0021-972X/00/$03.00/0
The Journal of Clinical Endocrinology & Metabolism
Copyright © 2000 by The Endocrine Society
Vol. 85, No. 2
Printed in U.S.A.
A Population-Based Study of Chronic Autoimmune
Hypothyroidism in Danish Twins*
THOMAS HEIBERG BRIX, KIRSTEN OHM KYVIK,
AND
LASZLO HEGEDÜS
Department of Endocrinology M, Odense University Hospital (T.H.B., L.H.), and the Danish Twin
Register, Odense University (T.H.B., K.O.K.), DK-5000 Odense C, Denmark
ABSTRACT
Hashimoto’s thyroiditis (HT), atrophic thyroiditis (AT), and
Graves’ disease are autoimmune thyroid diseases in which genetic
factors are suspected to play an important role in disease susceptibility. In a recent population-based twin study we rendered it probable that a substantial part of the susceptibility to Graves’ disease is
attributable to genetic factors. At present there are no populationbased twin studies supporting such a genetic influence in the etiology
of HT/AT.
To elucidate whether there is a genetic influence in the etiology of
HT/AT, we studied the distribution of HT/AT in a population-based
sample of 2945 Danish female-female twin pairs (5890 individuals)
born between 1953 and 1972. Information on hypothyroidism was
obtained from a nationwide questionnaire survey in 1994. Information from hospitals, out-patient clinics, general practitioners, and
specialists was sought to verify the diagnosis.
The overall prevalence of autoimmune hypothyroidism was 0.41%
(24 of 5890). The prevalence did not differ between monozygotic and
dizygotic twins (0.42% and 0.40%, respectively). The crude probandwise concordance rates were significantly higher for monozygotic compared to dizygotic twin pairs: 0.55 (95% confidence interval, 0.23–
0.83) vs. 0.0 (95% confidence interval, 0.0 – 0.25; P ⫽ 0.01). All of the
healthy cotwins (n ⫽ 15) of twins with clinically overt autoimmune
hypothyroidism were biochemically euthyroid. Overall, regardless of
zygosity 53% (8 of 15) of the healthy cotwins were positive for antithyroid antibodies. The prevalence of autoantibodies among the
monozygotic cotwins was 80% (4 of 5) and 40% (4 of 10) among dizygotic cotwins (P ⫽ 0.36).
In conclusion, the higher concordance rate in monozygotic compared to dizygotic pairs indicates that genetic factors play a role in the
etiology of HT/AT among Caucasian women living in areas with borderline iodine deficiency. However, the fact that the concordance rate
among MZ twins was below 1 suggests that environmental factors
also are of etiological importance. (J Clin Endocrinol Metab 85: 536 –
539, 2000)
A
contribution of the genetic influence on disease susceptibility
largely remains to be defined.
In a recent population-based twin study we rendered it
probable that a substantial part of the familial aggregation of
GD is attributable to genetic factors (9). This is based on the
probandwise concordance rates being significantly higher in
MZ than in dizygotic (DZ) twins (9). Whether this is also true
for HT/AT, as suggested by observations in individual twin
pairs (10, 11), remains to be investigated. The present study
was undertaken to determine the concordance rates for autoimmune hypothyroidism in a cohort of Danish twins from
a nationwide population-based twin register.
UTOIMMUNE thyroid disease (AITD) comprises several clinical variants. Roughly, patients can be divided
into those with hyperthyroidism [Graves’ disease (GD)] and
those with hypothyroidism with [Hashimoto’s thyroiditis
(HT)] or without [atrophic thyroiditis (AT)] goiter. Although,
GD and HT/AT have very different phenotypes, it is generally believed that they share a number of common etiological factors. Clearly, GD and HT/AT frequently occur in
the same family, and some individuals progress from one
form to another (1, 2). Moreover, there are descriptions of
monozygotic (MZ) twin pairs in which one twin has GD and
the cotwin has HT/AT (3, 4).
The etiology of AITD seems to involve complex interactions among genetic, environmental, and endogenous factors
(5, 6). A role for genetic factors in the etiology is suggested
by the aggregation of AITD within families (1, 7, 8). In addition, recent studies indicate that a number of genetic markers with association and/or linkage with phenotypic AITD,
especially GD, may exist (2, 5, 6). However, the relative
Subjects and Methods
Subjects
The twins were recruited from the young part of the Danish Twin
Register. The ascertainment procedure of this nationwide populationbased register was described in detail previously (12).
The study population consisted of 2945 female same sex twin pairs
(5890 individuals) born between 1953 and 1972; both twins in a pair had
participated in a questionnaire survey in 1994. This questionnaire survey
was performed in all twins born between 1953 and 1982 as a part of a
nationwide project about health and psycho-social conditions among
twins. The response rate was 86%, and there was no difference in the
response rate across the birth cohorts. All of the respondents were
residents of Denmark, which is a nonendemic goiter area with borderline iodine deficiency (median urinary iodine excretion of 70 –100 g/
24 h) (13).
The screening questions for thyroid disease were the following. Do
you have or have you ever had hyperthyroidism, hypothyroidism, or
goiter? Informed consent was obtained from all participants, and the
Received October 13, 1998. Revision received June 25, 1999. Rerevision received October 18, 1999. Accepted October 22, 1999.
Address all correspondence and requests for reprints to: Dr. Thomas
Heiberg Brix, The Danish Twin Register, Odense University, Winsløwparken 15 st., DK 5000 Odense C, Denmark. E-mail: tBRIX@HEALTH.
SDU.OK.
* This work was supported by grants from the Agnes and Knut Mørks
Foundation, the Dagmar Marshalls Foundation, the A. P. Møller and
Hustru Chastine McKinney Møllers Foundation, the Novo Nordisk
Foundation Committee, and the Clinical Research Institute, Odense
University.
536
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 15:47 For personal use only. No other uses without permission. . All rights reserved.
AUTOIMMUNE HYPOTHYROIDISM IN TWINS
study was approved by all of the regional scientific-ethical committees
in Denmark (case file 96/150 PMC).
One hundred and fifty subjects indicated present or previous hypothyroidism. These subjects and their cotwins were sent a second more
detailed questionnaire in 1996. This questionnaire contained questions
about signs and symptoms of thyroid disease in general. The name and
address of the general practitioner, specialists, or hospitals attended by
the twin because of thyroid disorders were also requested. After 1
reminder, 108 subjects (72%) responded. In 84 subjects the presence of
autoimmune hypothyroidism was excluded, the main reasons being
errors when filling out the 1994 questionnaire (46 subjects) or other
thyroid disease (38 subjects). In 42 subjects (150 –108) verification of the
self-reported hypothyroidism as stated in the 1994 questionnaire was
impossible due to nonresponse to the 1996 questionnaire. However, in
an attempt to verify or exclude the presence of the self-reported hypothyroidism as stated in the 1994 questionnaire, information on thyroid
disease was sought from the National Discharge Register as part of a
record linkage between The Twin Register and the National Discharge
Register. Three of the 42 nonresponders (7.1%) were recorded in the
National Discharge Register with a thyroid-specific International Classification of Disorders, World Health Organization Code; one had thyroid cancer and two had postpartum thyroiditis with temporary hypothyroidism. The twin with thyroid cancer was not considered further.
The 2 twins with postpartum thyroiditis were both DZ (representing 2
discordant pairs). These pairs were also excluded from further consideration because they only had temporary hypothyroidism. Thus, a total
of 24 subjects (21 twin pairs) could be classified as having autoimmune
thyroiditis (7 HT and 17 AT). Table 1 gives the characteristics of these
subjects stratified by zygosity.
A diagnosis of autoimmune hypothyroidism was based on biochemical evidence of primary hypothyroidism and present treatment with
levothyroxine in combination with the presence of thyroid autoantibodies (microsomal or thyroid peroxidase and/or thyroglobulin; n ⫽
22). In the remaining two subjects (representing one concordant pair) the
diagnosis, at ages 30 and 32 yr, was based on biochemical primary
hypothyroidism requiring thyroid hormone replacement and a diffuse
hypoechogenic pattern of the thyroid gland by ultrasound. Unfortunately, antibodies were not measured initially, and both subjects are
antibody negative today. However, iatrogenic causes of hypothyroidism
were ruled out in both subjects.
Determination of zygosity was primarily based on self-reported answers to specific questions about similarity and mistaken identity, which
is a well established and valid method (14). Moreover, the zygosity of
the concordant pairs was verified by means of DNAtyping of nine short
tandem repeat systems with the PE Applied Biosystems AmpFISTR
Profiler Plus Kit (Foster City, CA) (15).
Analysis of data
In the classical twin study the comparison of the degree of concordance in MZ and DZ twin pairs indicates whether the disease is genetically influenced. A higher concordance rate in MZ than DZ pairs suggests that genetic factors are important, whereas similar concordance
rates in MZ and DZ pairs indicates an environmental cause (16). Concordance was assessed by the probandwise concordance rates, which
reflects the risk of disease for a twin given that the cotwin is affected (17).
This concordance rate can be interpreted as the prevalence of disease in
cotwins of probands and can be compared directly to the disease prevalence in the background population and to estimates of recurrence risks
537
in other types of relatives (17). The 95% confidence intervals (CI) for
concordance were calculated based on the binomial distribution.
Results
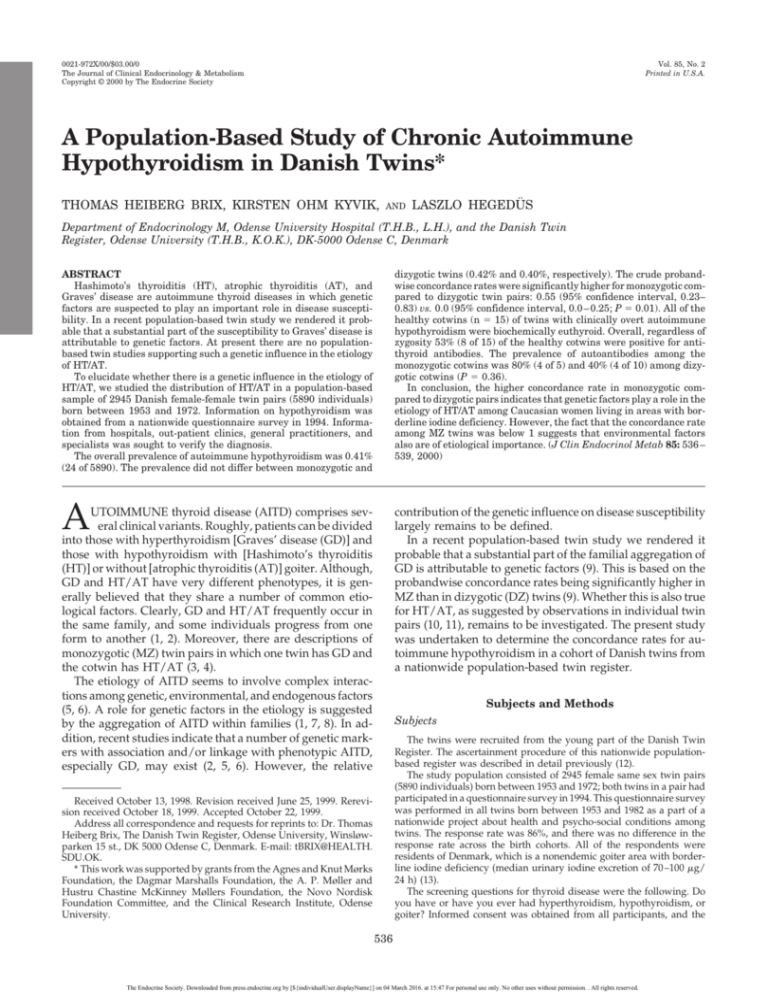
The overall prevalence of clinically overt autoimmune hypothyroidism was 0.41% (24 of 5890). The prevalence did not
differ between MZ and DZ twins (0.42% in MZ vs. 0.40% in
DZ). Results regarding concordance rates are summarized in
Table 1. There were 3 MZ and 0 DZ pairs concordant for
autoimmune hypothyroidism, giving a crude probandwise
concordance rate of 0.55 (95% CI, 0.23– 0.83) for MZ pairs and
0 (95% CI, 0.0 – 0.25) for DZ pairs (P ⫽ 0.01).
Among the 3 MZ pairs concordant for autoimmune hypothyroidism, the time from diagnosis in the first affected
twin until diagnosis in the cotwin was around 2 yr in 2 pairs
and 4 yr in the remaining pair. The follow-up period (time
span between disease onset in the proband and last contact
with the cotwin) tended to be lower in MZ than in DZ pairs
(Table 1). However, this difference was not statistically significant (5.5 vs. 7.7 yr; P ⫽ 0.42). In 2 of the 18 discordant pairs,
the cotwin to the twin with autoimmune hypothyroidism
had simple goiter. In both cases the cotwin was biochemically
euthyroid, and there was no evidence of coexisting autoimmunity, as the cotwins were antibody negative. In the remaining 16 discordant pairs the cotwin had no history of past
or present thyroid disease.
Prevalence of antithyroid antibodies in healthy cotwins
In 15 of the 18 discordant pairs, serum from the healthy
cotwin was available for analysis of antithyroid antibodies
(thyroid peroxidase and/or thyroglobulin). Due to emigration (1 pair) and unwillingness to give a blood sample (2
pairs) serum was not available in the remaining 3 pairs
(representing 3 DZ pairs). All of the healthy cotwins (n ⫽ 15)
to twins with clinically overt autoimmune hypothyroidism
were biochemically euthyroid. Overall, regardless of zygosity, 53% (8 of 15) of the healthy cotwins were positive for
antithyroid antibodies. The prevalence of autoantibodies
among the monozygotic cotwins was 80% (4 of 5) and 40%
(4 of 10) among DZ cotwins (P ⫽ 0.36).
Discussion
The complex nature of HT/AT has made the identification
of a possible susceptibility gene(s) problematic, and despite
several large investigations the pattern of inheritance and
major susceptibility genes have yet to be identified. It seems
likely that HT/AT, like other organ-specific autoimmune
TABLE 1. Characteristics and probandwise concordance rates for twins with autoimmune hypothyroidism
Mean age at
diagnosis
Zygosity
Monozygotic
Dizygotic
Mean follow-up of
cotwin
No. of pairs
Concordance rates
Yr
Range
Yr
Range
Concordant
Discordant
Probandwise
95% CI
28.2
30.0
21–34a
19– 40
5.5
7.7
3–10a
3–15
3
0
5
13 [15]
0.55
0.0
0.23– 0.83b
0.0– 0.25
The number in brackets includes the two DZ twins with postpartum thyroiditis found by record linkage between the Danish Twin Register
and the National Discharge Register.
a
Monozygotic vs. dizygotic, P ⬎ 0.40 by Mann-Whitney test (two tailed).
b
Monozygotic vs. dizygotic, P ⫽ 0.01.
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 15:47 For personal use only. No other uses without permission. . All rights reserved.
538
BRIX, KYVIK, AND HEGEDÜS
diseases, is polygenic, with no single gene being either necessary or sufficient for disease development. Most previous
studies of genetic factors in HT/AT have focused on human
leukocyte antigen genes, and there are significant, but weak,
associations with certain class II alleles that, on the other
hand, seem to vary between racial groups and even within
the same race (5). Furthermore, there is no evidence of linkage of HLA alleles and clinical HT/AT (5, 18). Thus, HLA
genes may increase susceptibility to HT/AT, but other genetic loci appear to represent major disease susceptibility
and/or severity factors. Other possible candidate genes, such
as the TSH receptor, CTLA-4, Ig heavy chain gene, and the
T cell receptor gene complexes, have recently been examined,
but no consistent associations have been demonstrated, and
linkage analysis has shown that these genetic loci do not
cosegregate with phenotypic HT/AT (18, 19). Thus, the influence, if any, of these new candidate genes in the etiology
of HT/AT seems at best weak.
The goal of this population-based twin study was to examine whether there is a genetic contribution to the etiology
of HT/AT. The higher concordance rate among MZ pairs
compared to DZ pairs indicates that genetic factors play a
role in the etiology of HT/AT, at least in women living in
areas with borderline iodine deficiency. However, the fact
that the concordance rate among MZ twins was below 1
suggests that environmental factors are also of etiological
importance. A detailed description of possible environmental factors in the etiology of autoimmune hypothyroidism is
beyond the scope of this article. Clearly, recent reviews point
toward certain infectious agents (20), smoking (21), and iodine intake (22) as some of the possible nongenetic factors.
Unfortunately, our twin cohort does not comprise enough
individuals with HT/AT to give a plausible estimate of the
relative influence of genetic and environmental factors in the
etiology of HT/AT. Moreover, it is important to point out
that our finding of a probandwise concordance rate of 0.0
among the DZ twin pairs reflects the small number of affected twins and not the lack of a genetic contribution to
HT/AT in DZ twins or siblings. In fact, according to the 95%
confidence interval, the concordance rate for the DZ twins
could lie anywhere between 0.0 – 0.25. Assuming that the
degree of familial aggregation in HT/AT is the same as that
reported in Graves’ disease (7), one would expect a probandwise concordance rate of 0.03– 0.06 among DZ twins,
which is clearly within the 95% confidence interval of our
concordance rate in DZ twins.
The prevalence of thyroid autoantibodies among young
Danish women is about 10 –15% (23, 24). In the present study,
however, as many as 80% of the MZ cotwins and 40% of the
DZ cotwins to twins with clinically overt autoimmune hypothyroidism were positive for thyroid autoantibodies.
Clearly, the prevalence of autoantibodies among the healthy
cotwins is much higher than that in the background population. This is consistent with the results of family studies,
which repeatedly demonstrate a much higher prevalence of
thyroid autoantibodies among first degree relatives of patients with autoimmune hypothyroidism than in the general
population (1, 25). This familial accumulation of thyroid
autoantibodies could be due to shared genes or shared environment within the family. Unfortunately, our twin sample
JCE & M • 2000
Vol 85 • No 2
does not comprise enough twin pairs to evaluate the precise
nature of the familial clustering of thyroid autoantibodies.
Our results should be interpreted in the context of a number of potential limitations. The data in this study were
obtained from Caucasian women living in Denmark, among
whom cultural background and living conditions are generally homogeneous. Thus, the results of this study cannot
uncritically be extrapolated to other groups or populations.
Although the Danish Twin Register is population based, our
final study sample is unlikely to be completely representative
of the entire twin population. Twins who did not answer/
return the questionnaires were not included. However,
based on record linkage between the Danish Twin Register
and the National Discharge Register, it seems unlikely that
twins with thyroid disease were less willing to answer/
return the questionnaires than healthy twins. Moreover, we
used the probandwise concordance rate. One of the great
advantages of this concordance rate is that it is independent
of ascertainment (26). Thus, it is not crucial that all twins be
studied, as long as there is no systematic bias in the ascertainment procedure.
The information on the presence or absence of hypothyroidism was based on self-reports. This may result in recall
bias. However, the diagnosis was confirmed by review of
medical records from hospitals, out-patient clinics, and general practitioners. Additionally, record linkage between the
Twin Register and the National Discharge Register did not
indicate a systematic underreporting of disease by twins
with hypothyroidism. In fact, the prevalence of confirmed
HT/AT in our study (0.42%) is comparable to that found in
women of a similar age group (⬍45 yr) in the Whickham
Survey (27) (The prevalence of HT/AT in Denmark among
women aged 20 – 40 yr is unknown.) The prevalence of
HT/AT was similar in MZ (0.42%) and DZ (0.40%) twins.
Thus, there is no evidence of overrepresentation of either
zygosity class and no evidence of any systematic bias in the
ascertainment procedure.
The follow-up period was not long in the healthy cotwins.
That is, not much time was allowed for the cotwin to develop
HT/AT, and hence, the concordance rates might be expected
to increase with increasing follow-up time. However, this is
a complex process, because new discordant pairs may also
appear with increasing follow-up time, and it seems unlikely
that such a potential increased concordance should be restricted to DZ compared to MZ twins. Indeed, the fact that
the follow-up time tended to be longer in DZ pairs in whom
concordance was lowest further strengthens our findings.
It could be argued that two of our patients did not have
autoimmune thyroiditis. In these subjects antibodies were
not measured initially, and both subjects turned out to be
antibody negative. However, 5–10% of patients with clinical
and ultrasound characteristics of chronic thyroiditis are thyroid antibody negative (28). Furthermore, it has repeatedly
been reported that treatment with levothyroxine in patients
with autoimmune thyroiditis can lead to a significant reduction in the serum concentrations of thyroid antibodies (29).
Additionally, iatrogenic causes of hypothyroidism were
ruled out in both subjects, making any other diagnosis highly
unlikely.
In conclusion, our data indicate that genetic factors play a
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 15:47 For personal use only. No other uses without permission. . All rights reserved.
AUTOIMMUNE HYPOTHYROIDISM IN TWINS
role in the etiology of HT/AT among Caucasian women
living in areas with borderline iodine deficiency.
References
1. Doniach D, Roitt IM, Taylor KB. 1965 Autoimmunity in pernicious anemia
and thyroiditis: a family study. Ann NY Acad Sci. 124:605– 625.
2. Tomer Y, Barbesino G, Greenberg DA, Conepcion E, Davies TF. 1999 Linkage
analysis of candidate genes in autoimmune thyroid disease. III. Detailed analysis of chromosome 14 localizes Graves’ disease-1 (GD-1) close to multinodular
goiter-1 (MNG-1). J Clin Endocrinol Metab. 83:4321– 4327.
3. Jayson MI, Doniach D, Benhamou Glynn N, Roitt IM, el Kabir DJ. 1967
Thyrotoxicosis and Hashimoto goitre in a pair of monozygotic twins with
serum long-acting thyroid stimulator. Lancet. 2:15–18.
4. Tani J, Yoshida K, Fukazawa H, et al. 1998 Hyperthyroid Graves’ disease and
primary hypothyroidism caused by TSH receptor antibodies in monozygotic
twins: case reports. Endocr J. 45:117–121.
5. Weetman AP, McGregor AM. 1994 Autoimmune thyroid disease: further
developments in our understanding. Endocr Rev. 15:788 – 830.
6. Brix TH, Kyvik KO, Hegedüs L. 1998 What is the evidence of genetic factors
in the etiology of Graves’ disease?–a brief review. Thyroid. 8:627– 634.
7. Stenszky V, Kozma L, Balazs C, Rochlitz S, Bear JC, Farid NR. 1985 The
genetics of Graves’ disease: HLA and disease susceptibility. J Clin Endocrinol
Metab. 61:735–740.
8. DeGroot LJ, Hall R, McDermott WV, Davis AM. 1962 Hashimoto’s thyroiditis: a genetically conditioned disease. N Engl J Med. 267:267–273.
9. Brix TH, Christensen K, Holm NV, Harvald B, Hegedüs L. 1998 A population
based study of Graves’ disease in Danish twins. Clin Endocrinol (Oxf). 48:397– 400.
10. Irvine WJ, Macgregor AG, Stuart AE, Hall GH. 1961 Hashimoto‘s disease in
uniovular twins. Lancet. 1:850 – 853.
11. Diamond MT, Joffe B. 1966 Monozygotic twins with chronic lymphocytic
thyroiditis (Hashimoto’s disease). JAMA. 198:182–183.
12. Kyvik KO, Green A, Beck-Nielsen H. 1995 The new Danish twin register:
establishment and analysis of twinning rates. Int J Epidemiol. 24:589 –596.
13. Rasmussen LB, Andersson G, Haraldsdóttir J, et al. 1996 Iodine. Do we need
an enrichment program in Denmark? Int J Food Sci Nutr. 47:377–381.
14. Hauge M. 1981 The Danish twin registre. In: Mednick SA, Baert AE, Bachmann
BP, eds. Prospective longitudinal research. An empirical basis for the primary
prevention of psychosocial disorders. Oxford: Oxford University Press; 217–221.
539
15. Perkin-Elmer Corp. 1997 User’s manual. Foster City: Perkin-Elmer Corp.
16. Hawkes CH. 1997 Twin studies in medicine–what do they tell us ? Q J Med.
90:311–321.
17. Smith C. 1974 Concordance in twins: methods and interpretation. Am J Hum
Genet. 26:454 – 466.
18. Tomer Y, Barbesino G, Keddache M, Greenberg DA, Davies TF. 1997 Mapping of a major susceptibility locus for Graves’ disease (GD-1) to chromosome
14q31. J Clin Endocrinol Metab. 82:1645–1648.
19. Barbesino G, Tomer Y, Conception E, Davies TF, Greenberg D. 1998 Linkage
analysis of candidate genes in autoimmune thyroid disease. I. Selected immunoregulatory genes. J Clin Endocrinol Metab. 83:1580 –1584.
20. Tomer Y, Davies T. 1993 Infection, thyroid disease, and autoimmunity. Endocr
Rev. 14:107–121.
21. Bertelsen JB, Hegedüs L. 1994 Cigarette smoking and the thyroid. Thyroid.
4:327–331.
22. Rose NR, Saboori AM, Rasooly L, Burek CL. 1997 The role of iodine in
autoimmune thyroiditis. Crit Rev Immunol. 17:511–517.
23. Feldt-Rasmussen U, Hoier MM, Rasmussen NG, Hegedus L, Hornnes P. 1990
Anti-thyroid peroxidase antibodies during pregnancy and postpartum. Relation to postpartum thyroiditis. Autoimmunity. 6:211–214.
24. Laurberg P, Pedersen KM, Vittinghus E, Ekelund S. 1992 Sensitive enzymelinked immunosorbent assay for measurement of autoantibodies to human
thyroid peroxidase. Scand J Clin Lab Invest. 52:663– 669.
25. Prentice LM, Phillips DIW, Sarsero D, Beever K, McLachlan SM, Rees Smith
B. 1990 Geographical distribution of subclinical autoimmune thyroid disease
in Britain: a study using highly sensitive direct assays for autoantibodies to
thyroglobulin and thyroid peroxidase. Acta Endocrinol (Copenh).
123:493– 498.
26. McGue M. 1992 When assessing twin concordance, use the probandwise not
the pairwise rate. Schizophrenia Bull. 18:171–176.
27. Vanderpump MPJ, Tunbridge WMG, French JM, et al. 1995 The incidence of
thyroid disorders in the community: a twenty-year follow-up of the Whickham
survey. Clin Endocrinol (Oxf). 43:55– 68.
28. Takamatsu J, Yoshida S, Yokozawa T, et al. 1998 Correlation of antithyroglobulin and antithyroid-peroxidase antibody profiles with clinical and ultrasound characteristics of chronic thyroiditis. Thyroid. 8:1101–1106.
29. Romaldini JH, Biancalana MM, Figueiredo DI, Farah CS, Mathias PC. 1996
Effect of l-thyroxine administration on antithyroid antibody levels, lipid profile, and thyroid volume in patients with Hashimoto’s thyroiditis. Thyroid.
6:183–188.
The Endocrine Society. Downloaded from press.endocrine.org by [${individualUser.displayName}] on 04 March 2016. at 15:47 For personal use only. No other uses without permission. . All rights reserved.