Journal of Exercise Physiologyonline
advertisement

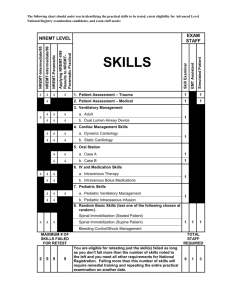
Aging, Ventilation and Cycle Exercise Time to Exhaustion 12 JEPonline Journal of Exercise Physiologyonline Official Journal of The American Society of Exercise Physiologists (ASEP) ISSN 1097-9751 An International Electronic Journal Volume 6 Number 1 February 2003 Systems Physiology: Cardiopulmonary AGE ASSOCIATED DECLINES IN EXERCISE TIME TO EXHAUSTION AND VENTILATORY PARAMETERS IN TRAINED CYCLISTS FRANK B. WYATT, JASON P. McCARTHY Department of Health, Human Performance, and Recreation, Baylor University ABSTRACT AGE ASSOCIATED DECLINES IN EXERCISE TIME TO EXHAUSTION AND VENTILATORY PARAMETERS IN TRAINED CYCLISTS. Frank B. Wyatt, Jason P. Mccarthy. JEPonline. 2002;6(1):1217. The purpose of this study was to investigate the cardiopulmonary parameters in a cross section of fit, aging cyclists to determine the associations between age, heart rate and ventilation on exercise time to exhaustion. Subjects were twenty-seven (N=27) males age 21 to 74 yrs. Each subject performed a maximal test on a cycle ergometer to volitional fatigue. Cardiopulmonary measures included; maximal oxygen consumption (VO2max, mL/kg/min, L/min), expired minute ventilation (VE, L/min), carbon dioxide production (VCO2, L/min), respiratory rate (RR) in breaths per minute (b/min), percent (%) O2 expired and % CO2 expired, ventilatory equivalents for O2 (VE/VO2) and CO2 (VE/VCO2), maximal heart rate (MHR, beats/min), ventilatory threshold (VT), heart rate threshold (HRT) and time to exhaustion (TE) in minutes (min). Through regression analyses with age as the independent variable, the following measures significantly declined with age: VO2, VE, VCO2, RR, MHR, VT, HRT and TE. Expired percent O2 and CO2, along with VE/VO2 and VE/VCO2 showed low coefficient values indicating little change between subjects with age. In conclusion, age decrements in cardiopulmonary related variables appear to be caused by diminished exercise capacities causing lowered maximal exercise intensities. The poor correlation between VE/VO2 and VE/VCO2 and age reveal that ventilatory capacities and function contribute little to the diminished exercise tolerance due to aging. Key Words: Aging, Exercise Tolerance, Hypercapnea, Ventilatory Threshold, Chemoreceptor INTRODUCTION With an increase in exercise intensity, there is an increased rate of ventilation (hyperpnea) facilitated by numerous neural and chemical mediators (1). The primary humoral mediators associated with exercise-induced increases in ventilation are increases in the arterial partial pressure of carbon dioxide (PaCO2) and decreases in blood pH (2). Whipp (3) has reported three phases of exercise hyperpnea. The initial phase is generally considered neurally mediated, while phases II and III are highly influenced by blood PaCO2 and H+ Aging, Ventilation and Cycle Exercise Time to Exhaustion 13 concentrations during prolonged and/or increased exercise intensity. This mechanism of ventilatory stimulation is a respiratory response to regulate acid/base balance (4). An increase in extracellular PCO2 decreases pH. By adjusting the PCO2 through increased ventilation the pulmonary system can effectively regulate the H+ concentration of the extracellular fluid (5). The onset of an exponential increase in ventilation during exercise in response to this regulation of H+ has been identified as the ventilatory threshold. During incremental exercise, the ventilatory threshold is sometimes detected through an exponential increase in expired volumes of carbon dioxide (VCO2) relative to VO2 (6). This is explained by the increase in arterial H+ and PaCO2, stimulating ventilation via the chemoreceptors in the carotid and aortic bodies (7). This hyperventilatory response dampens the extent of acidosis primarily through the reversal of the carbonic anhydrase reaction, resulting in proton (H+) and bicarbonate (HCO3-) conversion to carbon dioxide (8). With hyperventilation, there is a decrease in alveolar PCO2 and thus a compensatory fall in blood H+. Brooks et al. (5) notes that the hyperventilatory response increases pH in two ways: 1) by eliminating CO2 and thereby lowering blood PCO2, HCO3- and H+, and 2) by reducing CO2 as a denominator in the Henderson-Hasselbalch equation as follows: pH= 6.1+ log ([HCO3-] / [CO2]) Respiratory compensation due to metabolic acidosis allows for a decline in PaCO2, thus dampening the decrease in blood pH and offsetting fatigue. When elimination of CO2 becomes difficult through ventilatory constraints, alveolar and PaCO2 rise abruptly in spite of hyperventilation. There is a resultant accumulation of CO2 in the body (hypercapnea), which in turn further lowers blood pH and contributes to arterial hypoxemia and limitations in systemic oxygen (O2) transport and aerobic capacity (9). Should ventilatory constraints exist as with specific diseases and/or aging, resultant systemic limitations would facilitate decreased endurance and premature fatigue. Rossi, Ganassini, Tantucci and Grassi (10) reported that aging reduces lung elastic recoil , forced expiratory volume in the first second (FEV1) and increases residual and closing volume. Babb and Rodarte (11) studied aging subjects with normal pulmonary function and found reduced maximal expiratory flow indicating a loss of lung recoil. A reduced expiratory flow would hinder CO2 blow off, leading to a hypercapnic state and an earlier onset of fatigue. While evidence does indicate declines in myocardial function and an earlier time to fatigue with aging, questions remain as to the role specific ventilatory parameters and threshold measures play in this decline. In addition, while declines are evident, the rate of decline may vary in specific aging populations (i.e., fit versus unfit). Therefore, it is the purpose of this study to investigate the role of cardiopulmonary parameters in a fit, aging population on time to fatigue. METHODS Participants Subjects consisted of twenty-seven (N=27) male cyclists, age 21 y to 74 y. Prior to testing, each subject completed a medical/health questionnaire, the PAR-QTM Fitness Readiness questionnaire and signed an informed consent. The university Internal Review Board for Humans as Subjects approved all testing. The inclusion criteria required the subjects to utilize cycling as the primary mode of training. A minimum of four (4) days per week of cycle training was required with the stipulation that the training was being done for an "event". An event was defined as an organized cycling occurrence requiring formal registration. The subjects selected for inclusion were considered fit. Baseline values of height (cm), weight (kg), heart rate (beats/min), blood pressure (mmHg) and body-fat (3-site skinfold, %) were collected prior to exercise testing with the subjects in a rested state. Aging, Ventilation and Cycle Exercise Time to Exhaustion 14 Testing Procedures Subjects began the exercise testing with a warm-up on their bicycle set up on a cycle ergometer (VelodyneTM). Prior to testing, the ergometer was calibrated for power output measures. This was followed by an incremental workload test with the initial workload set at 50 watts (W), increasing 50 W every 3 min to volitional fatigue. Time to exhaustion (TE, min.) for each subject was recorded. The subjects were then allowed to cool down prior to de-briefing. Ventilatory and gas measures were collected continuously during the cycling protocol and data were averaged every 20 s utilizing a QuintonTM metabolic cart. Gas measures included the following: maximal oxygen consumption (VO2max, L/min, mL/kg/min), expired volume of minute ventilation (VE, L/min), expired minute volume of carbon dioxide (VCO2,L/min), breathing rate (RR, breaths/min), percent (%) O2 and %CO2 expired and the ventilatory equivalents for O2 (VE/VO2) and CO2 (VE/VCO2). Heart rate (beats/min) was continuously recorded and averaged every minute through electronic telemetry utilizing a PolarTM heart rate monitor. Ventilatory threshold (VT) was determined as the increase in VE/VO2 when ventilation outstrips oxygen consumption. This method showed high association with increased lactate and decreased pH during exercise (11). Ventilatory threshold was reported as VO2 in absolute terms (L/min) and in relative terms as a percentage of VO2max. Heart rate threshold (HRT) was identified as the point of disproportionate change in heart rate as the level of work expressed as VO2 increased proportionately. Statistical Analyses Descriptive statistics included mean, standard deviation, median and range. Simple regression analyses were utilized to determine correlations with age as the independent variable with myocardial and ventilatory parameters as the dependent variables. Through regression analyses, the slope or rate of change in measured variables across age was determined. Power analysis of the design indicated that an n-sample size of 15-22 yields high power of 0.8 to 0.95, respectively (13). Statistical significance was set a priori at p≤0.05. RESULTS Table 1: Descriptive data of the Subjects. Data for the mean, standard deviation (SD), Variable Median Range Mean± ± SD median and range of demographic information 42.5 21-74 Age (yr) 46.1±14.9 can be seen in Table 1. Ventilatory and heart 178 161.5-189 Height (cm) 178.3±7.7 rate measures across age with regression slopes 75.4 60.2-111.8 Weight (kg) 75.7±10.8 can be seen in Table 2. Maximal oxygen 11.5 4.8-19 Body fat (%) 11.5±3.6 consumption (VO2max), VCO2, VE, RR, MHR, VT (L/min), HRT (beats/min) and TE declined significantly (p≤0.05) across age. The measured variables of % O2 and % CO2 expired, VE/VO2, VE/VCO2, VT (%VO2max) and HRT (%MHR) were not significantly different across age. Ventilatory parameters measured within this study showed significant declines across age from 21 to 74 years (Table 2). However, the slope of decline in selected cardiopulmonary parameters was varied and did not necessarily profile the decline shown in TE (Figure 1). The ventilatory parameters of oxygen consumption and carbon dioxide production in absolute terms declined with age at a similar rate (Figure 2). Yet the rate of decline in expired ventilation (VE) was considerably greater (Figure 3). Aging, Ventilation and Cycle Exercise Time to Exhaustion 15 Table 2: Regression Analyses Between Age and Multiple Dependent Variables Pertaining to Ventilation, Heart Rate and Time to Exhaustion Variable R p Slope VO2max (mL/kg/min) -0.76 <0.0001 -.66 VO2 max (L/min) -0.73 <0.0001 -.05 VCO2 (L/min) -0.73 <0.0001 -.06 VE (L/min) -0.57 <0.002 -1.56 RR (beats/min) -0.58 <0.001 -.33 TE (min) -0.74 <0.0001 -.26 O2 expired (%) -0.19 =0.32 -.01 CO2 expired (%) -0.08 =0.70 -.002 VE/VCO2 0.29 =0.13 +.08 VE/VO2 0.29 =0.13 +.05 VT absolute (L/min) -0.63 <0.0004 -.04 VT relative (%VO2max) 0.16 =0.43 +.09 MHR (beats/min) -0.84 <0.0001 -.78 HRT absolute (beats/min) -0.72 <0.0001 -.75 HRT relative (%MHR) -0.13 =0.52 -.05 contributing factor to decreased TE with age. The reduced VO2 and VCO2 points to peripheral decline in oxygen consumption and carbon dioxide production, respectively. In addition, the MHR and absolute HRT measures allow for cardiovascular limitations with increased age (Figure 4). Higginbotham et al. (16) investigated the physiologic mechanisms of decline in aerobic capacity with an aging population. They found the age related decline in aerobic work performance resulted primarily from a reduced exercise heart rate when compared to peripheral oxygen utilization. This is consistent with the current research showing a greater rate of decline in MHR (-.78) and absolute HRT (-.75) than in relative VO2max (-.66) and absolute VT (-.04). DISCUSSION The current research indicates specific cardiopulmonary parameters decline with age. With the decline in these parameters there is an associated decline in time to exhaustion. The data indicate that that volume of gas exhaled is a contributing factor in time to exhaustion. McClaran, Wetter, Pegelow and Dempsey (14) examined expiratory flow limitation and it's effects on the ventilatory response during heavy exercise. They concluded expiratory flow limitations result in increased endexpiratory lung volume, reduced tidal volume, and inhibit respiratory motor output and ventilation. In the current study, the significant declines seen in VE and RR would reduce the effects of isocapnic buffering resulting in lowered pH, increased muscle fatigue and reduced time to exhaustion. Babb (15) concluded, in an investigation of mechanical ventilatory limitations with aging subjects, that at higher workloads mechanical ventilatory constraints inhibit VE. However, the non-significant changes in VE/VO2 and VE/VCO2 in the current study would indicate that ventilatory constraints were not the only 100 80 60 40 20 0 20 30 40 50 60 70 80 Age (y) VO2max (ml/kg/min) RR (b/min) TE (min) Figure 1. Mximal oxygen consumption, respiratory rate and time to exhaustion across age. Aging, Ventilation and Cycle Exercise Time to Exhaustion 16 7 6 240 5 200 4 3 160 2 120 1 80 0 20 30 40 50 60 70 80 40 Age (y) VO2 (L/min) 0 20 VCO2 (L/min) 30 40 50 60 70 80 Age (y) Figure 2. Asolute maximal oxygen consumption and carbon dioxide production across age. VE (L/min) TE (min) Figure 3. Expired minute ventilation and time to exhaustion across age. CONCLUSIONS 220 It is apparent that across the ages of this group (21-74 yrs), the cardiopulmonary variables 200 measured and time to exhaustion are shown to diminish. With aging it has been shown that 180 ventilation, cardiovascular and neuromuscular components are affected. Maharam et al. (17) in 160 studying the masters’ athlete found changes in 140 skeletal muscle, heart function and aerobic capacity. However, they note that declines with 120 aging may be attenuated with exercise. In the current study utilizing a fit population the rate of 100 20 30 40 50 60 70 80 decline varied across measures with significant slopes of decline highest in VE at –1.56 to a low Age (y) of –0.04 with absolute VT. This varies from past research indicating an overall approximate decline MHR (bpm) HRT (bpm) of 5% per decade (18). Yet studies to date have not compared different systems rate change across age. The current study utilizes a multi-variable Figure 4. Maximal heart rate and heart rate threshold across age. approach to physiologic declines associated with reduced time to exhaustion. Further studies are warranted to determine specific systems rate change related to the aging process and exercise performance. In conclusion, this study confirms the cardiopulmonary declines with fit, aging subjects and the associated effect on time to exhaustion. Aging, Ventilation and Cycle Exercise Time to Exhaustion 17 Address for Correspondence: Frank B. Wyatt, Ed.D., Department of Health, Human Performance, and Recreation, 500 Speight, P.O. Box 97313, Baylor University, Waco, TX 76798; Phone: (254) 710-3504; FAX: (254) 710-3527; Email: Frank_Wyatt@baylor.edu. REFERENCES 1. West, J.B. Respiratory Physiology-the essentials, 4th Edition. Baltimore:Williams & Wilkins, 1990. 2. Sutton, J.R., Jones, N.L. Control of pulmonary ventilation during exercise and mediators in the blood: CO2 and hydrogen ion. Med Sci Sports Exer. 1977;11 (2):198-203. 3. Whipp, B.J. Peripheral chemoreceptor control of exercise hyperpnea in humans. Med Sci Sports Exer 1994; 26 (3): 337-347. 4. Guyton, A.C., Hall, J. E. Textbook of Medical Physiology, 9th Edition. Philadelphia: W.B. Saunders company, 1996. 5. Robergs, R. A., Roberts, S. O. Exercise Physiology: Exercise, Performance, and Clinical Applications. St. Louis: Mosby Publishing, 1997. 6. Beaver, W.L., Wasserman, K., Whipp, B.J. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 1986; 60: 2020-2027. 7. Brooks, G.A., Fahey, T. D., White, T.P. & Baldwin, K.M. Exercise Physiology: Human Bioenergetics and Its Applications, 3rd edition. Mountain View:Mayfield Publishing Company, 2000. 8. Ganong, W.F. Review of Medical Physiology, 11th edition. Los Altos: Lange Medical Pubications, 1983. 9. McArdle, W.D., Katch, F.I., Katch, V.L. Exercise Physiology: energy, nutrition, and human performance, 5th Edition. Philadelphia: Lippincott Williams & Wilkins, 2001. 10. Rossi, A., Ganassini, A., Tantucci, C.,Grassi, V. Aging and the respiratory system. Aging 1996; 8 (3): 143-161. 11. Babb, T.G., Rodarte, J.R.. Mechanism of reduced maximal expiratory flow with aging. J Appl Physiol 2000; 89 (2): 505-511. 12. Farrell, S.W. and Ivy, J. L. Lactate acidosis and the increase in VE/VO2 during incremental exercise. J Appl Physiol 1987; 62 (4): 1551-1555. 13. Thomas, J.R., Nelson, J.K. Research Methods in Physical Activity, 3rd Edition. Champaign: Human Kinetics, 1996. 14. McClaran, S.R., Wetter, T.J., Pegelow, D.F., Dempsey, J.A. Role of expiratory flow limitation in determining lung volumes and ventilation during exercise. J Appl Physiol 1999; 86 (4):1357-1366. 15. Babb, T.G. Ventilatory response to exercise in subjects breathing CO2 or HeO2. J Appl Physiol 1997; 82 (3): 746-754. 16. Higginbotham, H.B., Morris, K.G., Williams, R.S., Coleman, R.E., and Cobb, F.R. Physiologic basis for the age-related decline in aerobic work capacity. Am J Cardiol 1986; 57 (1): 1374-1379. 17. Maharam, L.G., Bauman, P.A., Kalman, D., Skolnik, H., and Perle, S.M. Masters athletes: factors affecting performance. Sports Med 1999; 28 (4): 273-285. 18. Bortz, W.M. 4th; Bortz, W.M. 2nd. How fast do we go? Exercise performance over time as a biomarker. J Gerontol A; Biol Sci Med Sci 1996; 51 (5): M223-225.