Susquehanna Health - Pennsylvania General Assembly
advertisement

Susquehanna Health
The art of caring. The science of healing.
Testimony before the
House Democratic Policy Committee
Rep. Michael P. Sturla, Chairman
Rep. Richard Mirabito, Co-Chairman
Pennsylvania House of Representatives
Public Hearing on
Impact of Medicaid Expansion in the Pennsylvania
Williamsport, PA
March 5, 2013
Testimony of
Charles J. Santangelo, Chief Financial Officer
Susquehanna Health
700 High St.
Williamsport, PA 17701
(570} 321-3171
csantangelo@susguehannahealth.org
1
Susquehanna Health
The art of caring. The science of healing.
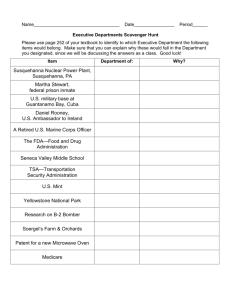
Good afternoon. My name is Charles Santangelo, and I am the Chief Financial Officer of
Susquehanna Health. On behalf of Susquehanna Health, I want to express my appreciation to you for
allowing us the opportunity to provide input on the impact on our institutions regarding the expansion
of the Medical Assistance program in Pennsylvania, under the provisions of the Patient Protection and
Affordable Care Act of 2010. What I would like to do for the next few minutes is to provide you with
background on our organization, our sources of funding, challenges in funding we face, and some
insight on impact of Medical Assistance and uninsured patients on the finances of our institutions.
First of all, Susquehanna Health is a not-for-profit health system headquartered in Williamsport.
The System was formed in 1994 with the consolidation of three (3) hospitals and two (2) medical groups
Into one fully integrated healthcare system - with a mission to provide high quality, compassionate,
accessible and cost effective health care to the residents in the region. Most recently, Laurel Health
System, in Tioga County, became part of Susquehanna Health, and System now operates 4 hospitals, 2
nursing homes, 2 personal care homes, an expanded homecare and hospice operation, an EMS
company, and employs approximately 200 physicians and physician extenders. The System operates the
only acute care hospitals in lycoming and Tioga Counties, with 332 licensed beds, 80,000 emergency
department visits each year and delivers 1,700 babies in the two maternity centers being operated by
the hospitals. Susquehanna Health Hospitals have been honored by such organizations as The Leapfrog
Group, HealthGrades, Truven (formerly Thomson Reuters) and Blue Cross for our commitment to quality
outcomes and patient safety.
The System provides the opportunity for medical students from urban settings to gain hands-on
experience in a rural setting through affiliations with medical schools such as Temple University, Drexel
2
Susquehanna Health
The art of caring. The science of healing.
University, Penn State- Hershey, and the Philadelphia College of Osteopathic Medicine. In 2007,
Susquehanna Health entered into an Academic Affiliation with The Commonwealth Medical College,
based in Scranton, whereby Susquehanna Health has become the western campus for the medical
school. This newly created affiliation is contributing to the success of the State's newest medical school.
Susquehanna Health also includes a growing physician group practice providing physician
services to the patients within our region. Through the group practice, the System looks to recruit new
physicians to the area, often replacing independent physicians who are retiring from practice. Besides
recruiting physicians, the group practice allows Susquehanna Health to fulfill its mission of providing
care for community residents, regardless of their insured status.
Given the accumulation of resources, Susquehanna Health has become an economic engine for
the communities in which we operate, with the employment of 3,500 employees and with an annual
payroll of $215 million.
Servicing patients from an 11-couty region, Susquehanna Health offers a wide array of nationally
recognized inpatient and outpatient services including cancer care, heart and vascular care, orthopedics,
infectious diseases, a certified stroke center, inpatient and outpatient rehab, home care and hospice.
The Williamsport Regional Medical Center, our flagship hospital, is the largest of the four {4) hospitals,
and provides a wide array of general acute care hospital services. The Medical Center's Emergency
Department is listed by the Department of Health as being one of the top 25 busiest in the state. 40% of
the patients seen in the Emergency Department are Medical Assistance patient and another 11% are
uninsured. The Medical Center also operates a 21-resident Family Medicine Residency Program. The
Clinic operated by the Residency program sees 18,000 patients per year with over 70% of the patients
3
Susquehanna Health
The art of caring. The science of healing.
being Medical Assistance patients and 2% being uninsured. Clearly, a significant number of uninsured
patients obtain their care in the Emergency Department. rather than a physician office setting.
Susquehanna Health Hospitals provide services to patients whose care is covered from a variety
of sources. For the past fiscal year, SO% of the services provided were to patients covered by Medicare
or Medicare Advantage Plans. Unfortunately, when all the bills are collected, Medicare payments will
total approximately 77% of the actual cost of care provided to Medicare patients. That shortfall totals
$30.6 million, which had to be made up in some way for the Health System to remain financially viable.
This shortfall will grow another $2.5 million for Susquehanna Hospitals as the Federal Sequester is
implemented.
For the past fiscal year, 12%of the services provided at SH Hospitals were provided to Medical
Assistance patients. Again, when all the bills are paid, Medical Assistance will have paid only 49% of the
actual cost of care provided to Medicare patients. That shortfall totaled $16.1 million, which again had
to be offset in some fashion for the Health System to remain financially viable.
For the past year, only 2.6% of the services provided at SH Hospitals were provided to uninsured
patients. Again, when all the bills are mailed and collection procedures carried out, we expect actual
collections to represent 25% of the actual cost of care provided to uninsured patients. That shortfall is
expected to total $4.8 million, which will be reflected in bad debt expense and Charity Care expense,
and again has to be offset in some fashion for the Health System to remain financially viable. lfthe
Amish were not classified as "uninsured", the actual results would be even worse for this category of
patients.
4
Susquehanna Health
The art of caring. The science of healing.
On a combined basis, 65% of the services provided at SH Hospitals were provided to Medicare,
Medical Assistance and uninsured patients. Unfortunately, the combined payments for these services
will only total 70% of the actual cost of care provided. The combined annual shortfall is $51.5 million. So
in other words, providing care to 65% of our patients results in a financial shortfall of $51.5 million that
has to be absorbed bv the other 35% of our patients ........ a condition similar to practically all hospitals in
Pennsylvania!
Commercial insurance and managed care insurers and covered patients utilize about 35% of the
services of SH Hospital, but pay about 57% of the total revenues. Those payments are significantly
above the actual cost of care, and the mark-up or "cost shifting", as it is sometimes referred to, is
necessary to offset the combined shortfalls from Medicare, Medical Assistance and uninsured patients.
"Cost shifting" is not new.... it has been occurring within Pennsylvania hospital pricing for
decades.... since Medicare went off cost reimbursement in 1985 and started underpaying hospitals for
the care to Medicare patients. Cost Shifting has been identified by the Pennsylvania Cost Containment
Council (PHC4) annual reports on the financial condition of Pennsylvania hospitals.
Two other methods for which hospitals and other providers attempt to offset government
payment shortfalls are: 1) to reduce operating costs and 2) to cut back on services, especially those that
add significantly to the shortfalls, i.e. highly subsidized services. Susquehanna Health employs regular
cost benchmarking and productivity methods for £!!.departments. We also constantly review our service
offering to determine if there is a more cost effective way to deliver care to our patients. In 2011, we
restructured an inner city outpatient clinic (with a 70% Medical Assistance service ratio) to an
independent Federally Qualified Health Center (FQHC). The FQHC is corporately independent from SH,
however SH has provided annual donations to the Center of $1.0-1.8 million. Because of financial
5
Susquehanna Health
The art of caring. The science of healing.
shortfalls, other decisions have been made in the past to cut back our service offering, but fortunately,
we have been able to limit those decisions.
In order to assist uninsured patients, the System contracts with a financial counseling firm to
provide Medical Assistance screening for all uninsured inpatients and outpatients requiring more
intensive services. The firm interviews uninsured patients and their guarantors to evaluate whether
they may qualify for the Medical Assistance Program. The firm's representatives are expert in the
Medical Assistance eligibility rules and categories, which are somewhat complicated. Many uninsured
patients do not qualify because their income exceeds maximum Income levels for their category. The
Income levels for various Medical Assistance categories are structured around the Federal Poverty
Guidelines, identified as follows:
2'l13 POYE.\l"t' Gl!ID[ll!or'tS fCA THL H.i COf'HICiU005 ST.t;,T'ES
A}~O TI1E. OiS.Ti!.K:'t cr li'JlV~· W\
Ptrsous ""'
fAr. u:·tJ~etn.ehc~d
P'ITe'll:rt)' ~~lint-
I
~
~ ll.i~O
-- .
-
I;, 510
3
Pl.'S
.3(•
...
I'J
Z3, 550
- ..
~
2?,HC•
...
(!
-';
- ..
~·
8
- ··-
..
~I . -~·;t:J
3·~.€.10
..
.. -·- .. --·
-· .
~·J •.:O~t)
·--
Fer- fJmllla:; households .....nt, lt)!r:\.• r:o.t.:w ~ r.••r·.a)u~.
-
-
;utd
~·1.1::
21.1
~ ur -t~;.,J, .:.:hliliun~I .::Hincn.
In addition to not meeting income requirements, patients are often disqualified for other reason, such
as:
Their assets exceed $3,200 (two people on GA, but medically needy)
6
Susquehanna Health
The art of caring. The science of healing.
Patient does not meet State residency requirement
Patient doesn't meet citizenship requirements or is not a qualified alien
Patient has an outstanding warrant for charges against them (that has not been satisfied)
Household composition disqualifies patient eligibility
In addition to not meeting specific requirements for Medical Assistance, some patients are not
compliant and simply do not follow through with the application process. They really do not care about
their lack of health insurance coverage and have no intent on paying the outstanding bills given to them
by the hospital or physicians. For the fiscal year ending June 30, 2012, 822 uninsured patients were
referred to the firm, with 469 or 57% qualifying for Medical Assistance. 353 patients did not qualify for
the reasons stated previously.
For our last fiscal year 2012, SH Hospitals in Lycoming County provided care for 445 inpatients
who did not qualify for any type of insurance coverage. The services provided included many medical
type cases, as well as high end specialty cases, including Cardiac Surgery, other Cardiac procedures,
Medical Oncology, Infectious Diseases, Endocrinology, Pulmonology, Stroke, Inpatient Rehab,
Neonatology and Psychiatry, which represented the largest percentage of inpatients. The total cost of
care to uninsured inpatients, net of any payments from patients or their guarantors, amounted to $2.1
million.
Also in fiscal year 2012, SH Hospitals In Lycoming County provided care for 19,351 outpatient
visits. Outpatient care was provided by most outpatient hospital departments however 63% of the total
outpatient services provided uninsured patients was provided in the Emergency Departments..... with
patients being treated and discharged. These patients are the most difficult to qualify for Medical
Assistance or for any type of coverage since their visit to the hospital is very brief and impractical for the
time requirement of conducting Medical Assistance application screening. Also, Federal EMTALA
regulations limit Emergency Department personnel in interviewing patients for insurance coverage or
self pay payment plans. As a result, Emergency Department bad debt write-offs from uninsured patients
are very high. The total cost of care to uninsured outpatients, net of any payments from patients or their
guarantors, amounted to $2.7 million.
The combined financial loss incurred in caring for uninsured patients in fiscal year 2012 was $4.8
million. If Medical Assistance income limits were expanded to 133% of the Federal Poverty Guidelines,
as identified in the Affordable Care Act, some ofthose self pay patients might have qualified. Assuming
7
Susquehanna Health
The art of caring. The science of healing.
50% of those patients qualified for Medical Assistance, SH Hospitals would have received additional
payments for inpatient and outpatient care of approximately $1.3 million....not enough to offset the loss
on uninsured patients, but certainly additional funding to help lessen the cost shifting to commercially
Insured patients. The additional funding would be provided from 100% Federal Medicaid funds for the
first three (3} years, so the added pavments to providers are not a "redistribution" of State dollars. but
rather an inflow of Federal dollars.
It should be noted that Williamsport Regional Medical Center receives approximately $2 million
in Medicare Disproportionate Share Hospital (DSH) payments. DSH payments are targeted to hospitals
which have a disproportionately high volume of poor patients (measured by the volume of Medicaid and
SSI patients) -the higher the volume, the higher the DSH payments. Under the ACA, as coverage is
extended to the uninsured population, DSH payments will be reduced under the assumption that there
will be more patients covered by Medicaid. If Medicaid expansion is not undertaken in Pennsylvania, it
is possible that the Medical Center will see a loss of part or all of the DSH payments and not see any
decrease in the uninsured population. This would be the experience of most hospitals located in urban
or rural areas with a higher than average level of poor residents.
Susquehanna Health Hospitals in Lycoming County are reasonably fortunate in that the county
has experienced economic improvement with development of Marcellus Shale. This has not "trickled
down" to the entire population, however and as of December 2012, the unemployment rate in
Lycoming County was 8.2%, higher than the statewide rate of 7.9%.
lycoming County Median Household Income, however, is very low, averaging only $42,163 16.1% lower than the statewide average of $50,221. As a result, the Poverty Rate for Lycoming County
1
is estimated to be 14.3% compared to the statewide rate of 13.7%
.
This statistic parallels the uninsured rate for the County which is estimated to be 13.1%,
compared to the uninsured rate for Pennsylvania of 10.1
2
•
Expanding the Medicaid enrollment in
Pennsylvania has to result in an improvement in the health status of citizens and the finances of local
providers and patients.
1
2
U. S. Census Bureau, Small Area Income and Poverty Estimates (SAIPE) Program, December 2012
U. S. Census Bureau, 2011 American Community Survey, Civilian non-Institutional population
8
Susquehanna Health
The art of caring. The science of healing.
As you can see, policy decisions made at the Federal and State levels directly impact the
financial condition of hospitals and other providers. Because of this direct financial impact, providers
have no other choice but react to such reductions through a combination of cost shifting or cost
reductions or service reductions.
Susquehanna Health looks to State Officials and the Secretary of the Department of Public
Welfare to sustain the Medical Assistance program. In Lycoming County, 18% of our residents are
covered by the State Medical Assistance Program according to the State MA rolls. Being the major
health care provider in the County, and the only full service general acute care hospital, Susquehanna
Health Hospitals rely on Medical Assistance coverage for our patients. In practically all cases, MA
payments are by far the lowest payment of all payers for similar cases (ruling out case complexity). The
payments however are much higher than payments from uninsured patients. For this reason, the
Susquehanna Health supports the expansion of the Medicaid Program in Pennsylvania In accordance
with the Affordable Care Act.
Several statements have been made indicating that Medical Assistance expansion will require
significant additional State funding. As providers, we are not privy to operational details and costs in
administering the State's MA Program. We would like to make several comments however about the
Department of Public Welfare "FACT SHEET: Medicaid Expansion and Pennsylvania".
The FACT SHEET indicates that " ... individuals currently eligible who have not enrolled
('woodwork') ... " would enroll when the Program is expanded because they would become more aware
of the enrollment process. This statement is a forecast of what might occur, but not a certainty. It
should be noted that the initiative to expand Health Choices throughout the state now places a
significant part of the operation of the Medicaid Program in the hands of selected managed care
9
Susquehanna Health
The art of caring. The science of healing.
organizations (HMO's and insurers). These companies already have an incentive to see that uninsured
individuals are aware of their potential benefits under Medicaid and will do their best to see that the
public is informed of the process. Additional enrollees in their plans will mean additional premium
funding- of which Federal participation will pick up about 56% of the added cost, instead of 100%.
Even with that said, the State should take some comfort in knowing that there is a group of
individuals (not insignificant) that will not follow the rules of the Medical Assistance application process,
even though they may qualify for coverage. The experience of Susquehanna Health Hospitals is that
over 10% of the uninsured, who were pursued for Medical Assistance applications, were not compliant
because they did not answer questions adequately or show up for scheduled appointments. There will
always be "woodwork" individuals who will want to stay in the "woodwork".
Another comment in the FACT SHEET is that " ... individuals that are currently insured but could
enter the program as a result of their employer dropping their insurance or a personal choice to drop
insurance ('droppers') because they would be eligible to enroll in benefits fully paid by taxpayers."
Again, this statement is a forecast of what might occur, but not a certainty. It should be noted that if
employers or individuals drop current coverage so that they could enroll in the expanded Medicaid
Program, the saving will accrue to Pennsylvania employers or citizens, with the cost being absorbed
predominately by the Federal Government. This would seem like a "win" for Pennsylvania and should
not be a deterrent to expanding the Medicaid Program under the Affordable Care Act.
Another point in the FACT SHEET indicates that the Medicaid Expansion will not include the
current state-only funded General Assistance medical benefits for adults who do not qualify for the
Federal Medicaid categories. The ACA expansion specifically excludes Medicaid expansion for those
categories of citizens already covered by state-only funded programs. The fact that the ACA expansion
10
Susquehanna Health
The art of caring. The science of healing.
does not address those already covered is not an objective of the law. The law's objective is to expand
coverage to those who are not already covered. The position expressed in the FACT SHEET is selfserving and does not acknowledge the purpose of the law ...to provide additional coverage to individuals
and therefore relieve the burden of the uninsured both to individuals and their communities.
The FACT SHEET provides other statements that seem very valid. There Is no question that the
State will pick up additional administrative costs to expand coverage for an estimated 800,000 new
enrollees. If that statement is accurate, that would be a 36% increase in enrollees. Given that
administrative costs are a small fraction of the total cost of covered individuals- probably around 5%10% - the increase in administrative costs should not be a deterrent to expanding the Medicaid Program
under the Affordable Care Act.
The 2013 - 2014 State Budget will be another very difficult process for State Officials and the
Legislature. The Governor has developed a proposed budget that reflects a 2.4% increase or $679
million in spending over the last year's general fund budget. With limited revenue enhancements,
lawmakers will need to deal with spending adjustments as way to balance the State Budget.
We in the hospital industry acknowledge that the Governor's proposed budget does not call for
significant changes to Medical Assistance inpatient payments, including special supplemental payments
for disproportionate share, medical education, and payments to burn centers, critical access hospitals,
obstetrics I neonatal services and trauma centers and uncompensated care payments to hospitals under
the tobacco settlement. The hospital community is committed to working with the Administration and
the General Assembly between now and June 30, to ensure the final details of the State Budget as it
relates to the regulation and payment of health care in the State of Pennsylvania. We believe that
11
_SusquehannaHealth
The art of caring. The science of healing.
Pennsylvania citizens will be best served in the coming months if these following three objectives are
accomplished:
1.
Preserve State Medical Assistance payment to hospitals and other providers, including all
supplemental funding;
2.
Enact legislation to re-authorize the Statewide hospital Quality Care Assessment and the
Philadelphia Hospital Tax, to maximize Federal matching funds in support of the existing
Medical Assistance Program; and
3.
Pursue full implementation of the Affordable Care Act, including the expansion of the State's
Medicaid Program for low-income Pennsylvanians.
That concludes my comments. I would like to thank the Committee for taking the time to visit
Lycoming County and providing an opportunity to share an opinion with you from the viewpoint of a
major health care provider for this region.
12