25
Journal of Pediatric Neurology 7 (2009) 25–43
DOI 10.3233/JPN-2009-0272
IOS Press
Review Article
EEG and the newborn
Maria Roberta Cilio∗
Division of Neurology, Bambino Ges ù Children’s Hospital, Rome, Italy
Received 22 December 2008
Accepted 24 December 2008
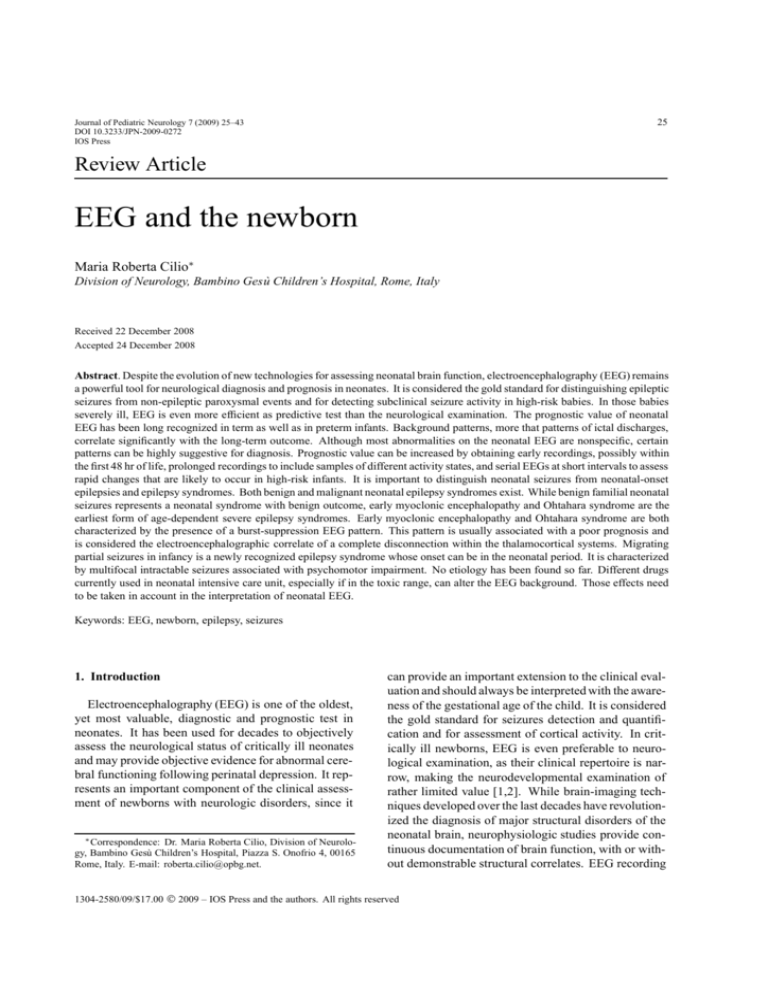
Abstract. Despite the evolution of new technologies for assessing neonatal brain function, electroencephalography (EEG) remains
a powerful tool for neurological diagnosis and prognosis in neonates. It is considered the gold standard for distinguishing epileptic
seizures from non-epileptic paroxysmal events and for detecting subclinical seizure activity in high-risk babies. In those babies
severely ill, EEG is even more efficient as predictive test than the neurological examination. The prognostic value of neonatal
EEG has been long recognized in term as well as in preterm infants. Background patterns, more that patterns of ictal discharges,
correlate significantly with the long-term outcome. Although most abnormalities on the neonatal EEG are nonspecific, certain
patterns can be highly suggestive for diagnosis. Prognostic value can be increased by obtaining early recordings, possibly within
the first 48 hr of life, prolonged recordings to include samples of different activity states, and serial EEGs at short intervals to assess
rapid changes that are likely to occur in high-risk infants. It is important to distinguish neonatal seizures from neonatal-onset
epilepsies and epilepsy syndromes. Both benign and malignant neonatal epilepsy syndromes exist. While benign familial neonatal
seizures represents a neonatal syndrome with benign outcome, early myoclonic encephalopathy and Ohtahara syndrome are the
earliest form of age-dependent severe epilepsy syndromes. Early myoclonic encephalopathy and Ohtahara syndrome are both
characterized by the presence of a burst-suppression EEG pattern. This pattern is usually associated with a poor prognosis and
is considered the electroencephalographic correlate of a complete disconnection within the thalamocortical systems. Migrating
partial seizures in infancy is a newly recognized epilepsy syndrome whose onset can be in the neonatal period. It is characterized
by multifocal intractable seizures associated with psychomotor impairment. No etiology has been found so far. Different drugs
currently used in neonatal intensive care unit, especially if in the toxic range, can alter the EEG background. Those effects need
to be taken in account in the interpretation of neonatal EEG.
Keywords: EEG, newborn, epilepsy, seizures
1. Introduction
Electroencephalography (EEG) is one of the oldest,
yet most valuable, diagnostic and prognostic test in
neonates. It has been used for decades to objectively
assess the neurological status of critically ill neonates
and may provide objective evidence for abnormal cerebral functioning following perinatal depression. It represents an important component of the clinical assessment of newborns with neurologic disorders, since it
∗ Correspondence: Dr. Maria Roberta Cilio, Division of Neurology, Bambino Gesù Children’s Hospital, Piazza S. Onofrio 4, 00165
Rome, Italy. E-mail: roberta.cilio@opbg.net.
can provide an important extension to the clinical evaluation and should always be interpreted with the awareness of the gestational age of the child. It is considered
the gold standard for seizures detection and quantification and for assessment of cortical activity. In critically ill newborns, EEG is even preferable to neurological examination, as their clinical repertoire is narrow, making the neurodevelopmental examination of
rather limited value [1,2]. While brain-imaging techniques developed over the last decades have revolutionized the diagnosis of major structural disorders of the
neonatal brain, neurophysiologic studies provide continuous documentation of brain function, with or without demonstrable structural correlates. EEG recording
1304-2580/09/$17.00 2009 – IOS Press and the authors. All rights reserved
26
M.R. Cilio / Neonatal electroencephalography
can detect seizures, with or without clinical manifestations, and especially if combined with video monitoring, it can differentiate them from paroxysmal nonepileptic events in order to avoid unnecessary treatment
and to institute the correct treatment when required [3,
4]. However, in the pediatric setting, this tool is not
always available, as it requires interpretation by a neurologist with expertise in neonatal EEG. These reasons
have led to the development of complementary types
of cerebral function monitoring, such as amplitudeintegrated EEG, which is intended to be applied and
interpreted independently by neonatologists in order to
allow a real-time interpretation of results. Nevertheless, EEG is necessary if precise classification into normal or mildly, moderately, or markedly abnormal backgrounds is desired, and it can be particularly helpful in
the newborn intensive care unite in identifying infants
suitable for neuroprotective strategies and allowing accurate diagnosis and stratification of encephalopathy, a
prerequisite for the evaluation of results of neuroprotective strategies [5,6].
2. Technique
For the proper assessment of neonatal EEGs, it is
mandatory to record at least a phase of active sleep and
quiet sleep. In infants less than 30 weeks of conceptional age who spend most of their time in indeterminate sleep, a record of approximately 40 min duration
comprising the most continuous and the most discontinuous pattern may be practically sufficient [7]. The
EEG in the neonatal period should be performed allowing some stimulations and in an environment as quiet
as possible.
There are several technical considerations when
recording from a neonatal scalp. High skin resistance
impedes low-resistance scalp-to-electrode contact. The
minimum standard required includes at least ten scalp
electrodes placed following the 10–20 International
System of Electrode Placement, modified for neonates
(Fig. 1) as well as non-cerebral channels. Whereas
the classification of sleep states was developed mainly
on the EEG patterns in adults, poligraphic recording
became the gold standard for state classification and
developmental physiology in the newborn. Therefore,
the EEG recording in the newborn should always be
a poligraphy that means a continuous and simultaneous recording of cerebral electrical activity, eye movements’ electrooculogram, muscle activity [electromyography (EMG)], heart activity (electrocardiogram) and
Fig. 1. Electrodes placement according to the 10-20 International
System modified for neonates.
respiratory activity. Respiratory monitoring should include two respiratory monitors: a thoracic strain gauge
or motion transducer to detect chest wall movements
in one channel, and a thermistor to detect airflow in
the other channel. EMG should include a submental EMG activity monitor. Such monitoring assists
in the identification of specific segments of the EEG
sleep cycle and, especially if used together with highsynchronized video, facilitates the characterization of
seizures by correlating the clinical manifestations with
the ictal electrical discharge. Concordance between
electrographic and polygraphic signals marks the maturation of the central nervous system (CNS), as reflected
in EEG sleep development. Non-cerebral physiologic
parameters may also be relevant to the clinical problem
that prompted the request for the EEG study, such as
apnea. Important sources of artifact can be identified
more readily or eliminated by using non-cerebral monitors. As with adults, physiologic and non-physiologic
artifacts must be properly identified in neonatal recordings because the may interfere with the interpretation of
cerebral activity. The technologist should not only try
to identify the source of the artifact but eliminate such
artifacts during the recording. Accurate description by
the technologist may help the neurologist in the diagnosis of a neurologic disorder in the neonate. It is important to annotate the tracing with particular attention
to the state of activity (awake or asleep), to the presence and type of eye movements, facial movements,
sucking, crying, and any other events [7].
M.R. Cilio / Neonatal electroencephalography
3. Indications
There are no indications for systematical recording
of every newborn in the intensive care unit. However,
an EEG should be considered when questions arise regarding the baby’s abnormal neurological status or the
possibility of seizures. For instance, EEG will be required for diagnosis of abnormal movements, autonomic signs (i.e. unexplained apnea, flushing of the face),
abnormal neurological status (i.e. lethargy or hyperactivity), or reported fetal distress. In those cases, EEG
may allow recognition of patterns suggestive of specific conditions such as inherited errors of metabolism
or herpetic encephalitis, to detect focal abnormalities
like in hemorrhagic or ischemic stroke or abscess, or
to identify ictal discharges [8]. Serial studies more accurately document normal ontogeny or the evolution
of encephalopathic changes than do single recordings.
The continuous changes that occur during early brain
development are often associated with striking changes
in EEG pattern over short periods. Indeed, EEG patterns are expected to change according to the gestational age. A trained interpreter of neonatal EEG can
estimate the electrical maturity of the neonatal brain
with an accuracy of 2 weeks of the gestational age for
preterm infants and 1 week for full term infant [8,9]. In
fact, CNS development of the immature brain in postnatal environment proceeds at about the same rate as
during fetal development and evolving electrical patterns reflect the conceptional age of the infant independently of his birth weight. Concordance between electrographic and polygraphic components of EEG sleep
begins as early as 30 weeks of estimated gestational
age and is complete after 36 weeks of estimated gestational age. The EEG also changes with behavioral
state cycles that show an increasing organization with
advancing conceptional age [10].
4. Prognostic value
It is generally accepted that the background EEG is
a good prognostic tool in preterm infants as well as
term infants [11–16]. The EEG features used for prognostic purposes differ among authors. For prognostic
purposes, serial EEG recordings are more useful than
a single recording [17]. Usually, various features are
grouped into different severity grades and correlated
with outcome [13]. Some authors use some selected
features such as discontinuity measures [18,19], maturational features [20,21], or sharp waves transient [22].
27
In the newborn with an acute hypoxic insult, the prognostic value of the EEG strongly depends on the day
of recording [17]. The longer the time between the
hypoxic event and the pathologic tracing, the worst the
prognosis. Conversely, EEGs obtained shortly after the
insult must be viewed with caution and a follow-up
study is highly recommended.
The relationship between neonatal EEG findings and
neurological outcome has been investigated in preterm
infants younger than 33 weeks of gestation by Watanabe et al. [15]. These authors defined changes in continuity, frequency, and amplitude as acute stage abnormalities, and changes in maturity and waves forms as
chronic stage abnormalities. They also used the EEG
to assess the timing of brain insult suggesting that acute
stage abnormalities in EEG immediately after birth may
have originated from insults occurring just before birth.
In their study, the absence of chronic stages abnormalities was associated with a favorable outcome in 88%,
while dysmature pattern was associated with mental
retardation or borderline outcome in 68%. Whereas
mildly disorganized patterns were associate with normal outcome in 52%, severely disorganized patterns
were associated with moderate or severe CP in 79%
of cases [15]. Also, serial EEG recordings beginning
immediately after birth demonstrated to be particularly useful to assess the timing and the degree of brain
injuries and to elucidate their pathogenesis in young
preterm infants [15].
The potential of neuroprotective therapies, such as
hypothermia, has raised the importance of accurate prediction of outcome in the first 6 hr of life [6,23,24].
EEG remains our best method of predicting neurologic
outcome in hypoxic ischemic encephalopathy [11,12,
14]. A normal or mildly abnormal EEG in the first 24 hr
of life has a positive predictive value of 94% in predicting a normal neurologic outcome. In contrast, a severely abnormal or inactive EEG predicts death or severe
disability in the great majority of cases. Moderate abnormalities will be associated with neurologic disability in 60% of cases. Sarnat scoring has a good predictive
value, but cannot be assessed until 24 hr of age, too late
for benefiting from currently available neuroprotective
therapies. In contrast, EEG grading can be assigned
soon after delivery and offers more reliable prognosis
than the Sarnat score alone [12,25] Early amplitudeintegrated EEG has been shown to accurately predict
the severity of encephalopathy and long-term neurologic outcome [26]. For this reason, this tool has been
used in the recruitment of infants with moderate and
severe encephalopathy to clinical trials of neuroprotec-
28
M.R. Cilio / Neonatal electroencephalography
tive hypothermia, giving promising results [23]. However, amplitude integrated EEG shows poor reliability
compared with continuous EEG when reported by inexperienced personnel, and does not allow localization
of pathology or seizure activity [27].
While most neonatal EEG patterns are nonspecific,
the EEG may be the first test to guide the clinician in
reaching an unsuspected diagnosis. For example, an
interhemispheric or regional asymmetry of background
pattern is often the first clue for underlying lesion, such
as a prenatal ischemic event, unsuspected by history or
examination. Several EEG features may suggest dysgenetic brain anomalies, inborn errors of metabolism,
such as non-ketotic hyperglycinemia and pyridoxine
dependency, CNS infections like herpes simplex virus
encephalitis. In the context of ictal disorders, the EEG
has been shown to be an excellent predictor of outcome
by the vast majority of prospective or retrospective investigations performed during three decades. Many
authors reached the conclusion that, for prognostic purposes, the background EEG patterns are more significant that the patterns of EEG discharge. In a study
of 137 full-term infants with neonatal seizures, Rose
and Lombroso [28] found that neonates with seizures
who had a normal EEG had an 86% chance of normal development at age 4 yr. Conversely, in neonates
with low amplitude, periodic or multifocal spikes in the
interictal EEG background had only a 7% chance for
normal development. Monod et al. [29] found similar correlations. for neonates presenting with seizures.
In a review of 691 EEGs performed in 270 mostly
term-born neonates recorded in the first month of age,
they showed that normal EEGs were highly correlated
with favorable outcome, while low-voltage, inactive,
or burst-suppression EEGs were highly prognostic of
poor outcome both in preterm and full-term infants. In
another study, Rowe et al. [30] supported these findings
in 74 full-term and preterm neonates with seizures, emphasizing that EEG background was more predictive of
outcome than interictal sharp waves.
Normalization of a previously abnormal pattern may
indicate a minimal impact of a brain insult on maturation. Conversely, progressive deterioration of previously normal or moderately abnormal patterns favors the possibility of long-term neurological sequelae.
Repeated recordings provide the clinician with greater
predictive information than those derived from a single
EEG [31]. However, some EEG patterns are so severely abnormal that they are considered sufficient for the
formulation of the prognosis, without the need for serial tests. Some authors feel that predictions can be accu-
rately be advanced when the initial EEG shows an inactive or isoelectric pattern or a burst-suppression pattern,
even if the test is obtained shortly after birth [11,28,29].
In order to diagnose an isoelectric pattern, most authors
require the absence of all discernible cerebral electrical
activity recording at a sensitivity of 2 µV/mm [32]. The
technical requirements for the diagnosis of isoelectric
recordings in neonates are the same as in adults, namely, using the highest gains, long time constants, and
long interelectrodes distances, and meticulous attention
to artifacts. An isoelectric pattern is most commonly
seen following severe asphyxia, circulatory collapse,
and massive intracerebral hemorrhages. It can also
been seen in severe malformation of the brain, such as
hydranencephaly or massive hydrocephalus. In the absence of drug intoxication, acute hypoxemia, hypothermia, and postictal state, this EEG pattern carries a poor
prognosis: most neonates with isoelectric EEG either
die in the neonatal period or suffer severe neurologic
deficits [11]. Very rarely in the newborn, EEG activity
may return normal after an isoelectric EEG recorded
in the first 24 hr following an acute hypoxic-ischemic
event. Usually, in the survivors, the isoelectric EEG is
followed by other abnormal patterns, particularly lowamplitude or burst-suppression backgrounds [33].
Burst suppression pattern on the neonatal EEG is
usually associated with a poor outcome. This pattern
is characterized by burst of high voltage activity (75–
200 µV) lasting 1 to 10 sec with mixed features (spikes,
sharp waves, theta, delta) but no age-appropriate activity, alternating with periods of marked background
attenuation (voltage < 10 µV) lasting 2 to 45 sec. This
periodic pattern is persistent throughout awake and
asleep states, unreactive and unaltered by exogenous
stimuli (Fig. 2).
Steriade et al. [34] have investigated the cellular
correlates of EEG burst-suppression patterns in animals. In this study, burst-suppression was elicited
by the administration of an anesthetic agent. About
95% of cortical cells entered burst-suppression, in close
time-relation with EEG activity, displaying sequences
of phasic depolarizing events associated with bursts
of EEG waves and an electrical silence of the neuronal membrane during flat EEG periods. In contrast
with cortical neurons, only 60–70% of thalamic cells
ceased firing before overt EEG burst-suppression and
was completely silent during flat periods of EEG activity, while the remaining 30–40% showed intrinsic
pacemaking properties discharging rhythmic (1–4 Hz)
spike bursts during periods of EEG silence. However,
with the deepening of burst-suppression, when silent
M.R. Cilio / Neonatal electroencephalography
29
Fig. 2. Burst-suppression pattern in a 3-day-old full-term newborn. An alternating pattern of high-voltage mixed frequency activity and voltage
attenuation indicates severe diffuse cerebral dysfunction. The bursts contain no age-appropriate activity. The muscle activity over the deltoids
and the irregular respiratory pattern differentiate the awake (A) from the sleep (B) state, while the cortical activity with the burst-suppression
pattern is invariant.
30
M.R. Cilio / Neonatal electroencephalography
Fig. 3. Tracé alternant during quiet sleep in a 10 days old full-term infant. This pattern is reactive to stimuli, and alternate with the continuous
pattern of the active sleep. It can be distinguished from the burst-suppression by the presence of high-voltage slow wave activity that alternate
with period of low voltage activity. The low voltage activity of the trace alternant is higher compared with the interburst activity of the
burst-suppression pattern.
EEG periods became longer than 30 sec, thalamic cells
also ceased firing. The assumption that full-blown
burst-suppression is achieved through virtually complete disconnection in brain circuits implicated in the
genesis of the EEG is corroborated by the revival of
normal cellular and EEG activities after volleys setting
into action thalamic and cortical networks. A recent
study demonstrated that a predominant interburst interval duration of more than 30 sec correlated with the occurrence of both unfavorable neurologic outcome and
subsequent epilepsy, suggesting that the interburst duration, an easily quantitated EEG parameter, could be
valuable for the early estimation of neurologic prognosis in those patients [35]. According to this study, an
infant whose EEG contains a predominant interburst
interval duration of more than 30 sec has a 100% probability of experiencing severe neurologic disabilities or
death and an 86% chance of developing subsequent
epilepsy. Burst-suppression pattern has been observed
in individuals with cerebral conditions disconnecting
the cortex from deep structures. Highly discontinuous pattern as seen in burst-suppression can result from
brain immaturity, extensive brain damage or dysfunction. Such dysfunction may be only temporary or be
long lasting when structural lesions or diffuse changes
of metabolic origin have taken place. Transient EEG
burst-suppression is seen in barbiturate anesthesia and
hypoxic-ischemic encephalopathy, while a persistent
burst-suppression is observed in deep brain tumors, severe congenital metabolic disorders such as non-ketotic
hyperglycinemia, or extensive brain malformation such
as hemimegalencephaly [36].
The burst-suppression pattern is easy to differentiate
from the discontinuous features normally seen during
non-rapidly eye moved or quite sleep in infants above
34–36 weeks corrected age, when trace alternant begins to emerge clearly. The discontinuous pattern of
trace alternant is distinguished from burst-suppression
by the presence of its interburst activity, by being reactive to stimulations, and by the presence of normal EEG
features for corrected ages (i.e., delta brushes, temporal theta, or frontal sharp transient), whereas there is
also cycling of the discontinuous pattern with the continuous one of the rapid eye movement sleep (Fig. 3).
Problems may arise in diagnosing burst-suppression in
preterm infants less than 33–32 weeks, because of the
trace discontinue that normally occurs at ages that are
more immature. The most reliable clue to distinguish
the pathological pattern of burst-suppression from the
normal pattern of trace discontinue is the clear knowledge of the infant’s conceptional age. Therefore, trace
alternant and trace discontinue are two patterns of dis-
M.R. Cilio / Neonatal electroencephalography
31
Fig. 4. Status epilepticus in a 2 days old full term infant with hypoxic ischemic encephalopathy. The background activity is low voltage.
Electrographic continuous seizures shift from an area to another, with one seizure starting from the fronto-central region of the left hemisphere
(A) and spreading in the occipital region of the same hemisphere (B), then affecting the frontal region of the contralateral hemisphere (C), and
spreading to the occipital region of the right hemisphere (D).
continuity that are normal for some conceptional ages
but may be abnormal for others, while burst- suppression is usually invariant and lack other features characteristic for the EEGs of neonates of various conceptional ages. Testing for reactivity, usually absent in burstsuppression, is also helpful. Nonetheless, in young
preterm infants, serial recording are advisable before
formulating the poor prognosis associated with burstsuppression. If such activity is persistent through repeated recordings, invariant and unresponsive to stimulation, with prolonged interburst intervals, then such a
pattern may be considered equivalent to the pathologic
burst-suppression seen at term, as suggested by Tharp
et al. [37] in 1981.
5. Seizures
Normal neonates commonly exhibit a variety of
paroxysmal movements including nonconjugate eye
movements, sucking movements without associated
eye abnormalities, and sleep-related myoclonus. These
32
M.R. Cilio / Neonatal electroencephalography
Fig. 4, continued.
normal behaviors as well as pathologic conditions can
be difficult to distinguish from epileptic seizures, which
can also have somewhat subtle manifestations. EEG is
a necessary tool in distinguishing among these entities.
In a study of EEG diagnosis of seizures in neonates,
90% of abnormal movements suspicious for seizures
were found to be nonepileptic on EEG recording [1].
The EEG should therefore be recorded at the beginning of the first symptoms, and, if possible, before any
seizure treatment. Epileptic seizures are most frequent
in the neonatal period than in any other time of the
life [38,39]. A generally accepted definition of what
constitutes an ictal discharge has not been established,
especially in the newborn. Most authors classify a discharge as ictal if it lasts at least 10 sec. However, documented clinical and electrical seizures have been described in neonates as lasting only a few sec, while with
increasing age seizure activity becomes usually longer
in duration. There are striking differences between
seizures in neonates and those of older patient in ictal
EEG patterns and their correlation with clinical symptoms and pathology [13,40]. Neonates more often have
brief albeit recurrent seizures with a brief interictal interval, as opposed to a single prolonged ictal event as
M.R. Cilio / Neonatal electroencephalography
33
Fig. 5. Focal seizure in a 10 hr old full-term infant with right middle cerebral artery infarct. The focal ictal discharge begins in the right
centro-parietal region and does not have a clinical correlate (uncoupling) (A). Four min after the onset of electroencephalography recording the
infants presents with left arm clonic movements (B) and the ictal discharge remains confined to the same region. Seven min later, the discharge
is still recorded from the same region (C).
observed in older infants. Seizures may have an erratic
evolution, shifting from one area to another even in the
presence of a diffuse pathological process (Fig. 4). Just
as seizures differ between neonates and older populations, so does status epilepticus [41]. Data from Mor-
ton et al. [42] showed that, while neonates with status
epilepticus presented with brief, partial, serial seizures
with multiple foci, infants older than 2 months of age
were capable of having prolonged seizures with typically one focus and possible secondary generalization.
34
M.R. Cilio / Neonatal electroencephalography
Fig. 5, continued.
In the newborn, seizures are unique because the neonatal brain differs in both structure and physiology from
those of older children and adults. Although the basic
organization of the cortex is in place, dendritic growth,
axonal-dendritic connections, and synaptic stabilization are not complete in the newborn [43,44]. Likewise,
myelination is immature, preventing the rapid wellorganized spread of epileptic discharges [45]. Therefore, newborns may present with focal ictal discharges
in metabolic disorders (i.e. in hypocalcemic or hypoglycemic seizures) as well as structural lesions (i.e. ischemic stroke). However, in localized structural lesions, seizures tend to be more consistently confined
in the affected region even in the case of prolonged or
recurrent event (Fig. 5). From a clinical point of view,
a seizure may be defined as a paroxysmal alteration
in neurological function, i.e. behavioral, motor, and/or
autonomic function, associated temporally with EEG
seizure activity (electro-clinical seizure). In some occasions, this correlation is lacking (clinical seizures without EEG correlate) but it is not clear whether these latter
phenomena are related to an epileptic condition [46–
49]. Mizrahi and Kellaway [48] in 1987 suggested
classifying as epileptic seizures only those paroxysmal
events associated with concurrent electrical seizure activity. However, the inconsistent electrographic capture
on the scalp recordings may depend on seizures arising
from foci deep within the brain, only inconsistently dis-
charging through final anatomic pathway. Conversely,
an electrical seizure without clinical correlate may be
the result of a discharge arising from an area of the
cerebral cortex, which does not express itself overtly
in the newborn, such as a sensory, or language area.
However, these considerations should not detract from
the use of EEG as the standard means for determining
the presence of seizures before consideration of drug
treatment. As it can be difficult to distinguish epileptic
from non-epileptic seizures, EEG may provide a more
accurate endpoint than clinical observation in assessing
treatment efficacy [4].
On the other hand, electrical seizures without clinical correlate are frequently recorded, particularly in
severely ill newborns, with severe brain damage, or in
those who are pharmacologically paralyzed [39]. In
one study, only 21% of neonates had a clinical correlate during electrographic seizures [3]. Another report
found that only 45% of preterm and 53% of full-term
neonates demonstrated clinical signs coincident with
their electrographic seizures [50]. This electroclinical
dissociation can also be seen after anti-epileptic drugs
(AEDs) treatment, particularly phenobarbital. Recently, Scher et al. [4] performed a prospective study on the
phenomenon of uncoupling in 59 neonates with electrically confirmed seizures. Uncoupling EEG-clinical
seizures was defined as the persistence of electrographic seizures despite the suppression of 50% clinical
M.R. Cilio / Neonatal electroencephalography
seizures after phenobarbital or phenytoin administration. The uncoupling was noted in 58% of the neonatal
cohort. Phenobarbital and phenytoin resulted in equal
rate of uncoupling. Therefore, continuous EEG monitoring during treatment of neonatal seizures is advisable in order to assess the efficacy of the treatment [4].
6. Neonatal epilepsy syndromes
It is important to distinguish neonatal seizures from
neonatal-onset epilepsies and epilepsy syndromes [51].
An epilepsy syndrome is defined by the combination of
age at onset, seizure types, interictal and ictal pattern
and, when known, etiology. This concept, developed
four decades ago by Gastaut [52] and the School of
Marseille, and established by the International League
Against Epilepsy (ILAE), remains the gold standard
for diagnosis in pediatric epileptology [53]. The recognition of epileptic syndromes allows an accurate diagnosis and management of seizure disorders, and it is
useful for research regarding treatments and etiologies,
including the genetic ones. The identification of new
syndromes is based mainly on clinical and EEG criteria, and advances in neuroimaging and genetics have
by no means contradicted this concept [54]. However,
most neonatal seizures are provoked seizures, rather
than a true epilepsy syndrome, and despite the high
prevalence of neonatal seizures, epileptic syndromes
in neonates are rare but often overlooked. Currently, four epilepsy syndromes with onset in the neonatal
period are recognized by the ILAE [55]: benign familial neonatal seizures (BNFS), early myoclonic encephalopathy (EME), Ohtahara syndrome (OS), also
known as early infantile epileptic encephalopathy, and
the newly recognized syndrome of migrating partial
seizures in infancy (MPSI) [56].
BNFS is a benign neonatal epilepsy syndrome classified among the autosomal dominant focal epilepsies
and characterized by onset of seizures during the neonatal period, normal neurologic examination, and negative evaluation for another etiology of the seizures,
normal developmental and intellectual outcome, and
positive family history of newborn seizures with benign outcome [57–61]. Seizures usually occur usually
in clusters for a few days and then stop after several
weeks or months. Seizures are generally brief, lasting
for approximately 1 to 2 min, but may occur as many
as 20 to 30 times a day. Although generalized seizures
have also been reported, seizures are often of a mixed
type, starting with tonic posture, apnea and other au-
35
tonomic features, and progressing to focal or multifocal clonic seizures. EEG and video-EEG recordings
showed that seizures started with bilateral, symmetrical
flattening of the EEG for 5 to 19 sec; simultaneously
there was apnea and tonic motor activity [58–61]. The
EEG flattening was followed by a long (1–2 min) bilateral discharge of spikes and sharp waves; simultaneously, there were vocalizations, chewing, and focal
or generalized clonic activity. The prominence of EEG
and motor abnormalities varied between the left and the
right from one seizure to the next in any given child.
The seizures stopped without EEG or clinical postictal depression. Interictal EEG is of little assistance in
making the diagnosis of BNFS. It may or may not be
abnormal interictally, and no diagnostic features have
been described. The abnormalities reported included
spikes, sharp waves, “epileptiform” patterns, “generalized periodicity”, and slowing, but abnormal findings
are mostly transient [58–61].
In many published case reports, EEG was not performed or the results were not described in sufficient
detail. This the only autosomal dominant epilepsy syndrome where the molecular basis has essentially been
defined, the vast majority of families carrying mutations or deletions of the potassium channel subunit
genes KCNQ2 or KCNQ3 on chromosomes twenty and
eight respectively [62,63].
MPSI is a newly recognized epileptic syndrome, labeled as “syndrome in development” in the ILAE diagnostic scheme [55]. It is characterized by the onset
in the first 6 months of age of nearly continuous multifocal partial seizures arising independently and sequentially from both hemispheres, progression through
a period of intractable seizures, subsequent neurological deterioration or arrest with complete loss of both
cognitive and motor abilities, and decline of head circumference percentile [56,64–66,68–70]. To date, no
etiology has been found for this disorder. Conventional
AEDs have proven ineffective as well as trials with various vitamins and ketogenic diet. Successful control
of seizures has been reported with potassium bromide
and levetiracetam [65–67]. Approximately 50 cases of
this unusual but easily overlooked epilepsy syndrome
have been studied. Although the usual time of seizure
onset is at 1 to 6 months, onset in the first days of life
has been reported, and approximately one-half of cases
had onset in the first month of life. Neuroimaging is
reported as normal at onset and, when abnormal, show
progressive atrophy on follow-up. At onset, interictal
EEG background varies from normal to diffuse slowing [56,64,68] and epileptiform discharges may be rare,
36
M.R. Cilio / Neonatal electroencephalography
Fig. 6. Ictal recording of an infant with migrating partial seizures in infancy. (A) A seizure starts over the left frontal region; (B) Another seizure
starts over the right frontal region before the end of the first event; (C) Simultaneous ictal discharges involve two different area of the brain, the
left frontal region and the right frontal region; (D) The first event ends while the second over the right frontal region persists; (E) Another ictal
discharge arises from the left frontocentral region.
with a unifocal or multifocal interictal patterns. The
multifocal character of the seizures may become evident only with prolonged video-EEG monitoring, sug-
gesting that long-term monitoring plays an important
role in the diagnosis of this disease [70]. EEGs reflect
the escalation of seizure activity as no infant continues
M.R. Cilio / Neonatal electroencephalography
37
Fig. 6, continued.
to have a normal EEG. The location of the ictal onset
varies not only from side to side but also within a hemisphere. Electrographically, the single ictal event can
shift from one region to another and from one hemisphere to the other and additional seizures beginning in
other areas in either hemisphere could start before the
end of the first event, or immediately follow it [56,64–
70] (Fig. 6). The clinical semiology of seizures begins
with focal motor movements that can alternate from
one side of the body to another with lateral deviation of
38
M.R. Cilio / Neonatal electroencephalography
Fig. 6, continued.
the head and eyes and eye jerks, twitching of the eyelids, limb myoclonic jerks, and increased tone of one
or both limbs. In addition, it is worth mentioning that
in very young patients motor and autonomic signs are
often the only clinically relevant symptoms of seizures.
Focal motor components are often accompanied by autonomic signs including flushing of the face, salivation
and apnea. Truly generalized tonic-clonic seizures are
very rare. Prolonged observation soon shows that both
sides are alternatively affected, which demonstrates the
involvement of the whole brain cortex. In a few cases [56,65–67,69] seizures were eventually controlled
and these children partly recovered motor and cognitive
abilities. In all series, developmental outcome appears
better in those with better seizure control, compared
with those with continued intractable seizures. Some
patients die [56,66,67,70]. More recently, Marsh et
al. [69] published a series of infants with MPSI and a
slightly better outcome than previously reported. Given
the unique clinical and EEG features exhibited by children with MPSI, it is extremely unlikely that this condition could be mistaken for one of the severe epileptic
syndromes of neonatal period, such EME and OS, as the
above entities do have a typical interictal EEG pattern,
such as burst-suppression in EME and OS. Differently
from OS, spasms are lacking in MPSI [56,64–70].
OS and EME represent the earliest forms of epileptic
encephalopathy. The concept of epileptic encephalopa-
thy has been recently introduced and indicated a condition in which the epileptiform abnormalities themselves
are believed to contribute to the progressive disturbance
in cerebral function [55].
OS and EME are both characterized by a very early onset, mainly within 1 month and often within the
first 10 days, and by a suppression-bursts pattern on
EEG [71,72]. For those reasons, they are also known
as neonatal epileptic encephalopathy with suppressionburst pattern [36].
EME is characterized clinically by the onset of fragmentary myoclonus appearing in the first month of life,
often associated with erratic focal seizures [73,74]. Onset sometimes occurs as early as a few hours after birth,
and postnatal movements are sometimes reported by
the mother to be of the same type as those felt at the
end of pregnancy. Erratic myoclonias shift typically
from one part of the body to another in a random and
asynchronous fashion. They are often restricted in a
finger, a toe, the eyebrows, eyelids, or lips, occurring in
the same muscle group and often migrating elsewhere
(Fig. 7). The polygraphic EEG recording demonstrates
the presence of myoclonias that are brief, single or
repetitive, and can be very frequent or nearly continuous. Massive, usually bisynchronous, axial myoclonic
jerks may start from the onset of the disease or occur
later, often interspersed with erratic myoclonias [75].
Simple focal seizures are usually subtle with eye devi-
M.R. Cilio / Neonatal electroencephalography
39
Fig. 7. Poligraphic electroencephalography recording in a 7-day-old full term infant with early myoclonic encephalopathy showing a
burts-suppression pattern. The bursts last 2–3 sec and appear synchronously and asynchronously on the two hemispheres. The polygraphic
recording show an altered respiratory pattern with chest movements occurring almost exclusively during the bursts phase. The electromyography
allows to demonstrate fragmentary low amplitude myoclonic jerks involving both extremities and shifting randomly from one side to another.
ation or autonomic symptoms such as flushing of the
face or apnea, but they can be focal clonic involving
any part of the body. Epileptic spasms are rare and generally appear late in the course of the disease, usually
at around 3–4 months of age. Neurological abnormalities are constant: very severe delay in psychomotor acquisitions, marked hypotonia, and disturbed alertness,
sometimes with a vegetative state. Signs of peripheral
neuropathy may also occur in rare cases. Although the
etiology is mostly unknown, nonketotic hyperglycinemia, pyridoxine or pyridoxal-phosphate deficiency or
dependent, and congenital deficiency of the mitochondrial glutamate transporter are known to produce a sim-
ilar clinical picture [75,76]. There is a high risk of
familial recurrence since in most cases the disease appears to be inherited as an autosomal recessive trait.
There is no effective treatment. The prognosis is poor:
children with the condition survive in a persistent vegetative state or die within the first or second year of life.
OS shares with EME the age at onset, the suppressionbursts EEG, and, often, the poor prognosis [36].
The main differences are the seizure types, myoclonic in EME and tonic spasms in OS. Therefore,
in order to distinguish these disorders, in addition to
the usual recording, it is extremely useful to record
the deltoid EMG to detect massive myoclonus or tonic
40
M.R. Cilio / Neonatal electroencephalography
spasms, and distal EMG (fingers, face) to detect erratic myoclonus. The distinction has a great importance
both from a diagnostic point of view, as the search of
etiology can be best directed, and from a therapeutic
point of view since vigabatrin might improve OS but
not EME [71,72]. Epileptic tonic spasms, the main
seizure type in OS, may occur in cluster or singly, both
in the awake or the sleep state. In addition, partial motor seizures are observed in more than half of the cases.
Brain imaging discloses gross structural abnormalities
in most cases, such as Aicardi syndrome, hemimegalencephaly, dento-olivary dysplasia, focal cortical dysplasia. However, recently a de novo mutation in the
gene encoding STXBP1 has been found in individuals
with OS [77]. STXBP1 is involved in synaptic vesicles release, suggesting that the functionally impaired
STXBP1 may affect synaptic functions in the human
brain. Psychomotor development is virtually absent or
markedly retarded. Neurological examination shows
variable signs, depending on the brain malformation,
and is frequently asymmetrical. Some patients may
show an improvement after resection of the cortical
dysgenesis [78].
7. Effect of drugs on neonatal EEG
Although there are few studies documenting the effect of drugs on the neonatal EEG, it is evident that,
as with older children, drugs, especially if in the toxic
range, can alter background activity. Prolonged periods of inactivity on the EEG recording usually occur
following a loading dose of phenobarbital and may last
longer than one hr following administration. Staudt et
al. [79] argued that infants with phenobarbital plasma
levels above 6 mg/dL show significant background suppression. Other authors also reported the appearance of
isoelectric or invariant discontinuous record after treatment with phenobarbital [11,80]. Levels greater that
25 µg/mL in neonates were reported to suppress EEG
activity [71]. In their study, Ashwal and Schneider [80]
found discordance between EEG activity and radionuclide uptake in infants with phenobarbital level between
25 and 35 µg/mL. The lack of EEG activity with presence of cerebral blood flood suggested that phenobarbital suppressed EEG activity. In the same study, one infant who met the clinical criteria for brain death had absent cerebral activity with level of 30 µg/mL. However,
he developed some cerebral activity when the phenobarbital level fell to zero [80]. These are important observations that should be taken in account by electroen-
cephalographers, as phenobarbital therapy is frequently administered to the neonate on a clinical basis, prior
to the first EEG recording. However, this correlation
was not confirmed in preterm infants. Benda et al. [19]
in studying 46 preterm infants found that a mean serum
level of phenobarbital of 34.5 µg/mL with a range 14–
64 µg/mL did not prolonged interburst intervals during trace discontinue in preterm infants. Among medication other than AEDs that may also affect the EEG
tracing, morphine has been found to produce profound,
largely reversible alteration of neonatal EEG as recorded in preterm as well as full-term infants [81]. Conversely, when Bye et al. [82] investigated the effect
of morphine and midazolam on background EEG of
a group of neonates undergoing extracorporeal membrane oxygenation, they noted that despite midazolam
and morphine serum levels were sufficient to produce
adequate sedation, no patients had burst-suppressed or
inactive EEG backgrounds. In addition, these authors
pointed out that prolonged immobility due to sedation
may lead to scalp edema and subsequent artifactual
attenuation of EEG background [82].
8. Conclusions
Despite being one of the oldest tests available, EEG
remains the only neurodiagnostic procedure that provides a continuous record of cerebral function over long
periods. Although other advanced methods of anatomic or functional investigations provide detailed snapshots into cerebral pathophysiology, EEG provides a
valuable assessment of cerebral functioning, and its
evolution and structure in time. However, after having
been in routine use for about half a century, EEG is
currently facing unprecedented challenges in the newborn because of the survival of high-risk infants and the
development of neuroprotective strategies. Therefore,
its use should be extended to those centers that do not
currently have access to either the equipment or expertise required for prompt neonatal EEG recording and
interpretation. Interictal EEG findings are particularly useful in predicting neurologic outcome in neonates
with seizures. Background EEG activity is an excellent
indicator of outcome. The combination of age at onset,
seizure types, interictal and ictal EEG patterns, defines
an epilepsy syndrome. Delineating epilepsy syndromes
in the newborn allows a greater precision in diagnosis, prognosis and treatment than simply classifying the
seizure types.
M.R. Cilio / Neonatal electroencephalography
References
[19]
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
[13]
[14]
[15]
[16]
[17]
[18]
M.S. Scher, M.J. Painter, I. Bergman, M.A. Barmada and
J. Brunberg, EEG diagnoses of neonatal seizures: clinical
correlations and outcome, Pediatr Neurol 5 (1989), 17–24.
G. Holmes, J. Rowe, J. Hafford, R. Schmidt, M. Testa and A.
Zimmerman, Prognostic value of the electroencephalogram in
neonatal asphyxia, Electroencephalogr Clin Neurophysiol 53
(1982), 60–72.
R.R. Clancy, A. Legido and D. Lewis, Occult neonatal
seizures, Epilepsia 29 (1988), 256–261.
M.S. Scher, J. Alvin, L. Gaus, B. Minnigh and M.J. Painter,
Uncoupling of EEG-clinical neonatal seizures after antiepileptic drug use, Pediatr Neurol 28 (2003), 277–280.
J.S. Wyatt, P.D. Gluckman, P.Y. Liu, D. Azzopardi, R. Ballard,
A.D. Edwards, D.M. Ferriero, R.A. Polin, C.M. Robertson, M.
Thoresen, A. Whitelaw and A.J. Gunn, CoolCap Study Group,
Determinants of outcome after head cooling for neonatal encephalopathy, Pediatrics 119 (2007), 912–921.
S. Sarkar, J.D. Barks and S.M. Donn, Should amplitudeintegrated electroencephalogram be used to identify infants
suitable for hypothermic neuroprotection? J Perinatol 28
(2008), 117–122.
M.S. Sher, Electroencephalography of the newborn: normal
features, in: Clinical Neurophysiology of Infancy, Childhood,
and Adolescence, (1st ed.), G.L. Holmes, S.L. Moshé and H.
Royden Jones Jr., eds, Philadelphia: Butterworth Heinemann
Elsevier, 2006, pp. 46–69.
C.T. Lombroso, Neonatal polygraphy in full-term and premature infants: a review of normal and abnormal findings, J Clin
Neurophysiol 2 (1985), 105–155.
R.A. Hrachovy, E.M. Mizrahi and P. Kellaway, Electroencephalography of the newborn, in: Current Practice of Clinical Electroencephalography, D.D. Daly and T.A. Pedley, eds,
New York: Raven Press, 1990, p. 201.
F. Torres and C. Anderson, The normal EEG of the human
newborn, J Clin Neurophysiol 2 (1985), 89–103.
C. Pezzani, M.F. Radvanyi-Bouvet, J.P. Relier and M. Monod,
Neonatal electroencephalography during the first twenty-four
hr of life in full-term newborn infants, Neuropediatrics 17
(1986), 11–18.
H.B. van Lieshout, J.W. Jacobs, J.J. Rotteveel, W. Geven and
M. v’t Hof, The prognostic value of the EEG in asphyxiated
newborns, Acta Neurol Scand 91 (1995), 203–207.
G.L. Holmes and C.T. Lombroso, Prognostic value of background patterns in the neonatal EEG, J Clin Neurophysiol 10
(1993), 323–352.
D. Selton and M. André, Prognosis of hypoxic-ischaemic encephalopathy in full-term newborns value of neonatal electroencephalography, Neuropediatrics 28 (1997), 276–280.
K. Watanabe, F. Hayakawa and A. Okumura, Neonatal EEG:
a powerful tool in the assessment of brain damage in preterm
infants, Brain Dev 21 (1999), 361–372.
S. Marret, D. Parain, J.F. Ménard et al., Prognostic value of
neonatal electroencephalography in premature newborns less
than 33 weeks of gestational age, Electroencephalogr Clin
Neurophysiol 102 (1997), 178–185.
T. Takeuchi and K. Watanabe, The EEG evolution and neurological prognosis of neonates with perinatal hypoxia, Brain
Dev 11 (1989), 115–120.
J. Connell, L. de Vries, R. Oozer, R. Regev, L.M. Dubowitz
and V. Dubowitz, Predictive value of early continuous electroencephalogram monitoring in ventilated preterm infants
[20]
[21]
[22]
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
41
with intraventricular hemorrhage, Pediatrics 82 (1988), 337–
343.
G.I. Benda, R.C. Engel and Y.P. Zhang, Prolonged inactive
phases during the discontinuous pattern of prematurity in the
electroencephalogram of very-low-birthweight infants, Electroencephalogr Clin Neurophysiol 72 (1989), 189–197.
J.S. Hanh and B.R. Tharp, The dysmature EEG pattern in infants with bronchopulmonary dysplasia and its prognostic implications, Electroencephalogr Clin Neurophysiol 76 (1990),
106–113.
E. Biagioni, L. Bartalena, P. Biver, R. Pieri and G. Cioni,
Electroencephalographic dysmaturity in preterm infants: a
prognostic tool in the early postnatal period, Neuropediatrics
27 (1996), 311–316.
E. Biagioni, A. Boldrini, U. Bottone, R. Pieri and G. Cioni,
Prognostic value of abnormal EEG transients in preterm and
full-term neonates, Electroencephalogr Clin Neurophysiol 99
(1996), 1–9.
S.E. Jacobs, Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: Multicentre randomised trial, Lancet 365 (2005), 663–670.
S. Shankaran, A.R. Laptook, R.A. Ehrenkranz et al., Wholebody hypothermia for neonates with hypoxic-ischemic encephalopathy, N Engl J Med 353 (2005), 1574–1584
D.M. Murray, C.A. Ryan, G.B. Boylan, A.P. Fitzgerald and S.
Connolly, Prediction of seizures in asphyxiated neonates: correlation with continuous video-electroencephalographic monitoring, Pediatrics 118 (2006), 41–46.
M.C. Toet, L. Hellström-Westas, F. Groenendaal, P. Eken and
L.S. de Vries, Amplitude integrated EEG 3 and 6 hr after birth
in full term neonates with hypoxic-ischaemic encephalopathy,
Arch Dis Child Fetal Neonatal Ed 81 (1999), F19–F23.
J.M. Rennie, G. Chorley, G.B. Boylan, R. Pressler, Y. Nguyen
and R. Hooper, Non-expert use of the cerebral function monitor for neonatal seizure detection, Arch Dis Child Fetal Neonatal Ed 89 (2004), F37–F40.
A.L. Rose and C.T. Lombroso, A study of clinical, pathological, and electroencephalographic features in 137 full-term babies with a long-term follow-up, Pediatrics 45 (1970), 404–
425.
N. Monod, N. Pajot and S. Guidasci, The neonatal EEG: statistical studies and prognostic value in full-term and pre-term babies, Electroencephalogr Clin Neurophysiol 32 (1972), 529–
544.
J.C. Rowe, G.L. Holmes, J. Hafford et al., Prognostic value of
the electroencephalogram in term and preterm infants following neonatal seizures, Electroencephalogr Clin Neurophysiol
60 (1985), 183–196.
R.L. Khan, M.L. Nunes, L.F. Garcias da Silva and J.C. da
Costa, Predictive value of sequential electroencephalogram
(EEG) in neonates with seizures and its relation to neurological
outcome, J Child Neurol 23 (2008), 144–150.
K. Aso, M.S. Scher and M.A. Barmada, Neonatal electroencephalography and neuropathology, J Clin Neurophysiol 6
(1989), 103–123.
C.T. Lombroso, Some aspects of EEG polygraphy in newborn
at risk for neurological disorders, Electroencephalogr Clin
Neurophysiol Suppl 36 (1982), 652–663.
M. Steriade, F. Amzica and D. Contreras, Cortical
and thalamic cellular correlates of electroencephalographic
burst-suppression, Electroencephalogr Clin Neurophysiol 90
(1994), 1–16.
42
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
[43]
[44]
[45]
[46]
[47]
[48]
[49]
[50]
[51]
[52]
[53]
M.R. Cilio / Neonatal electroencephalography
C.C. Menache, B.F. Bourgeois and J.J. Volpe, Prognostic value
of neonatal discontinuous EEG, Pediatr Neurol 27 (2002),
93–101.
J. Aicardi and S. Ohtahara, Severe neonatal epilepsies with
suppression-burst pattern, in: Epileptic Syndromes in Infancy,
Childhood and Adolescence J. Roger, P. Thomas, M. Bureau,
E. Hirsch, C. Dravet, P. Genton, eds, London: John Libbey
Eurotex, 2005, pp. 39–50.
B.R. Tharp, F. Cukier and N. Monod, The prognostic value
of the electroencephalogram in premature infants, Electroencephalogr Clin Neurophysiol 51 (1981), 219–236.
M.J. Lanska, D.J. Lanska, R.J. Baumann and R.J. Kryscio, A
population-based study of neonatal seizures in Fayette County,
Kentucky, Neurology 45 (1995), 724–732.
E.M. Mizrahi, P. Plouin and R.R. Clancy, Neonatal seizures,
in: Epilepsy: A Comprehensive Textbook, J. Engel, A. Pedley, J. Aicardi, M.A. Dichter, S. Moshé, eds, Philadelphia:
Lippincott-Raven Publishers, 2007, pp. 639–658.
S. Patrizi, G.L. Holmes, M. Orzalesi and F. Allemand, Neonatal seizures:characteristics of EEG ictal activity in preterm and
fullterm infants, Brain Dev 25 (2003), 427–437.
J.N. Gaitanis and J.J. Riviello, Status epilepticus in neonates,
in: Current Clinical Neurology: Status Epilepticus, F.W. Drislane, ed., Totowa, NJ: Humana Press Inc, 2005, pp. 339–352.
L.D. Morton, D.J. Leszczyszyn, L. Kopec-Garnett et al., Maturational changes in the EEG of status epilepticus in the first
six months of life, Neurology 54 (2000), 248.
J.J. Volpe, Neurology of the Newborn, (5th ed.), Philadelphia:
WB Saunders, 2008.
M.J. Litzinger, C.L. Mouritsen, B.B. Grover, M.S. Esplin
and J.R. Abbott, Regional differences in the critical period neurodevelopment in the mouse:implications for neonatal
seizures, J Child Neurol 9 (1994), 77–80.
C.G. Wasterlain, H. Hattori, C. Yang, P.H. Schwartz, D.G.
Fujikawa, A.M. Morin, B.E. Dwyer, Selective vulnerability
of neuronal subpopulations during ontogeny reflects discrete
molecula events associated with normal brain development,
in: Neonatal Seizures, C.G. Wasterlain and P. Vert, eds, New
York: Raven Press, 1990, pp. 77–80.
M. Mizrahi and P. Kellaway, Diagnosis and Management of
Neonatal Seizures, Philadelphia: Lippincott-Raven, 1998.
J.J. Volpe, Neonatal seizures: current concepts and revised
classification, Pediatrics 84 (1989), 422–428.
E.M. Mizrahi and P. Kellaway, Characterization and classification of neonatal seizures, Neurology 37 (1987), 1837–1844.
D.A. Shewmon, What is a neonatal seizure? Problems in definition and quantification for investigative and clinical purposes, J Clin Neurophysiol 7 (1990), 315–368.
M.S. Scher, K. Aso, M.E. Beggarly, M.Y. Hamid, D.A. Steppe
and M.J. Painter, Electrographic seizures in preterm and fullterm neonates: clinical correlates,associated brain lesions, and
risk for neurologic sequelae, Pediatrics 91 (1993), 128–134.
M. Mastrangelo, A. Van Lierde, M. Bray, G. Pastorino, A.
Marini and F. Mosca, Epileptic seizures, epilepsy and epileptic
syndromes in newborns: a nosological approach to 94 new
cases by the 2001 proposed diagnostic scheme for people with
epileptic seizures and with epilepsy, Seizure 14 (2005), 304–
311.
H. Gastaut, Clinical and electroencephalographical classification of epileptic seizures, Epilepsia 10 (1969), 2–13.
Commission on classification and terminology of the International League Against Epilepsy (No authors listed), Proposal for revised classification of epilepsies and epileptic syndromes, Commission on Classification and Terminology of the
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
International League Against Epilepsy, Epilepsia 30 (1989),
389–399.
R. Nabbout and O. Dulac, Epileptic syndromes in infancy and
childhood, Curr Opin Neurol 21 (2008), 161–166.
J. Engel Jr., International League Against Epilepsy. A proposed diagnostic scheme for people with epileptic seizures and
with epilepsy: report of the ILAE Task Force on Classification
and Terminology, Epilepsia 42 (2001), 796–803.
G. Coppola, P. Plouin, C. Chiron, O. Robain and O. Dulac,
Migrating partial seizures in infancy: a malignant disorder
with developmental arrest, Epilepsia 36 (1995), 1017–1024.
M.R. Cilio, Benign familial neonatal seizures, Orphanet Encyclopedia, March, 2004.
G.M. Ronen, T.O. Rosales, M. Connolly, V.E. Anderson and
M. Leppert, Seizure characteristics in chromosome 20 benign
familial neonatal convulsions, Neurology 43 (1993), 1355–
1360.
E. Hirsch, A. Velez, F. Sellal et al., Electroclinical signs of
benign neonatal familial convulsions, Ann Neurol 34 (1993),
835–841.
A.M. Bye, Neonate with benign familial neonatal convulsions:
recorded generalized and focal seizures, Pediatr Neurol 10
(1994), 164–165.
P. Plouin, Benign familial neonatal seizures and benign idiopathic neonatal seizures, in: Epilepsy: A Comprehensive
Textbook, J. Engel, A. Pedley, J. Aicardi, M.A. Dichter and
S. Moshé, eds, Philadelphia: Lippincott-Raven Publishers,
2007, pp. 2287–2296.
S.E. Heron, K. Cox, B.E. Grinton et al., Deletions or duplications in KCNQ2 can cause benign familial neonatal seizures,
J Med Genet 44 (2007), 791–796.
M.V. Soldovieri, M.R. Cilio, F. Miceli et al., Atypical gating
of M-type potassium channels conferred by mutations in uncharged residues in the S4 region of KCNQ2 causing benign
familial neonatal convulsions, J Neurosci 27 (2007), 4919–
4928.
M.R. Cilio, O. Dulac, R. Guerrini and F. Vigevano, Migrating
partial seizures in infancy, in: Epilepsy: A Comprehensive
Textbook,J. Engel, A. Pedley, J. Aicardi, M.A. Dichter, S.
Moshé, eds, Philadelphia: Lippincott-Raven, 2007, pp. 2323–
2328.
K. Okuda, A. Yasuhara, A. Kamei, A. Araki, N. Kitamura
and Y. Kobayashi, Successful control with bromide of two
patients with malignant migrating partial seizures in infancy,
Brain Dev 22 (2000), 56–59.
G. Hmaimess, H. Kadhim, M.C. Nassogne, C. Bonnier and K.
van Rijckevorsel, Levetiracetam in a neonate with malignant
migrating partial seizures, Pediatr Neurol 34 (2006), 55–59.
M.R. Cilio, R. Bianchi, C. Armelisasso et al., Intravenous
levetiracetam terminates refractory status epilepticus in migrating partial seizures in infancy, Epilepsia 49 (2008), 213,
(abstract).
R.H. Caraballo, E. Fontana, F. Darra et al., Migrating focal
seizures in infancy: analysis of the electroclinical patterns in
17 patients, J Child Neurol 23 (2008), 497–506.
E. Marsh, S.E. Melamed, T. Barron and R.R. Clancy, Migrating partial seizures in infancy: expanding the phenotype of a
rare seizure syndrome, Epilepsia 46 (2005), 568–572.
J.M. Wilmshurst, D.B. Appleton and P.J. Grattan-Smith, Migrating partial seizures in infancy: two new cases, J Child
Neurol 15 (2000), 717–722.
O. Dulac, Epileptic encephalopathy, Epilepsia 42 (2001), 23–
26.
M.R. Cilio / Neonatal electroencephalography
[72]
[73]
[74]
[75]
[76]
[77]
R. Nabbout and O. Dulac, Epileptic encephalopathies: a brief
overview, J Clin Neurophysiol 20 (2003), 393–397.
B. Dalla Bernardina, O. Dulac, N. Fejerman et al., Early myoclonic epileptic encephalopathy, Eur J Pediatr 140 (1983),
248–252.
R. Nabbout, Early infantile epileptic encephalopathy, Orphaned Encyclopedia, July, 2004.
M. Mastrangelo, L. Canafoglia, S. Franceschetti et al., Highfrequency rhythmic cortical myoclonus in a long-surviving patient with nonketotic hypergylcemia, J Child Neurol 23 (2008),
321–324.
D. Wang, J.M. Pascual, H. Yang et al., Glut-1 deficiency syndrome: clinical, genetic, and therapeutic aspects, Ann Neurol
57 (2005), 111–118.
H. Saitsu, M. Kato, T. Mizuguchi et al., De novo mutations in
the gene encoding STXBP1 (MUNC18-1) cause early infantile
epileptic encephalopathy, Nat Genet 40 (2008), 782–788.
[78]
[79]
[80]
[81]
[82]
43
J.M. Pedespan, H. Loiseau, A. Vital, C. Marchal, D. Fontan
and A. Rougier, Surgical treatment of an early epileptic encephalopathy with suppression-bursts and focal cortical dysplasia, Epilepsia 36 (1995), 37–40.
F. Staudt, M.L. Scholl, R.W. Coen and R.B. Bickford, Phenobarbital therapy in neonatal seizures and the prognostic value
of the EEG, Neuropediatrics 13 (1982), 24–33.
S. Ashwal and S. Schneider, Brain death in the newborn, Pediatrics 84 (1989), 429–437.
G.B. Young and O.P. da Silva, Effects of morphine on the electroencephalograms of neonates: a prospective, observational
study, Clin Neurophysiol 111 (2000), 1955–1960.
A.M. Bye, D. Lee, D. Naidoo and D. Flanagan, The effects
of morphine and midazolam on EEGs in neonates, J Clin
Neurosci 4 (1997), 173–175.
Video-EEG monitoring in newborns with
hypoxic-ischemic encephalopathy treated
with hypothermia
K.B. Nash, MD*
S.L. Bonifacio, MD*
H.C. Glass, MD
J.E. Sullivan, MD
A.J. Barkovich, MD
D.M. Ferriero, MD
M.R. Cilio, MD, PhD
Address correspondence and
reprint requests to Dr. Maria
Roberta Cilio, Division of
Neurology, Bambino Gesú
Children’s Hospital, Piazza S.
Onofrio 4, 00165 Rome, Italy
maria.cilio@ucsf.edu
ABSTRACT
Background: Therapeutic hypothermia (TH) is becoming standard of care in newborns with
hypoxic-ischemic encephalopathy (HIE). The prognostic value of the EEG and the incidence of
seizures during TH are uncertain.
Objective: To describe evolution of EEG background and incidence of seizures during TH, and to
identify EEG patterns predictive for MRI brain injury.
Methods: A total of 41 newborns with HIE underwent TH. Continuous video-EEG was performed
during hypothermia and rewarming. EEG background and seizures were reported in a standardized manner. Newborns underwent MRI after rewarming. Sensitivity and specificity of EEG background for moderate to severe MRI brain injury was assessed at 6-hour intervals during TH and
rewarming.
Results: EEG background improved in 49%, remained the same in 38%, and worsened in 13%. A
normal EEG had a specificity of 100% upon initiation of monitoring and 93% at later time points.
Burst suppression and extremely low voltage patterns held the greatest prognostic value only
after 24 hours of monitoring, with a specificity of 81% at the beginning of cooling and 100% at
later time points. A discontinuous pattern was not associated with adverse outcome in most
patients (73%). Electrographic seizures occurred in 34% (14/41), and 10% (4/41) developed
status epilepticus. Seizures had a clinical correlate in 57% (8/14) and were subclinical in 43%
(6/14).
Conclusions: Continuous video-EEG monitoring in newborns with HIE undergoing TH provides
prognostic information about early MRI outcome and accurately identifies electrographic seizures, nearly half of which are subclinical. Neurology® 2011;76:556–562
GLOSSARY
AED ⫽ antiepileptic drug; BS ⫽ burst suppression; HIE ⫽ hypoxic-ischemic encephalopathy; ROC ⫽ receiver operating
characteristic; SE ⫽ status epilepticus; TH ⫽ therapeutic hypothermia; UCSF ⫽ University of California, San Francisco.
Hypoxic-ischemic encephalopathy (HIE) after perinatal asphyxia is an important cause of
mortality and neurologic morbidity.1,2 Randomized clinical trials have demonstrated that moderate hypothermia is associated with a reduction in death and neurologic impairment at 18 to
22 months of age.3,4 As a result, many centers now offer therapeutic hypothermia (TH) as a
neuroprotective strategy for neonatal HIE.
Reliable early predictors of neurologic outcome in newborns after acute hypoxic-ischemic
insult are important for counseling families and for making thoughtful treatment decisions.
Clinical assessment can help with prognosis,5-7 although sedating medications and clinical
changes with TH8 are complicating factors. Brain MRI is highly predictive of neurologic
outcome,9,10 including in the setting of hypothermia,11 although it does not provide functional
*These authors contributed equally to this work.
From the Departments of Neurology (K.B.N., H.C.G., J.E.S., D.M.F., M.R.C.), Pediatrics (K.B.N., S.L.B., H.C.G., D.M.F.), and Radiology and
Biomedical Imaging (A.J.B.), and Newborn Brain Research Institute (K.B.N., S.L.B., H.C.G., J.E.S., A.J.B., D.M.F., M.R.C.), University of
California, San Francisco; and Division of Neurology (M.R.C.), Bambino Gesú Children’s Hospital, Rome, Italy.
Study funding: Supported by NIH/NCRR UCSF-CTSI UL1 RR024131 and NIH P50 NS035902-12. S.L.B. was supported by NIH
5T32HD007162. H.C.G. was supported by NIH/NCRR/OD UCSF-CTSI KL2 RR024130. M.R.C. was supported by E-Rare grant JTC 2007
EUROBFNS from the European Commission.
Disclosure: Author disclosures are provided at the end of the article.
556
Copyright © 2011 by AAN Enterprises, Inc.
assessment and its sensitivity for hypoxicischemic injury in the first 48 hours of life is
limited. A single EEG recording during the
first week of life in noncooled infants with
HIE,12-14 and in infants with HIE treated with
TH,15 may help predict neurologic outcome.
However, continuous video-EEG monitoring
is the gold standard for evaluating brain function and for recording electrographic seizures
in neonates with HIE16,17 and it has not yet
been reported in neonates with HIE undergoing TH.
Our aim was to describe the evolution of
the EEG background during TH and rewarming and to determine the incidence of
electrographic seizures in newborns with HIE
treated with moderate hypothermia. We also
sought to determine the prognostic value of
EEG background during TH using brain
MRI as an early outcome measure.
METHODS Consecutive newborns with HIE who underwent
TH with whole-body cooling at University of California, San
Francisco (UCSF), between November 2007 and July 2009 were
included in this cohort study. Our TH clinical protocol is based
on published trials.3,4 Selection for TH included 1) ⱖ36 weeks
gestational age at birth, 2) any of the following: cord or first gas
pH ⬍7.0, cord or first gas base deficit ⬎12, 10-minute Apgar
score ⬍5, or prolonged resuscitation, and 3) moderate to severe
encephalopathy within 6 hours of birth. Exclusion criteria included suspected or known congenital malformation and inborn
errors of metabolism. TH was initiated as soon as possible after
birth at UCSF or at the time of referral from the outside hospital
and consisted of whole-body moderate hypothermia (Cincinnati
Sub-Zero Blanketrol III) (target temperature 33.5°C) for 72
hours followed by rewarming over approximately 6 hours. All
patients received morphine infusion throughout TH to prevent
discomfort and shivering (10 –25 g/kg/h, with boluses as
needed). Clinical and electrographic seizures were treated with
antiepileptic drugs (AEDs) including lorazepam, phenobarbital,
fosphenytoin, and levetiracetam according to institutional guidelines. Clinical data were extracted from medical records.
Standard protocol approvals, registrations, and patient
consents. The Committee on Human Research at UCSF approved the retrospective review of the clinical, EEG, and imaging data for this study.
Video-EEG monitoring. Video-EEG was initiated as soon as
possible after admission to the nursery. As part of our clinical
protocol, infants are continuously monitored with a NicoletOne
video-EEG system throughout TH and rewarming. A trained
technician applied surface electrodes according to the international 10 –20 system, modified for neonates. EEG recordings
were interpreted by a pediatric neurophysiologist (J.S.) for clinical use in the acute setting. Using stored files, full video-EEG
recordings were scored in a standardized fashion by a pediatric
neurophysiologist (M.R.C.) blinded to all clinical factors except
patient age. Predominant background pattern and occurrence of
electrographic seizures and status epilepticus (SE), with or without clinical manifestations, were reported in 6-hour intervals
with the initiation of recording as time “0.” Clinical seizures
without EEG correlates were not considered. For the analysis, we
used the initial 6-hour interval (beginning of cooling), the 24- to
30-hour interval (midcooling), the last interval prior to rewarming (end of cooling), and the first interval after rewarming (postcooling). A seizure was defined as a repetitive, evolving, and
stereotyped pattern, with a definite beginning and end, a minimum duration of 10 seconds, and a minimal amplitude of 2
V.18,19 SE was defined as continuous seizure activity for at least
30 minutes or recurrent seizures for over 50% of 1–3 hours of
recording time.20 EEG background was classified into 5 patterns
as previously described21,22: 1) normal pattern for gestational age,
including recordings with transient periods of discontinuous activity occupying less than 50% of the recording, with presence of
distinct state changes; 2) excessively discontinuous, with persistence of discontinuous activity occupying more than 50% of the
recording and consisting of bursts of normal activity separated
by abnormally long, interburst intervals of more than 6 seconds
duration, and amplitude ⬍25 and ⬎5 V, with poor state
changes; 3) depressed and undifferentiated, with persistently
low-voltage background activity with amplitude between 5 and
15 V and without normal features; 4) burst suppression (BS),
invariant and unreactive pattern of bursts of paroxysmal activity
with mixed features but no age-appropriate activity lasting less
than 10 seconds alternating with periods of marked voltage attenuation with amplitude ⱕ5 V; 5) extremely low voltage, invariant and unreactive pattern, with amplitude ⬍5 V or with
no discernible cerebral activity.
Brain MRI. Infants were imaged shortly after rewarming (median of 5 days of life) using a specialized neonatal head coil on a
1.5-Tesla Signa EchoSpeed system (GE Medical Systems). Imaging sequences included T1- and T2-weighted MRI and
diffusion-weighted imaging. A pediatric neuroradiologist
(A.J.B.), blinded to the clinical history, evaluated all images. Injury was scored using a system strongly predictive of neurodevelopmental outcome following neonatal HIE.23 We defined
normal to mild MRI injury as basal ganglia/thalamus score ⬍2
and watershed score ⬍3 and moderate to severe MRI injury as
basal ganglia/thalamus score ⱖ2 (involving both the thalamus
and the lentiform nucleus) or watershed pattern ⱖ3 (involving
both watershed cortex and white matter). A similar classification
was highly predictive for neurologic disability at 18 months of
age in newborns with HIE treated with hypothermia.11
Statistical analysis. All analyses were performed with STATA
software (Stata 10.1, Stata Corporation, College Station, TX).
2 and Fisher exact tests were used to compare dichotomous
variables, and t test was used for continuous variables. Wilcoxon
rank sum test (Mann-Whitney U) was used to compare nonparametric data. Receiver operating characteristic (ROC) curves were
used to assess the prognostic value of EEG background patterns
at each time interval. We considered significant a p value ⬍ 0.05.
RESULTS Patient population. During the study period, 49 newborns were treated with hypothermia
and 46 had continuous video-EEG available for review. Of these, 41 were evaluated with MRI. Five
infants who were deceased following redirection of
care and were not studied with MRI were excluded.
Four of them had an initial extremely low voltage
Neurology 76
February 8, 2011
557
Table 1
EEG background at specified time intervals was
greatest at midcooling and beyond (table 4).
Beginning of cooling. None of the newborns with a
normal background at the beginning of cooling had
moderate to severe injury. Of the 15 newborns with
an excessively discontinuous pattern, 4 (27%) had
moderate to severe injury, 5 had mild injury, and 6
were normal. In contrast, of the 14 newborns with
BS or extremely low voltage patterns, 9 (64%) had
moderate to severe injury. Of these, 4 had maximal
MRI injury scores. Interestingly, 5 newborns with
BS or extremely low voltage patterns at the beginning
of cooling had a normal MRI or only mild injury. In
all 5 cases, however, the EEG improved by 12–18
hours of recording, and in 3 of them the background
normalized by midcooling.
Midcooling. One newborn whose EEG had normalized by this interval from a discontinuous background at the beginning of cooling had moderate to
severe MRI injury; none of the remaining 14 newborns with a normal EEG during midcooling had
moderate to severe injury. Of the 13 infants with a
discontinuous EEG, again about one-quarter (23%)
had moderate to severe injury, accounting for 2 infants
whose background was unchanged from the beginning
of cooling and an additional infant whose initial background was depressed and undifferentiated. By this
time period, all newborns (7/7, 100%) with BS or extremely low voltage patterns had moderate to severe injury, with 3 having maximal MRI injury scores.
End of cooling. Moderate to severe MRI injury was
present in 1 of the 12 infants (8%) whose background was normal and 3 of the 16 infants (19%)
whose background was excessively discontinuous,
compared with all 5 (100%) whose background
showed BS or extremely low voltage.
Postcooling. During this interval, the same newborn with a normal background (6%) and the same 3
newborns with a discontinuous background (27%)
had moderate to severe injury. All 6 infants with BS
Clinical characteristics and MRI outcome
Moderate to severe
MRI injury
(n ⴝ 15)
No or mild
MRI injury
(n ⴝ 26)
p Value
Gestational age, wk, mean ⴞ SD
39.4 ⫾ 1.5
39.1 ⫾ 1.4
0.4
Sex ratio, M:F
1:1.5
1:1
0.5
Birth weight, g, mean ⴞ SD
3,234 ⫾ 552
3,381 ⫾ 760
0.5
10-min Apgar, median (range)
4 (0–7)
5 (1–8)
0.07
Cord or blood gas pH, mean ⴞ SD
6.86 ⫾ 0.19
6.98 ⫾ 0.21
0.08
Inborn neonates, n (%)
0 (0)
4 (15)
0.09
cerebral activity, and one had BS pattern, both
persisting for more than 24 hours. Their clinical
severity was similar to those with persistent BS or
extremely low voltage activity and moderate to severe MRI injury. Clinical characteristics of newborns with respect to brain injury are presented in
table 1. Mean hour of life to reach target temperature was 5.2 ⫾ 1.9.
Video-EEG monitoring. EEG monitoring was initiated at a mean of 10.2 ⫾ 2.9 hours of life. All infants
reached target temperature before or within 1 hour
after EEG initiation. Mean duration of monitoring
was 90.9 ⫾ 28.2 hours. Nine infants received AEDs
prior to the onset of EEG monitoring, and one of
them subsequently developed subclinical seizures. In
2 newborns, monitoring was discontinued prior to
rewarming.
EEG background pattern. From the beginning of
cooling to rewarming, the background improved in
19 newborns (49%), remained the same in 15
(38%), and worsened in 5 (13%). EEG background
pattern and the burden of moderate to severe MRI
injury at each time interval are presented in table 2.
The background pattern for newborns with moderate to severe injury was significantly worse than for
those with no or mild injury for all monitoring time
points (table 3). The sensitivity and specificity of
Table 2
Evolution of EEG background with hypothermia by severity of MRI injurya
Phase of therapeutic hypothermia
Beginning
EEG background
Normal
Excessively discontinuous
a
None/mild
injury
8 (100)
Mid
End
Post
Moderate/severe
injury
None/mild
injury
Moderate/severe
injury
None/mild
injury
Moderate/severe
injury
None/mild
injury
Moderate/severe
injury
0
14 (93)
1 (7)
11 (92)
1 (8)
15 (94)
1 (6)
11 (73)
4 (27)
10 (77)
3 (23)
13 (81)
3 (19)
8 (73)
3 (27)
Depressed and
undifferentiated
2 (50)
2 (50)
2 (40)
3 (60)
2 (29)
5 (71)
2 (33)
4 (67)
Burst suppression
2 (29)
5 (71)
0
4 (100)
0
2 (100)
0
4 (100)
Extremely low voltage
3 (43)
4 (57)
0
3 (100)
0
3 (100)
0
2 (100)
Values are n (%).
558
Neurology 76
February 8, 2011
Table 3
EEG background evolution, seizures and status epilepticus, and
MRI outcomea
Moderate to severe
MRI injury
(n ⴝ 15)
No or mild
MRI injury
(n ⴝ 26)
p Value
4 (2–5)
2 (1–5)
0.003
EEG background pattern, median (range)
Beginning of cooling
Midcooling
3.5 (1–5)
1 (1–3)
0.0000
End of cooling
3 (1–5)
2 (1–3)
0.0001
Postcooling
3 (1–5)
1 (1–3)
0.0000
Seizures, n (%)
8 (53)
6 (23)
0.05
Status epilepticus, n (%)
4 (27)
0 (0)
0.01
EEG background scoring: 1 ⫽ normal; 2 ⫽ excessively discontinuous; 3 ⫽ depressed and
undifferentiated; 4 ⫽ burst suppression; 5 ⫽ extremely low voltage.
a
or extremely low voltage patterns after rewarming
had moderate to severe injury.
Electrographic seizures and SE. Electrographic sei-
zures were identified in 14 newborns (34%), 4 of
whom had SE. Among the 14 newborns with seizures, 13 (93%) had seizure onset within the first 18
hours of recording, 8 in the first 6 hours. One infant
had seizure onset during rewarming. Recurrent seizures were recorded during midcooling in 2 patients
and during rewarming in 3. Six of 14 patients (43%)
never showed a clinical correlate during seizures, including 3 with subclinical SE. All 4 infants with SE
had BS or extremely low voltage patterns at the beginning of cooling and never recovered better than
depressed and undifferentiated at last time point.
Isolated or recurrent seizures were more frequent in
patients with moderate to severe MRI injury compared with those with no or mild injury (53% vs
23%, p ⫽ 0.05), and SE was only seen in newborns
with moderate to severe injury ( p ⫽ 0.01).
Nonsurviving infants. Among the 5 nonsurviving in-
fants, 4 had persistent BS or extremely low voltage
Table 4
backgrounds throughout the duration of monitoring
and maximal MRI injury, and goals of care were redirected to comfort measures. One infant had an excessively discontinuous background at the initiation
of monitoring, depressed and undifferentiated by
midcooling, with less severe MRI injury. Goals of
care were redirected due to persistent multisystem
failure.
This study demonstrates that continuous video-EEG recording is an important diagnostic and prognostic tool in newborns with HIE
undergoing TH. In our cohort, EEG background
was associated with early MRI findings throughout
the treatment period. A normal EEG was associated
with no or mild MRI brain injury at all time points,
although a normal background at the beginning of
cooling was even more predictive of a favorable MRI
outcome (100% specific) than at later time points
(93% specific), as the EEG background of one newborn with moderate to severe MRI injury improved
from excessively discontinuous to normal over the
first 24 hours of monitoring. In contrast, the prognostic value of a BS pattern or extremely low voltage
background for moderate to severe injury increased
from the beginning of cooling (81% specific) to midcooling and thereafter (100% specific), reflecting 5
newborns with these concerning patterns at the onset
of monitoring who rapidly improved by midcooling
and were spared from moderate to severe MRI injury. The greatest prognostic value of EEG background in this population for predicting moderate to
severe MRI brain injury was not achieved until midcooling, highlighting the importance of continuous
monitoring or sequential EEGs in this population.
Our findings are substantiated by prior studies in
noncooled infants with HIE, which demonstrated
that a normal EEG within the first 2–7 days of life is
DISCUSSION
Sensitivity and specificity of EEG background during hypothermia for moderate to severe MRI injury
Phase of therapeutic hypothermia
Beginning
Mid
EEG background cutpointa
Sensitivity,
%b
Specificity,
%c
Sensitivity,
%b
1 vs 2, 3, 4, 5
100
31
93
1, 2 vs 3, 4, 5
73
73
1, 2, 3 vs 4, 5
60
81
1, 2, 3, 4 vs 5
27
88
Area under receiver
operating characteristic
curve
0.77
End
Specificity,
%c
Sensitivity,
%b
54
93
71
92
50
100
21
100
0.88
Post
Specificity,
%c
Sensitivity,
%b
Specificity,
%c
42
93
71
92
71
92
36
100
43
100
21
100
14
100
0.86
60
0.89
1 ⫽ normal, 2 ⫽ excessively discontinuous, 3 ⫽ depressed/undifferentiated, 4 ⫽ burst suppression, 5 ⫽ extremely low voltage.
Sensitivity: Given moderate to severe injury, % identified as positive by EEG.
c
Specificity: Given no moderate to severe injury, % identified as negative by EEG.
a
b
Neurology 76
February 8, 2011
559
associated with favorable developmental outcome
and a severely abnormal EEG (BS or extremely low
voltage) on the second day of life or thereafter is associated with poor outcome.12-14,24 The few studies that
reported EEG background in this population within
the first 24 hours of life17,25,26 showed a relatively
poor specificity for adverse developmental outcome
following a severely abnormal background during
the first 12 hours of life because of EEG normalization by 12 to 24 hours of life in some infants with
normal outcome. Similarly, in our cohort, a BS or
extremely low voltage EEG was not highly predictive
for moderate to severe MRI injury until the second
day of life, around the time of midcooling. This finding is supported by a prior study evaluating EEG
during hypothermia in neonatal HIE by a single
sample recorded sometimes in the first 48 hours of
life, which found that a background of ⬍5 V was
associated with death or major neurologic disability.15 Similarly, a recent study evaluating the prognostic value of amplitude-integrated EEG in newborns
with HIE exposed to normothermia compared to those
treated with TH showed that a severely abnormal background pattern in the hypothermia-treated group was
not specific for abnormal developmental outcome until
48 hours of life.27
Our findings differ from prior studies of noncooled newborns with HIE in 2 main ways. First,
prior studies have shown that a discontinuous EEG
in the first several days of life is often associated with
poor outcome,28-31 whereas the majority of newborns
in our cohort (73%) with an excessively discontinuous pattern after rewarming had no or only mild
MRI injury. While it is difficult to directly compare
our study to prior studies given the differences in
methodology and the wide range of definitions of
discontinuous background in the literature, the outcome of newborns with an excessively discontinuous
background appears to be different in newborns
treated with hypothermia. Interestingly, clinical encephalopathy on the fourth day of life following TH
has also been shown to be less predictive of outcome
in cooled infants compared to noncooled infants.8
Second, in comparison to the single study of continuous EEG monitoring in noncooled newborns with
HIE which showed improvement of the background
pattern over the first 3 days of life in all newborns,17
the background worsened over the course of monitoring in 13% of newborns in our cohort. Whether
the EEG differences seen in our cohort of infants
with HIE and cooling are attributed to hypothermia
itself or the evolution of injury in this population is
uncertain.
Electrographic seizures were present in 34% of
newborns during TH, and continuous video-EEG
560
Neurology 76
February 8, 2011
revealed that almost 50% of newborns with seizures,
including 3 with SE, had seizures without clinical
correlate. Although experimental studies showed a
potent effect of hypothermia in controlling seizures,32,33 a high incidence of seizures has been reported in children during TH.34 This discrepancy
may be related to the earlier and deeper cooling used
in animal models.32,33 Most studies rely on clinical
evaluation for seizure diagnosis and classification of
seizure severity in newborns.35,36 However, it is
known that the majority of seizures, especially in critically ill infants, do not have a clinical correlate and
will not be recognized without continuous
EEG.16,37,38 Moreover, it is often impossible to accurately differentiate between seizure-related and nonseizure movements in infants using clinical
evaluation alone.39 While isolated or recurrent seizures were recorded in more than 50% of infants
with moderate to severe brain injury, not all were
associated with moderate to severe brain injury. In
contrast, all newborns with SE had severely abnormal
MRI. These results are in keeping with a recent work
suggesting that a significantly worse outcome occurs
in newborns with SE compared to newborns with
recurrent seizures.20
There are several limitations to our study. First,
due to the referral pattern at our institution, newborns did not start monitoring at the exact same time
in the first day of life. However, in most of our patients, monitoring was initiated within the first 12
hours of life. Second, an excessively discontinuous
background by our system encompassed a broad
range of interburst intervals. Therefore, it is not surprising that a discontinuous pattern was a relatively
poor predictor of MRI brain injury. Third, we used
MRI as a short-term outcome measure and do not
yet know the long-term outcome in this cohort. It
has been reported that hypothermia does not affect the prognostic value of MRI in newborns with
HIE. 11 However, long-term developmental
follow-up of this cohort is needed to confirm our
results. Finally, as many patients with poor EEG
backgrounds and moderate to severe brain injury
were treated with AEDs, we were unable to assess
whether depressed background activity was an effect
of medication or due to underlying brain injury.
EEG monitoring in newborns is noninvasive,
provides data from the entire cortex, and can be easily performed at the bedside. Our findings underscore the importance of continuous EEG monitoring
in this population to assist with seizure management
and discussions regarding prognosis and goals of
care. Even in the setting of hypothermia, EEG remains a strong predictive tool, and its routine use
alongside clinical evaluation and MRI is warranted.
Establishing consensus on neonatal EEG nomenclature and classification will help future studies on the
prognostic value of EEG during TH. Particularly,
further analysis and revalidation of the excessively
discontinuous pattern in neonates being treated with
HIE is warranted. Given emerging data suggesting
that seizures may be associated with increased brain
injury following neonatal HIE,35,36,40 accurate seizure
detection is becoming an important issue in the context of neuroprotection. Future studies that evaluate
whether rapid and effective treatment of seizures will
improve neurologic outcome will rely on continuous
EEG monitoring.
7.
8.
9.
10.
11.
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. H.C. Glass, Dr. S.L. Bonifacio,
and Dr. K.B. Nash.
12.
ACKNOWLEDGMENT
The authors thank the neonatal research nurses of the Pediatric Clinical
Research Center at UCSF for their work on this study.
13.
DISCLOSURE
Dr. Nash reports no disclosures. Dr. Bonifacio has received fellowship
support from the NIH. Dr. Glass has received research support from the
NIH. Dr. Sullivan has received research support from Pfizer Inc. and the
NIH. Dr. Barkovich serves on the editorial boards of the American Journal
of Neuroradiology, Neuroradiology, Brain and Development, and Neuropediatrics; receives royalties from the publication of Pediatric Neuroimaging,
4th ed. (Lippincott Williams & Wilkins, 2005), Pediatric Neuroradiology
(Amirsys, 2008), and Neuroradiology, 2nd ed. (Amirsys, 2009); and receives research support from the NIH. Dr. Ferriero serves on a scientific
advisory board for the NIH/NINDS; serves as an Associate Editor for
Annals of Neurology and Pediatric Research; receives royalties from the publication of Principle and Practices of Pediatric Neurology (Elsevier, 2005);
and receives research support from the NIH. Dr. Cilio receives research
support from the European Commission.
14.
15.
16.
17.
Received June 7, 2010. Accepted in final form October 12, 2010.
18.
REFERENCES
1. Pierrat V, Haouari N, Liska A, Thomas D, Subtil D,
Truffert P. Prevalence, causes, and outcome at 2 years of
age of newborn encephalopathy: population based study.
Arch Dis Child Fetal Neonatal Ed 2005;90:F257–F261.
2. Pin TW, Eldridge B, Galea MP. A review of developmental outcomes of term infants with post-asphyxia neonatal
encephalopathy. Eur J Paediatr Neurol 2009;13:224 –234.
3. Shankaran S, Laptook AR, Ehrenkranz RA, et al. Wholebody hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005;353:1574 –1584.
4. Azzopardi DV, Strohm B, Edwards AD, et al. Moderate
hypothermia to treat perinatal asphyxial encephalopathy.
N Engl J Med 2009;361:1349 –1358.
5. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress: a clinical and electroencephalographic
study. Arch Neurol 1976;33:696 –705.
6. Mercuri E, Guzzetta A, Haataja L, et al. Neonatal neurological examination in infants with hypoxic ischaemic encephalopathy: correlation with MRI findings. Neuropediatrics
1999;30:83– 89.
19.
20.
21.
22.
23.
24.
Miller SP, Latal B, Clark H, et al. Clinical signs predict
30-month neurodevelopmental outcome after neonatal encephalopathy. Am J Obstet Gynecol 2004;190:93–99.
Gunn AJ, Wyatt JS, Whitelaw A, et al. Therapeutic hypothermia changes the prognostic value of clinical evaluation
of neonatal encephalopathy. J Pediatr 2008;152:55–58.
Barnett A, Mercuri E, Rutherford M, et al. Neurological
and perceptual-motor outcome at 5– 6 years of age in children with neonatal encephalopathy: relationship with neonatal brain MRI. Neuropediatrics 2002;33:242–248.
Miller SP, Ramaswamy V, Michelson D, et al. Patterns of
brain injury in term neonatal encephalopathy. J Pediatr
2005;146:453– 460.
Rutherford M, Ramenghi LA, Edwards AD, et al. Assessment of brain tissue injury after moderate hypothermia in
neonates with hypoxic-ischaemic encephalopathy: a nested
substudy of a randomised controlled trial. Lancet Neurol
2010;9:39 – 45.
Monod N, Pajot N, Guidasci S. The neonatal EEG: statistical studies and prognostic value in full-term and pre-term
babies. Electroencephalogr Clin Neurophysiol 1972;32:
529 –544.
Watanabe K, Miyazaki S, Hara K, Hakamada S. Behavioral state cycles, background EEGs and prognosis of newborns with perinatal hypoxia. Electroencephalogr Clin
Neurophysiol 1980;49:618 – 625.
Holmes G, Rowe J, Hafford J, Schmidt R, Testa M, Zimmerman A. Prognostic value of the electroencephalogram
in neonatal asphyxia. Electroencephalogr Clin Neurophysiol 1982;53:60 –72.
Mariani E, Scelsa B, Pogliani L, Introvini P, Lista G. Prognostic value of electroencephalograms in asphyxiated newborns treated with hypothermia. Pediatr Neurol 2008;39:
317–324.
Murray DM, Ryan CA, Boylan GB, Fitzgerald AP, Connolly S. Prediction of seizures in asphyxiated neonates: correlation with continuous video-electroencephalographic
monitoring. Pediatrics 2006;118:41– 46.
Murray DM, Boylan GB, Ryan CA, Connolly S. Early
EEG findings in hypoxic-ischemic encephalopathy predict
outcome at 2 years. Pediatrics 2009;124:e459 – e467.
Clancy RR, Legido A. The exact ictal and interictal duration of electroencephalographic neonatal seizures. Epilepsia 1987;28:537–541.
Scher MS, Hamid MY, Steppe DA, Beggarly ME, Painter
MJ. Ictal and interictal electrographic seizure durations in
preterm and term neonates. Epilepsia 1993;34:284 –288.
Pisani F, Cerminara C, Fusco C, Sisti L. Neonatal status
epilepticus vs recurrent neonatal seizures: clinical findings
and outcome. Neurology 2007;69:2177–2185.
Holmes GL, Lombroso CT. Prognostic value of background patterns in the neonatal EEG. J Clin Neurophysiol
1993;10:323–352.
Lamblin MD, André M, Challamel MJ, et al. Électroencéphalographie du nouveau-né prématuré et à terme: aspects maturatifs et glossaire. Neurophysiol Clin 1999;29:
123–219.
Barkovich AJ, Hajnal BL, Vigneron D, et al. Prediction of
neuromotor outcome in perinatal asphyxia: evaluation of MR
scoring systems. AJNR Am J Neuroradiol 1998;19:143–149.
Selton D, Andre M. Prognosis of hypoxic-ischaemic encephalopathy in full-term newborns–value of neonatal electroencephalography. Neuropediatrics 1997;28:276 –280.
Neurology 76
February 8, 2011
561
25.
Pezzani C, Radvanyi-Bouvet MF, Relier JP, Monod N.
Neonatal electroencephalography during the first twentyfour hours of life in full-term newborn infants. Neuropediatrics 1986;17:11–18.
26. Pressler RM, Boylan GB, Morton M, Binnie CD, Rennie
JM. Early serial EEG in hypoxic ischaemic encephalopathy. Clin Neurophysiol 2001;112:31–37.
27. Thoresen M, Hellström-Westas L, Liu X, de Vries LS. Effect
of hypothermia on amplitude-integrated electroencephalogram
in infants with asphyxia. Pediatrics 2010;126:131–139.
28. Biagioni E, Mercuri E, Rutherford M, et al. Combined use
of electroencephalogram and magnetic resonance imaging
in full-term neonates with acute encephalopathy. Pediatrics 2001;107:461– 468.
29. Wertheim D, Mercuri E, Faundez JC, Rutherford M, Acolet D, Dubowitz L. Prognostic value of continuous electroencephalographic recording in full term infants with
hypoxic ischaemic encephalopathy. Arch Dis Child 1994;
71:F97–F102.
30. van Lieshout HB, Jacobs JW, Rotteveel JJ, Geven W, v’t
Hof M. The prognostic value of the EEG in asphyxiated
newborns. Acta Neurol Scand 1995;91:203–207.
31. Menache CC, Bourgeois BF, Volpe JJ. Prognostic value of
neonatal discontinuous EEG. Pediatr Neurol 2002;27:93–101.
32. Liu Z, Gatt A, Mikati M, Holmes GL. Effect of temperature on kainic acid seizures. Brain Res 1993;631:51–58.
33.
34.
35.
36.
37.
38.
39.
40.
Schmitt FC, Buchheim K, Meierkord H, Holtkamp M.
Anticonvulsant properties of hypothermia in experimental
status epilepticus. Neurobiol Dis 2006;23:689 – 696.
Abend NS, Topjian A, Ichord R, et al. Electroencephalographic monitoring during hypothermia after pediatric
cardiac arrest. Neurology 2009;72:1931–1940.
Glass HC, Glidden D, Jeremy RJ, Barkovich AJ, Ferriero
DM, Miller SP. Clinical neonatal seizures are independently associated with outcome in infants at risk for
hypoxic-ischemic brain injury. J Pediatr 2009;155:318 –
323.
Miller SP, Weiss J, Barnwell A, et al. Seizure-associated
brain injury in term newborns with perinatal asphyxia.
Neurology 2002;58:542–548.
Murray DM, Boylan GB, Ryan CA, Connolly S. Early
continuous video-EEG in acute near-total intrauterine asphyxia. Pediatr Neurol 2006;35:52–56.
Clancy RR, Legido D, Lewis D. Occult neonatal seizures.
Epilepsia 1988;29:256 –261.
Malone A, Ryan CA, Fitzgerald A, Burgoyne L, Connolly
S, Boylan GB. Interobserver agreement in neonatal seizure
identification. Epilepsia 2009;50:2097–2101.
Bjorkman ST, Miller SM, Rose SE, Burke C, Colditz PB.
Seizures are associated with brain injury severity in a neonatal model of hypoxia-ischemia. Neuroscience 2010;166:
157–167.
Neurology® Launches Subspecialty Alerts by E-mail!
Customize your online journal experience by signing up for e-mail alerts related to your subspecialty
or area of interest. Access this free service by visiting http://www.neurology.org/cgi/alerts/
etoc.xhtml or click on the “E-mail Alerts” link on the home page. An extensive list of subspecialties,
methods, and study design choices will be available for you to choose from—allowing you priority
alerts to cutting-edge research in your field!
562
Neurology 76
February 8, 2011