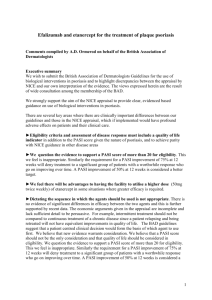
The Cardio-Respiratory Human System: The Cardio Respiratory
advertisement

“The The Cardio Cardio‐Respiratory Respiratory Human System: Human System: a simulation study” “P “Process System Engineering in Human Physiology” S t E i i i H Ph i l ” Elisa Montain, Anibal Blanco, Alberto Bandoni g g, Q ( ) Pilot Plant of Chemical Engineering, PLAPIQUI (UNS‐CONICET) Bahía Blanca, Argentina PASI 2011 PASI 2011 Process Modeling and Optimization for Energy and Sustainability S Saturday, July 23, 2011, Angra dos Reis, RJ, Brazil d J l 23 2011 A d R i RJ B il PASI 2011 - A. Bandoni 1 Background The cardiovascular system (CVS) is responsible for supplying oxygen and nutrients to tissues and organs organs.. CV diseases are a major cause of death in humans humans.. Many experimental studies have studied the mechanisms and therapy of the CV diseases Together with experimental approaches, mathematical modeling has become a popular way to analyze the CVS CVS.. Many models have been published since the preliminary and basic model of Godins in 1959 Approaches include include:: hemodynamic models of the vascular system, distributed impedance and pulmonary arterial stress, lumped parameter models of the integrated CVS, hemodynamic monitoring models, etc.. etc.. In the last few fe years ears there have ha e been important developments de elopments in integrated lumped parameter models of the circulatory and nervous control systems. systems. PASI 2011 - A. Bandoni 2 Motivation Assistance A i t iin th the d decision i i making ki off medical di l practice ti Diagnosis of diseases of the CVS (coronary arteries and heart muscles dysfunctions, valvular disorders and pulmonary disease. Comprehend the math. concepts and terms defining how CVS system behaves. To teach about the complex interactions of the cardiovascular system. system. H l tto vascular Help l surgeons iin treatment t t t planning l i and d tto engineers i iin designing d i i better medical devices. devices. A promising integration strategy involves the personalization of mathematical models based on biophysical measurements. measurements. Analysis of the hemodynamics (blood flow dynamics) of the CVS. Capacity to locate factors that are not directly observable . Key role in the measurement of pump efficiency and tissue stress, to assist treatment decisions. PASI 2011 - A. Bandoni 3 Motivation Anesthesia control and drug delivery control: control: Control of patient physiological variables during intensive care is achieved through drug g delivery. delivery y. Drug delivery process depends on the value of the physiological variable under control and on the patient's patient s condition Drugs such sodium nitroprusside (SNP) and dopamine (DP) are normally used for regulation of Media Arterial Pressure (MAP) or Cardiac Output (CO) (CO).. Doctors use their discretion to regulate variables that are difficult to quantify in practice or inferred from other measurements and patient responses to certain surgical procedures. procedures. Currently, the drug infusion is done manually or by programmable pumps. pumps. The professional is responsible for monitoring the controlled variable (MAP, CO) and g delivery y according g to the measurement. the drug PASI 2011 - A. Bandoni 4 Objectives Development of an integrated distributed parameter model of the human cardio respiratory system. Development of a computational tool to help physicians in the diagnosis of various heart diseases diseases. Studyy of the drug g delivery y ((SNP, DP, etc.)) The developed p model contain the following g sub-models: Circulatory system Baroreceptors Respiratory system Gas transport and distribution in organs Pharmacological effect of drugs on the hemodynamic variables. variables PASI 2011 - A. Bandoni 5 Anatomy and Ph i l Physiology PASI 2011 - A. Bandoni 6 The Cardiovascular System The Cardiovascular System: It consists of: The heart, which is a muscular pumping device A closed system of vessels (arteries, veins, and capillaries). The Heart The heart is a hollow muscular pump that provides the force necessary to circulate i l t the th blood bl d to t allll the th tissues ti i the in th body b d through th h blood bl d vessels. l The normal adult heart pumps about 5 liters of blood every minute throughout life. PASI 2011 - A. Bandoni 7 Heart Anatomy Aorta Superior vena cava Pulmonary truck Pulmonary vein Left Atrium Pulmonary valve Right atrium Mitral valve Tricuspid valve Aortic valve Left Ventricle Right ventricle Inferior vena cava PASI 2011 - A. Bandoni 8 Functions of the Heart Generates blood pressure Routes blood Heart separates pulmonary and systemic circulation Ensures oneone-way blood flow Heart valves ensure oneone-way y flow Regulates blood supply Changes Ch in i contraction t ti rate t and d fforce match t h bl blood dd delivery li tto changing metabolic needs Most healthy y people p p can increase cardiac output p by y 300– 300–500% Heart failure is the inability of the heart to provide enough blood flow to maintain i t i normall metabolism t b li PASI 2011 - A. Bandoni 9 The Chambers Separated by Interatrial Septum Interventricular Septum Right Atrium Blood Bl d ffrom S Superior i and d iinferior f i venae cavae and d th the coronary sinus i Right Ventricle Receives blood from the right atrium via the right AV valve valve, tricuspid valve Thin wall Left Atrium Receives blood from R and L Pulmonary Veins Left Ventricle Receives blood from the Left AV valve Thick wall Pumps to body via Aortic Semilunar Valve PASI 2011 - A. Bandoni 10 The Valves Two types off valves: T l k keep the h blood bl d flowing in the correct direction. Between atria and ventricles: called atrioventricular valves (also called cuspid p valves)) Bases of the large vessels leaving the ventricles: called semilunar valves. When the ventricles contract, contract atrioventricular valves close to prevent blood from flowing back into the atria. When the ventricles relax, relax semilunar valves close to prevent blood from flowing back into the ventricles. Vales V l close l passively i l under d blood bl d pressure. Responsible R ibl for f the th heart h t sounds. PASI 2011 - A. Bandoni 11 Circulatory System PASI 2011 - A. Bandoni 12 Circulatory System Deoxygenated D t d bl blood d returns t to t the heart via the superior and inferior vena cava, enters the right atrium, atrium passes into the right ventricle, and from here it is ejected to the pulmonary artery. Oxygenated blood returning from the lungs enters the left atrium via the pulmonary veins, passes into the left ventricle, and is then ejected to the aorta. PASI 2011 - A. Bandoni 13 Blood flow pattern through the heart 1.Blood 1. Blood enters right atrium via the superior and inferior venae cavae 2.Passes 2. Passes tricuspid valve into right ventricle 3 Leaves by passing pulmonary semilunar 3.Leaves 3. valves into pulmonary trunk and to the lungs to be oxygenated 4.Returns 4. Returns from the lung by way of pulmonary veins into the left atrium 5.From 5. From left atrium past bicuspid valve into left ventricle 6.Leaves 6. Leaves left ventricle past aortic semilunar valves into aorta 7.Distributed 7. Distributed to rest of the body PASI 2011 - A. Bandoni 14 Blood flow pattern through the heart PASI 2011 - A. Bandoni 15 Blood Vessels Blood vessels are divided into a pulmonary circuit and systemic circuit. Artery - vessel that carries blood away from the heart. Usually oxygenated. Exception, pulmonary artery. Vein - vessel that carries blood towards the heart. Usually deoxygenated. Exception pulmonary veins Capillary - a small blood vessel that allow diffusion of gases, nutrients and wastes between plasma and interstitial fluid. Systemic vessels Transport blood through the body part from left ventricle and back to right g atrium Pulmonary vessels Transport blood from right ventricle through lungs and back to left atrium Blood vessels and heart are regulated to ensure blood pressure is high enough for blood flow to meet metabolic needs of tissues PASI 2011 - A. Bandoni 16 The Real Thing PASI 2011 - A. Bandoni 17 The Real Thing PASI 2011 - A. Bandoni 18 History PASI 2011 - A. Bandoni 19 Mathematical Modelling in Physiology With mathematical models it is possible to simulate almost any kind of phenomena in nature on a computer. This is a scientific practice of modern science and engineering (biology, physiology, medicine, climate research, research, ecology, physics, chemistry etc.) chemistry, etc ) Mathematical modeling in medicine and biology has become so important that this type of research now has its own name: in silico Mathematical modeling undoubtedly will become the paradigm of scientific and medical research in the twenty‐ twenty‐first century. In research research, the ultimate goal is mechanisms‐ mechanisms‐based models models, but in reality models are more often used in a detective‐ detective‐like way to investigate the consequences of different hypotheses. The mathematics modeling is used as a microscope to unveil information 2011 - A. Bandoni 20 about reality, that is otherwisePASI inaccessible Heart and Blood Circulation Research History Since the dawn of civilization, civilization man has been concerned with the understanding of living things. In I one off the th mostt ancient i t medical di l ttreatises ti ((N (Nei Nei N i Jing, Ji 2697 2697--2597 BC) BC), blood is mentioned as originating in the heart and distributed in order to return to the starting point. Despite widespread knowledge of the anatomy of blood vessels, Greeks were unable to find the start of blood circulation by not knowing the principle of conservation of mass. The Western world had to wait for William Harvey (1578(1578-1657) to establish the concept of circulation. PASI 2011 - A. Bandoni 21 History Di Discovery off the th closed l d circulation i l ti off blood bl d by b William Willi H Harvey (1578‐‐1657). "De Motu Cordis" ("On the Motion of the (1578 Heart and Blood“. Frankfurt, 1628) Stroke volume is 70 ml. per beat and Heart beats 72 times per minute, therefore Cardiac Output should be 7.258 liters per day Before 1628, the Galenic view of the body prevailed and the concept of blood circulation was not imaginable. Galen or Galenius (Greek physician, II century AD), spent most of his lifetime observing the human body and its functioning. Galen believed that the heart acted not as a pump, but rather that it sucked blood from the veins, that blood flowed from one ventricle to the other of the heart through a system of tiny pores of the septum septum. Using a simple model, Harvey showed that the amount of blood leaving the h t iin a minute heart i t could ld nott conceivably i bl b be absorbed b b db by th the b body d and d continually replaced by blood made in the liver from chyle chyle.. PASI 2011 - A. Bandoni 22 History Consequently, this model based evidence established the concept that blood must constantly move in a closed circuit, otherwise the arteries and the body would explode under the pressure. This was discovered about 8 years before the light microscope. The concept or method of using mathematical modeling, as a tool for making an inaccessible system accessible or an invisible system visible, is therefore f being coined as “the “ mathematical microscope” in honor off William Harvey. The mathematical microscope p Ottesen (2011) PASI 2011 - A. Bandoni 23 Th Windkessel The Wi dk l Effect PASI 2011 - A. Bandoni 24 The Windkessel Effect The windkessel effect is use to describe: • Load faced by the heart in pumping blood through pulmonary or systemic arterial system. system • Relation between blood pressure and blood flow in the aorta or pulmonary artery Characteristic parameters of CVS such us compliance and peripheral resistance can be described in terms of the Windkessel models, which is useful f l iin: • Quantifying the effects of vasodilator or vasoconstrictor drugs. • The development and operation of mechanical heart and heart-lung machines. hi Windkessel: a german word that can be translated as air (wind) chamber Windkessel: (kessel kkessel). l). l) ) First description p by y German p physiologist y g Otto Frank in 1899. PASI 2011 - A. Bandoni 25 The Windkessel Effect Heart and systemic arterial system similar to a closed hydraulic circuit comprised of a water pump connected to a chamber. The circuit is filled with water except for a pocket of air in the chamber Arterial compliance Peripheral P i h l ressistance As water is pumped into the chamber, the water both compresses the air in the pocket and pushes water out of the chamber chamber. . PASI 2011 - A. Bandoni 26 The Windkessel Effect The compressibility of the air in the pocket simulates the elasticit elasticity y and extensibility of the major artery, as blood is pumped into it by the heart ventricle. This effect is commonly referred to as arterial compliance compliance.. The resistance water encounters while leaving the Windkessel, simulates the resistance to flow encountered by the blood as it flows through the arterial tree from the major arteries arteries, to minor arteries arteries, to arterioles arterioles, and to capillaries, due to decreasing vessel diameter. Thi resistance This i t to t flow fl is i commonly l referred f d to t as peripheral i h l resistance. resistance i t . PASI 2011 - A. Bandoni 27 The Windkessel Effect Hypotheses: • Unsteady flow. • The pressure diff. across the resistance is a linear function of the flow rate t • The working fluid is incompressible (constant air pressure to volume ratio) • The flow is constant throughout the ejection phase. The Windkessel 2-elements considers only y the arterial compliance p ((C)) and the peripheral resistance (R). Symbols: P : pressure generated by the heart (N.m-2) [mmHg] Q : blood flow in the aorta (m3.s-1) [l.mn-1] R : peripheral resistance (N (N.s.m s m-55) [dyne [dyne. ss.cm cm-55] C : arterial or systemic compliance (m5.N-1) [ml.mmHg-1] t : time [(s) T : period i d ((s)) Ts: ejection time (s) PASI 2011 - A. Bandoni 28 The Windkessel Effect Theoretical development of the Windkessel effect air P(t) Q Ts V(t) R Q(t) Q1(t) Pcv t T Schematic representation of a chamber Systolic phase: valve in open position PASI 2011 - A. Bandoni Diastole phase: valve in close position 29 The Windkessel Effect I - Systolic S t li phase h ( l iin open position) (valve iti ) 0 t T s Conservation of mass: Thus: Q Q1 dV dt Qin Qout Qcc Qcc: flow to the compliance chamber Pcv : central venus pressure: (Pcv<< P) (Pcv≅5 mmHg vs. P≅100 mmHg ]) Hyp.4: Q = Cte. throughout the systolic phase, thus: Therefore: Then: Q P dV P dV dP . R dt R dP dt Q (t ) P (t ) dP(t ) C. R dt P Pcv R.Q1 Compliance (C) or PASI 2011 - A. Bandoni dP (t ) P(t ) Q (t ) dt R.C C 30 The Windkessel Effect Solution of the differential equation a) Particular solution (Q = Cte.=0) P(t ) 1. exp( t ) R.C b) Method of variation of parameter ( α1=α1(t) ) 1 t t Q d ( ). exp( ) ( ). exp( ) t t 1 1 dt R.C R.C R.C C t t d1 (t ) t Q 1 1 t .1 (t ). exp( ) exp( ) ( ). exp( ) 1 R.C R.C R.C dt R.C R.C C Hence: d1 (t ) Q t . eexp( p( ) dt C R.C Then: 1 (t ) R.Q. exp( PASI 2011 - A. Bandoni t ) 2 R.C 31 The Windkessel Effect c) The general solution for systolic phase is t t Ps (t ) R.Q. exp( ) 2 . exp( ) R.C R.C To determine α2 we can use initial condition P(t=0)=P0 , then α2 = P0-R.Q P(t 0) P0 2 P0 R.Q Finally, the pressure waveform for the systolic phase can be written as t Ps (t ) R.Q P0 R.Q . exp( ) R.C PASI 2011 - A. Bandoni 32 The Windkessel Effect I – Diastolic Di t li phase h ( l iin close (valve l position) iti ) Ts t T air Following similar reasoning but with Q=Cte.=0 V(t) P(t) dP P Q dt R.C C Q1(t) With initial condition: P(t=Ts)= Ps(Ts), the solution to the differential equation is: P(t ) 3. exp( p( t ) R.C where 3 P0 exp( p( t ) 1. R.Q. R.C Fi ll the Finally, th pressure waveform f for f the th di diastolic t li phase h can be b written itt as: t t Pd (t ) P0 exp( p( ) 1.R.Q . exp( p( ) R.C R.C PASI 2011 - A. Bandoni 33 The Windkessel Effect C Complete l t model d l Systolic Phase 0 t Ts air t Ps (t ) R.Q P0 R.Q . exp( ) R.C Diastolic Phase V(t) P(t) Q1(t) Ts t T air t t Pd (t ) P0 exp( ) 1.R.Q . exp( ) R.C R.C Given: Q , R , C , T , Ts and P 0 ( data ) or PASI 2011 - A. Bandoni V(t) P(t) Q1(t) Ts ) 1 exp( R.C P0 R.Q. T ) 1 exp( R.C 34 The Windkessel Effect The term Th t R C it iis crucial R.C i l in i the th 2-W 2 W because b it determine d t i the th “speed” “ d” of the exponential decay. This product is called the “characteristic time”, called P P R.Q P0 Case: 0 t Case: PASI 2011 - A. Bandoni t 35 Case: The Windkessel Effect Hypertension: Ps > 140 mmHg 0, Pd > 90 mmHg PASI 2011 - A. Bandoni 36 The Windkessel Effect The electrical circuit equivalence Basic equation q of a 2-element Winkessel model: Electric circuit of 2 passive elements: I(t) I3 I2 Q (t ) P (t ) dP(t ) C. R dt I(t) : electrical l t i l currentt E(t) : electrical potential C : capacitance of the capacitor R : resistance of the resistor From the Ohm and Kirchhoff laws E(t) C R I (t ) E (t ) dE (t ) C. R dt I(t) ≡ Q(t) (blood flow) E(t) ≡ P(t) (arterial blood pressure) C ≡ C (arterial compliance) R ≡ R (peripheral resistance) PASI 2011 - A. Bandoni 37 The Windkessel Effect The 3-element Windkessel model I(t) E(t) R2 C R 1 I(t)) ≡ Q(t) (blood I( (bl d flow) fl ) E(t) ≡ P(t) (arterial blood pressure) C ≡ C (arterial compliance) R1 ≡ R1 (peripheral resistance (syst. and pulm.circuits)) R2 ≡ R2 ((resistance of valves (aortic and pulmonary)) R dE (t ) P(t ) dP (t ) 1 1 . I (t ) C.R1. C. dt R2 dt R2 PASI 2011 - A. Bandoni 38 The Windkessel Effect The 4-element Windkessel model I(t) E(t) E(t) R2 C L R1 I(t) ≡ Q(t) (blood flow) E(t) ≡ P(t) (arterial blood pressure) C ≡ C (arterial compliance) R1 ≡ R1 (peripheral resistance (syst. and pulm.circuits)) R2 ≡ R2 (resistance of valves (aortic and p pulmonary)) lmonar )) L ≡ L (inertia of the blood circulation) R1 L dE (t ) d 2 E (t ) P (t ) dP (t ) 1 . I (t ) R1.C . L.C. C . R2 dt dt 2 R2 dt R2 PASI 2011 - A. Bandoni 39 Compartment M d l Models PASI 2011 - A. Bandoni 40 Compartment Models They are used to describe transport material in biological sciences A compartment model contains a certain number of compartments, each one with a well mixed material Compartments exchange material following certain rules Material can be stored in the boxes and transported between them Every compartment has a number of connections entering and leaving it. Material can be added from the outside, can be removed or transported. Source Drain PASI 2011 - A. Bandoni 41 Compartment Models Material represent the amount of something that we wish to account for To account for the material, the models must fulfill certain conservation laws. Conservations laws state that the difference between input and output flows amounts how much will be stored. A compartment model can also represent: Ecological systems (material could be energy and the compartment different species of animals or plants) Physiologic system (material could be oxygen and compartment de organs) Compartment can not be thought as independent. Flow in and out may depend on the compartment volume Inflow to compartment may depend of outflow of other compartment. PASI 2011 - A. Bandoni 42 Compartment Models State variables depend on each other and on the state of the system as a whole. The transport in and out is characterized by the flows velocities. Limitations of the compartment model • Is the system closed. closed. Equation of conservation of mass is correct only if all material added or removed is included in the model. There is some lost of detailed information information. • Homogeneity assumption. assumption. Not always it is possible to keep this assumption. Then more compartments are needed but also more information it is required required. • Accuracy of the balance equation. equation. In real physiological system typically some mass balance are know and other are not. • R l Relevance off th the mass balance. balance b l . Not N t allll systems t can be b described d ib d in terms of mass balances. • Sensitivity analysis. analysis. Initial conditions and model parameters are not always known precisely. PASI 2011 - A. Bandoni 43 Mathematical M d l Models Cardiovascular, Respiratory and Pharmacodynamic PASI 2011 - A. Bandoni 44 Human Circulatory System Model The historical fascination of the heart has lasted for many centuries and continues to attract considerable attention both theoretically and clinically. clinically. To develop a physiologically founded model of the heart and the vasculature, it is essential to have a good model of the human short term press re control represented by pressure b the baroreceptor mechanism mechanism.. Using a lumped parameter compartment model, the entire human cardiovascular system may be described as a network of compliances, resistances and inductances not reflecting anatomical properties properties.. Although strikingly simple, the model gives a very good description of the input impedance of the arterial system. system. Such models are valuable tools for understanding cardiovascular diseases (hypertension weak and enlarged heart, (hypertension, heart hemorrhages, hemorrhages etc etc..) PASI 2011 - A. Bandoni 45 Human Circulatory System Model Models facilitates getting new insight into cardiovascular functions and the interaction with other system (central nervous system, respiratory systems, etc..) etc This type of models can be reliable and stable, simply enough to run in real time.. time ti Lumped cardiovascular models are divided into pulsatile and non non--pulsatile pulsatile.. In the pulsatile case, the heart functioning is guided by a time time--varying elastance function function.. A lumped pulsatile cardiovascular model that embraces principal features of the human circulation. circulation. PASI 2011 - A. Bandoni 46 Human Circulatory System Model Lumped cardiovascular models are divided into pulsatile and non non--pulsatile pulsatile.. I the In th pulsatile l til case, the th heart h t functioning f ti i iis guided id d by b a time ti -varying timei elastance function function.. A lumped pulsatile cardiovascular model that embraces principal features of the human circulation. circulation. PASI 2011 - A. Bandoni 47 Human Circulatory System Model Pulmonar circulation Ap3 Ap2 Vp1 Ap1 Vp2 RV LA Heart LV RA Vs2 As1 Vs1 As2 Systemic circulation As3 PASI 2011 - A. Bandoni 48 Human Circulatory System Model Pp3 Vp3 Qp2 Cp2 Rp2 Pp2 Vp2 Cp3 Rp3 Ap3 Qp3 Ap2 Ql1 Qp1 Cp1 Rp1 Lp1 Eminrv Emaxrv Erv(t) Lrv Pra Vra Pp11 P Vp1 Ap1 Qrv Era Rra Lra Vp2 PV TV Qra Qla RA AV Qv2 Cv2 Rv2 Lv2 Pv2 Vv2 Cv1 Rv1 Pv1 Vv1 Cl2 Rl2 Ll2 Pla Vla Ela Rla Lla Plv Vlv Eminlv Elv(t) Emaxlv Llv MV LV Qlv Pa1 Va1 As1 Vs2 Qa1 Qv1 As2 Vs1 Qa3 As3 Pa3 Va3 Cl2 Rl2 Pl2 Vl2 Ql2 LA RV Prv Vrv Pl1 Vl1 Vp1 Pa2 Va2 Ca1 Ra1 La1 Ca2 Ra2 Qa2 Ca3 Ra3 PASI 2011 - A. Bandoni 49 Human Circulatory System Model Model of a typical compartment (chamber) of the hemodynamic system V0 : volumen at p=0 R : ressistance L : inertia C : compliance li Blood input pi R Qin pi p0 Qin Qout L Blood output p0 C V0 Qout PASI 2011 - A. Bandoni Hemodynamic y element of a blood chamber Equivalence with an electric circuit 50 Circulatory System Model (Ottesen et al., 2003) • Heart Model o Heart H t ititself: lf 4 chambers h b (2 atria t i and d 2 ventricles) ti l ) o Vascular part Systemic part: 5 chambers (systemic arteries and veins) Pulmonary part: 5 chambers (arteries and veins) • Baroreceptor Model o Chronotropic effect (on heart rate) o Inotropic effect (on the cardiac contractility) o Vascular V l effect ff t (on ( arteries t i and d veins) i ) Respiratory System Model (Christiansen and Dræby, 1996) • Lung Model o Upper respiratory tracks: 1 chamber o Alveoli: 1 chamber • Gas Transport in Blood Model (O2, CO2, Anesthesia) o Vascular V l part: t 5 chambers h b o Organs and tissues: 8 compartments Organs compartments: one part of tissue and one part of blood (equilibrium of the substances distributed by the blood on both sides it is assumed) It is assumed constant blood (VB) and tissue (VT) volumes. o Capillaries and alveoli: 1 chamber Ph Pharmacodynamic d i Model M d l (Gopinath et al., 1995) • Drug Effect on Hemodynamic Variables Model PASI 2011 - A. Bandoni 51 The Cardiovascular Model The Pumping Heart Based on an elastance model where the cardiac contraction properties of the two ventricles are representing by a pair of time time--varying elastance functions.. functions The inertia of blood movements in the ventricles is considered through an inductance that introduce a phase shift between the ventricular pressure and the root aortic pressure. pressure. The viscous properties of blood in the two atria are included by ventricular filling g resistance PASI 2011 - A. Bandoni 52 Ql aR la pla Left Heart LA Right Heart Ros pa1 RA PA Ra1 La1 pa2 Qr aRra TV Lra pv1 a3 prv Era Rop pas LV Ra2 p Ra3 Ca2 Ca1 pra AV Elv(t) AA PV Pulm . Circ. Lla Ela pas Syst. Circ. Ql M vplv L lv V Ca3 Qrv Rrv PV Rv1 Cv1 pv2 Rv2 Lv2 CVi Cv2 pap RV Erv(t) pp1 Rp1 Cp1 Lp1 pp2 Rp2 Cp2 PASI 2011 - A. Bandoni Ra3 pp3 Cp3 Rl1 pl1 Cl1 R pl2 l2 Cl2 Ll2 CVs 53 The Pumping Heart dQla pla plv Rla .Qla dt Lla if pla plv Qla 0 if pla plv dVla Ql 2 Qla dt pla Ela .Vla Vd ,la t Vlv ,b * Qlv dt 2ml t Elv t Emin,lv .1 t Emax,lv . t .t 2. .t a . sin b . sin , 0 t tce tce tce t 0 , tce t th tce 0 1.th pas R0 s .Qlv pas dQlv plv pas d dt Llv Qlv 0 if plv pas if plv pas dVlv Qla Qlv dt plv Elv (t ). ) Vlv Vd ,lv PASI 2011 - A. Bandoni 54 The Pumping Heart Elastance model Emin,lv Emax,lv tce th 2. .t .t a . sin b . sin , 0 t tce tce tce t 0 , tce t th Elv t Emin,lv .1 t Emax,lv . t PASI 2011 - A. Bandoni 55 The Circulatory System Model Single chamber model pa1 Q 1 Qa1 pa2 Va2 Qa2 dVa 2 Qa1 Qa 2 dt V V pa 2 a 2 un ,a 2 Ca 2 Qa 2 PASI 2011 - A. Bandoni pa 2 pa 3 Ra 2 56 The Baroreceptors Model Baroreceptors (BR) are sensors of mean blood pressure that are located in the blood vessels of several mammals. BR nerves are stretch receptors which responds to changes in blood pressure. BR can send messages to the CNS to increase or decrease total peripheral resistance and cardiac output (CO). BR act immediately as part of a negative feedback system called the baroreflex, returning mean arterial blood pressure (MAP) to a normal level as soon as there is a change change. BR detect the amount of stretch of the blood vessel walls, and send the signal to the CNS system in response to this stretch. A hysteresis-like phenomena is observed: the response to a pressure increase is different to the response to a pressure-decrease PASI 2011 - A. Bandoni 57 The Baroreceptors Model ① Increased blood pressure stretched carotid arteries and aorta causing the baroreceptor to increase their basal rate of action potential generation. ② Action A ti potential t ti l are conducted d t db by the glossopharyngeal and the vagus nerves to the cardioregulatory and vasomotor t centers t in i the th medulla d ll oblongata. ③ As a result of increased stimulation from the baroreceptor, the cardioregulatory center increased parasymphatic stimulation to the heart, which decreases the heart rate. ④ Also, as a result of increased stimulation from the baroreceptor, the cardiorvascular center decreases sympathetic stimulation to the heart, which decreases heart rate stroke volume.PASI 2011 - A. Bandoni 58 The Baroreceptors Model ⑤ The vasomotor center decreases sympathetic stimulation to blood vessels, causing vasodilatation. The vasodilatation along with the decreased heart rate and decreased stroke volume bring the elevated blood pressure back toward normal. Iff the initial problem were decrease in blood pressure, the activities and effect of baroreceptors, cardiovascular center and vasomotor center would be opposite it off what h t was illustrated. ill t t d PASI 2011 - A. Bandoni 59 The Baroreceptors Model Baroreceptor system Heart frequency Systolic maximum elastance Cardiovascular System MAP Systemic resistance arteries H Emaxlv, Emaxrv Ra1, Ra2, Ra3 Compliance in veins and arteries Cv1, Cv2 Unstressed vol in syst. vol. syst veins Vunv1, Vunv2 PASI 2011 - A. Bandoni 60 The Baroreceptors Model Afferent sector MAP Efferent sector Central Nervous System n Sensors ns MAP n p MAP 1 MAP 1 np Eferent pathways th xi ib MAP i .ns .MAP i .n p .MAP i dxi t 1 xi t ib MAP , i E dt i 1 MAP 1 ns i E H , Emax , R ps ,Vun , Cv PASI 2011 - A. Bandoni 61 The Respiratory System Model The respiratory p y system y is concerned with the transport p of oxygen yg between atmosphere and the tissue and organs in the body O Oxygen iis continuously ti l transported t t d by b the th llung and d blood bl d circuit circuit. i it. Carbon dioxide is a waste product of the oxidative metabolism and is carried by the blood in the opposite direction PASI 2011 - A. Bandoni 62 The Respiratory System Model O2 CO2 Atmosphere Ventilation Alveoli O2 CO2 Gas exchange O2 CO2 Pulmonary circulation Right Ri ht Heart Gas transport Left L ft Heart Systemic circulation O2 Cell CO2 Gas exchange PASI 2011 - A. Bandoni metabolism 63 The Respiratory System Model Lung model: pressure R0 Alveoli Upper airway i Um (t) Atmosphere or respiratory i t mask ■ Connect atmosphere (mask) with alveoli trought expressions of gas flow C0 R1 R2 Ri C1 C2 Ci Ut (t) ■ The lung is divided in compartments ■ In each compartment gas flows are calculated (O2, CO2, Anesthesia) ■ The outputs of the model are: pressure in different sectors, Muscles the net volume of air flow, partial pa t a pressure p essu e o of e expired p ed a air and alveoli. PASI 2011 - A. Bandoni 64 The Respiratory System Model Distribution of substances in the organs through blood Alveolus Capillary Alveolus κ.pA pcp Central venous compartment Viscere venous compartment pv Metabolism s cvv Lean venous compartment cvl Adipose Adi tissue venous compartment cav pas Central C t l arterial compartment pli Liver pki Kidney phe Heart pbr Brain pre Other organs pco pmu pad Connective tissue Muscles Adipose tissue PASI 2011 - A. Bandoni Q.cb Q κ.p Vbcb (p) ((1- λ )).Q.c Q vs λ.Q.cvs Metabolism M- M+ Vtct (p) Vbcb (p) zi.Q(p).cb zi.Q.cas 65 The Respiratory System Model Upper airways p0 R0 C0 f0 Alveoli pcp pi RiCi fi U m p0 R0 .i 1 Ci . n dpi dt dp0 dt R0 .C0 dpi p0 pi U t , i 1...n A d dt Ri .Ci Pressure model I U m p0 n I pi p0 df0 RT . f e f0 . fi f 0 i 1 2 dt C0 p0 V00 p0 R0 Ri I p0 U t pi dfi RT . f0 fi κ . p f p cp i i 2 dt Ci . pi V0i . pi Ri 0 I x x x0 x0 Molar fractions model PASI 2011 - A. Bandoni 66 The Pharmacodynamic Model Pharmacology: the history, source, physical and chemical properties, Pharmacology: biochemical and physiological effect, mechanisms of action, absorption, distribution, biotransformation and excretion, and therapeutic and other uses of drugs. drugs. Pharmacokinetics: absorption, Pharmacokinetics: absorption distribution, distribution metabolism and excretion of drugs.. drugs Pharmacodynamics: biochemical and physiological effects and their Pharmacodynamics: mechanisms of action. action. PASI 2011 - A. Bandoni 67 Drug Concentrattion D The Pharmacodynamic Model Time Concentration of drug in the body as a function of time PASI 2011 - A. Bandoni 68 The Pharmacokinetic Model dc dp dc t Vt Vb b dt dp dp 1 0 cO2 M M O2 c O2 O2 caa M aa c aa aa dp dc b Vb dt dp 1 z i Qc as c b p M p M p M CO 2 M 0 0 Q1 c vs c b p p A p dp dc b Vb dt dp 1 Qc x c b p Pressure balance i the in th organs Pressure balance in the capillaries Q c Q2 c 2 cx 1 1 Q1 Q2 Pressure balance in the compartments p PASI 2011 - A. Bandoni 69 The Pharmacodynamic Model Cd Drug effect MAP Baroreceptors EmaxBARO RsisBARO Emax= EmaxBARO(1±Eff) R= RsisBARO(1±Eff) dEff k1.CdN .Eff max Eff k2 .Eff dt dEffCa 1 PFL dCa1 Ca1BASE . dt dt Cardiovascular system dEff Emax lvDP dEmax lv dEmax lvBARO 1 Eff Emax lvDP Emax lvBARO l BARO dt dt dt dEff RsisDP dEff RsisSNP dRsis dRsisBARO 1 Eff ff RsisDP Eff ff RsisSNP RsisBARO dt dt dt dt PASI 2011 - A. Bandoni 70 The Pharmacodynamic Model Drug (intravenous) Affected variable Action SNP (sodium nitroprusside) Peripheral resistance MAP DP ((dopamine) p ) Peripheral resistance, systolic maximum elastance MAP PFL (propofol) BIS MAP unconsciousness Systolic maximum elastance Peripheral resistance PASI 2011 - A. Bandoni 71 The Pharmacodynamic Model DP and SNP drugs are chosen to increase ventricular contractility and reduce d th resistance the i t off arteries t i to t blood bl d flow, fl respectively. respectively ti l . PFL is chosen to conduct unconsciousness by measured of BIS parameter.. parameter DP increases the MAP and CO. CO. SNP decreases and increases CO MAP.. MAP Sceneries are simulated by delivering a step of 1μg/kg/min of SNP, DP and PFL and registering the dynamic response of the physiological, pharmacokinetic and pharmacod pharmacodynamic namic variables. ariables PASI 2011 - A. Bandoni 72 Computational Implementation Model implemented in Fortran Diff. Eqs Eqs.. solved with a 4th order Runge Runge--Kutta method. Resolution sequence: (i) the cardiovascular model is solved until to reach steady state, (ii) the CO obtained from this model is used in the breathing g model,, ((iii)) the breathing g model is solved until to reach steady y state. Th d The drug iinjection j ti iis simulated i l t d for f a cycle l off breathing b thi (5 sec.). sec.)). Then Th the th cardiovascular model is fed with the drug concentration Cd to simulate the 0.8 sec. a heartbeat. heartbeat. The updated value of CO is fed back to the breathing model. PASI 2011 - A. Bandoni 73 Computational Implementation CO2, O2 Cd (alveoli) Cd(inhalable) Cd(inyectable) Transport and distribution, Pharmacokinetics of drugs Respiratory system Qa3, Qp3 Cd (organs) Cardiovascular C di l system Pharmacodynamics Ph d i of drugs Baroreflex MAP EmaxBARO Ra2BARO Ra3BARO Emax Rsis EffEmax EffRa2 EffRa3 Control Action PASI 2011 - A. Bandoni 74 Computational Implementation Dimensions of the integrated model Model Var./Eqs. Algebraics Var./Ecs. Differenctials Parameters Cardiovascular-Respiratory 37 39 53 Respiratory-Pharmacodynamic 60 93 85 Total 97 132 138 PASI 2011 - A. Bandoni 75 Results PASI 2011 - A. Bandoni 76 Results: cardio vascular system Wiggers Diagram PASI 2011 - A. Bandoni 77 Results: cardio vascular system Left ventricular volume vs. time Left ventricle and root aortic pressure vs. time PASI 2011 - A. Bandoni 78 Results: cardio vascular system Outflow of the left ventricle Left ventricular pressure Pressure vs. Volume left ventricle PASI 2011 - A. Bandoni 79 Results: baroreflex system Heart period vs. vs time Resist sect. Resist. sect As1 of syst. syst arteries vs vs. time Compliance in sect. Vs1 of sistemic Unstres. Vol. of sect. Vs1 of veins vs. time PASI 2011 - A. Bandoni sistemic veins vs. time 80 Results: baroreflex system Sistolic max. elastance of left ventr.vs. time Comparison of CO vs. time in front of 10 % bleeding, with and without baroreceptor Comparison of MAP vs. time in front of 10 % bleeding, with and without baroreceptor PASI 2011 - A. Bandoni 81 Results: gas transport Partial pressure of O2 in different compartments of the body Partial pressure of CO2 in different compartments of the body PASI 2011 - A. Bandoni 82 Results: respiratory system expiración inspiración Volume vs. Pressue diagram in lungs Partial pres. profile of CO2 in lung and alveoli. PASI 2011 - A. Bandoni Partial pres. profile of O2 in lung and alveoli. 83 Results: pharmacodymic system Effect of the SNP action 1µg/kg/min SNP concentration profile at the central arterial compartment Mean Arterial Pressure, MAP PASI 2011 - A. Bandoni Cardiac Output, CO 84 Results: pharmacodynamic system Effect of the SNP action 1µg/kg/min Resistance, Ra3 Resistance, Ra2 PASI 2011 - A. Bandoni 85 Results: pharmacodynamic system Effect of the DP action 5µg/kg/min DP concentration profile at the central arterial compartment Mean Arterial Pressure, MAP PASI 2011 - A. Bandoni Cardiac Output, CO 86 Results: pharmacodynamic system Effect of the DP action 5µg/kg/min Medial arterial resistances Elastance PASI 2011 - A. Bandoni 87 Results: pharmacodynamic system Effect of the DP action 2, 4, 6, 8 µg/kg/min Cardiac Index vs. infusion doses (time) Volume Index vs. infusion doses (time) Systolic and diastolic pressure vs. infusion doses (time) PASI 2011 - A. Bandoni 88 Results: pharmacodynamic system Effect of the DP action 2, 4, 6, 8 µg/kg/min Systemic Resistance vs. infusion d doses (ti (time)) Cardiac frequency vs. infusion doses (time) PASI 2011 - A. Bandoni 89 Results: pharmacodynamic system Effect of the PFL action 150µg/kg/min / / Mean Arterial Pressure, MAP PFL conc. at the central arterial comp. Cardiac Output, CO Compliance of sector a1 of systemic arteries PASI 2011 - A. Bandoni 90 Conclusions Development of an integrated cardiovascular, baroreceptor, respiratory, pharmacokinetic and pharmacodynamic model model.. The effect of certain drugs on hemodynamic variables was studied studied.. PASI 2011 - A. Bandoni 91 Future Works General model validation with real patient data. data. Collaboration with a research group formed by doctors (Favaloro University, Bs..As Bs As.. – Español Hospital, Hospital B. Blanca, Blanca Arg Arg..) Model validation for inhalable anesthesia effects effects.. Model validation for simultaneously drugs administration administration.. Development of a control model for handling dose of drug administration.. administration Development of a teaching simulation model of the cardiovascular system (Instituto Nacional de Tecnología Industrial, INTI, Bs. Bs.As As.., Arg Arg..) PASI 2011 - A. Bandoni 92 Basic References: Cardiovascular Model: Ottesen J., Olufsen M. and Larsen J. Applied Mathematical Models in Human Physiology . SIAM, Philadelphia. (2004) Pharmacodynamic Model: Gopinath R., Bequette B., Roy R. and Kaufman H. Issues in the Design of a Multirate Model- based Controller for a Nonlinear Drug Infusion System Biotechnol. System. Biotechnol Prog. Prog 11 (3) (3), pp 318 318–32. 32 (1995) Respiratory Model: Christiansen Ch i ti T and T. dD Dræby b C C. Modeling M d li the th R Respiratory i t S System t Technical. Report IMFUFA, Roskilde University Denmark Text No. 318. (1996) PASI 2011 - A. Bandoni 93 Other References: Dua P and Pistikopulos E. E Modelling and control of drug delivery systems systems. Comp. Comp Chem. Eng. 29 pp. 2290-96. (2005) Montain M, M Bandoni J y Blanco A . Modelado del sistema cardiorespiratorio humano: un estudio de simulación. VI CAIQ (Congreso Argentino de Ing. Química) Mar del Plata 26 al 29 de septiembre (2010). Rao R, Bequette B and Roy R. Simultaneous regulation of hemodynamic and anesthetic states: a simulation study; Annals of Biomedical Engineering, 28 pp. 71( ) 84. (2000) Dua P, Dua V and Pistikopoulos E. Modelling and mult-parametric control for delivery of anaesthetic agents. Med. Biol. Eng. Comput. 48 543-53. (2010). Massoud T., G. Eorge, J. Hademenos, W. Young , E. Gao, J. Pile-Spellman and F. Uela. Principles and philosophy of modeling in biomedical research.The FASEB Journal, vol. 12 no. 3, pp.275-285, March 1, 1998. Ottesen J.T. The Mathematical Microscope ‐ Making the inaccessible accessible. Bi Biomedical di l and d Lif Life Sciences S i S Systems t Bi l Biology ‐ Volume V l 2 2, 2011. 2011 PASI 2011 - A. Bandoni 94 “With growing emphasis being placed d on the information processing aspects of biomedical investigation, theoretical and experimental studies assume increasing importance. importance In many instances, however, there are questions that appear to be present experimental p techniques; q ; in such cases,, unanswerable byy p models can usefully augment direct scientific experimentation. The essential Th i l ingredient i di off the h scientific i ifi method h d is i the h use off models. Good modeling is more likely to be achieved by following the rules of good thinking. thinking However, However the ideal model cannot be achieved. Partial models, imperfect as they may be, are the only means developed p byy and available to scientists for understanding g the universe” Principles and philosophy of modeling in biomedical research. T. Massoud, G. Eorge, J. Hademenos, W. Young , E. Gao, J. Pile-Spellman and F. Uela (University of California at Los Angeles, Columbia University, University of Dallas) The FASEB Journal, vol. 12 no. 3, pp.275-285, March 1, 1998 PASI 2011 - A. Bandoni 95 PASI 2011 - A. Bandoni 96 Muchas gracias PASI 2011 - A. Bandoni 97 Cámara izquierda del corazón p plv Rla Qla dQla la Lla dt Qla 0 si Qlv 0 si pla Ela Vla Vd ,la si Vlv,b t * dQa1 p p a 2 Ra1Qa1 a1 dt La1 p a1 Va1 Vun, a1 C a1 dVa 2 Qa1 Qa 2 dt plv p as plv pas dVlv Qla Qlv dt t pla plv pla plv dVla Ql 2 Qla dt dQlv p p as lv dt Llv si Circulación sistémica Qa 3 plv Elv t Vlv Vd ,lv p as pv1 Ra 3 Va3 Vun, a3 dVa1 Qlv Qa1 dt Qa 2 p a 2 p a3 Ra 2 pa2 Va 2 Vun, a 2 Ca2 dVa3 Qa 2 Qa 3 dt Qv1 pv1 pv 2 Rv1 dVv1 Qa3 Qv1 dt pv1 Vv1 Vun, v1 Cv1 dVv 2 Qv1 Qv 2 dt dQv 2 p p ra Rv 2Qv 2 v2 dt Lv 2 p a3 C a3 Qlv dt 2ml Elv t E min,lv 1 t E max,lv t t 2t b sin a sin t ce t ce t 0 tce 0 1t h 0 t t ce t ce t t h pas R0 sQlv pa1 pv 2 Vv 2 Vun,v 2 Cv 2 PASI 2011 - A. Bandoni 98 Cámara derecha del corazón Circulación pulmonar dQra p prv Rra Qra ra dt Lra dQ p1 Qra 0 si p p1 pra Era Vra Vd , ra Q p3 prv pap prv Erv t Vrv Vd , rv dVrv Qra Qrv dt t Vrv,b Qrv dt 2ml t* p p3 pl 2 pap R0 pQrv p p1 Qrv Q p1 Q p1 Q p 2 p p2 V p 2 Vun, p 2 C p2 p ps pl1 R p3 dV p3 dt V p3 Vun, p3 Q p 2 Q p3 p pl 2 Ql1 l1 Rl1 Vl1 Vun,l1 pl1 Cl1 C p3 dQl 2 pl 2 pla Rl 2Ql 2 dt Ll 2 dVl 2 Ql1 Ql 2 dt Erv t Emin,rv 1 t Emax,rv t dt p p 2 p p3 R p2 dVl1 Q p3 Ql1 dt dV p1 Q p2 C p1 dV p 2 prv pap si p p1 p p 2 R p1Q p1 L p1 V p1 Vun, p1 dt dQrv prv pap dt Lrv sii dt pra prv dVra Qv 2 Qra dt Qrv 0 pra prv si Vl 2 Vun,l 2 Cl 2 Modelo respiratorio (fracción molar) df 0 RT dt C 0 p 02 V 00 p 0 I U m p 0 f e f 0 R0 df i RT dt C i p i2 V 0 i p i I p i p 0 f i f 0 Ri i 1 n I p 0 U t p i f 0 f i κ p cp p i f i R i PASI 2011 - A. Bandoni 0 I x x x0 x0 99 Barorreceptores n s MAP n p MAP 1 MAP 1 1 MAP 1 ib MAP i ns MAP i n p MAP i dxi t 1 dt i i E H , E max , R ps , Vun , C v Q c Q2 c 2 cx 1 1 Q1 Q2 0 cO2 M M O2 O2 cO2 caa M aa c aa aa x t b MAP, i E i i Modelo respiratorio (presión) dp0 dt U m p0 R0 n i 1 Ci R0C0 0.27273 1.96364 t 0.66943 0.53554 t Um 17.00005 8.50909 t 0.57034 0.05904 t dpi dt dpi p0 pi U t dt Ri Ci dp dc b Vb dt dp 1 1 H 3 a2 H 2 1 Qc x c b p M CO2 M 0 0 a1 H a0 0 0 x 0.278 0.278 x 1.806 a 2 K a ,Pr NaOH 0 K a ,CO 1.806 x 1.904 1.904 x 5 a1 K a ,CO N NaOH OH 0 cCO2 K a ,Pr K a ,CO NaOH N OH 0 H Pr P 0 Modelo de transporte de gases en sangre dc dp dc t Vt Vb b dt dp dp dp dc b Vb dt dp z i Qc as c b p M p M p Q1 c vs c b p p A p a 0 K a ,CO K a ,Pr NaOH 0 H Pr 0 cCO2 Ery p, pH c bCO2 p, pH c CO 2 c Hb c Hb Pla c p , pH 1 CO2 Ery c Ery c Hb Hb 1 10 Ery Ery p, pH CO c CO p cCO 2 1 10 pH 2 2 Ery Ery p, pH CO c CO p cCO 2 2 2 PASI 2011 - A. Bandoni Ery p , pH pK Ery p , pH pH Ery p , pH pK Ery p , pH 100 Pla Pla p, pH CO c CO p cCO 2 1 10 pH pK 2 2 pK Ery p, pH 6.125 log 10 1 10 Pla pH p , pH Ery p , pH 7.84 0.06 sO2 p , pH pH Ery p, pH 7.19 0.77 pH 7.4 0.035 1 sO2 p, pH pK K Pla p, pH H 6.125 log l 10 1 10 pH 8.7 1 1 e y p hp 3.5 ap xp log p O2 / kPa t p t p aa c aa pCO2 mmol 0.07 0.03xHbf cdpg / 5 ap 0.72 pH cCO2 p 7.4 0.09log l 5.33kPa 0.386xHbCO 0.174xHi 0.28xHbf b p b p aa c aa y p 1.875 xp x0 p hp tanh 0.5343xp x0 p c bO2 p, pH O2 pO2 c Hb sO2 s O2 T 37 x0 p 1.946 a p 0.055 ºC t Pla l Hb p, pH cCO p, pH 1 cEry cCO 2 2 c Hb cOt 2 p O2 pO2 Modelo farmacodinámico dEffCa1PFL dCa1 Ca1BASE dt dt dEff k1C N Eff max Eff k 2 Eff d dt dEff RsisDP dEff RsisSNP dRsis dRsisBARO 1 Eff RsisDP Eff RsisSNP RsisBARO dt dt dt dt dEff d ff E max lvDP dEmax lv dEmax lvBARO 1 Eff E max lvDP E max lvBARO dt dt dt PASI 2011 - A. Bandoni 101