Smooth Muscle Cells: To Be or Not To Be?: Response to Nguyen et al
Zhenyu Tang, Aijun Wang, Dong Wang and Song Li
Circ Res. 2013;112:23-26; originally published online October 23, 2012;
doi: 10.1161/CIRCRESAHA.112.281055
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2012 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/112/1/23
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/
Downloaded from http://circres.ahajournals.org/ at CONS CALIFORNIA DIG LIB on August 26, 2013
Perspective
Smooth Muscle Cells: To Be or Not To Be?
Response to Nguyen et al
Zhenyu Tang, Aijun Wang, Dong Wang, Song Li
T
he conversion of contractile vascular smooth muscle
cells (SMCs) to a synthetic or proliferative phenotype
is thought to play a major role in vascular diseases, such as
atherosclerosis and restenosis.1–3 Our recent work presents evidence that challenges this widely accepted dogma. Our findings suggest that multipotent vascular stem cells (MVSCs) are
a major contributor to vascular remodeling.4 The experimental
results demonstrate that the major population of the traditionally defined proliferative/synthetic SMCs is derived from the
differentiation of MVSCs rather than the dedifferentiation
of mature SMCs. Both in vitro and in vivo results suggest
that vascular disease is a stem cell disease, which raises the
question on the previous dogma: Is vascular disease a SMC
disease?
In this issue of Circulation Research, a group of leaders in
the area of SMC biology wrote a commentary on this work.5
They present evidence in the literature that seems to support
the SMC dedifferentiation hypothesis. However, in many previous studies, it was incorrectly assumed that the vascular
cells in the primary culture and in injured blood vessels were
mostly derived from SMCs. Thus, the previous experimental findings on vascular cells were often attributed to SMCs,
which resulted in data misinterpretation and the overstatement on SMC functions. We agree that further investigations
are needed to determine the relative contribution of MVSCs
and SMCs to vascular remodeling in various animal models;
­however, we respectfully disagree on some of the arguments
in the commentary.
Vascular SMC biology has been studied in vitro and in vivo
extensively in the past 50 years since the method for SMC culture was established. The concept of phenotypic modulation
of SMCs was originated from the ultrastructural characterization of SMC culture in 1960s to 1970s, which has been summarized in the comprehensive review by Chamley-Campbell
et al.6 The contractile SMCs are characterized by the cytoplasm largely filled with thick and thin myofilaments, whereas
synthetic SMCs have few myofilaments but have large amount
of rough endoplasmic reticulum, free ribosomes, and Golgi
The opinions expressed in this article are not necessarily those of the
editors or of the American Heart Association.
From the Department of Bioengineering, University of California,
Berkeley, CA (Z.T., D.W., S.L.); Department of Surgery, UC Davis
Medical Center, University of California, Davis, Sacramento, CA (A.W.);
and SARI Center for Stem Cell and Nanomedicine, Shanghai Advanced
Research Institute, Chinese Academy of Science, Shanghai, China (Z.T.).
Correspondence to Song Li, Department of Bioengineering, University
of California, Berkeley, CA 94720. E-mail song_li@berkeley.edu
(Circ Res. 2013;112:23-26.)
© 2012 American Heart Association, Inc
Circulation Research is available at http://circres.ahajournals.org
DOI: 10.1161/CIRCRESAHA.112.281055
complexes.6 A correlative conclusion suggests that the phenotypic modulated SMCs, which barely grow in the first week
of the primary culture, account for a sudden cell expansion
afterward and that these expanded cells can undergo redifferentiation under the same culture condition. These expanded
cells are traditionally characterized as proliferative/synthetic
SMCs, assuming that they are derived from mature SMCs. As
shown later by numerous studies, this expanded cell population expresses the markers of immature SMCs, such as smooth
muscle α-actin (SMA), calponin-1, and SM-22α, which seems
to support the conclusion. However, to date, there is no direct
evidence (eg, by using rigorous lineage tracing) to show that
these fast growing cells are indeed derived from mature SMCs.
Thus, it is not unreasonable to ask the following questions:
Can the phenotypically modulated SMCs grow fast enough to
account for the cell expansion in SMC primary culture? Is it
possible that the fast growing cells are derived from a minority
population of stem cells in SMC culture?
Indeed, our data provide a reasonable explanation: the fast
expansion of SMCs after the first week of in vitro culture may
be mainly attributed to the expansion of a minority population
of cells (ie, MVSCs), and MVSCs can spontaneously differentiate into proliferative/synthetic SMCs. In addition, the lineage tracing experiments using smooth muscle myosin heavy
chain (SM-MHC) as a marker suggest that these proliferative/
synthetic SMCs indeed are not derived from mature SMCs.4
Therefore, although our data interpretation and conclusion are
different from the previous theory, the experimental data in
the classical studies do not contradict our findings. Our findings imply that SMCs in many previous in vitro studies may
be derived from MVSCs. Indeed, as exemplified in Figure 1, a
commercially available human aortic SMC line expresses low
level of Sox10, an MVSC marker, suggesting that these cells
are likely derived from MVSCs. In contrast, human MVSCs
of primary culture have high level of Sox10 expression and
low level of SMA that is not incorporated into stress fibers.
There are >40 000 articles on vascular SMCs. If the proliferative/synthetic SMCs may be derived from MVSCs, many
previous conclusions on SMCs may need to be revisited.
Do phenotypically modulated SMCs grow as fast as
previously thought? In the primary culture of SMCs, mitotic
bodies were observed in phenotypically modulated SMCs but
were not commonly found in mature SMCs.6,7 Consistently,
we did not find proliferative cells in SM-MHC+ population
in the primary culture, but we did observe a small percentage
of newly differentiated SM-MHC+ cells in the cell cycle.4
However, by using SM-MHC as a marker for lineage tracing,
we showed that SMCs in the primary culture did not expand
as much as expected and that MVSCs outgrew SMCs and
became proliferative/synthetic SMCs,4 suggesting that
Downloaded from http://circres.ahajournals.org/ at 23
CONS CALIFORNIA DIG LIB on August 26, 2013
24 Circulation Research January 4, 2013
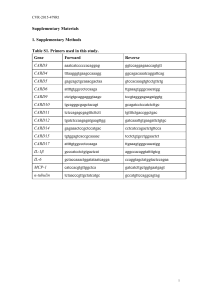
Figure 2. The distribution and dynamics of multipotent
vascular stem cells (MVSCs) in a mouse descending thoracic
aorta. Sox10 was used for the lineage tracing of MVSCs.
The descending thoracic aorta was isolated from Sox10-Cre/
Rosa26-loxP-tdTomato mouse, cut into small rings, and cultured
ex vivo. A, The cross section of the aorta ring was imaged by
2-photon fluorescence microscopy. Sox10+ cells (in red) were
found in both medial and adventitial layers (indicated by arrows).
B, The same sample was imaged 3 days later, showing the
multiplication of existing Sox10+ cells (indicated by arrows) and
the appearance and activation of a Sox10+ cell (indicated by an
arrowhead).
Figure 1. The expression of Sox10 and smooth muscle αactin (SMA) in human aortic smooth muscle cells (SMCs)
and human aortic multipotent vascular stem cells (MVSCs).
Human aortic SMCs (A–D) were obtained from a commercial
source. Human aorta MVSCs were isolated from the medial layer
of a human aorta (E–H). The cells were immunostained with
antibodies against Sox10 (A, E) or SMA (B, F). Nuclei were
stained by diamidino-2-phenylindole (DAPI) (C, G).
MVSC expansion dominates over SMC multiplication. SMC
multiplication, if any, may be a much slower process compared
with MVSC expansion. Because our study is the only report
on the tracing of SMC fate in culture, further studies are being
performed in several laboratories with different transgenic
mouse lines to verify the results.
As discussed in the commentary, there are numerous studies showing proliferative cells in neointima.7–10 However,
these studies did not directly show that proliferative cells were
derived from mature SMCs and therefore cannot exclude the
involvement of MVSCs and other cell types. Nevertheless,
SMCs do show changes in gene expression after injury.11
Figure 2 in the commentary5 provides evidence that SMCs
can indeed replicate DNA and get into S phase in vivo after
ligation or wire injury. Figure 2A5 is the only lineage tracing
data in the literature showing that SMCs or SMC-derived cells
can proliferate in vivo, although the diffused β-gal staining
throughout the vascular wall (including matrix) is questionable. It is noted that the SMCs appear to be the only cell type
in the injured arteries,5 which is contradictory to the previous reports that the cells from diverse origins, including bone
marrow,12,13 circulation,14 and adventitia15–17 besides the medial
layer of blood vessel wall, are also involved in the vascular
remodeling after the injury. In contrast, in our animal model,
after wire injury, extensive SMC death was observed within
2 days, and we did not observe proliferative SM-MHC+ cells.
In some regions of injured vessel, all cells in the vessel wall
were replaced by MVSC-derived cells within a week.4 One
explanation for the discrepancy between the data shown in the
commentary5 and ours is that the extent of injury in the arteries was different. As we pointed out, “the extent of MVSC activation, proliferation, and differentiation could be dependent
on the extent of vascular injury and SMC damage.”4 We agree
that a less severe injury could allow the investigation of how
SMCs contribute to neointima formation. Regarding SMC lineage tracing model, the tamoxifen-inducible SM-MHC-Cre
mouse line18 does have an advantage because it only traces
existing SMCs but not newly differentiated SMCs.
Can SMCs dedifferentiate? Although the phenotype of
SMCs could be modulated, there is no direct evidence suggesting that SMCs can dedifferentiate and return to a multipotent state, which was noted 30 years ago6 and is still the
case to date. In many previous studies, the conclusion on the
phenotypic modulation of SMCs in vivo was mostly based on
the assumption that the cells in injured arteries were derived
from mature SMCs, which is not necessarily true. As cited
in the commentary, one of the classical studies showed that,
after artery ligation, the cells in the neointima had synthetic
phenotype and differed from SMCs in ultrastructure, which
was assumed to be dedifferentiated SMCs without rigorous
cell tracing.19 Similarly, the loss of the expression of SMC
markers, such as SMA, SM-22α, and SM-MHC, in response
to injury was attributed to the silence of these genes in SMCs
in many previous studies.20 It is intriguing that SMA and
SM22α, the 2 immature SMC markers downregulated but
not completely silenced in proliferative/synthetic SMCs, are
not expressed in the vascular cells after the injury.20 Is it possible that the cells in the neointima arise from other vascular
Downloaded from http://circres.ahajournals.org/ at CONS CALIFORNIA DIG LIB on August 26, 2013
Tang et al Smooth Muscle Cells 25
cells such as MVSCs? In another study, SM-22α was used
as the lineage tracing marker to show that SMCs contribute
to the chondrogenic and osteogenic remodeling of arteries.21
However, SM-22α is also expressed in many other types of
cells in blood vessels, including adventitia myofibroblasts,22,23
activated macrophages,24 and MVSC-derived cells.4 Therefore,
the lineage tracing using SM22α as a marker cannot specifically trace mature SMCs, thus compromising the conclusion
on SMC dedifferentiation. As recently reviewed by Gomez
and Owens,25 there is a lack of studies that directly trace the
fate of mature SMCs.
Where are MVSCs located? Indeed it is impossible to isolate cells only from the medial or adventitial layer without
the contamination of cell type from the other layer, especially
in rat and mouse vascular tissues. Therefore, the cell isolation method is not accurate to define the origin and location
of MVSCs in the rodent models and may lead to misinterpretation. Recently, we were able to isolate MVSCs from human blood vessels in which the medial and adventitial layers
can be separated, and we found that MVSCs could be isolated from both media and adventitia. In addition, we have
used Sox10 as a marker to identify and trace MVSCs in mouse
blood vessels with a higher spatial resolution. As shown in
Figure 2, MVSCs are present in both the medial layer and the
adventitial layer of mouse thoracic aorta, and MVSC multiplication and activation (emergence of Sox10+ cells) can be
observed with ex vivo 2-photon time-lapse microscopy. This
ex vivo model provides a valuable tool to further investigate
the dynamics of MVSCs and SMCs in injured blood vessels.
In addition, the commentary also raises the question on the
relationship of MVSCs with previously identified vascular
progenitors. As we reported previously,4 MVSCs are negative
for Sca-1, Sox2, c-kit, and CD146 and are different from other
vascular progenitors, such as Sca-1+ cells,26,27 CD44+/CD29+/
Sox2+/Oct4+ cells,28 and CD146+ pericytes,29 in the aspects of
marker expression and multipotency. Whether these markers
may be expressed in MVSCs under in vitro and in vivo conditions needs close examination. It seems that MVSCs are a major contributor of proliferative/synthetic SMCs in vitro. The
relative contribution of MVSCs and other vascular progenitors to vascular diseases needs further investigation.
In summary, we provided compelling evidence that MVSCs
can be activated on vascular injury and that the rapid expansion and the aberrant differentiation of MVSCs contribute to
neointima formation. However, the relative contribution and
importance of vascular stem cells and SMCs need further investigation. The findings on MVSCs provide a new perspective on vascular biology and may lead to the development of
new therapies for vascular diseases. Nevertheless, besides the
possibility of SMC de-differentiation, SMCs may play a role
in mediating inflammatory responses and cell-cell signaling.
We hope that this debate will promote the research to further
elucidate the roles of MVSCs and SMCs in vascular remodeling and address this fundamental issue: Is vascular disease a
stem cell disease or SMC disease, or both?
Sources of Funding
This work was supported, in part, by the grants from National Institute
of Health (EB012240 to S. Li), California Institute for Regenerative
Medicine (RB3-05232 to S. Li and TG2-01164 fellowship to Z.
Tang), the Telemedicine and Advanced Technology Research Center
(TATRC) at the US Army Medical Research and Materiel Command
(USAMRMC) (W81XWH-11-1-0791 to S. Li), and Siebel Stem Cell
Institute (to D. Wang).
Disclosures
None.
References
1.Ross R. Atherosclerosis is an inflammatory disease. Am Heart J.
1999;138:S419–S420.
2. Alexander MR, Owens GK. Epigenetic control of smooth muscle cell
differentiation and phenotypic switching in vascular development and
disease. Annu Rev Physiol. 2012;74:13–40.
3. Libby P, Ridker PM, Hansson GK. Progress and challenges in translating
the biology of atherosclerosis. Nature. 2011;473:317–325.
4.Tang Z, Wang A, Yuan F, Yan Z, Liu B, Chu JS, Helms JA, Li S.
Differentiation of multipotent vascular stem cells contributes to vascular
diseases. Nat Commun. 2012;3:875.
5. Nguyen AT, Bell RD, Campbell JH, et al. Smooth muscle cell plasticity:
fact or fiction? Circ Res. October 23, 2012. doi:10.1161/CIRCRESAHA.
112.281048. http://circres.ahajournals.org/content/­early/2012/10/23/
CIRCRESAHA.112.281048.long. Accessed December 21, 2012.
6. Chamley-Campbell J, Campbell GR, Ross R. The smooth muscle cell in
culture. Physiol Rev. 1979;59:1–61.
7. Clowes AW, Schwartz SM. Significance of quiescent smooth muscle migration in the injured rat carotid artery. Circ Res. 1985;56:139–145.
8. Thomas WA, Florentin RA, Reiner JM, Lee WM, Lee KT. Alterations
in population dynamics of arterial smooth muscle cells during atherogenesis. IV. Evidence for a polyclonal origin of hypercholesterolemic
diet-induced atherosclerotic lesions in young swine. Exp Mol Pathol.
1976;24:244–260.
9. Clowes AW, Reidy MA, Clowes MM. Kinetics of cellular proliferation
after arterial injury. I. Smooth muscle growth in the absence of endothelium. Lab Invest. 1983;49:327–333.
10. Goldberg ID, Stemerman MB, Schnipper LE, Ransil BJ, Crooks GW,
Fuhro RL. Vascular smooth muscle cell kinetics: a new assay for studying patterns of cellular proliferation in vivo. Science. 1979;205:920–922.
11. Miano JM, Vlasic N, Tota RR, Stemerman MB. Localization of Fos and
Jun proteins in rat aortic smooth muscle cells after vascular injury. Am J
Pathol. 1993;142:715–724.
12. Yajima N, Takahashi M, Morimoto H, Shiba Y, Takahashi Y, Masumoto
J, Ise H, Sagara J, Nakayama J, Taniguchi S, Ikeda U. Critical role of
bone marrow apoptosis-associated speck-like protein, an inflammasome
adaptor molecule, in neointimal formation after vascular injury in mice.
Circulation. 2008;117:3079–3087.
13. Tanaka K, Sata M, Hirata Y, Nagai R. Diverse contribution of bone marrow cells to neointimal hyperplasia after mechanical vascular injuries.
Circ Res. 2003;93:783–790
14. Tanaka K, Sata M, Natori T, Kim-Kaneyama JR, Nose K, Shibanuma M,
Hirata Y, Nagai R. Circulating progenitor cells contribute to neointimal
formation in nonirradiated chimeric mice. FASEB J. 2008;22:428–436.
15. Zalewski A, Shi Y, Johnson AG. Diverse origin of intimal cells: smooth
muscle cells, myofibroblasts, fibroblasts, and beyond? Circ Res.
2002;91:652–655.
16.Sartore S, Chiavegato A, Faggin E, Franch R, Puato M, Ausoni S,
Pauletto P. Contribution of adventitial fibroblasts to neointima formation
and vascular remodeling: from innocent bystander to active participant.
Circ Res. 2001;89:1111–1121.
17. Li G, Chen SJ, Oparil S, Chen YF, Thompson JA. Direct in vivo evidence
demonstrating neointimal migration of adventitial fibroblasts after balloon injury of rat carotid arteries. Circulation. 2000;101:1362–1365.
18.Nemenoff RA, Horita H, Ostriker AC, Furgeson SB, Simpson PA,
VanPutten V, Crossno J, Offermanns S, Weiser-Evans MC. SDF-1α
induction in mature smooth muscle cells by inactivation of PTEN is a
critical mediator of exacerbated injury-induced neointima formation.
Arterioscler Thromb Vasc Biol. 2011;31:1300–1308.
Downloaded from http://circres.ahajournals.org/ at CONS CALIFORNIA DIG LIB on August 26, 2013
26 Circulation Research January 4, 2013
19. Buck R. Intimal thickening after ligature of arteries an electron-microscopic study. Circulation.research. 1961;9:418–426
20. Regan CP, Adam PJ, Madsen CS, Owens GK. Molecular mechanisms of
decreased smooth muscle differentiation marker expression after vascular injury. J Clin Invest. 2000;106:1139–1147.
21. Speer MY, Yang HY, Brabb T, Leaf E, Look A, Lin WL, Frutkin A,
Dichek D, Giachelli CM. Smooth muscle cells give rise to osteochondrogenic precursors and chondrocytes in calcifying arteries. Circ Res.
2009;104:733–741.
22. Faggin E, Puato M, Zardo L, Franch R, Millino C, Sarinella F, Pauletto
P, Sartore S, Chiavegato A. Smooth muscle-specific SM22 protein is expressed in the adventitial cells of balloon-injured rabbit carotid artery.
Arterioscler Thromb Vasc Biol. 1999;19:1393–1404.
23. Hinz B, Gabbiani G, Chaponnier C. The NH2-terminal peptide of alphasmooth muscle actin inhibits force generation by the myofibroblast in
vitro and in vivo. J Cell Biol. 2002;157:657–663.
24. Iwata H, Manabe I, Fujiu K, Yamamoto T, Takeda N, Eguchi K, Furuya
A, Kuro-o M, Sata M, Nagai R. Bone marrow-derived cells contribute to
vascular inflammation but do not differentiate into smooth muscle cell
lineages. Circulation. 2010;122:2048–2057.
25. Gomez D, Owens GK. Smooth muscle cell phenotypic switching in atherosclerosis. Cardiovasc Res. 2012;95:156–164.
26. Hu Y, Zhang Z, Torsney E, Afzal AR, Davison F, Metzler B, Xu Q.
Abundant progenitor cells in the adventitia contribute to atherosclerosis
of vein grafts in ApoE-deficient mice. J Clin Invest. 2004;113:
1258–1265.
27. Sainz J, Al Haj Zen A, Caligiuri G, Demerens C, Urbain D, Lemitre
M, Lafont A. Isolation of “side population” progenitor cells from
healthy arteries of adult mice. Arterioscler Thromb Vasc Biol. 2006;26:
281–286.
28. Klein D, Weisshardt P, Kleff V, Jastrow H, Jakob HG, Ergün S. Vascular
wall-resident CD44+ multipotent stem cells give rise to pericytes and
smooth muscle cells and contribute to new vessel maturation. PLoS
ONE. 2011;6:e20540.
29. Crisan M, Yap S, Casteilla L, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell. 2008;3:
301–313.
Key Words: differentiation ■ stem cell plasticity
biology ■ vascular smooth muscle
■
stem cells
Downloaded from http://circres.ahajournals.org/ at CONS CALIFORNIA DIG LIB on August 26, 2013
■
vascular