Help seeking and delay literature – Key insights
advertisement
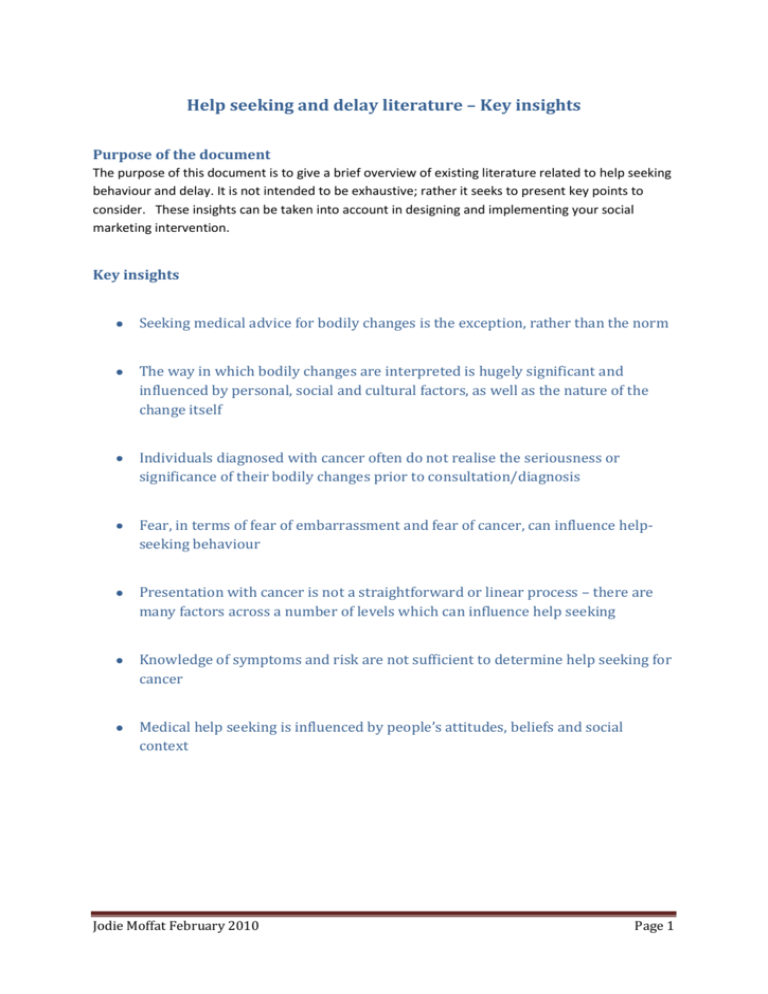
Help seeking and delay literature – Key insights Purpose of the document The purpose of this document is to give a brief overview of existing literature related to help seeking behaviour and delay. It is not intended to be exhaustive; rather it seeks to present key points to consider. These insights can be taken into account in designing and implementing your social marketing intervention. Key insights Seeking medical advice for bodily changes is the exception, rather than the norm The way in which bodily changes are interpreted is hugely significant and influenced by personal, social and cultural factors, as well as the nature of the change itself Individuals diagnosed with cancer often do not realise the seriousness or significance of their bodily changes prior to consultation/diagnosis Fear, in terms of fear of embarrassment and fear of cancer, can influence helpseeking behaviour Presentation with cancer is not a straightforward or linear process – there are many factors across a number of levels which can influence help seeking Knowledge of symptoms and risk are not sufficient to determine help seeking for cancer Medical help seeking is influenced by people’s attitudes, beliefs and social context Jodie Moffat February 2010 Page 1 Background / Detail The health service and the study of ‘illness behaviour’ When the National Health Service was first established in 1948, it was based on the assumption that people would know when they were ill and in need of medical attention, and would seek help/use the service accordingly (Calnan, 1987; Hardey, 1998). However, it soon became clear, when people who didn't need medical advice sought it, and when people who did need medical advice didn't, that it's a very complex picture and people don't necessarily behave how you would want or expect them to. Recognition of this helped to pave the way for study into what is broadly known as 'illness behaviour' - essentially, how people recognise, interpret and respond to bodily changes (Mechanic, 1979). Of key interest in the study of illness behaviour are evaluation or interpretation of bodily changes and decisions about the most appropriate course of action (Morgan, 2003). Researchers have been investigating these areas for decades and much valuable insight has been gained. Interpreting ‘bodily changes’ The process of recognising a bodily change is not straightforward. People aren’t automatically alerted when something has changed – whether and when they notice that something is different depends on attentional and interpretive processes (Cioffi, 1991; Gijsbers van Wijk and Kolk, 1997). So if a person has competing priorities, it may take them longer to realise that something has changed because they are not focused on, or thinking about, their body. In much the same way, when individuals have recognised a change, they don’t automatically know what it means or understand its significance – they have to bring meaning to it through a process of interpretation. Through this process an individual may link their bodily change to disease, in which case it becomes a symptom, or associate it with something entirely normal or benign. Lots of different factors can impact on how a bodily change is interpreted; it depends on the nature of the change itself, as well as personal, social and cultural factors. As Alan Radley writes, ‘there are cultural expectations about which bodily disturbances require medical attention and which ones are ‘normal’’ (1994, p83). An interpretation is not fixed, so if the bodily change worsens or another one develops, the interpretation can be revised. People often look to other people to help them work out what their bodily changes might mean and how they could/should respond – this has been referred to as the ‘lay referral network’ (Radley, 1994). Different people will use their friends and relatives in different ways and to different extents – it’s been shown to vary with age, gender and social class (Radley, 1994). The way in which an individual interprets their bodily change is important for how they act on it. Even if an individual interprets their bodily change as a symptom, there are many things they might do other than consult the doctor, for example, do nothing, decide to ‘wait and see’ or self-medicate. Indeed, research has found that people experience bodily changes on a very regular basis, but only a small proportion of these will ever be brought to the attention of health services. This is commonly referred to as the illness or clinical iceberg (Wadsworth et al, 1971; Scambler and Scambler, 1984; Jodie Moffat February 2010 Page 2 Rogers et al, 1999). So, not seeking advice for a bodily change is the norm, rather than the exception. Help seeking Coming from the position that not seeking advice is the norm, rather than the exception, the question is not ‘Why did the person delay?’ but ‘Why go now?’. Working from this thesis, Zola 1973) has suggested that people don’t seek help at their sickest point, but when they can no longer accommodate the changes they are experiencing, and has suggested five ‘triggers’ for help-seeking: 1) Occurrence of an interpersonal crisis, such as death of a relative, which may call attention to a person’s bodily changes and prompt them to do something about them 2) Perceived interference with social or personal relations – a bodily change interferes with friendships, relationships and everyday living, prompting action 3) Sanctioning – family, friends or significant others agree that help-seeking is needed/justified 4) Perceived interference with vocational or physical activity – changes stop someone carrying out their job or other physically demanding activity 5) A kind of temporalizing of symptomatology – people place a time limit on their changes, and consult if they haven’t resolved by that time, for example “I’ll go to the doctor if this cough is still here in a couple of weeks” (Zola 1973; Earle, 2007). David Mechanic’s insights on illness behaviour feature widely in the literature, as do Zola’s triggers. The insights are useful, not least because they highlight the range of different factors which can influence both interpretation and help-seeking: 1) Visibility, recognizability, or perceptual salience of deviant signs and symptoms 2) The extent to which the symptoms are perceived as serious 3) The extent to which symptoms disrupt family, work, and other social activities 4) The frequency of the appearance of the deviant signs or symptoms, their persistence, or their frequency of recurrence 5) The tolerance threshold of those who are exposed to and evaluate the deviant signs and symptoms 6) Available information, knowledge, and cultural assumptions and understandings of the evaluator – knowledge about, and understanding of, what bodily changes may mean 7) Basic needs which lead to autistic psychological processes – anxiety about the perceived seriousness 8) Needs competing with illness responses – competing needs and priorities 9) Competing possible interpretations that can be assigned to the symptoms once they are recognized Jodie Moffat February 2010 Page 3 10) Availability of treatment resources, physical proximity, and psychological and monetary costs of taking action (Mechanic, 1968; Earle, 2007). ‘Delay’ and cancer ‘Delay’ has been investigated in relation to many disease types, but arguably the largest amount of enquiry is in the field of cancer. As early as 1938, a paper was published titled ‘The culpability for delay in the treatment of cancer’ (Pack and Gallo, 1938). Since this time, there has been a great deal of interest in ‘patient delay’ and cancer (see Andersen et al, 2009 for an interesting discussion). Some of the studies have been descriptive observational studies, often relying on examination of medical records or questionnaires, to assess the extent of ‘delay’ for particular cancer types. Others have sought to establish factors associated with delay and have highlighted the importance of individuals not realising the seriousness or significance of (Ramirez et al, 1999; Macdonald et al, 2004; Macleod et al, 2009). Studies have also drawn upon qualitative methods to explore help-seeking and delay with individuals diagnosed with cancer. Smith and colleagues (Smith et al, 2005) have brought together many of these studies in a qualitative synthesis. The analysis of 32 papers across more than 20 different cancer types, highlighted key similarities irrespective of cancer site and country. The main themes associated with delay in presentation were Recognition and interpretation of symptoms Fear of consultation (with respect to embarrassment and to the idea of cancer itself). The patient’s gender and the sanctioning of help-seeking also affected help-seeking (Smith et al, 2005). It’s helpful to realise that there are many factors across a number of different levels which can influence help-seeking behaviour, just as there are many which influence interpretation. As Una Macleod and colleagues write, ‘Overall, research into the risk factors for patient delay indicates that presentation with cancer is not a straightforward or linear process. Knowledge of symptoms and risk may be necessary, but not sufficient to determine help seeking for cancer. People’s attitudes, beliefs and social context clearly influence the process of medical help seeking’ (Macleod et al, 2009, pS98). References Andersen, RS., Vedsted, P., Olesen, F., Bro, F., Sondergaard, J (2009) Patient delay in cancer studies: a discussion of methods and measures. BMC Health Services Research 9:189 doi:10.1186/1472-69639-189 Armstrong, A (2003) Outline of Sociology as Applied to Medicine (5th Edition). London: Arnold Calnan, M (1987) Health and Illness The Lay Perspective. London: Tavistock Publications Jodie Moffat February 2010 Page 4 Cioffi, D. (1991) Beyond attentional strategies: A cognitive-perceptual model of somatic interpretation. Psychological Bulletin 109 (1) 25-41 Earle, S (2007) Exploring health, In Earle, S., Lloyd, CE., Sidell, M., Spurr, S (Editors) Theory and research in promoting public health. Milton Keynes: The Open University Gijsbers van Wijk, C.M.T., Kolk, A.M. (1997) Sex differences in physical symptoms: the contribution of symptom perception theory. Social Science and Medicine 45 (2) 231-246 Hardey, M (1998) The Social Context of Health. Buckingham: Open University Press Macdonald, S, Macleod, U, Mitchell, E, Weller, D, Campbell, N, Mant, D (2004) Factors influencing patient and primary care delay in the diagnosis of cancer: A database of existing research and its implications for future practice. Report to the Department of Health Macleod, U., Mitchell, ED., Burgess, C., Macdonald, S., Ramirez, AJ (2009) Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. British Journal of Cancer 101:S92-101 Mechanic, D (1968) Medical Sociology: A Selective Review. New York: The Free Press Mechanic, D. (1979) Future Issues in Health Care. Social Policy and the Rationing of Medical Services. New York: The Free Press Morgan, M (2003) Patients’ help-seeking and access to health care, In Gulliford, M., Morgan, M (Editors) Access to Health Care. London: Routledge Pack, GT, Gallo, JS (1938) The culpability for delay in the treatment of cancer. American Journal of Cancer 33:443-462 Radley, A (1994) Making Sense of Illness The Social Psychology of Health and Disease. London: Sage Publications Ramirez, AJ, Westcombe, AM, Byrgess, CC, Sutton, S, Littlejohns, P, Richards, MA (1999) Factors predicting delayed presentation of symptomatic breast cancer: A systematic review. Lancet 353:1127-1131 Rogers, A., Hassell, K., Nicolaas, G (1999) Demanding Patients? Analysing the Use of Primary Care. Buckingham: Open University Press Scambler, G, Scambler, A (1984) The illness iceberg and aspects of consulting behaviour, In Fitzpatrick, R, Hinton, J, Newman, S, Scambler, G. Thompson, J (Editors) The Experience of Illness. London: Tavistock Publications, pp32-53 Smith, LK, Pope, C, Botha, JL (2005) Patients’ help-seeking experiences and delay in cancer presentation: A qualitative synthesis. Lancet 366:825-831 Wadsworth, MEJ, Butterfield, WJH, Blaney, R (1971) Health and Sickness The Choice of Treatment. London: Tavistock Publications Zola, IK (1973) Pathways to the doctor – from person to patient. Social Science and Medicine 7:677689 Jodie Moffat February 2010 Page 5