. Lunsford BR: Clinical indicators of endurance. Phys Ther 58:704-709, 1978 23. Bassey EJ, Fenten PH, MacDonald IC: Self paced walking as a method for exercise testing in elderly and young men. Clinical Science and Molecular Medicine 5 1 : 6 0 9 - 6 1 2 , 1 9 7 6 24. Blessey RL, Hislop HJ, Waters RL, et al: Metabolic energy cost of unrestrained walking. Phys Ther 56:1019-1024, 1976 25. Saltin B, Blomqvist B, Mitchell JH, et al: Response to exercise after bedrest and after training. Circulation 38(Suppl 7 ) : 1 78, 1968 1787