FEMALE GENITAL ORGANS
advertisement

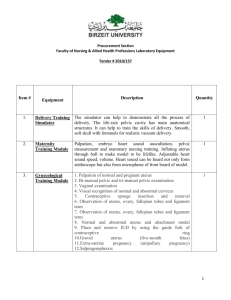
FEMALE GENITAL ORGANS are divided into • internal: ovaries uterine tubes uterus vagina • external: mons pubis labia majora labia minora vestibule of vagina clitoris bulbus vestibuli greater vestibular glands INTERNAL FEMALE GENITAL ORGANS OVARY - is a reproductive organ and endocrine gland - is located in the pelvic cavity - it is applied on the lateral pelvic wall - placed in the ovarian fossa – in front of the ureter displaced during and after pregnancy Ovary is attached to the posterior surface of the broad ligament of uterus - it is ovoid in shape, flattened, mesuring 3x 1,5x 1 cm -it has smooth surface before puberty, but uneven surface in adult (marked by growing follicles) ovoid in shape, ovary has surfaces, borders, extremities • surfaces: lateral surface – is oriented to the lateral pelvic wall medial surface – is partly covered with the uterine tube and is in contact with: ileum and appendix - right ovary sigmoid colon - left ovary • borders: free border mesovarian border – this is attached to the broad ligament by the mesovarium – contains vessels, nerves and embryonic remains (epoophoron, paroophoron) • extremities: tubal extremity - is oriented superiorly - it is covered with the fimbriae of uterine tube suspensory ligament ascends from it upwards (contains ovarian vessels!!) uterine extremity - is oriented inferiorly - is attached to uterus by ligament of the ovary 71 THE STRUCTURE OF THE OVARY The surface of ovary is covered by germinal epithelium - transition between it and the peritoneum is marked by white line around the mesovarian border tunica albuginea lies beneath the germinal epithelium cortex contains ovarian follicles and corpora lutea embedded in the connective tissue medulla - is a richly vascular connective tissue deep to the cortex Blood supply: ovarian a. (arises from the abdominal aorta!) Nerve supply: ovarian plexus (containing PS fibres from the vagus) Lymph drainage: lumbar lymph nodes UTERINE TUBE (FALOPIAN TUBE) transmits ova from the ovary to the uterus fertilisation occurs in the tube - it is located in free border of the broad ligament of the uterus - it is 10 – 15 cm long one end opens into the uterus – uterine opening opposite end opens into the pelvic part of the peritoneal cavity – abdominal opening Relations: Right tube- ileum, appendix Left tube - sigmoid colon uterine tube is subdivided into: • infundibulum • ampulla • isthmus • uterine part ● Infundibulum - is funnel shaped expansion of the abdominal end - the circumference of it is marked by fimbriae which are loosely applied on the ovarian surface ovarian fimbria – the longest of all, is firmly attached to the ovary ● Ampulla - is thin-walled, tortuous, forms more than 1/2 of entire lenght of tube ● Isthmus - is narrow, round, cord like, constitutes medial 1/3 of tube ● Uterine part - is the narrowest, short part traversing the uterine wall STRUCTURE the wall of uterine tube is composed of: mucous coat – lines interior, folded into numerous folds muscular coat serous coat – peritoneum 72 Blood supply: tubal branches of ovarian and uterine arteries Nerve supply: pelvic autonomic plexus Lymph drainage: lumbar lymph nodes UTERUS - is situated in the pelvic cavity - connected to the lateral pelvic walls by a peritoneal fold – broad ligament - it is placed between the urinary bladder and the rectum separated from them by the vesicouterine and the rectouterine pouches Uterus is pear shaped, flattened anteroposteriorly - its position varies with the state of bladder and rectum Uterus forms almost a right angle with the vagina – - uterus is anteverted uterus is subdivided into: • body • isthmus • cervix ● Body is wider superiorly, narrower inferiorly has parts: fundus, surfaces, margins, horns ∗ fundus is upper wider convex part ∗ surfaces: - vesical surface – directed to the urinary bladder, covered with the peritoneum, separated from the bladder by the vesicouterine pouch - intestinal surface – directed upwards and backwards - covered with the peritoneum related to: coils of ileum sigmoid colon rectum - separated from the rectum by the rectouterine pouch surfaces meet in ∗ margins – the broad ligament joins the margins to the lateral pelvic walls margins and fundus meet in ∗ horns – here uterine tubes enter the uterus Below the horns ligaments are attached: - the round ligament (anteriorly) - the ligament of ovary (posteriorly) - body meets with the cervix in ● the isthmus ● the cervix is lower narrower part of the uterus - the cervix is less movable than the body (it is more fixed to the pelvic walls by ligaments) - its axis forms with the axis of the body an angle opened anteriorly 73 so that uterus is anteflexed cervix is divided by attachment of the vagina into upper – supravaginal portion and lower – vaginal portion – this projects into the vagina and is encircled by circular space – vaginal fornix vaginal portion of cervix shows ostium of cervical canal - ostium of uterus - round in shape in nuliparous woman - transverse slit – shaped in parous woman here bordered by anterior and posterior lips THE INTERIOR OF THE UTERUS cavity of the body is flattened anteroposteriorly, triangular uterine tubes open into it in the horns the cavity is continuous inferiorly into the canal of the cervix - fusiform in shape inner surface is folded into the palmate folds THE UTERINE WALL is composed of mucous, muscular and serous coats - mucous coat – endometrium contains uterine glands which undergo regular monthly changes - menstrual cycle - muscular coat – myometrium is composed of smooth muscles - external layer – longitudinal fibres - are continued into the ligaments of uterus (broad, round, sacrouterine and ligament of ovary) - middle and - internal layers – muscle fibres are arranged in all directions (longitudinally, circularly, obliquely) - serous coat – perimetrium is derived from the peritoneum LIGAMENTS OF THE UTERUS - PARAMETRIUM uterus is connected to the pelvic walls and neighbouring organs by a numbre of ligaments 1. to the lateral pelvic wall by: BROAD LIGAMENT – this is a peritoneal fold containing suspensory lig. of ovary (contains ovarian vessels) ligament of ovary round ligament of uterus = ligamentum teres – runs from the uterine horn to the labium majus TRENSVERSE LIGAMENT = ligamentum cardinale - is placed in the lower part of the broad ligament - extends from the cervix to the lateral pelvic walls 2. to the bladder and pubis by: vesicouterine lig. pubovesical lig. 74 3. to the rectum and sacrum by: rectouterine lig. sacrouterine lig. Blood supply: uterine a. Nerve supply: pelvic autonomic plexus Lymph drainage:internal iliac lumbar and inguinal lymph nodes (along the round ligament of the uterus) VAGINA extends from the uterus to the vestibule – here it opens as vaginal orifice (situated behind the ext. uretral orifice) vagina is situated behind the bladder and urethra in front of the rectum it is directed down and anteriorly (in right angle with the uterus – anteversion of the uterus) Vagina is flattened anteroposteriorly - it has anterior and posterior walls - anterior wall is shorter than the posterior wall - upper part of vagina surrounds vaginal portion of the cervix to form vaginal fornix subdivided into ∗ the anterior fornix ∗ the posterior fornix (deeper) – this is covered with the peritoneum separated from rectum by the rectouterine pouch lower part of vaginal wall is connected to the rectum by fibroareolar tissue – rectovaginal septum – this is thickened inferiorly into the perineal body VAGINAL WALL consists of: - mucous membrane – folded on the ant. and post. walls into the transverse ridges – rugae which form columns of vagina (columnae rugarum) - muscular coat – external longitudinal and internal circular - external layer of areolar tissue – connects vagina to bladder, urethra and rectum - contains large plexuss of veins Blood supply: vaginal branches from the uterine middle rectal and internal pudendal arteries Nerve supply: pelvic autonomic plexus and Pudendal n. Lymph drainage: internal iliac and inguinal lymph nodes EXTERNAL FEMALE GENITAL ORGANS MONS PUBIS is a cutaneous eminence in front of pubic symphysis composed of fatty tissue beneath the skin at puberty – skin is covered with the hairs 75 LABIA MAJORA are two cutaneous folds containing fatty tissue - extend from the mons to the perineal region labia majora border pudendal cleft and meet in anterior commissure and posterior commissure outer surface of labia majora is pigmented and covered with hairs! inner surface of labia majora contains sebaceous glands round ligament of uterus terminates in the labium majus LABIA MINORA are small cutaneous folds placed medially to the labia majora - contain no fat! anteriorly labia are divided into two portions to form: the prepuce of clitoris and the frenulum of clitoris posteriorly labia meet in frenulum of labia minora the skin of labia minora contains sebaceous glands labia minora border the vestibule VESTIBULE is a space between the labia minora lined with the mucosa containing minor vestibular glands ∗ external urethral orifice and ∗ vaginal orifice open into the vestibule vaginal orifice in virgin is partly enclosed by mucous fold – hymen ext. urethral orifice lies in front of the vaginal orifice!! CLITORIS It is a homologue of the penis is an erectile structure between the labia minora anteriorly is composed of: crura of clitoris – are attached to pubis covered with the ischiocavernosus m. crura join to form body of clitoris which terminates as glans of clitoris – this is covered with the prepuce of clitoris BULB OF VESTIBULE is homologous with the bulb of the penis it is composed of two elongated masses of erectile tissue - placed in the depths of the labia majora on sides of vaginal vestibule - covered with the bulbospongiosus m. the bulb is rounded posteriorly and narrowed anteriorly – here bulbs are fused to form commissure of bulbs GREATER VESTIBULAR GLANDS (of Bartholini) are two in numbre, homologous with the bulbourethral glands in male each gland is placed on the outer surface of urogenital diaphragm, near the dorsal part of the bulb of vestibule the duct of gland opens into the vestibule near the vaginal orifice 76 Blood supply of external genital: internal and external pudendal vessels Nerve supply: mainly Pudendal n. Lymph drainage: inguinal lymph nodes THE BREASTS exist in both sexes in male – rudimentary in female – rudimentary before puberty - undergoes considerable development at puberty - greatest development – during the pregnancy and lactation the shape and size depends upon many factors – genetic, age, parity… - located in the pectoral region extends from the 2nd to the 6th ribs from the parasternal to near mid-axillary lines - axillary tail projects into the axillary fossa (towards pectoral lymph nodes) - gland lies within the superficial fascia on the pectoralis major m. and pectoral fascia separated from it by retromammary space – filled with areolar tissue – retromammary fat the nipple – cylindrical eminence near the centre of the breast pink or light brown contains smooth muscle fibres - circular - erection - longitudinal - retraction of the nipple lactiferous ducts traverse the nipple, open on the summit areola - surrounds the nipple - becomes enlarged and darker in colour during the pregnancy and lactation skin of areola – sebaceous areolar glands – protective lubricant for the skin of the nipple during lactation Inner structure: 15 – 20 lobes composed of lobules lobes arranged radially lobules and lobes are connected by areolar tissue - intramammary - praemammary (subcutaneous) - retromammary fat lactiferous ducts drain the lobes, converge radially towards the nipple lactiferous sinuses – dilatations of ducts near the areola 77 Blood supply: branches from - internal thoracic a. - intercostal a. - axillary - lateral thoracic a. and corresponding veins Nerves: 4th-6th intercostal nerves - ant. and lateral cutaneous branches Lymph drainage: lymph vessels accompany blood vessels - pectoral lymph nodes - parasternal lymph nodes (deep thoracic) - inferior deep cervical lymph nodes THE PELVIS the pelvic walls are formed by • bones and • muscles • Pelvic bones: pubis, ischium, body of ilium, sacrum, coccyx • MUSCLES OF THE PELVIS 1. muscles on the lateral and dorsal wall: - obturator internus m. - piriformis m. 2. muscles of the pelvic floor – THE PELVIC DIAPHRAGM - levator ani m. - coccygeus m. Levator ani m.: has two parts - pubococcygeus O: pubic bone - iliococcygeus O: obturator fascia ischial spine I: coccyx and median raphe = perineal body perineal body is lower thickened part of the rectovesical septum in male and rectovaginal septum in female Function: - supports the pelvic organs - sphincter ani externus m. is derived from it - and levator prostatae m., puborectalis m. NS: Pudendal n. Coccygeus m. O: ischial spine I: sacrum, coccyx F: helps levator ani to close the pelvic outlet 78 NS: sacral plexus FASCIAE OF THE PELVIS – PELVIC FASCIA fasciae of the muscles – parietal fascia fasciae of the pelvic organs – visceral fascia PERINEAL MUSCLES – UROGENITAL DIAPHRAGM - transversus perinei profundus O: ramus of ischium and pubis I: median raphe = perineal body sphincter urethrae externus is derived from it -transversus perinei superficialis O: ischial tuberosity I: perineal body - ischiocavernosus - bulbospongiosus NS: Pudendal n. F: - help to support pelvic organs fascie of perineal muscles form – PERINEAL FASCIAE ISCHIOANAL FOSSA (ISCHIORECTAL FOSSA) is a triangular space under the pelvic diaphragm borders: superiorly (and medially) : pelvic diaphragm (levator ani m.) laterally: ischium and pubis, obturator int. m. inferiorly: perineal fascia – in the dorsal part of space urogenital diaphragm – in the ventral part of space contains - areolar fatty tissue - Internal pudendal vessels, Pudendal n. 79